Cells and Tissues
1/175
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
176 Terms
What is the correct order of the hierarchy of life from smallest to largest?
Cell → Tissue → Organ → Organ System → Organism
What is a cell?
A cell is the smallest functional unit that can perform all of life’s tasks.
Do cells live in isolation?
No, cells do not live in isolation. They are in direct contact with their neighbors (other cells or connective tissue). Points of contact between cells are called junctions.
What are the types of cell junctions?
Tight Junction – Seals cells together, preventing leakage (e.g., intestines)
Adherens Junction – Connects cells using actin filaments for strength (e.g., skin)
Desmosome – Provides strong adhesion using intermediate filaments (e.g., heart, skin)
Gap Junction – Allows direct communication between cells (e.g., heart, nerves)
Hemidesmosome – Anchors cells to the basement membrane (e.g., skin)
How are animal and plant tissues organized?
Cells are grouped into organized tissues, with their appearance and structure closely linked to function.
Different tissues have different roles depending on location:
Outer tissues → Contact with the environment (e.g., skin, epidermis)
Inner tissues → Line body cavities (e.g., intestine lining)
Middle tissues → Most tissues, performing various internal functions (e.g., muscles, vascular tissues)
Easily identifiable due to specialized structures.
What are the four basic tissues in plants?
Dermal Tissue
Ground Tissue
Vascular Tissue
Meristem Tissue
What are the four basic tissues in animals?
Epithelium
Connective Tissue
Muscle
Nerve
What is dermal tissue in plants?
Outer layer of roots, stems, and leaves
Functions as a protective cover
Includes epidermis, stomata, guard cells, and trichomes (hair cells)
What are the functions of dermal tissue in plants?
Transpiration barrier
Gas exchange
Defense
What do stomata in dermal tissue allow for?
Stomata (openings) allow the release of:
CO2 and O2
Water vapor
How does the waxy cuticle affect transpiration in plants?
The waxy cuticle on the surface of leaves lowers transpiration (reduces water loss).
What are the three types of ground tissues in plants?
Parenchyma tissue
Collenchyma tissue
Sclerenchyma tissue
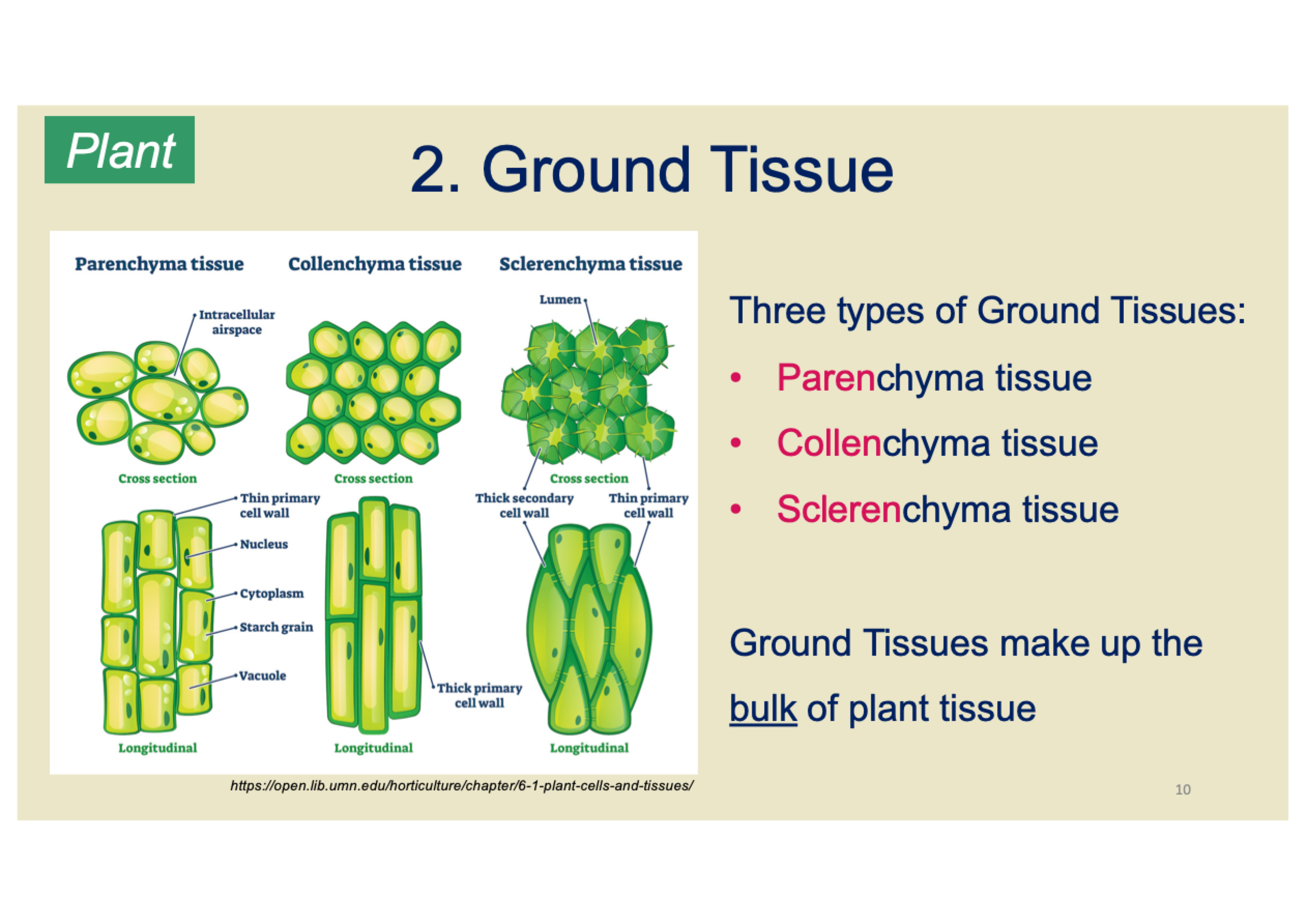
What are the characteristics of parenchyma tissue in plants?
Most common ground tissue (live cells)
Thin primary cell wall
Primary component of young plant organs
Totipotent (can differentiate into any cell type)
Important for regeneration and healing
What are the functions of parenchyma tissue in plants?
Storage of starch and other metabolites
Photosynthesis (packed with chloroplasts)
What are the characteristics of collenchyma tissue in plants?
Live, mature cells with thickened cell walls
Elongated cells that form resilient strands (e.g., celery stalk)
Found beneath the epidermis of stems and leaves
What is the function of collenchyma tissue in plants?
Provides adaptable, mechanical support
Tissues can change in response to external stimuli (e.g., strong wind)
What are the characteristics of sclerenchyma tissue in plants?
Cells have both primary and secondary cell walls
Primary cell wall made of cellulose
Secondary cell wall made of lignin (provides rigidity)
What are the two types of cells in sclerenchyma tissue?
Fibres
Long, non-living strands
Used in fabric materials (e.g., hemp and flax)
Sclereids
Hard coverings around seeds of stone fruits (e.g., cherries, walnuts)
Found in pear pulp
What is vascular tissue in plants?
The "plumbing system" of a plant
Two main types: Xylem and Phloem
What is the function of xylem in plants?
Unidirectional transport of water
Moves water from root → stem → leaves
Made of dead cells at maturity (hollow)
What is the function of phloem in plants?
Transport of nutrients absorbed by roots
Transports sugars (sucrose) made by photosynthesis
Multidirectional transport (from source to sink)
What are meristems in plants?
Sites of active growth
Made up of undifferentiated parenchymal cells
Similar to stem cells in animals
Generate new cells that can differentiate into new cell types
What is the function of apical meristems in plants?
Responsible for growth of roots and shoots
Primary growth: Increases length or height (apical)
Secondary growth: makes new xylem/phloem (vascular cambium)
What are tissues?
Tissue: A collection of cells and extracellular materials specialized for a particular function
Tissues are grouped in a well-ordered arrangement and are easily recognizable
The organization of tissues is directly associated with their functions
What are the functions of the four basic types of animal tissues?
Nervous Tissue – Communication (e.g., brain, nerves)
Muscle Tissue – Movement (e.g., skeletal, cardiac, smooth)
Epithelial Tissue – Linings and coverings (e.g., skin, intestines)
Connective Tissue – Connecting, binding, supporting, and space-filling (e.g., bone, blood, cartilage)
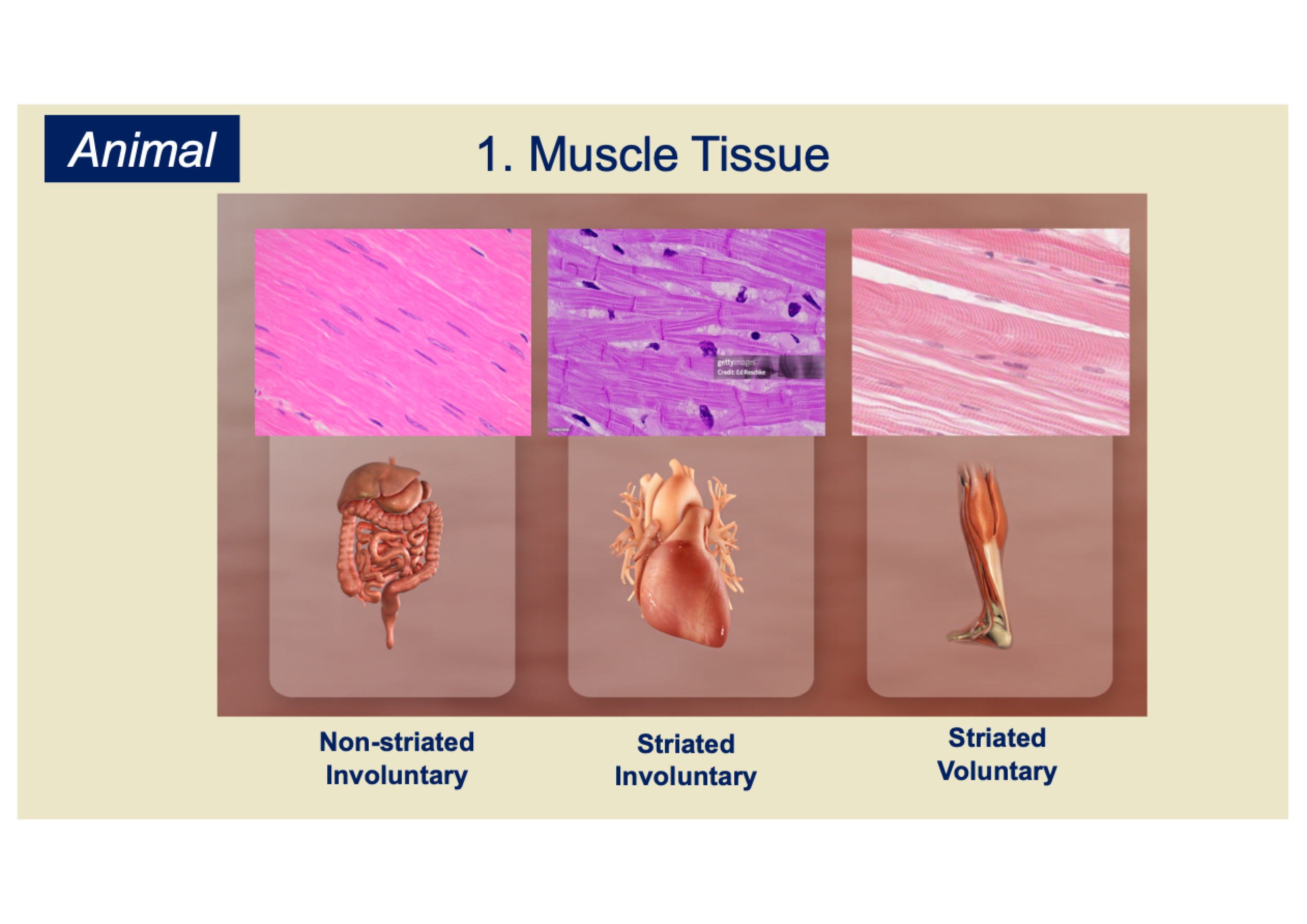
What are the types of muscle tissue?
Non-striated (Smooth): Involuntary, found in internal organs
Striated (Cardiac): Involuntary, found in the heart
Striated (Skeletal): Voluntary, attached to bones for movement
What are the characteristics of skeletal muscle tissue?
~640 muscles in the adult human body
Voluntary movements, posture, force generation
Attached to bones via tendons
Work in pairs to move joints
Striated due to organized sarcomeres
Produces unidirectional force
What are the characteristics of cardiac muscle tissue?
Involuntary, pumps blood through the heart
Contracts rhythmically and continuously
Striated, branched, cylindrical cells with intercalated discs
Abundant mitochondria for energy
Specialized connections for rapid electrical impulse transmission
Enables synchronized contractions
What are the characteristics of smooth muscle tissue?
Involuntary muscle
Non-striated, filaments not organized in a sarcomere
Spindle-shaped cells
Locations: blood vessels, intestines, bladder, uterine wall
Functions:
Peristalsis in the gut
Vasoconstriction in blood vessels
Uterine contractions in childbirth
Bladder release
What are the characteristics of nerve tissue?
Communication through electrical and chemical signals
Made up of neurons and glial cells
Includes motor neurons and sensory neurons
Central Nervous System (CNS): Brain + Spinal Cord
Peripheral Nervous System (PNS): e.g., Sciatic nerve
Nerve tissue consists of motor neurons, sensory neurons, and connective tissue
Additional tissues: skull, vertebral column, meninges, cerebrospinal fluid
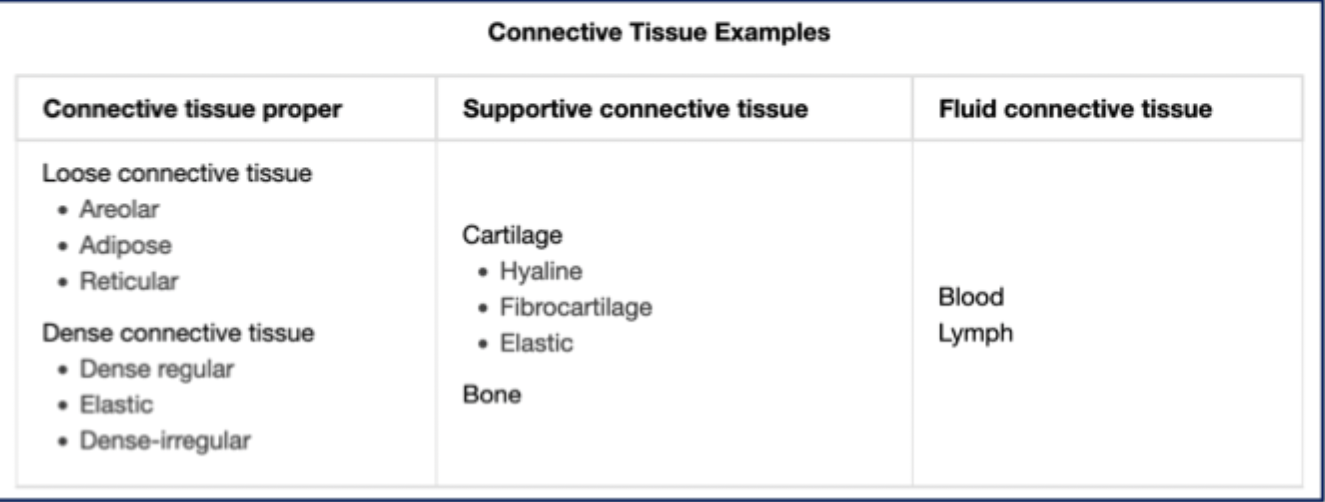
What is connective tissue?
Tissue with cells embedded in an extensive extracellular matrix (ECM)
Serves mechanical functions
What are the functions of connective tissue?
Support
Wrapping & binding
Packing & space-filling
Wound healing
Storage of energy
Infection control
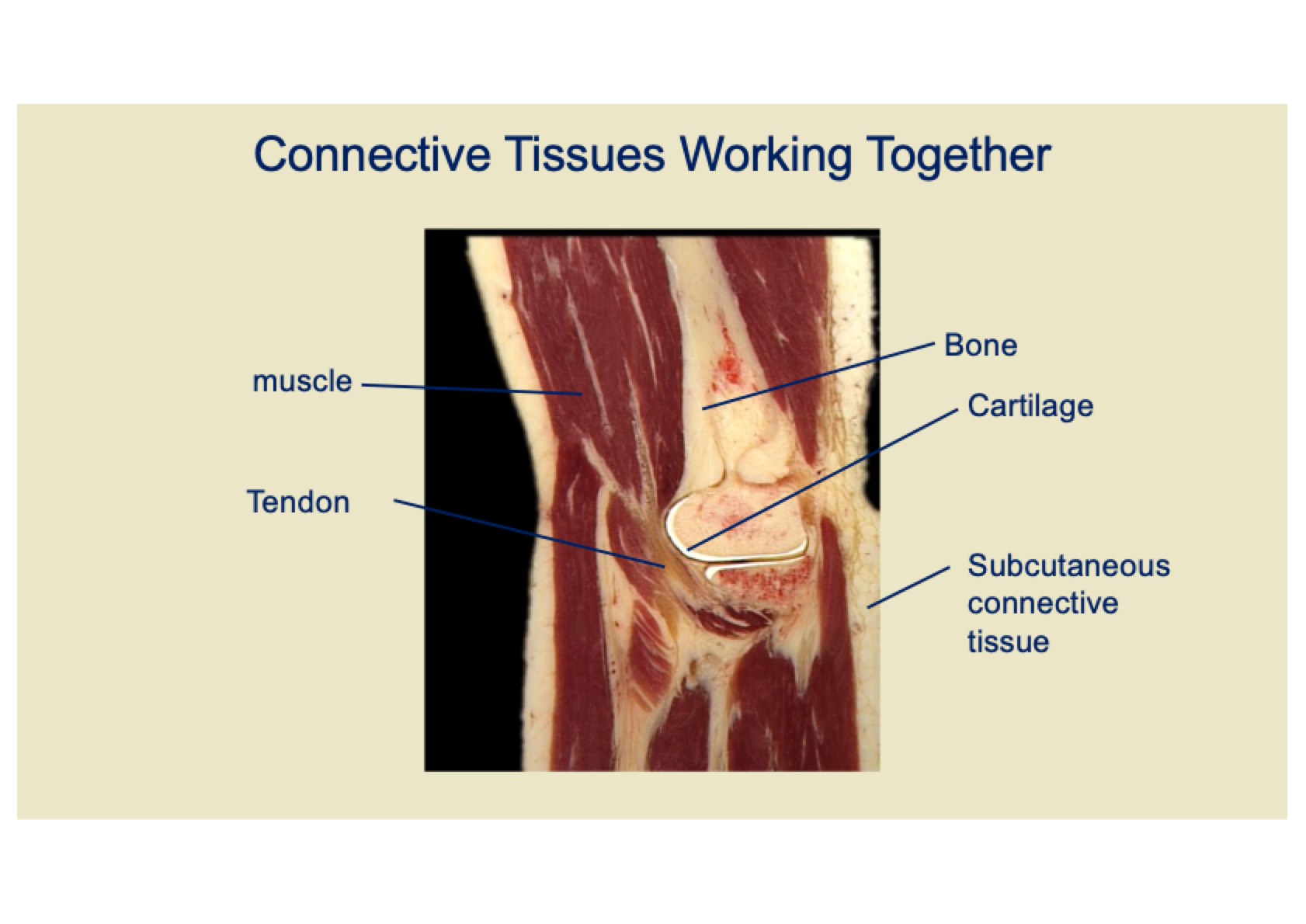
What structures can connective tissue form?
May form structures like bones, tendons, or be part of other tissues/organs.
What are the characteristics of bone connective tissue?
Living tissue
Primarily made of ECM (Collagen), ~90% of the organic matrix
Calcified with Calcium Phosphate
High compression resistance due to calcification
High tension resistance due to collagen
Highly vascularized and highly innervated
What are the cells in connective tissue and their functions?
Fibroblasts: Secrete ECM
Adipocytes: Store lipids as droplets
Mesenchymal cells: Stem cells, differentiate into other CT cells
Connective tissue cells:
Secrete matrix
Sense tension/strain on matrix
Modify matrix according to load
What makes up the extracellular matrix (ECM) in connective tissue?
Fibres:
Collagen (provides tensile strength)
Elastic fibres (stretch & recoil)
Ground substance:
Complex glycosaminoglycans (resist compression)
What is an organ?
A distinct functional unit formed from 2 or more tissue types
What is an organ system?
A collection of organs with related functions
What are the three major cell lineages established within an embryo?
Ectoderm ("outer"): Forms the outer layer and develops into skin, nervous system, etc.
Mesoderm ("middle"): Develops into muscles, bones, and circulatory system.
Endoderm ("inner"): Forms the digestive system and internal organs.
From which germ layers do epithelial tissues originate, and what structures do they form?
Epithelial tissues originate from all three germ layers, contributing to various body structures.
Ectoderm: Forms epithelial tissues in skin, mouth, nose, and anus.
Mesoderm: Forms epithelial tissues in the lymphatic lining.
Endoderm: Forms epithelial tissues in the airway lining and digestive system.
What is the function of epithelial tissue and where is it found?
Epithelial tissue covers and lines both the interior and exterior surfaces of the body.
An obvious example of epithelial tissue is the skin.
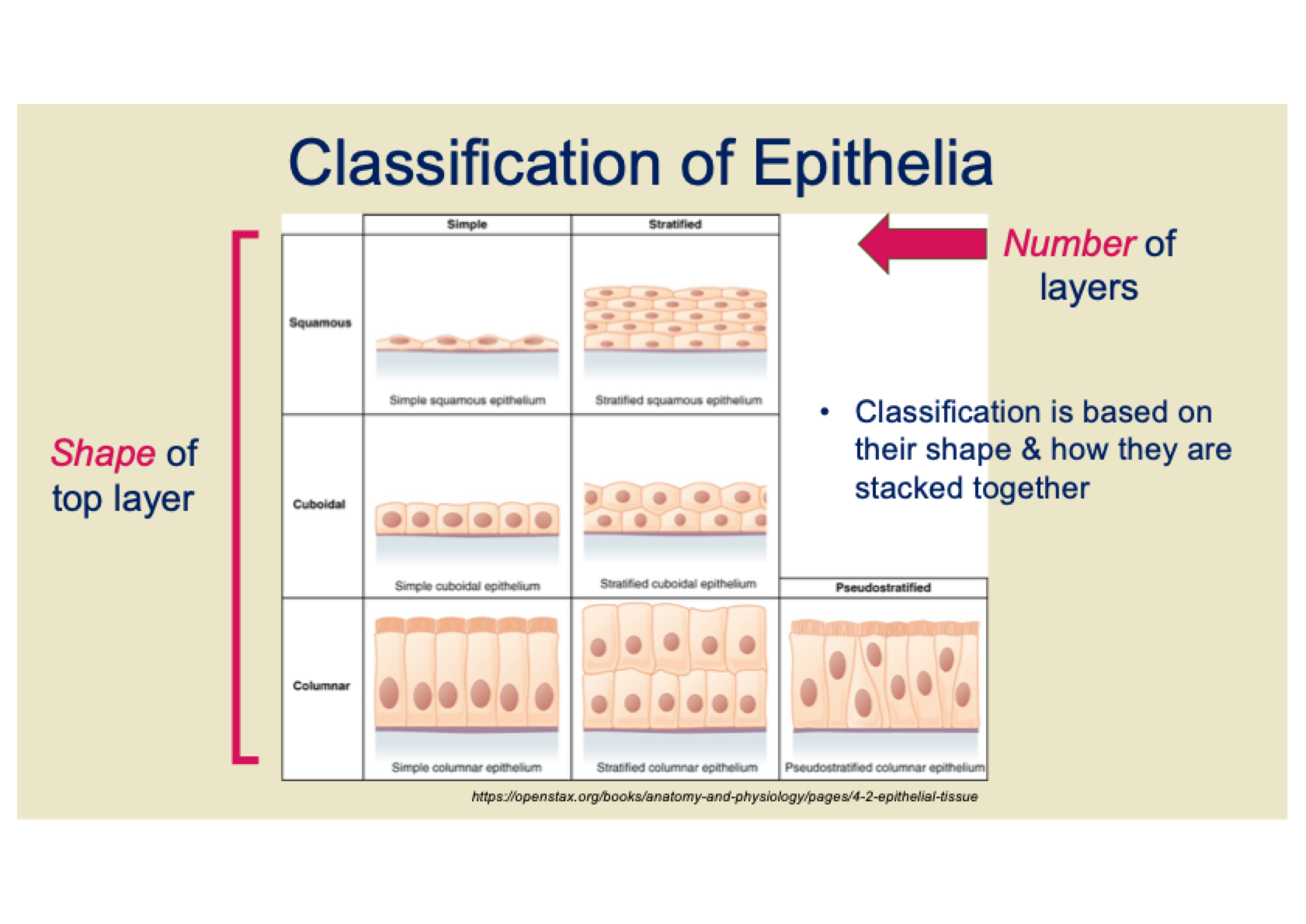
How is epithelial tissue classified?
Epithelial tissue is classified based on two key features:
Number of layers:
Simple: Single layer of cells
Stratified: Multiple layers of cells
Pseudostratified: Appears stratified but is actually a single layer
Shape of cells:
Squamous: Flat, scale-like cells
Cuboidal: Cube-shaped cells
Columnar: Tall, column-like cells
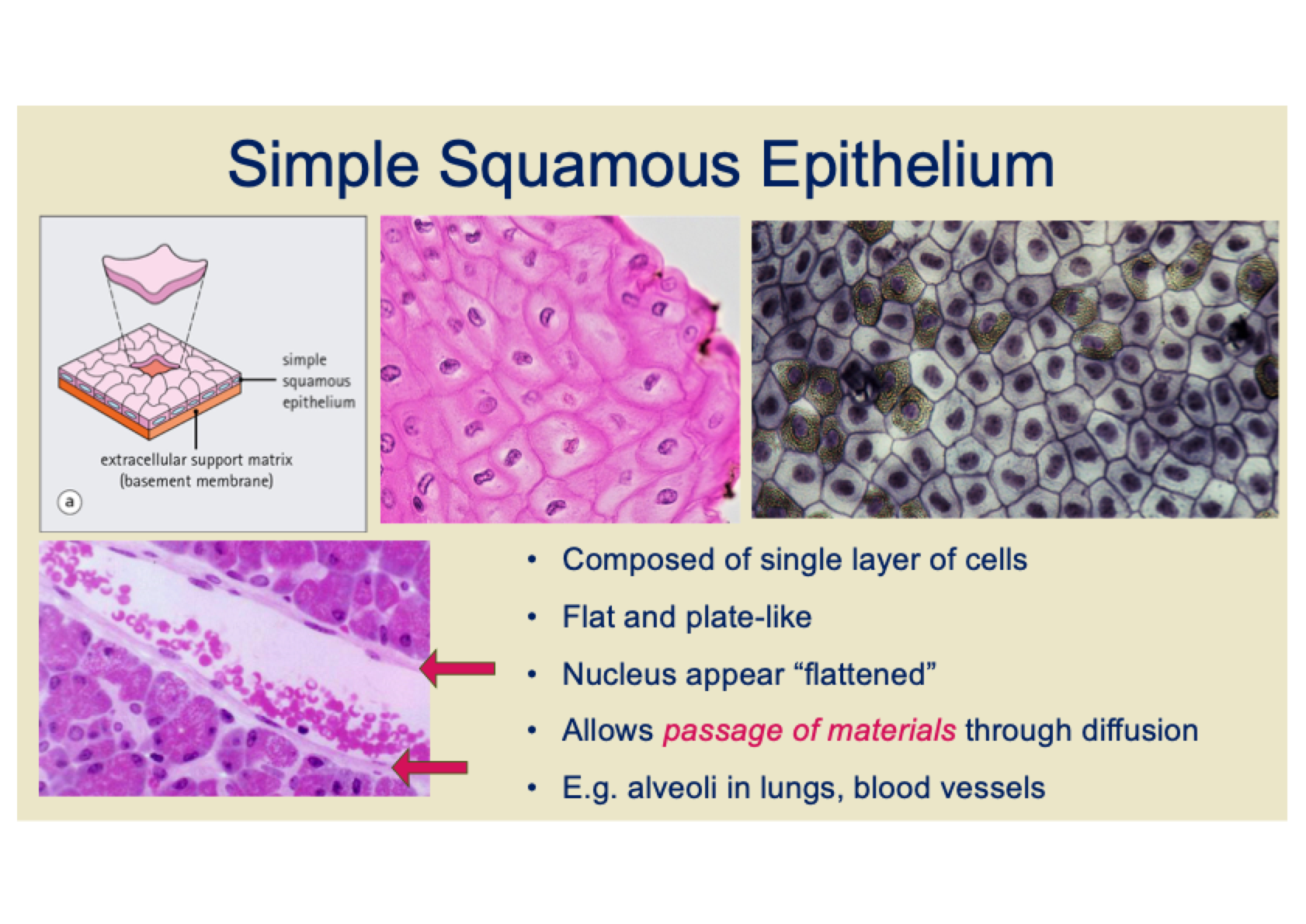
What are the characteristics and functions of simple squamous epithelium?
Single layer of flat, plate-like cells
Flattened nuclei
Allows passage of materials through diffusion
Found in areas where rapid diffusion is needed, such as the alveoli in the lungs and blood vessels.
What are the characteristics and functions of simple cuboidal epithelium?
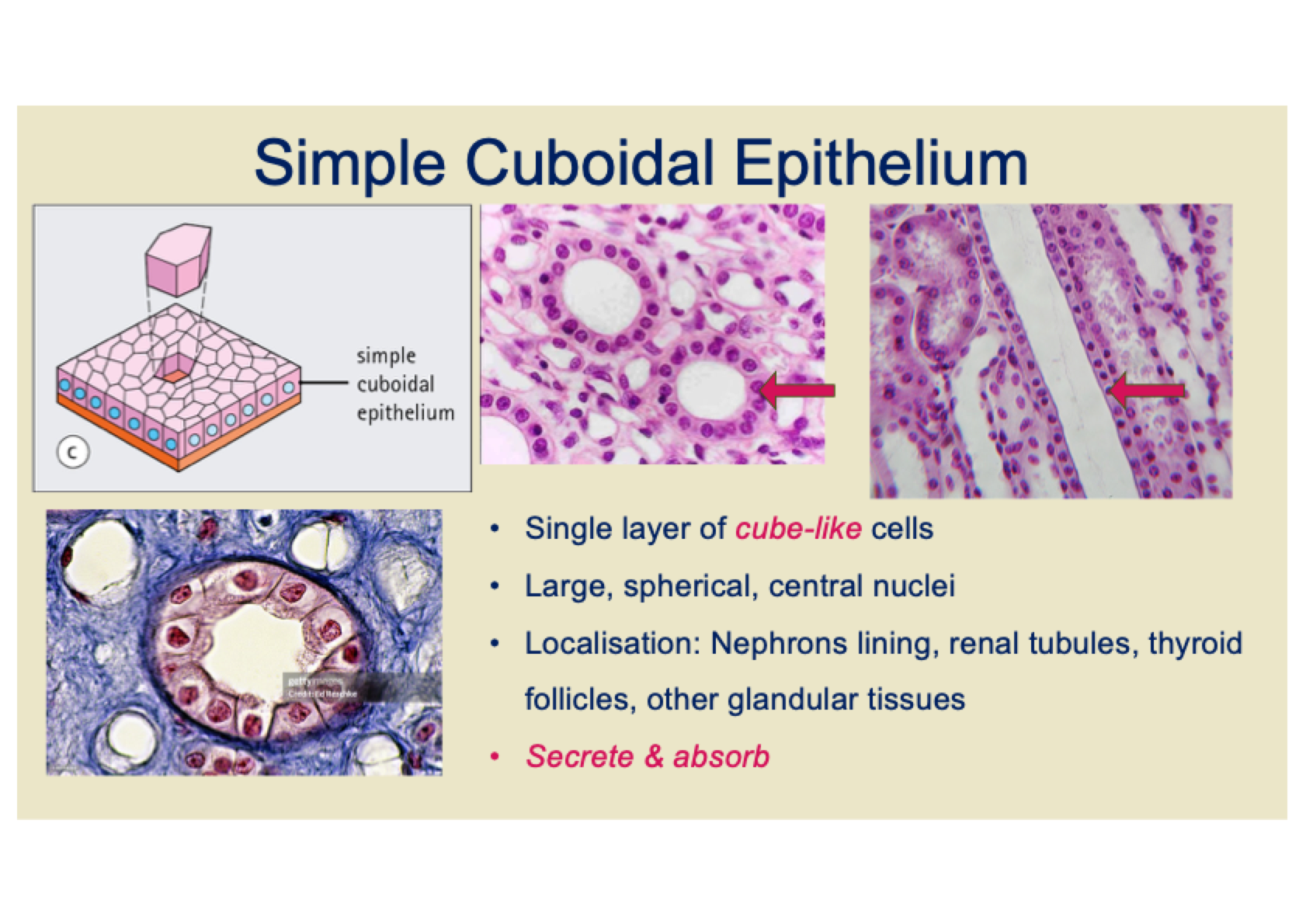
Single layer of cube-like cells
Large, spherical, central nuclei
Found in the nephrons lining, renal tubules, thyroid follicles, and glandular tissues
Functions: Primarily involved in secretion and absorption.
What are the characteristics and functions of simple columnar epithelium?
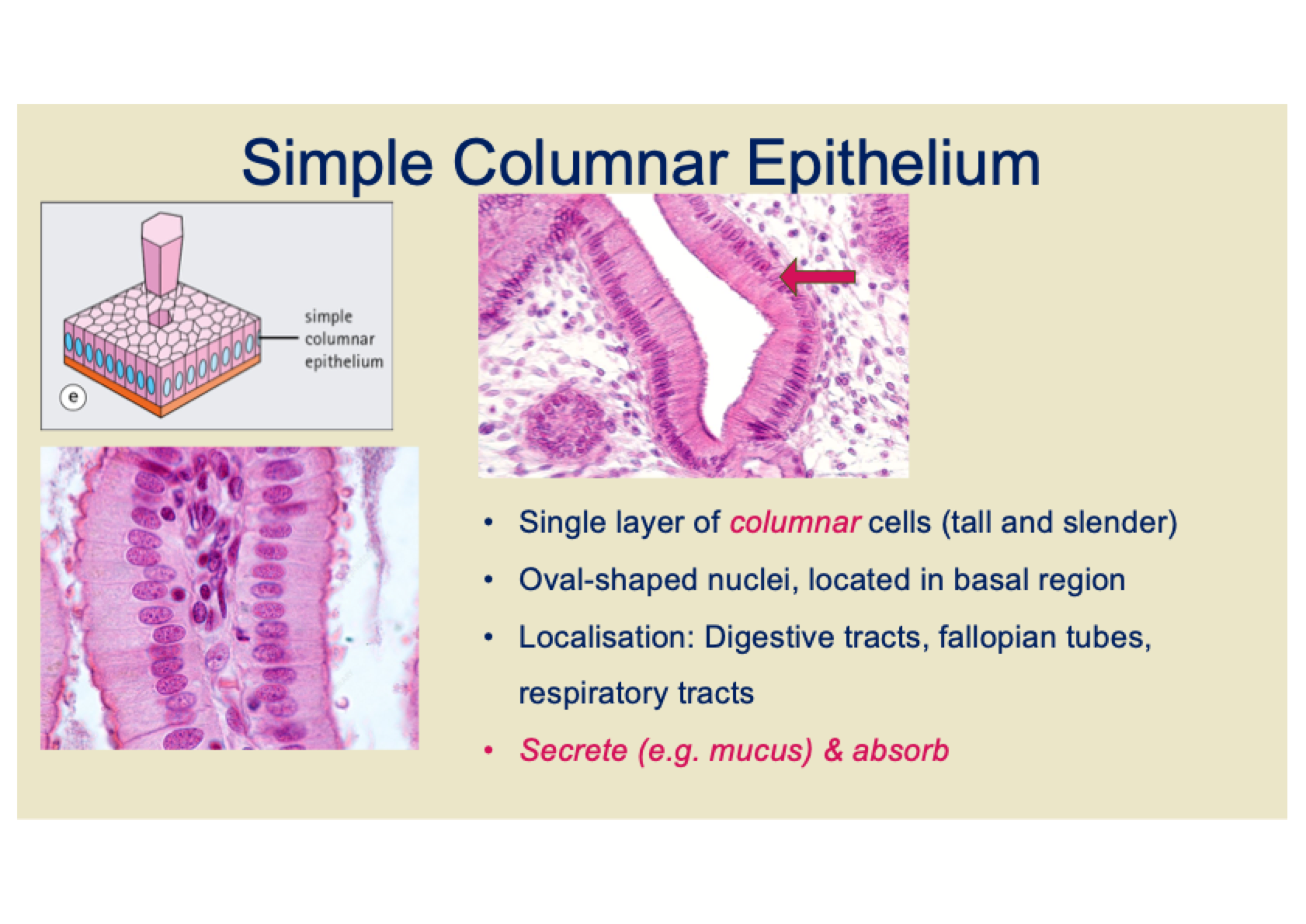
Single layer of tall, slender columnar cells
Oval-shaped nuclei, located in the basal region
Found in the digestive tracts, fallopian tubes, and respiratory tracts
Functions: Primarily involved in secretion (e.g. mucus) and absorption.
What are the characteristics and types of stratified squamous epithelium?
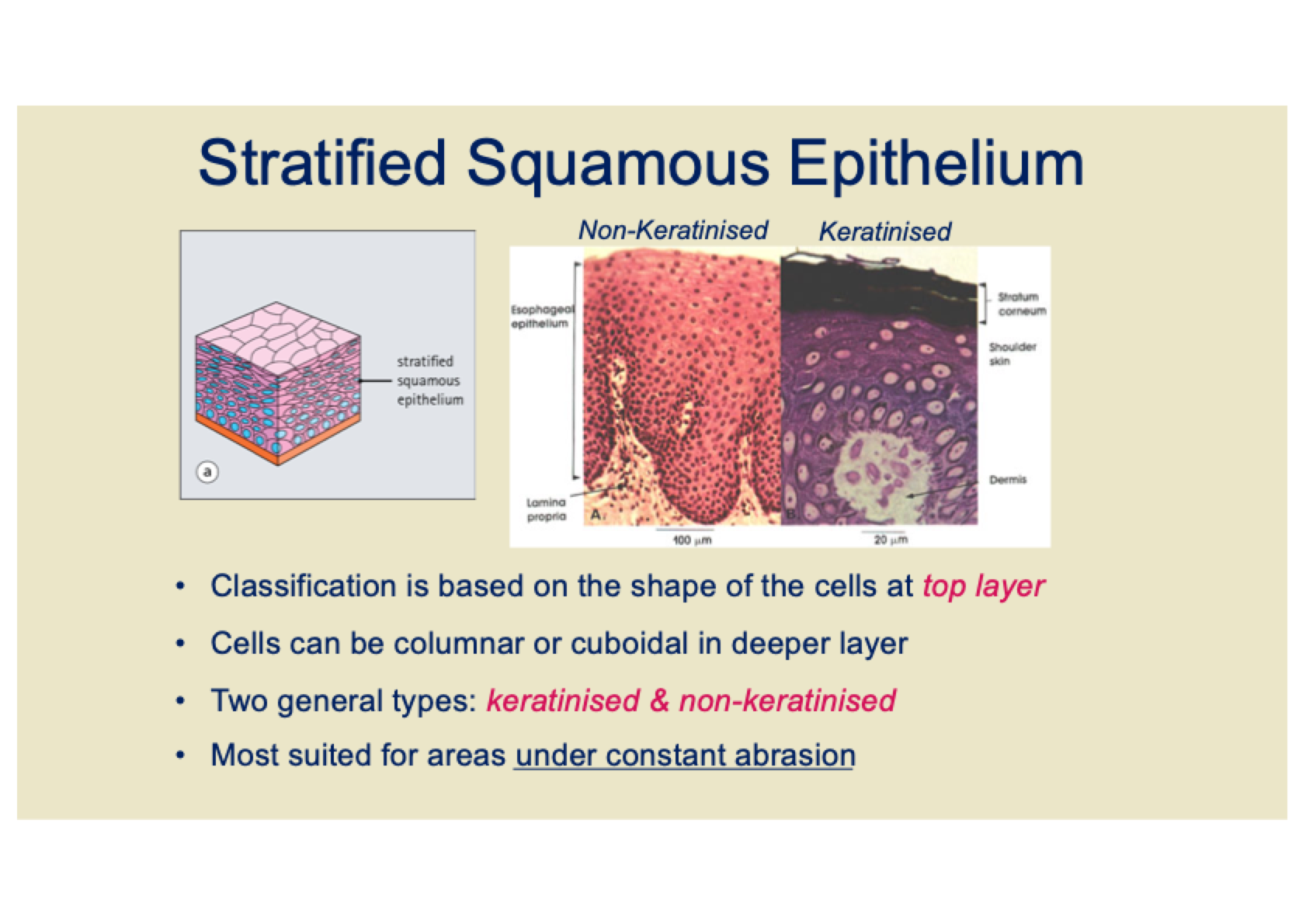
Classification based on the shape of the cells at the top layer (squamous)
Deeper layers may contain columnar or cuboidal cells
Two types:
Keratinised: Found in dry areas like skin
Non-keratinised: Found in moist areas like the mouth or esophagus
Function: Suited for areas under constant abrasion, providing protection.
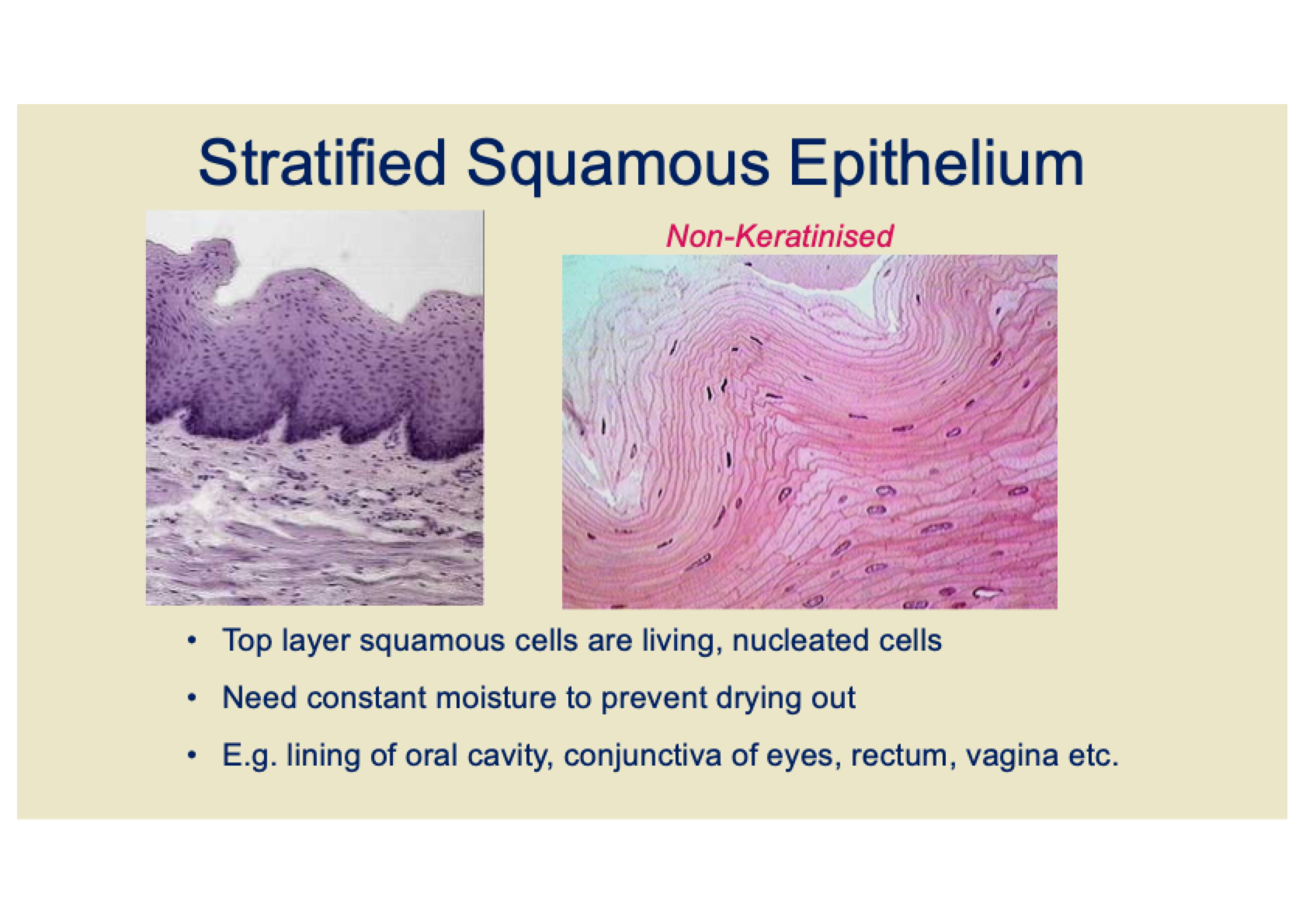
What are the characteristics and functions of non-keratinised stratified squamous epithelium?
Top layer: Squamous cells are living and nucleated
Requires constant moisture to prevent drying out
Found in moist environments such as the oral cavity, conjunctiva of eyes, rectum, vagina, etc.
Function: Provides protection in areas that are exposed to mechanical stress but need to remain moist.
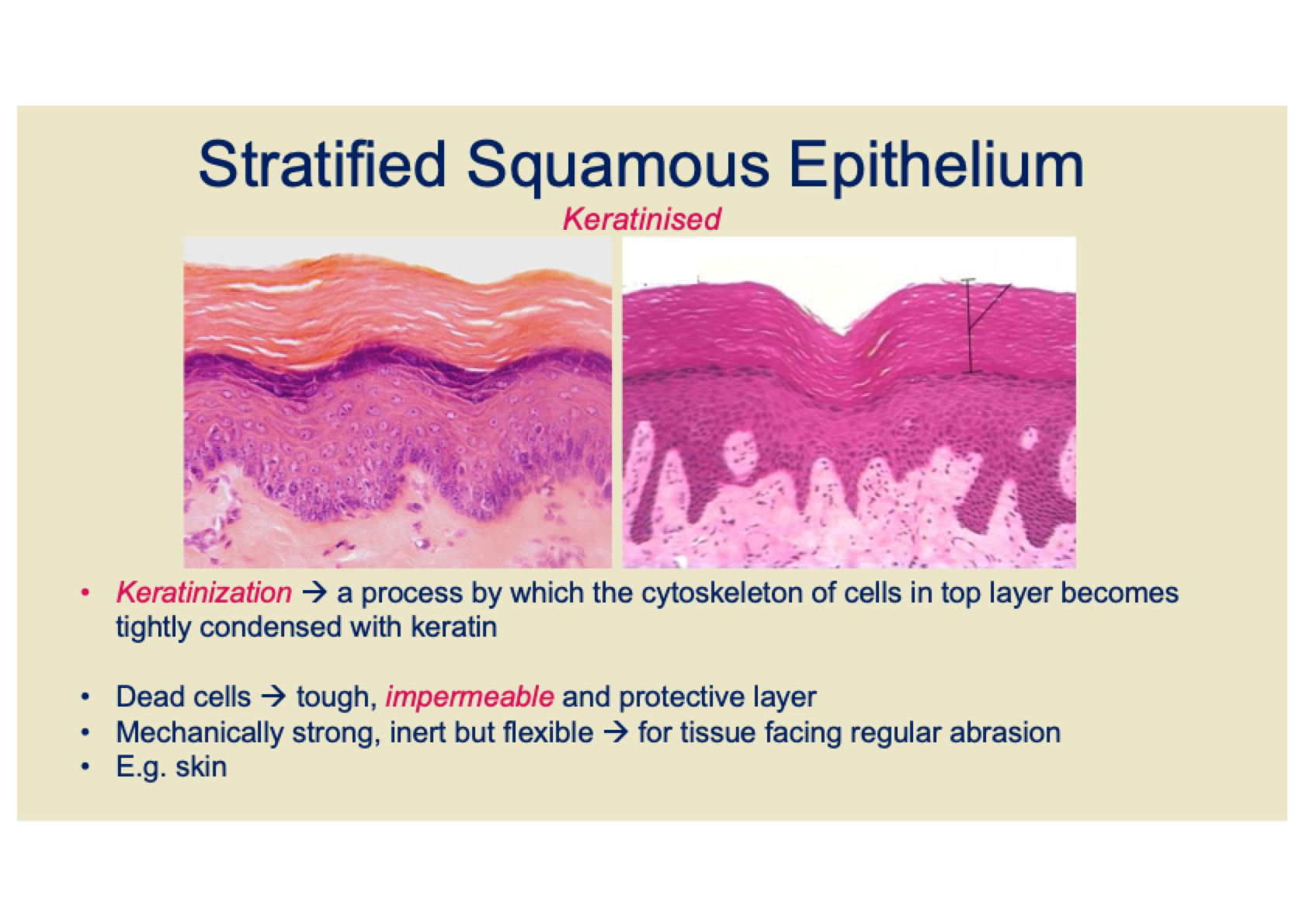
What are the characteristics and functions of keratinised stratified squamous epithelium?
Keratinization: Cells in the top layer undergo a process where their cytoskeleton becomes tightly condensed with keratin
The top layer consists of dead cells that form a tough, impermeable, and protective barrier
Provides mechanical strength, flexibility, and is inert, making it ideal for areas facing regular abrasion
Found in areas like the skin where protection from physical damage and environmental stress is needed.
What are stratified columnar and stratified cuboidal epithelium?
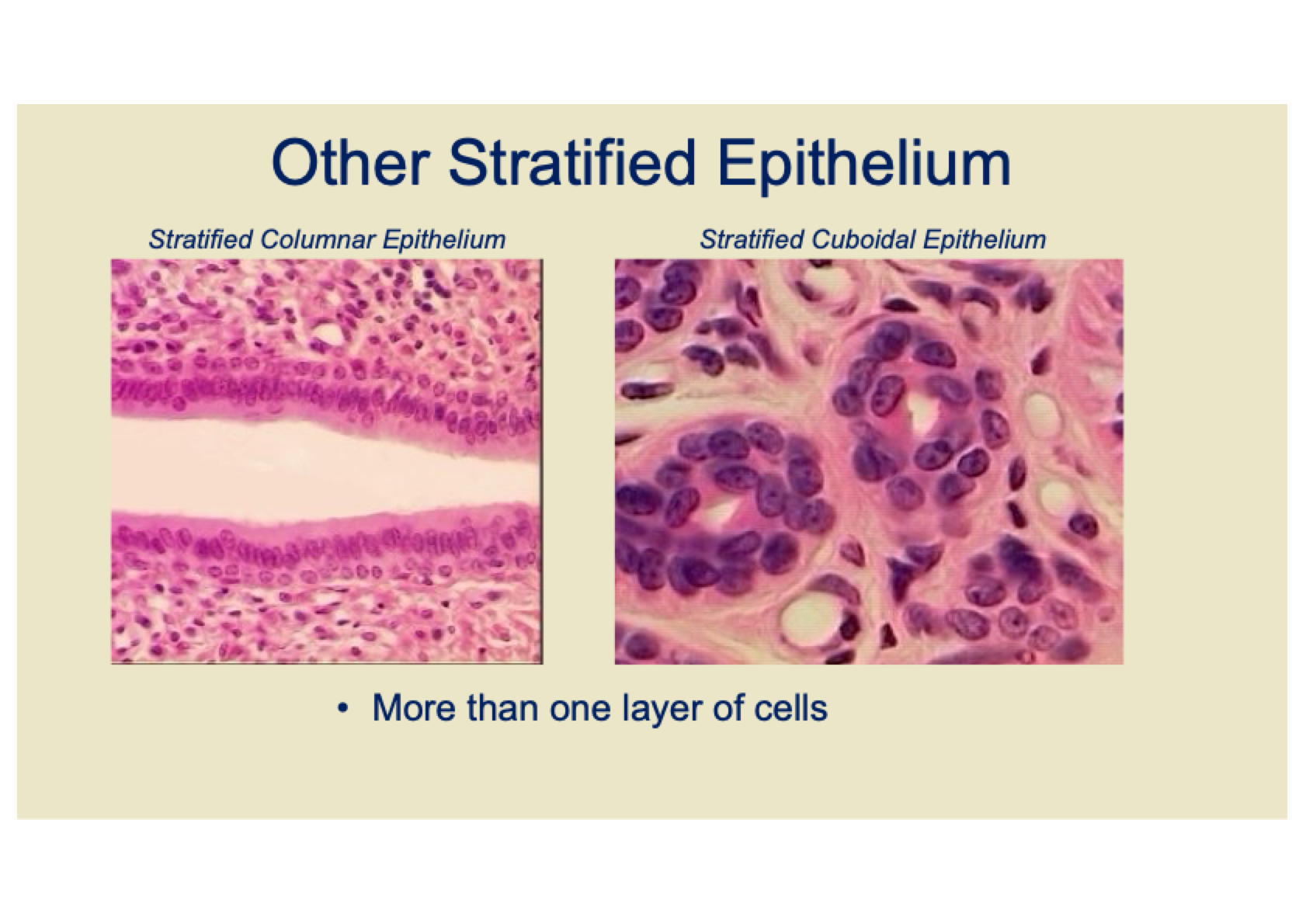
Both have multiple layers of cells.
Stratified columnar: Top layer cells are column-shaped.
Stratified cuboidal: Top layer cells are cube-shaped.
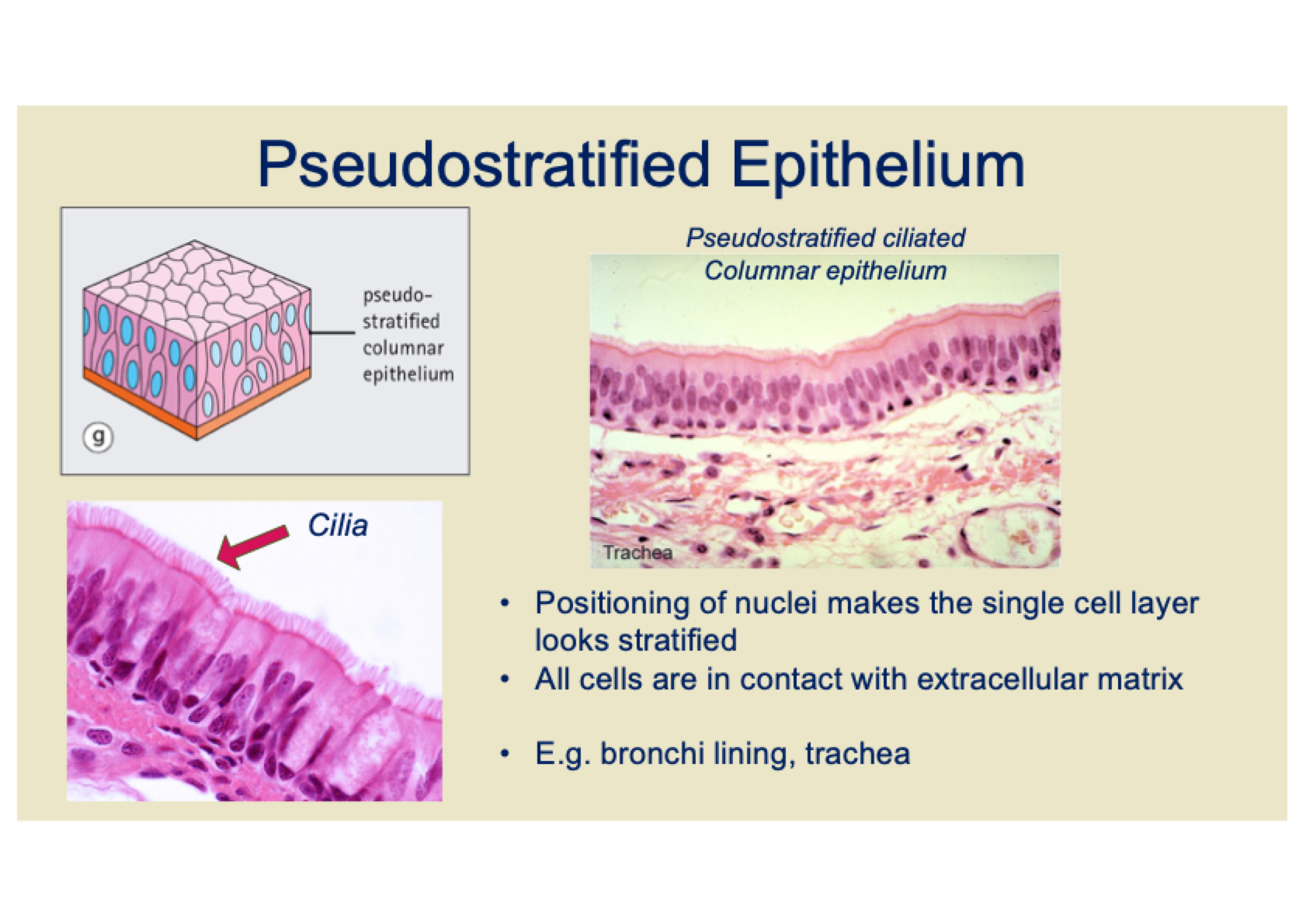
What is pseudostratified epithelium?
Appears stratified due to the nuclei positioning, but is actually a single layer.
All cells are in contact with the extracellular matrix.
Found in the lining of bronchi and trachea.
Functions in secretion and movement of mucus.
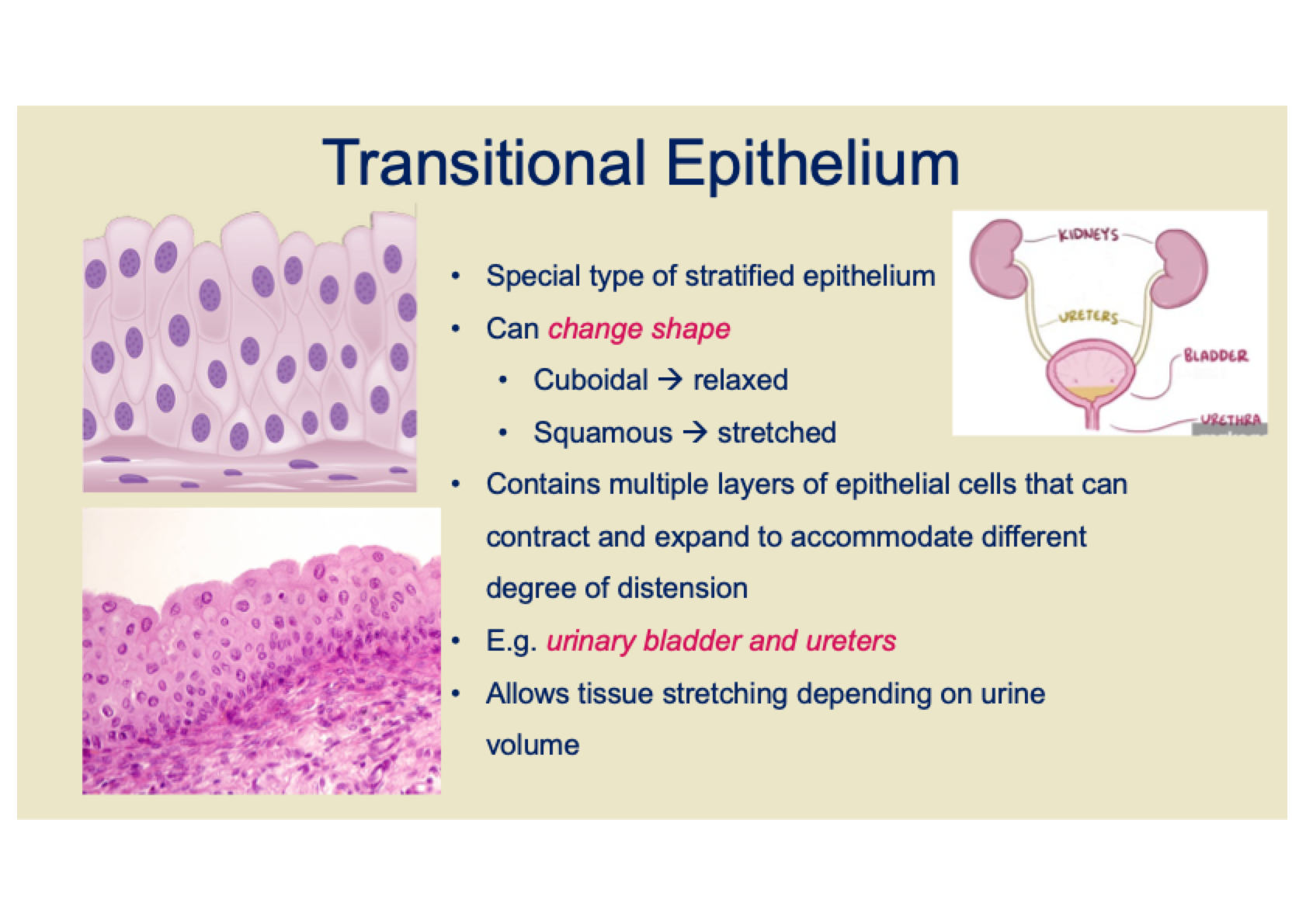
What is transitional epithelium?
A special type of stratified epithelium that can change shape.
Cuboidal when relaxed and squamous when stretched.
Contains multiple layers of cells that contract and expand to accommodate different levels of distension.
Found in the urinary bladder and ureters.
Allows for tissue stretching depending on urine volume.
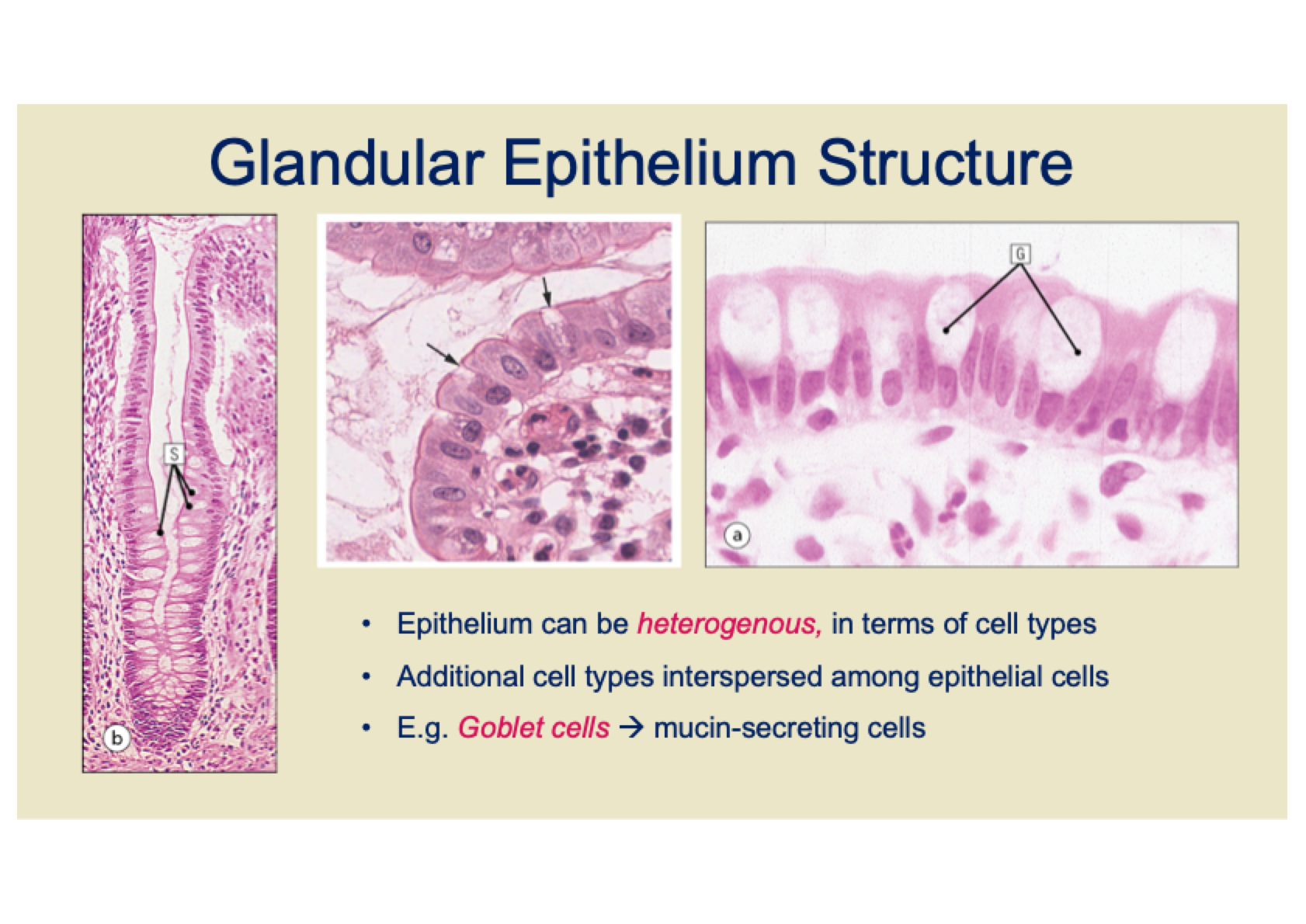
What is the structure of glandular epithelium?
Glandular epithelium grows as a tube into underlying tissue, not just on the surface.
It forms specialized secretory gland structures, such as exocrine glands (e.g., sebaceous gland, mammary gland, salivary gland).
The epithelium can be heterogeneous, meaning it may contain different cell types interspersed among the epithelial cells.
For example, Goblet cells are mucin-secreting cells found in some epithelia.
What are the common features of epithelia?
Cellularity
2. Specialised intercellular contacts
3. Cell polarity
4. Basement Membrane
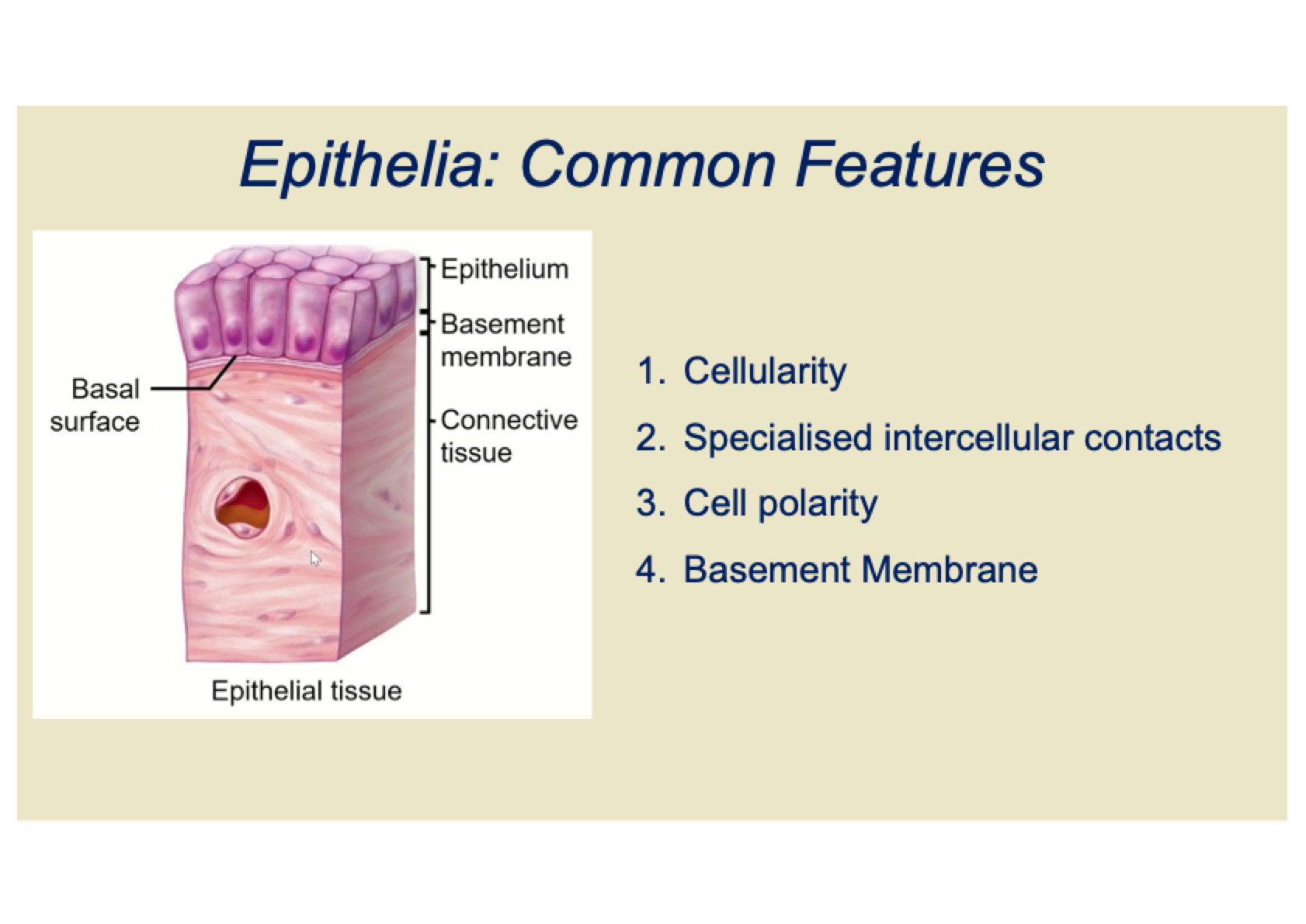
What is the feature of cellularity in epithelia?
Epithelia are composed entirely of cells.
Can be a single layer or multiple layers of cells.
Acts as a barrier, separating internal and external environments.
Regulates material transfer between these environments.
What are tight junctions in epithelia?
Provide a tight seal to prevent leakage of water-soluble molecules between cells.
Forces material to pass through cells, not between them.
Found in locations like the blood-brain barrier, seminiferous tubules in the testis, and the gut epithelium.
What are the three main types of anchoring junctions?
Adherens
Desmosomes
Hemidesmosomes
What are anchoring junctions and how do they function?
Form strong mechanical attachments between cells.
Built around transmembrane proteins – Cadherin protein superfamily.
Cadherin molecules bind directly to an identical Cadherin molecule of its neighbour.
Requires Ca2+ to be present in the extracellular medium.
Intracellularly, Cadherin is tethered to cytoskeletal filaments via linker proteins.
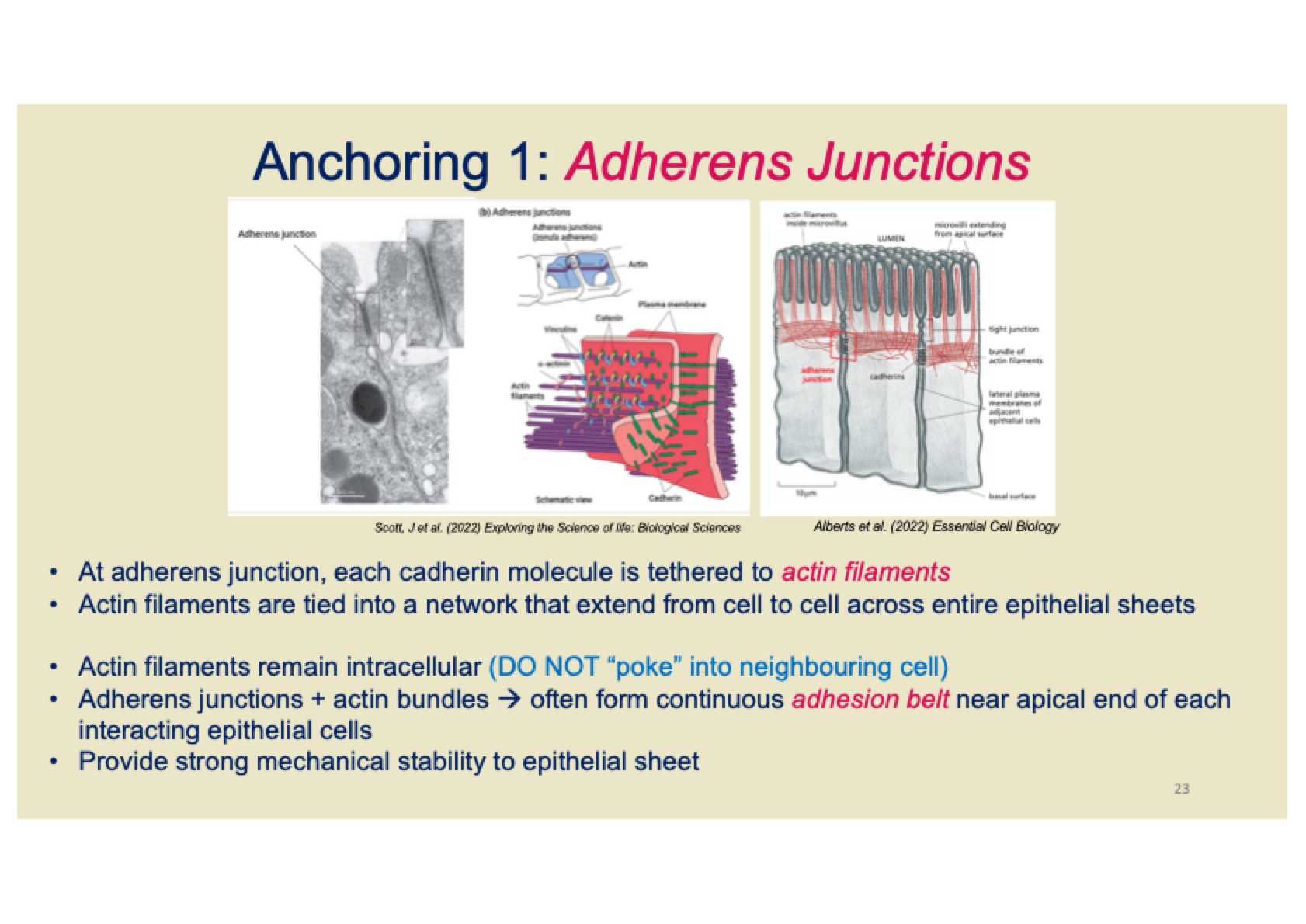
What are Adherens Junctions and how do they function?
Cadherin molecules are tethered to actin filaments at adherens junctions.
Actin filaments form a network that extends across entire epithelial sheets, linking cells.
Actin filaments remain intracellular and do not enter neighboring cells.
Adherens junctions with actin bundles often form a continuous adhesion belt near the apical end of epithelial cells.
They provide strong mechanical stability to the epithelial sheet.
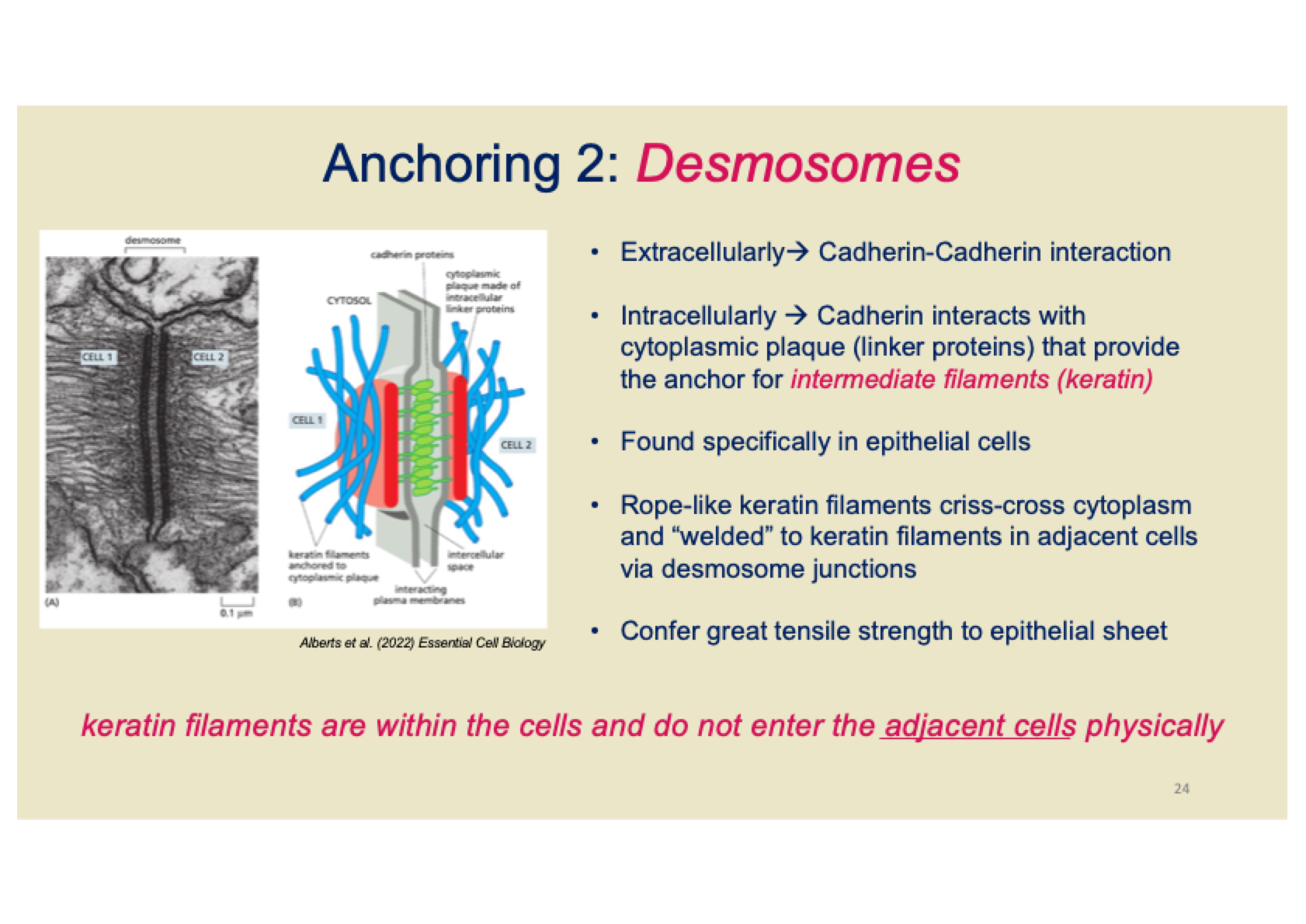
What are Desmosomes and how do they function?
Extracellularly: Cadherin molecules interact with each other (Cadherin-Cadherin interaction).
Intracellularly: Cadherin molecules bind to a cytoplasmic plaque made of linker proteins, which anchor intermediate filaments (keratin).
Found specifically in epithelial cells.
Keratin filaments form a rope-like network within the cytoplasm and are "welded" to keratin filaments in adjacent cells via desmosome junctions.
Desmosomes confer great tensile strength to the epithelial sheet.
Keratin filaments stay within the cells and do not enter adjacent cells.
How do desmosomes relate to Pemphigus?
Pemphigus is a condition where autoantibodies attack desmoglein (a type of Cadherin protein), which is crucial for desmosome function.
This attack causes separation of cells in the skin epithelium, leading to epidermis detachment.
As a result, blisters form on the skin.
Pemphigus severity can vary and in severe cases, it can be fatal.
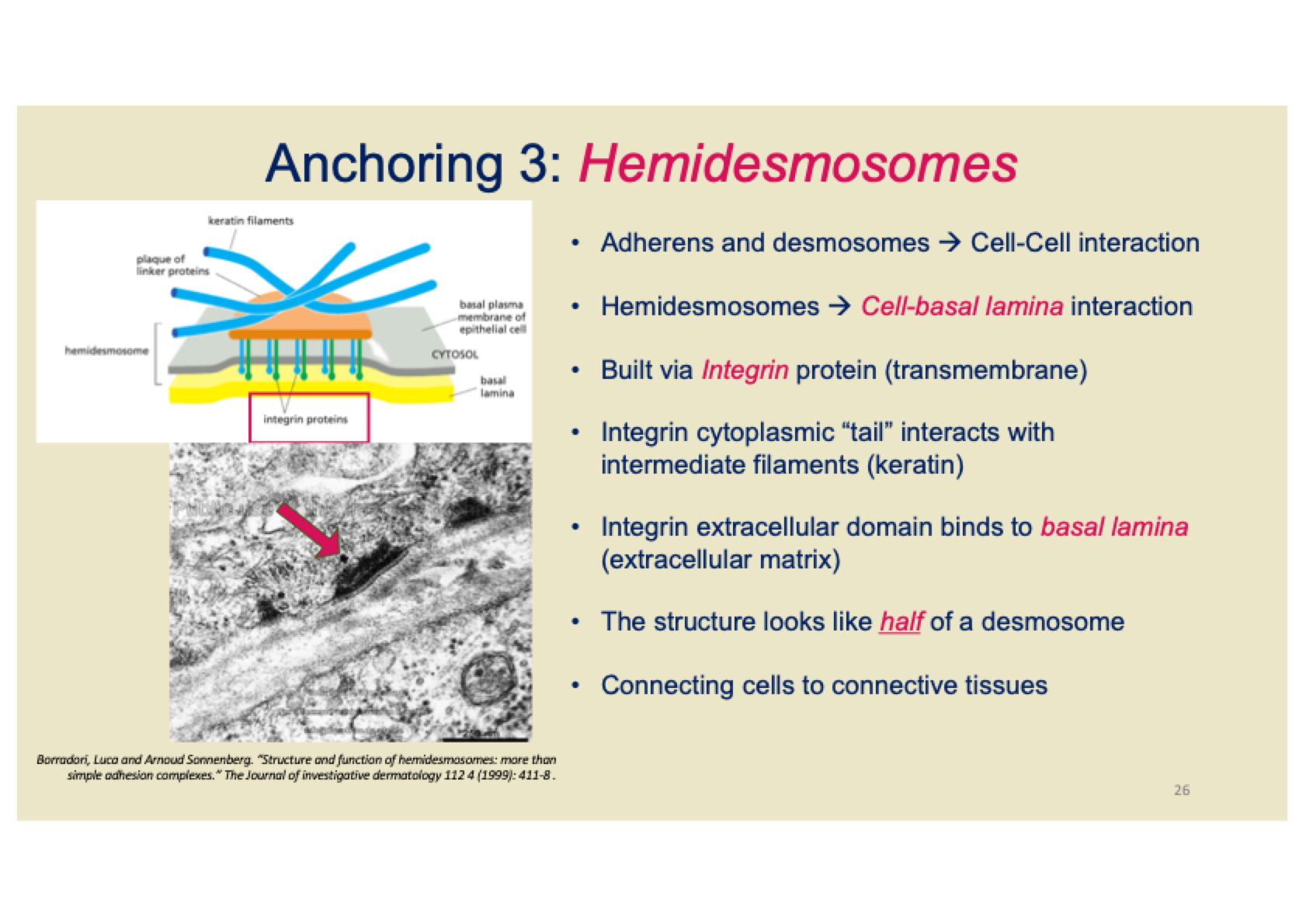
What are hemidesmosomes and how do they function?
Hemidesmosomes are involved in cell-basal lamina interaction, unlike adherens and desmosomes that mediate cell-cell interactions.
They are built using Integrin proteins as the key transmembrane proteins.
The cytoplasmic tail of Integrin interacts with intermediate filaments like keratin.
The extracellular domain of Integrin binds to the basal lamina (part of the extracellular matrix).
Hemidesmosomes are structurally like half of a desmosome, connecting epithelial cells to connective tissue.
What are gap junctions?
Gap junctions are specialized connections that bridge a narrow gap (2-4nm) between adjacent cells' plasma membranes.
They are formed by connexons, which are transmembrane protein complexes that span the gap.
How do gap junctions function?
Connexons align end-to-end to form water-filled channels.
These junctions allow inorganic ions and small water-soluble molecules (<1000 Da) to pass through.
They enable electrical or metabolic flow between cells.
What are some examples of gap junction functions?
Cardiac muscle cells: Allow for synchronous beating.
Ciliary beating in lung epithelium.
Islet of Langerhans in the pancreas: Enable coordinated secretion of insulin and glucagon.
Neurons in the retina: Gap junctions are reduced in response to dopamine due to bright light exposure.
What controls the opening and closing of gap junctions?
Gap junctions can flip between open and closed states in response to various signals:
Electrical signals
pH changes
Neurotransmitters
What is cell polarity in epithelial cells, and what are some specializations of the apical and basal surfaces?
Cell polarity refers to the distinct differences between the top (apical) and bottom (basal) surfaces of epithelial cells:
Apical surface: Faces the external environment and can have structures like cilia (to move fluids or particles) and microvilli (to increase surface area for absorption).
Basal surface: Faces the basement membrane and may have basal folds to increase surface area for exchange or transport.
What is the basement membrane in epithelial tissue, and what are its components?
The basement membrane is a layer that epithelial cells sit on, separating them from the underlying connective tissue.
It consists of multiple extracellular matrices, including:
Type IV collagen
Laminin (a glycoprotein)
Perlecan (a proteoglycan)
What are the common features of epithelial tissues?
Completely cellular layer
Little or no extracellular material between cells
Cells are joined by cell junctions
Avascular (no blood vessels)
Sits on top of a basement membrane
Usually over vascular connective tissue
Controls entry and exit of all materials from body tissues
What are the general functions of epithelial tissues?
Protection – serves as a physical barrier
Absorption – specialized surface structures for absorption
Secretion – adapted to secrete macromolecules
Dialysis – in kidney and lung epithelium
Sensation – in structures like taste buds and olfactory epithelium
What is the difference between normal and pathological epithelial cells?
Normal Cells: Follow growth control mechanisms.
Pathological Cells: Lose growth control, leading to tumour (neoplasm) formation.
Carcinoma: Malignant tumour derived from epithelium.
Squamous Carcinoma: Malignant tumour from squamous epithelium.
Adenocarcinoma: Malignant tumour from glandular epithelium.
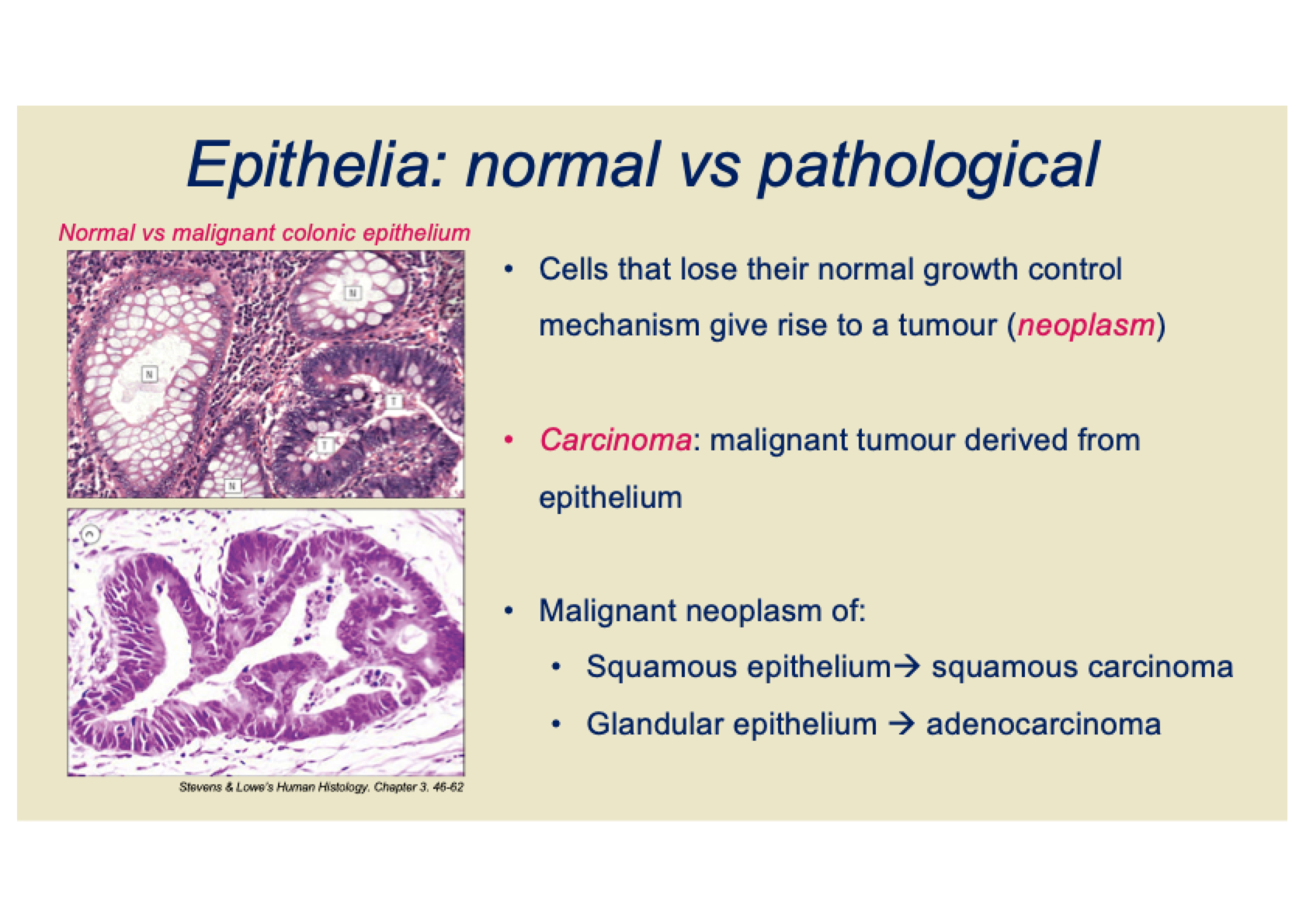
Diagram of connective tissues working together
Where is loose connective tissue typically found?
It is found between many organs.
What are the main functions of loose connective tissue?
Space filling & binding
Energy storage
Cushioning
Allows planes of movement
Immune function
What are the main components of loose connective tissue?
Fibres:
Collagen (stretch resistance)
Elastic (recoil)
Ground substances:
Polysaccharides (e.g., hyaluronan, which holds water)
Cells
What are the main functions of adipose tissue in loose connective tissue?
Energy storage
Insulation & protection (e.g., protecting vital organs)
Heat generation (in brown adipose tissue)
What is areolar in loose connective tissue?
• Widely distributed
• E.g. subcutaneous layer,
around blood vessels and
nerves, space between
organs
• Structural support
What is reticular in loose connective tissue?
• Made of reticular fibres that
form mesh-like network
• Structural support, but with
spaces to enable cell
movement
What are the resident cells in loose connective tissue?
Fibroblast
Adipocytes
Mast cells
Endothelial cells and pericytes
What are the immigrant cells in loose connective tissue?
Monocytes
Macrophages
Lymphyocytes
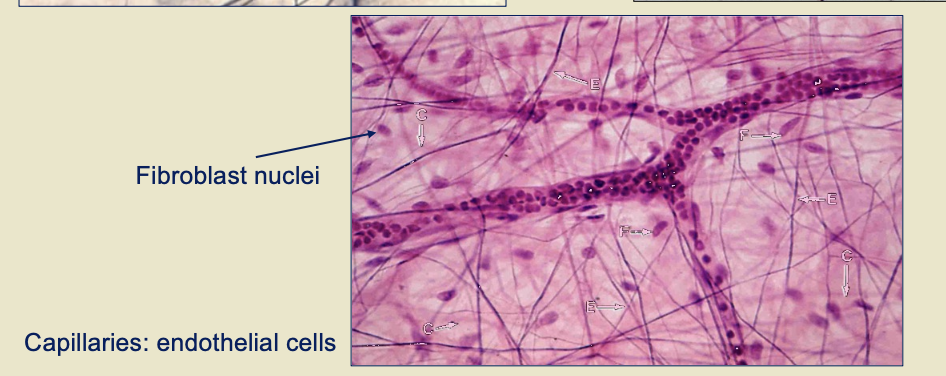
What is the function of fibroblasts in loose connective tissue?
Fibroblasts are the most abundant cells in loose connective tissue.
They secrete polysaccharides and proteins to form the extracellular matrix.
What do adipocytes do in loose connective tissue?
Adipocytes store lipids as droplets, filling most of the cytoplasm.
There are two basic types: white and brown adipocytes.
What is the function of mast cells in loose connective tissue?
Mast cells contain many cytoplasmic granules, including histamine and heparin.
Histamine release plays a key role in the inflammatory response.
What is the role of endothelial cells and pericytes in loose connective tissue?
Endothelial cells are thin and tightly joined, providing a "barrier" function.
Pericytes help maintain the stability and integrity of capillaries.
What is the role of monocytes in loose connective tissue?
Monocytes migrate to loose connective tissue during immune responses.
They circulate in the bloodstream for surveillance and differentiate into macrophages or dendritic cells.
What do macrophages do in loose connective tissue?
Macrophages carry out phagocytosis (engulfing pathogens and cell debris).
They also present antigens to T-cells.
What is the role of lymphocytes in loose connective tissue?
Lymphocytes constantly circulate between blood, lymphoid organs, and loose connective tissue.
Examples include T cells, B cells, and natural killer cells.
They are attracted to infection or inflammation sites by chemotactic signals.
What is the function of T cells in the immune response?
T cells directly attack pathogens.
What do B cells do in the immune response?
B cells form plasma cells that produce antibodies.
Diagram of mast cells

Diagram of adipocytes
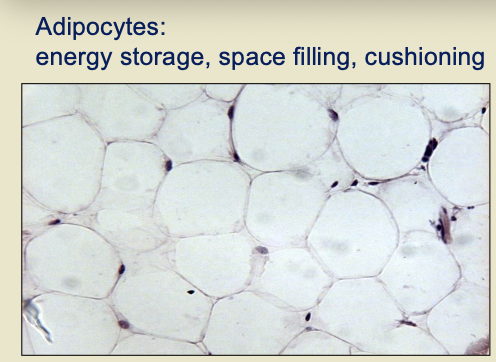
Diagram of fibroblast nuclei
How does dense connective tissue differ from loose connective tissue?
Dense connective tissue contains more collagen fibres, giving it greater resistance to stretching compared to loose connective tissue.
What are the two major types of dense connective tissue?
Regular Dense Connective Tissue
Irregular Dense Connective Tissue
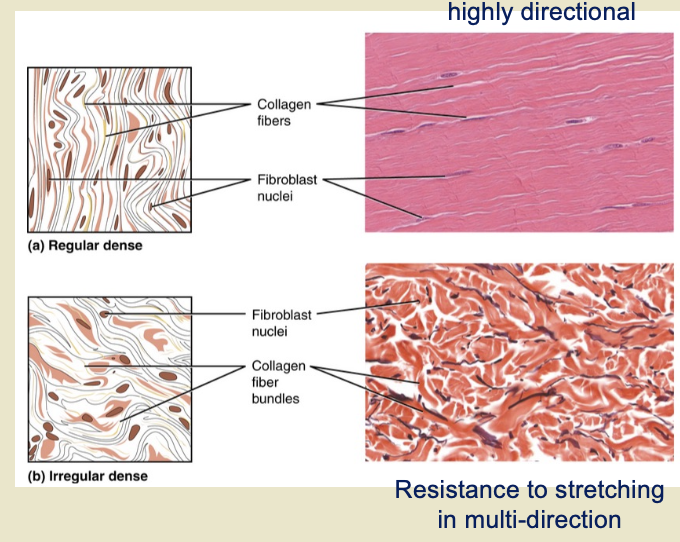
What is the structure and function of regular dense connective tissue?
The fibres are parallel to each other.
It provides enhanced tensile strength.
Example: ligaments and tendons.
May also contain elastin fibres for added flexibility.
What is the structure and function of irregular dense connective tissue?
The direction of fibres is random.
It offers greater resistance to stretching in all directions.
Example: dermis of the skin and the arterial wall.
What are the main functions of cartilage?
Connecting bones
Cushioning joints (articulations)
Protecting the ends of bones
Providing shock absorption
What gives cartilage its distinctive appearance?
The polysaccharide Chondroitin Sulphate, which forms proteoglycans.
What are the three types of cartilage?
Hyaline Cartilage
Elastic Cartilage
Fibrocartilage
What are the characteristics of Hyaline Cartilage?
Most common type of cartilage
Contains short and dispersed collagen fibres
High amounts of proteoglycans
"Glass-like" (clear tissue) appearance
Smooth, strong, flexible, and resistant to compression
Stiff structure