Pharmacokinetics I: Key Concepts and Principles
1/143
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
144 Terms
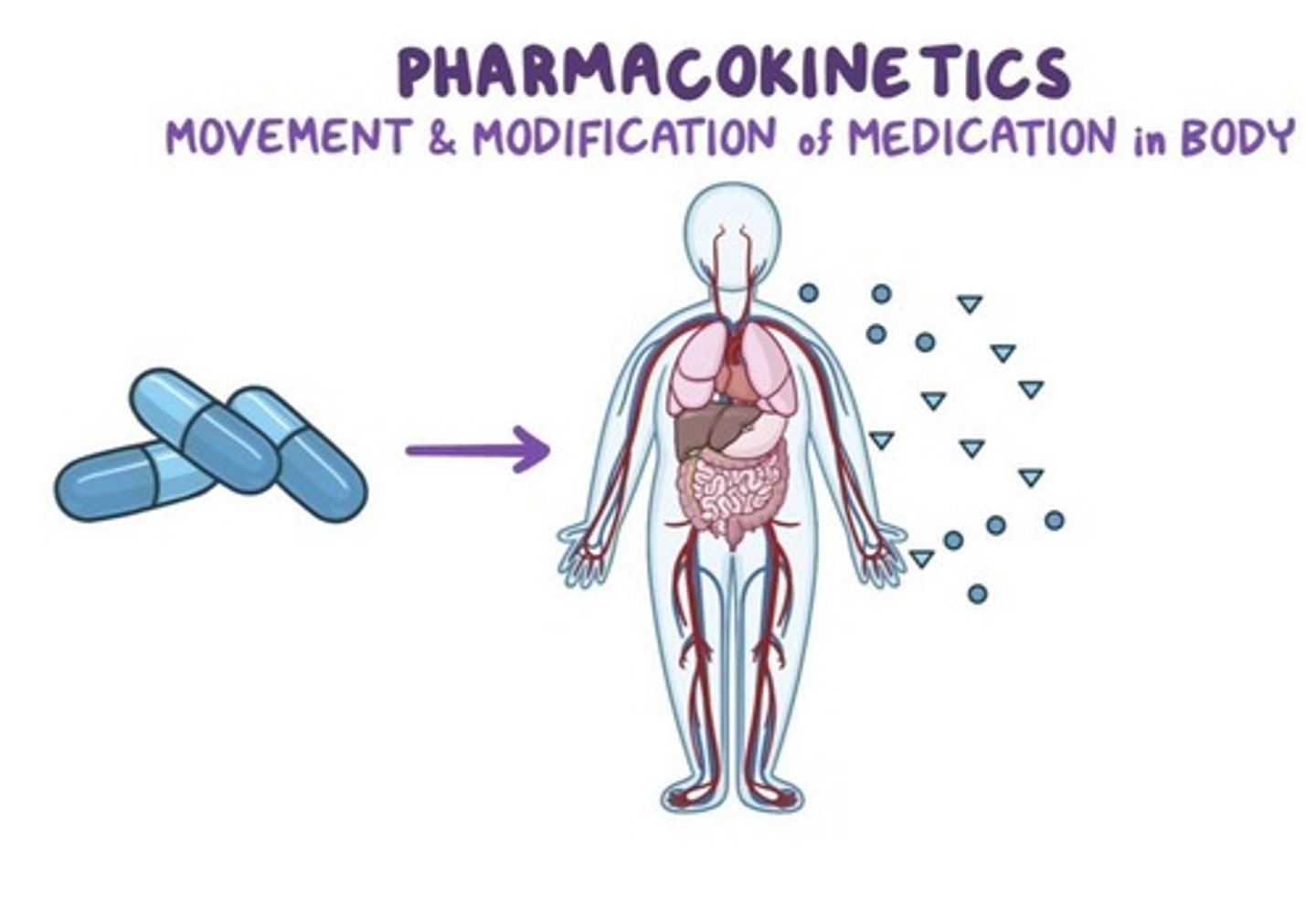
Pharmacokinetics
Movement and modification of medications in the body.
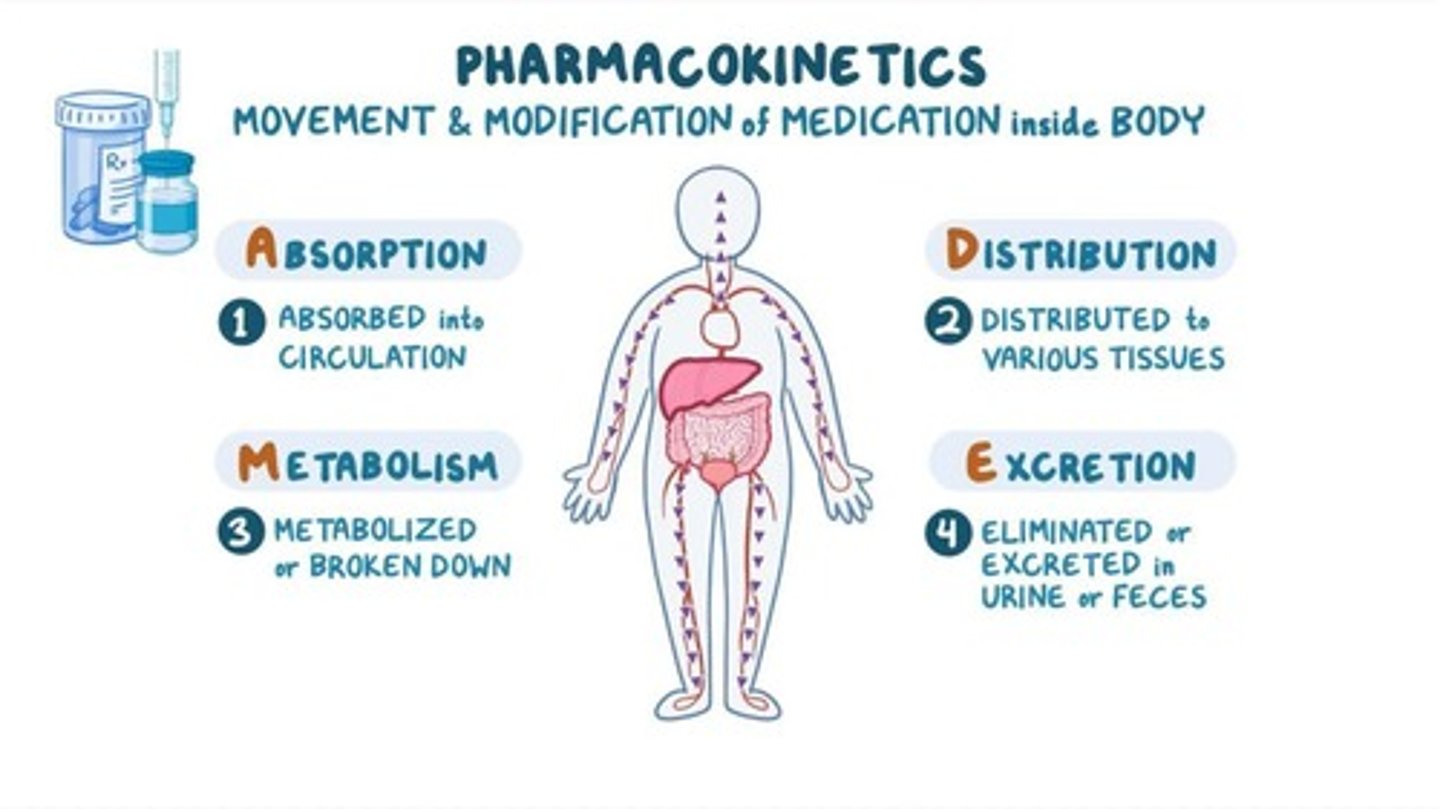
Absorption
Transfer of medication from site of administration into circulation.
Distribution
Process by which drug reversibly leaves bloodstream and enters extracellular fluids and tissues.
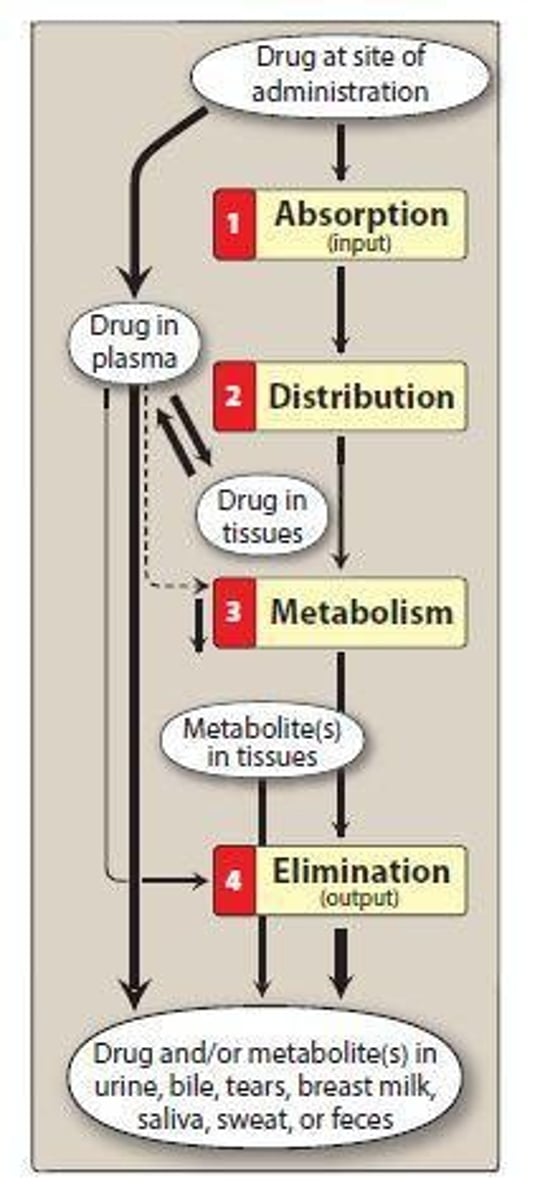
Metabolism
Process by which body chemically modifies drugs to allow drug to be eliminated from body more easily.
Prodrug
Inactive precursor chemical that is absorbed and then converted to active drug.
Bioavailability
The relevance of a drug's absorption in terms of the proportion of the drug that enters circulation when introduced into the body.
Apparent volume of distribution
A pharmacokinetic parameter that describes the distribution of a drug within the body.
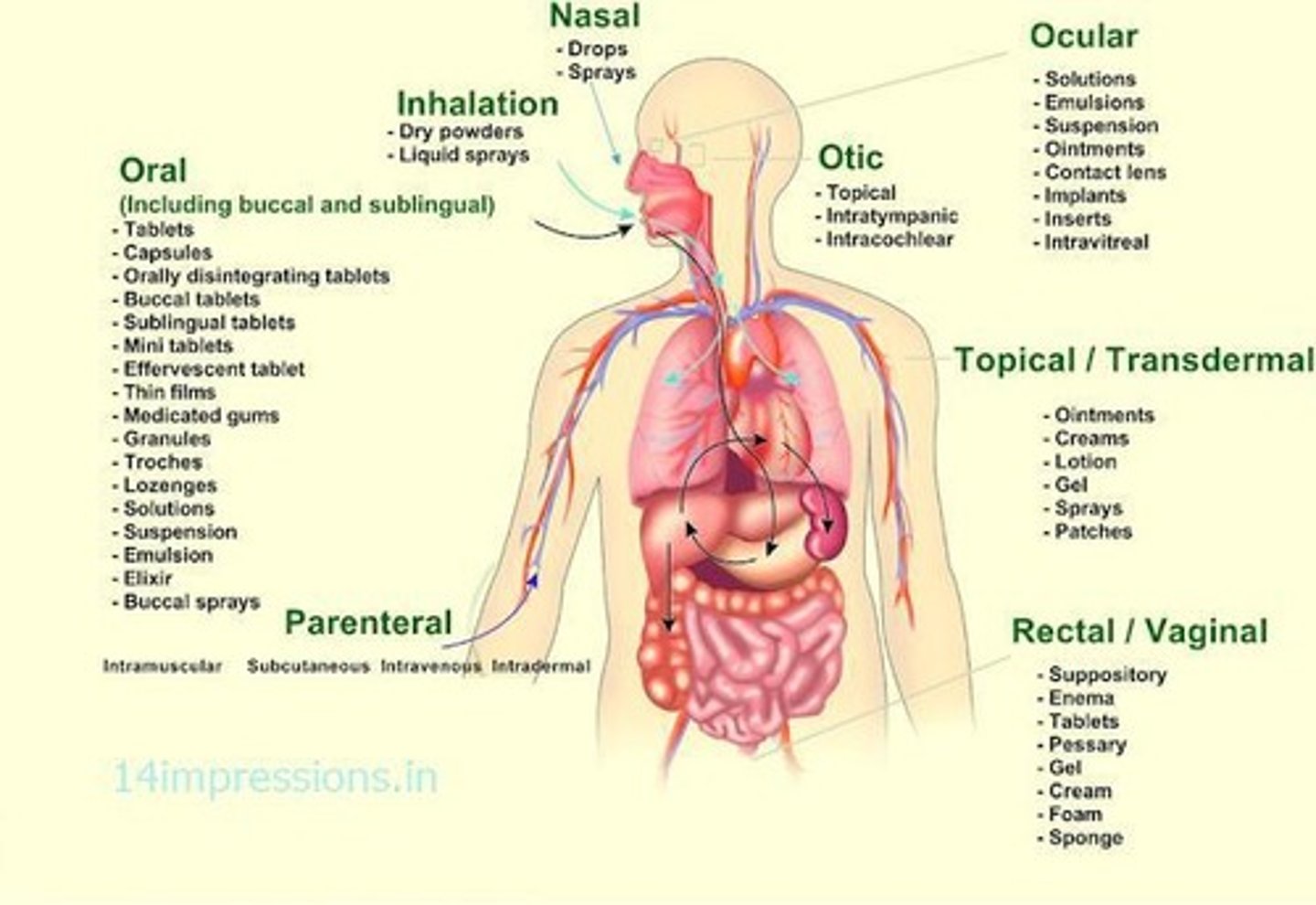
Routes of administration
Different methods by which drugs can be delivered into the body, each with distinct characteristics.
Factors affecting drug absorption
Various elements that influence the rate and extent to which a drug is absorbed into the bloodstream.
Factors affecting drug distribution
Elements that influence how a drug is distributed throughout the body's tissues and fluids.
PK Parameters
Four pharmacokinetic principles: Absorption, Distribution, Metabolism, and Elimination.
Elimination
The process by which drugs are removed from the body.
Drug transformation
The process that occurs from absorption to elimination of the drug.
Site of action
The specific location in the body where a drug exerts its therapeutic effect.
Extracellular fluids
The body fluids outside of cells where drugs can distribute.
Characteristics of each route of administration
Distinctive features and implications of each method used to administer drugs.
Clinical significance of pharmacokinetics
The importance of understanding pharmacokinetics in the context of drug therapy and patient care.
Excretion
Process by which drugs or their metabolites are eliminated from the body.
ADME
Affects different drug factors including Onset, Intensity, and Duration.
Drug Regimens
Used to design appropriate drug regimens.
Route of Administration
The method by which a drug is delivered to the body.
Dose
The amount of drug administered.
Frequency
How often a drug is administered.
Length of Treatment
Duration for which a drug is administered.
Enteral Administration
Administration through the mouth.
Types of Enteral Administration
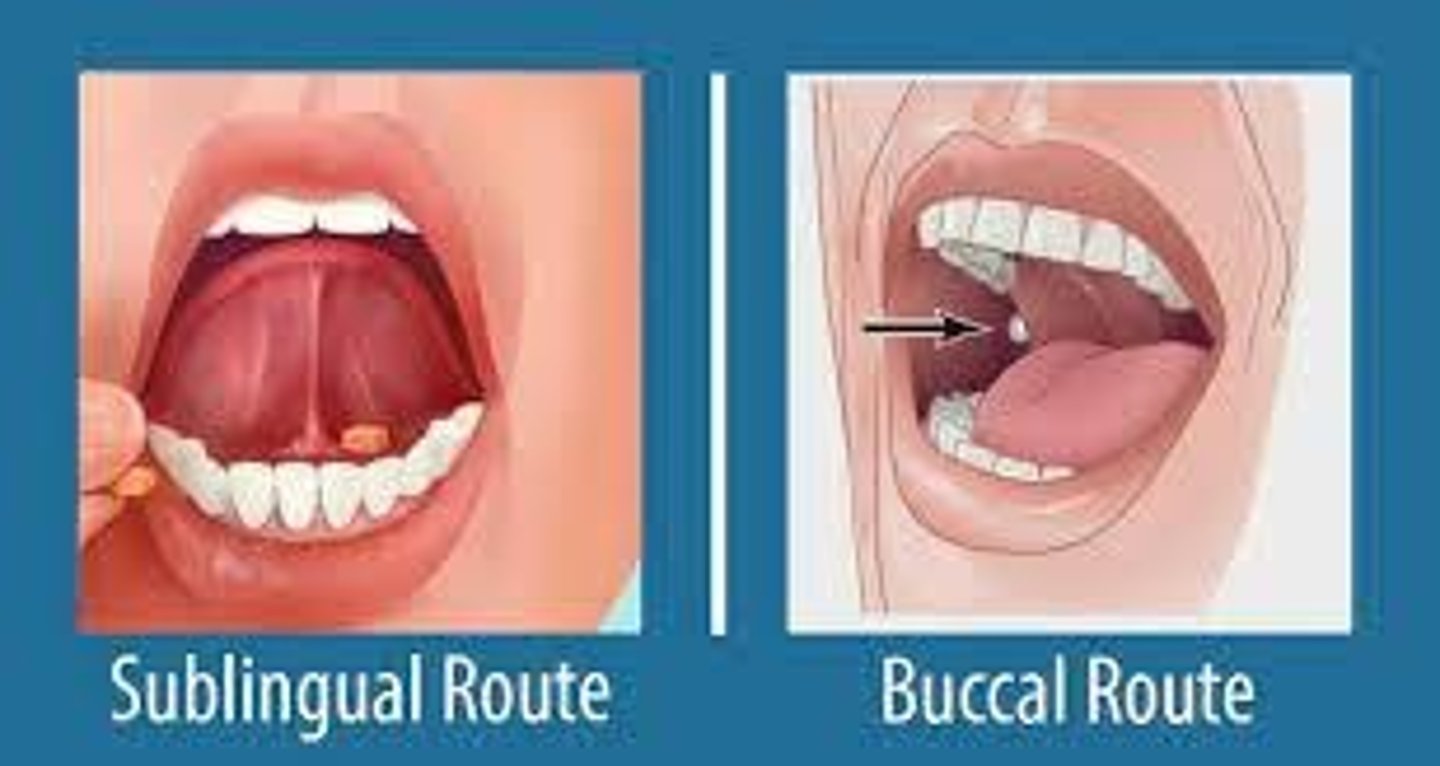
Includes Oral (PO), Sublingual (SL), and Buccal.
Oral (PO)
Convenient, easy administration but has disadvantages including pathways involved with drug absorption.
Sublingual/Buccal
Rapid absorption directly into the bloodstream, bypassing GI and avoiding first pass metabolism.
Parenteral Administration
Drug introduced directly into systemic circulation.
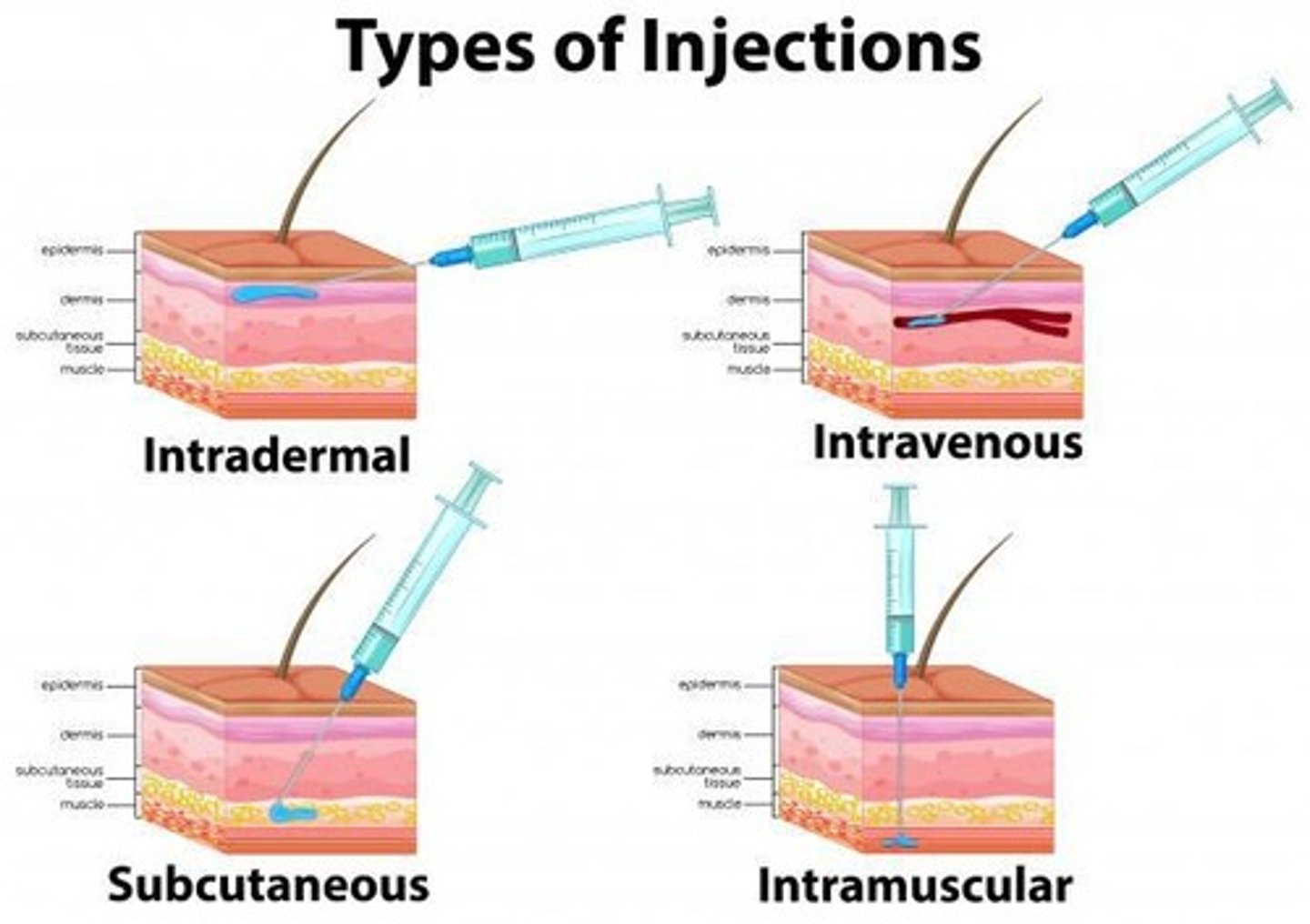
Advantages of Parenteral Administration
Rapid onset of action and dosing control.
Disadvantages of Parenteral Administration
Local tissue damage/infections.
Types of Parenteral Administration
Includes Intramuscular (IM), Subcutaneous (SC), Intravenous (IV), and Intradermal (ID).
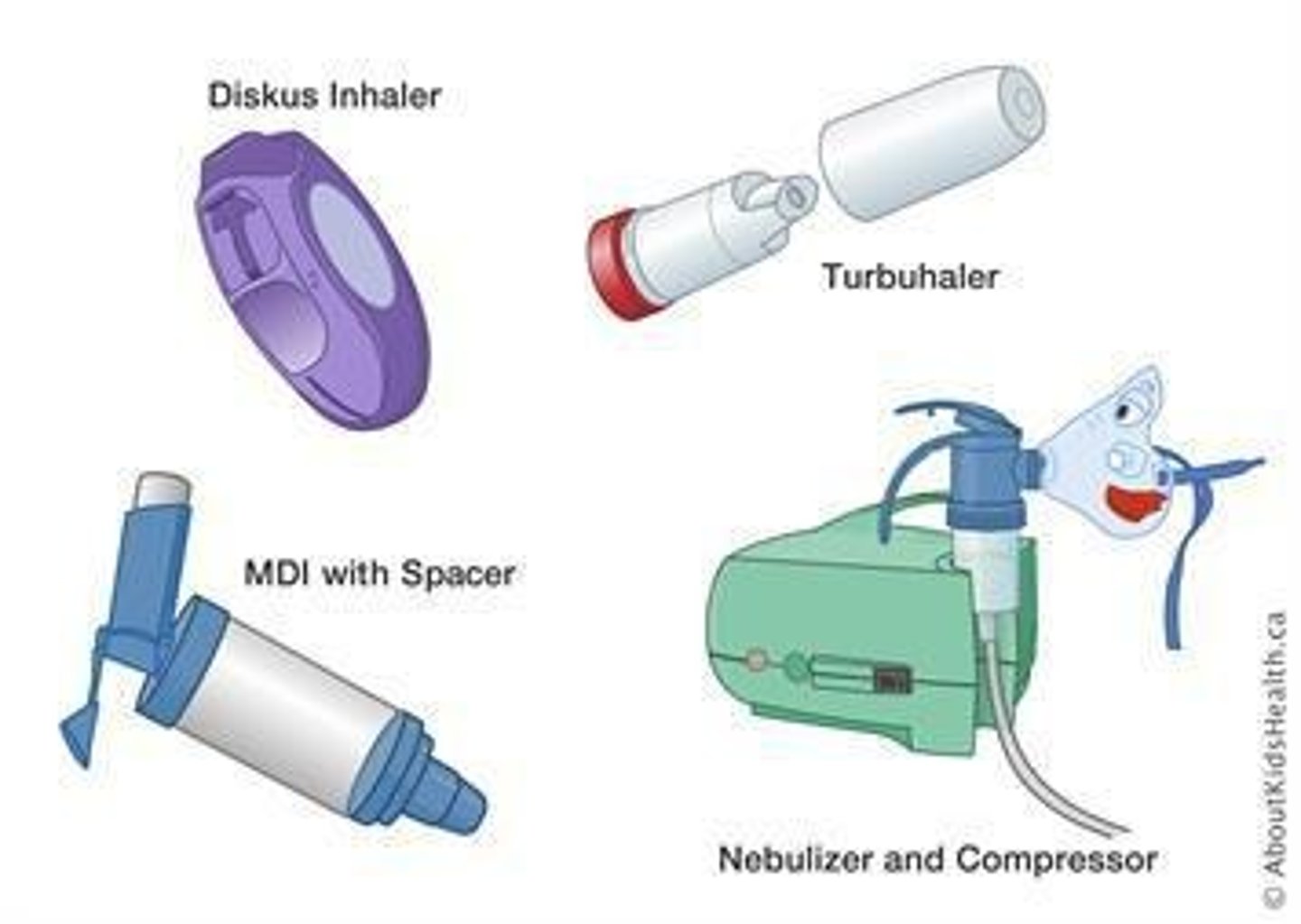
Inhalation/Nasal Preps
Rapid delivery of drug with effects almost as rapid as with IV bolus.
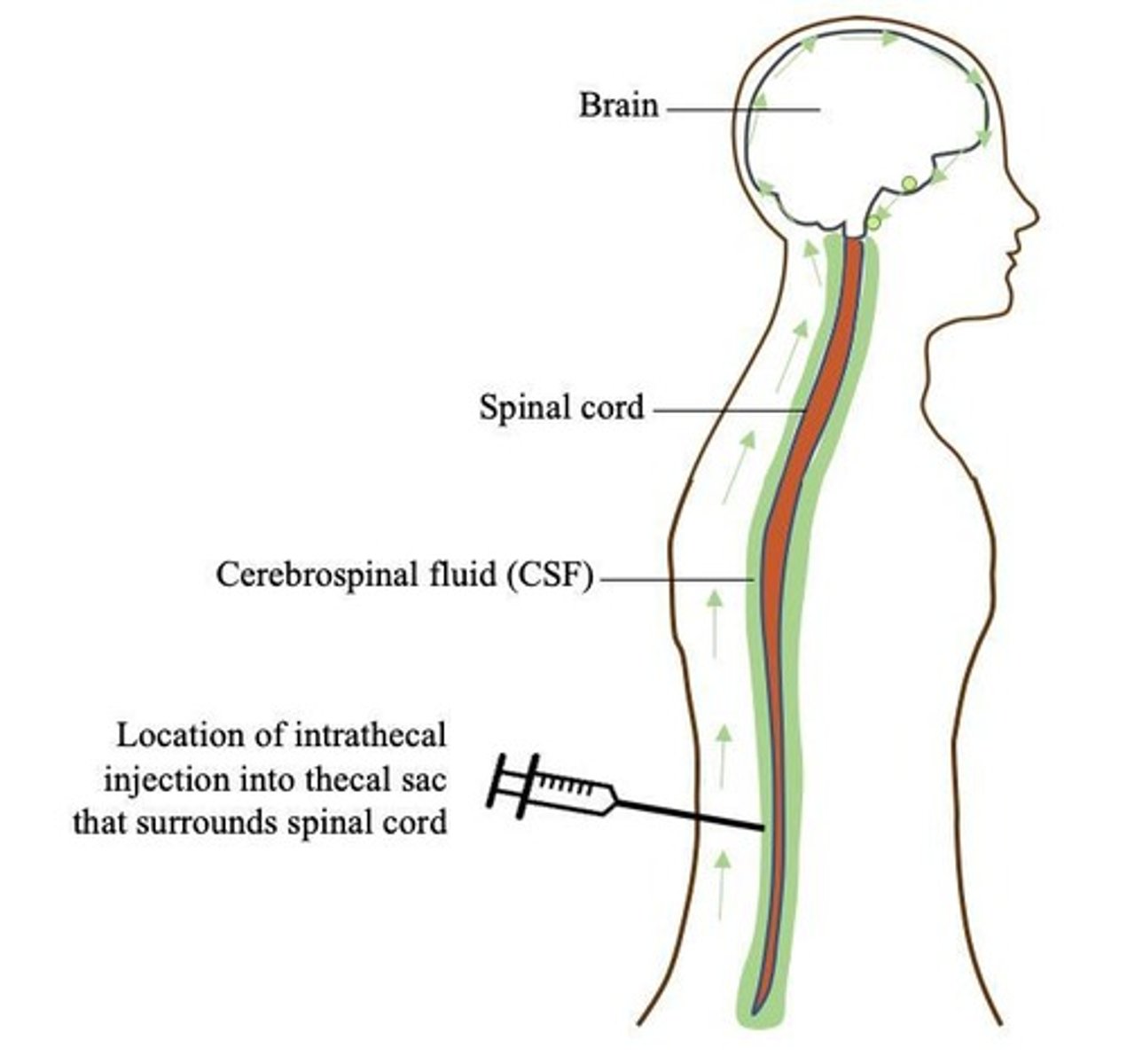
Intrathecal/Intraventricular
Directly into the CSF for local, rapid effects.
Topical Administration
Used for local effect.
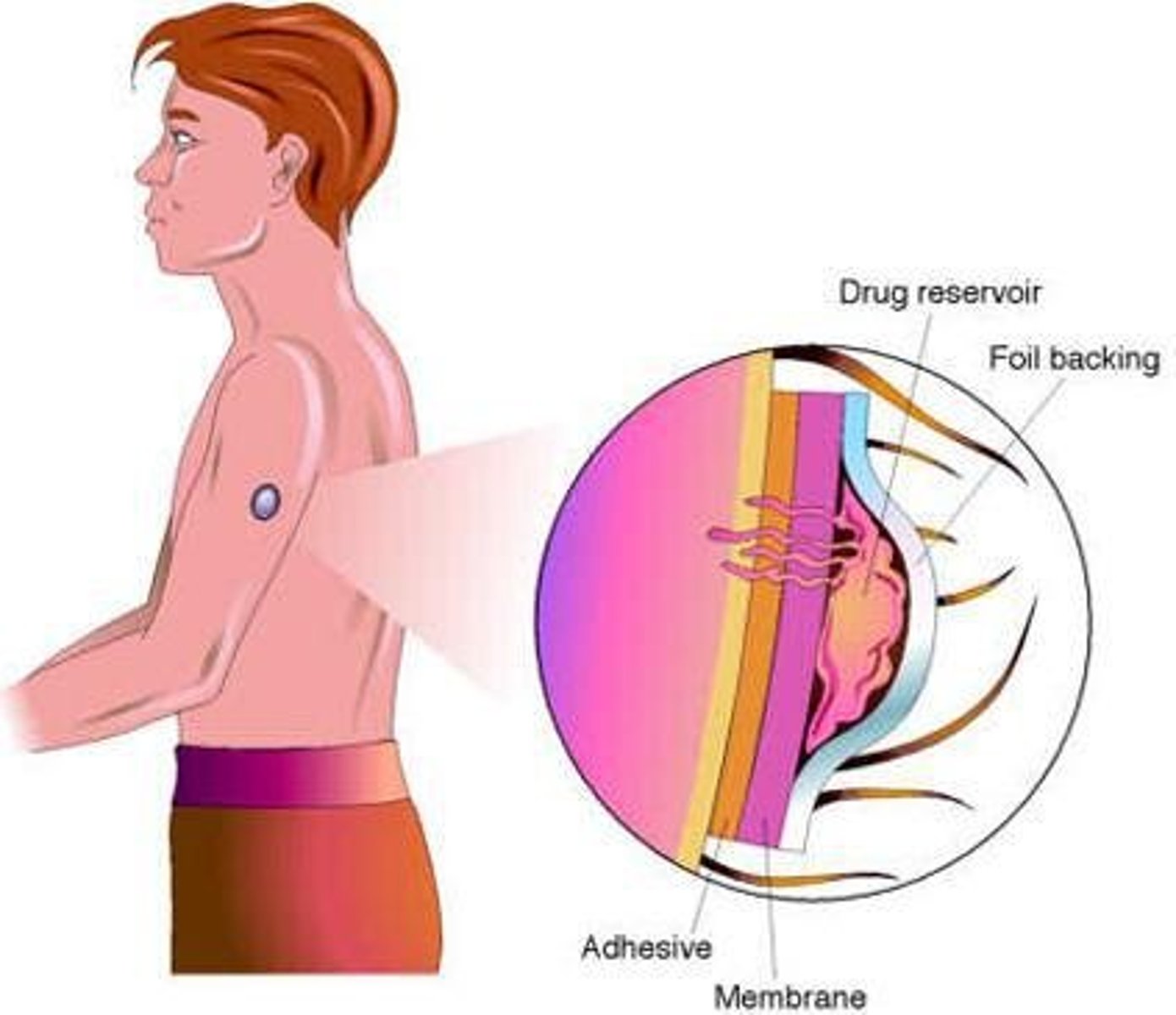
Transdermal Administration
Systemic effects with slower absorption and prolonged duration of action.
Rectal Administration
Bypasses ~50% of portal circulation, minimizing biotransformation of drugs by liver.
Absorption
Transfer of medication from site of administration into bloodstream.
Bioavailability
Percent of medication reaching circulation.
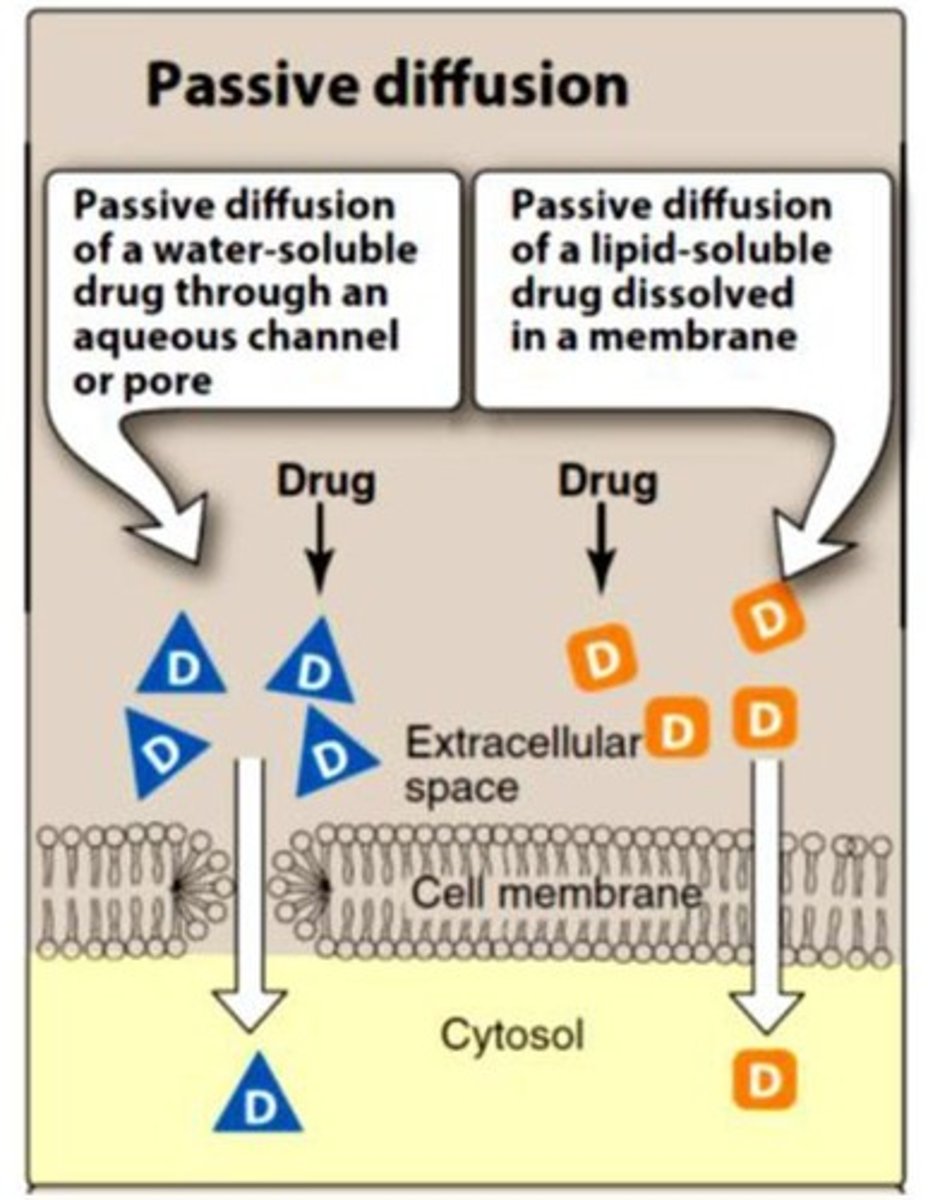
Passive Diffusion
Movement of drugs across membranes without energy, following concentration gradient.
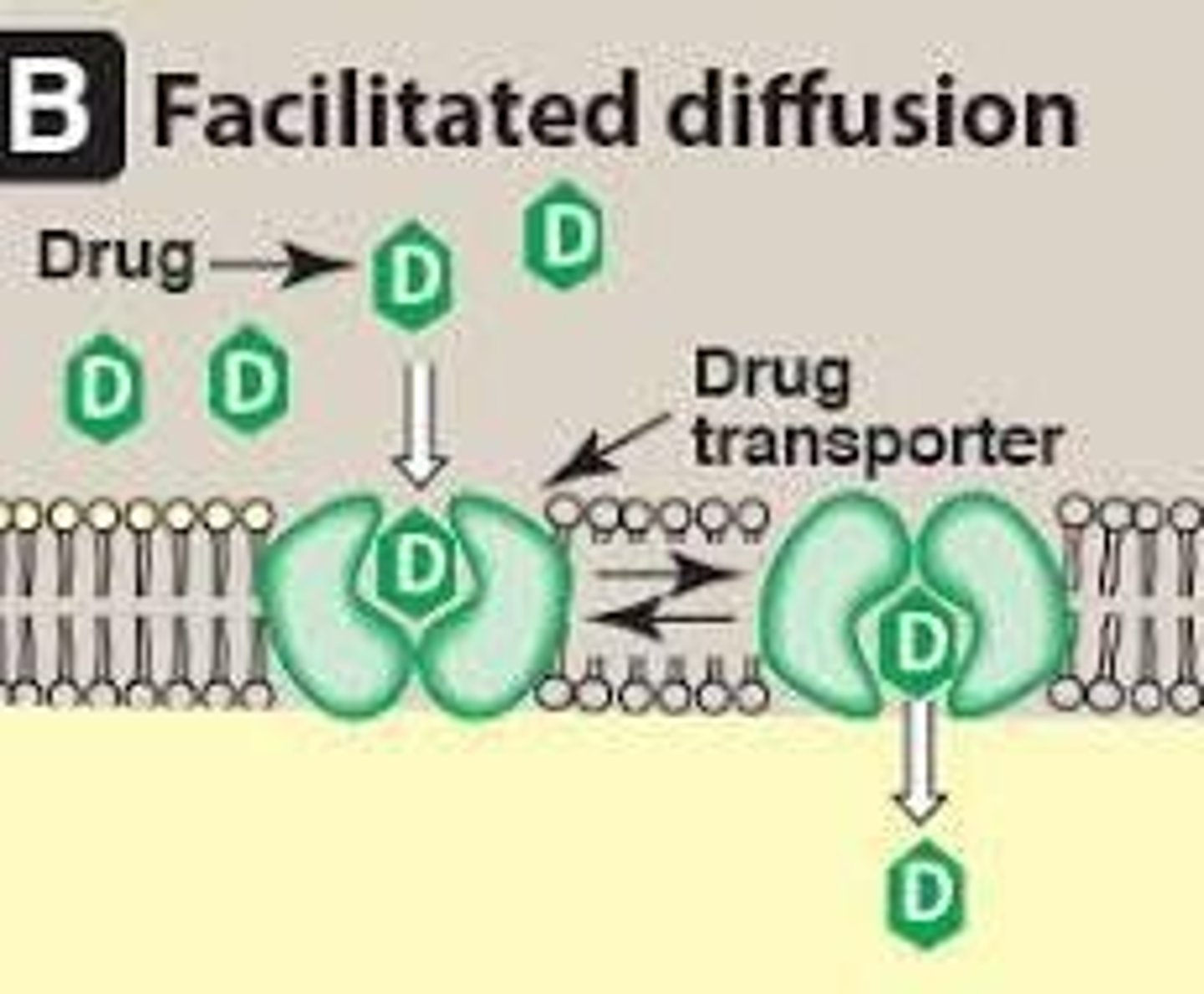
Facilitated Diffusion
Transmembrane carrier proteins undergo conformational changes to transport large molecules without energy.
Active Transport
Energy dependent movement of drugs across a concentration gradient.
Endocytosis
Process of taking large drugs into the cell.
Exocytosis
Process of expelling large drugs out of the cell.
Factors Influencing Absorption
Includes physicochemical properties of drug, pH, blood flow, total surface area, contact time, and expression of P-glycoprotein.
pKa
Measure of strength of interaction between compound and a proton.
Bioavailability Calculation
F = mass of drug delivered to plasma ÷ total mass of drug administered.
Oral Bioavailability
The oral bioavailability (F) of a drug is 50%.
Excretion
Process by which drugs or their metabolites are eliminated from the body
ADME
Affects different drug factors including Onset, Intensity, and Duration
Drug Regimens
Used to design appropriate drug regimens
Route of Administration
The method by which a drug is delivered to the body
Dose
The amount of drug administered
Frequency
How often a drug is administered
Length of Treatment
Duration for which a drug is administered
Enteral Administration
Administration through the mouth
Types of Enteral Administration
Includes Oral (PO), Sublingual (SL), and Buccal
Oral (PO)
Convenient, easy administration; disadvantages include pathways involved with drug absorption
Sublingual/Buccal
Rapid absorption directly into bloodstream, bypasses GI, avoids first pass metabolism
Parenteral Administration
Drug introduced directly into systemic circulation
Advantages of Parenteral Administration
Rapid onset of action and dosing control
Disadvantages of Parenteral Administration
Local tissue damage/infections
Types of Parenteral Administration
Includes Intramuscular (IM), Subcutaneous (SC), Intravenous (IV), and Intradermal (ID)
Inhalation/Nasal Preparations
Rapid delivery of drug; effects almost as rapid as with IV bolus
Intrathecal/Intraventricular
Directly into the CSF for local, rapid effects
Topical Administration
Used for local effect
Transdermal Administration
Systemic effects with slower absorption and prolonged duration of action
Rectal Administration
Bypasses ~50% of portal circulation, minimizing biotransformation of drugs by liver
Absorption
Transfer of medication from site of administration into bloodstream
Bioavailability
Percent of medication reaching circulation
Passive Diffusion
Movement of drugs across membranes without energy, not saturable
Facilitated Diffusion
Involves transmembrane carrier proteins, faster than passive diffusion, does not require energy
Active Transport
Energy dependent movement of drugs across a concentration gradient
Endocytosis
Process of taking large drugs into the cell
Exocytosis
Process of expelling large drugs out of the cell
Factors Influencing Absorption
Includes physicochemical properties of drug, pH, blood flow, total surface area, contact time, and expression of P-glycoprotein
pKa
Measure of strength of interaction between compound and a proton
Bioavailability Calculation
F = mass of drug delivered to plasma ÷ total mass of drug administered
Calculating Bioavailability
If oral bioavailability (F) of a drug is 50% and standard IV dose is 50mg, the appropriate oral dose would be calculated accordingly.
Bioavailability
F= mass of drug delivered to plasma ÷ total mass of drug administered
First-pass metabolism
PO drugs pass through GIT and portal circulation before reaching systemic circulation
Metabolism
Metabolism in liver and gut wall
Solubility of the drug
Very hydrophilic meds poorly absorbed- lipid rich cell membranes
Chemical instability
Instability in stomach pH and GI tract enzymes
Nature of drug formulation
Drug formulation effects dissolution and rate of absorption
Drug Distribution
Process by which drug reversibly leaves bloodstream and enters extracellular fluids and tissues
Distribution factors
Cardiac output and local blood flow, capillary permeability, binding of drugs to plasma proteins and tissues, lipophilicity, volume of distribution
Blood flow
The greater the blood flow to tissues, the greater the distribution
Capillary structure
Determined by capillary structure & chemical nature of drug
Slit junctions
Allow delivery of large protein-bound molecules
Tight junctions
Prevent large, protein-bound and hydrophilic drugs from easily passing through; form barrier
Blood-brain barrier (BBB)
Capillary structure continuous with tight junctions that form a barrier preventing certain drugs from entering the brain
Lipid soluble drugs
Readily penetrate CNS
Ionized or polar drugs
Cannot enter CNS
Plasma proteins
Albumin- major drug binding protein
Tissue proteins
Drugs tend to accumulate in tissues, serving as a source of drug
Apparent Volume of Distribution
Vd= Amount of drug in body ÷ Plasma drug concentration (C)
Theoretical volume of distribution
Based on relationship between total amount of drug administered and measured concentration in plasma
Chloroquine
Apparent volume of distribution = 13,000L/70kg patient
Digoxin
Apparent volume of distribution = 500L/70kg patient