Urinary System Development
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
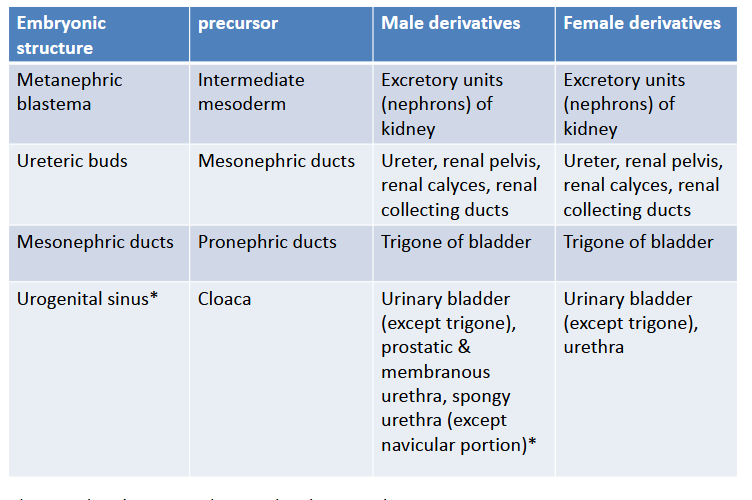
Describe how the Urinary & Genital systems are embryologically & anatomically interwoven
Both develop from common pair of intermediate mesoderm
elevations located on each side of the the median plane along the
embryonic posterior abdominal wall.
Describe the gross structures of the kidneys:
Hilum
Renal Sinus
Renal Pelvis
Major Calyces
Minor Calyces
Renal Cortext
Renal Medula
Renal Column
Renal Pyramids
Medullary rays
Renal Papilla
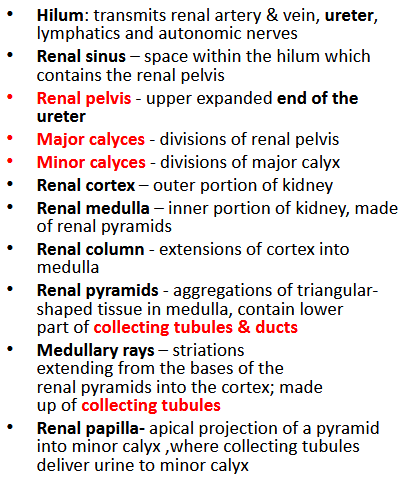
Describe the two systems that the kidneys have and the components of each system
Filtration System: filter blood and produce urine
Renal corpuscle: glomerulus (arterial
capillaries)+ Bowman’s capsuleProximal convoluted tubule
Henle’s loop (thick and thin limbs)
Distal convoluted tubule
Collecting System collect urine for transport to the bladder by the ureter
Collecting tubules & ducts
Minor calyces
Major calyces
Renal pelvis
Ureter
What are the three stages of kidney development; Where and when do they appear?
Pronephros (cranial, week 4)
Mesonephros (thoracic & lumbar, week 4-8)
Metanephros (pelvic, week 5-40)
***Three overlapping kidney systems develops in a cranial-caudal sequence during gestation***
Describe the Pronephros’ characteristics
What is the Pronephric Duct? What does it become and why is it important?
Pronephros
non-functional excretory tubules: no glomeruli & no
connection w/ pronephric duct
Pronephric duct
collecting duct runs caudally and opens into anterior portion of cloaca at the end of 4th week
becomes mesonephric duct
plays essential part as inductor of mesonephos
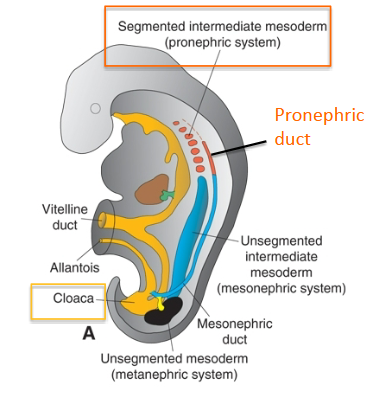
Describe the Mesonephros:
How is it formed? Components?
Describe how the Mesonephros can persist after the 8th week? Describe its excretory tubules
Where is the Wolffian duct derived/open to? What does this structure form in the future?
Mesonephros Formation:
During Growth/Folding of Embryo → intermediate
mesoderm forms a bulge (urogenital ridge) that comprises:Gonadal ridge
Mesonephros
Mesonephric duct
Paramesonephric duct
Mesonephros:
some caudal tubules of mesonephros becomes efferent ductules of testis
Excretory Tubes:
Has Bowman’s Capsule surrounded by Arterial Glomerulus
No Loop of Henle
Opens into mesonephric ducts
Mesonephric (wolffian) duct
Derived from pronephric duct
Opens into urogenital sinus (ventral derivative of cloaca)
DEVELOPS INTO/GIVE RISE TO:
uretic bud of metanephros system (future ureter)
trigone region of the bladder (Caudal End of Duct)
Persists As
ductus deferent
seminal vesicles
(degenerate in female)
Describe the Metanephros
When does it produce urine?
What 2 sources develops into this?
Describe the metanephric diverticulum or ureteric bud
Where does this developed from?
How does it contribute to the adult Kidneys
Describe the metanephric mesoderm or metanephic blastema
How does it contribute to the adult kidneys
How does the kidney’s shape change from infancy to adult
Metanephros: permanent kidney
Arrived by the 5th week, produces urine in the 10th
Developed from ureteric bud & metanephric blastema
Both of intermediate mesodermal origin
metanephric diverticulum or ureteric bud
Developed from outgrowth of mesonephric duct near the cloaca
Penetrates metanephric blastema → Subdivision → COLLECTING SYSTEM
Metanephric blastema induces branching of ureteric bud
metanephric mesoderm or metanephic blastema:
metanephric tissue caps induces Nephron (near collecting tubules) Development
Nephron develops Bowman’s Capsule, surrounded by glomerulus
Distal end of bowmans → Rest of nephron (PT, LOH, DT, etc)
At birth, kidneys = lobulated appearance ;disappears as
nephrons growth in size but not in number during infancy
Describe the Ascent & rotation of the kidneys
Describe the blood supply
Ascent & rotation of the kidneys:
Moves from Pelvis to Abdomins → Reretroperitoneal on posterior abdominal wall by 9th week
90 ̊ medial rotation from facing anteriorly
Blood Supply:
supplied by arteries closest to them at higher levels while ascending
Main Blood Supply:
caudal arteries = degenerate;
Cranial Branches from abdominal aorta = permanent renal arteries
Accessory renal arteries:
persistence of embryonic vessels > enter
superior or inferior pole of kidneycan obstruct ureter & enlarged renal pelvis
Note: Prior to birth, the placenta is the primary remover of nitrogenous wastes from the fetus via the allantois. After birth,
the kidney takes on this role. The urachus (median umbilical ligament) is remnant of allantois.
Describe Renal Agenesis:
How does this happen?
Compare agenesis of one vs two kidneys
Renal Agenesis:
Absence of kidney(s) when metanephric diverticulum (ureteric bud) fails to develop or degenerates early → no nephrons
Unilateral Abscence:
relatively asymptomatic b/c remaining kidney can take up the slack
Bilateral Absence:
Incompatible w/ postnatal life
results in oligohydramnios → (no micturition)
Potter sequence
(flattened face, hypoplastic lungs, limb deformities)
Describe Cystic Kidney Disease:
Multicystic dysplastic disease
Polycystic Kidney Disease
Multicystic dysplastic disease:
Kidney consists of irregular cysts (bunch of grapes)
Genetic factors & certain drugs
Unilateral = Good outcome; Bilateral = fatal after birth
associated with Potter sequence
Abnormal Induction = Renal Agenesis
Polycystic Kidney Disease:
Kidneys contain multiple small to large cysts--severe renal insufficiency
Autosomal recessive (childhood): Cysts develop from the collecting duct
death usually occurs after birth, but survival has increased due to hemodialysis and kidney transplants
Potter sequence
Autosomal dominant (adult): mutation in ADPKD genes (polycystin 1& 2) that play a role in renal tubular development & function
cysts develop from parts of nephron
renal failure in adult, more common
Describe the types of Renal Ectopia/ Consequences
What is Malrotated Kidney/ Consequences
Renal Ectopia:
Simple: one or both kidneys in an abnormal position
Usually more inferior than usual; failure to ascend
discoid or pancake kidney: Pelvic kidneys may fuse to form a round mass; does not ascend
Crossed: Developing Kidneys Fused, then ascend
Consequences
urinary tract infections, kidneys stones, kidney failure b/c of blockage or vesicouretral reflux
Malrotated:
no rotation > face anteriorly; too far > face posteriorly; also can face laterally
Usually asymptomatic but hydronephrosis and stone formation more frequent
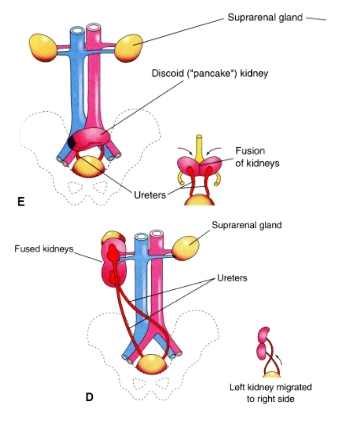
What is a horseshoe Kidney
Which conditions increases risk of this
Horseshoe Kidney:
results from fusion of poles of kidneys, usually inferior poles
U-shaped kidney in hypogastrium, anterior to lumbar
vertebrae because normal ascent prevented by the root
of inferior mesenteric arteryAsymptomatic
Higher Risk of Horseshoe Kidney:
Turner Syndrome (45,XO)
Wilms‘ tumor (nephroblastoma)
Increased risk of infection (pyelonephristis)
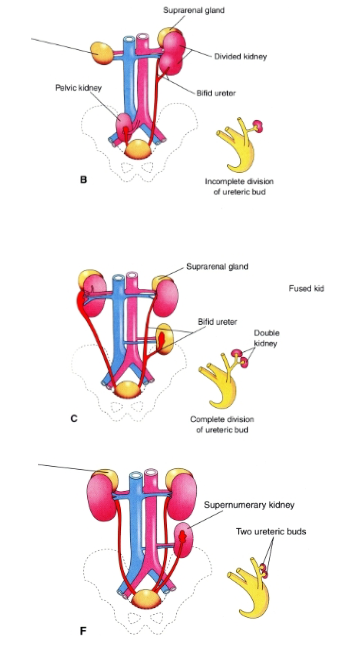
Describe the various ways duplication of the Urinary Tract can occur
Duplications of the Urinary Tract:
result from division of one ureteric bud
incomplete division --> divided kidney with a bifid ureter (B)
complete division --> double kidney with bifid ureter (C)
formation of 2 ureteric buds
supernumerary kidney with own ureter (F)
Describe the development of the bladder and urethra
What can abnormalities create?
Development of the bladder and urethra:
Begin to develop w/ division of the cloaca by the urorectal septum into the urogenital sinus anteriorly and anorectal canal posteriorly
Tip of urorectal septum forms perineal body
Abnormalities:
rectourethral & rectovaginal fistula where hindgut opens in urethra or vagina
What is the perineal body?
Attachment point for many muscles and fascial structures of the pelvis and perineum
Between anal aperture and vestibule (female) or bulb of penis (male)
Describe the three portions of the urogenital sinus
Urinary bladder (minus trigone) superiorly
Pelvic part:
Male: prostatic & membranous parts of the urethra
Female: Upper urethra
Phallic part:
Male: penile (spongy) urethra
Female: lower urethra with external urethral orifice opening in vestibule
Describe the Development of urinary bladder
Development of urinary bladder
embryonic allantois → urachus
connects the apex of the bladder to the umbilicus and has peritoneum raised over it as the median umbilical fold.
forms a thick, fibrous cord, when its lumen is obliterated after birth.
If lumen of urachus persists → urachal fistula → drain urine from umbilicus of newborn
caudal portions of the mesonephric ducts and proximal portions of the ureters (ureteric buds) absorbed into posterior wall of urinary bladder → trigone
w/ time: mesoderm is replaced by endoderm so that the
bladder is completely lined by endodermal epithelium.***Rest of bladder origins from uroginal sinus that has an
endodermic origin***
What is an Ectopic ureteral orifices
How can this happen
Consequences?
Ectopic ureteral orifices:
ureters that open anywhere except into the urinary bladder
results when ureter is not incorporated into the posterior part of the urinary bladder but is carried caudally into the developing prostatic urethra in males and the entire urethra in females
incontinence common because urine does not enter the bladder but continually dribbles from the urethra in both genders and/or from vagina in females
Describe Bladder Exstrophy
Who is it more common in?
Consequence of this?
Bladder exstrophy
ventral body wall defect due to incomplete body folding or a failure of mesodermal migration may expose the bladder to the surface
associated with defect in musculature of anterior abdominal wall.
More Common In Males
associated with a urinary tract (urethra) open dorsally on the penis (epispadias)
In female, the vagina is not fully formed
Consequences:
can’t store urine or function normally → incontinence
Defects in pelvic bones, rectum and anus can also occur
Reconstructive surgery is required