Bio Sci: Anxiety Disorders
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
Generalized Anxiety Disorder Criteria
Experience 3 of the following over past 6 months
Restlessness (on edge), easily fatigued, Difficulty concentrating or mind going blank, Irritability, Muscle Tension, Sleep Disturbances
Must cause significant distress or impairment
Cannot be attributed to other medical disorders, side effects of other substances, or medical conditions
Social Anxiety Disorder Criteria
Marked fear in social situations where person is exposed to possible scrutiny by others.
Fear that they will act in a way that will be humiliating, embarrassing, or rejected by others.
Exposure to feared social situations provokes anxiety or panic attacks; fear is out of proportion to actual threat
Social or performance situations are avoided or endured with intense anxiety or distress, interferes significantly with the person’s normal routine, occupational functioning, relationships, or social activities
Specific Phobia Criteria
The fear must be unreasonable, excessive, have an immediate anxiety response, lead to avoidance/extreme distress, and be life-limiting
4 categories of phobias; Natural (e.g. a fear of thunder or lightning), Mutilation (e.g. a fear of injections), Animal (e.g. fear of dogs), and Situational (e.g. fear of enclosed spaces)
Panic Disorder Criteria
Recurring, unexpected panic attacks, where one attack has been followed for a month by one of the following:
Persistent concern about having additional panic attacks; worry about attack implications or its consequences; a significant change in behavior related to the attacks.
Panic Attack symptoms: Accelerated heart rate, sweating, trembling, shortness of breath, chest pain, nausea, feeling dizzy, feeling detached, numbness, chills, hot flushes, and fear of losing control or dying
Agoraphobia Criteria
All of the following must be present:
Marked fear when confronted with two different situations, e.g. open spaces or crowded areas. (person thinks the space to be unsafe with no easy way of escape)
Immediate anxiety response (panic attack) when exposed to the phobic stimulus.
Recognition of the fear as disproportionate.
Avoidance behaviors, distress, or anticipatory anxiety that significantly disrupts normal routine, relationships, occupational or social activities.
6 months of symptoms across all age groups.
No other underlying condition that may explain the symptoms.
Obsessive Compulsive Disorder (OCD) Criteria
Characterized by presence of either obsessions, compulsions, or both.
Obsessions: Recurrent and persistent thoughts, urges, or impulses that are experienced as intrusive and unwanted. In most individuals causes marked anxiety or distress
Individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize them with another thought or action (i.e., by performing a compulsion).
Compulsions: Repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, counting, repeating words silently). Driven to perform in response to an obsession or according to rules that must be applied rigidly.
Aimed to prevent or reduce anxiety or distress, or prevent some dreaded event or situation; are not connected realistically with what they are designed to neutralize or prevent.
These obsessions or compulsions are time-consuming (take at least more than 1 hour per day) or cause significant distress or impairment in social, occupational, or other important areas of functioning
Post-Traumatic Stress Disorder (PTSD) Criteria
Criterion A:
Exposed to: death or threatened death, actual or threatened serious injury, or threatened sexual violence.
Criterion B: Symptoms associated with the aforementioned traumatic event:
Unexpected or expected reoccurring, involuntary, and intrusive upsetting memories of event. Repeated upsetting dreams related to event. Experience of dissociation (for example, flashbacks) feeling traumatic event happening again.
Strong/persistent distress upon exposure to cues connected to traumatic event.
Strong bodily reactions (for example, increased heart rate) upon exposure to reminder of event.
Criterion C: Frequent avoidance of reminders associated with event by one of following:
Avoidance of thoughts, feelings, or physical sensations.
Avoidance of people, places, conversations, activities, objects, or situations.
Criterion D: At least three of the following symptoms:
Inability to remember an important aspect of the traumatic event. Persistent and elevated negative evaluations about themself, others, or the world. Elevated self-blame or blame of others about cause or consequence of event. Negative emotional state (e.g. shame, anger, or fear) that is pervasive. Loss of interest in activities once enjoyable; feeling detached from others. Inability to feel positive emotions (for example, happiness, love, joy).
Criterion E: At Least three of the following symptoms:
Irritability or aggressive behavior. Impulsive or self-destructive behavior. Feeling constantly "on guard" or hypervigilance. Heightened startle response. Difficulty concentrating. Problems sleeping
Acute Stress Disorder Criteria
Criterion A: Exposure to actual or threatened death, serious injury, or sexual violation.
Criterion B: Presence of at least nine of the following symptoms from following categories:
Intrusion:
Recurrent, involuntary, and intrusive distressing memories/dreams of the traumatic event(s). Dissociative reactions (e.g., flashbacks). Intense or prolonged psychological distress or marked physiological reactions.
Negative Mood:
Persistent inability to experience positive emotions.
Dissociative:
Altered sense of the reality of one's surroundings or oneself (e.g., seeing oneself from another's perspective, being in a daze, time slowing.) Inability to remember an important aspect of the traumatic events(s) (dissociative amnesia; not to other factors such as head injury, alcohol, or drugs).
Avoidance:
Efforts to avoid distressing memories, thoughts, feelings about or closely associated with the traumatic event(s), or reminders (people, places, conversations, activities, objects, situations).
Arousal:
Sleep disturbance. Unprovoked irritable behavior and angry outbursts; typically verbal or physical aggression. Hypervigilance. Problems with concentration. Exaggerated startle response.
Criterion C: Duration of the disturbance (symptoms in Criterion B) is 3 days to 1 month after the trauma exposure.
Think of the difference between ASD and PTSD to be similar to hypomanic vs hypermanic, where ASD is the lesser form of PTSD
Anxiety Second to Drug use or Substance use Criteria
Panic attacks/anxiety during/shortly after the use of a substance
If anxiety symptoms persist after the substance has left the body or after the withdrawal phase, this suggests that another primary mental health condition might be present.
The anxiety symptoms must not be attributable to a medical condition that is independent of substance use (e.g., a brain injury, endocrine condition, etc.).
The symptoms must not occur during a delirium (an acute confusional state, typically seen with intoxication or withdrawal).
Use and Method For Brain Imaging of PET (Positron Emission Tomography)
Measures blood flow or glucose metabolism by using a radioactive substance called a tracer that can be imaged using a scanner to create images of the body’s metabolic activity.
Use: shows activity level in different brain in regions such as: the amygdala, medial frontal cortex and frontal cortical areas. This can show how the brain of someone suffering from PTSD reacts differently when compared to healthy subjects.
Use and Method For Brain Imaging of SPEC (Single-Photon Emission Computed Tomography)
Uses a radio-active substance and a special camera to create 3D pictures
Use: It generates a 3D image of the brain
Use and Method For Brain Imaging of fMRI (Functional Magnetic Resonance Imaging)
Is a neuroimaging technique that measures brain activity by detecting changes in blood flow and measuring blood oxygen level-dependent (BOLD) signal changes.
Use: Can show hyperactivity in the amygdala for those who are suffering from PTSD
Two Ways That Hyperactivity of the Amygdala is Measured in PTSD Patients.
Both an fMRI and a PET scan can show the hyperactivity of the amygdala in PTSD patients.
Describe How Combat Training Influences Regional Brain Activity and Hypothesize What These Findings Suggest is Causing PTSD in Veterans.
Those with PTSD have a more active dorsal anterior cingulate cortex (dACC) during recall of extinguished cure and extinction context. Plus less active ventromedial prefrontal cortex (vmPFC) during this.
Changing levels of activity could be responsible for PTSD in veterans as the vmPFC receives a signal from the PFC to inhibit the fear response from the ACC. This is backed by the evidence that both areas are dysfunctional in those with anxiety disorders.
Describe Tests Used to Diagnose Hyperactive Amygdala For GAD & Social Phobia.
Place the patient under fMRI scan to measure response to aversive odors and neutral human faces.
In healthy individuals, the response will be different. For those with GAD or Social Phobia, the response will be the same bc of their fear response to human faces that a typical person would not experience.
Evaluate What The CCK Experiments Confirmed About the Causality of Panic Attacks.
While the patients were waiting for the next CCK-4 induced panic attack their anterior cingulate cortex was activated. - Key difference between people who have a panic attack and others is not the panic itself that causes a panic disorder, but rather the anticipation of panic.
Hypothesize What Benzodiazepine Binding Studies Tell Us About the Cortical Excitability for Patients With Panic Disorder.
Benzodiazepine activates gamma-aminobutyric acid (GABA), which is the primary inhibitor of glutamate (primary excitatory neurotransmitter).
In those with panic disorders, there is less GABA binding when compared to healthy individuals.
Meaning Benzodiazepine through activating our GABA receptors helps our brain control the levels of glutamate levels that excite our brain and can cause panic disorders.
Describe the relationship between the cingulate cortex and prefrontal cortex in anxiety disorders.
Prevalence loop
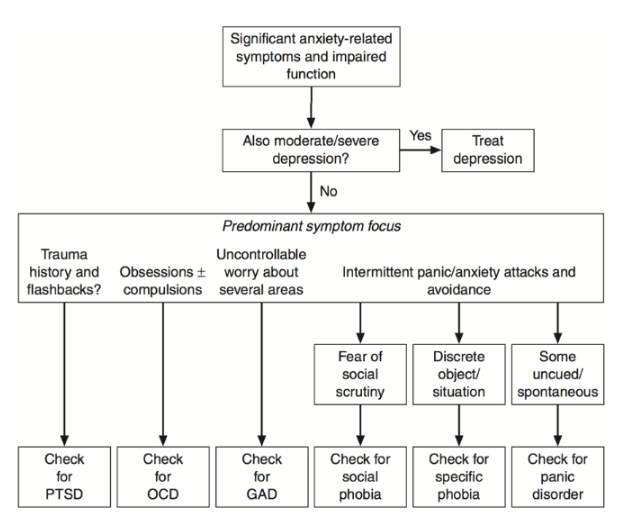
Read a diagnostic flow chart.
Compare and Contrast The Difference Between Benzodiazepines and Barbiturates.
Benzodiazepines
Anxiolytics
Work by activating the GABA neurotransmitter system
Effective in many anxiety disorders
Use should be short-term
Only considered beyond this in treatment-resistant cases because of risks with dependence and side effects
Barbiturates
Can kill you really fast w/ alcohol
Not used as often because of this
Use GABA Receptor Binding Data to Explain The Role of Excitation in Panic Disorder.
Decreased GABA Binding means an increase in prefrontal activity in those with panic disorders
Binding to the GABA receptors allows for chloride ions (CL-) to be released. Which inhibits neuronal firing which leads to a decrease in excitement.
Use GABA Receptor Binding Data to Evaluate The Effectiveness of GABA Agonists As Anxiolytics.
GABA anxiolytics are effective anxiolytics (anti-stressors), because their binding to GABA-A receptors lead to an increase in inhibitory neurotransmissions and reduced neuronal excitability. In effect, it leads to lesser anxiety symptoms
Fewer receptors, you’d give them something that activates those receptors (i.e. Benzodiazepines)
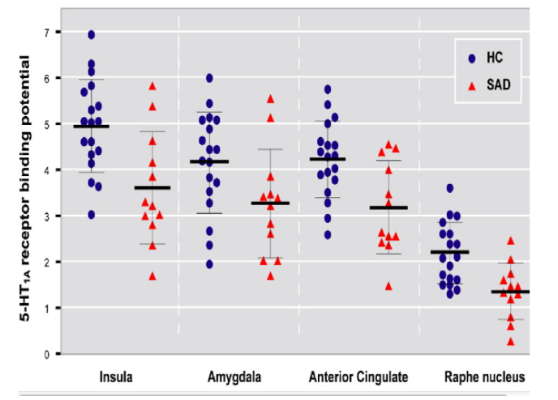
Use Charts of 5-HT1A Receptor Binding To Evaluate The Role of Serotonin in Anxiety as well as Potential For Serotonergic Treatments.
5-HT1A, a specific serotonin receptor, shows that more serotonin through additional binding can reduce levels of anxiety
Why we prescribe SSRIs to those suffering from anxiety disorders to reduce anxiety levels
First and Second Line Treatments of Social Anxiety Disorder
First Line: SSRIs, SNRIs & CBT (Cognitive Behavioral Therapy)
Second Line: Beta-Blockers and Benzodiazepines
First and Second Line Treatments of Panic Attacks
First Line: SSRIs, SNRIs
Second Line: Benzodiazepines (also known as Anti-Anxiety medication)
First and Second Line Treatments of Panic & Agoraphobia
First Line: SSRIs, SNRIs & CBT
Second Line: Benzodiazepines
First and Second Line Treatments of OCD
First Line: SSRIs & CBT
Second Line: Antipsychotics
First and Second Line Treatments of PTSD
First Line: SSRIs, SNRIs & CBT
Second Line: Antipsychotics
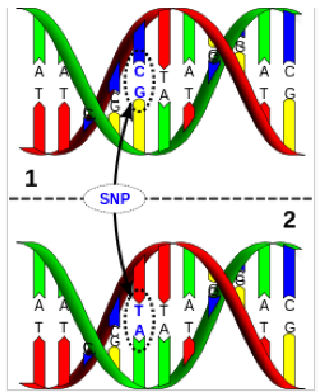
Define SNPs and How They Relate To Mood Disorders.
SNPs are Single Nucleotide Polymorphisms
Refers to variation in a single base pair in DNA sequencing and occurs on a single nucleotide (the A, T, C, and Gs that make up our genetic sequence)
They relate to mood disorders as there is a trend of specific SNPs and Mood Disorders
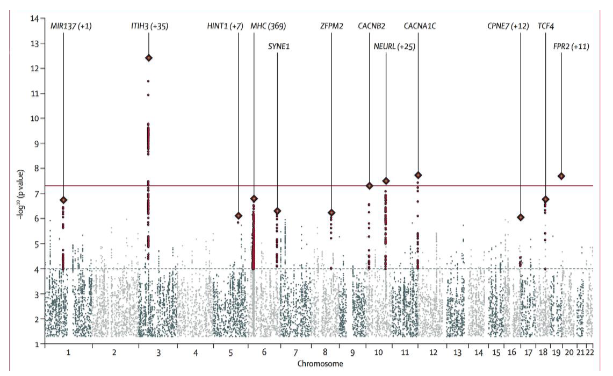
Use Figures Showing –log of pValues To Determine Significance of SNPs
Chart shows that specific SNPs (ITIH3, AS3MT, CACNA1C & CACNB2) are more prevalent in those with specific mood disorders
Why Does it Make Sense that Mood Disorders Would Have Genetic Overlap?
Makes sense since genetic overlap could be responsible for the difference we see in those with mood disorders (i.e. the decreased GABA binding present in those with Anxiety Disorders)
Describe The Types of Proteins Made By Genes That Have Mutations in Mood Disorders.
Proteins that affect Neurotransmitter signaling, especially glutamate
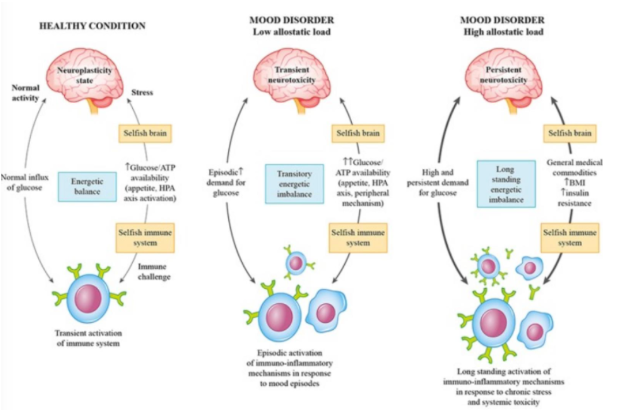
Explain How Allostatic Load Drives Mood Disorders, Considering the Theory of the Selfish Brain and Immune System.
Selfish brain theory: above all else, the brain will prioritize itself and its needs over the rest of our body. Can lead to immune dysregulation and inflammation
Allostatic load is our wear and tear caused by stress and a dysregulated stress response
Combining the two means only our brain is receiving the proper amount of nutrients and will place a large demand on glucose.
Glucose is needed to regulate our mood but cannot be as it is being siphoned away by the brain
Why would glutamate receptors be a good candidate for treatment?
They would help replenish the lack of glucose supply our body needs to properly regulate our mood and prevent us from getting mood disorders.