Drug Addiction
1/91
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
92 Terms
Addiction
biomedical disorder characterized by compulsive urge to use a substance or substances
Behavioral syndrome in which drug procurement and use seem to dominate the individuals motivation and where the normal constraints (Control) on behavior are largely ineffective. May or not be accompanied by the development go physical dependence on the drug (Bozarth)
Substance use disorder
Involving actions individuals continuously perform despite negative consequences
Cluster of cognitive, behavioral and physiological symptoms
Symptoms of SUDS (DSM-5)
Taking the substance in larger amounts or for longer than intended
Want to reduce substance use but not managing to do so
Spending increasing amounts of time procuring, using or recovering from substance use
Experiencing cravings and urges to use the substance
Having difficulty managing work/school and personal responsibilities
Continuing substance use despite causing relationship issues
Abandon social, occupational or recreational activities to use the substance
Continuing substance use despite repeatedly being placed in dangerous situations
Continue to use drugs when they know they have an existing physical or psychological issue can be exacerbated by substance use
Need more of substance to achieve desired effect (tolerance)
Developing withdrawal
2-9 psychological dependence
10-11 physical dependence
Mild: 2-3 symptoms
Moderate: 4-5 symptoms
Severe: 6+ symptoms
Intoxication
Alteration in consciousness, cognition, perception and behavior
Tolerance
Decrease in drug effect or increase in amount to achieve the same drug effect
Withdrawal
Symptoms, physical changes in physiology that are unpleasant
Physical Drug Dependence
Tolerance and withdrawal
Psychological Drug Dependence
obsession to acquire drugs and neglect other activities
Relapse
follows short or long period of abstinence
Overdose
died or could have died
Substance Use Disorder by WHO (ICD-11)
Must have 3 of 6
Have a strong desire or compulsion to take substance
Have difficulty in controlling when to take the substance, how much of the substance to take and when to stop using
Develop withdrawal
Needing more of the substance to get desired effect
Neglect other interest because time taken up by drug
Continue substance use even when harmful consequences
Meet category of harmful use, one must be met
Use of substance where impairment could be dangerous
Continue use despite of physical, psychological or cognitive issues
Detrimental behaviors and social problems related to use
All or none diagnosis
DEA Schedule of Drugs
Federal evaluation of the social effects (legality). Based on 2 factors
Is there medical use for the drug?
Abuse Potential: focus on abuse as harm, dependence liability/addiction liability
Policed by DEA
Regulated by congress with Controlled Substance Act (1970)
Schedule 1
No medical use/highest potential for dependence
heroin,
lysergic acid diethylamide (LSD),
marijuana (cannabis), 3,4-methylenedioxymethamphetamine (ecstasy)
methaqualone,
Schedule 2
Some medical use/highest potential for dependence
hydrocodone per dosage unit (Vicodin),
cocaine,
methamphetamine,
methadone,
hydromorphone (Dilaudid),
oxycodone (OxyContin),
fentanyl,
Adderall,
Ritalin
Schedule 3
Some medical use/ moderate potential for dependence
Codeine per dosage unit (Tylenol with codeine)
ketamine,
anabolic steroids,
testosterone
Schedule 4
Some medical use/ low risk potential for abuse/Rdependence
Xanax,
Valium,
Tramadol
Schedule 5
Some medical use/ lower risk potential for abuse/dependence
cough preparations with less than 200 milligrams of codeine or per 100 milliliters (Robitussin AC),
Lomotil,
Lyrica,
Route of Administration
A notable feature of drug effect lies in route of administration
Determine
How Fast
How Much
How Long
ROA: Oral or GI
How fast- one of the slowest, 30-90 min
How much- one of the lowest, high degrees of metabolism and excretion
How long- one of the longest
ROA: Transdermal (Skin)
How Fast: one of slowest 30min-24hr
How much: one of lowest, very long path, variable capillary access
How long: one of longest
ROA: Sublingual or Buccal (Nasal, Rectal, vaginal)
How fast: one of the slowest, 30-90 min
How much: one of the lowest, non-soluble barrier, time spread, metabolism, excretion
How Long: one of the longest 24hr
ROA: Injection (Subcutaneous (SC), Intramuscular(IM), intra-peritoneal (IP), IV and intracerebreal (IC)
How Fast: fastest IC>IV» SC = IM=IP
How much: Most IC>IV» SC = IM=IP
How Long: shortest IC>IU» SC = IM=IP
ROA: Inhalation (Smoking)
How Fast: one of the fastest, secondary to IC, equal to IV
How much: Close to most, 2nd to IC, = to IV
How Long: short, equal to IV
Concurrent Drug Use
the use of more than one drug over the past year, month or lifetime (exploratory)
Simultaneously Polydrug Use
Use of more than one drug at same time (combined or consecutively) over the past year, month or lifetime
extending or enhancing high or inhibiting side effects
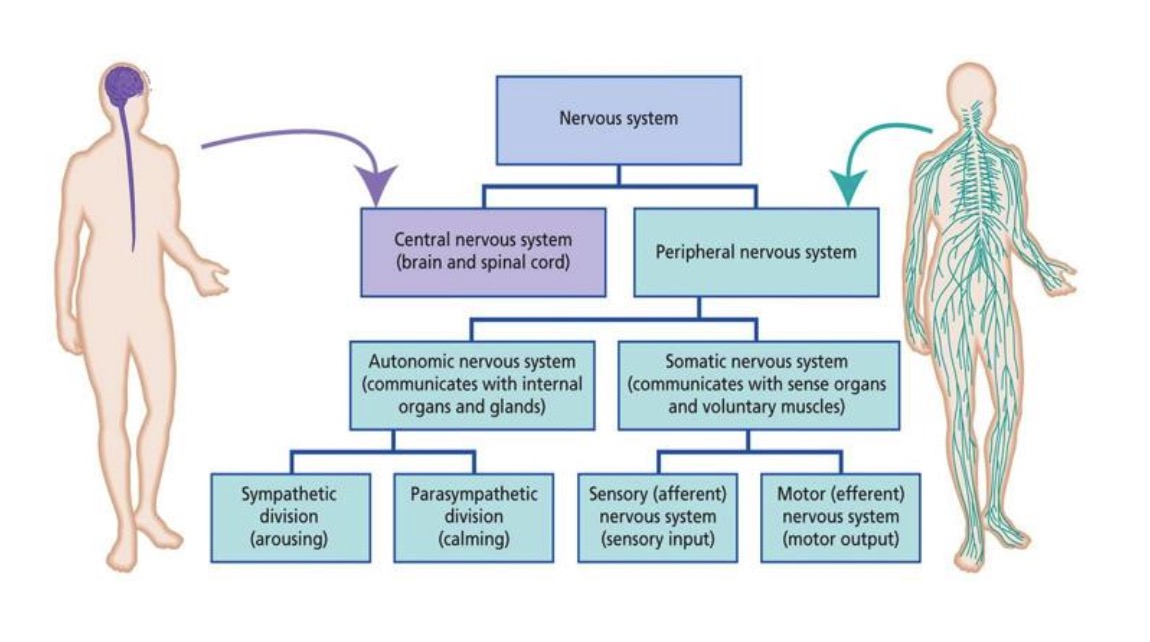
The Nervous System
3 parts, central, peripheral, enteric
Built on networks/pathways
CNS and PNS are connected
Interconnected like serial pathways
Basic unit of a pathway is a neuron
Enteric Nervous System
Digestive tract, muscular and mucousal parts, Each plexus has nodes of cell bodies (ganglia)
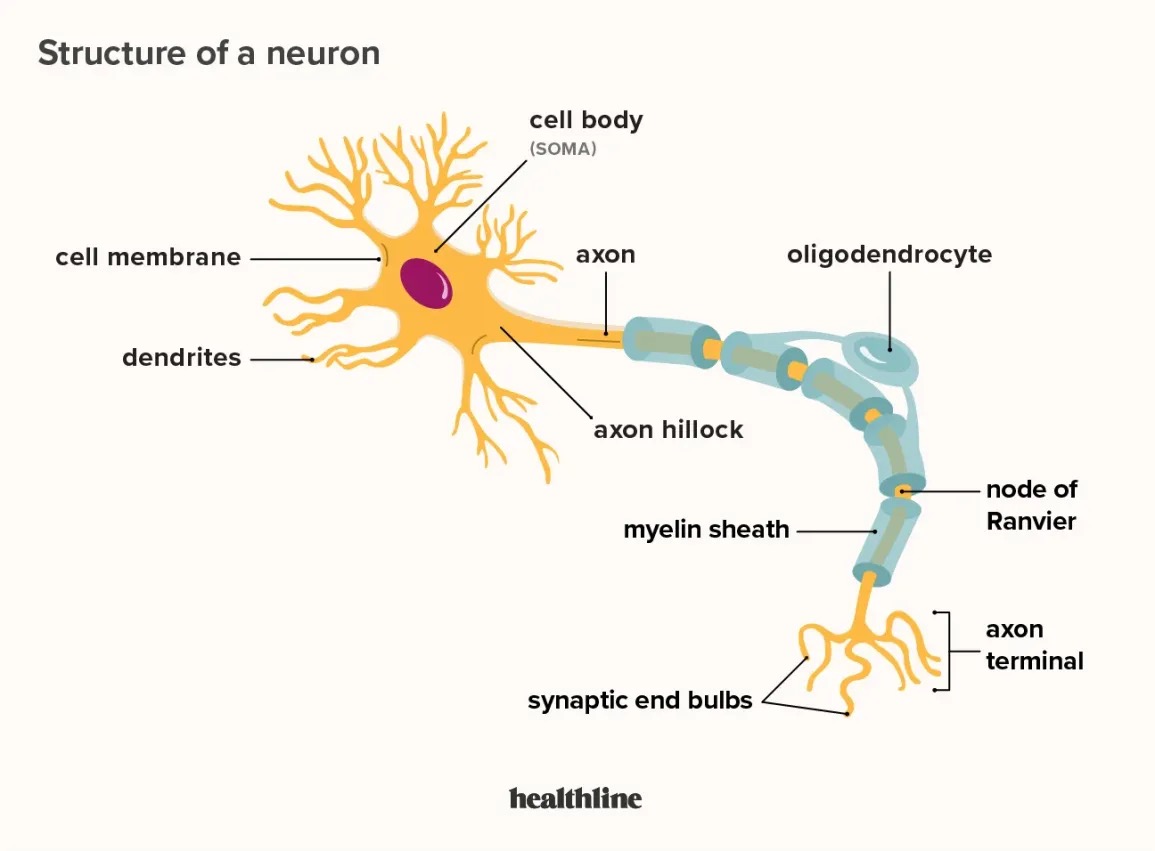
Neuron
Information processing.
Long and short distance communication
Connected into pathways by intercellular signals (neurotransmitters)
Sensory Neuron
specialized nerve cells that transmit sensory information from the body's receptors to the central nervous system (brain and spinal cord).
Motor Neuron
regulate voluntary and involuntary movements via transmitting signals from the brainstem and sensory systems to muscle cells.
Interneurons
the central nodes of neural circuits, enabling communication between sensory or motor neurons and the central nervous system (CNS)
Only in CNS
Local
Projection Neurons
Motor and sensory neurons (only in peripheral nervous system)
Afferent
Incoming projection
Efferent
Outgoing projection
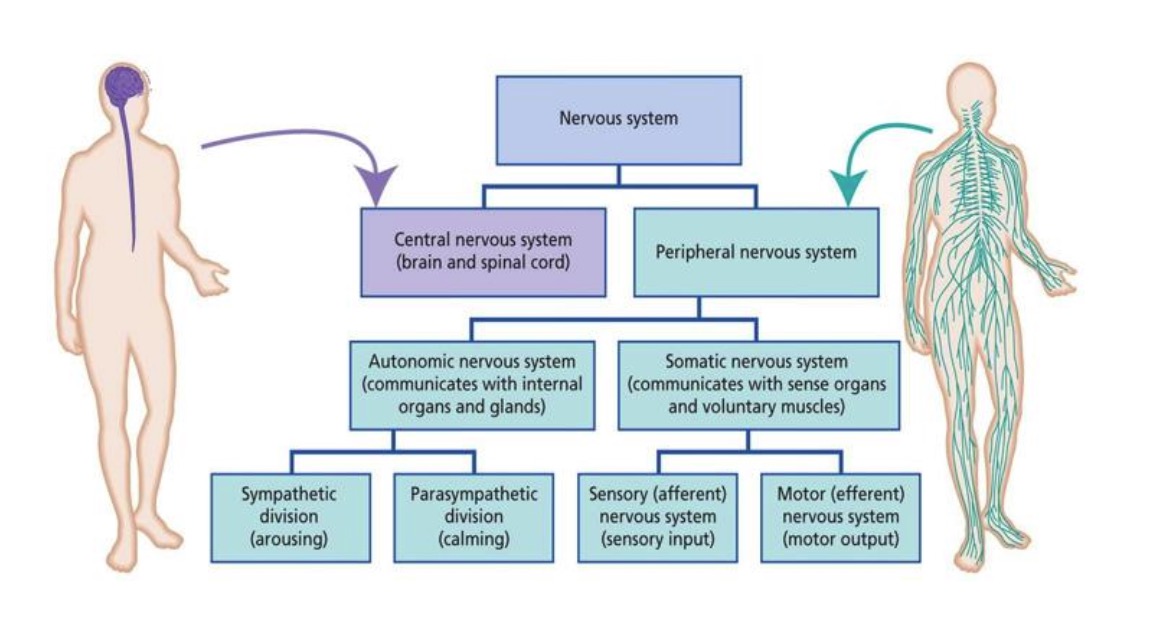
Somatic Nervous System
Connect Central Nervous System to skin, joints and bones (sensory) and striated muscle (motor)
Spinal nerves and cranial nerves
Each nerve contains 1 sensory (S) nerve and 1 motor nerve (M)
S uses glutamate as Neurotransmitter
M uses acetylcholine as neurotransmitter
Topographically organized- a spatial map
42 pairs of nerves (21 on each side of body)
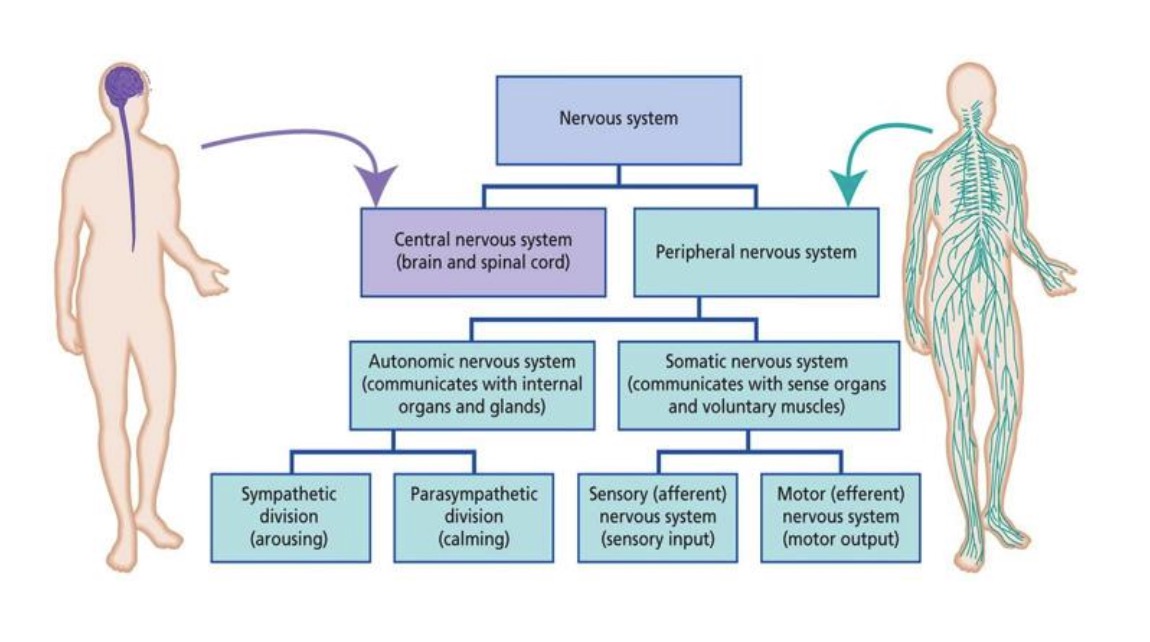
Autonomic Nervous System
2 systems Sympathetic and Parasympathetic
Connect to most organs
Sensory/motor neuron innervation targets vary
Sensory for hollow organs
Fewer ANS nerves
each nerve contains 1 sensory nerve and 2 motor nerves
Peripheral ganglia connect motor neuron 1 and motor neuron 2
Topographically organized but not very well, enter and exit different nerves
Sensory neurons use Glutamate
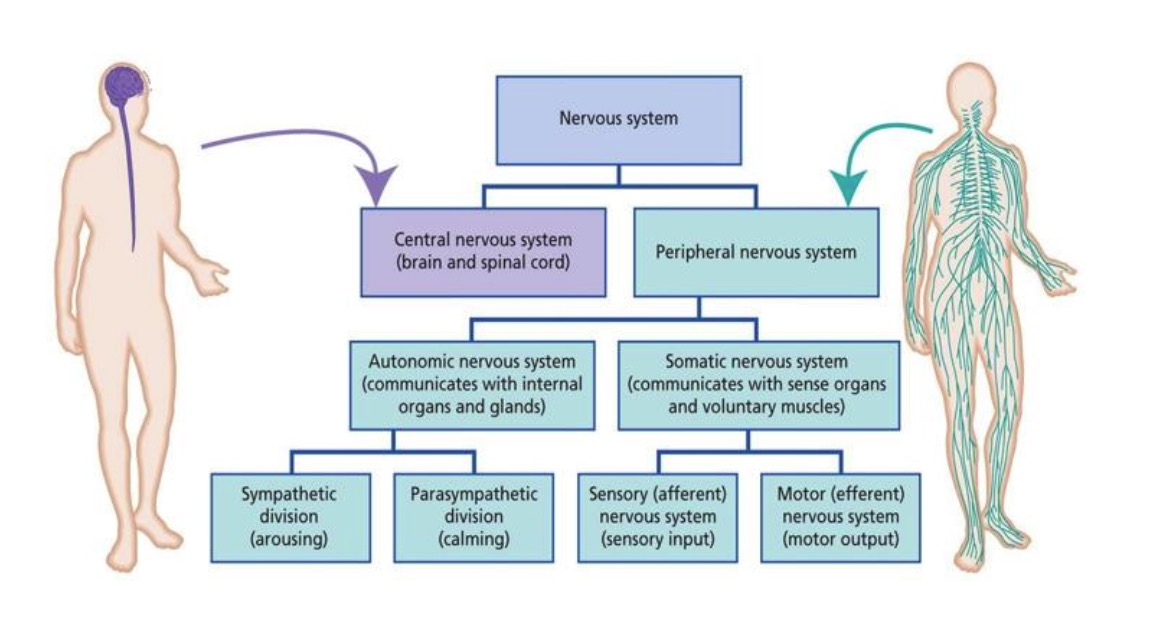
Sympathetic Nervous System
Motor contraction, sensory organ function and touch
Fight or flight
Sympathetic ganglia near spinal cord
Motor neurons use acetylcholine and then norepinephrine
Parasympathetic Nervous System
Motor relaxation, sensory-organ function
Rest and digest
Parasympathetic ganglia closer to organs
Motor neurons uses acetylcholine in both neurons
Vagus nerve, goes to every organ
Central Nervous System
the primary control center of the body, consisting of the brain and spinal cord. It receives, processes, and sends signals to coordinate all bodily functions.
In the CNS
Grey matter and white matter (myelinated)
Nuclei and tract
Interneurons (unmyelinated) and projection neurons (afferent and efferent, few myelinated)
Peripheral Nervous System
The peripheral nervous system is a network of nerves that runs throughout the head, neck, and body. It carries messages to and from the central nervous system (the brain and spinal cord).
In the PNS
Ganglia and nerves
None ———--Projection neurons (sensory and motor)
Glial Cells
Structure, support, communication
Act as barriers
Provide information to neurons
Help out with long and short distance communication in different ways
Astroycte, microglia, ogliodendrocyte, Schwann cell and ependymal cell
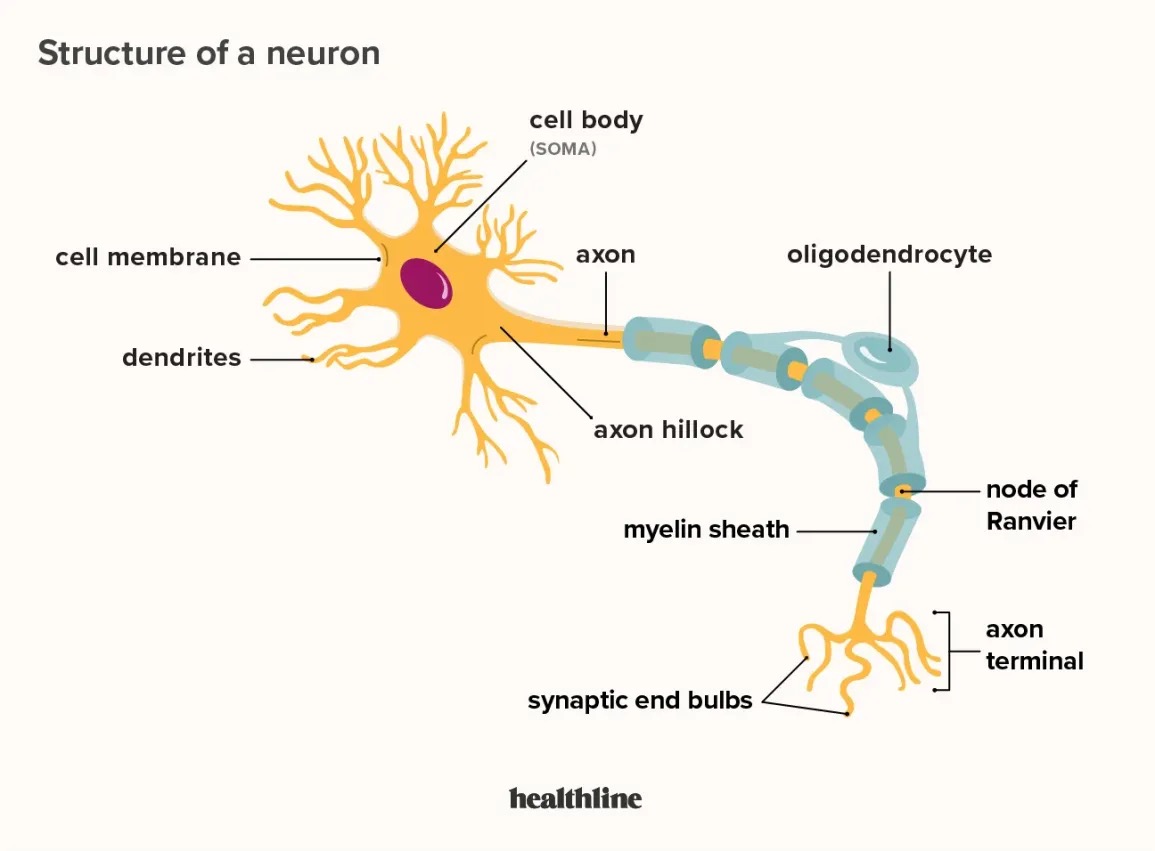
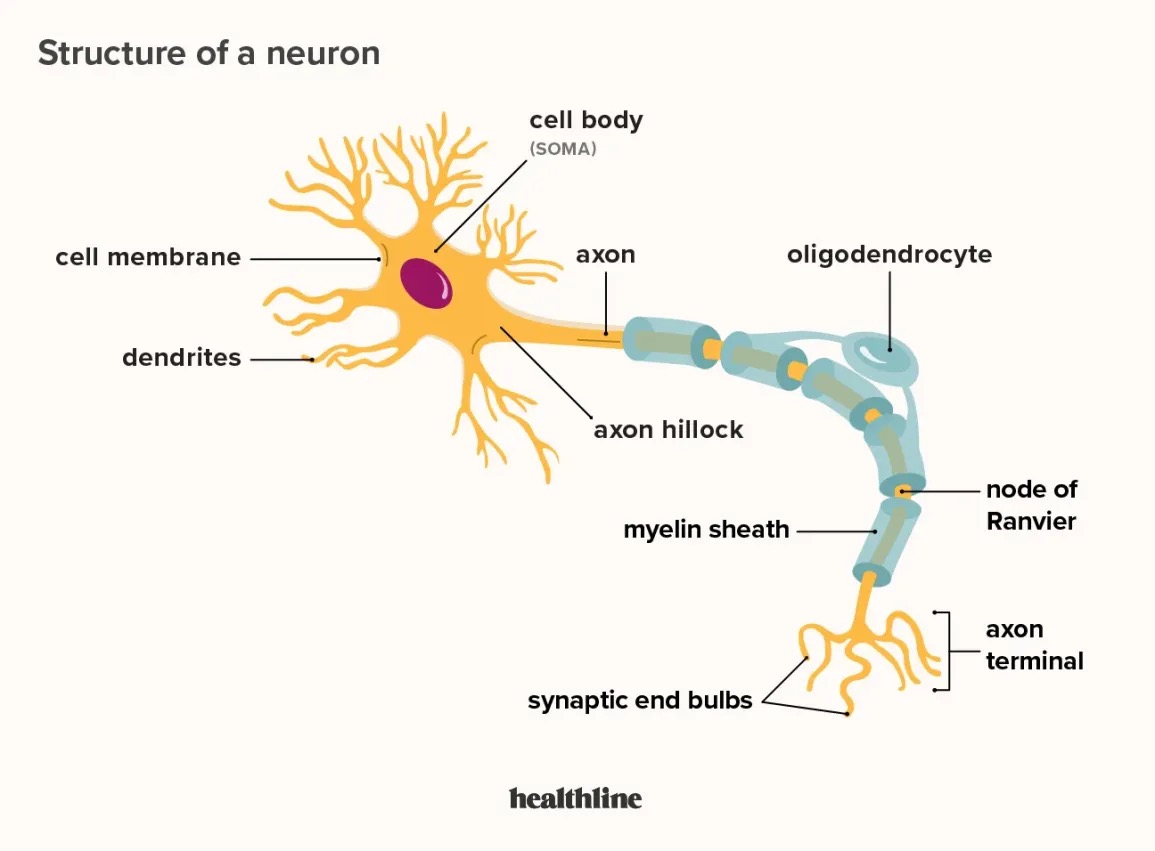
Cell Body
Function: listen and keep cell alive/integrate information
Includes:
Nucleus- protein recipes (DNA, Genes)
Mitochondria- gather, store and release energy
Rough Endoplasmic Reticulum- build proteins
Smooth Endoplasmic Reticulum-build/add on lipids
Golgi apparatus- local transport
Endosomes- recycle proteins
Lymsosomes- collect cellular waste
Microtubules and non-tubules- long distance transport
Receptors
Dendrites
Project off of cell body
-Dendritic spines contain receptors, spines can change
-Receptors
Function:Listen/integrate information
Excitatory
Activate cell activity (EPSP)
Inhibitory
Inhibit cell activity (IPSP)
Neurotransmitters
bind and activate the receptors
Are natural endogenous ligands that produce the intended and expected effect on the receptor
Receptors
Transmembrane protein embedded in phospholipid membranes.
receptors transduce biochemical message (neurotransmitter) into:
Bioelectric message
Another biochemical message
Ligand Gated Ionotropic Receptor (channels)
Different kinds, specific to charge and favor molecule.
Common ions are sodium (Na+), Chloride (Cl-), and Potassium (K). Fast and carry message
This receptors transduce. Carry forward- the ongoing message in the pathway
Lingand Gated Metabotropic Receptors (G-proteins)
Several kinds, most common is G-protein
Slow, tweak next message
G-protein receptors, 3 types Gs, Gq and Gi
Activate of inhabit enzymes that in turn activate a 2nd messenger (Neurotransmitter is the 1st messenger)
Each type activates a different 2nd messenger
These receptors help the post-synaptic neuron REMEMBER, important for memory
G-proteins structure has 3 parts: Alpha, Beta, Gamma
Receptor activation releases alpha—> biochemical domino effect
Gs
Alpha release is excitatory and activated adenyl cyclase enzyme
Adenyl cyclase increase cAMP (adenosine monophosphate) which is the 2nd messenger
Function:
1. Opens sodium (Na+) channels that can detect cAMP.
Activates PKA protein (protein kinase A) another enzyme that changes biochemical activities
Gi
Alpha release is inhibitory and opposes Gs (inhibits ongoing adenyl cyclase activity)
Net consequence decrease cAMP 2nd messenger
Function: decrease all functions
Gq
Alpha release is excitatory and activates phospholipase c (PLC) enzyme
PLC increases PIP2 (Phosphatidylinositol,4, 5, bisphosphate) Changes biochemical activities
PIP2 activates IP3 (Inositol triphosphate) and DAG (diacylgycerol) both 2nd messengers that increase calcium (Ca++)
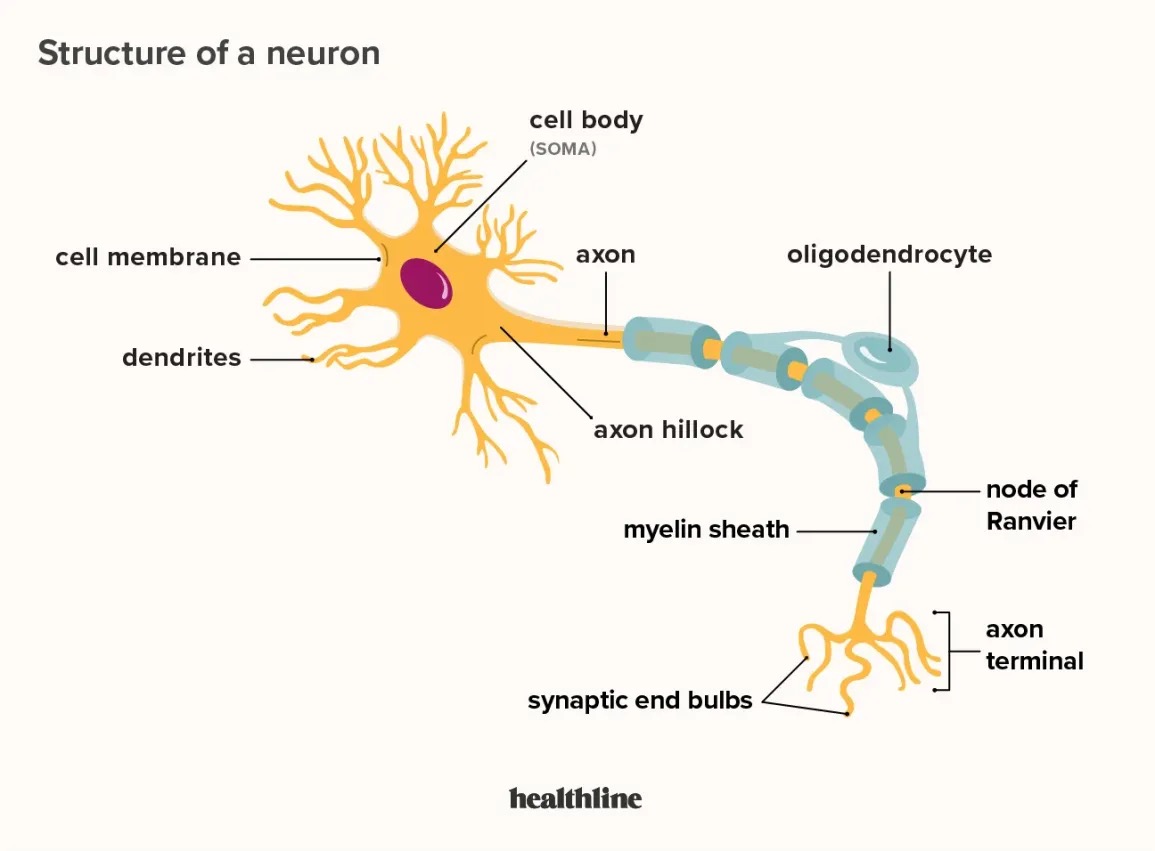
Axon
Projects to the next cell over short (interneuron) or long (projection neuron)
No dendritic spines
Myelin on many projection neurons
Tapered-thicker at beginning
The thicker part is the Axon Hillock- integration
Branchy ends branch out to multiple large branches
Specialized to regenerate bioelectric signals with great precision and machinery and messages (microtubules)
Function- integrate and transmit
Biochemical Transmission
Between cells (intercellular)
Involves presynaptic cell (axon terminal) where the message comes from to go to the post-synaptic cel
Action potentials collapse into graded potentials (EPSP) in axon terminals—→ calcium-gated channels (receptors)
Bioelectircal Transmission
Within cell (intracellular)
Secretory (Volumetric) Exocytosis
Larger vesicles
extrasynaptic space
Slower
need bigger Ca++ signal
Common
Fills up more space quicker
Synaptic Exocytosis
Smaller vesicles
Synaptic space
Fast
Needs less Ca++ signal
Unique/specific to one synapse
Drugs take synaptic exocytosis and make it more volumetric which can lead to addiction
Exocytosis
Neurotransmitters are stored in small sacs called synaptic vesicles.
When a neuron is active, a vesicle fuses with the cell membrane.
The contents of the vesicle are released into the synaptic cleft, the space between neurons.
Acetylcholine
Function- is important for controlling multiple processes in the peripheral nervous system, such as heart rate. One of its most important roles is controlling skeletal muscles.
Within the central nervous system, is important for keeping us alert and sustaining our attention, and it has been shown to be an important mediator of learning and memory.
Chemical Structure- Amine
Synthesis:- made from two things: the precursor choline and acetyl-coenzyme A. The enzyme choline acetyltransferase converts choline and acetyl-coenzyme A into Acetylcholine
Synthesis Location: Axon terminal
Receptors: Nicotine Receptors (Ionotropic)- Na+ channels, excitatory (EPSP)
Muscarinic Receptors (Metabotropic)- M1,M3,M5: Gq 2nd messenger, excitatory (activates IP3 and DAG)
M2,M4: Gi 2nd messenger, inhibits cAMP (pre and post synaptic)
Release: Synaptic
Stored: Vesicles via VAChTs
After Release: Extracellular: enzymatic degradation. an enzyme called acetylcholinesterase. Acetylcholinesterase breaks down acetylcholine into choline and acetic acid. Choline reuptake, acetic acid is excreted
Location in CNS: Basal forebrain and dorsolateral tegmental
Dopamine (DA)
Function- Reward learning, movement, executive functioning, arousal, motivation, lactation and nausea.
Chemical Structure- Catecholamine
Synthesis: from tyrosine
Synthesis Location: Axon terminal
Receptors: 1. All dopamine receptors are metabotropic.
- of D 1 and D 5 receptors, which are G s -coupled. Excitatory (activate cAMP 2nd messenger) The excitatory D 1 -like receptors are located on the postsynaptic neuron only,
- of D 2 , D 3 , and D 4 receptors, and they are G i -coupled and inhibit cAMP. D 2 -like receptors are located on both dendrites of the postsynaptic neuron and on the presynaptic neuron.
Release: Synaptic
Stored: Vesicles via VMATS
After Release:
- Extracellular: Reuptake via DAT
- Intracellular: Monoamine oxidase (MAOA/MAOB) and COMT, vesicularuptake by VMATS
Location in CNS: Ventral tegmental and substantial Nigra
Norepinephrine (NE)
Function- Fight or flight response. Norepinephrine is the major neurotransmitter of the parasympathetic nervous system. Prepares us to respond to a stressful situation. Vigilance, wakefulness, attention and memory.
Chemical Structure- Catecholamine
Synthesis: From tyrosine. Dopamine is a precursor to norepinephrine.
Synthesis Location: Axon terminal
Receptors: 1. Metabotropic Type: Peripheral Nervous System
- A1, B1: Gs excitatory (activate cAMP)
A2-Gi inhibitory (inhibits cAMP). Pre and post synaptic
Release: Synaptic
Stored: Vesicles via VMATS
After Release:
Extracellular: Reuptake via NET
Intracellular: Monoamine oxidase (MAOA/MAOB) and COMT, vesicular uptake by VMATS
Location in CNS: Locus coeruleus
Serotonin (5-HT)
Function- Control mood, sleep, appetite, bowel movements and nausea. Cognition. Mostly found in GI tract (ENS)
Chemical Structure- Indolamine
Synthesis: From tryptophan
Synthesis Location: axon terminal
Receptors: 1. Ionotropic Type: Only 5 HT3 receptor: Na+ channel
2. Metabotropic Type: Serotonin receptors are metabotropic
- Most 5-HT receptors are excitatory- Gs excitatory (activate cAMP)
- 5-HT 1 and 5- HT 5 families- Gi inhibitors (inhibit cAMP) both pre and post synaptic.
Release: Synaptic
Stored: Vesicles via VMATS
After Release: Serotonin Transporter (SERT)
- Extracellular: reuptake via SERT
- Intracellular: Monoamine oxidase (MAOA/MAOB) and vesicular reuptake by VMATS
Location in CNS: Raphe Nuclei
Glutamate
Function- Major excitatory. Learning and memory. Sensation, as many neurons transmitting information about vision, hearing and pain
Chemical Structure- Amino acid
Synthesis: Synthesized from the amino acid glutaminase. I
Synthesis Location: axon terminal
Receptors: Can bind to either metabotropic or ionotropic receptors
1. Ionotropic Type:
AMPA receptors, Na+ channel, excitatory pre and post synaptic.
l NMDA , Na+
NMDA receptors is that they are dependent on AMPA receptors to function. .
Kanic- Ca++ and Na+
2. Metabotropic Type:
- mGluR 1 and mGluR 5 , which are excitatory G q -coupled (IP3 and DAG) and located on the postsynaptic neuron.
- mGluR 2 and mGluR 3- Gi inhibitory (inhibits cAMP) pre and post synaptic
- mGluR 4 , mGluR 6 , mGluR 7 , and mGluR 8 . Gi inhibitory (inhibits cAMP) pre and post synaptic
- The Group II and Group III metabotropic receptors can function as heteroreceptors or as autoreceptors.
Release: Synaptic
Stored: Vesicle via VGluTs
After Release:
- Extracellular: Excitatory amino acid transporters EAATS take up glutamate into astrocytes
Intracellular (astrocytes):enzymatic degradation with glutamine synthetase
Location in CNS: - Transmission is everywhere
- Mostly projection neurons- move from nucleus to nucleus
- Cortico- brainstem pathways (descending) prefrontal cortex to monoamine nuclei in brain
- Cortico-striatal pathway (descending) prefrontal cortex to basal ganglia (cortico-accumbens and cortico-striatal)
- Thalamic- cortical pathway- (ascending) to all of cortex
- Cortico-thalamic pathway- (descending) from all cortex
- Cortico-cortico pathways- between columns in the cortex
· Glutamate part of cortico-striatal thalamic loop
GABA
Function- Major inhibitory in nervous system. Regulating release of other neurotransmitters. Specific roles in growth and sleep.
Chemical Structure- Amino acid
Synthesis: Synthesized from glutamate via glutamic acid decarboxylase
Synthesis Location: axon terminal
Receptors: 1. Ionotropic Type: GABA A five subunits. There are approximately 16 different possible subunits: six alpha, four beta, four gamma, one delta, and one epsilon. most GABA A receptors are composed of two alpha subunits, two beta subunits, and one gamma subunit. Once GABA has activated the receptor, the ion channel opens, allowing Cl- to enter the cell. This inhibits the neuron
2. Metabotropic Type: GABA B inhibitory These receptors are located on both the pre and the postsynaptic neurons. Inhibits cAMP, Gi
Release: Synaptic
Stored: Vesicles vis VGAT
After Release:
- Extracellular: reuptake using GAT
- Intracellular: enzymatic degradation GABA GABA transaminaseglutamate
Location in CNS: everywhere in CNS
- Interneurons- all CNS nuclei
- Projection neurons
o Subcortical to cortical (ascending)
o Cerebellar output (Purkinje cells)
o Subcortical projection neurons: Hippocampus, amygdala, striatum, hypothalamus, olfactory bulb
Endogenous Opioids (endorphins, enkephalins and Dynorphins )
Function- Pain reduction
Chemical Structure- peptide
Synthesis: Protein synthesis of large pro peptides cleaved in vesicles or extracellular to NT.
Synthesis Location: Cell body
Receptors: Metabotropic Type:
Mu: endorphin and enkephalin
Delta: endorphin and enkephalin
Kappa: dynorphin
NOP: Nociceptin
All Gi inhibits cAMP
- Gi couples and inhibit cAMP
Release: Secretory (volumetric)
Stored: Vesicles (propetide) stored in cell body and transported to terminal
After Release: Once released into the synapse, the endogenous opioids bind to their respective receptors before they are quickly metabolized.
- Extracellular: enzymatic degradation endopeptides
Location in CNS: - Mostly interneurons in CNS nuclei, and enteric NS
- One known projection neuron (b-endorphin): hypothalamus to brainstem nuclei and spinal cord.
Endocannabinoids (Anandamide and 2-AG)
Function- Appetite, pain suppression, motor control and cognition
Chemical Structure- Lipid
Synthesis: Cell membrane lipids using phospholipase D and C
Synthesis Location: Post synaptic membrane (intracellular)
Receptors: Metabotropic Type:
- CB 1 receptors are found primarily in the central nervous system, Gi inhibits cAMP
- CB 2 are located in the peripheral nervous system.
Release: Diffusional to extra and intracellular areas
- Intracellular: acts like a 2nd messenger, modifies activity of ion channels
- Extracellular: acts like a neurotransmitter (retrograde)
Stored: Not stored, on demand
After Release: Intracellular, Excess anandamide is degraded primarily by the enzyme fatty acid amide hydrolase (FAAH) into ethanolamine, but it can also be oxidized by other lipid metabolic enzymes
Location in CNS: CB1R dense at neocortex, hippocampus, basal ganglia, cerebellum, brainstem
Found in most cells
Adenosine
Synthesis: From AMP with 5-nucelotidase
Synthesis Location: axon terminal or synaptic cleft
Chemical Structure: Nucleoside
Storage: Not stored, on demand release, diffusional to extra and intracellular areas
- Extracellular: Adenosine mono phosphate (AMP) ecto-5-nucleotidase adenosine
- Intracellular: same using a soluble enzyme
Release: Intracellular, synaptic and volumetric, cellular transporter
Receptors: Metabotropic
- A1 (P1) or A3 (p3)- Gi inhibits cAMP, pre and post synaptic
- A2a-Gs activates cAMP pre and post synaptic
After Release: Reuptake through nucleoside transporter and enzymatic degradation into uric acid or changed to ADP recycle
Location: Hippocampus, cortex, cerebellum, less in striatum
Drug Action: Cocaine
Block transporters (reuptake) DAT> NET»> SERT
Directly impacts dopamine system
Drug Action: Methylphenidate
Block transporters (reuptake) DAT> NET»> SERT
Directly impacts dopamine system
Same as cocaine
Drug Action: Methamphetamine/ Amphetamine
Reverses cellular reuptake and vesicular transporters (VMATS). Stronger at VMATS (more release)
Directly impacts dopamine system,
DAT=NET»SERT
Increase neurotransmitter release thru cellular transporters, decrease reuptake
Also inhibits MAO activity
Drug Action: MDMA
everses cellular reuptake and vesicular transporters (VMATS). Stronger at VMATS (more release)
Directly impacts dopamine system,
SERT» DA=NE
Increase neurotransmitter release thru cellular transporters, decrease reuptake
Also inhibits MAO activity
Drug Action: Nicotine
AChNR agonist
enhances DA release in basal ganglia
Enhances glutamate release in basal ganglia→ glutamate increases DA activity
Drug Action: Opioids
Opiod receptor agonists
In the Ventral Tegmental nucleus (midbrain), inhibit GABA release which which “disinhibits” DA neuron activity. Increase DA release in basal ganglia
Indirect
Drug Action: Benzodiazepines and Barbituates
GABAa receptor modulators (potentiate GABAa receptor response to GABA)
In the basal ganglia, increase Dopamine, vis disinhibition
Indirect
Drug Action: Alcohol
Modifies the activity of many receptors depending on dos
indirect
Opioid receptor activation
Lower dose: potentiate GABA, receptor response to GABA and inhibit NDMA receptors
Higher dose: facilitate opioid receptor activation
Very high doses: disrupts the structure of the cellular brain so most receptors are disabled
Drug Action: Hallucinogens (LSD and Psilocybin)
5-HT2a agonists and MGlu2R
Serotonin increases DA release via 5-HT2a receptor, but not MGlu2r except possibly psychotic states
Indirect
Drug Action: Hallucinogens (Dissociative Anesthetics, Ketamine/PCP)
NMDA antagonists, noncompetitive
Seem to displace Mg++ (magnesium) and then not voltage sensitive
In basal ganglia (spinal cord), these drugs work on presynaptic NMDA receptors on GABA neurons—> decrease GABA release and increase DA and glutamate then glutamate can activate DA neurons
Indirect
Agonist
substance or drug that binds to a specific receptor in the brain and activates it, mimicking the effects of the natural neurotransmitter that normally binds to that receptor.
Antagonist
a chemical substance that blocks the activation of receptors on cells. This prevents a biological response.
Drug Action:Cannabis
CB1 Partial Agonist
increases DA by inhibiting GABA release
Drug Action: Inhalants
multiple mechanisms
Toluene- increases 5HT2a activity, GABA activity and decrease NMDAR activity
Drug Action: Caffeine
A1, A2a- competitive antagonists
enhances the sensitivity of dopamine receptors
Pharmacotherapies for Nicotine
Nicotine gum/patches- agonist therapy
All delivery at lower and slower dose
Vacreline (Chantix)- partial agnosts, agonist therapy
Bupropion (Zyban)- blocks DA and NE transporterrs and uncompetitive antagonists at the AChN receptor, enhance activity—> decrease dopamine
Rimonabant (Acompra)- off label, CB1 inverse agonist, decrease CB1 activity—> increase GABA activity—> decrease dopamine
Pharmacotherapies for Alcohol
Disulfiram (Antabuse)- blocks aldehyde dehydrogenase and the full metabolism of alcohol, leaving aldehyde dehydrogenase (TOXIC)
Naltrexone (revia)- competitive antagonist at opioid receptors, antagonist treatment
Acamprosate (Acampral)- NMDA competitive antagonist and GABA agonist
Bupropion (Zyban)- blocks DA and NE transporterrs and uncompetitive antagonists at the AChN receptor
Modafinil (Provigil)- weak DAT blocker-agonist treatment
Topiramate- inhibits voltage gated Na+ channels (inhibits AP) anti-seizure medication
Pharmacotherapies for Opioids
Methadone- agonist therapy, slower onset
Burprenorphine (Bupex)- agonist therapy
Partial agonist, stave off withdrawal but provides a weak high
Naltrexone- competitive agonist, antagonist therapy
Suboxone- buprenorphine and naloxone- antagonist therapy, administered sublingual
Dose of naloxone big enough to block receptor if injected but not if taken orally
Pharmacotherapies for Psychostimulants
Cocaine- D- amphetamine (meth) low doses, agonist therapy
Disulfiram- MAO inhibitor, fail to degrade DA so you have a bit more
Caffeine- coffee, tea, energy drinks, stave off withdrawal
Pharmacotherapies for Cannabinoids
Rimonabanat- off label, CB1 antagonist
Counteracts CB1 effects-antagonist therapy
Synthetic THC- agonist therapy
Naltrexone- competitive agonist
N-acetyclysteine- decrease glutamate activity and oxidate stress metabolism
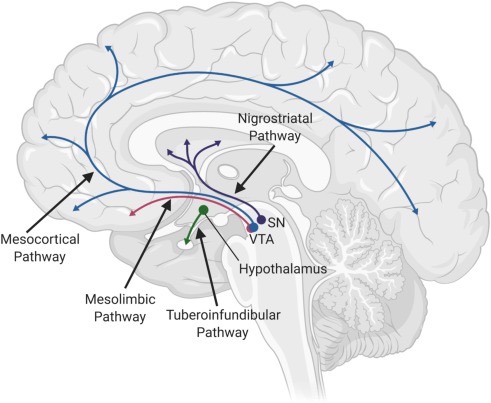
Nigrostriatal Pathway
Substantia nigra (midbrain) to dorsal striatum (basal ganglia)
Dopamine pathway
Dopamine Neural Pathways
Involved in reward
4 pathways
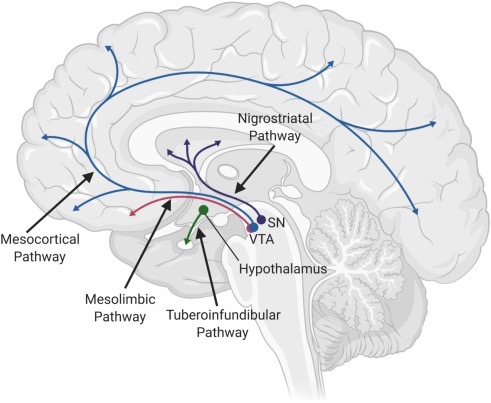
Mesolimbic Pathway
Ventral tegmental Area (midbrain) to nucleus accumbent (ventral stratum in basal ganglia)
Dopamine pathway
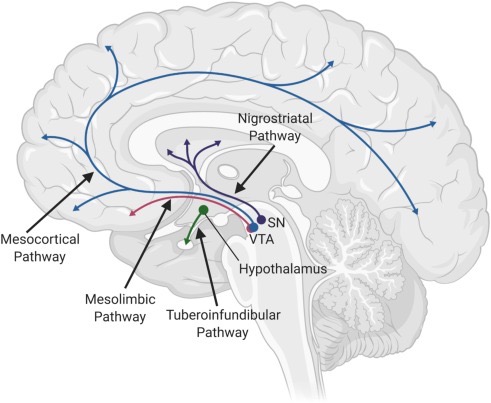
Mesocortical Pathway
Ventral tegmental area (midbrain) to prefrontal cortex
Dopamine pathway
Mesocorticolimbic Pathway
Paths 2 and 3 Mesolimbic and mesocortical pathways combined