(25.5.6) S2: Tubular Reabsorption & S3: Tubular Secretion
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
Describe the Location and Function of Tubular Reabsorption
Begins as soon as filtrate enters the proximal tubules
Quickly reclaims most of tubular contents and returns them to blood
Selective process
Almost all organic nutrients are reabsorbed
Water and ion reabsorption is hormonally regulated and adjusted
Name the mechanisms underlying water and solute reabsorption from the renal tubules into the peritubular capillaries
Includes active and passive tubular reabsorption
Transcellular Route
Paracellular Route
Describe Steps of Transcellular Route
Transport across the apical membrane
Diffusion through the cytosol
Transport across the basolateral membrane
Often involves the lateral intercellular spaces because membrane transporters transport ions into these spaces
Movement through the interstitial fluid into the capillary
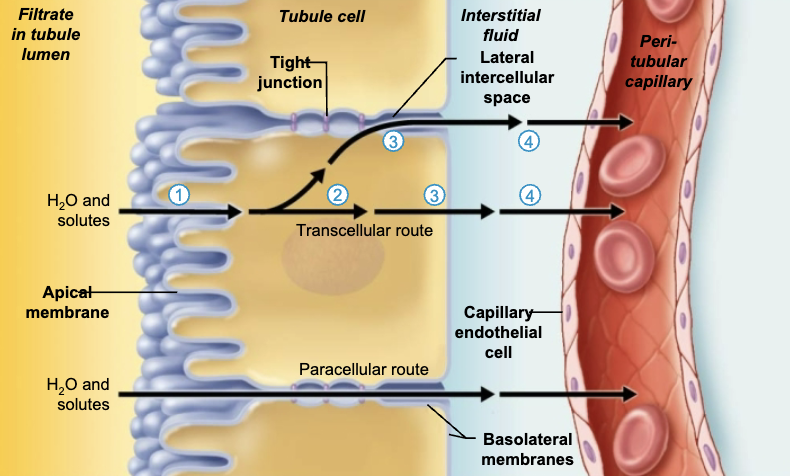
Describe Steps of Paracellular Route
Movement through leaky tight junctions, particularly in the proximal convoluted tubule
Movement through the interstitial fluid and into the capillary
Through which pathway are most water and solutes reabsorbed in the kidney tubule?
→ Transcellular
This means that transport must take place across the apical membrane and across the basolateral membrane for the substance to move from the lumen of the kidney tubule into the blood.
T/F: Tubular Reabsorption includes only active tubular reabsorption
→ FALSE
Tubular Reabsorption includes active AND passive tubular reabsorption
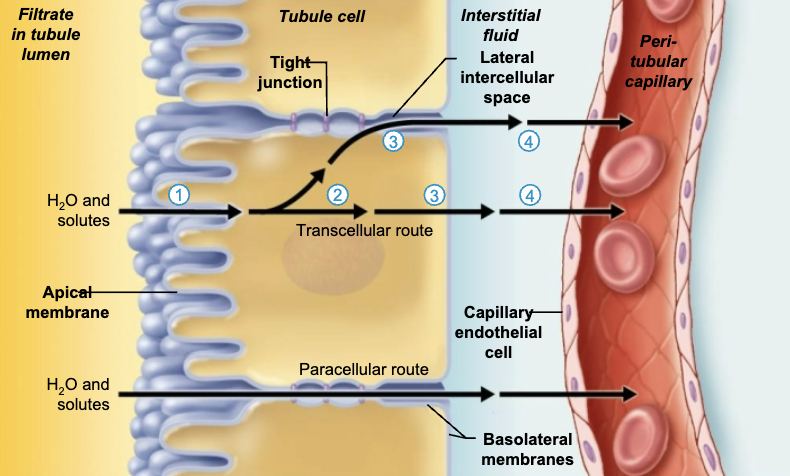
Describe Sodium Transport Across the Basolateral Membrane
Primary Active Transport
Na+ is most abundant cation in filtrate
Transport of Na+ across basolateral membrane of tubule cell is via primary active transport
Na+-K+ ATPase pumps Na+ into interstitial space
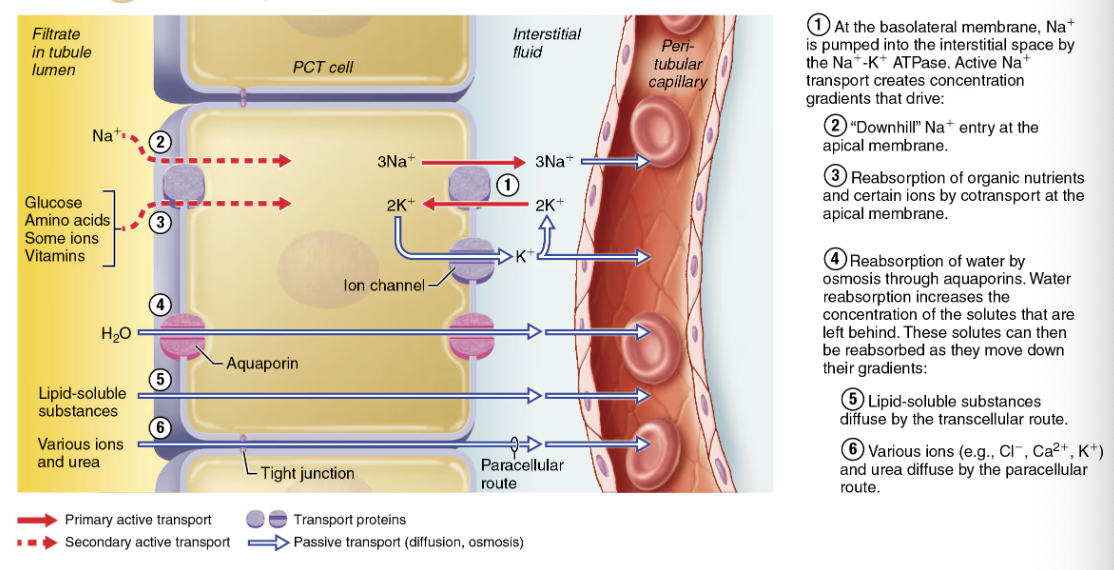
Steps of Tubular Reabsorption of water and nutrients Using Active & Passive Transport
At basolateral membrane, Na+ is pumped into the intestinal space by the Na+-K+ ATPase → Active Na+ transport creates concentration gradients that drive:
“Downhill” Na+ entry at the apical membrane
Reabsorption of organic nutrients and certain ions by co-transport at the apical membrane
Reabsorption of water by osmosis through aquaporins → Water reabsorption increases the concentration of the solutes that are left behind. These solutes can then be reabsorbed as they move down their gradients:
Lipid-soluble substances diffuse by the transcellular route
Various ions (Cl-, Ca2+, K+) and urea diffuse by the paracellular route
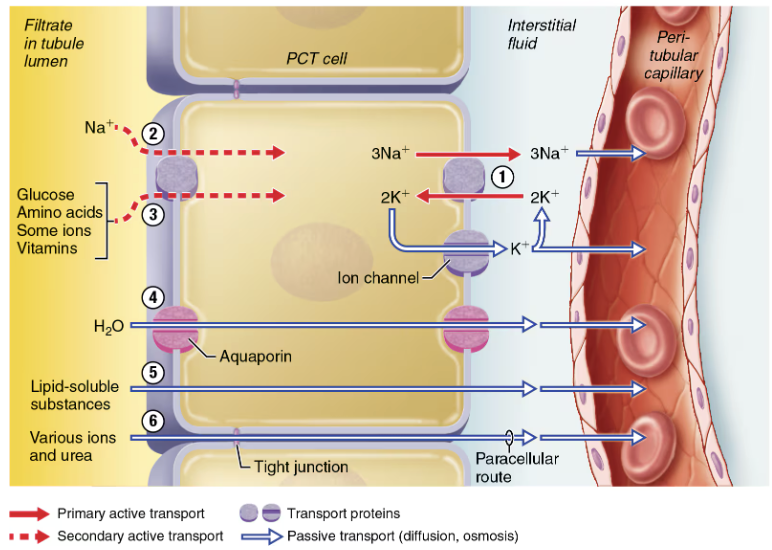
Describe Sodium Transport Across the Apical Membrane
Secondary Active Transport
Electrochemical gradient created by pumps at basolateral surface give “push” needed for transport of other solutes
Organic nutrients reabsorbed by secondary active transport are co-transported with Na+
Glucose, amino acids, some ions, vitamins
Distinguish between Passive Tubular Reabsorption of Water vs Solutes
Passive Tubular Reabsorption of Water
Obligatory water reabsorption
Aquaporins are ALWAYS present in PCT
Facultative water reabsorption
Aquaporins are inserted in collecting dusts ONLY if ADH is present
Passive Tubular Reabsorption of Solutes
Solute concentration in filtrate increases as water is reabsorbed
Creates concentration gradients for solutes, which drive their entry into tubule cell and peritubular capillaries
Fat-soluble substances, some ions, and urea will follow water into peritubular capillaries down their concentration gradients
For this reason, liquid-soluble drugs and environmental pollutants are reabsorbed even through it is not desirable
SUMMARY List and Describe Sodium Transport Across the Basolateral Membrane
Primary Active Transport
Na+ is most abundant cation in filtrate
Transport of Na+ across basolateral membrane of tubule cell is via primary active transport
Na+-K+ ATPase pumps Na+ into interstitial space
Secondary Active Transport
Electrochemical gradient created by pumps at basolateral surface give “push” needed for transport of other solutes
Organic nutrients reabsorbed by secondary active transport are co-transported with Na+
Glucose, amino acids, some ions, vitamins
Passive Tubular Reabsorption of Water
Obligatory water reabsorption
Aquaporins are ALWAYS present in PCT
Facultative water reabsorption
Aquaporins are inserted in collecting dusts ONLY if ADH is present
Passive Tubular Reabsorption of Solutes
Solute concentration in filtrate increases as water is reabsorbed
Creates concentration gradients for solutes, which drive their entry into tubule cell and peritubular capillaries
Fat-soluble substances, some ions, and urea will follow water into peritubular capillaries down their concentration gradients
For this reason, liquid-soluble drugs and environmental pollutants are reabsorbed even through it is not desirable
Define Transport Maximum
Transcellular transport systems are specific and limited
Transport maximum (Tm) exists for almost every reabsorbed substance
Reflects number of carriers in renal tubules that are available
When carriers for a solute are saturated, excess is excreted in urine
EX: hyperglycemia leads to high BG levels that exceed Tm, and glucose spills over into urine
Patients with uncontrolled diabetes mellitus often have glucose in their urine. This is because the concentration of glucose in the filtrate exceeds the ____________ of the carrier proteins in the proximal tubule.
→ Transport maximum
Normally, all of the glucose in the filtrate gets reabsorbed by transport proteins in the proximal tubule. When an individual has extremely high levels of blood glucose that enter the filtrate (as in uncontrolled diabetes mellitus), there are not enough transport proteins to reabsorb all of the glucose. The glucose that doesn't get reabsorbed remains in the filtrate and is excreted.
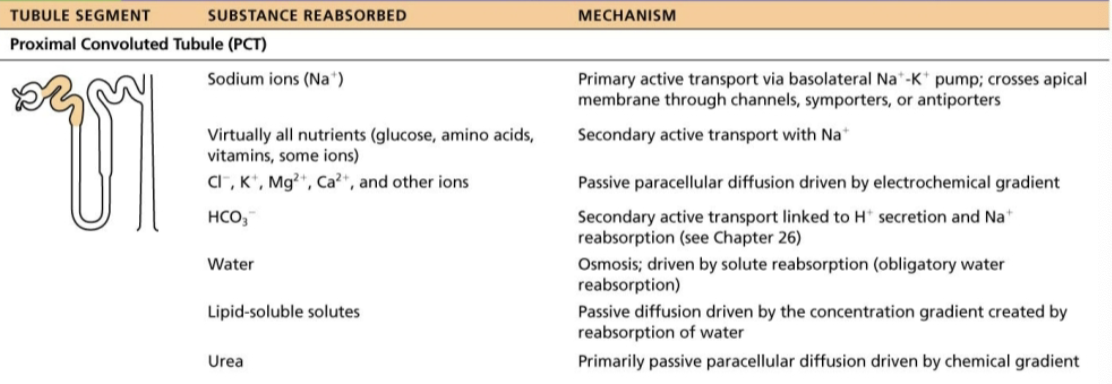
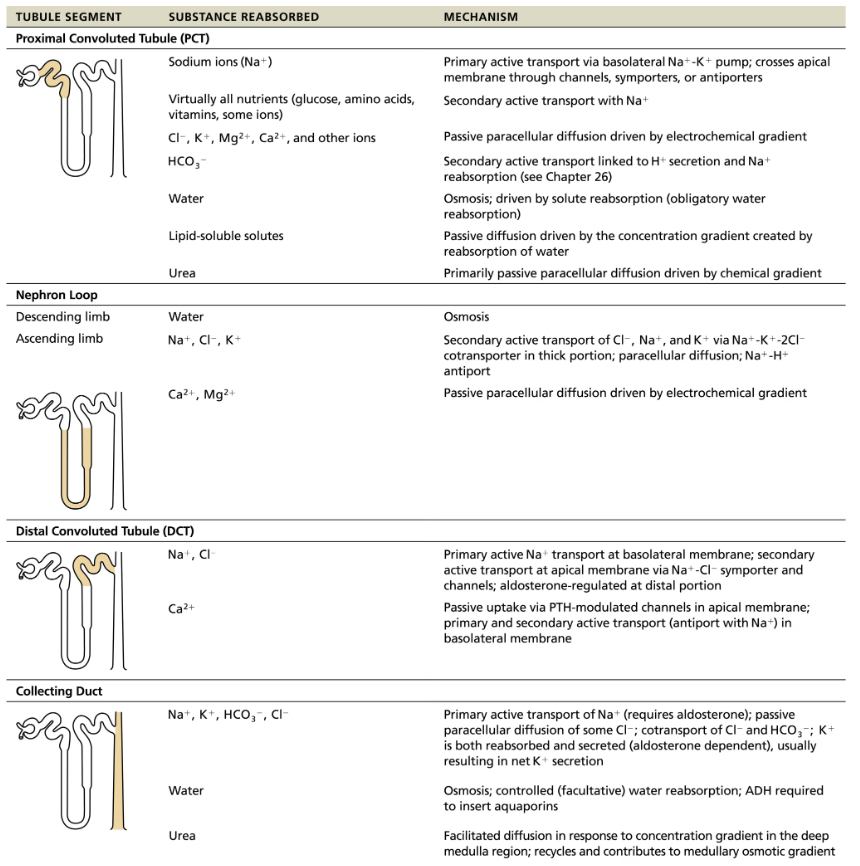
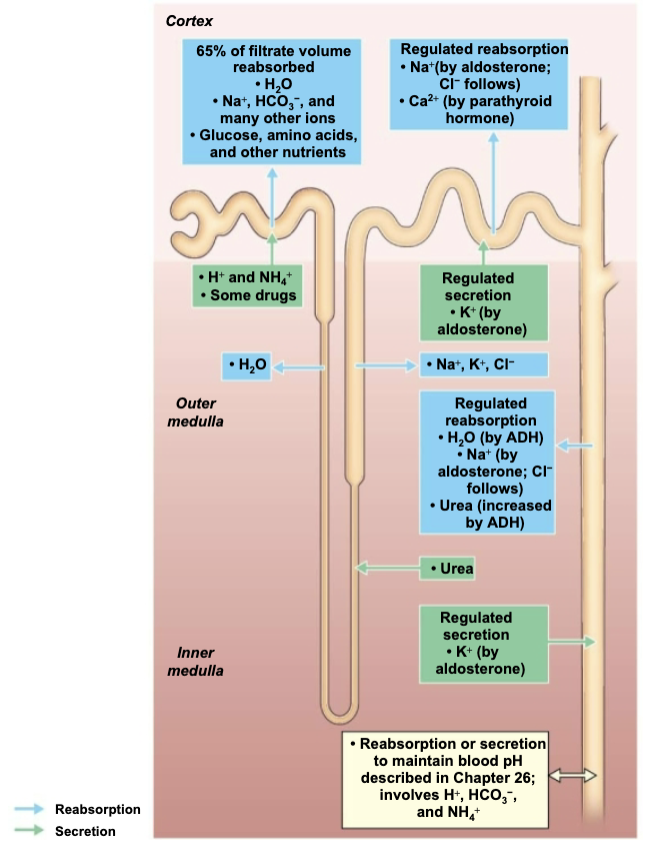
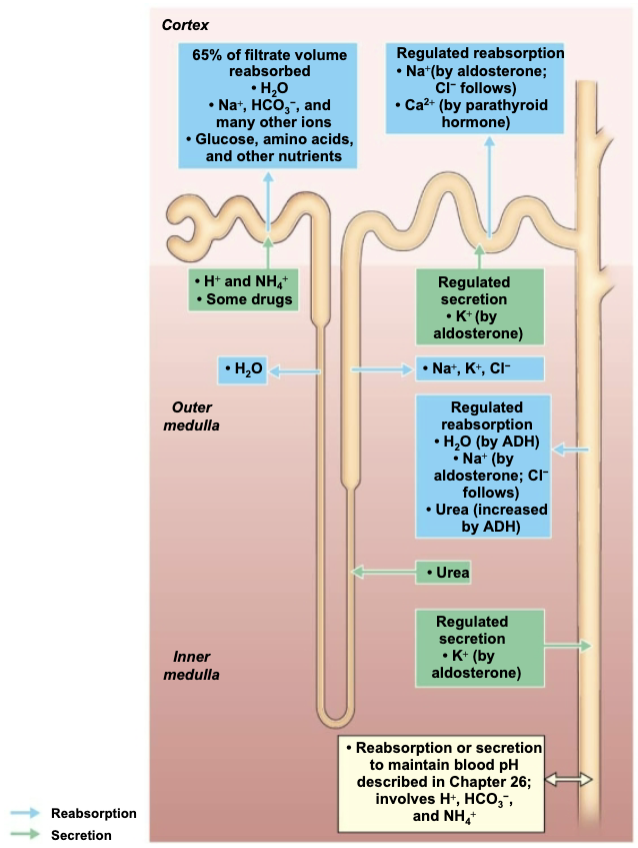
Describe the Reabsorptive Capabilities of Renal Tubules and Collecting Ducts @ Proximal Convoluted Tubule
Site of MOST reabsorption
All nutrients, such as glucose and amino acids are reabsored
65% of Na+ and water reabsorbed
Ions
Almost all uric acid
About half of urea (later secreted back into filtrate
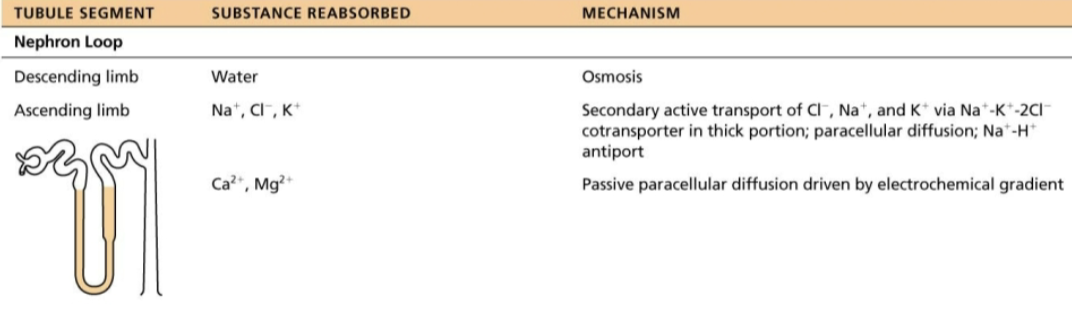
Describe the Reabsorptive Capabilities of Renal Tubules and Collecting Ducts @ Nephron Loop
Descending limb
H2O can leave and Solutes cannot
Thin segment is passive to Na+ movement
Ascending limb
H2O cannot leave and Solutes can
Thick segment has Na+-K+-2Cl- symporters and Na+-H+ antiporters that transport Na+ into cell
Some Na+ can pass into cell by paracellular route in this area of limb
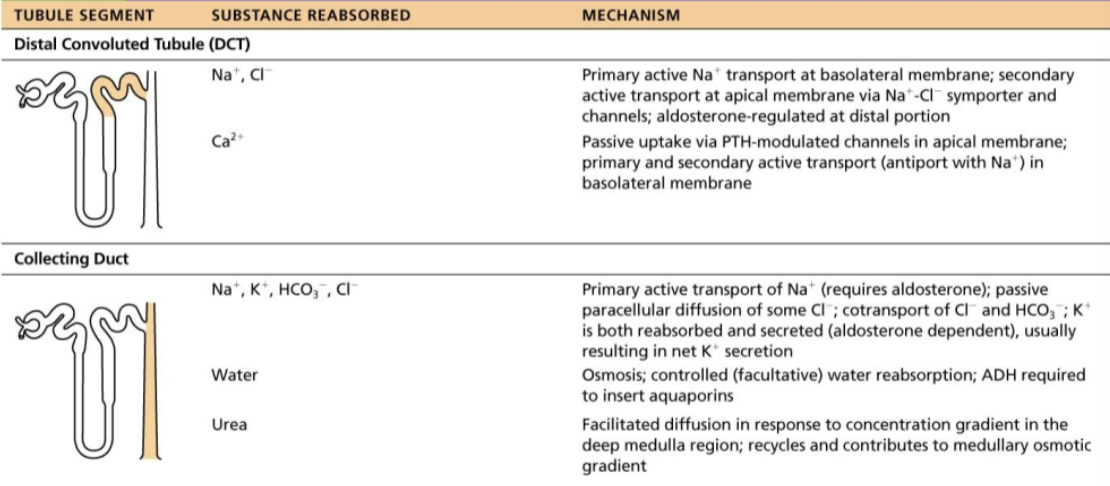
Describe the Reabsorptive Capabilities of Renal Tubules and Collecting Ducts @ Distal Convoluted Tubule & Collecting Duct
Reabsorption is hormonally regulated in these areas
Antidiuretic hormone (ADH)
Aldosterone
Atrial natriuretic peptide
Parathyroid hormone
Reabsorption of which of the following drives the reabsorption of water and many other solutes in the proximal tubule?
→ Sodium
Sodium ions are reabsorbed down their concentration gradient into the tubular cells. Na+K+pumps in the tubular cell membranes are responsible for maintaining the concentration gradient. The energy provided by the Na+ gradient is used to fuel secondary active transport of many other substances
SUMMARY of Reabsorptive Capabilities of Renal Tubules and Collecting Ducts
Proximal Convoluted Tubule
Site of MOST reabsorption
All nutrients, such as glucose and amino acids are reabsored
65% of Na+ and water reabsorbed
Ions
Almost all uric acid
About half of urea (later secreted back into filtrate
Nephron Loop
Descending limb
H2O can leave and Solutes cannot
Thin segment is passive to Na+ movement
Ascending limb
H2O cannot leave and Solutes can
Thick segment has Na+-K+-2Cl- symporters and Na+-H+ antiporters that transport Na+ into cell
Some Na+ can pass into cell by paracellular route in this area of limb
Distal Convoluted Tubule & Collecting Duct
Reabsorption is hormonally regulated in these areas
Antidiuretic hormone (ADH)
Aldosterone
Atrial natriuretic peptide
Parathyroid hormone
List how sodium and water reabsorption are regulated in the distal tubule and collecting duct
Antidiuretic hormone (ADH)
Aldosterone
Atrial natriuretic peptide
Parathyroid hormone
Role of Antidiuretic Hormone (ADH)
Released by posterior pituitary gland
Causes principal cells of collecting ducts to insert aquaporins in apical membranes, increasing water reabsorption
INCREASED ADH levels cause an increase in water reabsorption
Role of Aldosterone
Targets collecting ducts (principal cells) and distal DCT
Promotes Na+ reabsorption (water follows)
As a result, little Na+ leaves body
Function: INCREASES BP and DECREASE K+ levels
Role of Atrial Natriuretic Peptide
Released by cardiac atrial cells if blood volume or pressure elevated
Reduces blood Na+ → resulting in decreased blood volume and BP
Role of Parathyroid hormone
Acts on DCT to increase Ca2+ reabsorption
When given to a patient, which of the following substances would increase his or her urinary output?
A.) intravenous saline
B.) albumin
C.) aldosterone
D.) antidiuretic hormone
→ A.) intravenous saline
SUMMARY of Tubular Reabsorption and Secretion
Antidiuretic hormone (ADH)
Released by posterior pituitary gland
Causes principal cells of collecting ducts to insert aquaporins in apical membranes, increasing water reabsorption
INCREASED ADH levels cause an increase in water reabsorption
Aldosterone
Targets collecting ducts (principal cells) and distal DCT
Promotes Na+ reabsorption (water follows)
As a result, little Na+ leaves body
Function: INCREASES BP and DECREASE K+ levels
Atrial natriuretic peptide
Released by cardiac atrial cells if blood volume or pressure elevated
Reduces blood Na+ → resulting in decreased blood volume and BP
Parathyroid hormone
Acts on DCT to increase Ca2+ reabsorption
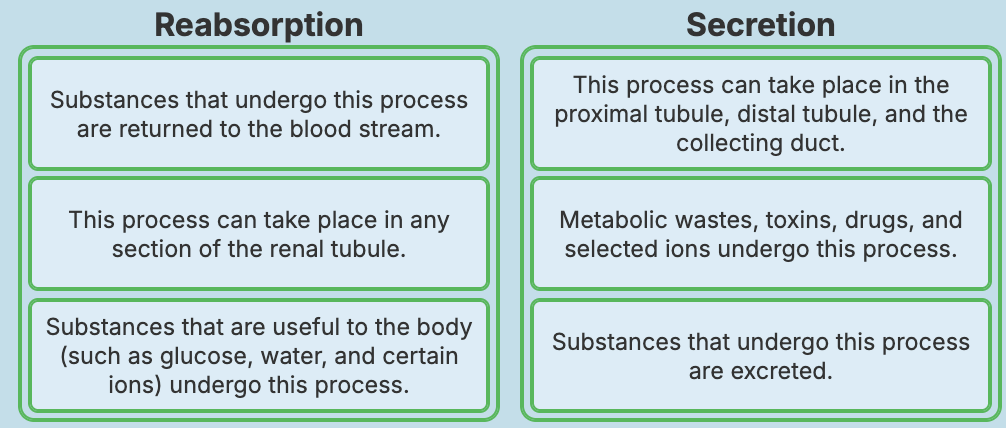
Describe the Location and Function of Tubular Secretion
Occurs almost completely in PCT
Tubular secretion is reabsorption in reverse
Selected substances are moved from peritubular capillaries through tubule cells out into filtrate
List several substances that are secreted from Tubular secretion
K+
H+
NH4+
Creatinine
Organic acids and bases
Substances synthesized in tubule cells also are secreted (EX: HCO3-)
Describe the importance of Tubular secretion
Disposing of substances, such as drugs or metabolites
Eliminating undesirable substances that were passively reabsorbed
EX: urea and uric acid
Ridding body of excess K+ (aldosterone effect)
Controlling blood pH by altering amounts of H+ or HCO3- in urine
SUMMARY of Tubular Reabsorption and Secretion
Predict the Effect of HIGH and LOW GFR on Tubular Reabsorption & Explain Tubuloglomerular Feedback would respond to HIGH and LOW GFR