Osteoporosis and Osteosarcoma
1/475
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
476 Terms
When is the peak adult bone mass get reached?
Early 20’s to 30/35
When is the greatest amount of bone mass decline?
Immediately after menopause
What is osteopenia?
A bone condition characterized by bone loss that is not as severe as in osteoporosis
What is the definition of osteoporosis?
Osteoporosis is characterized by low bone mass, microarchitectural disruption, and skeletal fragility, resulting in decreased bone strength and increased risk of fracture
What is osteoporosis known as in the medical field?
Silent disease
When are symptoms first shown for osteoporosis?
First fracture
What is the rate of bone formation and bone resorption for osteoporosis?
Bone formation is normal and bone resorption is increased
What happens to the bone and structural integrity from osteoporosis?
Incapable of maintaining structural integrity of the skeleton due to depleted bone integrity
Name the four most common fractures from most to least frequent
Vertebral compression fracture, distal radial fracture, hip fracture, and pelvic fracture
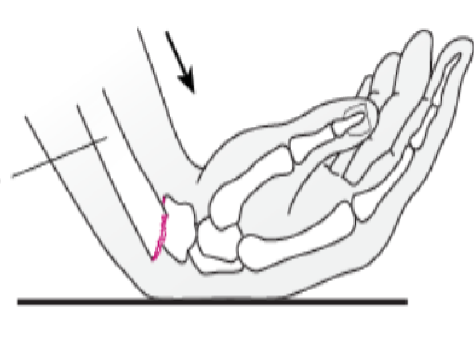
What is the main cause distal radial fractures (Abbreviation)?
FOOSH
What does FOOSH stand for?
Fall on an outstretched hand
What kind of fracture is the most life changing?
Hip fracture
What gender is most susceptible to Osteoporosis?
Women
What is a pathologic fracture?
Fragility fracture
How much trauma is needed for a fragility fracture?
Minor trauma
What is used to treat fractures?
ORIF
What does ORIF stand for?
Open reduction and internal fixation
What is primary osteoporosis?
Bone loss that occurs during the normal human aging process
What is secondary osteoporosis?
Bone loss that results from specific, well-defined clinical disorders
What are the most common risk factors for osteoporosis (the four things he listed)?
Aging, taking corticosteroid, alcohol, and post menopausal
What is the main cause of secondary osteoporosis?
Taking corticosteroids
What medications increase your chance of osteoporosis?
Steroids, thyroid medications, hormone suppressants (Lupron), and cancer treatment
What medical conditions increase your chance of osteoporosis (One of my answerers are different than the packet, he misspelled something)?
Rheumatoid arthritis, eating disorder, hyperthyroidism, hyperparathyroidism, and osteogenesis imperfecta
What are all the symptoms of osteoporosis?
Asymptomatic
What is the quote from Rosen and Drezner about symptoms?
Osteoporosis has no clinical manifestation until there is a fracture. This is an important fact because many patients without symptoms incorrectly assume that they must not have osteoporosis.
What is the first kind of diagnosis for osteoporosis (diagnosis A)?
Fragility fracture, particularly at the spine, hip, wrist, humerus, rib, and pelvis
What is the second kind of diagnosis for osteoporosis (diagnosis B)?
T-score -2.5 or higher standard deviations at any site based upon bone mineral density measurement by DXA scan
When can a clinical diagnosis of osteoporosis?
If there is a elevated rick for fracture
Give me all the classifications and the T-score involved (classification T-score, classification T-score, …).
Normal -1.0 or greater, Osteopenia between -1.0 and -2.5, osteoporosis -2.5 or less, and severe osteoporosis -2.5 or less with fragility fracture
Give me to T-scores and when to repeat a DXA scan (T-score frequency, T-score frequency, …).
-1.0 to -1.5 every 5 years, -1.5 to -2.0 every 3-5 years, and under -2.0 every 1-2 years
What population is a T-score based on?
Young adult
What population is a Z-score based on?
Age-matched population
What is T-score and Z-score based on (from the patient, and no abbreviation)
Bone mineral density
What Z-score should prompt careful scrutiny for coexisting problems?
-2 or lower
What does DXA stand for?
Dual-energy x-ray absorptiometry
What is the gold standard for evaluation of bone density?
DXA scan
What are DXA scans used to determine the density of?
Lumbar spine and hip
What does a DXA scan deliver?
Negligible radiation with an accuracy that is considerate
What lifestyle factors contribute to bone loss?
Smoking, excessive alcohol, physical inactivity, and poor nutrition
Most of the conditions can causing osteoporosis can be excluded with a what?
Careful history and physical examination
What should be measured in a physical examination for osteoporosis?
Height and weight
What does FRAX stand for?
Fracture risk assessment tool
What does FRAX estimate?
10-year probability of hip fracture and major osteoporotic fractures for untreated patients between ages 40 and 90
X-rays are ___________ to the detection of osteoporosis unless very severe or if there is an acute fracture?
Very insensitive
What are the baseline laboratory tests that are performed to judge the risk of osteoporosis?
Thyroid function, vitamin D assessment, serum protein electrophoresis, 24-hour urine calcium, testosterone level, and LH and FSH
Where do we get vitamin D
Sun
What is vitamin D good for when dealing with osteoporosis?
Calcium absorption
Where do we absorb calcium for vitamin D?
Small intestine
Write the quote from the International Osteoporosis Foundation (I learned he likes to use names just like the way I worded this question, so make sure you know who wrote the thing, so you know what to write)
Osteoporosis, which literally means porous bone, (porous bone matrix) is a disease in which the density and quality of bone are reduced (bones are brittle, porous, and prone to fracture). As bones become more porous and fragile, the risk of fracture is greatly increased. The loss of bone occurs silently and progressively. Often there are no symptoms until the first fracture occurs.
What is the quote from Rosen and Drezner from UpToDate about diagnosis (I heard we need to know quotes, which they got one of last year, this one, and a few others are important due to boldness and highlighting)?
Early diagnosis and quantification of bone loss and fracture risk are important because of the availability of therapies that can slow or even reverse the progression of osteoporosis
What are the signs of a hip fracture?
One leg shorter and externally rotated
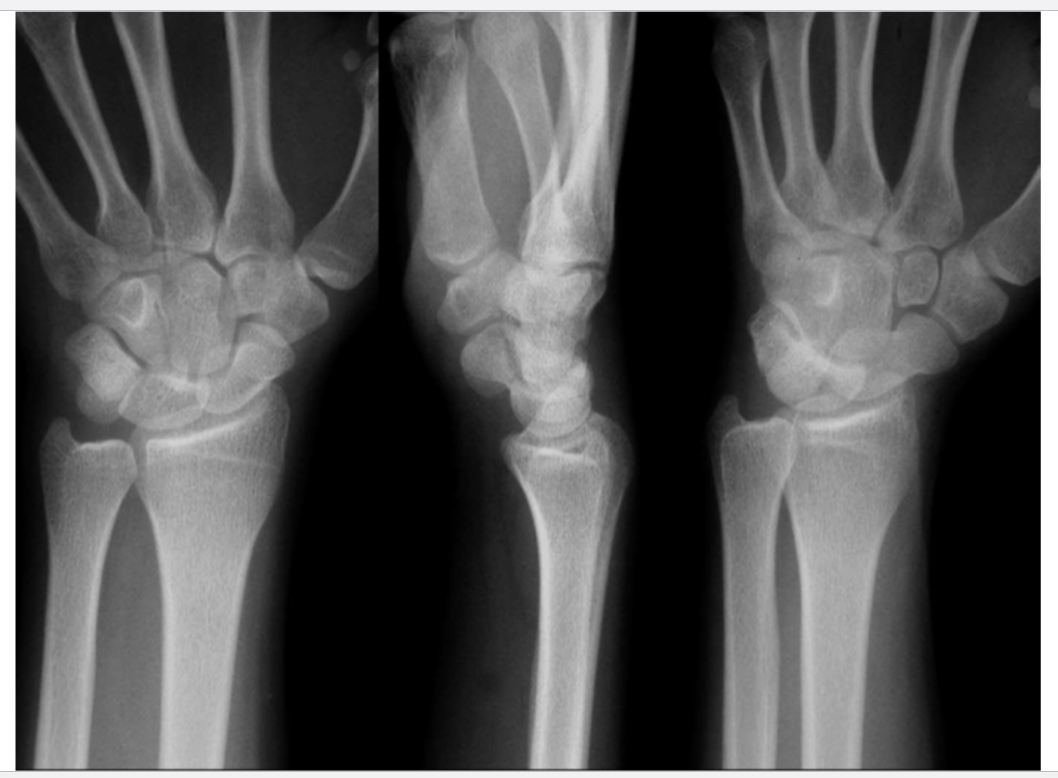
What is this?
Normal
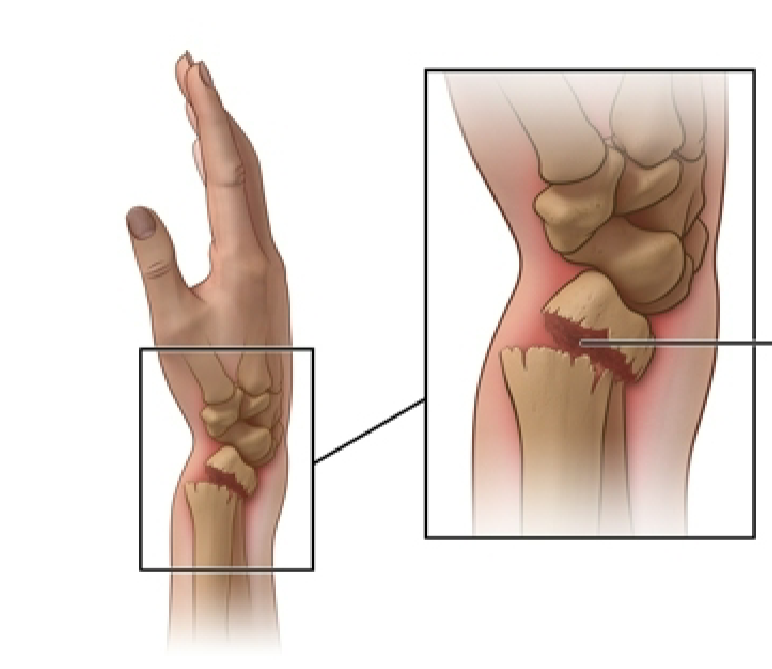
What is this?
Colles fracture

What kind of fracture would this lead to?
Colles fracture

What is this?
Colles fracture

What is this?
Smith fracture
What is this?
Smith fracture

What is this?
Smith fracture

What does this show?
Vertebral compression fracture

What is this?
Growth plates

What is this?
Cast treatment

What is this?
External fixation
What is it called when you fix a distal radial fracture without opening the skin?
Closed reduction
What are the nutritional and lifestyle modifications that can be done to prevent osteoporosis?
Diet should be adequate in protein, total calories, calcium, and vitamin D, corticosteroid doses should be reduced or discontinued if possible, high impact physical activity (jogging) significantly increases bone density in both men and women, stair climbing increases bone density in women, weight training (increase muscle strength as well as bone density), and fall avoidance
List 5 high calcium foods (he asked this question as if it’s going to be an exam question, and you can remember this or other things if you find it easier).
Milk, yogurt, cheese, sardines, and salmon
What is the most important preventative lifestyle change for osteoporosis?
Fall avoidance
What are some things you can remove or be watchful for to decrease your chance of falling?
Loose rugs, cluttered floors, pets underfoot, wet or cracked paving, ice, and snow
What are things you can install and use to decrease your chance of falling?
Handrails on stairs, handholds in bathroom, and use of cane or walker
What are things you can do to decrease your chance of falling?
Balance exercises and avoiding smoking and alcohol
What increases your chance of falling?
Impaired vision (cataracts) and footwear with slipper soles or high heels
How long could an elderly patient fall down for until someone finds them?
Hours
What should you be concerned about when someone has fallen and laid down for hours?
Rhabdomyolysis
What is Rhabdomyolysis
Breakdown of damaged skeletal muscle
In rhabdomyolysis, what does the skeletal muscle breakdown cause?
Release of myoglobin into the bloodstream
In rhabdomyolysis why is too much myoglobin in the blood bad?
It can cause kidney damage
What does myoglobin do?
Stores oxygen in your muscles
What are three signs of rhabdomyolysis?
Dark or tea colored urine, increase BUN/Cr, and EKG changes
When should pharmacologic intervention happen in postmenopausal women and men 50 years and older?
History of hip or vertebral fracture, T-score of -2.5 or less at the femoral neck or spine (after appropriate evaluation to exclude secondary causes), and a T-score between -1 and -2.5 at the femoral neck or spine with a 10-year probability of hip fracture of 3% or higher or a 10-year probability of any major osteoporosis-related fracture of 20% or higher.
What is the first line of therapy for osteoporosis?
Bisphosphonates
Who is indicated for Bisphosphonates?
Patients with DXA of -2.5 or higher in spine, hip, or femoral neck or fracture of spine or hip
What is the MOA for bisphosphonates?
Inhibit osteoclast-induced bone resorption
What do bisphosphonates do for the person?
Increase bone density significantly and reduce the incidence of both vertebral and non-vertebral fractures
To ensure intestinal absorption when and how should bisphosphonates be taken?
In the morning with at least 8 ounces of water and at least 40 minutes before consumption of anything else
What are the three bisphosphonates?
Alendronate (Fosamax), Risedronate (Actonel), and Ibandronate sodium (Boniva)
What is the strength and frequency of Alendronate (Fosamax)?
70mg once weekly
What is the strength and frequency of Risedronate (Actonel)?
35mg once weekly
What is the strength and frequency of Ibandronate Sodium (Boniva)?
150mg once monthly
What route do bisphosphonates get taken?
Oral
What are the side effects of bisphosphonates?
Abdominal pain, heartburn, irritation of esophagus, anemia, and joint and muscle pain
What is Bisphosphonates helpful in preventing?
Corticosteroid induced Osteoporosis
What are all the pharmacological therapies for osteoporosis?
Bisphosphonates, vitamin D and calcium, calcitonin, SERMs, and estrogen/progestin therapy
Sun exposure and vitamin D supplementation are useful in preventing and treating what?
Osteomalacia
What must be added to vitamin D uptake to prevent and treat osteoporosis?
Calcium
What is the advised amount of vitamin D and calcium daily?
800mg of vitamin D and 1200mg of elemental calcium
How do you get vitamin D?
Synthesized in skin on exposure to sunlight and in foods
What are some foods that good for vitamin D uptake?
Egg yolks, fish, liver, cereals, milk, and OJ
What does vitamin D do to deal with Osteoporosis?
Absorbs calcium in the GI tract
Supplementation for calcium is recommended for what groups?
Those with low dietary intake of calcium, high risk for osteoporosis, and those with osteoporosis
What is calcitonin?
Antiresorptive medication
What does calcitonin do for people?
Reduces risk of vertebral body fractures