9) Photon beams and dose
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
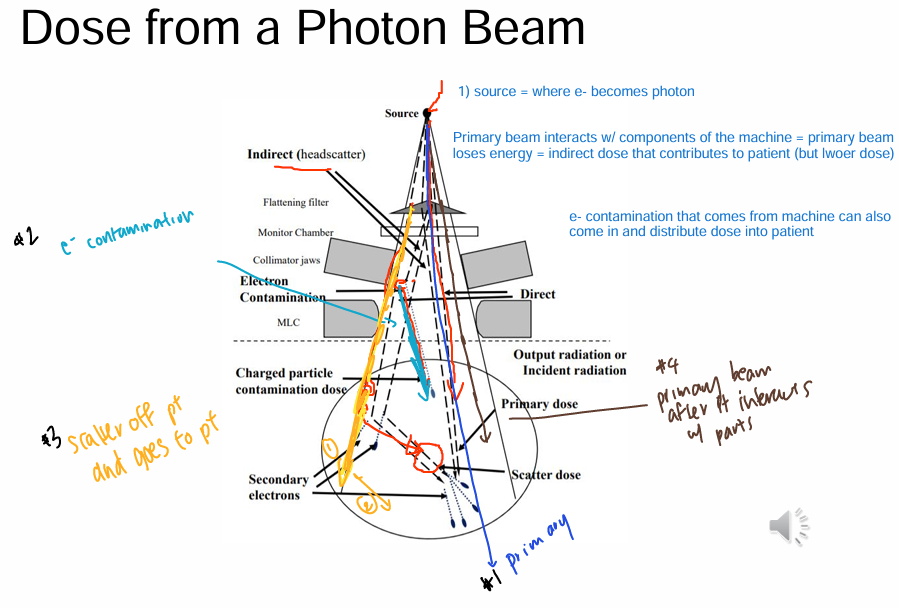
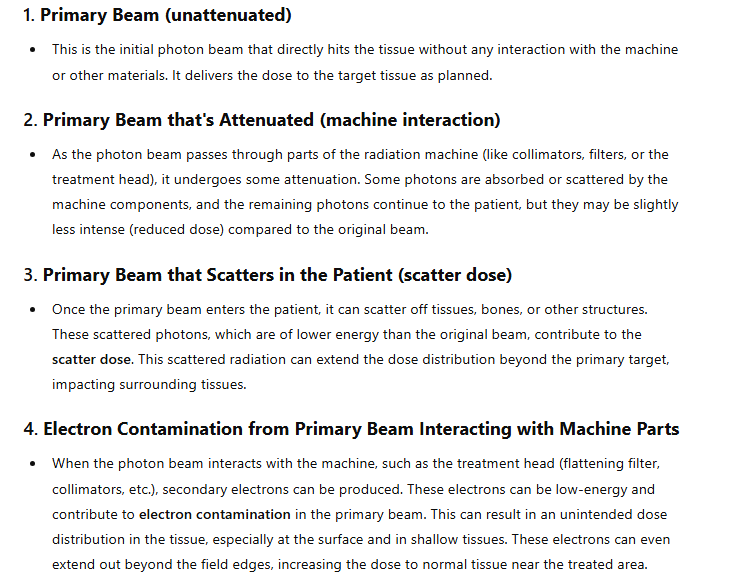
What are the components of a photon beam?
1) Primary beam
2) Head scatter
- primary beam interacts with machine components
4) Contamination
- primary beam interacting w/ machine components also has e- interactions (Ithink)
→ e- then become absorbed by the person
→ actual = e- contamination that comes from machine → can distribute dose into patient
3) Phantom scatter
- primary beam interacts w/ tissue/phantom
→ creates SCATTER photon
→ can either be direct towards wall
OR
→ be directed back towards person (becomes absorbed)
*Note
1) e- leave a trail of dose → therefore dose passing through area is PROPORTIONAL to # of e- passing through
2) # of photons DECREASE w/ depth
- therefore fewer e- (contamination) & scattered photons as depth increases (quite intuitive)
- aka: if there is no photon beam, then you wouldn’t get the e- contamination/scattering
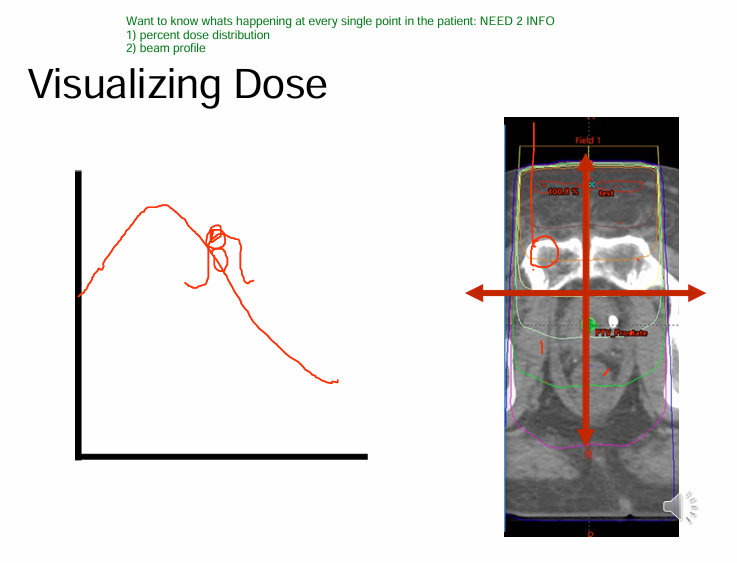
What are ways we can visualize dose?
1) Percent dose distribution
2) Beam profile
3) Isodose lines
4) Color wash
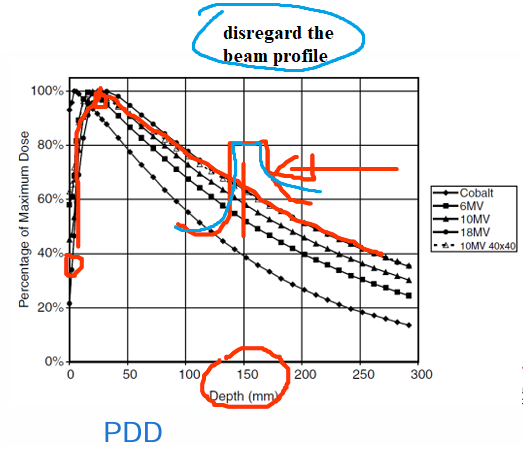
What is PDD?
Percent dose distribution = dose as a function of depth
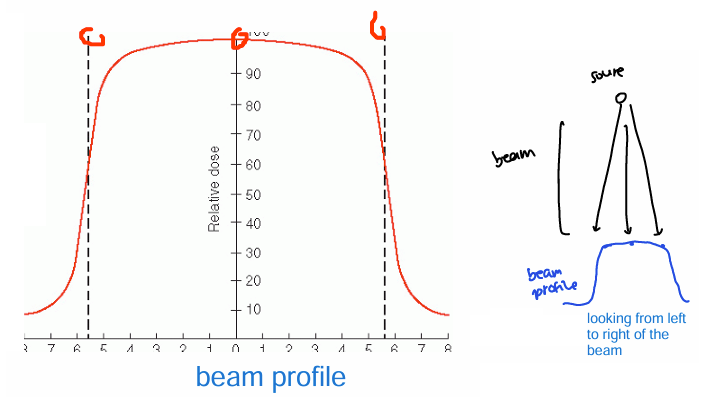
What is beam profile?
dose as a function of
distance from the central axis
(looking at the beam from left to right)
What is the isodose line?
PDD + beam profile
= how a photon beam will deposit dose into tissue
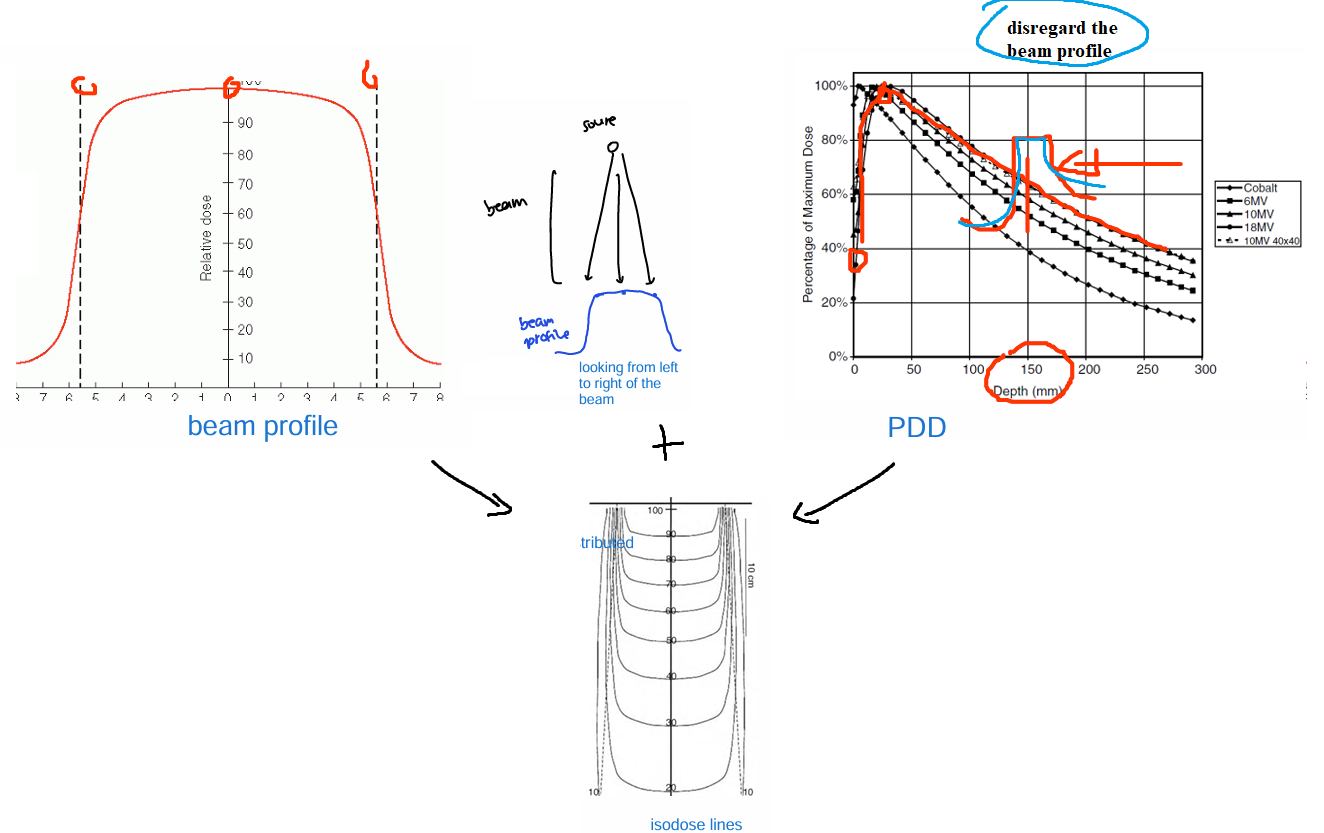
What is a color wash?
where the hot/cold spots are
-indicated where the dose is being distributed
*Note: Kerma does NOT accurately track where the energy ends up
Makes sense, not all energy transferred is absorbed right at that moment. Energy transferred can be absorbed later on (remember the kerma dose graph from MT1)
Kerma = only initial energy transfer
Visualizing dose is __
ONE DIMENSIONAL (except isodose lines = 2d)
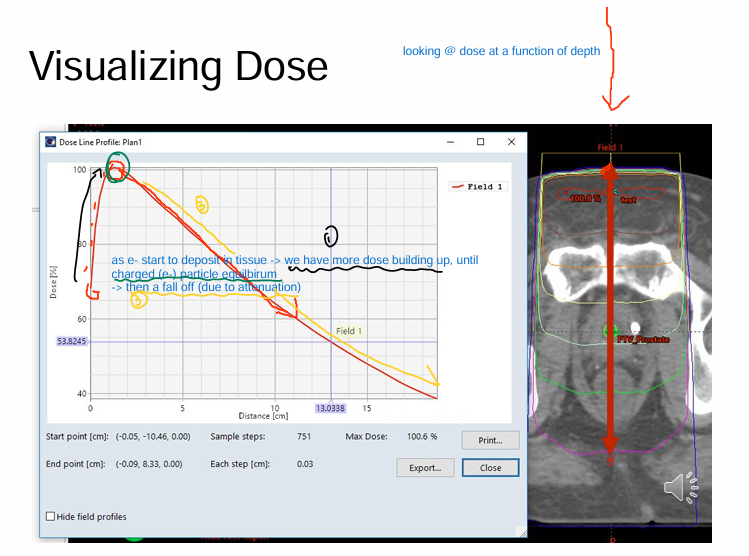
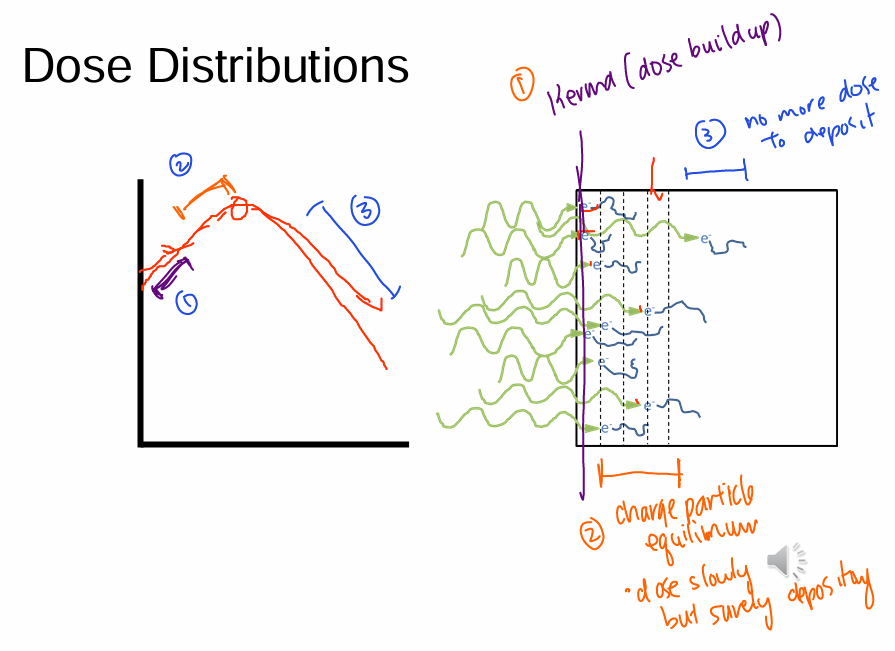
(see image) (visualizing dose)
Percentage dose distribution
Looking @ dose as a function of depth
1) Photon beam from source
2) Transfer energy into tissue
3) e- bumped out etc
4) dose continues to build up until charge particle equilibrium (e- in = e- out)
5) dose falls off due to attenuation
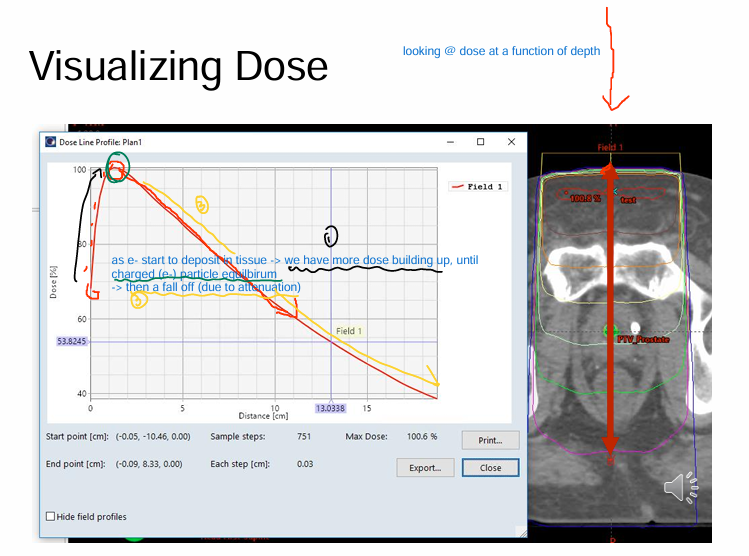
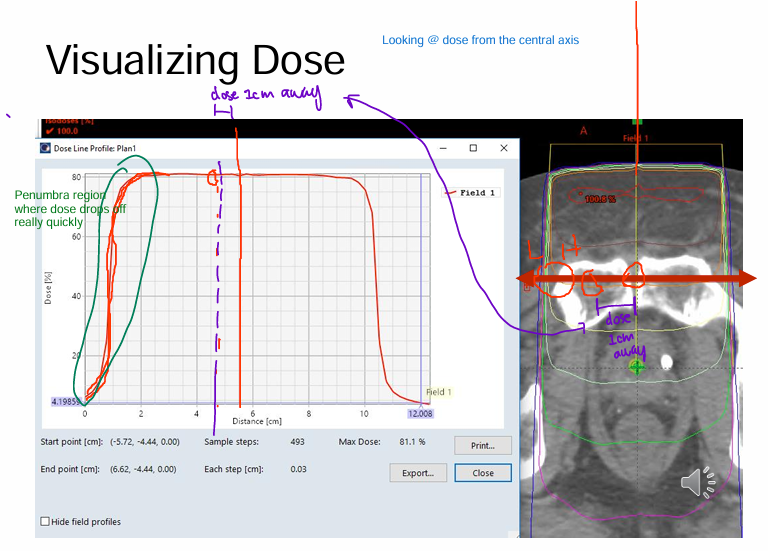
(see image) (visualizing dose)
Beam profile
*Note: Penumbra regions at the very end = where dose drops off rapidly
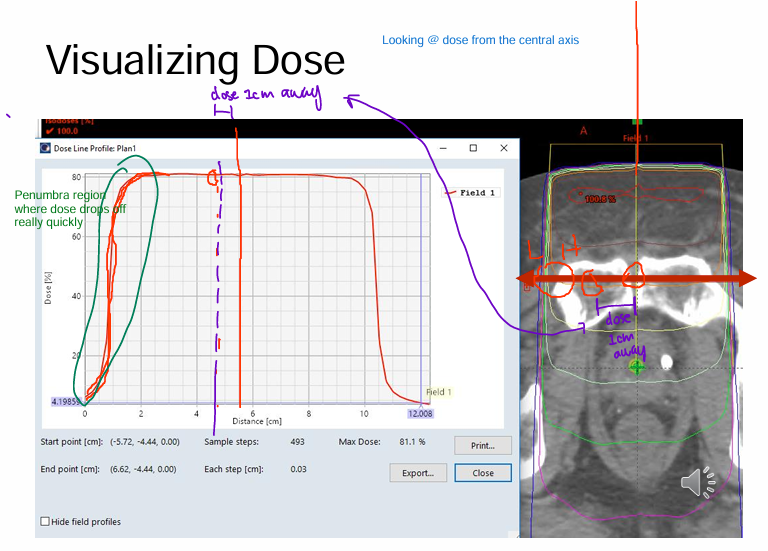
(visualizing dose)
If we we want to know what’s happening at EVERY POINT in the patient what information do we need?
1) Percent dose distribution
2) beam profile
which combine to form isodose lines
What is the POINT of dosimetry?
accurately predict dose distributions of radiation beams
*Note: Understanding dose
- there are many factors that impact dose
- these factors may be small individually and you may think its INSIGNIFICATION
- but when you consider them all TOGETHER (the shits add up)
factors to consider:
beam energy
field size
distance
(depth)
What is a phantom?
Material w/ tissue like properties
What criteria should a phantom meet?
1) absorb/scatter photons in the same way as tissue
2) same density as tissue
3) same e- density as tissue
*note: principle mode of interaction b/w photon and e- is compton scattering
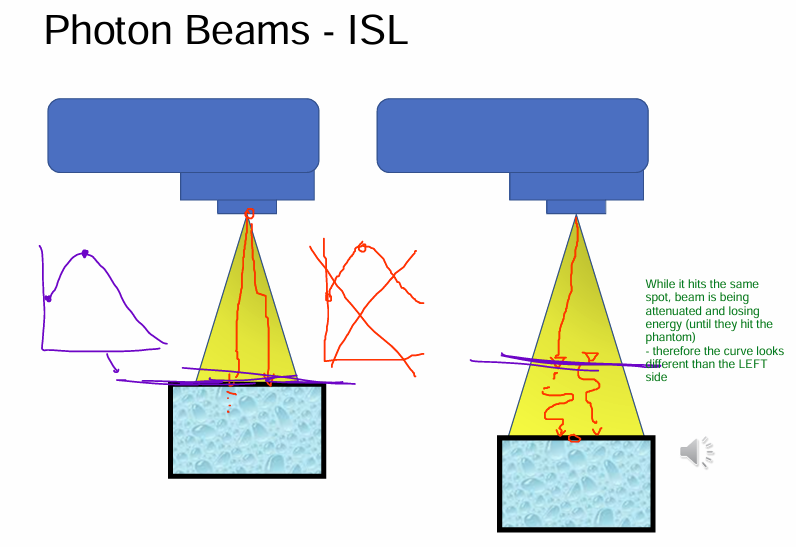
What effects make the DOSE DEPOSITION in a phantom/patient complicated?
1) Inverse square law
- further you are, less dose (intensity decreases)
2) Attenuation of photon beam inside the patient/phantom
- aka as beam penetrates further and further through the material
3) Scattering of photon beam inside the phantom/patient
- field size affects scatter @ head & scatter @ patient
(1of3)
How does INVERSE SQUARE law affect photon beams?
Longer distance = less intensity from beam
(intuitive)
(beam is being attenuated by “air” and losing energy until they hit the spot we are measuring)
(2of3)
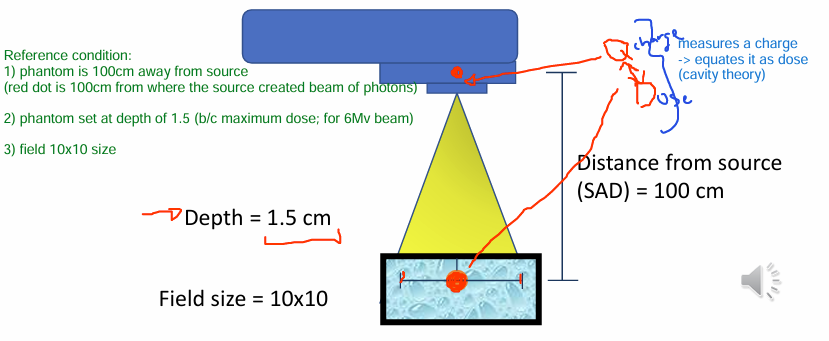
How does SCATTER affect photon beams?
Increasing FIELD SIZE
- ex. 10×10 field size to 25×25cm field size
1) Primary beam just goes to target (phantom/patient scatter)
- 1.5) primary beam could also scatter off patient and that scatter can deposit dose
2) Primary beam gets attenuated a lil (head scatter)
→ 2ndary collimators open up more
→ primary beam photon from source interacts w/ 2ndary collimators more
→ 2ndary collimators attenuate beam more and more b/c of large SA from opening up field size
→ this beam that hits pt will have less energy (makes sense, it got attenuated)
3) e- can also be produced (contamination) from beam getting attenuated by collimator (2ndary e- production)
→ which can give dose to the patient
4) primary beam - nothing touches it
(3of3)
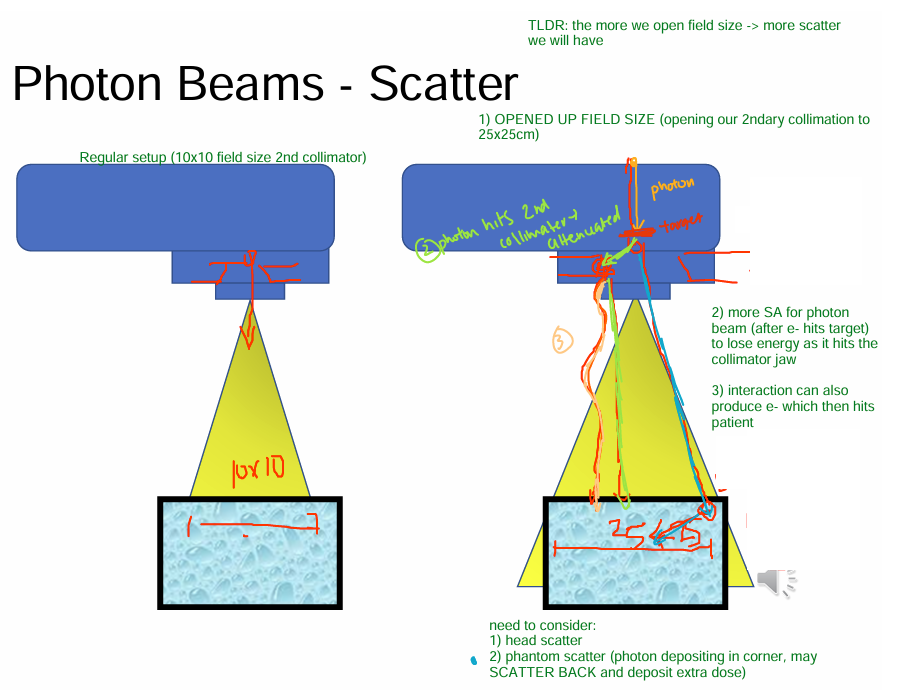
How does IATTENUATION affect photon beams?
Thicker the material, the more the beam gets attenuated (intuitive)
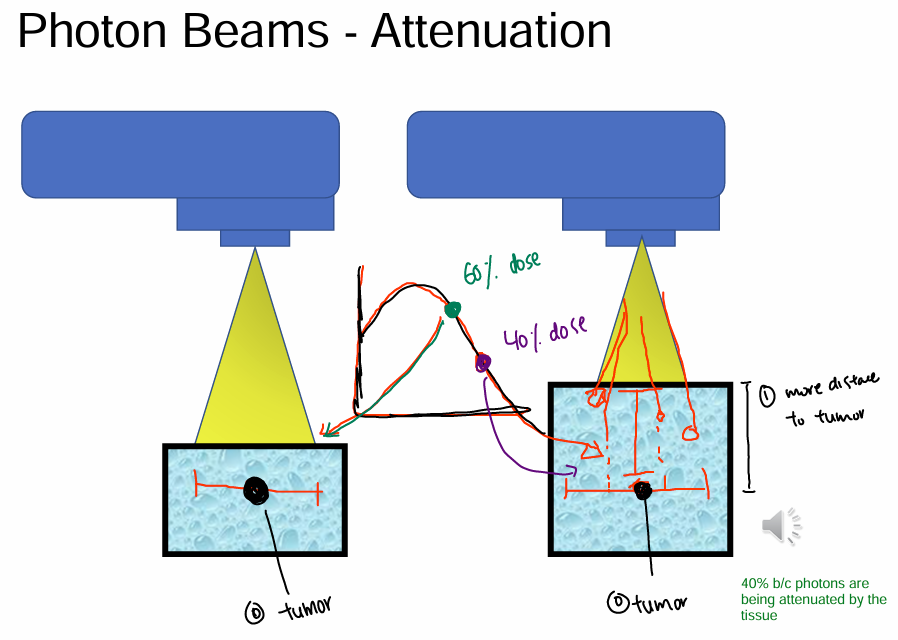
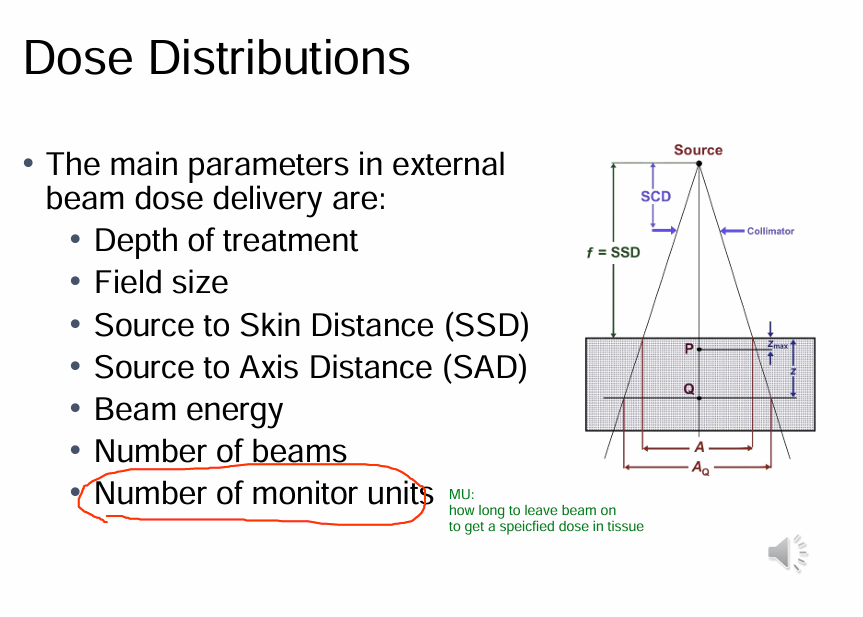
For radiation treatment to be successful, we need to accurately & precisely know the dose distribution in the target & surrounding tissues.
How is this done?
Radiation detectors in tissue w/ tissue equivalent phantoms
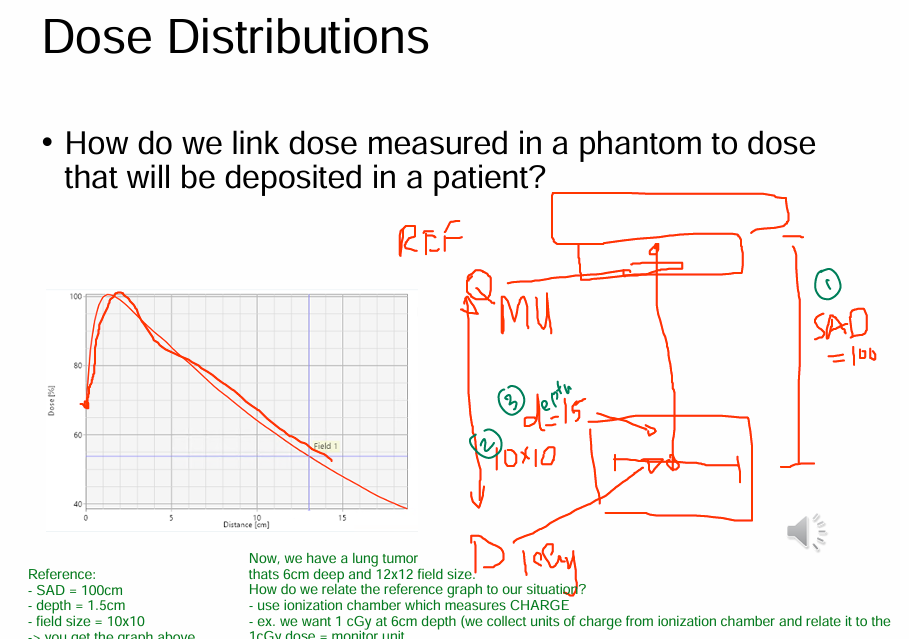
Where dose is determined at REFERENCE CONDITIONS:
1) SAD = 100cm (distance from source)
2) Depth = 1.5cm
3) Field size = 10×10
Dose distribution image
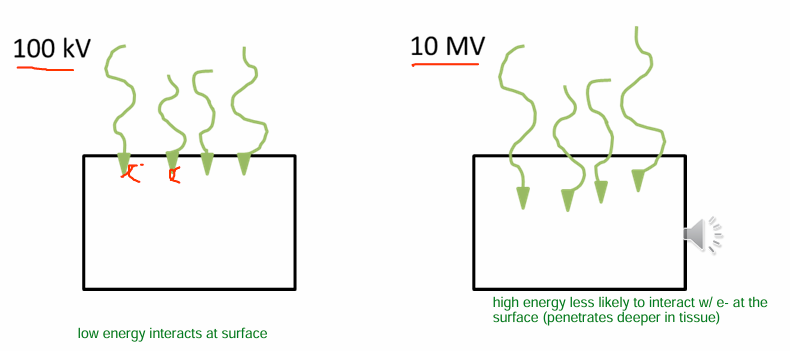
For megavoltage x ray beams (high energy), the ___ is generally much __ than the maximum dose.
This is known as what EFFECT?
1) surface dose is LOWER than maximum dose
(makes sense, higher energy = can penetrate through material easily compared to a low energy; aka high energy won’t easily be deposited on surface)
2) skin sparing effect
What can contribute to surface dose?
1) Photons scattered from head of machine
2) photons backscattered from patient (aka photon scatters from patient → and then deposits dose in that patient)
3) high energy e- produced by photon interactions in air
The region b/w the surface and dmax is called the __
build up region
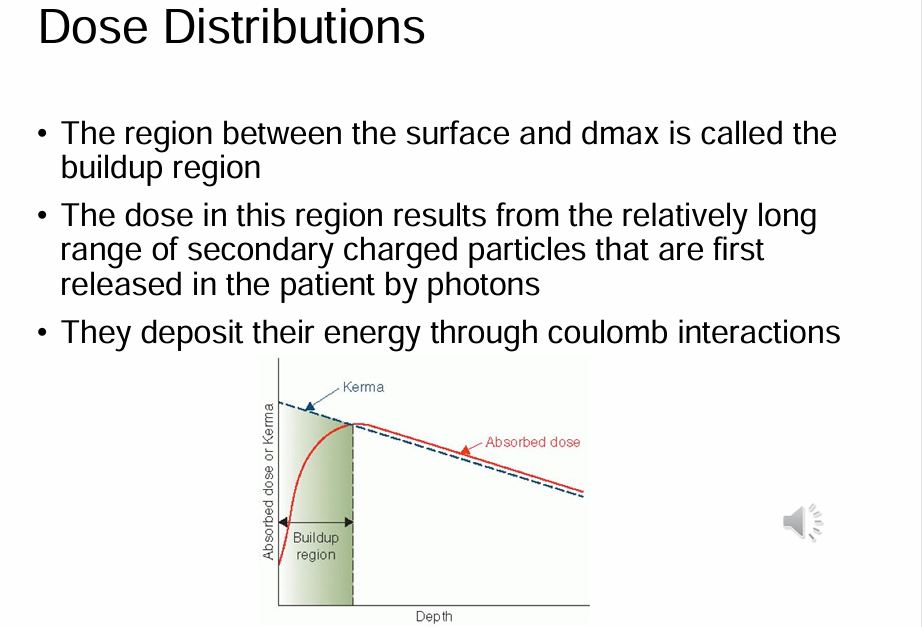
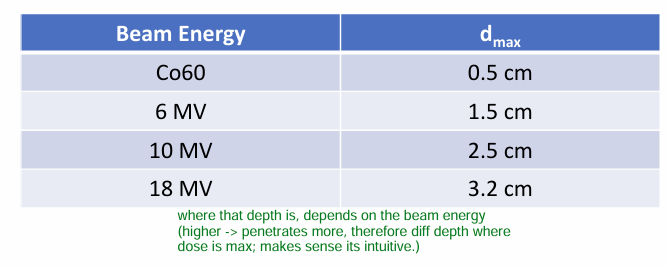
What does the DEPTH of dmax depend on?
1) Beam energy (primary effect)
- makes sense; higher energy = can penetrate deeper → less is lost at the surface, and most energy reaches/goes to the depth intended
2) Field size (secondary effect)
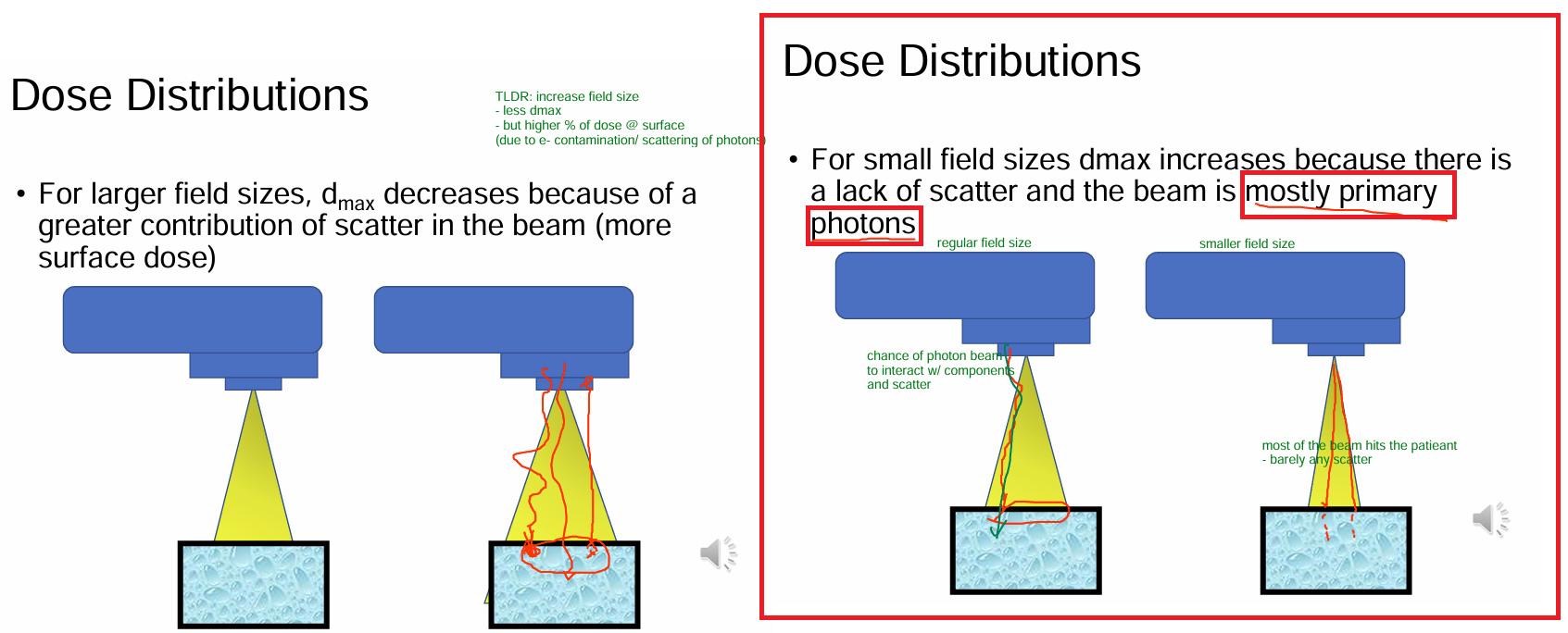
Why does dmax change when we open/close the field size (SEE IMAGGEe)
Open field size = more SA of 2ndary collimators
→ more scatter interactions
→ beam is attenuated
→ once beam hits the surface (its less dose compared to our beam w/ smaller field size)
→ doesn’t penetrate as deeply = LESS dmax
*In addition, the e- produced from contamination also deposit dose at the surface, increasing surface dose
TLDR: less dmax, more dose @ surface
What is the purpose of MONITOR UNITS?
how long to LEAVE THE BEAM ON to get a specified dose in tissue
How do we link dose measured in a phantom
to dose that is deposited in the patient?
Aka adjust machine output via
Monitor units (MU)
- aka how long we will leave the beam on for
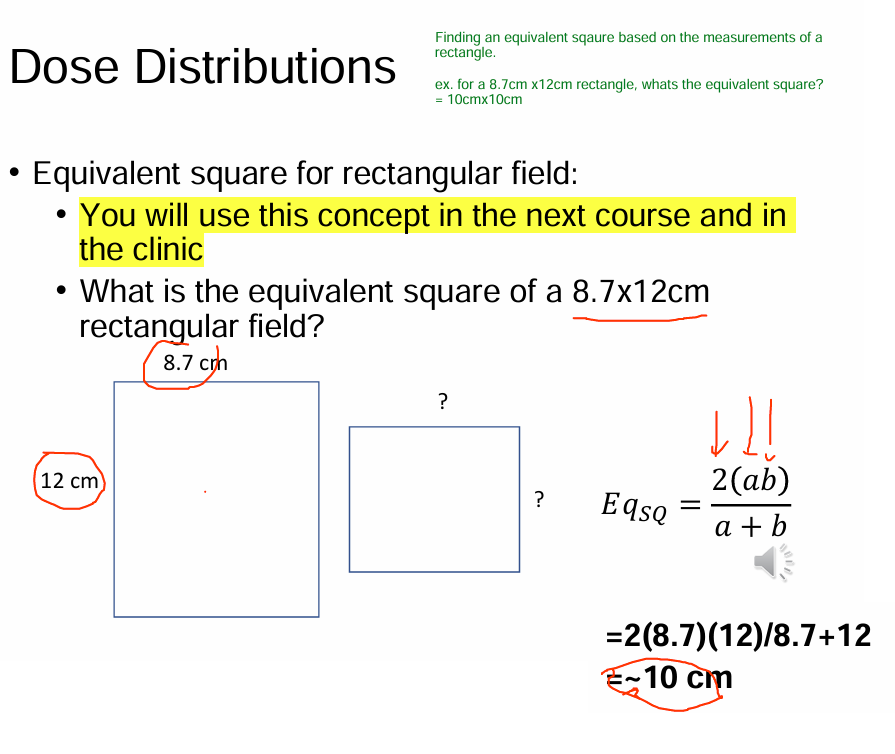
For any arbitrary radiation field (aka NOT a square field size), something like a rectangular field size, what will we do?
find the equivalent square for the rectangular field