MCQs FINAL Gen. Path.
1/340
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
341 Terms
What is pathology? (2)
a) the science that studies the changes at cellular, tissue and organ level caused by diseases
b) the science that studies the body structure and morphology
c) medical discipline which aims to find the cause of death when a crime is suspected
d) medical discipline which provides the morphological diagnosis for the clinical practice
What is pathology? (2)
a) the science that studies the changes at cellular, tissue and organ level caused by diseases
b) the science that studies the body structure and morphology
c) medical discipline which aims to find the cause of death when a crime is suspected
d) medical discipline which provides the morphological diagnosis for the clinical practice
Define the main branches of pathology: (3)
a) general pathology
b) clinical pathology
c) systemic pathology
d) experimental pathology
Define the main branches of pathology: (3)
a) general pathology
b) clinical pathology
c) systemic pathology
d) experimental pathology
Mark the correct statements: (2)
a) “clinical pathology” builds up a theoretical idea of the pathological process
b) “general pathology” studies the specific morphological changes in organs and systems caused by a particular disease
c) “experimental pathology” researches the diseases using experimental animals and follows up the morphological changes caused by their treatment
d) a and b statements are correct in reverse manner
Mark the correct statements: (2)
a) “clinical pathology” builds up a theoretical idea of the pathological process
b) “general pathology” studies the specific morphological changes in organs and systems caused by a particular disease
c) “experimental pathology” researches the diseases using experimental animals and follows up the morphological changes caused by their treatment
d) a and b statements are correct in reverse manner
What are the possible outcomes of a disease?
a) recovery
b) to become chronic
c) death
d) all of the above
What are the possible outcomes of a disease?
a) recovery
b) to become chronic
c) death
d) all of the above
Which of the following isn’t a sign of death?
a) livores
b) rigor mortis
c) decay
d) calor
Which of the following isn’t a sign of death?
a) livores
b) rigor mortis
c) decay
d) calor
Mark the correct statement(s):
a) Algor mortis is stiffness of muscles after death
b) Rigor mortis is drying of the body after death
c) Livores are a violet-colored skin areas which develop after death
d) Decay is an early sign of death
Mark the correct statement(s):
a) Algor mortis is stiffness of muscles after death
b) Rigor mortis is drying of the body after death
c) Livores are a violet-colored skin areas which develop after death
d) Decay is an early sign of death
algor mortis - cooling
think of alaska - cold
rigor mortis - stiffness, rigidity
Which are the specific methods of pathology? (2)
a) autopsy
b) biopsy
c) clinical examination
d) clinical laboratory tests
Which are the specific methods of pathology? (2)
a) autopsy
b) biopsy
c) clinical examination
d) clinical laboratory tests
Which of the followings are methods for taking biopsy?
a) excision
b) incision
c) surgical
d) all of the listed
Which of the followings are methods for taking biopsy?
a) excision
b) incision
c) surgical
d) all of the listed
Which are the purposes of pathological autopsy? (2)
a) to accuse the clinicians of medical malpractice
b) to establish the cause of death and the definitive diagnosis
c) to help and educate clinicians and to improve their work
d) to help the relatives of the deceased to convict the doctors
Which are the purposes of pathological autopsy? (2)
a) to accuse the clinicians of medical malpractice
b) to establish the cause of death and the definitive diagnosis
c) to help and educate clinicians and to improve their work
d) to help the relatives of the deceased to convict the doctors
Which are the conditions for an autopsy to be done?
a) death occurred in a hospital due to a disease
b) available medical history of the patient
c) presence of the treating doctor
d) all of the listed above
Which are the conditions for an autopsy to be done?
a) death occurred in a hospital due to a disease
b) available medical history of the patient
c) presence of the treating doctor
d) all of the listed above
What are the characteristics of a frozen section? (3)
a) urgent diagnosis given during an operation
b) the preparation of the tissue samples is done by a paraffin method
c) the preparation of the tissue samples is done on a freezing microtome
d) sometimes the diagnosis is not exactly clear because of the preparation method but information like “malignant tumor”, “benign tumor” or “inflammation” is given to the surgeons to know how to proceed with the operation
What are the characteristics of a frozen section? (3)
a) urgent diagnosis given during an operation
b) the preparation of the tissue samples is done by a paraffin method
c) the preparation of the tissue samples is done on a freezing microtome
d) sometimes the diagnosis is not exactly clear because of the preparation method but information like “malignant tumor”, “benign tumor” or “inflammation” is given to the surgeons to know how to proceed with the operation
Which fixative is most commonly used?
a) Bouin solution
b) absolute alcohol
c) formalin 10%
d) salts of heavy metals
Which fixative is most commonly used?
a) Bouin solution
b) absolute alcohol
c) formalin 10%
d) salts of heavy metals
What fixative should be used for a liver biopsy from a baby with a suspected inherited metabolic disease?
a) formalin 10%
b) 1,5-4% glutaraldehyde
c) frozen section
d) Zenker’s fixative
What fixative should be used for a liver biopsy from a baby with a suspected inherited metabolic disease?
a) formalin 10%
b) 1,5-4% glutaraldehyde
This is because glutaraldehyde is commonly used for electron microscopy, which is essential for the evaluation of many inherited metabolic diseases
It preserves cellular structures well and is ideal for the examination of intracellular organelles, which can be critical in diagnosing these conditions
c) frozen section
d) Zenker’s fixative
What is the role of immunohistochemical stains? (2)
a) to give urgent answers about the diagnosis or at least orientation about the pathological process during surgery
b) to determine the histogenesis of the tumor especially in highly undifferentiated malignant tumors
c) to determine the proliferative activity and the hormonal receptors of the tumor that is highly important for the treatment
d) to help determine the cause of death
What is the role of immunohistochemical stains? (2)
a) to give urgent answers about the diagnosis or at least orientation about the pathological process during surgery
b) to determine the histogenesis of the tumor especially in highly undifferentiated malignant tumors
c) to determine the proliferative activity and the hormonal receptors of the tumor that is highly important for the treatment
d) to help determine the cause of death
Cytokeratin, S-100 protein, Vimentin, Desmin, CD-20 are examples of:
a) special stains to prove different substances
b) immunohistochemical markers
Cytokeratin, S-100 protein, Vimentin, Desmin, CD-20 are examples of:
a) special stains to prove different substances
b) immunohistochemical markers
they common, there is no stains called “S-100 protein” and the rest of them, names of proteins - so immunohistochemical to detect them!
Cytokeratin, S-100 protein, Vimentin, Desmin, and CD-20 are examples of immunohistochemical markers.
These markers are used to identify specific types of cells, tissues, or diseases in pathology, and each one is associated with certain cell types or conditions:
Cytokeratin: Found in epithelial cells.
S-100 protein: Typically expressed in neural cells, especially Schwann cells, melanocytes, and dendritic cells.
Vimentin: A marker of mesenchymal cells (e.g., fibroblasts, endothelial cells).
Desmin: Found in muscle cells, particularly in smooth muscle and striated muscle.
CD-20: A marker for B cells, used in immunophenotyping, particularly for lymphomas.
These markers are used in pathology
In which cases a pathological autopsy is performed?
a) when there is suspicion for diagnostic or therapeutic malpractice
b) death of a person outside the hospital
c) when there is suspicion of violent death
d) death of a patient in the hospital and when the relatives don’t ask the principal to cancel the autopsy
In which cases a pathological autopsy is performed?
a) when there is suspicion for diagnostic or therapeutic malpractice
b) death of a person outside the hospital
c) when there is suspicion of violent death
d) death of a patient in the hospital and when the relatives don’t ask the principal to cancel the autopsy
PATHOLOGOGICAL AUTOPSY subjects are ALWAYS NON-VIOLENT DEATHS!!!
if violent, it would be sent for FORENSICS!!
Which of the followings is not a part of performing an autopsy?
a) dissection of organs
b) opening the body
c) taking biopsy from organ changes
d) extraction of abdominal and thoracic organs
Which of the followings is not a part of performing an autopsy?
a) dissection of organs
b) opening the body
c) taking biopsy from organ changes
d) extraction of abdominal and thoracic organs
biopsy is for LIVING organisms - a small part of the affected organ, whereas autopsy takes the ENTIRE ORGANS/TISSUES
An autopsy involves the examination and dissection of the body and its organs after death, with the aim of determining the cause of death or investigating the disease process
However, taking a biopsy (which typically refers to removing a small sample of tissue for further examination in a living patient) is not a standard part of the autopsy process, as the entire organ or tissue is usually examined during the procedure
Size, shape, elasticity, consistency, color and cut surface are characteristics of:
a) microscopic examination of organs
b) gross examination of organs
c) ultramicroscopic examination of organs
d) none of the listed
Size, shape, elasticity, consistency, color and cut surface are characteristics of:
a) microscopic examination of organs
b) gross examination of organs
c) ultramicroscopic examination of organs
d) none of the listed
Indicate correctly the name of the described test. The pericardial sac is cut in Y-like section and filled with water, after that, in the presence of a witness, the right ventricle is punctured with a knife.
a) test for thromboembolism
b) test for pneumothorax
c) test for air and gas embolism
d) test for fat embolism
Indicate correctly the name of the described test. The pericardial sac is cut in Y-like section and filled with water, after that, in the presence of a witness, the right ventricle is punctured with a knife.
a) test for thromboembolism
b) test for pneumothorax
c) test for air and gas embolism
d) test for fat embolism
if WATER is involved, then they want to see bubbling (gas)
Indicate correctly the name of the described test. The pulmonary artery is cut at the place of truncus pulmonalis. Tweezers are inserted and the content of the artery is taken out for examination.
a) test for pneumothorax
b) test for air and gas embolism
c) test for thromboembolism
d) test for fat embolism
Indicate correctly the name of the described test. The pulmonary artery is cut at the place of truncus pulmonalis. Tweezers are inserted and the content of the artery is taken out for examination.
a) test for pneumothorax
b) test for air and gas embolism
c) test for thromboembolism
d) test for fat embolism
Indicate correctly the name of the described test. A pocket between the skin and the ribs is formed and is filled with water. In the presence of a witness, the thorax is punctured with a thin knife in an intercostal space.
a) test for air and gas embolism
b) test for fat embolism
c) test for thromboembolism
d) test for pneumothorax
Indicate correctly the name of the described test. A pocket between the skin and the ribs is formed and is filled with water. In the presence of a witness, the thorax is punctured with a thin knife in an intercostal space.
a) test for air and gas embolism
b) test for fat embolism
c) test for thromboembolism
d) test for pneumothorax
Where is the main accumulation of glycogen in patients with diabetes?
a) in epithelial cells of convoluted tubules and Henle’s loop
b) in epithelial cells of gastrointestinal mucosa
c) in the nuclei and in the cytoplasm of the hepatocytes
d) endothelial cells of the vessels
Where is the main accumulation of glycogen in patients with diabetes?
a) in epithelial cells of convoluted tubules and Henle’s loop
b) in epithelial cells of gastrointestinal mucosa
c) in the nuclei and in the cytoplasm of the hepatocytes
d) endothelial cells of the vessels
A - you remember from another MCQ and diabetic nephropathy, but ALSO remember that diabetic hepatopathy or non-alcoholic fatty liver disease=
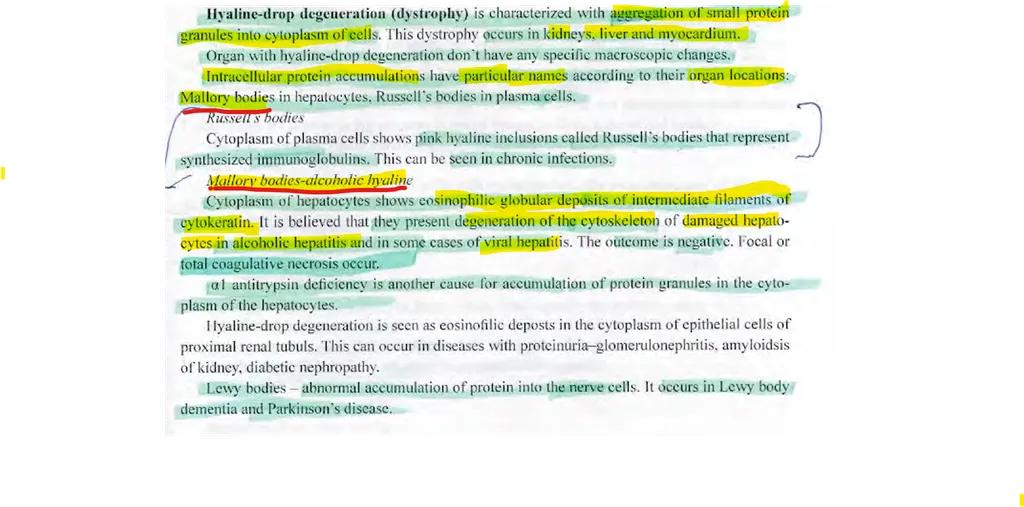
Mark the correct statement(s) for Mallory bodies?
a) they are accumulations of glycogen in the cytoplasm of the hepatocytes
b) they are hyaline inclusions in the cytoplasm of the hepatocytes
c) they are caused by consumption of toxic mushrooms
d) they are seen in Wilson’s disease, liver cancer, primary biliary cirrhosis but mainly in alcoholic disease
Mark the correct statement(s) for Mallory bodies?
a) they are accumulations of glycogen in the cytoplasm of the hepatocytes
b) they are hyaline inclusions in the cytoplasm of the hepatocytes
c) they are caused by consumption of toxic mushrooms
d) they are seen in Wilson’s disease, liver cancer, primary biliary cirrhosis but mainly in alcoholic disease
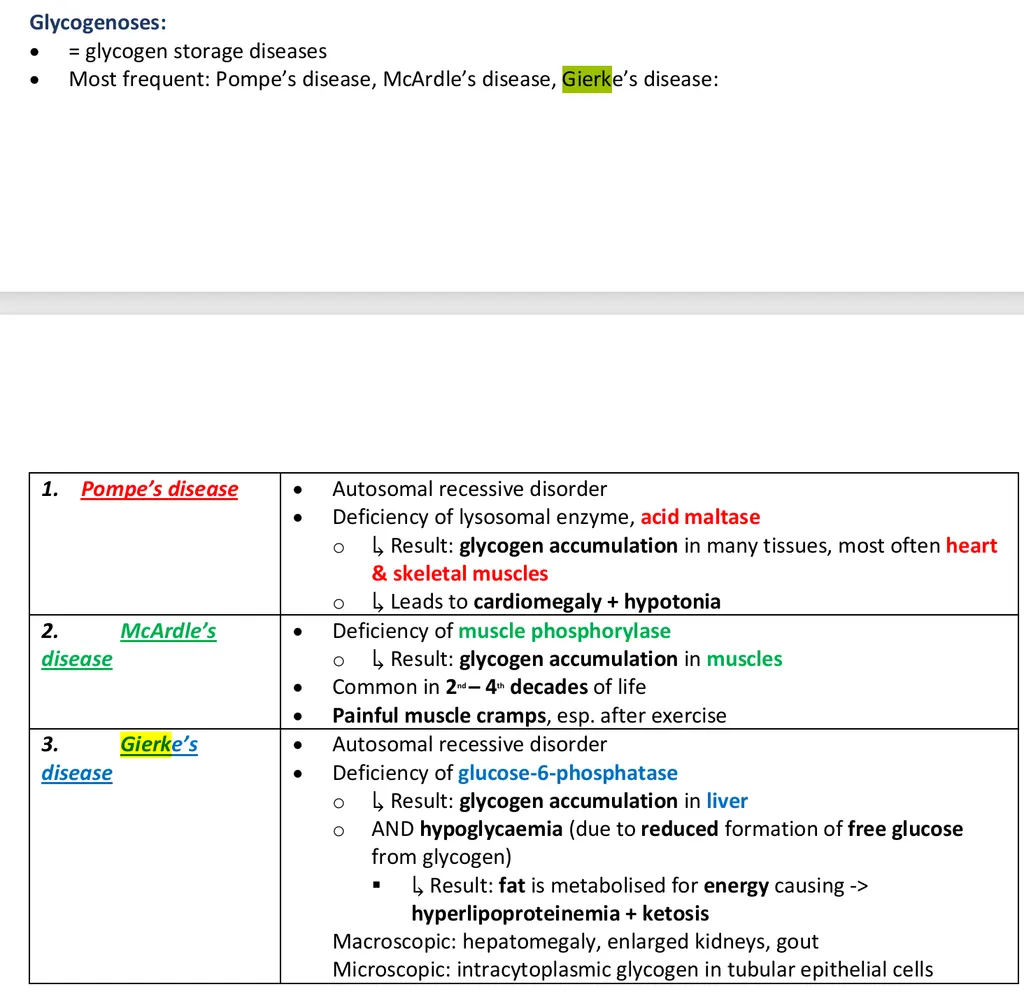
Mark the correct statement(s) for Von Gierke’s disease? (2)
a) it is a genetic autosome-recessive disease
b) another name is glycogenosis type II
c) it affects mainly the heart leading to severe heart failure in infants
d) there is excessive storage of normal glycogen in the liver and kidneys
Mark the correct statement(s) for Von Gierke’s disease? (2)
a) it is a genetic autosome-recessive disease
b) another name is glycogenosis type II
c) it affects mainly the heart leading to severe heart failure in infants
d) there is excessive storage of normal glycogen in the liver and kidneys
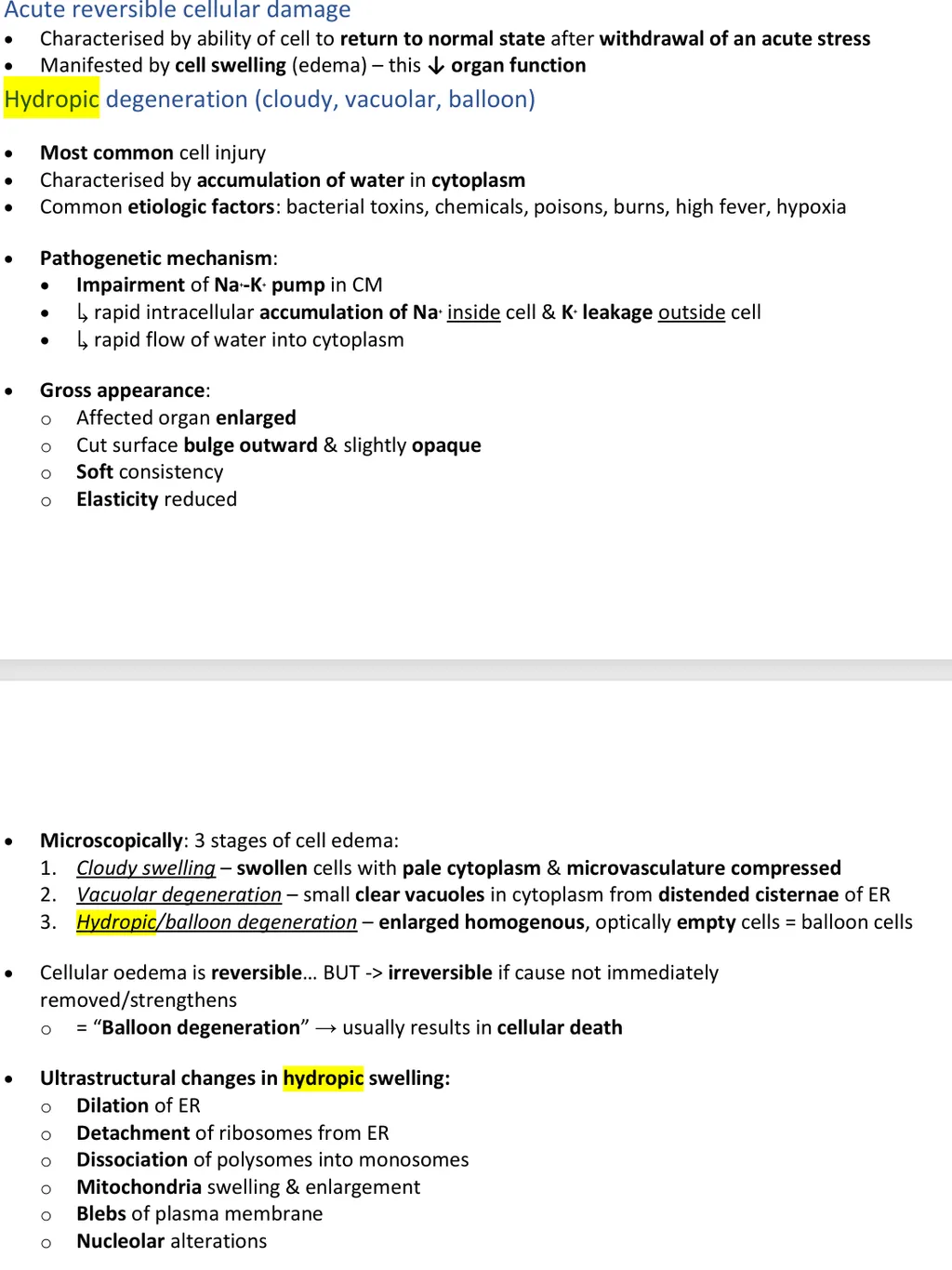
Mark the correct statement(s) for cellular edema
a) it is abnormal accumulation of water in the cytoplasm
b) it is reversible cellular injury
c) cells are small and shrunken
d) there are a few etiological factors that caused cellular edema
Mark the correct statement(s) for cellular edema
a) it is abnormal accumulation of water in the cytoplasm
b) it is reversible cellular injury
c) cells are small and shrunken
d) there are a few etiological factors that caused cellular edema
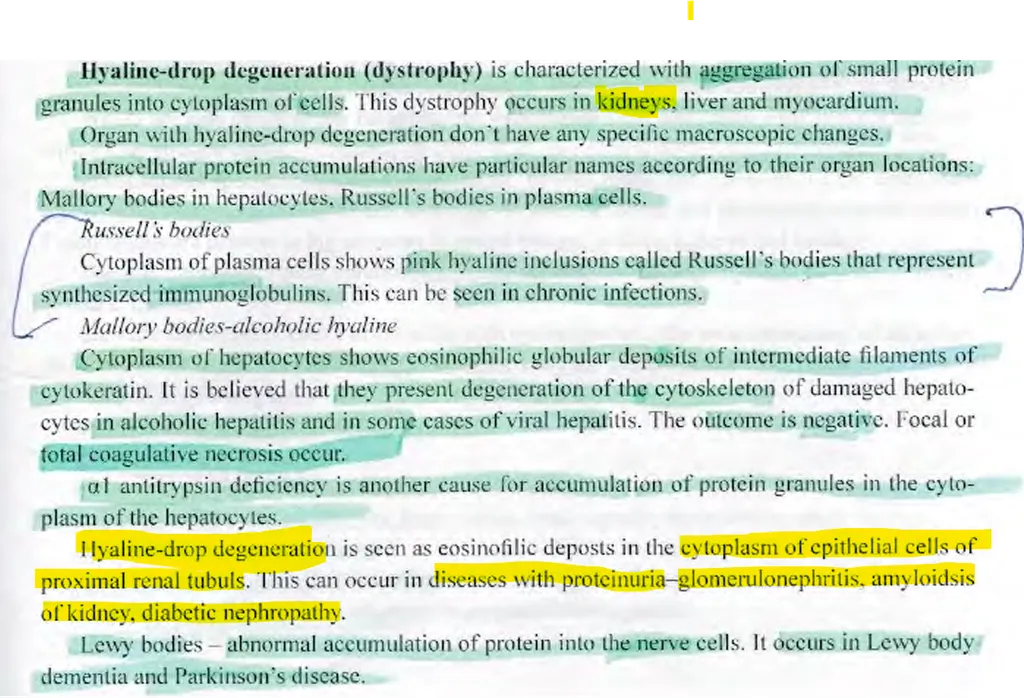
Abnormal intracellular accumulation of proteins can be seen in:
a) the epithelial cells of the proximal tubules in proteinuria
b) in the cardiomyocytes in heart infarction
c) in the plasma cells in chronic inflammatory diseases as Russel’s bodies
d) in the cells of pancreatic islets in diabetes mellitus
Abnormal intracellular accumulation of proteins can be seen in:
a) the epithelial cells of the proximal tubules in proteinuria
b) in the cardiomyocytes in heart infarction
c) in the plasma cells in chronic inflammatory diseases as Russel’s bodies
d) in the cells of pancreatic islets in diabetes mellitus
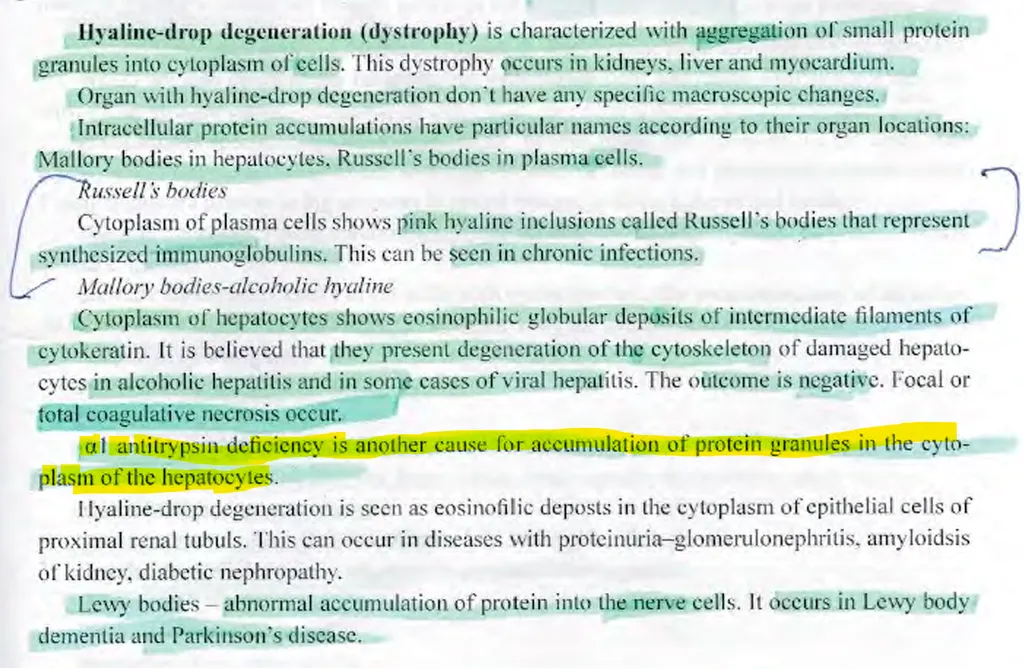
The abnormal inclusions in the hepatocytes in alpha-1 antitrypsin deficiency are composed of:
a) glycogen
b) lipids
c) bile
d) proteins
The abnormal inclusions in the hepatocytes in alpha-1 antitrypsin deficiency are composed of:
a) glycogen
b) lipids
c) bile
d) proteins
“Hyaline droplets” in the epithelial cells of renal tubules is another name for:
a) glycogen inclusions
b) protein inclusions
c) vacuolar degeneration
d) lipid inclusions
“Hyaline droplets” in the epithelial cells of renal tubules is another name for:
a) glycogen inclusions
b) protein inclusions
c) vacuolar degeneration
d) lipid inclusions
Vacuolar degeneration and hydropic degeneration are more severe stages of:
a) fatty degeneration
b) protein degeneration
c) cellular edema
d) glycogen accumulation
Vacuolar degeneration and hydropic degeneration are more severe stages of:
a) fatty degeneration
b) protein degeneration
c) cellular edema
d) glycogen accumulation
PAS reaction with PAS control is used to distinguish:
a) cholesterol from other lipids
b) glycogen from mucus
c) DNA from RNA
d) denatured intracellular proteins from accumulated extracellular proteins
PAS reaction with PAS control is used to distinguish:
a) cholesterol from other lipids
b) glycogen from mucus
c) DNA from RNA
d) denatured intracellular proteins from accumulated extracellular proteins
PAS-control is done using:
a) sulfuric acid
b) hydrochloric acid
c) amylase
d) picric acid
PAS-control is done using:
a) sulfuric acid
b) hydrochloric acid
c) amylase
d) picric acid
PAS-control is done to check the presence of
mucopolysaccharides fromglycogenIt is stained magenta/red with PAS and with amylase added the red colour disappears
What is fatty degeneration?
a) abnormal accumulation of lipids in parenchymal cells
b) abnormal accumulation of lipids in the specialized fatty cells
c) abnormal accumulation of lipids in the ECM of an organ
d) abnormal accumulation of cholesterol in the large and medium-sized vessels
What is fatty degeneration?
a) abnormal accumulation of lipids in parenchymal cells
b) abnormal accumulation of lipids in the specialized fatty cells
c) abnormal accumulation of lipids in the ECM of an organ
d) abnormal accumulation of cholesterol in the large and medium-sized vessels
fatty degeneration - deposition of fats in parenchymal cells of e.g. liver → hepatocytes, heart → papillary muscles (tiger heart), kidney → nephrotic syndrowme “large white kidney”
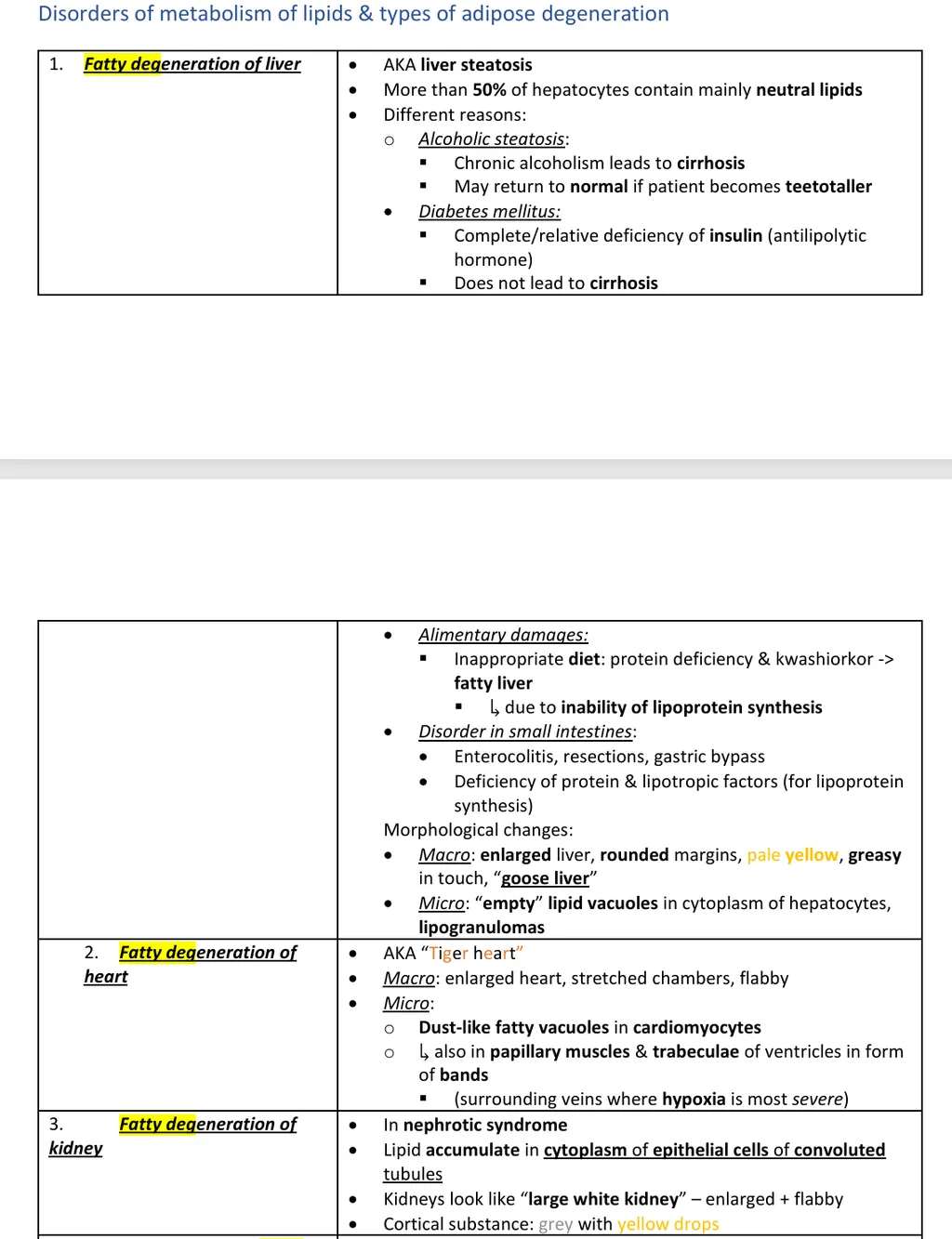
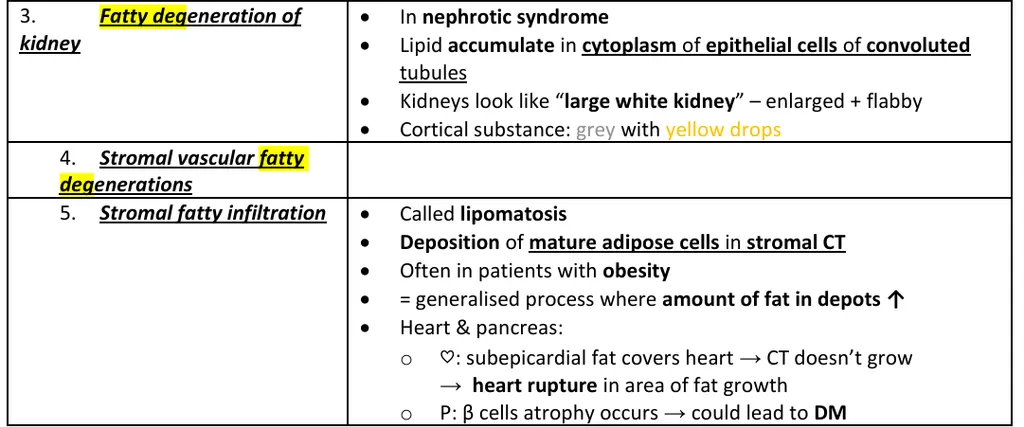
What is lipomatosis?
a) abnormal accumulation of lipids in parenchymal cells
b) abnormal accumulation of lipids in the specialized fatty cells
c) abnormal accumulation of lipids in the cells of the interstitium of an organ
d) abnormal accumulation of cholesterol in the large and medium-sized vessels
What is lipomatosis?
a) abnormal accumulation of lipids in parenchymal cells
b) abnormal accumulation of lipids in the specialized fatty cells
c) abnormal accumulation of lipids in the cells of the interstitium of an organ
d) abnormal accumulation of cholesterol in the large and medium-sized vessels
What is obesity?
a) abnormal accumulation of lipids in parenchymal cells
b) abnormal accumulation of lipids in the specialized fatty cells
c) abnormal accumulation of lipids in the cells of the interstitium of an organ
d) abnormal accumulation of cholesterol in the large and medium-sized vessels
What is obesity?
a) abnormal accumulation of lipids in parenchymal cells
b) abnormal accumulation of lipids in the specialized fatty cells
c) abnormal accumulation of lipids in the cells of the interstitium of an organ
d) abnormal accumulation of cholesterol in the large and medium-sized vessels
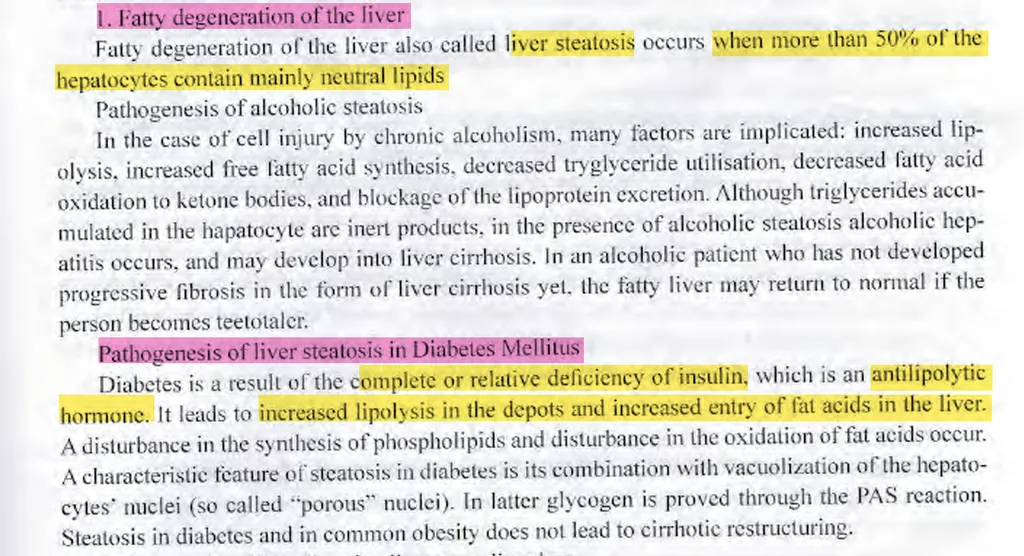
What is the relation between fatty degeneration of the liver and diabetes?
a) there is no relation between them
b) patients with diabetes have increased intake of lipids to provide more energy
c) the fatty liver in diabetes is caused by increased lipolysis and increased delivery of fatty acids in the liver
d) the fatty liver leads to diabetes mellitus
What is the relation between fatty degeneration of the liver and diabetes?
a) there is no relation between them
b) patients with diabetes have increased intake of lipids to provide more energy
c) the fatty liver in diabetes is caused by increased lipolysis and increased delivery of fatty acids in the liver
d) the fatty liver leads to diabetes mellitus
What is android type of obesity?
a) also called “male” or “apple” type, it is the accumulation of lipids in the fatty cells around the shoulders, thorax and waist
b) also called “female” or “pear” type, it is the accumulation of lipids in the fatty cells around the hips, tights and legs
c) generalized obesity predominantly on the face, shoulders and thorax
d) generalized obesity predominantly in the tights, hips and legs
What is android type of obesity?
a) also called “male” or “apple” type, it is the accumulation of lipids in the fatty cells around the shoulders, thorax and waist
b) also called “female” or “pear” type, it is the accumulation of lipids in the fatty cells around the hips, tights and legs
c) generalized obesity predominantly on the face, shoulders and thorax
d) generalized obesity predominantly in the tights, hips and legs
What is gynoid type of obesity?
a) also called “male” or “apple” type, it is the accumulation of lipids in the fatty cells around the shoulders, thorax and waist
b) also called “female” or “pear” type, it is the accumulation of lipids in the fatty cells around the hips, tights and legs
c) generalized obesity predominantly on the face, shoulders and thorax
d) generalized obesity predominantly in the tights, hips and legs
What is gynoid type of obesity?
a) also called “male” or “apple” type, it is the accumulation of lipids in the fatty cells around the shoulders, thorax and waist
b) also called “female” or “pear” type, it is the accumulation of lipids in the fatty cells around the hips, tights and legs
c) generalized obesity predominantly on the face, shoulders and thorax
d) generalized obesity predominantly in the tights, hips and legs
What is upper type of obesity?
a) also called “male” or “apple” type, accumulation of lipids in the fatty cells around the shoulders, thorax and waist
b) also called “female” or “pear” type, it is the accumulation of lipids in the fatty cells around the hips, tights and legs
c) generalized obesity predominantly on the face, shoulders and thorax
d) generalized obesity predominantly in the tights, hips and legs
What is upper type of obesity?
a) also called “male” or “apple” type, accumulation of lipids in the fatty cells around the shoulders, thorax and waist
b) also called “female” or “pear” type, it is the accumulation of lipids in the fatty cells around the hips, tights and legs
c) generalized obesity predominantly on the face, shoulders and thorax
d) generalized obesity predominantly in the tights, hips and legs
What is lower type of obesity?
a) also called “male” or “apple” type, it is the accumulation of lipids in the fatty cells around the shoulders, thorax and waist
b) also called “female” or “pear” type – accumulation of lipids in the fatty cells around the hips, tights and legs
c) generalized obesity predominantly on the face, shoulders and thorax
d) generalized obesity predominantly in the thighs, hips and legs
What is lower type of obesity?
a) also called “male” or “apple” type, it is the accumulation of lipids in the fatty cells around the shoulders, thorax and waist
b) also called “female” or “pear” type – accumulation of lipids in the fatty cells around the hips, tights and legs
c) generalized obesity predominantly on the face, shoulders and thorax
d) generalized obesity predominantly in the thighs, hips and legs
Which type of obesity has worse prognosis?
a) gynoid type
b) male type
c) the obesity doesn’t affect the patient’s health
d) all of the obesity types have the same prognosis
Which type of obesity has worse prognosis?
a) gynoid type
b) male type
c) the obesity doesn’t affect the patient’s health
d) all of the obesity types have the same prognosis
In “tiger heart” the abnormal accumulation of lipids is:
a) in the cell of the heart’s interstitium,
b) in the cells around the pericardium,
c) in the cardiomyocytes of the papillary muscles along the venules and the venous part of the capillaries,
d) in the cardiomyocytes of the anterior wall of the left heart chamber
In “tiger heart” the abnormal accumulation of lipids is:
a) in the cell of the heart’s interstitium,
b) in the cells around the pericardium,
c) in the cardiomyocytes of the papillary muscles along the venules and the venous part of the capillaries,
d) in the cardiomyocytes of the anterior wall of the left heart chamber
Which exogenous pigment could be accumulated in the eyes?
a) copper,
b) lead,
c) coal dust,
d) none of the above
Which exogenous pigment could be accumulated in the eyes?
a) copper,
b) lead,
c) coal dust,
d) none of the above
Which exogenous pigment could be deposited in the oral cavity?
a) coal dust,
b) copper,
c) lead,
d) none of the above
Which exogenous pigment could be deposited in the oral cavity?
a) coal dust,
b) copper,
c) lead,
d) none of the above
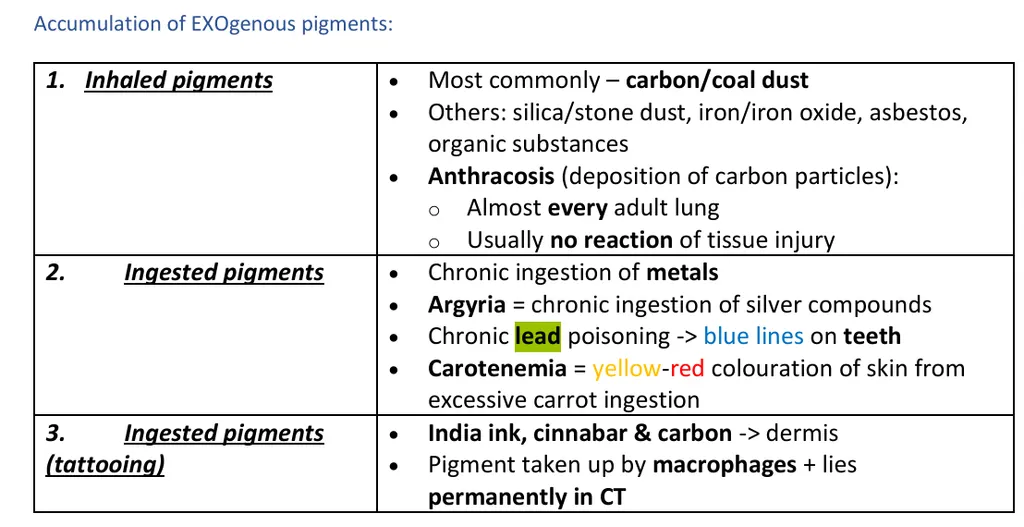
Which exogenous pigment(s) could be deposited in the skin?
a) carotene,
b) silver,
c) tattoo ink,
d) all of the above
Which exogenous pigment(s) could be deposited in the skin?
a) carotene,
b) silver,
c) tattoo ink,
d) all of the above
Which exogenous pigments could be deposited in the liver? (2)
a) copper,
b) silver,
c) tattoo ink,
d) coal dust
Which exogenous pigments could be deposited in the liver? (2)
a) copper,
b) silver,
c) tattoo ink,
d) coal dust
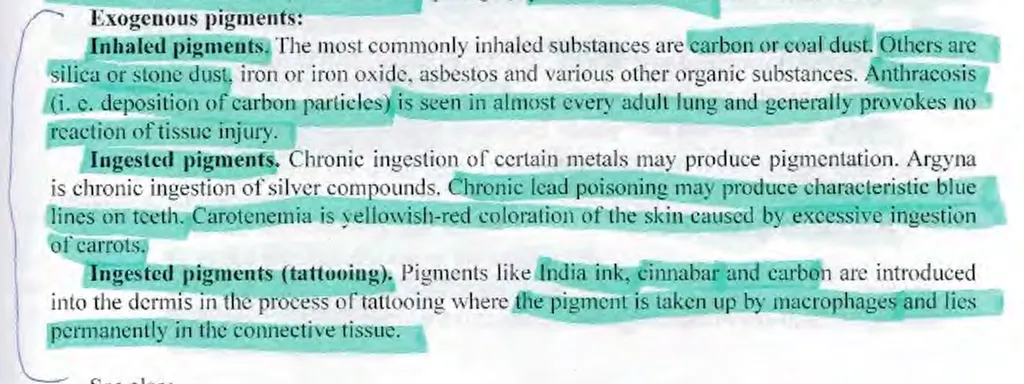
Which exogenous pigment could be deposited in the kidney?
a) coal dust,
b) copper,
c) silver,
d) all of the above
Which exogenous pigment could be deposited in the kidney?
a) coal dust,
b) copper,
c) silver,
d) all of the above
Which exogenous pigment could be deposited in the lungs and lymph nodes?
a) coal dust,
b) carotene,
c) tattoo ink,
d) none of the above
Which exogenous pigment could be deposited in the lungs and lymph nodes?
a) coal dust,
b) carotene,
c) tattoo ink,
d) none of the above
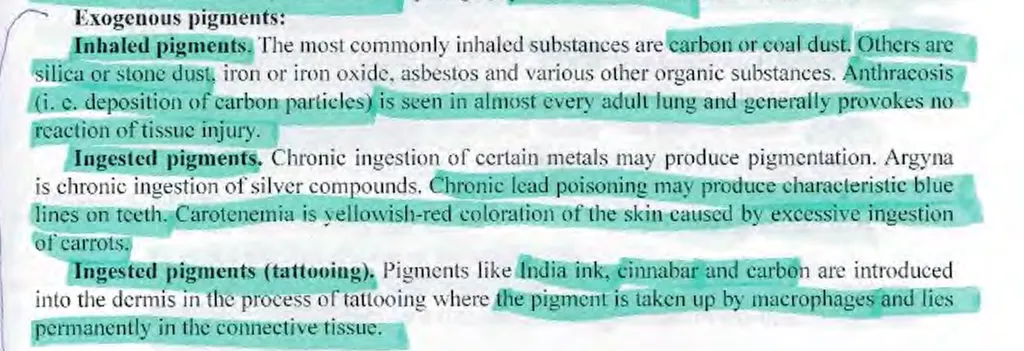
Which exogenous pigment could be deposited in the brain?
a) coal dust,
b) carotene,
c) copper,
d) tattoo ink
Which exogenous pigment could be deposited in the brain?
a) coal dust,
b) carotene,
c) copper,
d) tattoo ink
Examples for non-organic pigments are: (3)
a) coal dust,
b) lead,
c) carotene,
d) silver
Examples for non-organic pigments are: (3)
a) coal dust,
b) lead,
c) carotene,
d) silver
Indicate the types of jaundice.
a) haemolytic/pre-hepatic,
b) obstructive/post-hepatic,
c) hepatocellular/parenchymal,
d) all of the above
Indicate the types of jaundice.
a) haemolytic/pre-hepatic,
b) obstructive/post-hepatic,
c) hepatocellular/parenchymal,
d) all of the above
Haemolytic jaundice is characterized by the following laboratory findings:
a) increased indirect bilirubin in the serum, hypercholic stools and increased urobilinogen in the urine,
b) both types of bilirubin are increased in the serum, normal colour of the stools, both bilirubin and urobilinogen are increased in the urine,
c) increased direct bilirubin in the serum, hypoholic or acholic stool, increased bilirubin in the urine,
d) none of the above
Haemolytic jaundice is characterized by the following laboratory findings:
a) increased indirect bilirubin in the serum, hypercholic stools and increased urobilinogen in the urine,
b) both types of bilirubin are increased in the serum, normal colour of the stools, both bilirubin and urobilinogen are increased in the urine,
c) increased direct bilirubin in the serum, hypoholic or acholic stool, increased bilirubin in the urine,
d) none of the above
Mechanical jaundice is characterized by the following laboratory findings:
a) increased indirect bilirubin in the serum, hypercholic stools and increased urobilinogen in the urine,
b) both types of bilirubin are increased in the serum, normal colour of the stools, both bilirubin and urobilinogen are increased in the urine,
c) increased direct bilirubin in the serum, hypocholic or acholic stools, increased bilirubin in the urine,
d) none of the above
Mechanical jaundice is characterized by the following laboratory findings:
a) increased indirect bilirubin in the serum, hypercholic stools and increased urobilinogen in the urine,
b) both types of bilirubin are increased in the serum, normal colour of the stools, both bilirubin and urobilinogen are increased in the urine,
c) increased direct bilirubin in the serum, hypocholic or acholic stools, increased bilirubin in the urine,
d) none of the above
as mechanical jaundice is a type of post-hepatic jaundice
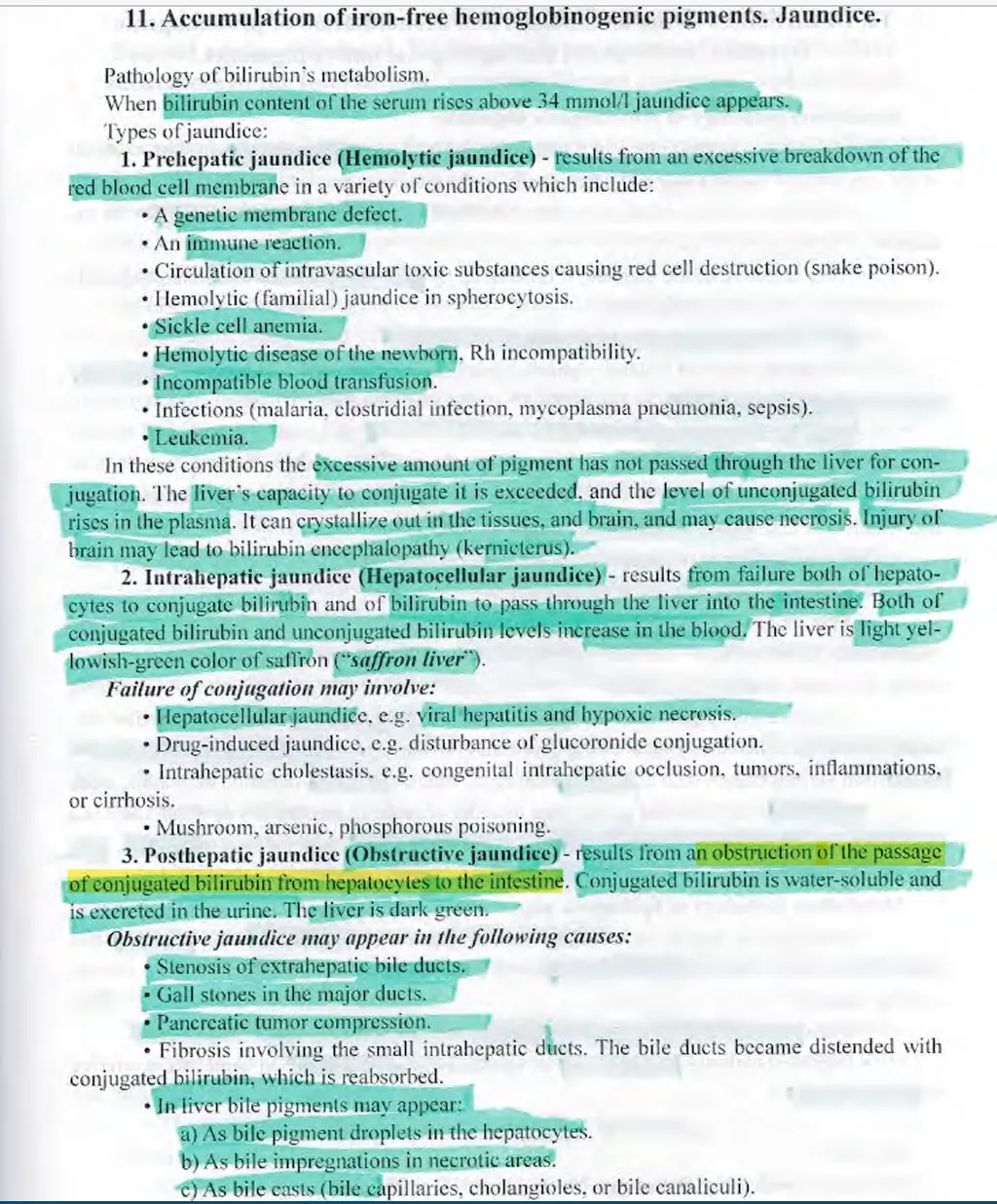
Parenchymal jaundice is characterized by the following laboratory findings:
a) increased indirect bilirubin in the serum, hypercholic stools and increased urobilinogen in the urine,
b) both types of bilirubin are increased in the serum, normal colour of the stools, both bilirubin and urobilinogen are increased in the urine,
c) increased direct bilirubin in the serum, hypocholic or acholic stools, increased bilirubin in the urine,
d) none of the above
Parenchymal jaundice is characterized by the following laboratory findings:
a) increased indirect bilirubin in the serum, hypercholic stools and increased urobilinogen in the urine,
b) both types of bilirubin are increased in the serum, normal colour of the stools, both bilirubin and urobilinogen are increased in the urine,
c) increased direct bilirubin in the serum, hypocholic or acholic stools, increased bilirubin in the urine,
d) none of the above
Which of the following stains are used to prove hemosiderin?
a) Sudan III in orange colour,
b) Congo-Red in brick-red colour,
c) Perls in blue-green colour,
d) Van Gieson in red colour
Which of the following stains are used to prove hemosiderin?
a) Sudan III in orange colour,
b) Congo-Red in brick-red colour,
c) Perls in blue-green colour,
d) Van Gieson in red colour
What is the etiology of brown induration of the lungs? (2)
a) chronic left sided heart failure,
b) chronic right sided heart failure,
c) mitral valve stenosis,
d) acute left sided heart failure
What is the etiology of brown induration of the lungs? (2)
a) chronic left sided heart failure,
b) chronic right sided heart failure,
c) mitral valve stenosis,
d) acute left sided heart failure
the book doesn’t give enough information to discern these answers, but if you think about it..
it’s mainly because of chronic heart failure.
also, left HF means congestion in the LA which means that the pulmonary arteries are congested, hence the pulmonary hypertension leads to alveolar haemorrhages thus Hb ingestion by macrophages → pigmented “heart failure cells” hence the brown colour of the lungs and “brown induration” name
What is the common between fibrosis, sclerosis and cirrhosis?
a) the common is the increased development of connective tissue in the organ,
b) the common is the lipid accumulation in the interstitium of the organ,
c) the common is the fibrinoid degeneration of the organ,
d) they are different processes and don’t have anything common between them
What is the common between fibrosis, sclerosis and cirrhosis?
a) the common is the increased development of connective tissue in the organ,
b) the common is the lipid accumulation in the interstitium of the organ,
c) the common is the fibrinoid degeneration of the organ,
d) they are different processes and don’t have anything common between them
Which of the following extracellular changes shows basophilia on H-E stain?
a) fibrinoid degeneration,
b) hyalinosis,
c) mucoid degeneration,
d) amyloidosis
Which of the following extracellular changes shows basophilia on H-E stain?
a) fibrinoid degeneration,
b) hyalinosis,
c) mucoid degeneration,
d) amyloidosis
the others are proteins - eosinophilic (protein-rich structures, cytoplasm)
mucin and GAG accumulation are -vely charged polysaccharides which attract the basic dye (Hematoxylin → blue stain)
Which of the following changes are characterized by eosinophilia on H-E stain? (2)
a) mucoid degeneration,
b) vacuolar degeneration,
c) fibrinoid necrosis,
d) fibrinoid degeneration
Which of the following changes are characterized by eosinophilia on H-E stain? (2)
a) mucoid degeneration,
b) vacuolar degeneration,
c) fibrinoid necrosis,
d) fibrinoid degeneration
Metachromasia can be seen in which of the following changes on Toluidin-Blue stain?
a) fibrinoid degeneration,
b) mucoid degeneration,
c) fibrinoid necrosis,
d) hyalinosis
Metachromasia can be seen in which of the following changes on Toluidin-Blue stain?
a) fibrinoid degeneration,
b) mucoid degeneration,
c) fibrinoid necrosis,
d) hyalinosis
Special stains for fibrin are also used in: (2)
a) fibrinoid degeneration,
b) fibrinoid necrosis,
c) mucoid degeneration,
d) amyloidosis
Special stains for fibrin are also used in: (2)
a) fibrinoid degeneration,
b) fibrinoid necrosis,
c) mucoid degeneration,
d) amyloidosis
don’t confuse the amyloidosis fibrillar proteins with Fibril proteins - 90% and P component 10%
FIBRIL is not FIBRIN
Infiltration of lymphocytes and plasma cells is typical for: (2)
a) mucoid edema,
b) fibrinoid necrosis,
c) fibrinoid degeneration,
d) none of the above
Infiltration of lymphocytes and plasma cells is typical for: (2)
a) mucoid edema,
b) fibrinoid necrosis,
c) fibrinoid degeneration,
d) none of the above
What is the clinical significance of hyalinosis of the heart arterioles?
a) it causes myocarditis,
b) it causes rheumatic heart disease,
c) it causes ischaemic heart disease,
d) it causes subacute endocarditis
What is the clinical significance of hyalinosis of the heart arterioles?
a) it causes myocarditis,
b) it causes rheumatic heart disease,
c) it causes ischaemic heart disease,
d) it causes subacute endocarditis
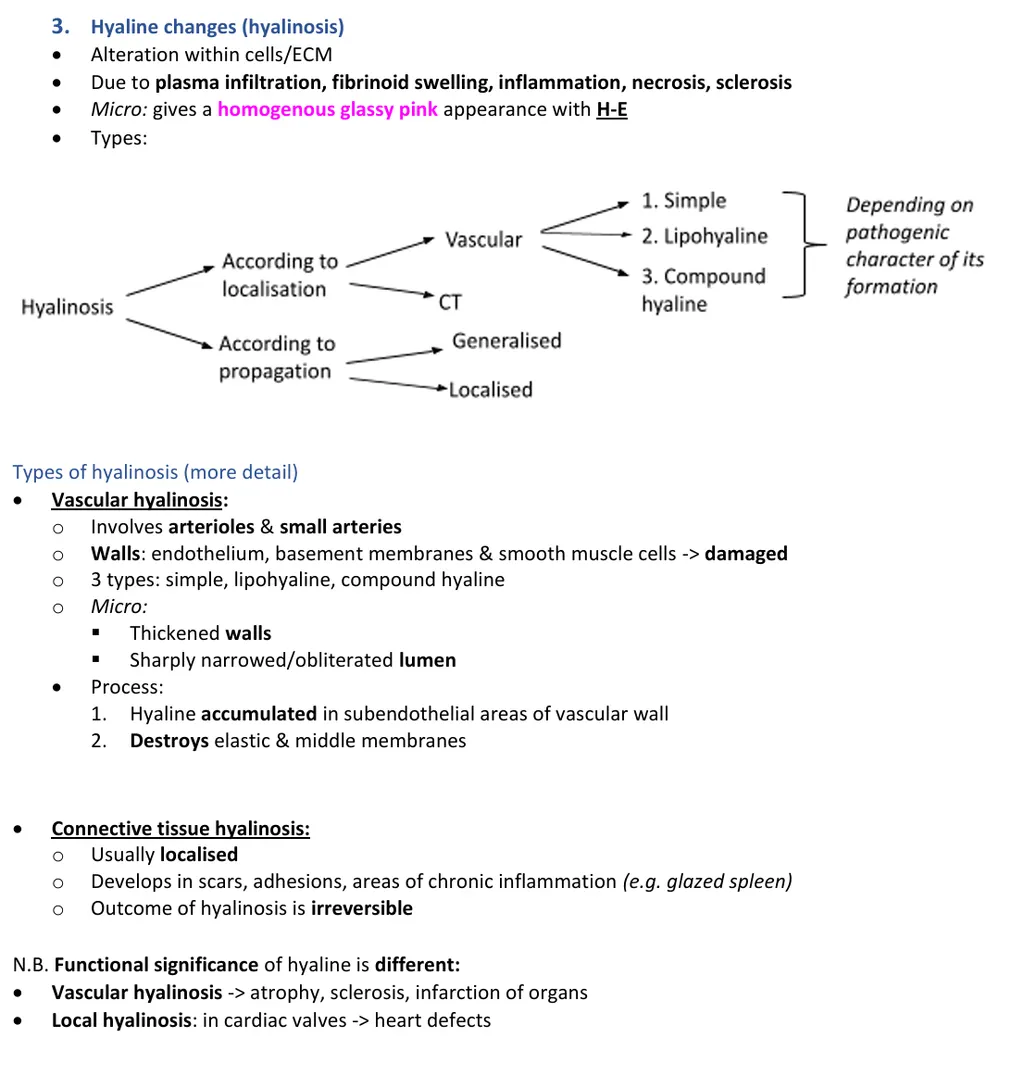
What is the clinical significance of hyalinosis of the pancreatic arterioles?
a) it can cause diabetes mellitus,
b) it can cause pancreatic cancer,
c) it can cause acute pancreatitis,
d) hyalinosis in the pancreas is a physiological process related with ageing
What is the clinical significance of hyalinosis of the pancreatic arterioles?
a) it can cause diabetes mellitus,
b) it can cause pancreatic cancer,
c) it can cause acute pancreatitis,
d) hyalinosis in the pancreas is a physiological process related with ageing
What is the common between “glazed spleen” and corpus albicans ovarii?
a) the process in both is hyalinosis,
b) the process in both is fibrosis,
c) the process in both is fibrinoid degeneration,
d) the process in both is amyloidosis
What is the common between “glazed spleen” and corpus albicans ovarii?
a) the process in both is hyalinosis,
b) the process in both is fibrosis,
c) the process in both is fibrinoid degeneration,
d) the process in both is amyloidosis
just remember that the glazed spleen is hyalinosis
Which stain is used to prove rheumatism in acute stage in a heart valve?
a) Prussian Blue,
b) Toluidin-Blue,
c) Congo-Red,
d) Perls
Which stain is used to prove rheumatism in acute stage in a heart valve?
a) Prussian Blue,
b) Toluidin-Blue,
c) Congo-Red,
d) Perls
In the context of diagnosing rheumatic heart disease (rheumatism) in the acute stage, particularly in the heart valve, Toluidine-Blue is a useful stain to highlight aschoff bodies and other features characteristic of rheumatic heart disease
Aschoff bodies are granulomatous lesions found in the heart tissue during the acute phase of rheumatic fever, and they are typically stained with Toluidine-Blue to better visualize the inflammatory cells and changes in the affected tissue
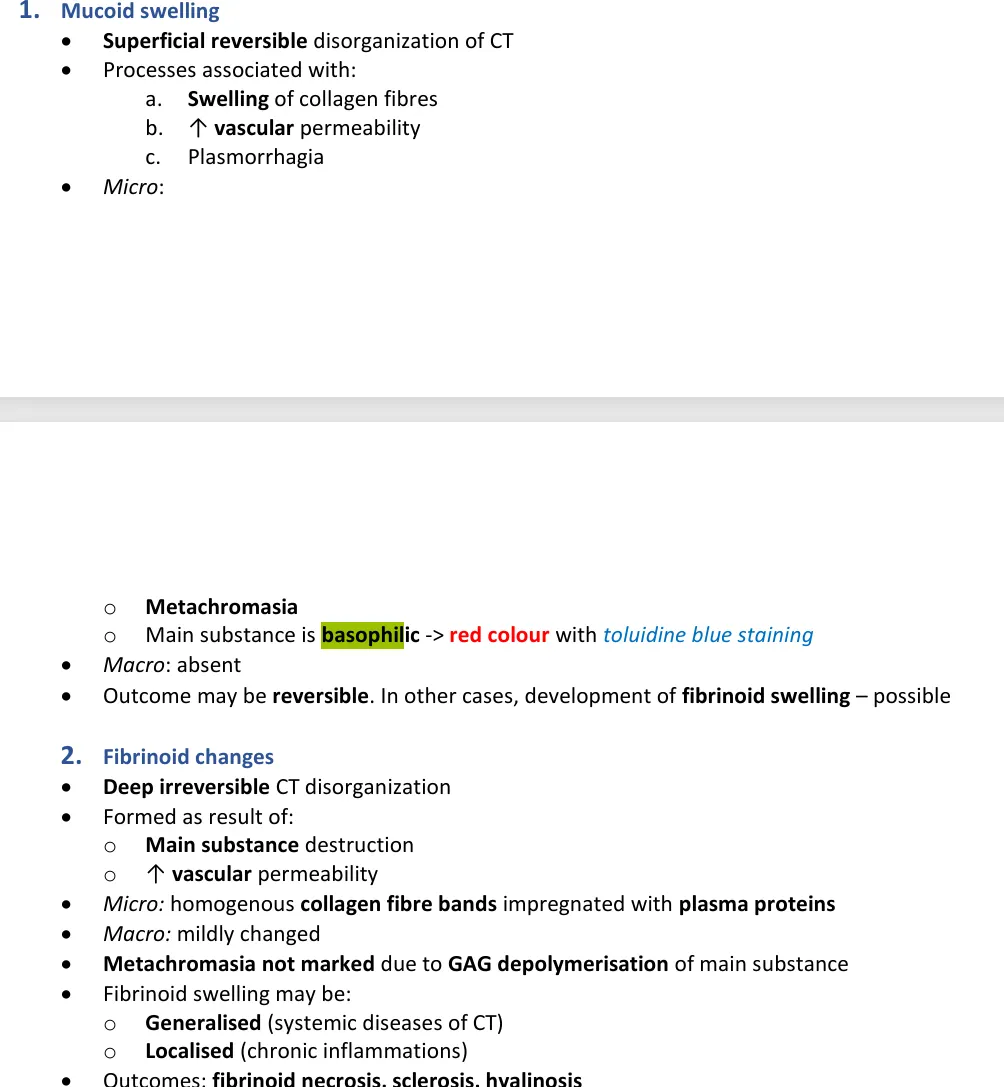
Mucoid swelling can be seen in:
a) heart valves in rheumatism,
b) Basedow’s dermopathy,
c) myxedema,
d) all of the listed above
Mucoid swelling can be seen in:
a) heart valves in rheumatism,
b) Basedow’s dermopathy,
c) myxedema,
d) all of the listed above
Mucoid swelling refers to the accumulation of mucopolysaccharides or glycosaminoglycans, which are components of mucin. This swelling is often seen in conditions where there is altered metabolism of these substances. It is associated with the following conditions:
Heart valves in rheumatism: In rheumatic fever, particularly in rheumatic heart disease, mucoid swelling can occur in the heart valves as part of the inflammation and degeneration of the valves. This process can lead to valvular thickening and dysfunction.
Basedow’s dermopathy (also known as Graves' disease dermopathy): This condition is associated with thyroid disease (hyperthyroidism) and involves mucoid swelling of the skin, especially on the shins (pretibial myxedema). The mucoid material accumulates in the dermis, causing swelling and skin changes.
Myxedema: This term refers to the severe form of hypothyroidism, where mucoid swelling occurs due to the accumulation of glycosaminoglycans in the skin and connective tissues, leading to the characteristic puffy appearance (especially in the face and extremities).
Thus, mucoid swelling can be seen in rheumatic heart disease, Graves' disease (Basedow's dermopathy), and myxedema, making all of the listed conditions correct.
Which are the types of fibrinoid? (3)
a) fibrinoid related to immune complexes in autoimmune diseases,
b) physiological fibrinoid degeneration with aging,
c) fibrinoid caused by the influence of biological, chemical and physical factors,
d) fibrinoid caused by fast plasmorrhagia in the vessel walls in malignant hypertension
Which are the types of fibrinoid? (3)
a) fibrinoid related to immune complexes in autoimmune diseases,
b) physiological fibrinoid degeneration with aging,
c) fibrinoid caused by the influence of biological, chemical and physical factors,
d) fibrinoid caused by fast plasmorrhagia in the vessel walls in malignant hypertension
The necrosis which develops at the base of an acute or chronic active ulcer in the stomach or duodenum is:
a) coagulative,
b) caseous,
c) fibrinoid,
d) liquefactive
The necrosis which develops at the base of an acute or chronic active ulcer in the stomach or duodenum is:
a) coagulative,
b) caseous,
c) fibrinoid,
d) liquefactive
Which degeneration in the extracellular matrix is seen during the acute stages of autoimmune diseases?
a) hyaline,
b) fibrinoid,
c) amyloid,
d) none of the above
Which degeneration in the extracellular matrix is seen during the acute stages of autoimmune diseases?
a) hyaline,
b) fibrinoid,
c) amyloid,
d) none of the above
I think the timeline that makes sense is first mucoid swelling (reversible) → fibrinoid (deep irreversible CT disorganisation) → hyalinosis (alteration within cells or in ECM, occurs as a result of fibrinoid swelling and other etiologies)
Indicate the correct statement(s) for nephrosclerosis arteriolosclerotica: (3)
a) it affects microscopically the afferent and efferent arterioles,
b) it is a result of prolonged benign hypertension,
c) it is a reversible process,
d) the process is hyalinosis
Indicate the correct statement(s) for nephrosclerosis arteriolosclerotica: (3)
a) it affects microscopically the afferent and efferent arterioles,
b) it is a result of prolonged benign hypertension,
c) it is a reversible process,
d) the process is hyalinosis
What are the microscopic changes seen in the brain in benign long-term hypertension? (2)
a) hyalinosis of the vessels’ walls,
b) edema around vessels,
c) accumulation of lymphocytes and plasma cells in the soft brain membranes,
d) developments of specific granulomas in the brain tissue
What are the microscopic changes seen in the brain in benign long-term hypertension? (2)
a) hyalinosis of the vessels’ walls,
b) edema around vessels,
c) accumulation of lymphocytes and plasma cells in the soft brain membranes,
d) developments of specific granulomas in the brain tissue
The gross description: thick, hard, glassy whitish depositions, non-digestible by enzymes, is indicative for
a) steatonecrosis,
b) liquefactive necrosis,
c) hyalinosis,
d) fibrinoid deposition
The gross description: thick, hard, glassy whitish depositions, non-digestible by enzymes, is indicative for
a) steatonecrosis,
b) liquefactive necrosis,
c) hyalinosis,
d) fibrinoid deposition
Mark the correct statements for Corpus albicans ovarii (white bodies of the ovaries). (2)
a) they are example of physiological hyalinosis,
b) they are example for pathological hyalinosis after inflammatory processes in the ovaries,
c) they are example for physiological accumulation of fibrinoid,
d) they develop after the regression of corpus luteum
Mark the correct statements for Corpus albicans ovarii (white bodies of the ovaries). (2)
a) they are example of physiological hyalinosis,
b) they are example for pathological hyalinosis after inflammatory processes in the ovaries,
c) they are example for physiological accumulation of fibrinoid,
d) they develop after the regression of corpus luteum
since its physiological shouldn’t be inflammatory processes as that’s a disease/pathological process. and its an example of hyalinosis (remember the question about glazed spleen and corpus albicans ovarii)
The following diseases are examples of amyloid depositions. Find the mistake!
a) rheumatoid arthritis – AA amyloid,
b) multiple myeloma – AL amyloid,
c) medullary carcinoma of the thyroid gland – AA amyloid,
d) Alzheimer’s disease – A4 amyloid
The following diseases are examples of amyloid depositions. Find the mistake!
a) rheumatoid arthritis – AA amyloid,
b) multiple myeloma – AL amyloid,
c) medullary carcinoma of the thyroid gland – AA amyloid,
d) Alzheimer’s disease – A4 amyloid
AL - primary amyloid - multiple myeloma, B cell lymphoma …
AA - secondary amyloid - cancers, chronic inflammation, mediterranean fevers
AA - familial amyloidosis

‘Sago spleen and lardaceous spleen’ are:
a) gross appearance of the localized (sago-spleen) and generalized (lardaceous spleen) amyloidosis of the spleen,
b) sago spleen is amyloidosis of the spleen, while lardaceous spleen is hyalinosis of the spleen,
c) gross appearance of the spleen in Hodgkin’s lymphoma depending on the severity of the process,
d) in lardaceous spleen the amyloid is deposited in the white pulp only, while in sago spleen both white and red pulp have amyloid deposition
‘Sago spleen and lardaceous spleen’ are:
a) gross appearance of the localized (sago-spleen) and generalized (lardaceous spleen) amyloidosis of the spleen,
b) sago spleen is amyloidosis of the spleen, while lardaceous spleen is hyalinosis of the spleen,
c) gross appearance of the spleen in Hodgkin’s lymphoma depending on the severity of the process,
d) in lardaceous spleen the amyloid is deposited in the white pulp only, while in sago spleen both white and red pulp have amyloid deposition

Systemic amyloidosis is proven by a biopsy from? (2)
a) gingiva,
b) heart,
c) fat tissue from abdominal wall,
d) ileum
Systemic amyloidosis is proven by a biopsy from? (2)
a) gingiva,
b) heart,
c) fat tissue from abdominal wall,
d) ileum
What type of calcification develops in the complicated atherosclerotic plaques?
a) metastatic,
b) dystrophic,
c) metabolic,
d) physiological
What type of calcification develops in the complicated atherosclerotic plaques?
a) metastatic,
b) dystrophic,
c) metabolic,
d) physiological

Which are the causes for hypocalcaemia?
a) hypoparathyroidism,
b) hyperparathyroidism,
c) intoxication with vit. D,
d) senile osteoporosis
Which are the causes for hypocalcaemia?
a) hypoparathyroidism,
b) hyperparathyroidism,
c) intoxication with vit. D,
d) senile osteoporosis
What kind of gout can develop in a patient with leukemia?
a) gout caused by excessive consumption of meat and meat products,
b) genetic gout caused by error in the metabolism of uric acid,
c) renal injury because kidneys cannot excrete the excessive amount of uric acid,
d) patients with leukemia never develop gout
What kind of gout can develop in a patient with leukemia?
a) gout caused by excessive consumption of meat and meat products,
b) genetic gout caused by error in the metabolism of uric acid,
c) renal injury because kidneys cannot excrete the excessive amount of uric acid,
d) patients with leukemia never develop gout
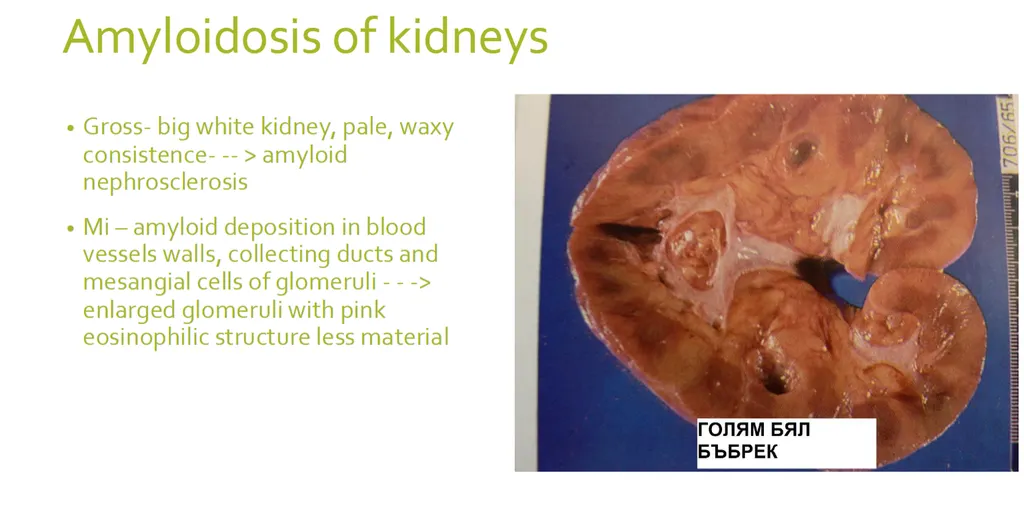
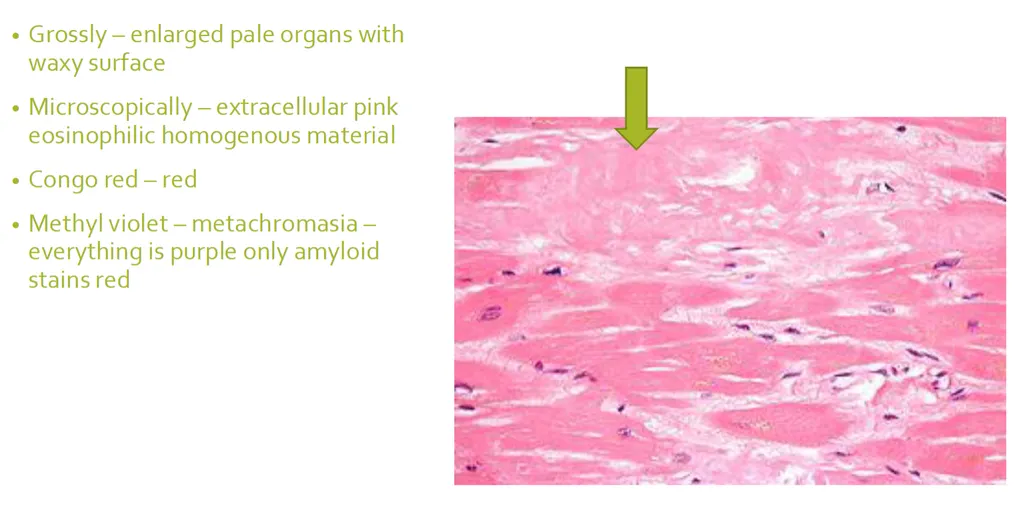
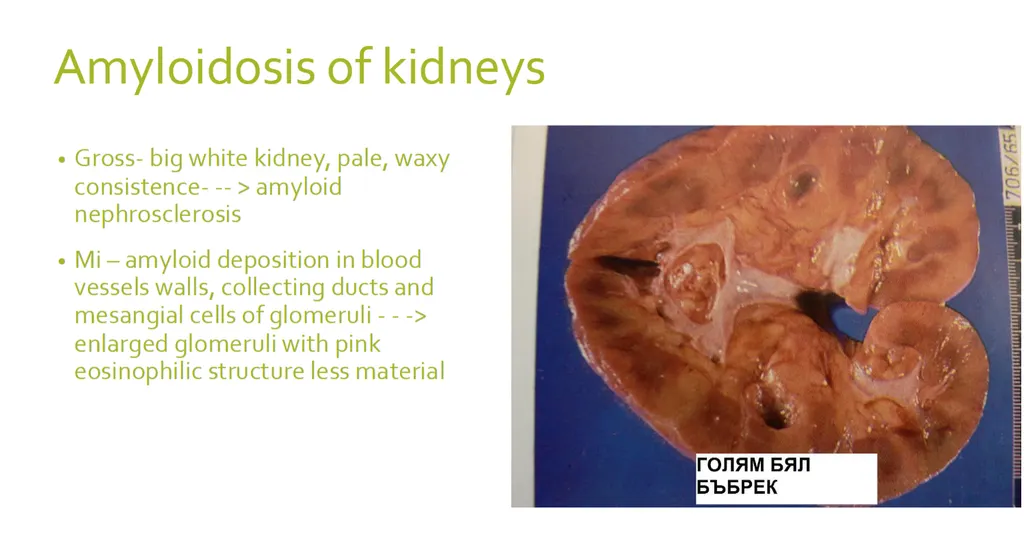
Which of the following microscopic descriptions most likely suggest kidney amyloidosis? The stain is H-E in all the described specimens.
a) highly enlarged glomeruli, the capillary tufts filled almost all of the capsular space, capillary lumens are obliterated; pink homogeneous substance is deposited also in the mesangium, in the basement membranes of the tubules and in the walls of the blood vessels,
b) afferent and efferent arterioles have homogenously thick walls stained in pink, some of the glomeruli look smaller, with totally effaced structure and homogenously pink in color, while others may look normal in size, or even with compensatory hypertrophy,
c) the interstitium shows chronic inflammatory reaction, the main change is seen in the kidney tubules which look dilated and filled with pinkish substance (these tubules look like thyroid follicles),
d) many glomeruli show crescent proliferations, encompassing 2/3 of the Bowman’s space; the process ends with global sclerosis of the glomerulus
Which of the following microscopic descriptions most likely suggest kidney amyloidosis? The stain is H-E in all the described specimens.
a) highly enlarged glomeruli, the capillary tufts filled almost all of the capsular space, capillary lumens are obliterated; pink homogeneous substance is deposited also in the mesangium, in the basement membranes of the tubules and in the walls of the blood vessels,
b) afferent and efferent arterioles have homogenously thick walls stained in pink, some of the glomeruli look smaller, with totally effaced structure and homogenously pink in color, while others may look normal in size, or even with compensatory hypertrophy,
c) the interstitium shows chronic inflammatory reaction, the main change is seen in the kidney tubules which look dilated and filled with pinkish substance (these tubules look like thyroid follicles),
d) many glomeruli show crescent proliferations, encompassing 2/3 of the Bowman’s space; the process ends with global sclerosis of the glomerulus
Which of the following stain(s) is used to prove amyloidosis? (2)
a) Perls,
b) Congo-Red,
c) Van Gieson,
d) Methyl violet
Which of the following stain(s) is used to prove amyloidosis? (2)
a) Perls,
b) Congo-Red,
c) Van Gieson,
d) Methyl violet
Congo red - red/orange = positive
Methyl violet - metachromasia, everything purple just amyloid - red
Mark the correct statement(s) for kidney amyloidosis
a) small, shrunken kidneys with granular surface and difficult decapsulation,
b) enlarged pale kidneys with waxy texture,
c) amyloidosis affects only one of the kidneys and doesn’t lead to chronic renal failure,
d) kidney amyloidosis is reversible after the treatment of the primary disease and has very good prognosis
Mark the correct statement(s) for kidney amyloidosis
a) small, shrunken kidneys with granular surface and difficult decapsulation,
b) enlarged pale kidneys with waxy texture,
c) amyloidosis affects only one of the kidneys and doesn’t lead to chronic renal failure,
d) kidney amyloidosis is reversible after the treatment of the primary disease and has very good prognosis
Mark the terms which indicate amyloidosis of the spleen. (2)
a) lardaceous spleen,
b) glazed spleen,
c) sago spleen,
d) porphiric spleen
Mark the terms which indicate amyloidosis of the spleen. (2)
a) lardaceous spleen,
b) glazed spleen,
c) sago spleen,
d) porphiric spleen
Granulomatous structures, consisting of uric acid crystals, lymphocytes, macrophages, fibroblasts and giant multinucleated cells type “foreign body” are characteristic for which disease?
a) tuberculosis,
b) sarcoidosis,
c) gout,
d) brucellosis
Granulomatous structures, consisting of uric acid crystals, lymphocytes, macrophages, fibroblasts and giant multinucleated cells type “foreign body” are characteristic for which disease?
a) tuberculosis,
b) sarcoidosis,
c) gout,
d) brucellosis
Calcification of the aorta characterizes with: (2)
a) hard, rigid wall of the aorta,
b) soft, elastic wall of the aorta,
c) can be complicated with mural thrombosis and aneurysm,
d) is a result of metabolic calcification
Calcification of the aorta characterizes with: (2)
a) hard, rigid wall of the aorta,
b) soft, elastic wall of the aorta,
c) can be complicated with mural thrombosis and aneurysm,
d) is a result of metabolic calcification
Amyloidosis of the liver: (2)
a) develops because of liver dysfunction and liver failure due to chronic liver disease,
b) is characterized grossly with small, brown liver with decreased elasticity,
c) can develop in chronic inflammatory diseases or in autoimmune diseases,
d) is characterized grossly with enlarged, pale liver with waxy texture
Amyloidosis of the liver: (2)
a) develops because of liver dysfunction and liver failure due to chronic liver disease,
b) is characterized grossly with small, brown liver with decreased elasticity,
c) can develop in chronic inflammatory diseases or in autoimmune diseases,
d) is characterized grossly with enlarged, pale liver with waxy texture
Renal complications of gout include:
a) Uric crystals nephrolithiasis,
b) uric-acid infarction,
c) urate nephropathy,
d) all of the listed above
Renal complications of gout include:
a) Uric crystals nephrolithiasis,
b) uric-acid infarction,
c) urate nephropathy,
d) all of the listed above
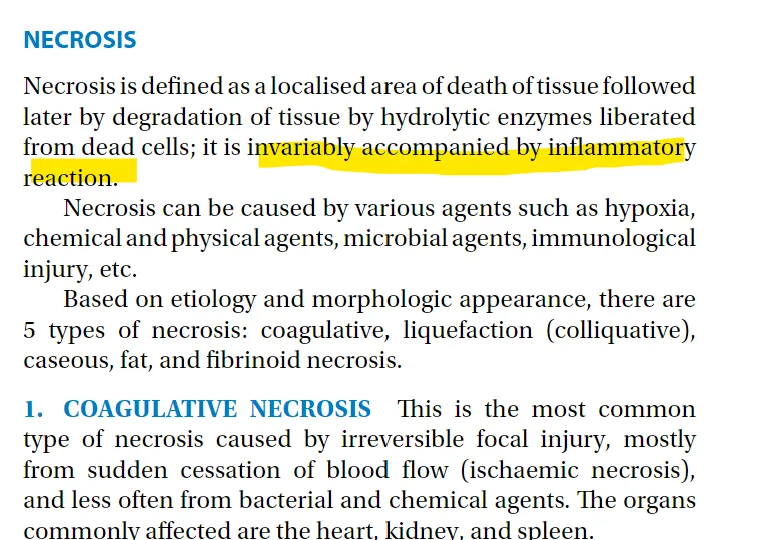
Indicate the correct statement(s) for necrosis. (2)
a) It is a programmed cell death,
b) It is provoked cell death,
c) It affects single cells and the extracellular matrix is not involved in the process,
d) there is a demarcation inflammation at the periphery of the affected area
Indicate the correct statement(s) for necrosis. (2)
a) It is a programmed cell death,
b) It is provoked cell death,
c) It affects single cells and the extracellular matrix is not involved in the process,
d) there is a demarcation inflammation at the periphery of the affected area
Indicate the correct statement(s) for apoptosis. (2)
a) it affects single cells and the extracellular matrix is not involved,
b) there is demarcation inflammation at the periphery of the affected area,
c) it ends with phagocytosis of the cellular fragments,
d) it is always accompanied by inflammation at the periphery of the area
Indicate the correct statement(s) for apoptosis. (2)
a) it affects single cells and the extracellular matrix is not involved,
b) there is demarcation inflammation at the periphery of the affected area,
c) it ends with phagocytosis of the cellular fragments,
d) it is always accompanied by inflammation at the periphery of the area
What is the difference between fibrinoid degeneration and fibrinoid necrosis?
a) fibrinoid degeneration is accumulation of fibrinoid in the extracellular space while fibrinoid necrosis includes not only fibrinoid degeneration but also death of cells and extracellular components in the area of fibrinoid degeneration,
b) these isn’t any difference, the two terms are synonyms,
c) fibrinoid degeneration is a physiological process while fibrinoid necrosis is a pathological process,
d) fibrinoid degeneration is accumulation of fibrin in the extracellular matrix while fibrinoid necrosis is necrosis of the fibrin in the extracellular matrix
What is the difference between fibrinoid degeneration and fibrinoid necrosis?
a) fibrinoid degeneration is accumulation of fibrinoid in the extracellular space while fibrinoid necrosis includes not only fibrinoid degeneration but also death of cells and extracellular components in the area of fibrinoid degeneration,
b) these isn’t any difference, the two terms are synonyms,
c) fibrinoid degeneration is a physiological process while fibrinoid necrosis is a pathological process,
d) fibrinoid degeneration is accumulation of fibrin in the extracellular matrix while fibrinoid necrosis is necrosis of the fibrin in the extracellular matrix
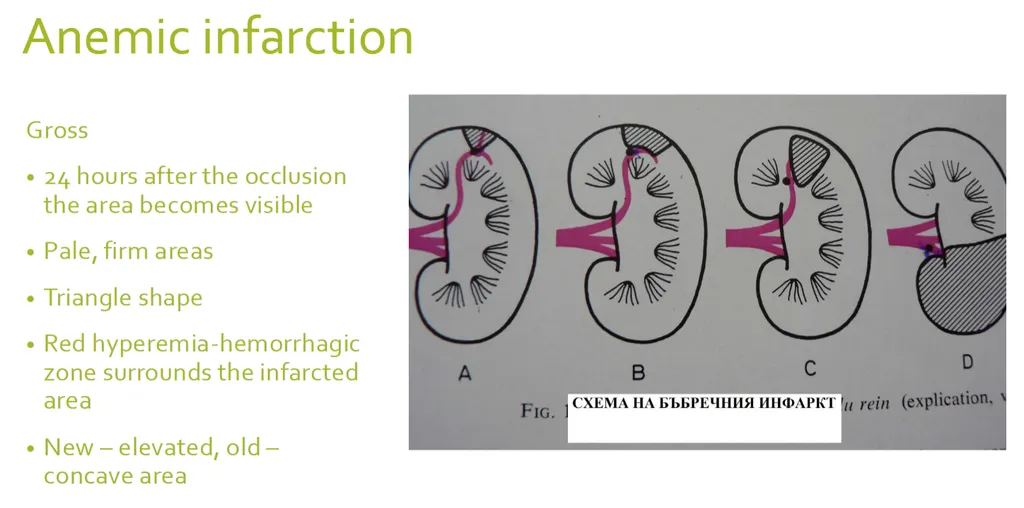
Indicate the correct statement(s) for anemic infarction. (2)
a) the term is synonym of white infarction
b) the term is synonym of red infarction
c) it develops as a result of absolute ischemia after total obstruction of an “end-type artery”
d) it mainly affects the lungs and liver
Indicate the correct statement(s) for anemic infarction. (2)
a) the term is synonym of white infarction
b) the term is synonym of red infarction
c) it develops as a result of absolute ischemia after total obstruction of an “end-type artery”
d) it mainly affects the lungs and liver
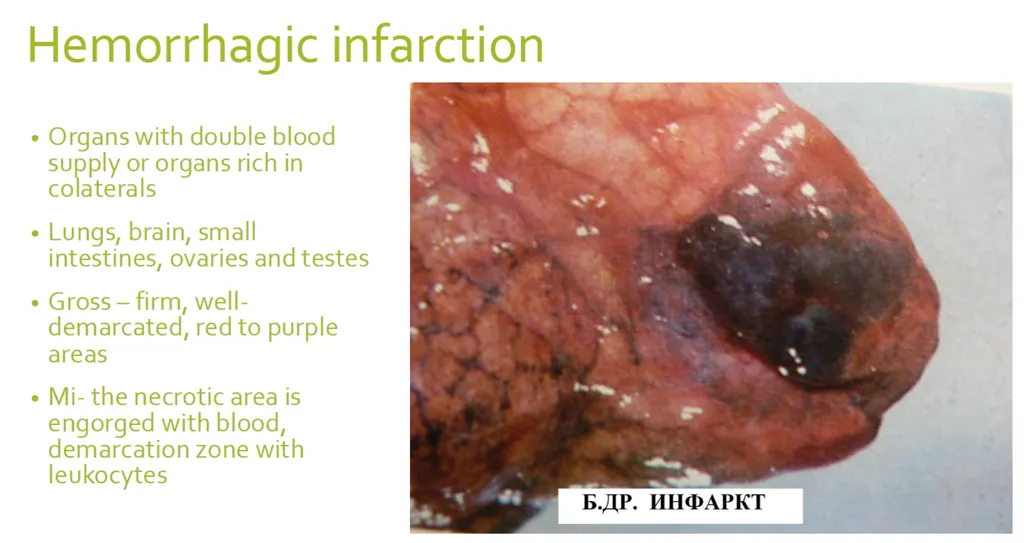
Indicate the correct statement(s) for haemorrhagic infarction. (2)
a) it develops in organs with double circulation
b) it mainly affects the brain and the heart
c) it affects organs which have contact with the outside environment
d) it may affect the small intestine
Indicate the correct statement(s) for haemorrhagic infarction. (2)
a) it develops in organs with double circulation
b) it mainly affects the brain and the heart
c) it affects organs which have contact with the outside environment
d) it may affect the small intestine
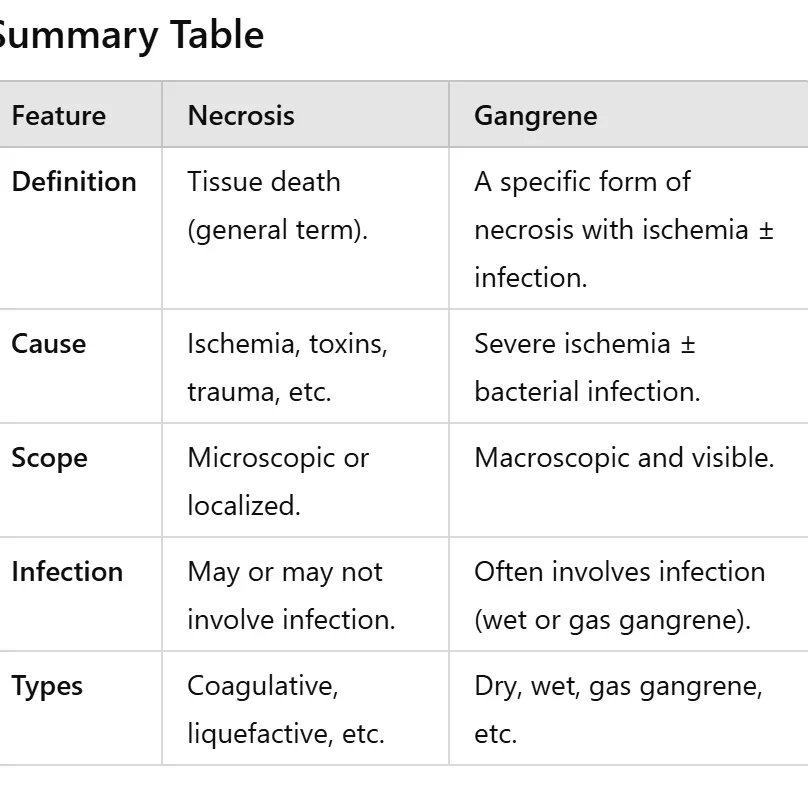
Indicate the correct statement(s) for gangrene. (2)
a) it is ischemic necrosis which develops in organs with contact with the external environment
b) it can be wet or dry
c) the dry gangrene is accompanied by severe bacterial infection
d) it can develop on the extremities, intestines, spleen and kidney
Indicate the correct statement(s) for gangrene. (2)
a) it is ischemic necrosis which develops in organs with contact with the external environment
b) it can be wet or dry
c) the dry gangrene is accompanied by severe bacterial infection
d) it can develop on the extremities, intestines, spleen and kidney
Necrosis:
Refers to the death of cells or tissues in a living organism due to irreversible damage. It is a pathological process and not specific to any particular condition or location. Necrosis can occur in any tissue and is caused by various factors, including ischemia, toxins, infections, and trauma.
Gangrene:
A specific type of necrosis that occurs when there is ischemia (lack of blood flow) and often involves secondary infection. Gangrene typically affects tissues in contact with the external environment, such as the skin, extremities, or intestines.
unlikely in paranchematous organs like kidney and spleen
Which of the following terms are used to describe liquefactive necrosis of the brain? (3)
a) ramolicio cerebri
b) encephalomalacia
c) infarctus anemicus cerebri
d) hydrocephalus
Which of the following terms are used to describe liquefactive necrosis of the brain? (3)
a) ramolicio cerebri
b) encephalomalacia
c) infarctus anemicus cerebri
d) hydrocephalus
just remember, hydrocephalus is about accumulation of CSF in brain ventricles. the others all mean softening or infarction which would soon be proceeded with liquefactive necroses due to autolysis enzymes released by dead brain cell
Which of the followings are not affected by gangrene?
a) lower limb
b) liver
c) lung
d) intestines
Which of the followings are not affected by gangrene?
a) lower limb
b) liver
c) lung
d) intestines
What type of necrosis develops in the spleen?
a) liquefactive necrosis
b) caseous necrosis
c) coagulative necrosis
d) fibrinoid necrosis
What type of necrosis develops in the spleen?
a) liquefactive necrosis
This is characteristic of brain tissue or abscesses where enzymatic digestion of dead cells occurs, leading to a liquefied appearance. It is not typical for the spleen
b) caseous necrosis
This is associated with granulomatous inflammation, especially in tuberculosis
While TB can affect the spleen (miliary TB), caseous necrosis is not the typical form of necrosis in the spleen
c) coagulative necrosis
Coagulative necrosis is the primary type of necrosis observed in the spleen
This occurs because the spleen is a solid organ with a high vascular supply, and ischemic events (e.g., infarction due to arterial blockage) result in coagulative necrosis
The architecture of the tissue is preserved initially but becomes firm due to protein denaturation.
d) fibrinoid necrosis
This is seen in blood vessel walls during immune-mediated diseases (e.g., vasculitis) and is not a characteristic type of necrosis in the spleen itself
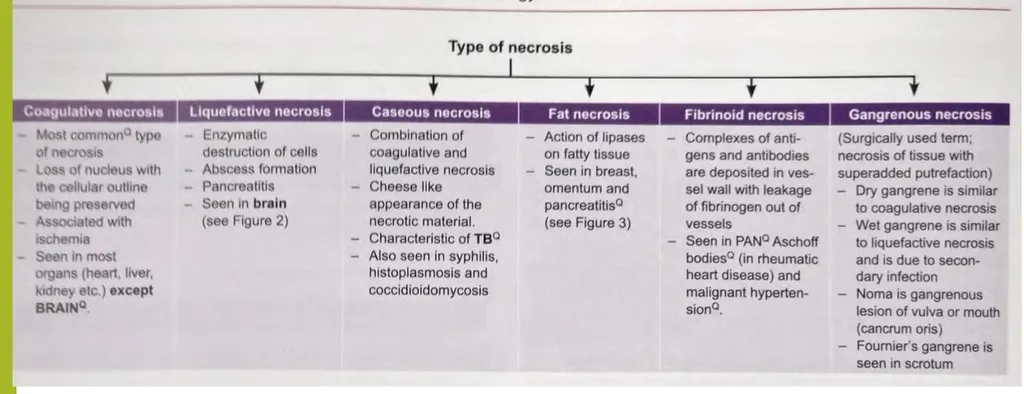
What type of necrosis develops in the brain?
a) caseous necrosis
b) coagulative necrosis
c) steatonecrosis
d) liquefactive necrosis
What type of necrosis develops in the brain?
a) caseous necrosis
b) coagulative necrosis
c) steatonecrosis
d) liquefactive necrosis
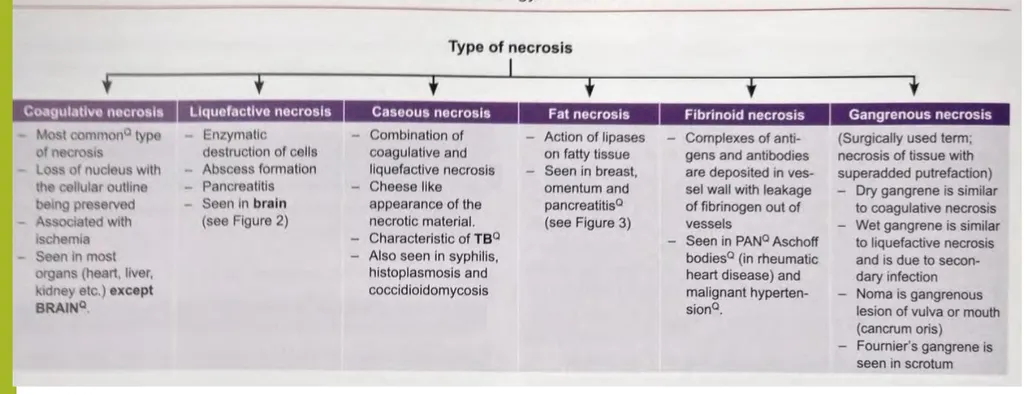
What type of necrosis develops in the pancreas?
a) steatonecrosis/fat necrosis
b) coagulative necrosis
c) liquefactive necrosis
d) caseous necrosis
What type of necrosis develops in the pancreas?
a) steatonecrosis/fat necrosis
b) coagulative necrosis
c) liquefactive necrosis
d) caseous necrosis
What type of necrosis develops in the specific granuloma in tuberculosis?
a) liquefactive necrosis
b) coagulative necrosis
c) caseous necrosis
d) steatonecrosis
What type of necrosis develops in the specific granuloma in tuberculosis?
a) liquefactive necrosis
b) coagulative necrosis
c) caseous necrosis
d) steatonecrosis
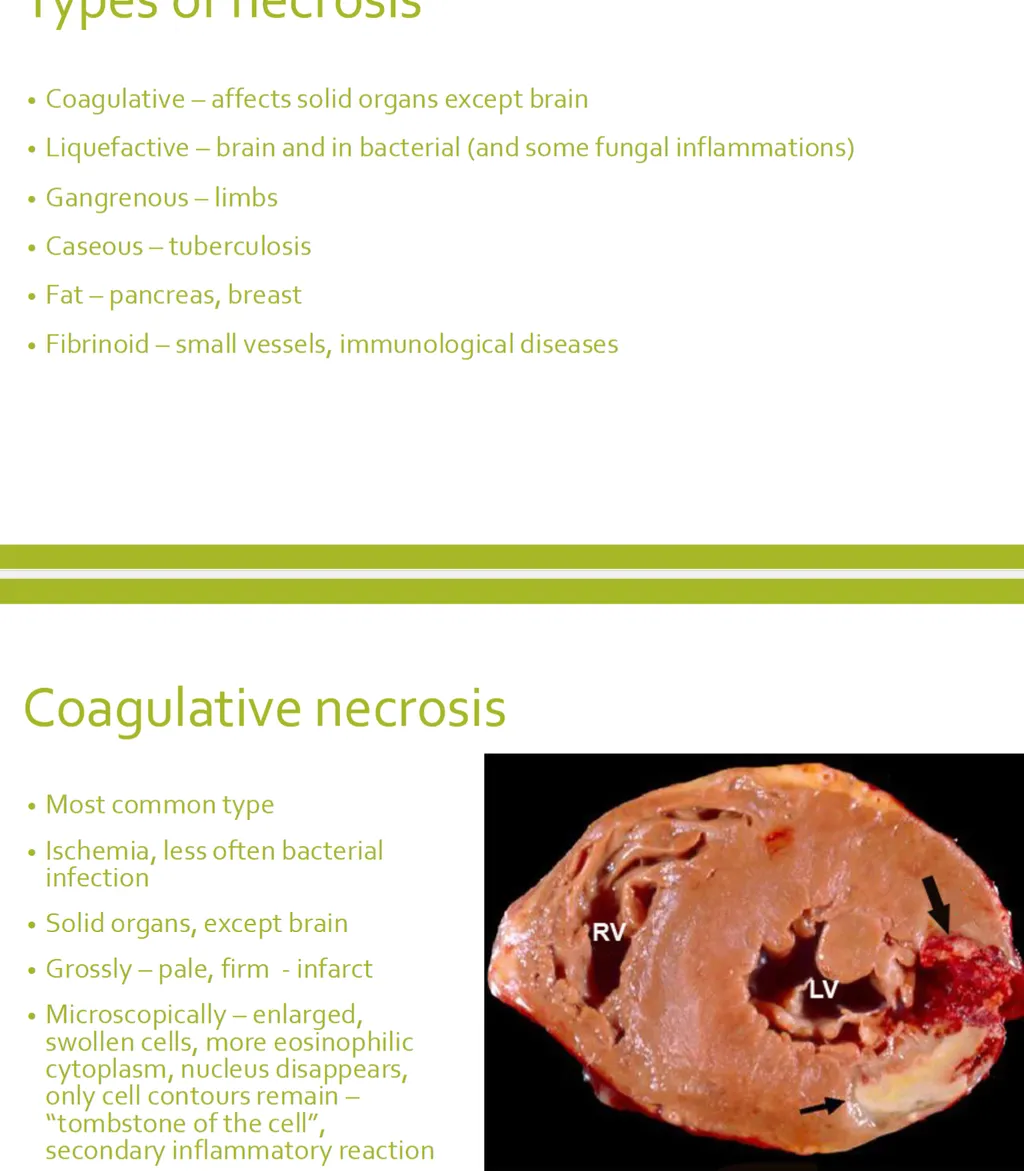
Indicate the correct statement(s) for coagulative necrosis. (2)
a) it develops in organs composed mainly of proteins and containing less water and enzymes
b) “shadows” of previous structures can be seen microscopically
c) it develops as a result of acute pancreatitis
d) there is total effacement of the previous structures microscopically
Indicate the correct statement(s) for coagulative necrosis. (2)
a) it develops in organs composed mainly of proteins and containing less water and enzymes
b) “shadows” of previous structures can be seen microscopically
c) it develops as a result of acute pancreatitis
d) there is total effacement of the previous structures microscopically