NUR 305 Neurological Disorders III
1/60
Earn XP
Description and Tags
Neurological Diseases
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
Spinal Cord Trauma
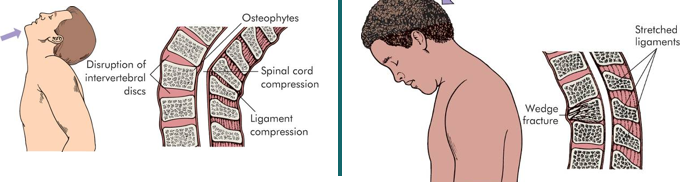
Traumatic injury of vertebral and neural tissues as a result of:
Compressing forces
Pulling forces
Shearing forces
Vertebral Injuries
Simple fracture
Compressed fracture
Comminuted fracture
Dislocation
Vertebrae get out of alignment.
T/F: Spinal Cord Trauma most commonly occurs due to vertebral injuries.
True
Most Common Locations of Spinal Cord Trauma/Injury
Cervical (1-7)
T1-L2 Lumbar Vertebrae
Why do Spinal Cord Injuries/Trauma occur at C1-7 and T1-L2 most commonly?
These are the most mobile portions of vertebral column.
Ligament/muscle damage can cause vertebral weakness/instability.
These are areas where the spinal cord occupies most of the vertebral canal.
In patients with C4 injury or above, _____ function and _____ should be monitored. Mechanical ventilation is commonly needed.
respiratory; ABCs
What are the 4 types of Spinal Cord Trauma?
Spinal Shock
Paraplegia (legs affected)
Quadriplegia (legs and arms affected)
Autonomic Hyperreflexia (dysreflexia)
Spinal Shock
Normal activity of the spinal cord stops at and below the level of injury.
Inflammation or bruising to the spinal cord = loss of communication to the areas below the injury.
Sites lack continuous nervous discharges from the brain.
Complete loss of reflex function (skeletal, bladder, bowel, sexual function, thermal control, and autonomic control) below level of lesion.
Flaccid Paralysis
Neurogenic Shock
*Different from spinal shock.
Injuries at the 6th thoracic vertebrae or above.
Results in the lack of normal sympathetic outflow from the T1–L2 region of the spinal cord.
The SNS does NOT release norepinephrine.
Parasympathetic system takes over instead. Leads to:
Bradycardia
Peripheral vasodilation
Blood pools in extremities
Decreased venous return to the heart
Low cardiac output
Low systemic blood pressure
Why is norepinephrine so important? Why does it cause issues when sympathetic outflow is lost during Neurogenic shock?
Norepinephrine attaches to adrenergic receptors in blood vessels, controlling vasomotor tone through vasoconstriction.
Without norepinephrine, blood vessels do not constrict, resulting in peripheral vasodilation.
Blood begins to pool in the extremities due to vasodilation.
Venous return to the heart is decreased due to fluid overload in peripheries.
CO and BP decreases as a result of vasodilation and low venous return.
What CMs differentiate neurogenic shock from hypovolemic shock?
Neurogenic Shock
Bradycardia with hypotension is present.
Hypovolemic Shock
Tachycardia with hypotension is present.
How can Neurogenic Shock be treated?
We can give norepinephrine through IV.
Autonomic Dysreflexia
Description
Potentially dangerous and, in rare cases, lethal clinical syndrome.
Develops in individuals with spinal cord injury (SCI).
Occurs in patients with SCI at or above the sixth thoracic vertebral level (T6)
Results in acute, uncontrolled hypertension.
What causes Autonomic Dysreflexia?
Massive, uncompensated cardiovascular response to noxious stimulation of the sympathetic nervous system.
Below the level of injury, the body still senses baroreceptors → The brain ends up overreacting to stimuli.
Noxious Stimulation leads to overreaction of the sensory receptors below the level of the cord lesion.
Ex) Full bladder/bowel, ulcers, syringes left in the bed.
Clinical Manifestations of Autonomic Dysreflexia
Facial flushing
Profuse sweating
Goose bumps above injury level
Blurred vision
Nasal congestion
Headache
Anxiety
Sudden increase in BP (20mmHg systolic/10mmHg diastolic)
How is Autonomic Dysreflexia treated?
Determine the cause/noxious stimulus (blocked catheter, full bladder, impacted stool) and correct it.
If not the cause, survey the entire body for a sore or other cause of pain.
T/F: If an injury occurs at T6 or higher, you should worry about the respiratory system.
True; The diaphragm and accessory muscles, such as the abdominal muscles, aid in respiration and may lose innervation/function with a T6> SCI.
What are the 5 types of Headaches?
Tension
Migraine
Trigeminal Autonomic Cephalgia
Sinus
Trigeminal Neuralgia
Tension Headache
Bilateral pain with mild to moderate pressure.
No change in severity of pain.
Migraine Headache
Periodic, throbbing headaches that are characterized by altered perceptions, nausea, and severe pain.
Chronic headaches
Photophobia possible (sensitivity to light)
Trigeminal Autonomic Cephalgia/Cluster Headache
Attacks of severe, strictly unilateral pain.
Occur in the orbital, supraorbital, temporal, or in any combination of these sites.
Can last from 15 to 180 minutes and occur from once every other day to eight times a day.
Thought to be related to Histamine response.
Treatment = 100% O2 via NC for 10 minutes.
Sinus Headache
Pain and pressure in frontal and maxillary sinuses.
Pain increases when leaning over (increased pressure on sinuses).
Trigeminal Neuralgia Headache
Caused by irritation of the trigeminal nerve (cranial nerve V).
Causes severe facial pain.
Characterized by severe jaw pain going up to the temple.
Treatment = Burning of CN V.
What are symptoms of headaches or other neurological issues that need further evaluation to rule out the possibility of a brain tumor?
Abnormal neurological examination.
Change in prior headache patterns.
Worsening of headache with a change in body position.
Bending over
Coughing, sneezing
Maneuvers that raise intrathoracic pressure or intracranial pressure.
Worsening headaches at night that awaken the patient from sleep.
Parkinson's Disease
Destruction of the substantia nigra in the brain results in a lack of dopamine (cerebrum).
Dopamine is required for smooth, coordinated movement.
Symptoms appear after 80% of dopamine producing cells destroyed.
Has a progressive decline.
Unknown cause.

Manifestations of Parkinson's
Problems w/Movement & Tremors of the Hands & Head
Pill rolling tremor.
See image.
Tremors may disappear during purposeful movement.
Difficulty initiating movement.
Difficulty getting up from chairs or walking.
Loss of fine hand movements.
Change in handwriting.
Shuffling gait.
Not picking up feet when walking.
Slowed movements.
The classic symptoms of Parkinson's Disease are TRAP. What does this stand for?
Tremor at rest
Rigidity
Akinesia (lack of movement) or bradykinesia (slow movement)
Postural/gait instability (MSK rigidity)
Diagnosing Parkinson's
History
Physical examination
Neurologic assessment
Oher tests to rule out other conditions.
Neuromuscular testing.
Treatment for Parkinson's
Treatments
Medications to increase dopamine.
One for the liver, which likes to metabolize dopamine quickly. (Stops liver from metabolizing dopamine)
One is dopamine.
Deep brain stimulation.
Stimulates dopamine-producing cells to prod. dopamine.
Brain surgery.
Physical and occupational therapy along with assistive devices.
Health Promotion
Coping strategies
Support
Proper nutrition
Adequate rest
These can all increase dopamine levels.
Multiple Sclerosis (MS)
Demyelinating Disorder
Sensory and Motor Disorder.
Chronic, Autoimmune, Progressive, Inflammatory disorder of the CNS.
The immune system destroys myelin.
Most common in women 18-48 yrs, northern European heritage
Schwann cells myelinate the ____; Oligodendrocytes myelinate the ____.
PNS; CNS
What are the 3 types of Multiple Sclerosis (MS)?
Mixed (general)
Spinal
Cerebellar
Diagnosing Multiple Sclerosis (MS)
History & Physical exam
Change in vision is early sign
Progresses to bilateral numbness or unusual sensations.
MRI
CSF analysis (high protein, gamma globulin, & lymphocytes)
Nerve conduction studies
Stimulate a nerve, see how long it takes to travel.
What does MS cause/result in?
Inflammation and damage to the myelin within the CNS, then the peripheral nerves.
CNS damage and neurological disability.
Characterized by remissions and exacerbations (chronic condition).
Causes damage to diffuse patches throughout CNS.
Common Symptoms of MS
Most Common
Weakness
Numbness
Tingling sensations
Balance problems
Blurred vision (early)
Fatigue
Relapsing-Remitting MS
Symptoms involving the eyes
Optic nerves are heavily myelinated.
Sensory symptoms
Numbness
Paresthesia
Cerebellar symptoms (coordination)
Ataxia
Tremor
Dysarthria
Motor symptoms (late symptoms)
Hemiparesis, paraparesis, and quadriparesis.
Spinal cord involvement
Fecal and urinary incontinence.
Diagnosing and Treating Multiple Sclerosis
Diagnosis
Lesions of demyelination detected on imaging studies.
Patient report of specific neurological deficits.
McDonald criteria.
Treatment
Medications to prevent inflammatory cells from traveling across the blood-brain barrier.
Reduce clinical attacks of new MS lesions.
Guillain-Barré syndrome
Peripheral NS Disorder
Acquired inflammatory, autoimmune disease.
Causes demyelination of the peripheral nerves.
Acute onset, ascending motor paralysis.
Begins in feet and moves upward.
Heals in a descending fashion.
Return of motor functions.
Causes of Guillain-Barré Syndrome
Humoral and cellular immunologic reaction.
May be preceded by a viral or bacterial infection.
Ex. Campylobacter jejuni
Vaccination may precede Guillain-Barré Syndrome (unusual)
Treatment of Guillain-Barré Syndrome
Plasmapheresis
High dose immunoglobulin therapy (IV IGG)
Why is catching Guillain-Barré Syndrome early crucial?
If caught early the worst symptoms can be prevented. If not, then the patient may lose ventilatory muscle function and require mechanical ventilator support.
Once the paralysis affects (ascends) the muscles of breathing then we have to support their breathing with a ventilator.
When healing occurs, the paralysis descends, they regain the ability to breath effectively.
Amyotrophic Lateral Sclerosis (ALS)
AKA Lou Gehrig Disease
Affects upper and lower motor neurons of the cerebral cortex, brain stem, and spinal cord.
Whole body movement.
Prognosis is usually poor.
< 5 yr survival rate.
Patient has normal intellectual and sensory function until death.
Cognitive thinking is not changed.
Causes of ALS
Specific gene mutations (FUS gene) are under investigation as the instigators of motor neuron death.
Toxins/toxic cell byproducts.
Manifestations of ALS
Respiratory Failure
Most serious manifestation.
Progressive neuromuscular weakness in all muscles.
ALS Complications
Dysphagia Resulting From ALS
Increases the patient's risk for aspiration of food and oral secretions.
Can lead to aspiration pneumonia.
Dysfunction of the Diaphragm Muscle
Causes respiratory failure in patients with ALS.
Why does dysphagia occur in persons with degenerative neuromuscular disorders?
Occurs because of weakened esophageal muscles.
Assessment of the gag reflex is necessary before feeding a patient.
Why is assessment of respirations imperative in persons with degenerative neuromuscular disorders?
The diaphragm can weaken; therefore, assessment of respirations is also necessary.
Myasthenia Gravis
Neuromuscular Junction Disorder.
Chronic Autoimmune disease.
An IgG antibody (← autoimmune) is produced against acetylcholine receptors.
AKA anti-acetylcholine receptor antibodies.
Loss of Ach, or a blockage of Ach receptors.
Clinical Manifestations of Myasthenia Gravis
**Muscle weakness that worsens after periods of activity and improves after periods of rest.**
Ach reserves get depleted w/ increasing activity.
Weakness and fatigue of muscles of the eyes and the throat.
Causes diplopia
Difficulty chewing, talking, swallowing.
Muscles that control breathing, and neck and limb movements may also be affected.
Why is assessing respiratory function and gag reflex in patients affected with severe MG important?
The diaphragm, intercostal muscles, and swallowing muscles can be weakened or fatigued.
Gag reflex tests for dysphagia from weakening of throat muscles.
If their medication dose is not high enough or they miss a dose they could lose the ability to breath.
Diagnosing Myasthenia Gravis
Physical & Neurological Exam.
Test for bilateral weakness.
Edrophonium Test
Injections of edrophonium chloride to briefly relieve weakness.
Usually used for ocular weakness.
Blood Test
Tests for abnormally elevated levels of acetylcholine receptor antibodies.
Electrodiagnostics
Nerve-muscle stimulation.
Diagnostic Imaging
CT of the chest for thymoma
Enlarged thymus; can be curative if removed.
Pulmonary Function Testing
Predicts risk of pulmonary failure due to myasthenic crisis.
Myasthenia Gravis Therapies
Anticholinesterase (AchE) Inhibitors
Help build up acetylcholine reserves.
Immunomodulating Agents
Intravenous Immune Globulin (IVIg)
Plasmapheresis
Filters antibodies.
Thymectomy
Removal of thymus.
Myasthenia Crisis
Medical Emergency
Occurs when the muscles that control breathing weaken to the point where individuals require a ventilator to help them breathe.
Cholinergic Crisis
Medical Emergency
Caused by patient consuming too much medication.
Patient has excessive cholinergic stimulation (PNS).
Leads to excessive secretions
Clinical Manifestations of Cholinergic Crisis
Cramps
Increased salivation
Lacrimation
Muscular weakness
Paralysis
Muscular fasciculation
Diarrhea
Blurry vision
Dementia
Progressive failure of cerebral functions that is not caused by an impaired level of consciousness.
Alzheimer's most common.
What are the 4 types of Non-Alzheimer’s Dementia?
Lewy Body
Vascular
Frontotemporal
Creutzfeldt-Jakob
Lewy Body (Non-Alzheimer's Dementia)
Lewy Bodies (Protein Deposits) develop in nerve cells in the brain regions involved in thinking, memory and movement (motor control).
Vascular (Non-Alzheimer's Dementia)
Decline in thinking skills.
Caused by conditions that block or reduce blood flow to the brain.
Deprives brain cells of vital oxygen and nutrient.
Creutzfeldt-Jakob (Non-Alzheimer's Dementia)
Caused by a prion.
Quickly fatal.
Alzheimer's
Familial Alzheimer’s
Genetic
Early (50’s) and late (70’s) onset.
Nonhereditary Alzheimer’s
Sporadic, late onset.
Theories of Manifestation
Mutation for encoding amyloid precursor protein.
Creation of amyloid plaque.
Alteration in apolipoprotein E.
Loss of neurotransmitter stimulation of choline acetyltransferase.
Inadequate sleep.
Neurofibrillary tangles & Senile plaques
Only found post-mortem.
Clinical Manifestations of Alzheimer's
Forgetfulness
Emotional upset
Disorientation
Confusion
Lack of concentration
Decline in abstraction, problem solving, and judgment
Diagnosing Alzheimer’s
Diagnosis is made by ruling out other causes of dementia.
Neurologist will administer the mini-mental state exam.
A series of tasks and questions focused on calculations and problem solving.
Ex) Drawing the face of a clock.