Palmer General Pathology Section 2: Inflammation and Repair
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
73 Terms
Why is inflammation important?
Kills and eliminates microbes
Removes debris
Initiates repair
What are the 2 types of immune cells? What is the difference?
Sentinel cells - Already in tissues (EX: Macrophages, mast cells, dendritic cells)
White Blood Cells/Leukocytes - In circulation and must leave to enter tissues (Lymphocytes, monocytes, neutrophils, eosinophils, and basophils)
Inflammatory Mediators Chemicals are released by what cells?
Immune cells
Where are Mass cells located? What is their function in regards to inflammation?
Location: System wide in connective tissues
Function: Releases histamine. Associated with allergic response
Where are Macrophages cells located? What is their function in regards to inflammation?
Location: Free moving through tissue OR fixed within specific organ
Function: Perform phagocytosis, present antigens to T-cells, and release cytokines (TNF)
Where are Neutrophils cells located? What is their function in regards to inflammation?
Location: Within blood vessels
Function: Perform phagocytosis, MOST ABUNDANT, short lived (< 1 day), response to bacteria
Where are Dendritic cells located? What is their function in regards to inflammation?
Location: In most tissues
Function: Present antigens to T-cells, perform phagocytosis
What is the source of Histamine? What is its function?
Source: Mast cells
Function: Vasodilation, increase vascular permeability (allergies)
What is the source of Cytokines (TNF, Interleukins, etc)? What is its function?
Source: Macrophages and activated lymphocytes
Function: Endothelial activation, stimulate fibroblasts, protein catabolism (muscle atrophy)
What is the source of Leukotrienes? What is its function?
Source: Macrophages, mast cells, neutrophils
Function: Increase vascular permeability, chemotaxis, WBC adhesion
What is the source of Prostaglandins? What is its function?
Source: Macrophages, Mast cells, and endothelial cells
Function: Pain, fever, and vasodilation
A monocyte which leaves the blood stream is now named what?
A Macrophage
What stimulus triggers inflammation?
Injury to normal vascular tissues
What are the 5 cardinal signs of inflammation?
Heat - Due to Vasodilation
Redness - Due to vasodilation
Swelling - Due to increased vascular permeability
Pain - Due to stimulation of chemo-nociceptors
Loss of function
What are the 5 R's of inflammation?
1. recognition of injurious agent
2. recruitment of leukocytes
3. removal of agent
4. regulation of response
5. resolution (repair)
What is acute inflammation?
Rapid onset - Minutes to hours
Short duration
Cardinal signs present - Local and systemic signs. NO FIBROSIS (AKA Scar tissue)
Neutrophils present
What is chronic inflammation?
Slow onset
Longer duration
Few signs, angiogenesis, and fibrosis
Macrophages and lymphocytes present
In what 2 ways does the body recognize a stimulus in Acute Inflammation?
1. Recognition of non-self (pathogens or damaged cells) - PAMPS (in plasma membranes and endosomes)
2. Recognition of damage - DAMPS (Released from dying cells)
What things, when out of place in a cell, indicate damaged or dying cells?
Uric acid, ATP, decreased potassium, DNA
DAMPs stimulate damaged cells to release what? What does this do? What is this a major implication for?
IL-1
Induces inflammation and recruits inflammatory cells to the area
Implication for inflammatory diseases like Rheumatoid arthritis, lupus, etc.
What are the 2 steps in the inflammatory process?
1. Recognition of damage
2. Vascular change
What are the 3 types of vascular change?
1. Vasoconstriction
2. Vasodilation - to increase blood flow (which may make the area red and warm)
3. Increased vessel permeability - which can lead to edema and also increase blood viscosity
What are the 3 mechanisms of increasing vascular permeability?
1. Endothelial contraction - Gaps in postcapillary venules which respond to histamine
2. Endothelial necrosis - Which are leaky until repaired. Seen with burns, severe infections and even radiation
3. Angiogenesis - New vessels are made and have immature (leaky) endothelia. Seen in tissue repair and tumors
Where does vasodilation occur?
In the arterioles
Where does increased permeability occur?
In the venules
What is exudate edema?
Protein rich acute inflammation
What is Transudate edema?
Protein poor inflammation
When does edema occur?
When lymphatic drainage can't keep up. May transport microbes or cellular debris
What is Lymphadenopathy?
Disorder of Lymph Nodes
What is Lymphadenitis?
Inflamed lymph nodes. Increased size and pain
What is Lymphangitis?
Inflamed lymphatic channel. Causes a red streak on the surface of skin
What are the steps for leukocytes exiting vasculature?
1. Margination and rolling - Via selectins
2. Firm adhesion - Via integrins
3. Diapedesis (AKA Transmigration, extravasation, emigration) - Process of WBC squeezing out of the vessel
4. Chemotaxis - WBC travelling external to blood vessel to where it needs to go
What are neutrophils replaced by?
Macrophages and lymphocytes
What is "Leukocyte Activation?"
Stimulated by microbes, necrotic tissues, or foreign bodies
What are the 2 components in Phagocytosis?
1. Opsonization
2. Engulfment and degradation
What is opsonization?
Targeting or labelling a cell for destruction
What are opsonins?
Antibodies (IgG) and Complement proteins which enhance macrophages binding and breakdown
What are symptoms Acute-Phase Reaction of inflammation?
Fever - Via pyrogens, which lead to prostaglandin synthesis, which stimulates the hypothalamus to increase body temp
Elevated plasma proteins - Cytokines stimulate increased C Reactive Protein (CRP), increased fibrinogen, and increased Erythrocyte Sedimentation Rate (ESR)
What are the 2 inflammatory mediators?
Prostaglandins - Pain and fever
Substance P - Pain, neurotransmitter
What is the Normal Leukocyte count?
4500-10,000
What is leukocytosis?
When there are more than 10,000 leukocytes in blood
>Typically 15k-30k
Shift to the left
Depends on the infection:
>Bacterial has increased neutrophil counts
>Viral has increased lymphocyte count
What is a Leukemoid reaction?
Extreme leukocytosis
>Leukocyte count of 40k-100k
>Chronic inflammation
>Mimics leukemia
What is Leukopenia?
low leukocyte count
Under 4000 leukocytes
Seen in: HIV, Chemotherapy, and radiation therapy
What are the 6 patterns of inflammation?
1. Serous - blister
2. Fibrinous - scarring
3. Suppurative - pus, abscess
4. Ulcerative - peptic ulcers, canker sore
5. Pseudomembranous - C-diff
6. Granulomatous
What is serous inflammation?
"Blister"
Serum accumulates in or below epidermis
Seen in burns, viral infections, and autoimmunity

What is Fibrinous inflammation?
Seen in severe injury, which increases vessel permeability.
Fibrin rich exudate (Keep in mind fibrin is used in clotting and scarring)
What is a Suppurative AKA Purulent inflammation?
Pus forming local infection.
What is pus?
Neutrophils, necrotic cells, and edema
What is an abscess?
Pus acucmulation
What is ulcerative inflammation?
Superficial area of necrosis
What is pseudomembranous inflammation?
Formed on a mucosal surface and a membranous film composed mainly of fibrin, pus and necrotic cells
What is granulomatous inflammation?
Pattern of chronic inflammation.
>Build up of macrophages
What are the 3 outcomes of acute inflammation?
Resolution (Regen and repair) - Minimal injuries in cells which can replicate. Tissue returns to normal
Chronic inflammation - Severe injury or low ability to replicate. Failure to remove affecting agent. Frequent scarring
Scarring (Fibrosis) - Tissues can't replicate. Alters function
Unresolved inflammatory reactions can lead to what things?
Persistent infection/injury
Immunosuppression
Hypersensitivity
What are some features of chronic inflammation?
Mononuclear leukocytes, tissue destruction, angiogenesis and fibrosis (Scarring and clotting)
What are the 2 types of macrophage activation? Describe each
Classically active: Microbial, inflammation, and stimulate inflammation
Alternatively activated: Anti-inflammatory, tissue & wound repair, inhibit inflammation
What is lymphocytes role in chronic inflammation?
Sustain chronic inflammation
What is macrophages role in chronic inflammation?
Dominant cell at areas of inflammation
Phagocytosis of microbes and injured cells
Initiate angiogenesis and fibrosis
What are the 2 mechanisms of tissue repair?
Regeneration: Replace damaged cells
Scarring: Deposit fibrotic tissue to severely damaged cells which cannot divide/proliferate
What are labile cells?
Cells which constantly divide such as skin and epithelia
What are stable cells?
Capacity to repair but aren't constantly dividing
What is fibrosis/scarring?
Abnormal/extensive collagen deposition
Occurs following:
>Chronic inflammation
>Death of terminally differentiated cells
In myocardial infarction, what is an "infarct"?
A site which will result in fibrosis
When do scars form?
When tissues can't regenerate due to:
>Severe damage
>Prolonged injury
>Injury to terminally differentiated cells
What are the 4 steps in scar formation?
1. Angiogenesis - Generation of capillaries
2. Fibroblast migration & proliferation - build fibrous tissue
3. Collagen deposition
4. Remodeling
How long does it take for granulation tissue to develop? What does it contain?
3-5 days
Contains fibroblasts, WBC's, capillaries, and connective tissue
Macrophages secrete ________ which then activates ________ .
GF's; Fibroblasts
True or false, scars are always vascular
False, initially they are vascular. Later the become progressively avascular, hence why they get a pale colour
How is connective tissue remodeled?
Continually remodeled by a Balance between ECM synthesis and breakdown
What are Matrix Metalloproteinases (MMP's)? What does it break down? What is it produced by? What is its cofactor?
Breakdown collagen
Produced by: Fibroblasts, macrophages, neutrophils, and epithelial cells
Cofactor: Zinc ions
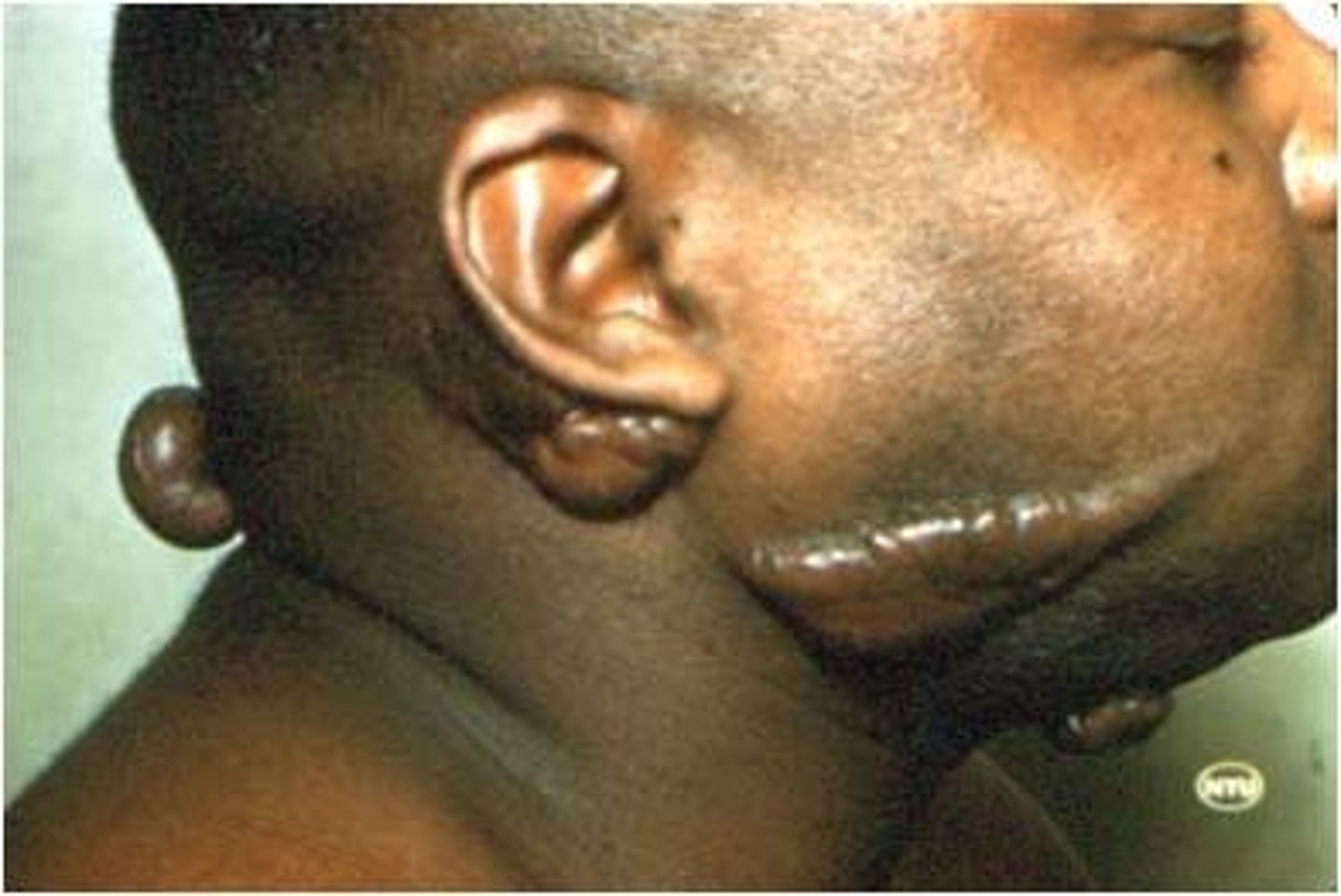
What are keloids? What descent of people are these more common with?
Scarring beyond boundaries of wound due to excessive granulation tissue and excessive collagen
African people
What factors impair healing?
Infection -> Which prolongs inflammation
Nutritional deficiency -> Specifically vitamin C, which decreased the basement membrane and makes vessels fragile
Glucocorticoids (Steroids) -> Reduce fibroblast activity
Poor perfusion - Reduced arterial supply and reduced venous drainage
Increased age, mechanical pressure, anemia, UV light, etc.
The healing of skin wounds is the combination of? What are the phases?
Epithelial regeneration and fibrosis