Specific autoimmune diseases
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
autoimmune hemolytic anemia, autoimmune thrombocytopenic purpura, goodpasture's syndrome, pemphigus vulgaris, acute rheumatic fever
what are some examples of autoimmune diseases with a type II hypersensitivity component
mixed essential cryoglobulinemia, systemic lupus erythematosus, rheumatoid arthritis
what are some exmplae of autoimmune diseases with a type III hypersensitivity component
insulin-dependant diabetes mellitus, rheumatoid arthritis, experimental autoimmune encephalomyelitis (EAE), multiple sclerosis
grave's disease, myasthenia gravis, insulin-resistant diabetes, hypoglycemia
give some examples of autoimmune diseases mediated by AUTOANTIBODIES AGAINST CELL SURFACE RECEPTORS
thyroid stimulating hormone receptor, hyperthyroidism
what is the receptor that there are antibodies against in Graves disease?
What is the consequence of this?
acetylcholine receptor, progressive weakness
what is the receptor that there are antibodies against in myasthenia gravis?
What is the consequence of this?
insulin receptor (antagonist), hyperglycemia and ketoacidosis
what is the receptor that there are antibodies against in insulin-resistant diabetes?
What is the consequence of this?
insulin eceptor (agonist), hypoglycemia
what is the receptor that there are antibodies against in hypoglycemia?
What is the consequence of this?
skin, most outwardly apparent
What is the (possibly) the most clinically recognized organ where autoimmune issues take place?
Why?
autoimmune (lymphaocytic) thyroiditis
hyperthyroidism
lymphocytic parathyroiditis
What are some common t cell mediated diseases of the thyroid? (2)
And the parathyroid? (1)
atrophic pancreatitis
autoimmune adrenitis
insulin-dependent diabetes mellitus (type I)
What is a common t cell mediated diseases of the pancreas?
The adrenal gland?
Whats a systemic one?
graves disease
which autoimmune thyroiditis causes HYPERthyroidism
hashimoto's disease (lymphocytic thyroiditis)
which autoimmune thyroiditis causes HYPOthyroidism
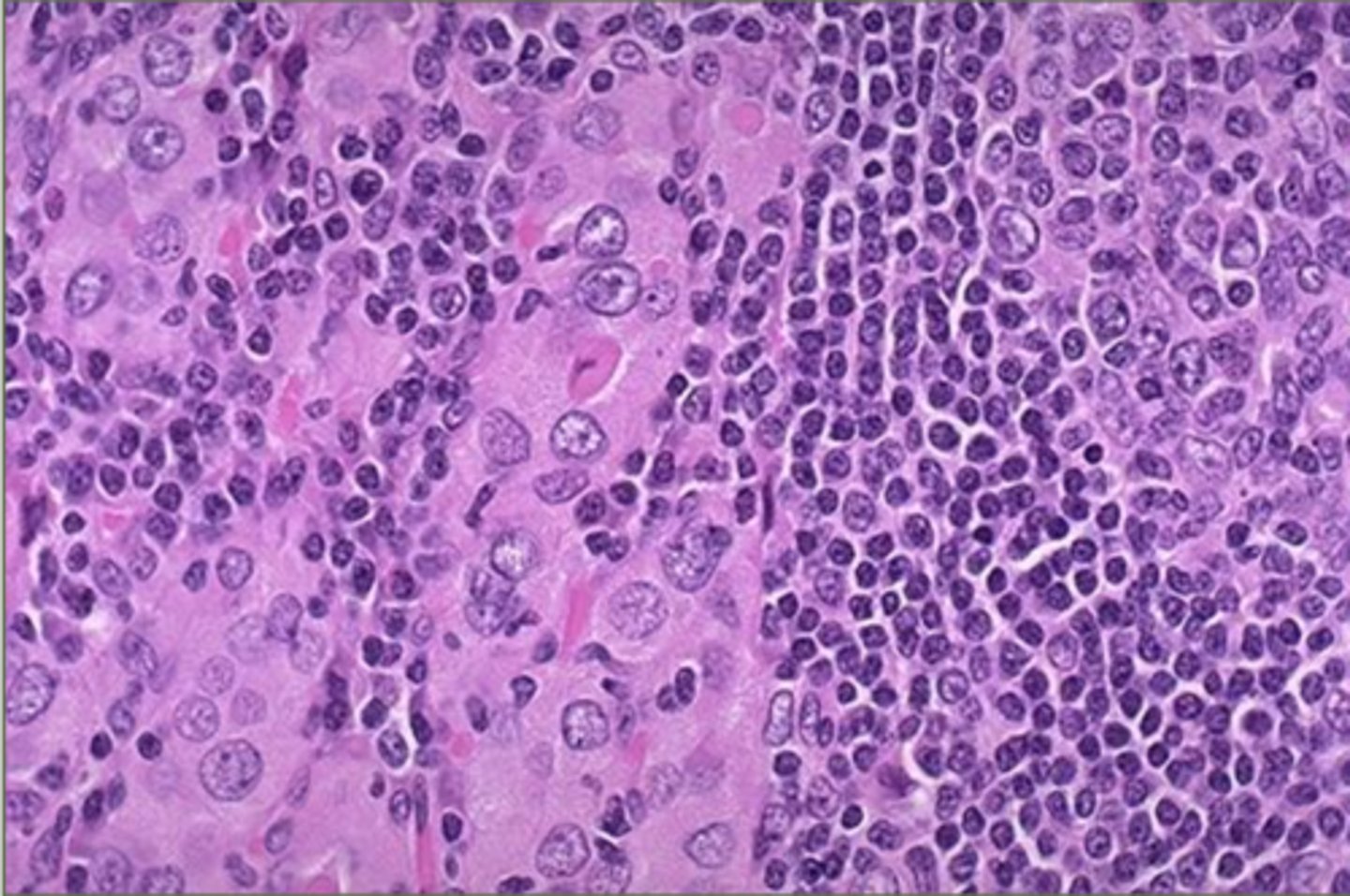
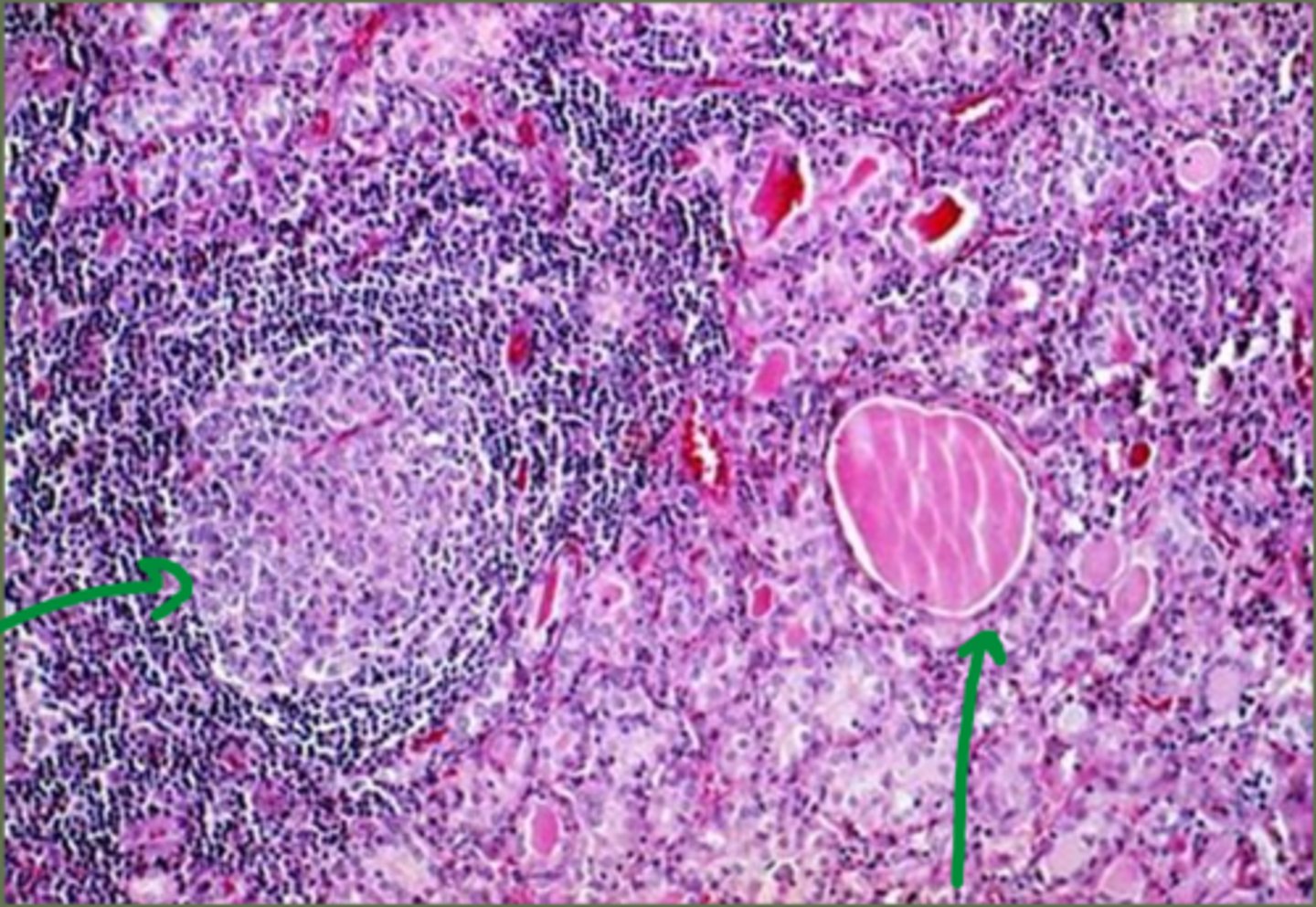
huge influx of lymphocytes is destroying the normal thyroid tissue (hashimotos disease)
What is happening to this thyroid tissue
thyroid stimulating hormone receptor, chronic overproduction of thyroid hormones
graves disease is mediated by antibodies that bind ___________________.
These mimic the natural ligand and cause ______________________________ (that cant respond to TSH regulation)
heat intolerance, weight loss, nervousness, irritabilty, enlargement of the thyroid, outwardly bulging eyes
what are some symptoms of graves disease?
antibodies react with the eye muscles
Why does graves disease lead to bulging eyes?
thyroid follicular cells, antithyroid antibodies, T cell activation, fibrosis
hashimotos thyroiditis is caused by the destruction of _________________. And is characterized by the formation of ________________ and _________________________.
This results in a progressive _____________ of the thyroid gland
unexplained weight gain, lethargy, cold intolerance, hair loss, increased skin pigment, dull/dry skin and coat
what are some symptoms of autoimmune hyopthyroidism?
the left is diseased - lymphocytes destroyed the follicle and its not producing collagen, the right is normal
Which of these follicles from a thyroid gland is typical of hashitmotos disease?
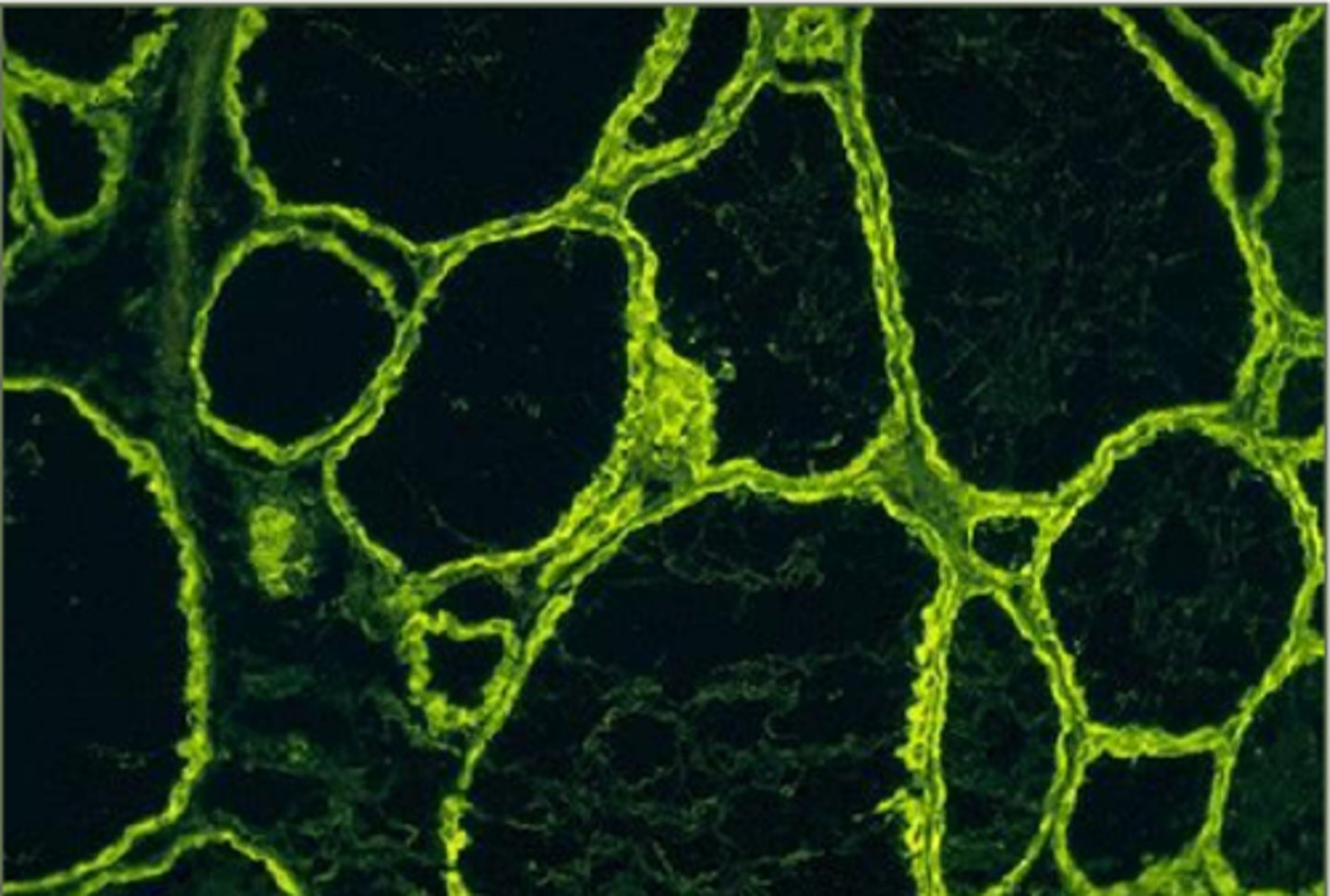
the interior should also glow, this shows us the follicles are inactive and not producing collagen
This is a thyroid from a hashimotos dog under immunofluorescence. How can you tell the dog has hypothyroidism?
autoimmune hemolytic anemia, systemic lupus erythematosus, pemphigus diseases, myasthenia gravis
what are common antibody mediated diseases that are systemic? (2)
Which one is a skin disease? (1)
Which one is neuromuscular? (1)
self destruction of red blood cells
what even IS autoimmune hemolytic anemia? (AIHA)
autoagglutinating, IgG>>>IgM, intravascular agglutination
What is the name, Ab isotype, and clinical effect of type I AIHA?
intravascular hemolysis, IgM, intravascular hemolysis (duh, srry)
What is the name, Ab isotype, and clinical effect of type II AIHA?
warm-reacting, IgG, anemia, splenomegaly
What is the name, Ab isotype, and clinical effect of type III AIHA?
cold agglutinin, IgM, cyanosis, of extremities
What is the name, Ab isotype, and clinical effect of type IV AIHA?
cold extravascular hemolysis, IgM, anemia
What is the name, Ab isotype, and clinical effect of type V AIHA?
1 and 2, anemia
Which types of AIHA are the most common?
And at the end of the day, what symptom do ALL of the cause
antibodies bind RBCs, macrophages recognize the Fc portion, phagocytize the RBC
There are two basic mechanisms of red blood cell lysis.
Which of them leads to EXTRAvascular hemolysis?
activation of the classical complement cascade
There are two basic mechanisms of red blood cell lysis.
Which of them leads to INTRAvascular hemolysis?
Coombs test,
What test is used for the detection of erythrocyte surface antigen or complement?
washed RBCs are added to anti-dog antibodies.
If there are autoantibodies on the RBCs, they will bind Anti-dog antibodies and agglutinate
What causes the agglutination in a coombs test? Like... how does it work?
systemic lupus erythematosus
Which autoimmune disease is characterized by antibodies directed at components of the cell nucleus
inflammation, vasculitis, immune complex deposition (type III), vasculopathy
the exact etiology is still unknown, but the primary pathological finding is SLE are ____________(4)
suggested etiologies for SLE that likely have some kind of additive effect
What do the following things have in common?
•Infectious agents.
•Genetic influences.
•Anti-lymphocyte antibodies.
•Organ specific autoantibodies.
•Complement deficiencies.
skin, kidney, immunofluorescence
In SLE, immune complexes may be deposited in a variety of organs, most notably the _____ and ______ and _____________________ is used for a definitive diagnosis
two
At least how many of the following symptoms must be present for a diagnosis of SLE?
-Typical skin lesions.
-Polyarthritis.
-Coombs-positive hemolytic anemia.
-Thrombocytopenia.
-Proteinuria.
one
in addition to the previous list, How many of THESE following symptoms must be present for an SLE diagnosis?
-Positive ANA test
-Positive LE test
At least TWO of: typical skin lesions, polyarthritis, coombs-positive emolytic anemia, thrombocytopenia, proteinuria....
positive ANA test OR positive LE cell test
Okay... lets see how closely we cared about this list....
List at least TWO of the symptoms that would have to be present for an SLE diagnosis AND list at least one of the two tests that would need to be present
(extensive, skip if you want, as per usual, this slide might only be for Gina)
antinuclear antibody test, immunofluorescence microscopy
so what does ANA test stand for? And what test is actually run?
False; ANA is not definitive and other tests are neede to confirm
true/false: the ANA test is a definitive diagnostic test for SLE
false: titers may be important, and higher titers may indicate more serious autoimmune condition
true/false: titer levels of ANAs in the blood DO NOT correlate to the severity of disease
LE cell, LE body
_________: a neutrophil or macrophage that has phagocytized the denatured nuclear material of another cell. and the denatured material seen is an __________
true
true/false: bullous autoimmune skin diseases are TRULY limited to the skin
adhesion proteins, pemphigus, desmosomes/hemidesmosomes
___________________ hold the various layers of skin together. __________ represents a group of diseases caused by a type II response that involves autoantibodies produced against the proteins responsible for keratinocyte cell to cell adhesion (____________).
transient vesicles, bullae, acantholysis
Pemphigus is characterized by ________ or _______ and hisologically by ___________
pemphigus foliaceus
______________________: the most common autoimmune skin disease in dogs and cats. It is often observed in middle-aged and older patients
pemphigus vulgaris
________: This form of pemphigus attacks the deepest layers of the epidermis, making it the most severe type of pemphigus.
within granular layers of superficial skin
where are blisters formed in pemphigus foliaceus?
(im gonna ask these both ways)
in mucous membranes between basal and immediate suprabasal keratinocytes
Where are blisters formed in pemphigus vulgaris?
beneath the basal layer
where are blisters formed in bullous pemphigoid?
during lifestyle changes (whelping)
when is the most likely time for pemphigus foliaceus to start presenting itself
mucocutaneous junctions
where do we SEE lesions most commonly ni pemphigus vulgaris?
pemphigus foliaceus
which type of pemphigus causes blisters within granular layers of superficial epidermis?
pemphigus vulgaris
which type of pemphigus causes blisters in mucous membranes between basal and suprabasal keratinocytes?
bullous pemphigoid
which type of pemphigus causes blisters beneath the basal layer?
desmoglein 1
pemphigus foliaceus causes antibodies against what?
desmoglein 3
pemphigus vulgaris causes antibodies agaisnt what?
bullous pemphigoid antigens (collagen); lamina lucida of dermal epidermal junction
bullous pemphigoid has antibodies against what?
This ones a bit more weird, so also of note, these have attachment at ___________________________________________ (deeper than pemphigus)
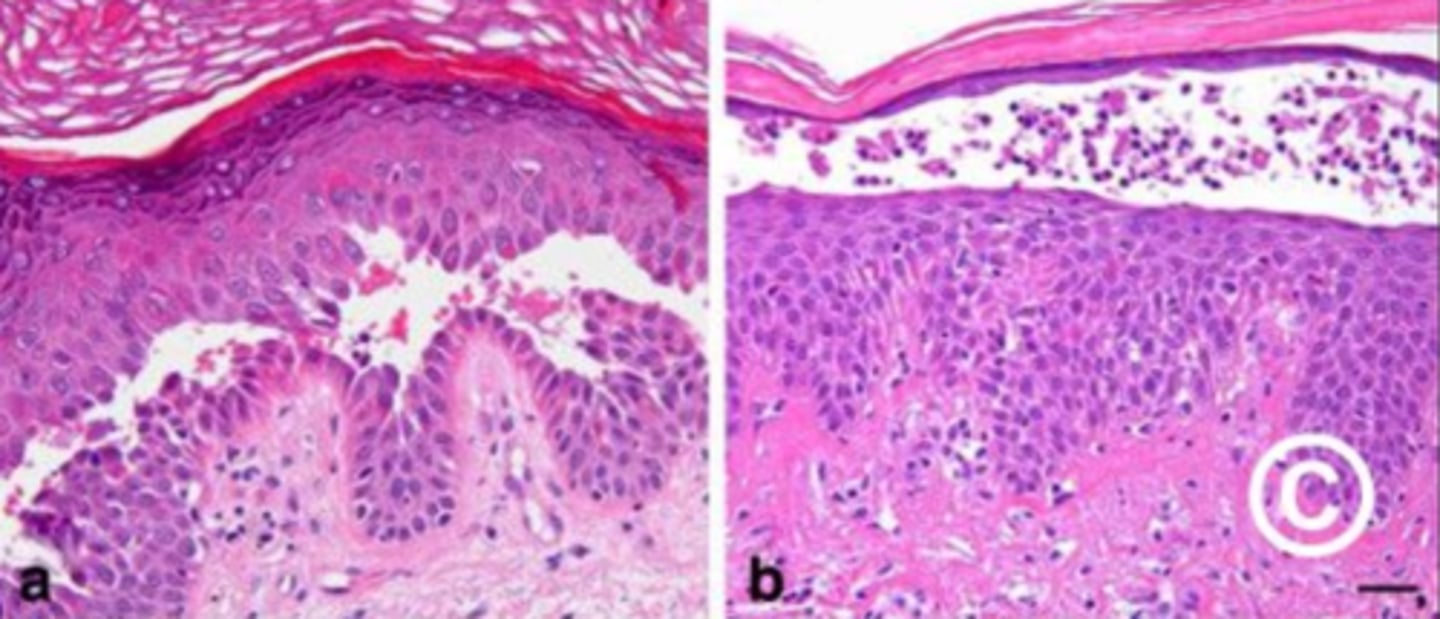
pemphigus foliaceus
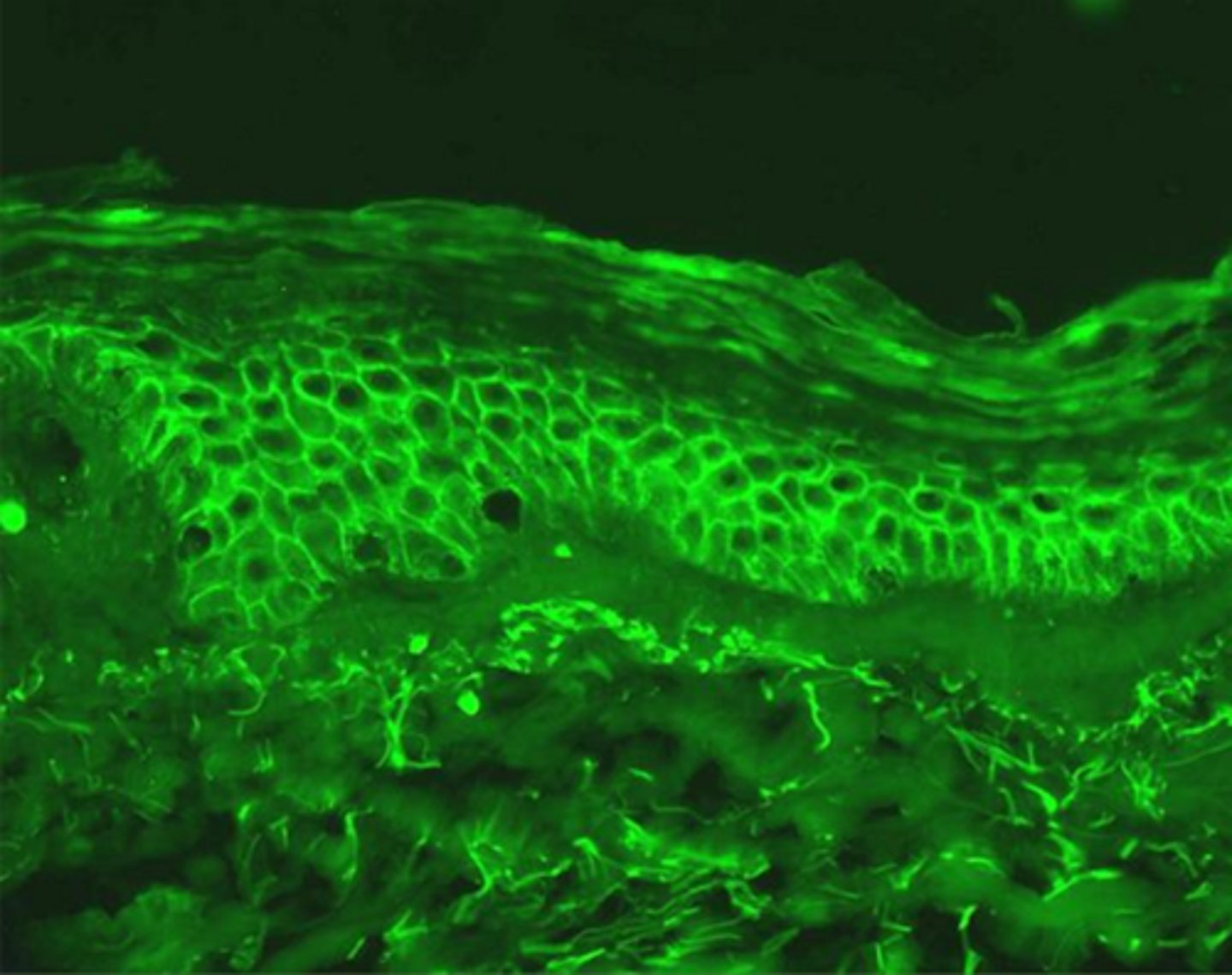
what type of pemphigus

pemphigus vulgaris
What type of pemphigus

bullous pemphigoid
What type of pemphigus

vulgaris is on the left, foliaceus is on the right
Which pemphigus is which?
acanthocytes
Non adherent epithelial cells are rounded and are called:
pemphigus vulgaris
which pemphigus?
bullous pemphigoid
which pemphigus?
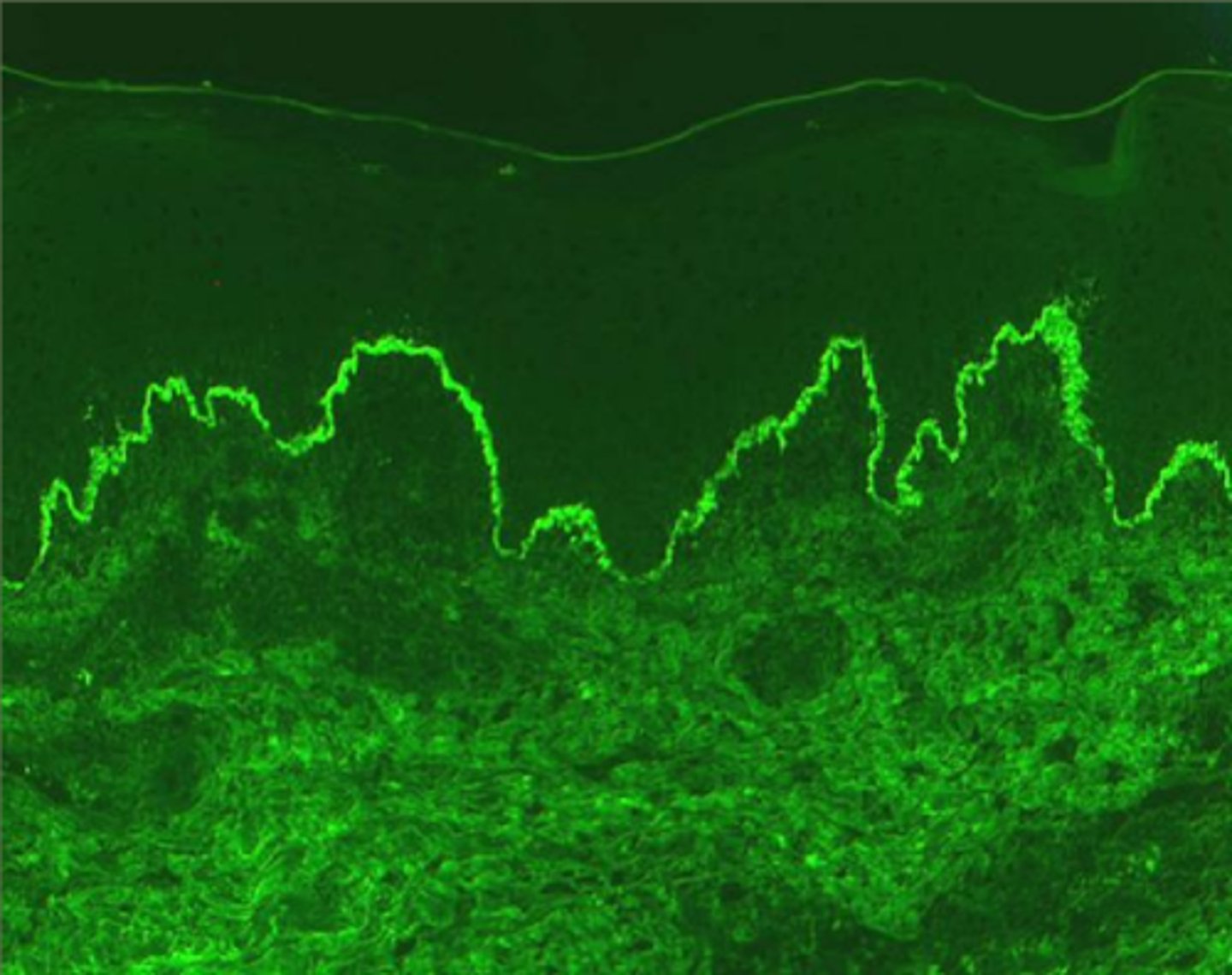
immunofluorescence
pemphigus diagnosis is confirmed using __________________
myasthenia gravis
__________: Antibodies to acetylcholine receptors
true
true/false: in myasthenia gravis, the Ach receptors are blocked, so the body still emits Ach, it just can't bind
anticholinesterase drugs
what is used as a diagnostic method for myasthenia gravis?