Applied epidemiology
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
What is epidemiology? (2)
- The study of disease in populations
- Observing populations and making inferences from these observations
What is veterinary public health?
- Veterinarians role in human public health
- Mainly in the recognition and control of zoonotic disease
also mental and emotional well being
What does epidemiology and veterinary public health encompass?
Studying animal diseases that affect humans and animals
what are the principles of being an epidemiologist
- Reduce and control the amount of disease
- Limit the effects of disease within populations
- Protect populations from disease
What are the main steps taken to investigate disease? (5)
1- Observation and recording of the natural occurrence of disease
Basic parameters e.g. morbidity
2- Presentation and analysis of the observations
3- Determine the cause of the disease
Causal principles and approaches
4- Understand transmission, clinical signs, diagnosis
I.e. 'disease ecology'
5- Efficiency of different techniques to combat disease
E.g. control, prevention...
What is a contagious disease? (2)
- A disease transmitted by direct or indirect contact with a host that is the source of the pathogenic agent (not including vector transmission so in contagious disease there is no need for an intermediate organism).
- The same disease can be contagious in some species and not in others.
What is a communicable disease? (2)
- I.e. transmissible disease
- A disease whose causal agent can be transmitted from successive hosts to healthy subjects, from one individual to another.
What is the difference between contagious and communicable diseases?
Communicable just means the disease can be transmitted from one individual to another either:
- Contagiously (from one infected animal to a healthy animal without an intermediate organism, e.g. through direct contact or indirectly by infected foodstuffs).
- Non-contagiously (from one healthy animal to another through an intermediate organism/vector, e.g. a mosquito or tick).
Thus, communicable diseases include contagious and non-contagious diseases. But a vector-borne disease is communicable only, not contagious.
What is infectious disease?
A disease caused by a microorganism (bacterial, viral, or parasitic) that can be transferred from one host to another (communicable).
What is prevalence? (2)
- Measure of disease occurence
- Total individuals with condition at a particular time/ period/ population at risk of condition at that time/ midway through the period.
What is incidence? (2)
- Number of new health-related events in a defined population within a specified period of time.
- Measured as frequency count, rate, or proportion.
What is mortality?
Death
What is morbidity? (2)
- Any departure, subjective or objective, from a state of physiological or psychological well-being.
- I.e. sickness
What is an endemic disease?
Disease common, or restricted to a particular region, or demographic (e.g. one region of a country or in one type of population):
The disease is constantly present in a specific area but usually at a relatively low, stable rate.
An endemic does not necessarily refer to a smaller disease burden. Some endemic diseases can affect large populations (e.g., malaria, tuberculosis), but they remain at a relatively stable, predictable level.
how is endemic disease transmission controlled and stabilised and what does this do to R₀
due to immunity, interventions, or behavioural factors,
keeping R₀ close to or below 1.
What is an epidemic disease?
A level of disease in a population significantly greater than usual:
The disease spreads more quickly and affects a larger number of people than usual in a given time and place.
An epidemic is typically an unexpected surge in cases, and the "size" refers to the rapid and often uncontrolled increase in new cases, which could be much higher than normal levels.
what is the transmission of epidemic diseases like and what does this mean for R₀
Transmission increases suddenly,
R₀ rises above 1, leading to widespread outbreaks (no longer manageable so no longer endemic).
what is R0
basic reproduction number per transmissibility rate. The average number of cases infected by a primary case when the population is naive.
what is the average R 0 for endemic disease
average number of cases infected by a primary case is <1
what is the average R0 number for epidemic disease
a level of disease significantly greater than usual in a population >1
What is a pandemic disease?
An epidemic disease that occurs worldwide.
What is sensitivity?
The ability of a test to detect disease in a diseased patient: probability (positive predictive value) that a patient with a disease will have a positive result (a true positive).
What is specificity?
The ability of a test to rule out the presence of disease in a healthy patient: probability (negative predictive value) that a healthy patient without a disease will have a negative result (a true negative).
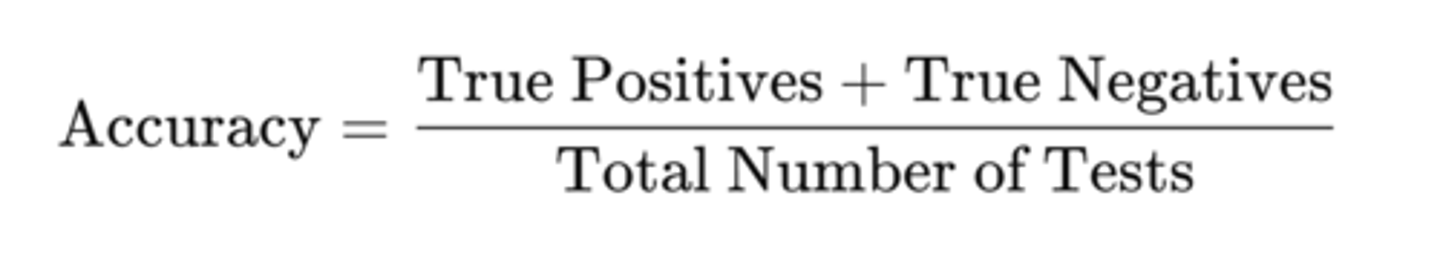
What is accuracy in diagnostics?
The precision (reproducibility/consistency of a result) and correctness (PPV and NPV of a result) of a diagnostic test or procedure in detecting a disease. More specifically, it involves how well a test correctly identifies those with and without the disease.
How is accuracy measured in diagnostics?
The overall accuracy of a test can be thought of as the proportion of correct results (both true positives and true negatives) out of all tests performed.
What is a gold standard diagnostic test? (3)
- Highest accuracy: The gold standard test is the one that has the fewest errors, meaning it produces the most reliable results (i.e., minimal false positives and false negatives).
- Widely accepted: It is universally recognized by the medical community as the most reliable diagnostic method for that specific disease.
- Definitive diagnosis: It is the test used to confirm the presence or absence of the condition, often after other less accurate tests have been performed.
what is the R number
R= reproduction number at any time point during an outbreak
the population is no longer naive so need to consider those recovering from disease or currently infected when calculating these
What is disease control?
The reduction of disease incidence, prevalence, morbidity or mortality to a locally acceptable level as a result of deliberate efforts; continued intervention measures are required to maintain the reduction.
What is disease prevention?
The process of reducing risks and alleviating disease to promote, preserve, and restore health and minimize suffering and distress.
What is disease eradication?
Complete elimination of the disease AND the agent from a population/region.
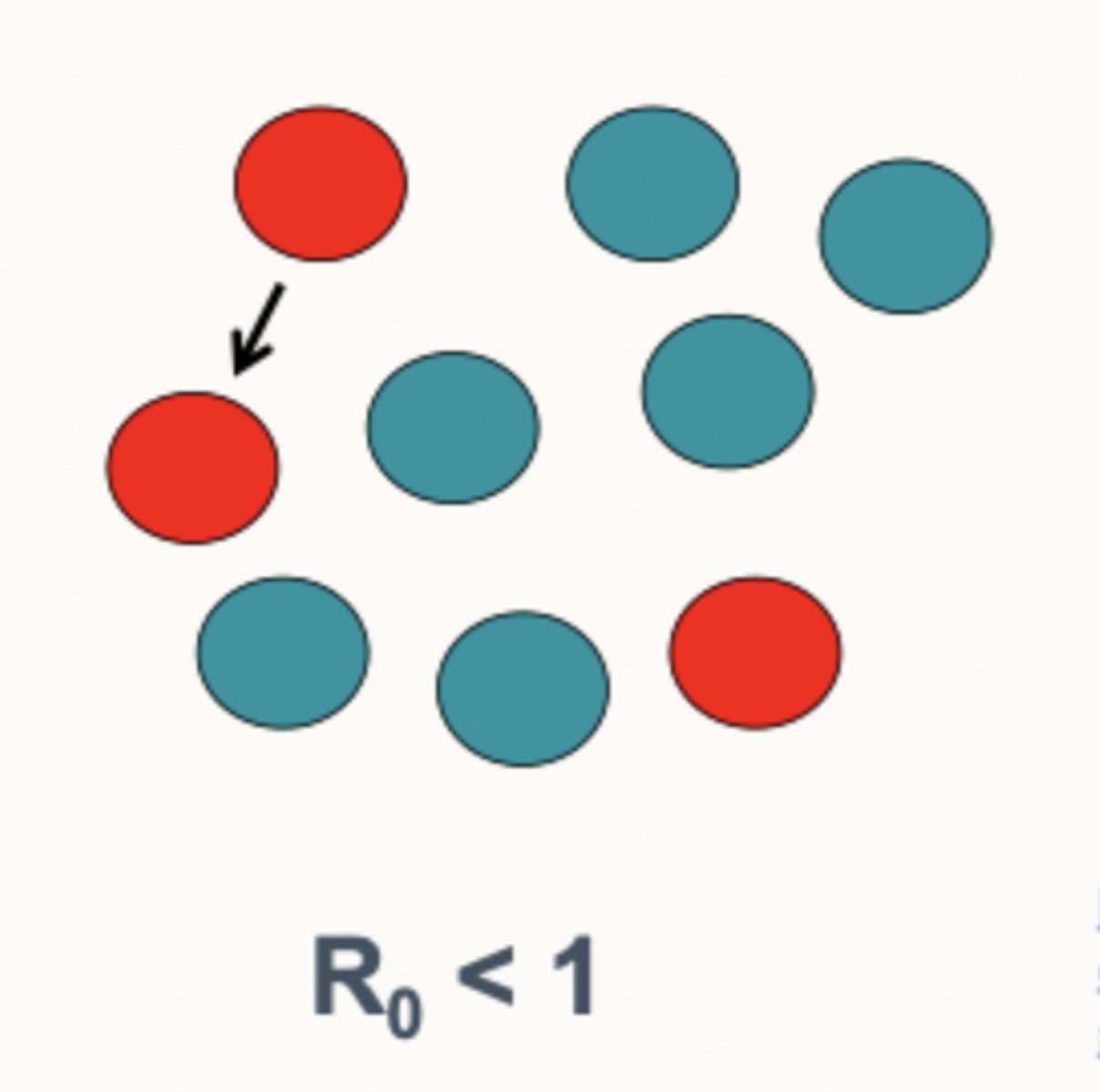
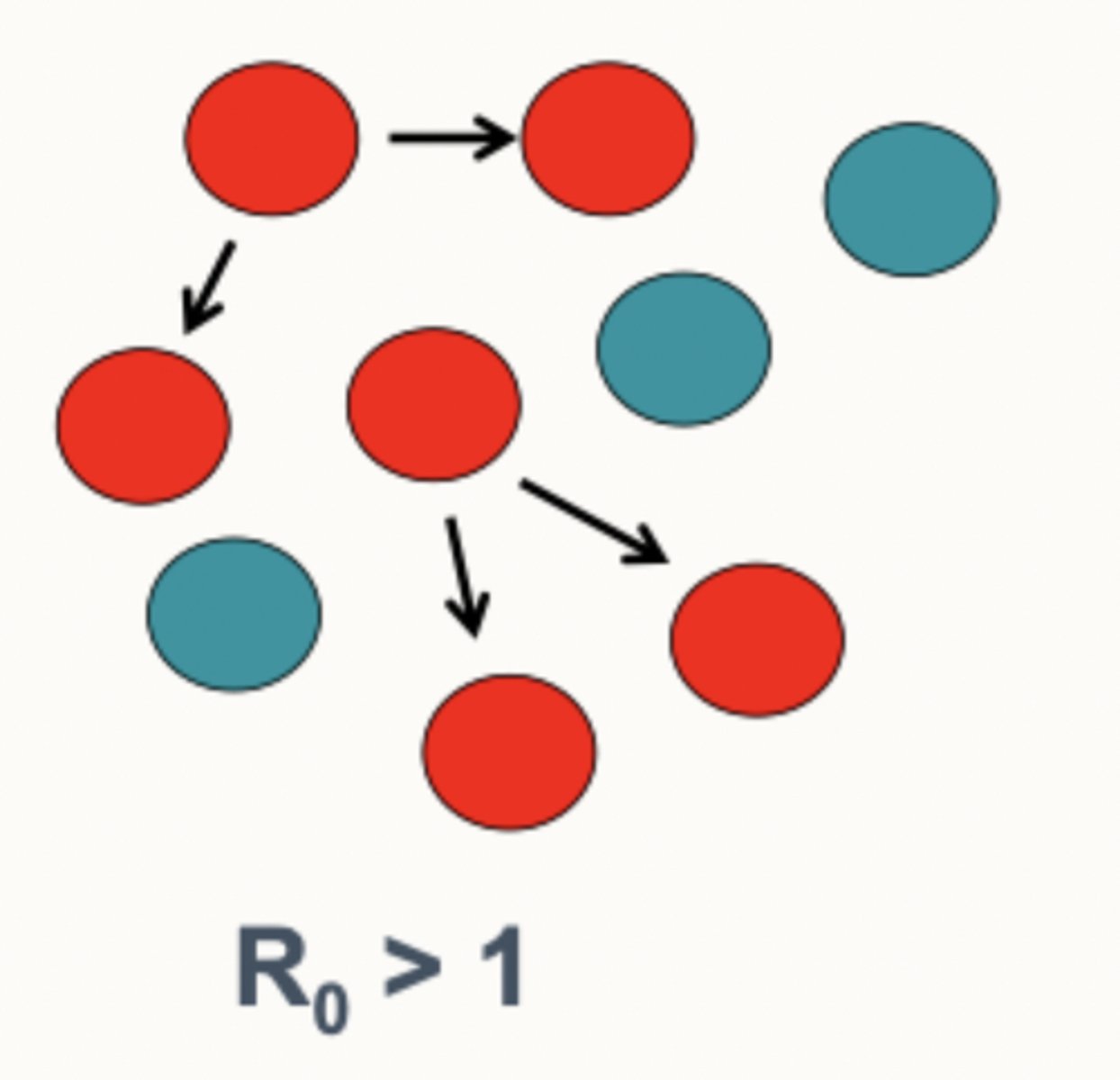
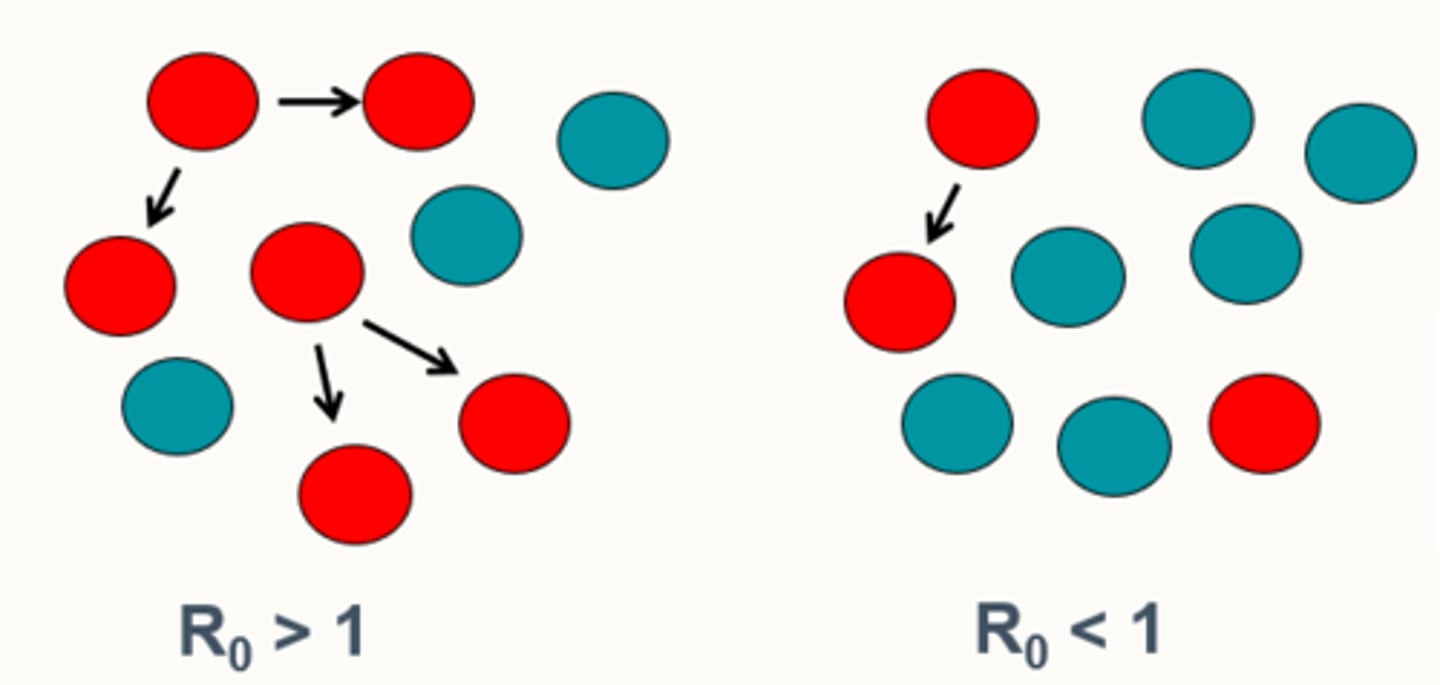
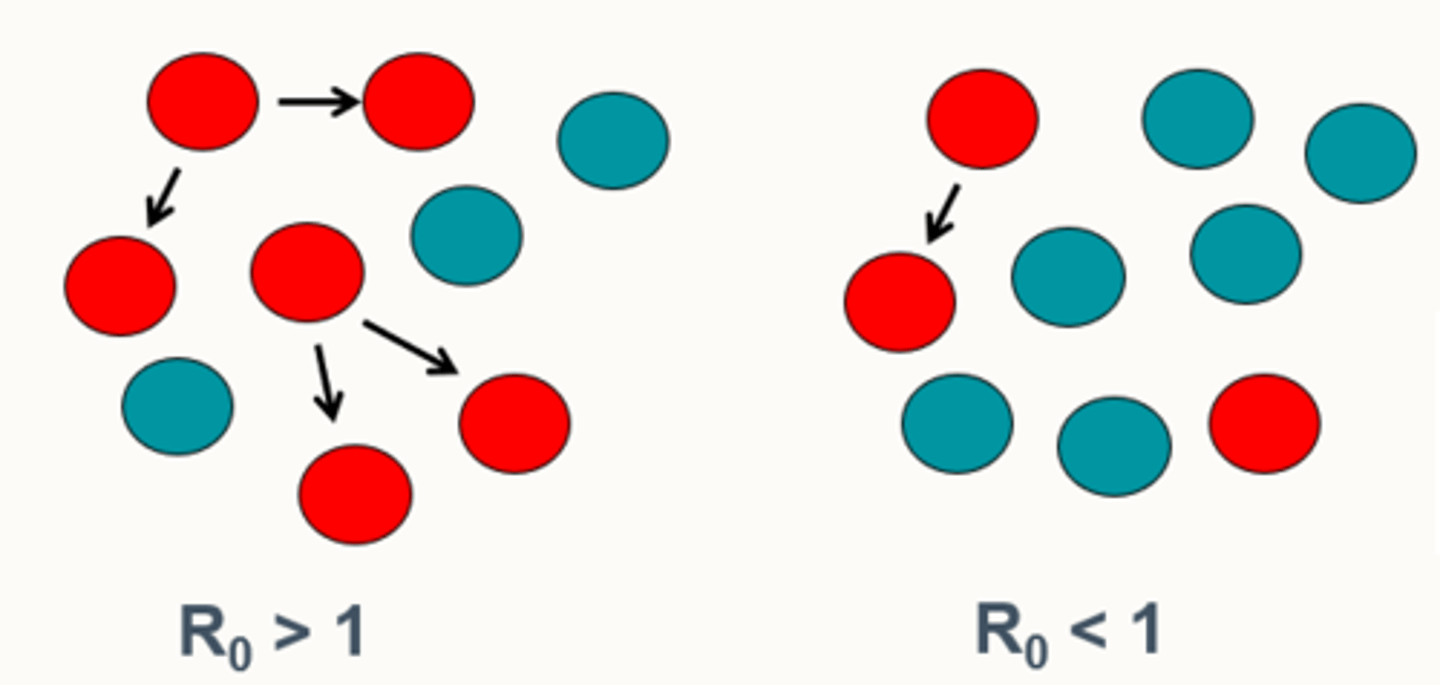
What is R₀ (pronounced R nought)?
The basic reproduction number/transmissibility rate of a disease, i.e. a measure of the average number of people that one infected individual (usually used to refer to as the primary case) will go on to infect in a naïve population (not considering factors like immunity or disease preventions):
- If R₀ > 1, the disease will spread in the population because each infected person is passing the disease on to more than one other person.
- If R₀ < 1, the disease will gradually decline and eventually disappear, because each infected person is infecting fewer than one other person on average.
What is the R0 in an:
- Endemic
- Epidemic?
- Endemic: R₀ < 1
Average number of cases infected by a primary case is less than 1
- Epidemic: R₀ > 1
Average number of cases infected by a primary case is greater than 1
Why is R₀ Less Than 1 in an Endemic Situation?
In an endemic situation, the disease continues to circulate at a stable level within the population, but the overall R₀ may be less than 1 due to the following reasons:
- Herd immunity (pre-existing immunity in some from disease or vaccination means reduced the number of suspectable individuals than are naïve).
- Behavioural changes (more people use masks reducing the transmissibility of a pathogen).
- Public health measures like vaccination, surveillance, treatment (disease interventions to reduce the spread, reducing incidences of infection).
- Pathogenic factors like if the disease can only spread slowly, or is not highly contagious/communicable, or environmental conditions like seasonality that are affecting the pathogens survival outside the body. Or a disease can evolve to be less virulent over time, causing less severe disease or becoming less transmissible.
What is the R number?
Reproduction number at any time point during an outbreak (unlike R nought, taking into account real-time considerations that can affect how the transmission rate of a disease changes over time) so is the current/real-time transmission rate of a disease in a population.
- If R > 1, the disease is still spreading.
- If R < 1, the disease transmission is under control and may eventually decline.
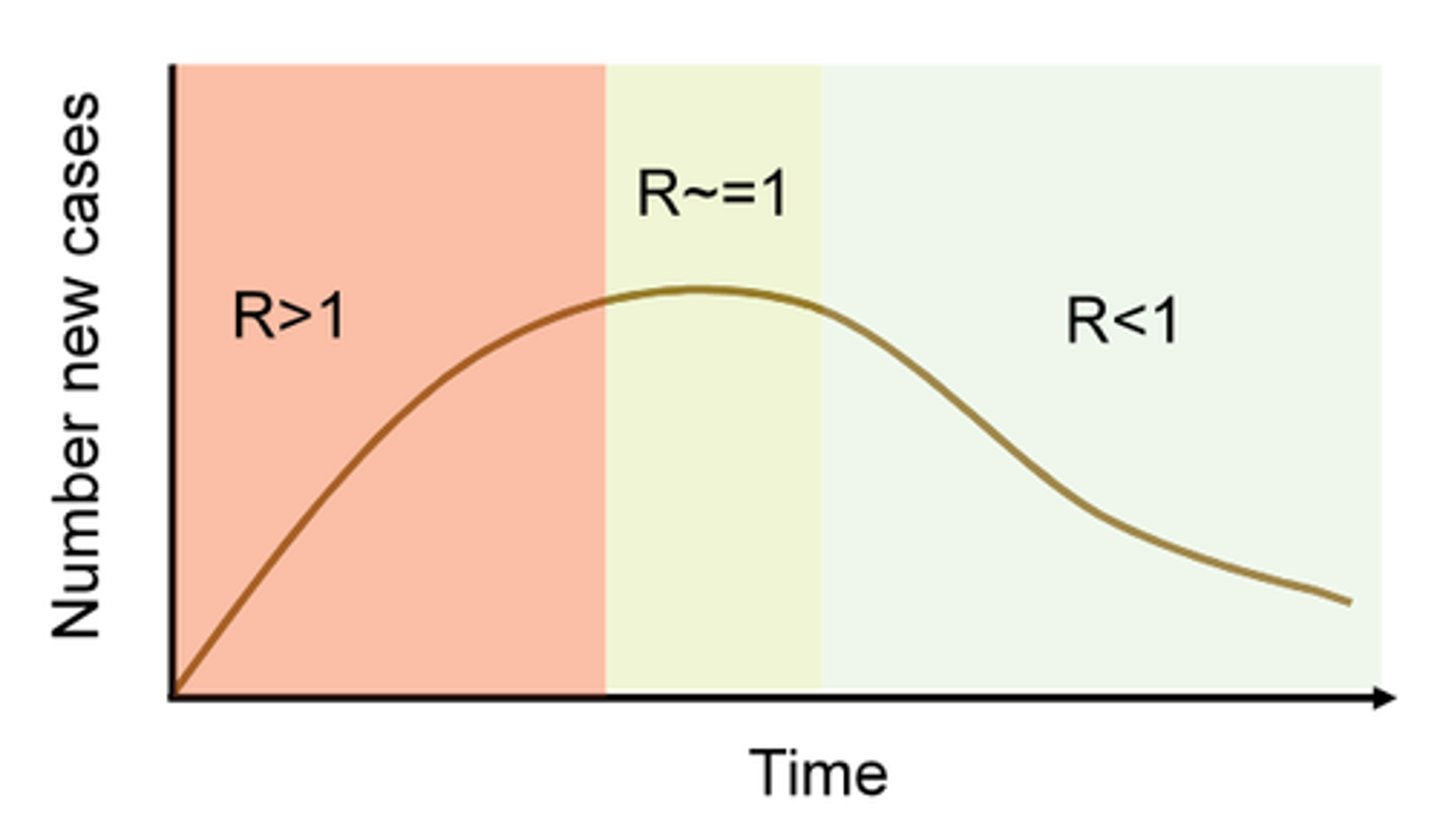
What is a consideration to be made when calculating the R number? (3)
Unlike R₀, which assumes no immunity and no interventions, R reflects how the disease is actually spreading in the population at a given moment:
It can vary over time based on the level of immunity (from prior infection or vaccination), public health measures (such as social distancing or mask mandates), and the behaviour of individuals in the population (such as the number of close contacts or social gatherings).
What questions/observations should be made when investigating a disease outbreak? (5)
Number of cases
How does it relate to the number 'normally' seen (endemic)?
What animals/people are at risk of infection and who is the denominator?
Distribution of disease - which areas? are there multiple areas on a farm?
Rates - over what time?
Are specific subgroups are being infected?
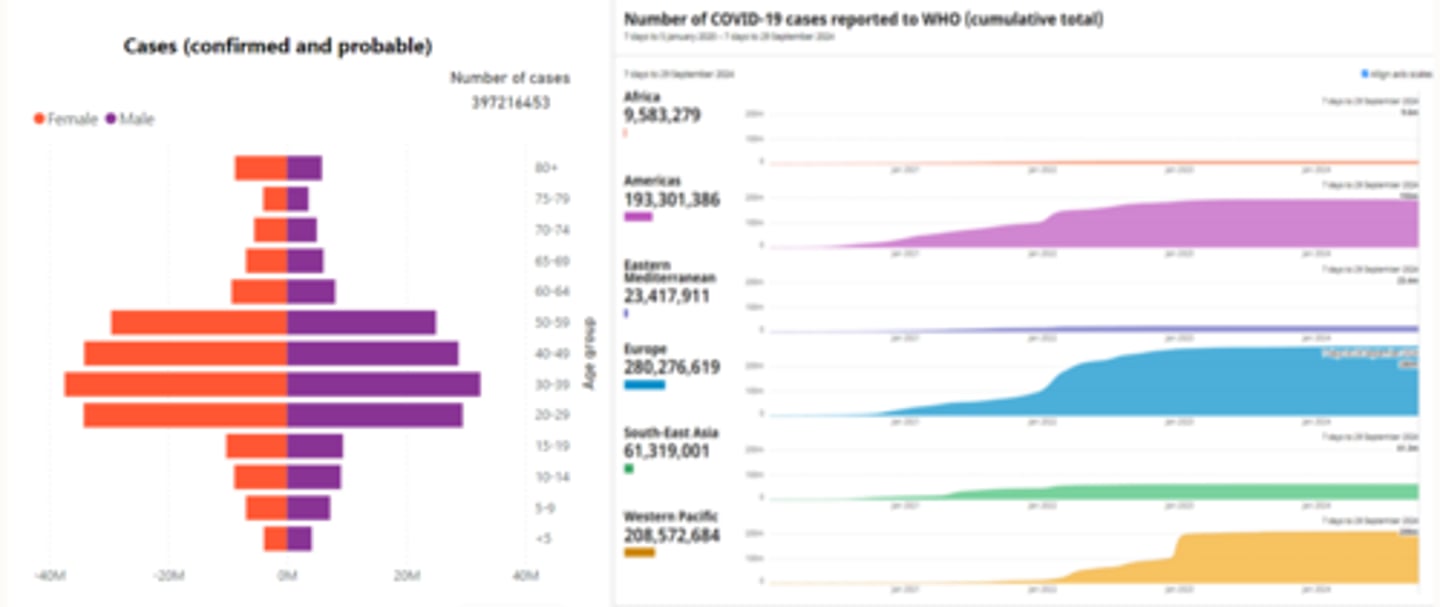
How can observations be presented and analysed? (4)
- Statistics
- Maps (distribution/density of disease over regions)
- Epidemic curve (distribution of disease over time)
- Distribution charts (can show what individuals in different groups are affected for example, who appears to be the denominator).
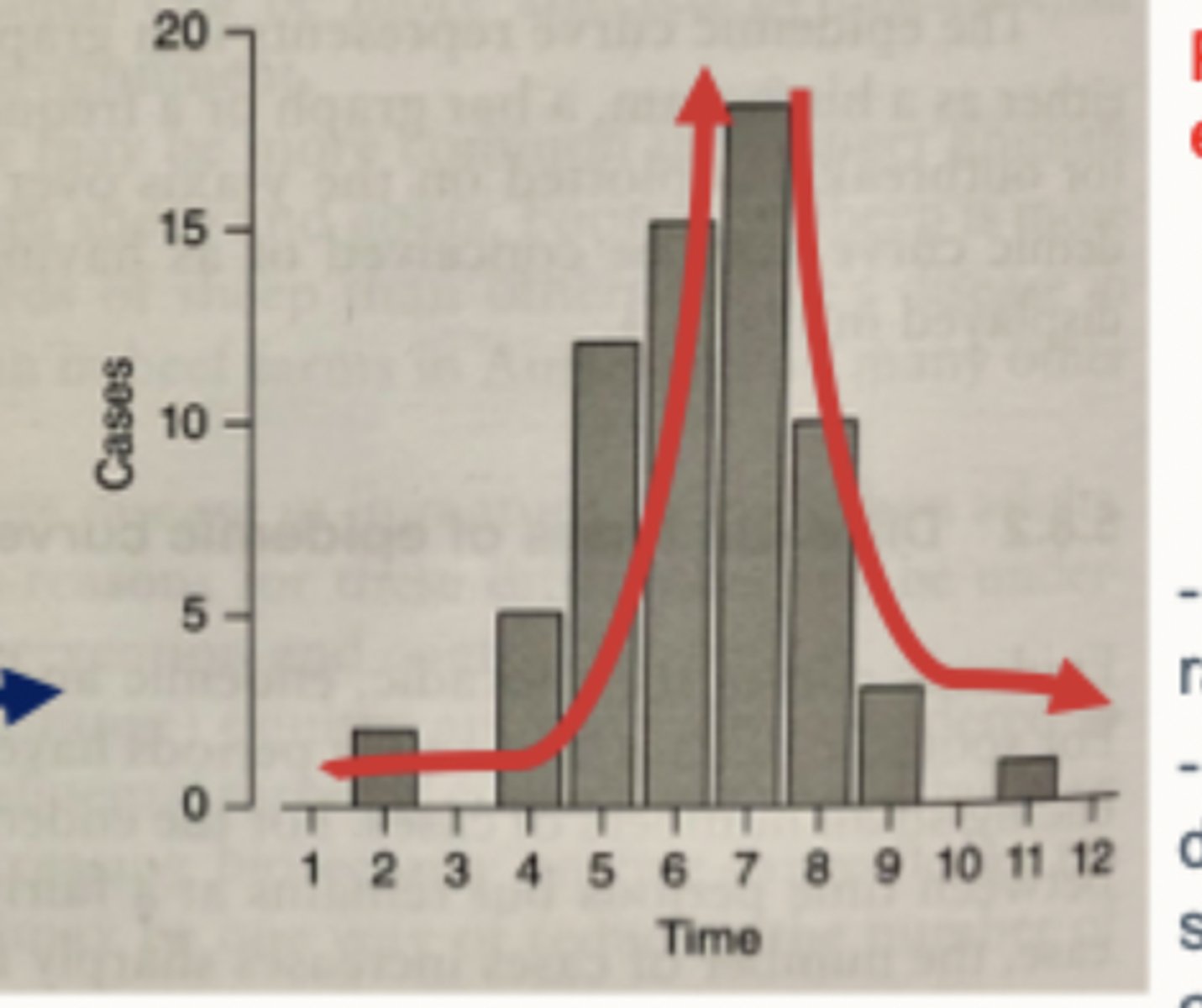
What can an epidemic curve tell you?
The shape of an epidemic curve can give you a preliminary guess at what is causing a problem when you don't know the cause.
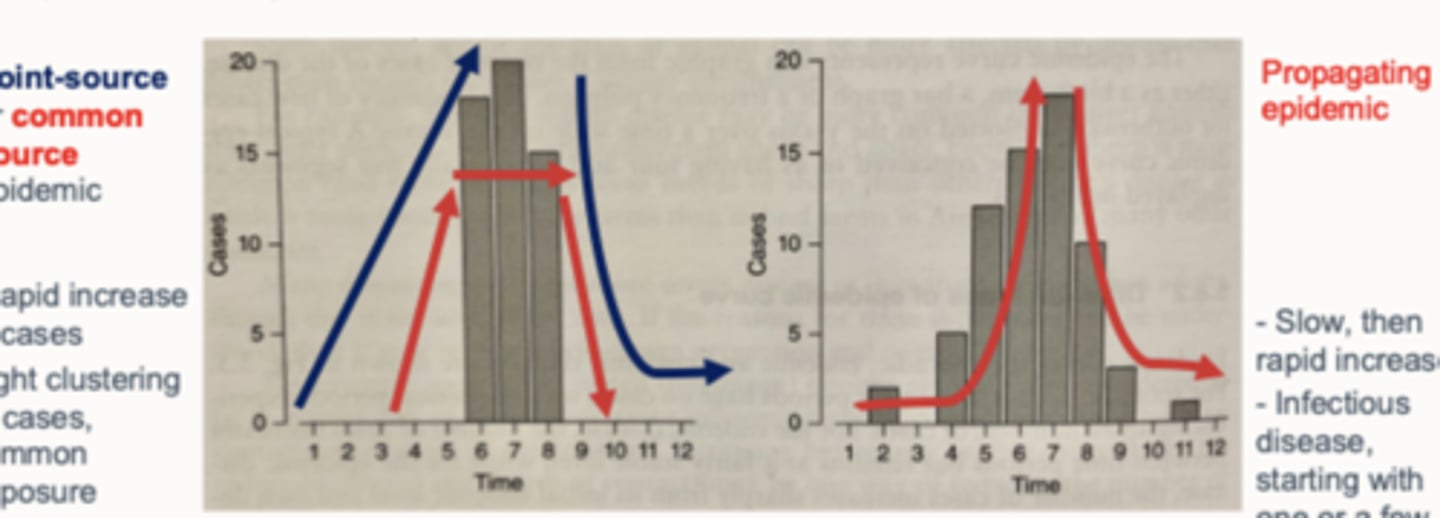
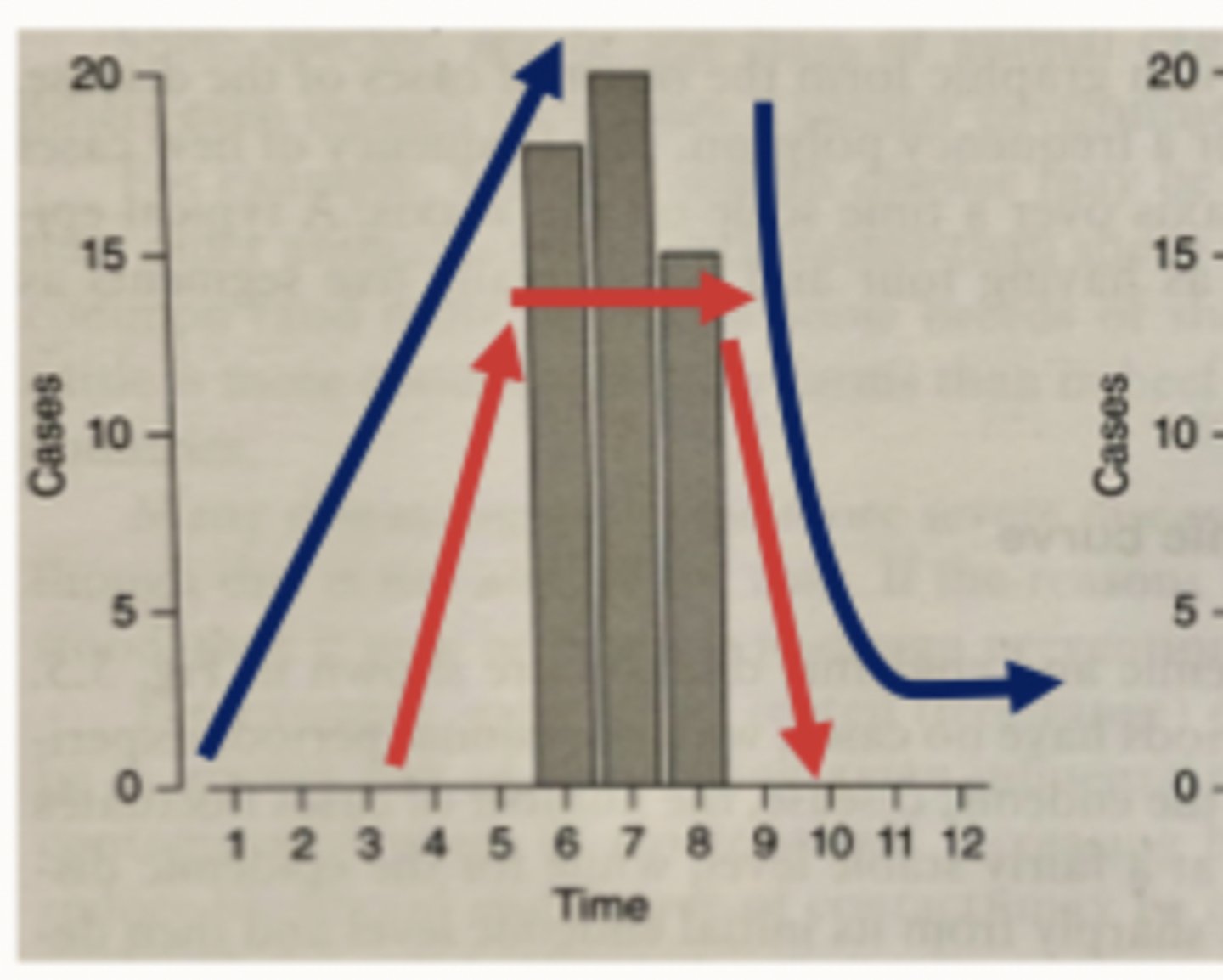
what are the 2 types of epidemic curves
point-source/common source epidemic
propagating epidemic
What is a point-source or common source epidemic?
How does it appear on an epidemic curve?
- Caused by common exposure e.g. food poisoning by feed contamination
- Rapid increase, tight clustering of cases and rapid decrease in cases
What is a propagating epidemic?
How does it appear on an epidemic curve?
- Caused by infectious disease, starting with one or a few infected individuals
- Slow, then rapid increase
What are the principles of causation?
Criteria for establishing cause of disease (Hill's criteria):
Temporal Relationship: Does the potential cause occur before the disease?
Strength of the Association: Is there a strong statistical relationship between the cause (agent) and the disease?
Dose-Response Relationship: Is there a pattern where a greater exposure to the cause leads to a higher risk of the disease?
Consistency: Is the association observed consistently across different studies, populations, or settings?
Biological Plausibility: Does the association make sense based on what we know about biology? For example, does it fit with our understanding of how diseases and their symptoms work? (e.g., flu causing flu-like symptoms like a cough). (common diseases are common)
What is a risk factor when studying causation of disease?
A risk factor is any characteristic, condition, or behaviour that increases the likelihood of an individual developing a disease or health condition. These factors can be genetic, environmental, lifestyle-related, or even demographic in nature. E.g. smoking in those with lung cancer.
What are common approaches to establishing causation?
- Case-control studies
- Cohort studies
Both longitudinal observational studies.
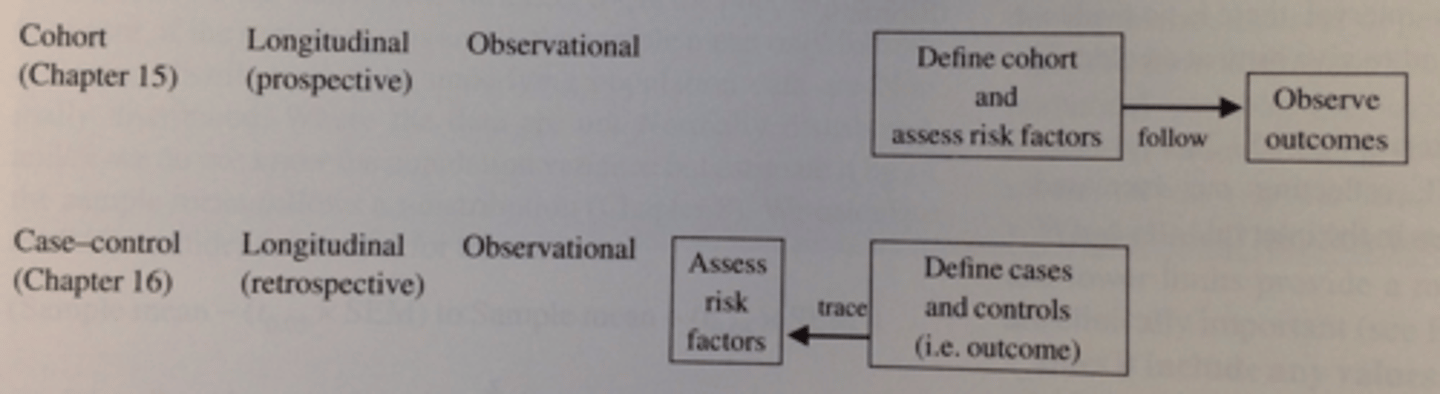
when would you do case-control studies and what are they?
(retrospective): Compare between cases and non-cases (diseased and non-diseased), e.g. looking retrospectively at the differences in exposure to risk factors in cases and non-cases.
when would you do cohort studies and what would you do ?
(prospective): Look prospectively at individuals exposed and not exposed to risk factors and see if they develop disease.
The results collected from causation studies can be used to look at relationships/associations in the data between risk factors they were exposed to and demographics of diseased individuals to identify what?
The strength of association (who is at risk).
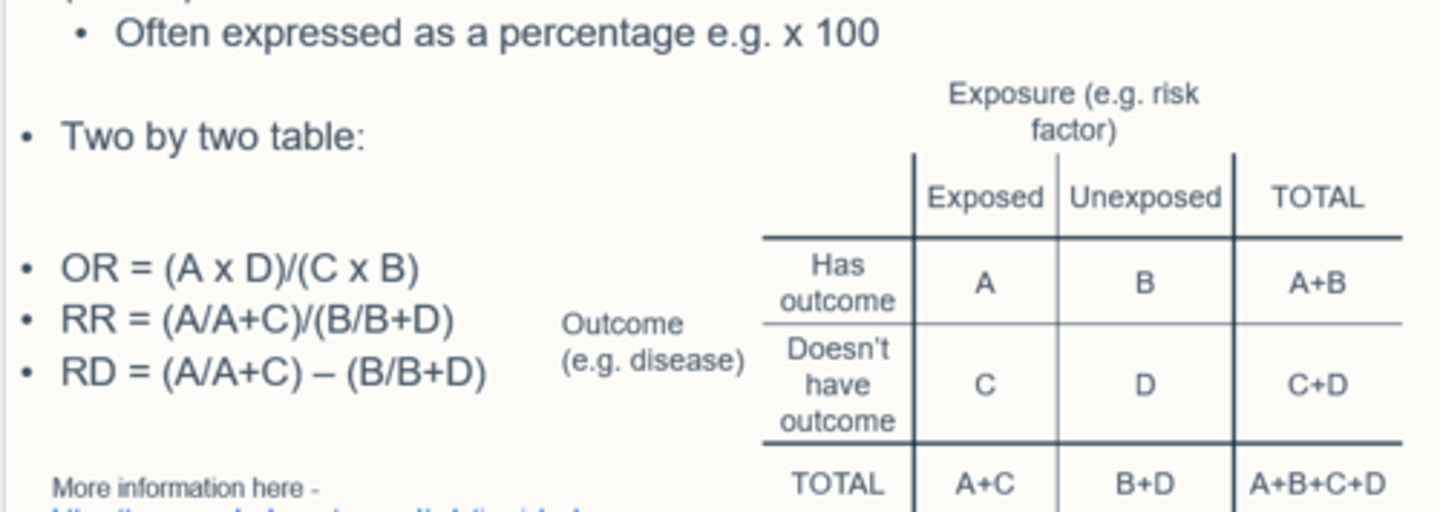
How can the strength of association be measured? (2)
- Odds ratio (OR)
- Relative risk (RR); risk ratio
What is the odds ratio measure?
What study is it used in?
What do its interpretations mean? (2)
- Odds of the disease (having the disease or not) in the exposed group vs. with odds of the disease in the unexposed group
- Common in case-control studies (diseased and non-diseased)
- OR>1 (Risk factor - RF - associated with disease)
- OR<1 (RF not associated with disease - 'protective')
What is the relative risk /risk ratio measure?
What study is it used in?
What do its interpretations mean? (2)
- Ratio of risk of disease developing in exposed group to risk of disease developing in unexposed group
- Common in cohort studies (do those exposed to risk develop disease)
- RR>1 (RF associated with disease)
- RR<1 (RF not associated with disease)
What is the general interpretation of OR and RR?
The greater the numbers, the more likely the risk factors associated with outcome (with a caveat for confidence intervals).
What is risk difference (RD)? What study is it used in?
Risk Difference (RD)/Attributable Risk measures the absolute difference in the risk. The absolute difference measures the difference in the actual risk (observed probability of disease occurring in a group calculated as the diseased in the group divided by total number of people in the group) of an outcome between two groups.
- Such as the exposed group and the unexposed group. (used in cohort studies)
What is the confidence interval (CI) and how does this allow us to predict confidence level?
A Confidence Interval (CI) is a statistical range or interval, derived from sample data, that is used to estimate the true population parameter (such as a population mean, proportion, or risk) with a certain level of confidence. It provides a range of values within which the true value is likely to lie, based on the data from a sample.
- The confidence level (often 95%) refers to the probability that the true population parameter is contained within the interval if the study were repeated multiple times under the same conditions.
Why is a larger sample size better in relation to CI?
The width of the CI reflects the precision of the estimate:
- A narrower CI indicates a more precise estimate (i.e., the sample data gives you a relatively clear idea of the population parameter).
- A wider CI suggests more uncertainty or variability in the estimate, meaning the data doesn't provide as precise an estimate of the population parameter.
Narrower range means a truer result to what the result actually is, e.g. more spot on, less room for guessing.
What is the importance of characterising pathogenic microorganisms in the investigation of disease outbreaks? (4)
- Can help determine causation
- Can identify 'carriers' and transmission/lifecycle
- If identified earlier can reduce spread of outbreak
- Can influence prevention or control programmes
What are the main strategies used to prevent, control and eradicate animal diseases?
- Testing to identify causation
- Via sub-typing genetic material for pathogen identification
How does genetic typing work? (3)
-An assortment of techniques e.g. RFLP, PCR fingerprinting, DNA sequencing
-Amplify targeted pieces/whole of the pathogen's DNA/RNA in order to determine either speciation (if unknown) or strain identification
-Compare the 'fingerprint' from human and animal cases and see if they are the same
What are the advantages of genetic typing in the prevention, control and eradication of animal diseases? (7)
- Increased sensitivity and specificity of diagnosis
- Faster
- Good for organisms difficult to culture (M.bovis and prions)
- Outbreaks can be detected and controlled earlier on
- Can provide evidence of causation when combined with epidemiological evidence
- Can identify 'carriers'
- Can improve prevention or control programmes
What is a consideration when presenting and analysing disease data? (4)
- Is it based on assumptions/predictions or actual data
- How accurate is the testing e.g. lateral flow vs PCR
- Is the testing active or passive
- What is the source of information? may be under/overrepresented on purpose e.g. country response to COVID
What is disease ecology?
Study of host-pathogen interactions within the context of their environment and evolution
What are the prerequisites for disease ecology? (2)
Knowledge of pathogen (which increases over time with novel pathogens:
- Pathogen action
- Transmission routes
- Optimal environmental conditions etc.
Knowledge of what 'states' animals/people within your population can be in:
- Susceptible (not got disease)
- Infected (have disease)
- Recovered (have had disease)
- Potentially susceptible again (can be re-infected)