BPK 205 Post Midterm 2
1/158
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
159 Terms
Blood
-Makes up ~7% of body weight; 5L in 70 kg male, 4L in 58 kg female
-A form of connective tissue; composed of watery, extracellular matrix (plasma) and cellular elements
-Plasma makes up about 1/4 of ECF
Cellular elements of blood
Red blood cells (erythrocytes) - function in gas transport
White blood cells (leukocytes) - includes lymphocytes, monocytes (macrophages in tissue), neutrophils, eosinophils, basophils (mast cells in tissues); function in immune response
Platelets (thrombocytes) - function in clotting and hemostasis --> are not complete cells
-When centrifuged, plasma = 58%, WBC and platelets < 1%, RBC = 42% of volume
Hematopoesis
-Synthesis of new blood cells; occurs in the bone marrow (pelvis, spine, ribs, cranium, proximal ends of long bones)
-About 25% of developing cells = RBC, 75% = WBC --> due to different in lifespan; RBC = 120 days, WBC = 6 - 12 hours
-New blood cells come from pluripotent stem cells (partially differentiated)
-Pluripotent hematopoietic stem cell --> WBC/RBC precursor --> fully differentiated cell
Cytokines and blood cell production
-Cytokines (proteins released from one cell that affect another) control production/development of blood cells
-Erythropoietin (EPO) = produced in kidneys in response to hypoxia (low arterial O2); stimulates erythropoiesis --> production of RBC
-Thrombopoietin (TPO) = produced in liver; influences growth/development of megakaryocytes --> platelets
Red Blood Cells
-120 day lifespan
-Biconcave and bendy discs
-No nucleus or mitochondria
-Contain hemoglobin --> 2 α and 2 β subunits; can bind 4 oxygen (one per subunit)
-Contains an iron atom at the centre of porphyrin ring in each heme group (in each subunit) --> where oxygen binds (weakly --> reversible)
Anemia
-Low RBC count
-Results in decreased hemoglobin content --> reduced O2 carrying capacity
-Can be due to accelerated RBC loss (blood loss, hemolytic anemia --> degradation > production --> genetic (sickle cell) or acquired (malaria)) or due to decreased RBC production (aplastic anemia (drugs/radiation) or dietary insufficiency (iron, folic acid or vitamin B12 deficiency))
-Malaria cannot infect sickle cells --> selected gene in areas with malaria
Hemostasis and tissue repair
-Hemorrhage = loss of blood from vessels
-Hemostasis = keeping blood inside vessels
-4 steps in hemostasis in response to damage:
1) Vasoconstriction
2) Platelet plug formation
3) Coagulation (formation of clot)
4) Dissolution of clot (fibrinolysis)
Formation of platelet plug
-Exposed collagen in damaged vessel wall attracts and activates platelets
-As platelets begin to stick --> release platelet factors --> recruits more platelets
-Platelets aggregate into platelet plug
Coagulation Cascade
-Converts platelet plug into fibrous clot
-2 pathways: intrinsic and extrinsic --> both involve plasma proteins (factors) in cascade to activate factor X
Intrinsic - everything needed is found within vessel; activates in response to exposed collagen (rupture) --> sets of cascade --> activated factor X
Extrinsic - requires something outside vessel to activate; begins when tissue factor leaks out of damaged tissue of wall --> cascade --> activated factor X
-Active X converts Prothrombin to Thrombin --> Thrombin converts fibrinogen to fibrin --> fibrin cross-links to form mesh and stabilized platelet plug
Hemostasis pathway
Vasoconstriction due to paracrine signals from endothelium (decreased blood flow and pressure in vessel) --> Platelets adhere to exposed collagen; form plug --> Activation of coagulation cascade generates fibrin mesh to stabilize plug and form clot --> Fibrinolysis = tissue is repaired and clot dissolves
ABO-Rh Blood Groups
-Blood type refers to antigens expressed on RBCs --> antigens = inherited surface proteins
-Body makes antibodies against antigens you do not have (e.g. if type A blood --> have A antigens, B antibodies)
-Positive (+)/Negative (-) refers to if Rh antigen is present --> only make Rh antibodies in response to presence of Rh
Blood type and transfusion compatibility
-Blood clumps if given wrong blood type due to reaction of RBC antigens and plasma antibodies
-Type O- = universal donor (no antigens); Type AB + = universal acceptor (no plasma antibodies)
-Rh- patients can only receive Rh- blood
Rh factor incompatibility and pregnancy
-If Rh+ blood crosses placenta or fetal/maternal blood mixing occurs (in Rh- mother), mother produces anti-Rh antibodies
-Anti-Rh antibodies can cross placenta and damage second fetus that is Rh+ (due to Rh+ father) --> hemolytic disease of the newborn
-Prevention = inject mother with anti-Rh antibodies before first pregnancy --> injected antibodies attack Rh blood rather than mother producing own Rh antibodies
Respiratory Anatomy
Upper - Nasal cavity --> pharynx --> larynx --> (Lower) Trachea --> primary bronchi (L/R) --> smaller bronchi --> bronchioles --> alveoli
Functions of the respiratory system
-Gas exchange (O2 uptake, CO2 release)
-Homeostatic regulation of blood pH
-Conditioning inspired air
-Protection (filtering and clearing foreign particles)
-Vocalization
Steps of External Respiration
-Exchange I = atmosphere to lung (ventilation - breathing [inhale/exhale])
-Exchange II = lungs to blood
-Transport of gases in the blood
-Exchange III = blood to cells
Inspiration vs expiration
Inspiration = air moves into lungs
Expiration = air moves out of lungs
Ventilation vs respiration
Ventilation = breathing (inhale/exhale)
Respiration = gas exchange
Muscles of Ventilation
-Scalenes, external intercostals and diaphragm used at rest (inhalation); exhalation = relaxation of these muscles
-Sternocleidomastoids recruited for forced inhalation; internal intercostals and abdominal muscles recruited for forced exhalation
Pleural membranes
-Like a fluid filled balloon that surrounds lungs
-Visceral pleural membrane = inner; stuck to lungs
-Parietal pleural membrane = outer; stuck to ribs
-Each membrane composed of a thin layer of secretory epithelial cells (secrete pleural fluid) and a thin layer of connective tissue
Pleural fluid
-Fluid-filled pleural sac protects lungs
-Lubricates membranes and allows them to slide against each other as they move during breathing
-"Sticks" the lungs to thoracic wall (keeps lungs inflated) --> ribs expand, outer membrane pulled out, brings inner membrane and lungs with it
-Collapsed lung = loss of integrity of interpleural space
Role of airways
-Filter out foreign substances (ciliated epithelium in trachea/bronchi)
-Warm air to body temperature
-Add water vapour
Ciliated epithelium in respiratory tract
-Columnar ciliated epithelial cells filter out particles trapped in mucus
-Mucus secreted by goblet cells
-Watery saline layer (fluid and ions) between mucus and cilia --> critical for cilia to be able to move mucus layer up and out
-Some channels and pumps to form watery layer
--> move ions out, water follows by osmosis
-Cystic fibrosis = watery saline layer missing, mucus sits on epithelium
Airways and resistance to flow
-Flow ∝ ΔP/R
-R∝Lη/r^4
L = length of airway
η = viscosity of air
r = radius of airway
-Radius is the only factor that can change (due to bronchodilation/constriction) --> only at bronchioles
-Trachea and bronchi cannot change diameter due to cartilage in walls, but mucus buildup can decrease radius
-Histamine = paracrine trigger for bronchoconstriction --> use bronchodilator to cure
-Obstructive lung disease = increased airway resistance
Resistance and cross-sectional area
-Resistance depends on total cross-sectional area
-Most of resistance to flow is in trachea and bronchi (low cross-sectional area)
-Total cross-sectional area of bronchioles is large, so resistance is normally low
Modulation of bronchiolar radius
-Bronchodilation = decreased resistance to air flow --> paracrine response to CO2; SNS response = epinephrine/norepinephrine on β2-adrenergic receptors --> relaxation of muscle (Gs --> AC --> cAMP --> PKA --> MLCK)
-Bronchoconstriction = increased resistance to air flow --> paracrine response to histamine released in immune response by mast cells; PNS response to ACh on muscarinic M3 receptors --> constriction of muscle (Gq --> PLC --> IP3 --> IP3R --> Ca2+)
Alveoli
-Made up of a single layer of epithelium; surrounded by capillaries
-Make up the bulk of lung tissue
-95% of SA = Type I alveolar cells (gas exchange), 5% = Type II alveolar cells (make/secrete surfactant --> lines alveoli making them easier to expand and preventing collapse)
Alveolar exchange surface
-Very thin; very little interstitial fluid
-Alveolus and capillary held close together by fused basement membranes
-Gases must cross 4 membranes during diffusion --> very small distance
Surfactant
-Secreted by Type II alveolar cells
-Decreases surface tension in alveoli
-Prevents alveoli from collapsing
-Makes alveoli easier to expand
Surfactant and surface tension
-At an air-fluid interface, surface of fluid is under tension (attraction b/w fluid molecules)
-Results in an inward directed pressure
-Surfactant decreases tension --> decreases pressure making alveoli easier to expand
Law of LaPlace
P = 2T/r
P = pressure, T = tension, r = radius
Surfactant and Law of LaPlace
-Without surfactant, alveoli would have high inward pressure --> difficult to expand and prone to collapse --> exaggerated effect in small alveoli
-Surfactant reduces surface tension and inward pressure --> reduces work to inflate alveoli
-Smaller alveoli = more surfactant
-Equalizes pressure between large and small alveoli --> equalizes air flow to all alveoli
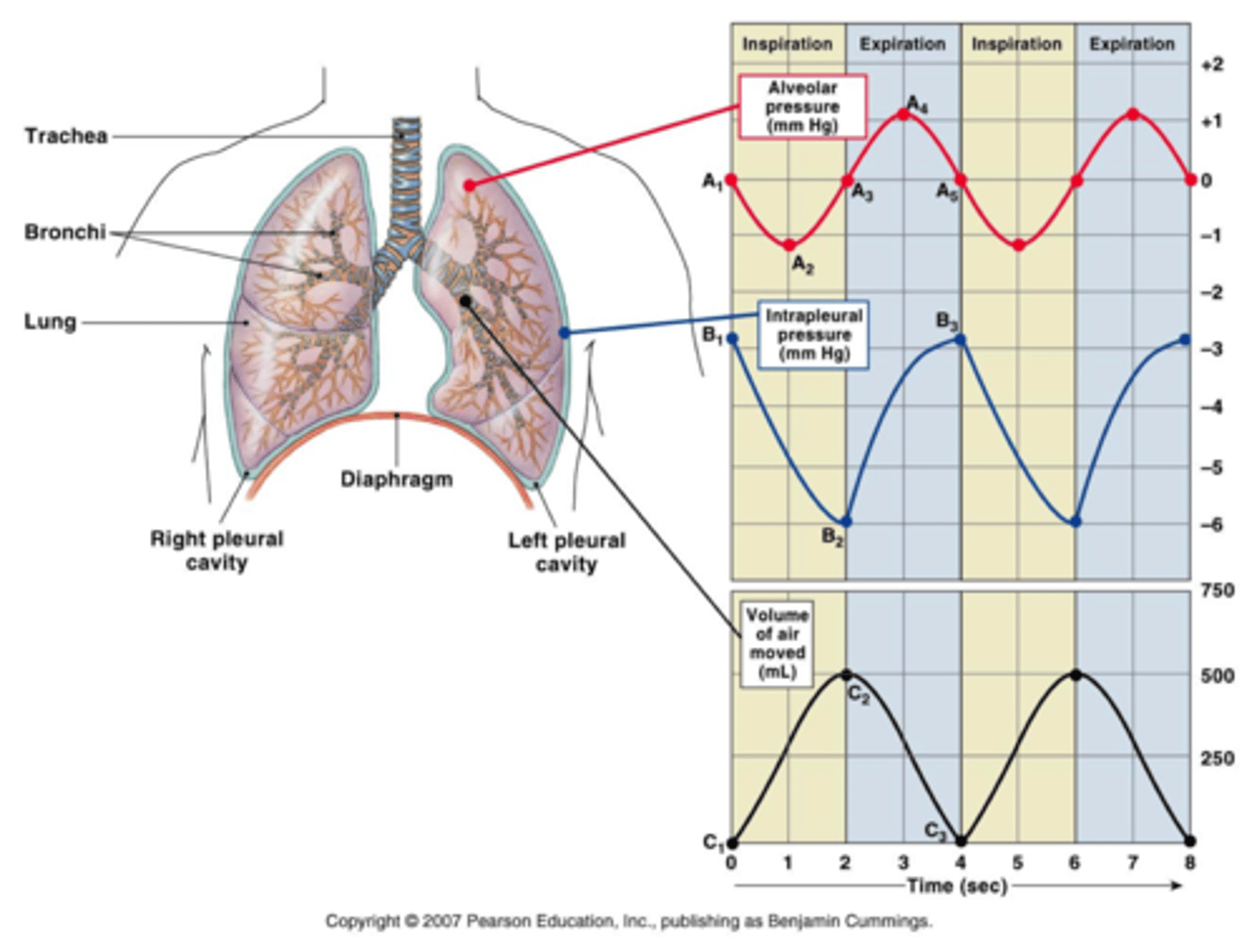
Lung Pressures at rest
-P_atm = 760 mm Hg, used as reference at 0
-P_alv = 0 mm Hg (same as atm)
-P_ip (intrapleural) = -4 mm Hg --> inward pressure between membranes (should always be negative during normal quiet breathing)
-Transpulmonary pressure = pressure difference across lung wall = P_alv - P_ip = 4 mm Hg
-Transpulmonary pressure (distending pressure) is driving force for inflation of lungs
Pneumothorax
-Air enters pleural sac; intrapleural pressure is no longer negative
-Bond holding lungs to chest wall is broken --> lung collapses
Pressure changes during quiet breathing
-During inspiration, P_alv decreases as lungs expand, then increases to equalize air pressure (as air moves into lungs)
-Intrapleural pressure becomes more negative (parietal pulls more due to rib cage movement)
-As P_alv decreases, gradient --> air moves in
-During exhalation, volume of lungs decreases, P_alv increases and then decreases to equalize (as air leaves)
-Intrapleural pressure rises (ribs move in, less opposite pull b/w two pleural membranes)
-As P_alv increases, gradient --> air flows out
Lung compliance
-Ability of lung to stretch
-Due to presence of collagen fibres and elastic fibres (balance of two --> too much collagen = less compliance --> collagen ≠ very stretchy)
-Decreased in restrictive pulmonary diseases (e.g. fibrosis)
Lung elastance
-Ability of lung to spring back after being stretched
-Due to presence of elastin fibres
-Decreased in emphysema (loss of elastin)
Boyle's Law
P1×V1 = P2×V2, Flow ∝ ΔP/R
-When inspiratory muscles contract --> lung volume increases --> pressure inside decreases --> air is "sucked" into lungs
-When inspiratory muscles relax --> lung volume decreases --> pressure inside increases --> air is "blown" out of lungs
Mechanical changes during ventilation
During quiet inspiration
-Diaphragm contracts and flattens
-Muscles of inspiration contract and pull ribs up and out, sternum lifts up
-Thoracic and lung volumes increase, P_ip and P_alv decrease, P_atm>P_alv, air enters
During passive exhalation
-Diaphragm relaxes and moves up
-Muscles of inspiration relax, ribs and sternum "fall" back down
-Thoracic and lung volumes decrease, P_ip and P_alv increase, P_alv>P_atm, air exits
Spirometry
-Measures pulmonary function using a spirometer
Lung Volumes and Capacities
4 Volumes: Tidal volume (V_T), Inspiratory and Expiratory Reserve Volume (IRV/ERV) and Residual Volume (RV)
4 Lung Capacities: Inspiratory capacity (V_T + IRV), Vital Capacity (VC = V_T + IRV + ERV), Total lung capacity (TLC = V_T + IRV + ERV + RV) and Functional residual capacity (ERV + RV)
-Total Pulmonary Ventilation (minute ventilation) = ventilation rate × tidal volume (12 breaths/min × 500 mL/breath) = 6 L/min
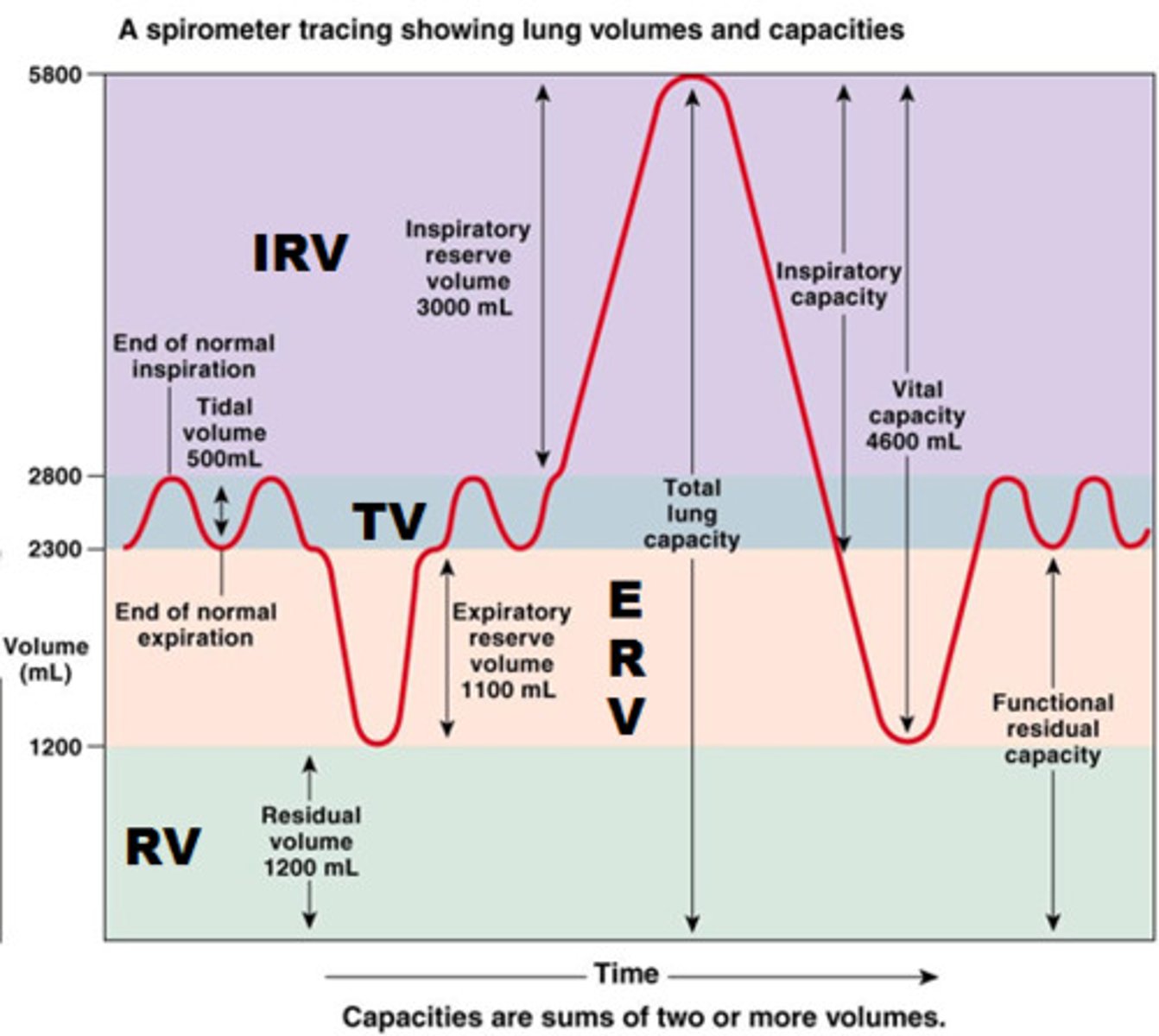
Tidal Volume (V_T)
-Normal breathing volume = 500 mL (inhaled or exhaled)
Expiratory Reserve Volume (ERV)
-Amount of air physiologically capable of exhaling (1100 mL)
Inspiratory Reserve Volume (IRV)
-Amount of air physiologically capable of inhaling (3000 mL)
Residual Volume (RV)
-Volume of air left in lungs (1200 mL)
Inspiratory Capacity
Tidal volume (V_T) + IRV = 500 mL + 3000 mL = 3500 mL
Vital Capacity (VC)
Tidal Volume + IRV + ERV = 500 mL + 3000 mL + 1100 mL = 4600 mL
Total Lung Capacity
Tidal Volume + IRV + ERV + RV = 500 mL + 3000 mL + 1100 mL + 1200 mL = 5800 mL
Functional Residual Capacity
-Amount typically left in lungs during normal breathing = ERV + RV = 1100 mL + 1200 mL = 2300 mL
Ventilation
-Total pulmonary ventilation = ventilation rate * V_T = 6 L/min
-Gas exchange does not occur in conducting airways --> anatomical dead space = 150 mL
-Better indication of ventilation efficiency = alveolar ventilation (volume moved in/out of alveoli per minute)
Alveolar ventilation
Ventilation rate × (V_T - V_d (dead space volume)) = 12 breaths/min × (500 mL - 150 mL) = 4.2 L/min
Alveolar ventilation and anatomical dead space
-At end of inspiration, dead space is filled with fresh air (oxygen rich)
-Exhalation of 500 mL (tidal volume) = first exhaled air from dead space, only 350 mL leaves alveoli
-At end of expiration, dead space is filled with stale (slightly depleted) air from alveoli
-Inhale 500 mL of fresh air --> only 350 mL of fresh air reaches alveoli + 150 mL of stale air from dead space (dead space now filled with fresh air)
Dalton's Law
-The total pressure exerted by a mixture of gases is the sum of the individual partial pressures
Dalton's Law and air pressure
P atm = P_N2 + P_O2 + P_CO2 (78% N2, 21% O2, 0.033% CO2)
-In humid air, P_atm = P_N2 + P_O2 + P_CO2 + P_H2O
Dalton's Law of Partial Pressures
-In dry air, P_gas = P_atm × % of gas in atmosphere
-In humid air, P_gas = (P_atm - P_H2O) × % of gas in atmosphere
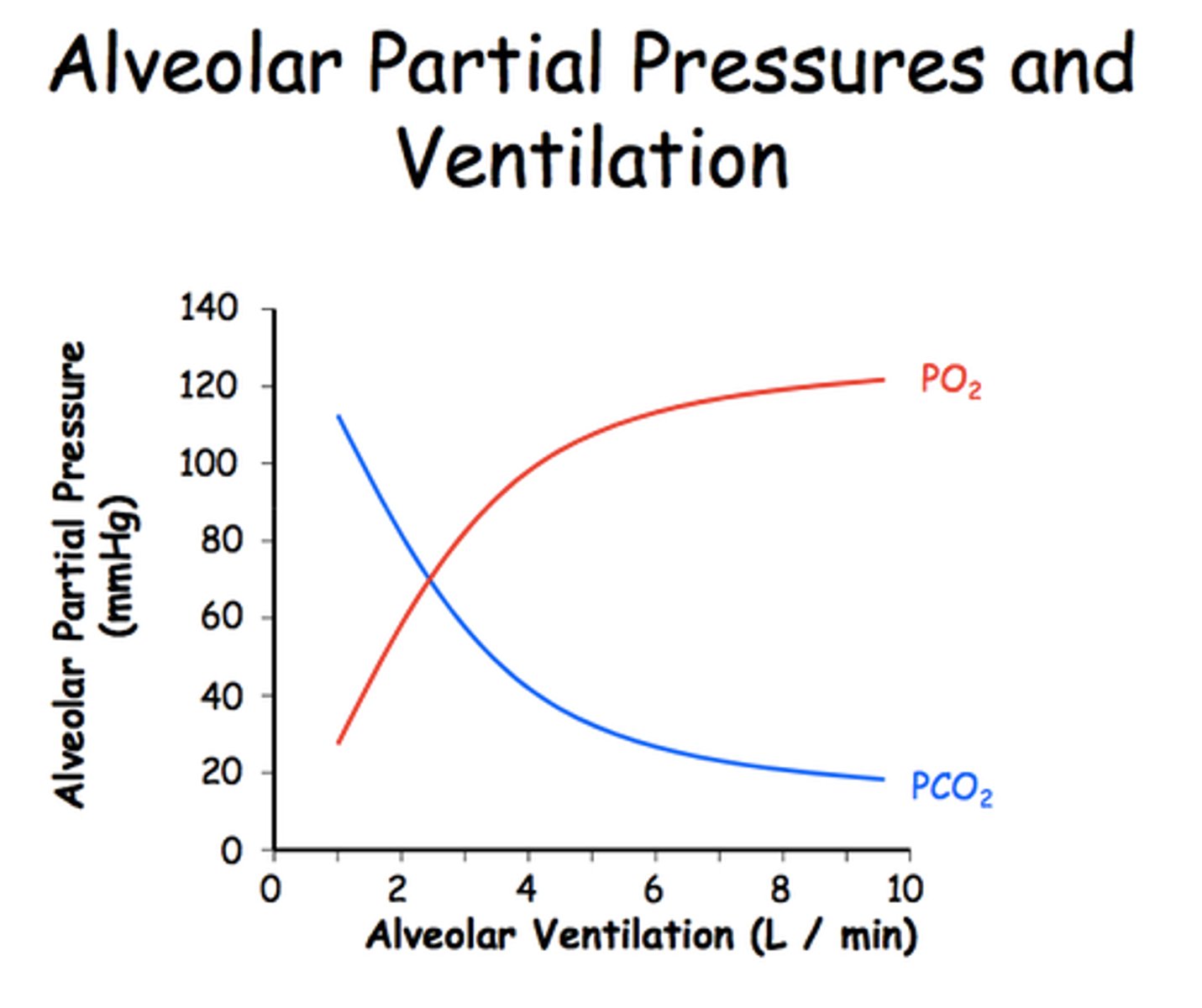
Gas Composition
-In atmosphere, P_O2 = 160 mm Hg, P_CO2 = 0.25 mm Hg
-In alveoli, relatively constant during quiet breathing; P_O2 = 100 mm Hg, P_CO2 = 40 mm Hg
-Match ventilation (breathing) with perfusion (rate of blood flow through pulmonary capillaries)
Pulmonary Gas Exchange/Transport
-Oxygen enters blood at alveolar-capillary interface
-Most of O2 transported attached to Hb in RBC (small amount dissolved in plasma)
-Oxygen diffuses into cells
-Cellular respiration determines metabolic CO2 production --> CO2 diffuses out of cells
-CO2 is transported back via Hb or as HCO3-, or dissolved in plasma (more soluble than O2)
-CO2 enters alveoli at alveolar-capillary interface
Fick's Law
Diffusion Rate ∝ [A × D × (ΔP_gas)]/T^2
A = surface area
D = membrane permeability (D = diffusion constant)
ΔP_gas = partial pressure gradient
T = diffusion distance (depends on membrane thickness, interstitial fluid)
Gasses and Partial Pressure Gradients
-Air moves by bulk flow down partial pressure gradients
Dry Air: PO2 = 160 mm Hg, PCO2 = 0.25 mm Hg
Alveoli: PO2 = 100 mm Hg, PCO2 = 40 mm Hg
Venous Blood: PO2 = <40 mm Hg, PCO2 = >46 mm Hg (want O2 diffusing in, CO2 out)
Tissues: PO2 = <40 mm Hg, PCO2 = >46 mm Hg
Arterial Blood: PO2 = 100 mm Hg, PCO2 = 40 mm Hg
-Diffusion reaches equilibrium under normal circumstances
Factors that affect gas exchange
-Inefficient exchange can lead to low O2 content in blood
Hypoxia = not enough O2 to meet body's needs
Gas exchange is affected by:
-O2 reaching the alveoli (composition of inspired air; alveolar ventilation)
-Alveolar ventilation --> rate/depth of breathing, airway resistance, lung compliance, CNS depression (drugs, alcohol overdose)
-Adequate perfusion of alveoli
-Gas diffusion between alveoli and blood --> surface area; diffusion distance --> barrier thickness, amount of fluid
Emphysema
-Destruction of alveoli = less surface area for gas exchange (affects surface area and gradient)
Asthma
-Increased airway resistance decreases alveolar ventilation
-Affects partial pressure gradient (constricted bronchioles = low PO2 in alveoli)
Fibrotic lung disease
-Thickened alveolar membrane slows gas exchange
-Loss of lung compliance may decrease alveolar ventilation
-Caused by build-up of scar tissue around alveoli from particulate irritants (e.g. asbestos)
-Affects partial pressure gradient, diffusion distance
Pulmonary edema
-Increased fluid in interstitial fluid (often due to heart failure) increases diffusion distance
-Affects diffusion distance
Gas in Solution
-At equilibrium, PO2 in water and air are equal, but low O2 solubility means concentrations are NOT equal
-CO2 is 20x more soluble than O2 --> for same partial pressure, more CO2 dissolved in water --> capacity of plasma for O2 is very low
O2 Transport in Blood
-Total O2 in blood = amount dissolved in plasma + amount bound to Hemoglobin
-In lungs, PO2 is high; drives O2 exchange into plasma --> high plasma PO2 drives binding to Hb (98% bound to Hb, 2% dissolved in plasma)
-In tissues, PO2 is low --> drives O2 exchange out of plasma --> low plasma PO2 drives release from Hb
Hemoglobin
-Found in RBC
-Reversibly binds to O2 (O2 binds to Fe in porphyrin ring)
-Each Hb molecule has the ability to bind 4 O2 molecules
-HbO2 (Hb bound to O2) = oxyhemoglobin
-Greatly increases O2 carrying capacity of blood
O2-Hb Dissociation Curve
-Sigmoidal curve due to cooperative binding --> steep portion 0-40 mm Hg, plateau portion 60-100 mm Hg
-Left shift = increased affinity, right shift = decreased affinity
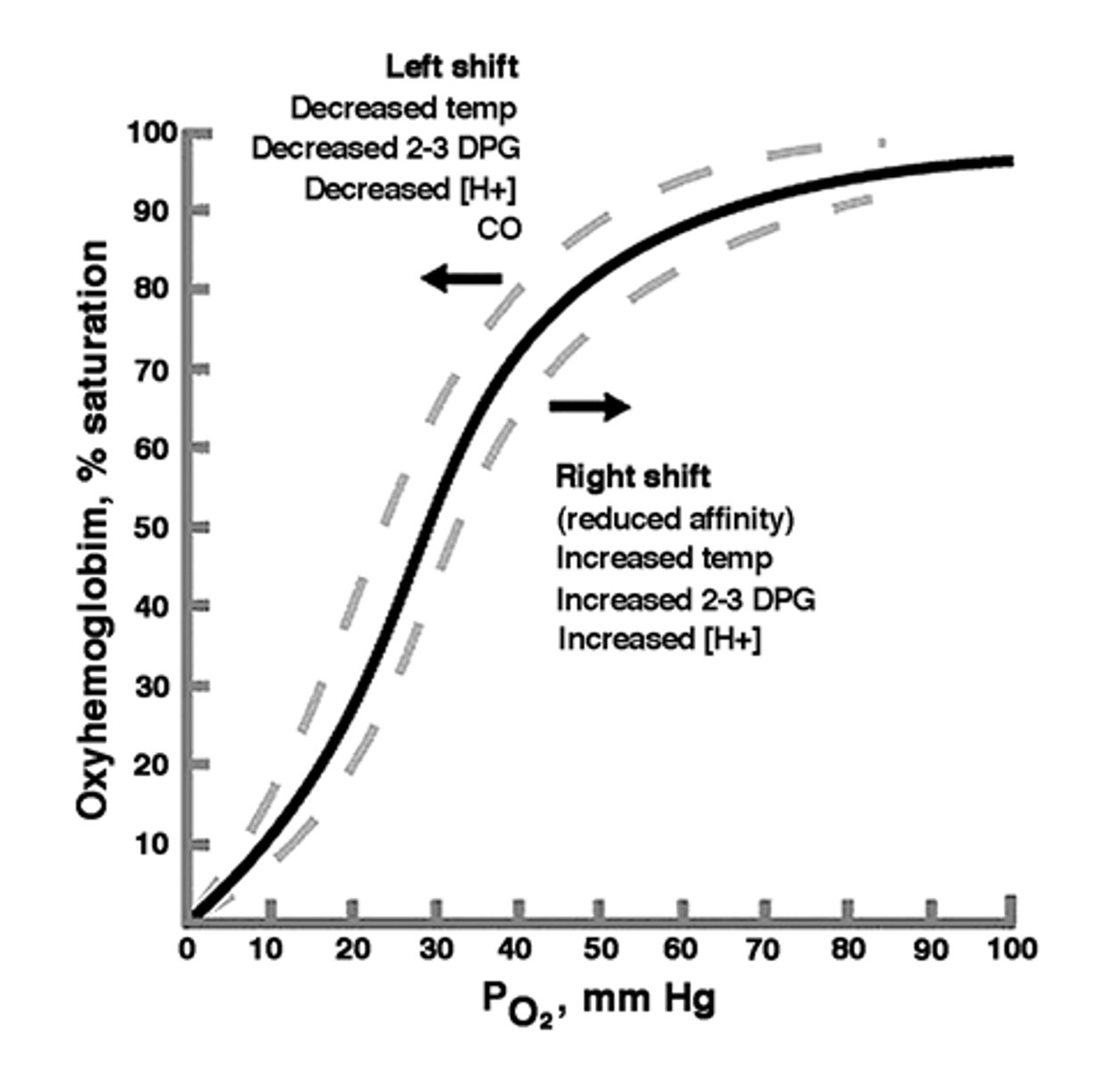
Cooperative binding of O2 to Hb
-Binding of O2 molecules to Hb increases binding affinity of remaining sites
-Creates sigmoidal shape of O2-Hb curve --> in steep region, small change in PO2 results in large change in %Hb saturation
P_50
-The oxygen partial pressure at which hemoglobin is 50% saturated
-As P_50 increases, affinity for O2 decreases
Factors that affect Hb-O2 dissociation curve
Changing pH - Low pH (more acidic) reduces O2 carrying capacity --> right shift
-Normal plasma pH = 7.4; tissues = 7.2 (more acidic due to lactic acid, etc.) --> O2 dissociates more readily in acidic conditions (i.e. tissues)
Changing PCO2 - High PCO2 reduces O2 carrying capacity --> right shift
-Normal PCO2 in plasma = 40 mm Hg, tissues = 80 mm Hg; O2 dissociates more readily at tissues (higher PCO2)
CO2 Transport in Blood
-7% transported dissolved in plasma
-23% transported as HbCO2
-70% transported as bicarbonate (HCO3-) dissolved in plasma
-Converted to bicarbonate by tissues, transported back through venous circulation as bicarbonate, converted back to CO2 at pulmonary circulation for exhalation
-Forward and reverse reactions catalyzed by carbonic anhydrase
Carbonic Anhydrase Reaction
CO2 + H2O <-> H2CO3 (carbonic acid) <-> (HCO3-) + (H+)
-Both forward and reverse reactions catalyzed by carbonic anhydrase
-H+ buffered by Hb in RBC; if excess H+ present = respiratory acidosis
CO2/Bicarbonate Conversion
-CO2 is converted to bicarbonate in RBC's
-Exits RBC and enters plasma as Cl- enters RBC (maintain membrane potential/electrochemical gradient --> chloride shift)
-Re-enters RBC at alveoli to be converted back into CO2; diffuses from plasma to alveoli
-As plasma PCO2 drops, CO2 diffuses out of RBC's (HbCO2 and bicarbonate)
Regulation of Ventilation
-Emotions/voluntary control --> higher brain centres/limbic system --> medulla oblongata/pons --> somatic motor neurons (inhalation and exhalation)
-CO2 --> medullary chemoreceptors --> medulla oblongata/pons --> etc.
-CO2, O2, pH --> carotid/aortic chemoreceptors
--> afferent sensory neurons --> medulla oblongata/pons --> etc.
Chemoreceptors and Ventilation
-Sensory receptors convert chemical signals to action potentials
-Central chemoreceptors = in brainstem (medulla) --> increase activity in response to elevated PCO2 --> increases rate and depth of breathing
-Peripheral chemoreceptors = in aortic arch and carotid artery --> increase activity in response to elevated PCO2 or [H+], or low PO2 --> afferents signal back to respiratory control centre of medulla --> increases rate/depth of breathing
Urinary System
-Composed of kidneys, ureters and urinary bladder
-Kidneys are retroperitoneal (behind peritoneal membrane)
-Ureters carry urine from kidneys to bladder; urethra carries urine to outside of body
Kidney Functions
-Regulation of extracellular fluid volume and blood pressure
-Regulation of osmolarity
-Maintenance of ion balance (Na+, K+, Cl-, Ca2+, PO4(3-))
-Homeostatic regulation of pH (variable excretion of H+ and HCO3-
-Excretion of wastes (creatinine, urea, hormones, uribilinogen)
-Production of hormones (erythropoeitin --> stimulates RBC synthesis; renin --> important regulator of blood pressure)
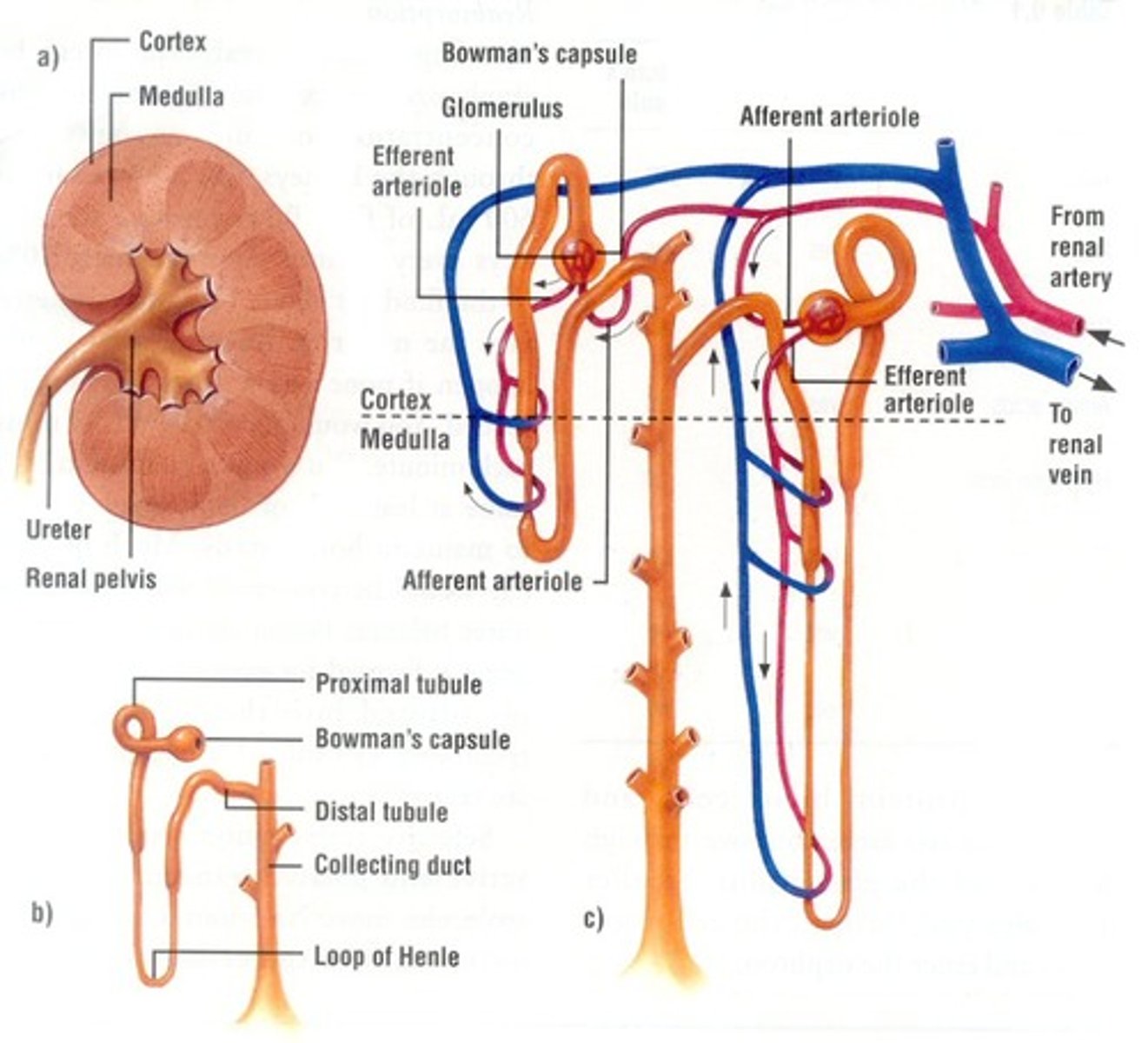
Kidney Anatomy
-Cortex = outside
-Medulla = inside
-Renal pelvis = where smaller collecting ducts join
-Cortex and medulla only differ in what part of nephron is in them

Nephrons
-Cortical nephron = shorter loop (mostly in cortex)
-Juxtamedullary nephron = longer loop of Henle (dips down into medulla) --> arguably more important
-Cortex contains all Bowman's capsules, proximal/distal tubules (for both types of nephrons)
-Medulla contains loops of Henle and collecting ducts
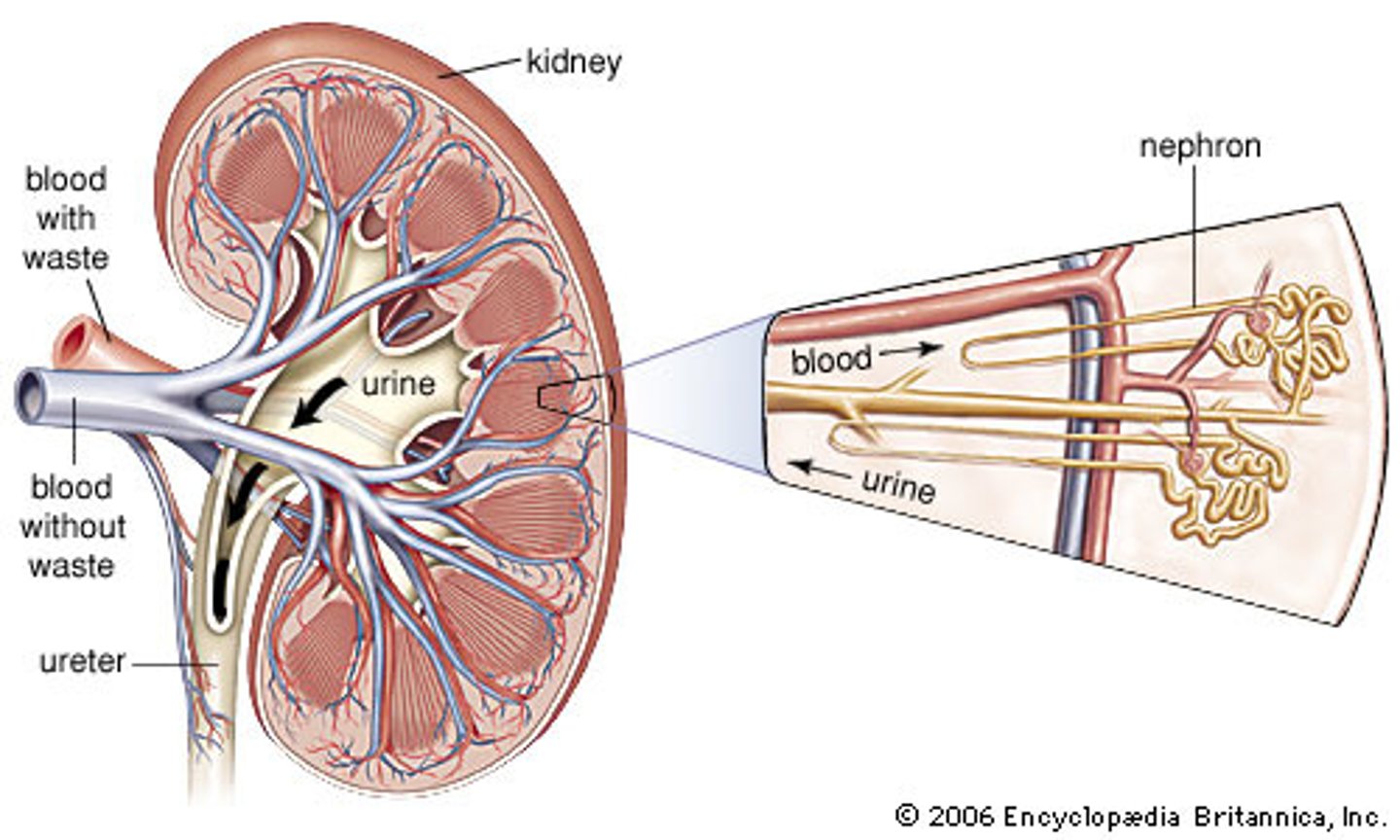
Vasculature of Kidney
-Efferent arteriole = top of glomerulus; afferent = bottom
-Peritubular capillaries surround glomerulus, loop of Henle --> important for recapturing substances (e.g. glucose)
Nephron Anatomy
- Blood from afferent arteriole to glomerulus (inside of Bowman's Capsule)
--> where filtration occurs
- Glomerulus = ball of capillaries
-Glomerulus + Bowman's capsule = renal corpuscle
- Inside Bowman's capsule (outside of glomerulus) = tubular fluid
- Most reabsorption occurs in proximal tubule (e.g. Na+, glucose, amino acids)
- Loop of Henle = down and up (descending limb and ascending limb) --> different functions; permeable to either salt or water --> maintain osmotic gradient
- Variable reabsorption of water depending on body's needs (in distal tubule)
-Collecting duct = no more modifications
--> now urine (no longer tubular fluid)
Processes of the nephron
-Filtration = movement from blood to lumen (passive filtration out of blood) --> occurs at glomerulus/Bowman's capsule
-Secretion = from blood to lumen --> using transporters (e.g. K+, Na+) --> occurs at proximal/distal tubule, collecting duct
-Reabsorption = movement from lumen to blood (e.g. glucose, Na+) --> occurs at proximal/distal tubule, loop of Henle, collecting duct
-Excretion = anything left after filtration, secretion and reabsorption --> at end of collecting duct
Urine excretion
Amount of solute excreted = Amount filtered - amount reabsorbed + amount secreted
Filtration
-Filtration fraction = the % of total plasma volume that filters into the tubule
-100% of plasma volume enters afferent arteriole; 20% filters , 80% leaves via efferent arteriole
-99%+ of filtrate is reabsorbed; <1% of volume is excreted to external environment
Renal Corpuscle and filtration
-Filtered substances cross 3 barriers: glomerular capillary endothelium, basal lamina, epithelium of Bowman's capsule (podocytes)
-Endothelium of capillaries = leaky
-Podocytes have "feet" --> creates spaces for stuff to be filtered
-Endothelium of capillaries --> basal lamina --> podocytes
Glomerular Filtration Rate (GFR)
-The volume of fluid that filters into Bowman's capsule per unit time
-Usually ~180 L/day (100 mL/min)
-Influenced by pressure --> hydrostatic pressure (P_H), Colloid osmotic pressure gradient (π), and fluid pressure within Bowman's capsule (P_fluid)
Osmolarity
-Number of osmotically active particles per litre of solution (osmoles/litre)
-Osmotically active = particles that work to set up an osmolar gradient
-E.g. 1 M glucose = 1 OsM glucose; 1 M NaCl ≈ 1 OsM Na+ and 1 OsM Cl- (≈2 OsM total)
Osmotic Pressure
-The driving force for osmosis
-Can be measured as the force that must be applied to prevent osmosis (water wants to move via osmosis to equalize concentrations)
Colloid osmotic pressure gradient (protein)
-Osmotic pressure gradient due largely to presence of proteins in plasma but not in filtrate
Pressures affecting GFR
Net filtration pressure = P_H - π - P_fluid
-Typically: 55 - 30 - 15 = 10 mm Hg net filtration pressure
GFR and blood pressure
-GFR changes very little despite MAP changing between 80 - 180 mm Hg
-GFR is maintained by regulating renal blood flow
GFR Regulation
-Primarily via altering arteriole resistance
-Increased afferent arteriole resistance --> decreased flow --> decreased P_H and GFR
-Increased efferent arteriole resistance --> blood "pooling" in glomerulus --> increased P_H and GFR
Autoregulation of GFR
-Myogenic response to changes in BP --> intrinsic ability of vascular smooth muscle (stretch due to increased pressure causes vasoconstriction of afferent arterioles --> stretch activated cation channels = smooth muscle contraction)
-Tubuloglomerular feedback = paracrine signalling --> occurs at juxtaglomerular apparatus (JGA) - where ascending/descending limbs of loop of Henle pass between afferent/efferent arterioles --> Macula densa (specialized cell of ascending limb) sense increased [Na+] and [Cl-] due to high GFR
--> release paracrines --> causes vasoconstriction of afferent arteriole
Tuboglomerular feedback
-GFR increased = flow through tubule increases = flow past macula densa increase
-Macula densa releases paracrines on afferent arteriole --> causes vasoconstriction
-Increased resistance --> decreased P_H and GFR
-Senses based on [Na+] and [Cl-] b/c if GFR is high, fluid moves too quickly to reabsorb
Nephron Reabsorption
-Movement from tubule lumen into blood
-Most reabsorption occurs in proximal tubule
-Both transepithelial (crosses both apical and basolateral membranes via transporters) and paracellular (passes through tight junctions of adjacent cells) pathways
Nephron Reabsorption and Na+
-Primarily driven by Na+ movement
-Na+ reabsorbed by primary active transport (enters cell via membrane proteins, moving down electrochemical gradient; pumped out of basolateral side by Na+-K+-ATPase) --> electrochemical gradient drives anion reabsorption --> water follows by osmosis --> permeable solutes reabsorbed by diffusion through membrane transporters/paracellular pathways (lumen concentrations increase as water leaves)
Sodium-linked Secondary Active Transport
-E.g. glucose
-Different types of transporters --> e.g. in proximal tubule, high [glucose], can use uniport (GLUT)
-For lower [glucose], cannot use GLUT; use SGLT (sodium glucose linked transporter --> Na+ down gradient, glucose up)
Reabsorption
-Peritubular capillaries have low hydrostatic pressure
-Colloid osmotic pressure creates gradient that favours reabsorption
Secretion (Nephron)
-Important in homeostatic regulation (K+/H+)
-Important in removing organic compounds from the body (metabolites produced by the body - creatinine, urea, NH4+, etc.; foreign substances - drugs)
-Increasing secretion enhances nephron excretion (more tubular fluid)