1.5 Hypoxic-ischemic encephalopathy
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
Hypoxic-ischemic encephalopathy (HIE)
Serious condition characterized by a decrease in oxygenation to the organs (hypoxia) and abnormal blood flow to the organs (ischemia).
It is a significant cause of morbidity and mortality
20 to 30% of affected individuals dying during the neonatal period.
33 to 50% of survivors may experience significant long- term consequences or sequelae.
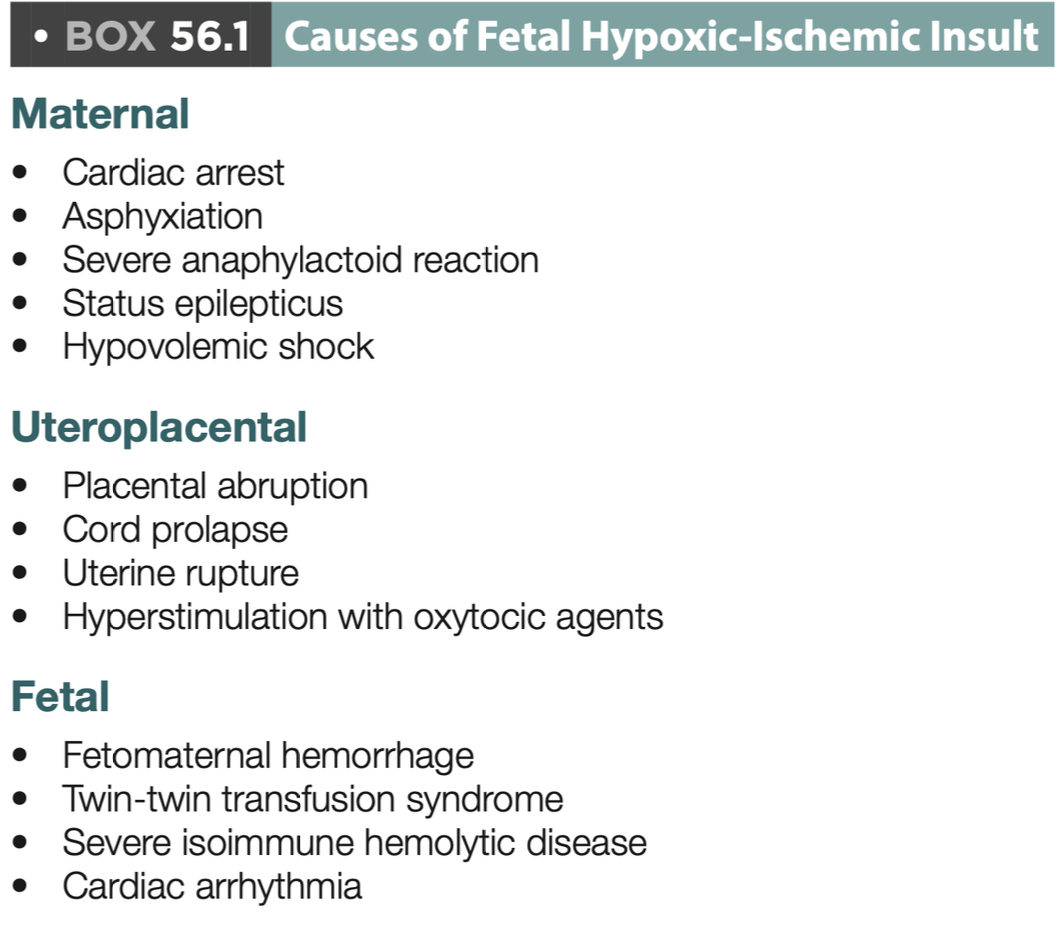
Etiology
Most cases are caused by perinatal events.
80% are due to acute injuries.
Less than 1% have prenatal injuries.
Maternal alterations
Inadequate blood oxygenation.
Low blood pressure.
Alteration in uterine relaxation.
Premature placental abruption.
Placental insufficiency.
Causes of fetal hypoxic-ischemic insult
Physiopathology during the normal course of pregnancy
Decrease in flow due to uterine contractions.
Decrease in oxygen to the fetus.
Increase in oxygen consumption.
Physiopathology after a hypoxic event
Anaerobic metabolism.
Increased lactate.
Electrolyte disturbances (Ca, Na).
Cytotoxic edema and neuronal death.
Physiopathology during complicated birth due to brief asphyxia:
Increased heart rate (HR), blood pressure (BP), central venous pressure (CVP).
Redistribution of cardiac output.
Physiopathology during complicated birth due to prolonged asphyxia:
Loss of cerebral vascular autoregulation.
Decreased cardiac output.
Decreased BP, HR.
Anaerobic metabolism.
Indicators of fetal hypoxia
Delayed growth with increased vascular resistance.
Alteration in heart rate.
Clinical manifestations during birth
Amniotic fluid with meconium.
Abnormalities in breathing.
Pallor, cyanosis.
Hypotonia.
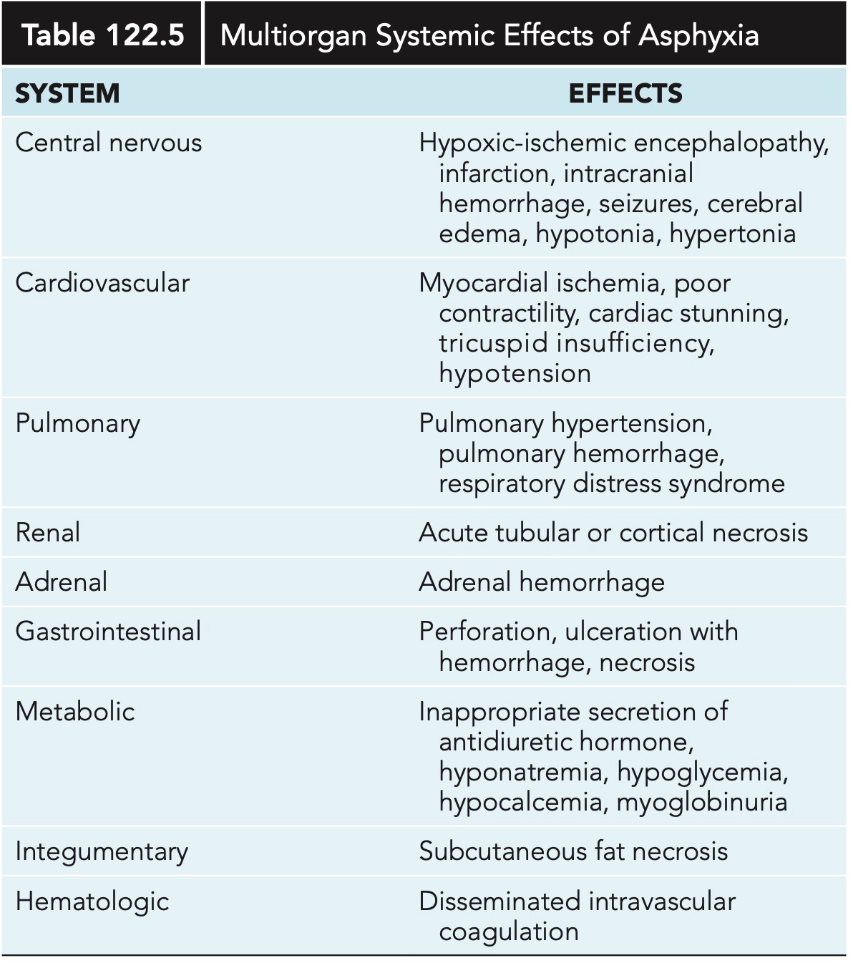
Clinical manifestations after birth
Cerebral edema (36 to 72 hours).
Seizures (20 to 50%).
Metabolic abnormalities (hypoglycemia, hypocalcemia).
Organ dysfunction (heart, kidneys, liver).
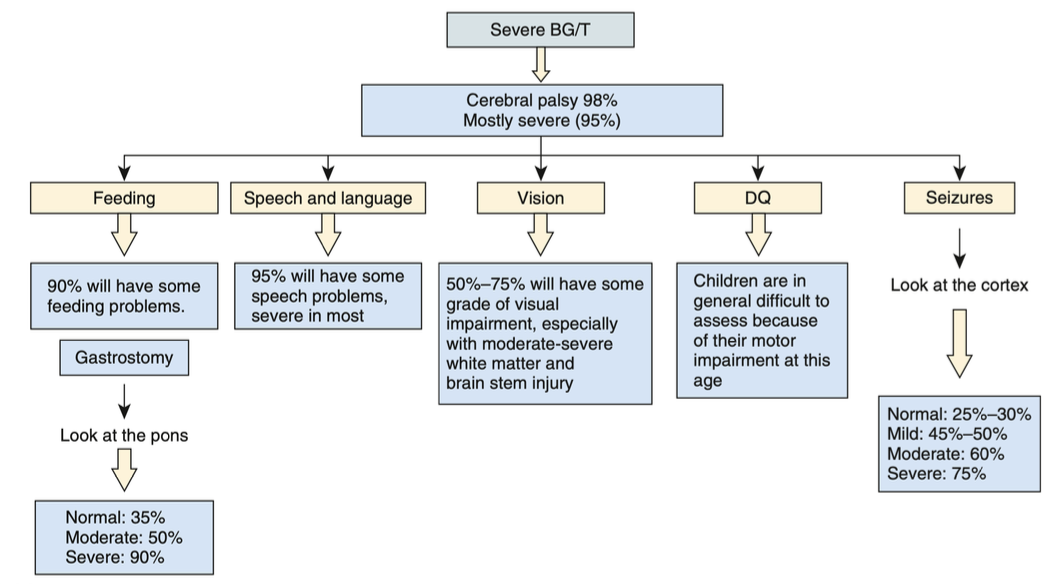
Multiorgan systemic effects of asphyxia
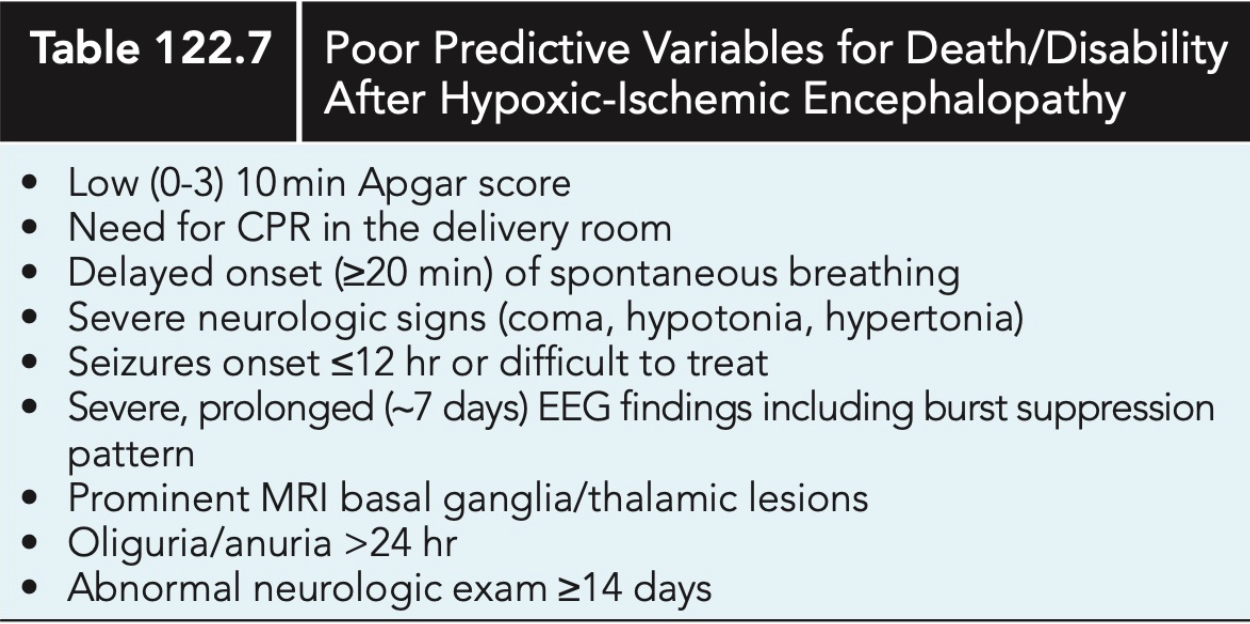
Predictive variables
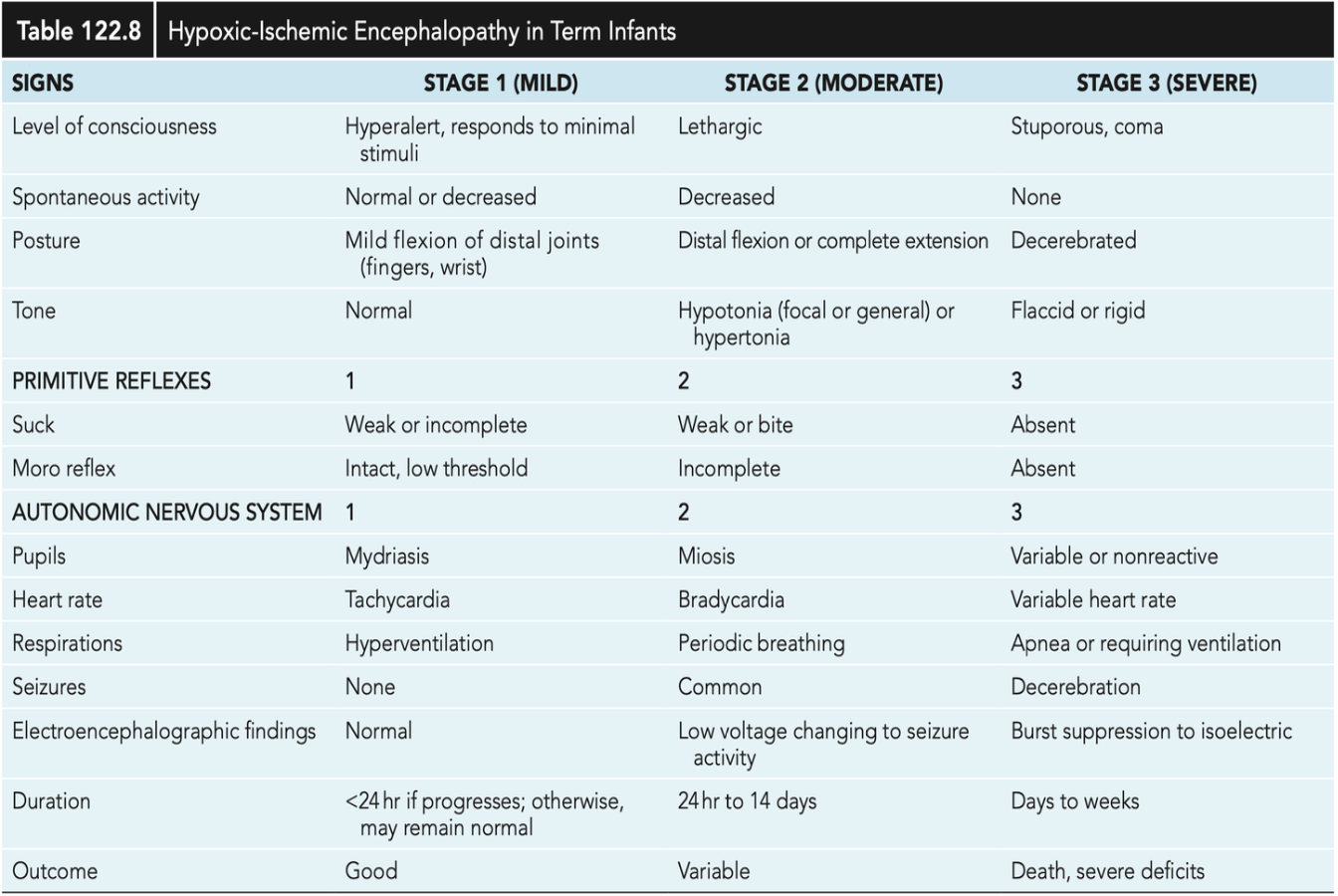
Stageification
When to suspect HIE?
Apgar score 0 to 3 at 5 minutes.
Umbilical cord pH < 7.0.
Neurological abnormalities
Multiorgan dysfunction.
MRI
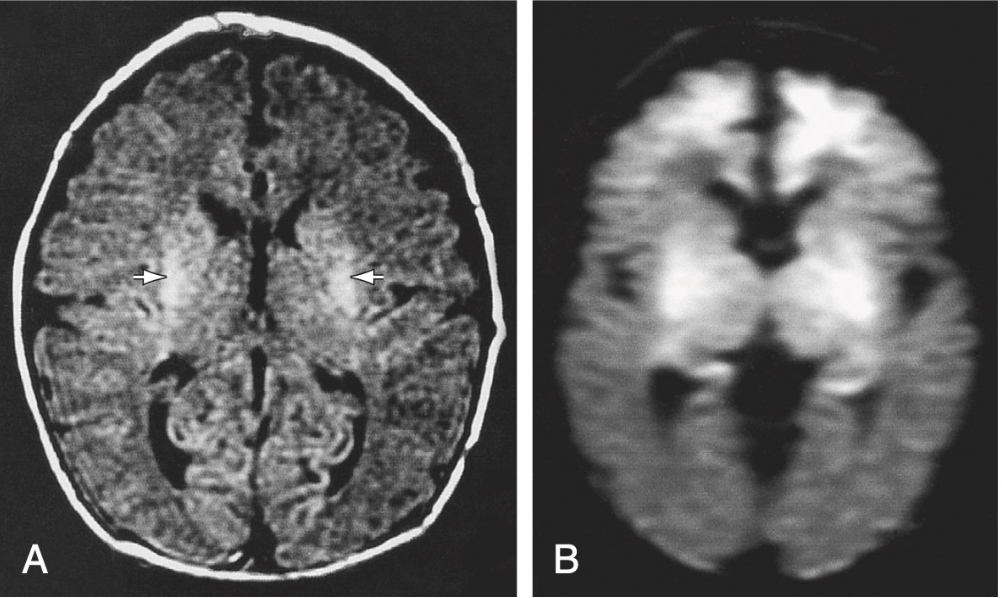
Most sensitive imaging method for detecting injury.
It will be performed within the first 3 to 5 days.
EEG
Helps determine which areas may have sequelae.
PPV 85% and NPV 91 to 96%.
Cardiac evaluation
Troponin I: 0-0.28 +/- 0.42 mcg/Lat 48 to 72hrs
Troponin T: 0-0.097 mcg/L
CPK MB: > 5 to 10%
Brain evaluation
CPK-BB: 12 hours of life
Renal evaluation
Elevation of BUN and creatinine: 2 to 4 days
Elevation of B-2 Microglobulin
Treatment
Therapeutic hypothermia.
33.5°C (to be initiated from 6 hours of life up to 72 hours).
Reduces morbidity and mortality.
Improves neurodevelopment at 18 months of life.
Less neuronal injury on MRI.
Decreases apoptosis and toxic products.
Seizures treatment
Phenobarbital (first-line).
Levetiracetam (second-line, increasingly used as the first option).
Supportive treatment according to the disturbance:
Adequate oxygenation.
Adequate perfusion (blood pressure).
Correction of acid-base status.
Correction of electrolytes.
Prognosis
Depends on how severe the hypoxia was.
pH < 6.7 has a 90% chance of death.
Apgar <3, lesions in the thalamus, severe HIE are associated with death and dysfunction.
Risk of cerebral palsy 5 to 10%.
Some survivors of perinatal asphyxia have problems in school.
Sarnat 2: 65 to 75% expected performance at 8 years old.