Formative Non-Medical Sciences
1/321
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
322 Terms
What is illness behaviour?
How people experience, define and interpret the symptoms of illness
How they interact with social networks as they try to cope with these symptoms
What are Zola's 5 triggers to consultation?
Interpersonal crisis
Perceived interference with vocational / physical activity
Perceived interference with social / personal relations
Sanctioning - pressure from others to consult
Temporalizing of symptomology - setting a personal deadline for resolving the symptoms
List the social factors which can influence utilisation of medical services (6)
gender (eg. women are more likely to consult than men)
age (eg. children and elderly people are more likely to consult than young adults and middle aged people)
social class
ethnic origin
marital status
family size
What is the biomedical model?
Assumes that all disease can be explained in terms of physiological processes
Treatment acts on the disease and not the person
The person as a whole is not considered
What is the biopsychosocial approach? (2)
Takes into account biological, psychological, social, ethnic and cultural factors
Responsibility for health and illness rests on the individual
Why is the biopsychosocial approach an improvement on the biomedical approach?
Links psychological and social factors to health explicitly opposed to assuming illness is caused purely by pathogens
Holistic
What are some criticisms of the biomedical approach? (3)
Only attributes disease to biological factors e.g. viruses and genes
It is reductionist
The biomedical model considers the patient to be a passive recipient of treatment and a victim of circumstance with no accountability for their disease.
What are some criticisms of the biopsychosocial approach?
It has over reliance on subjective outcome measures
What are the challenges of acute illness? (3)
uncertainty of illness/treatment
unfamiliar people/environments and procedures
disclosing weakness, anxiety or suffering to others
What do specific concerns of patients often reflect?
previous experience or the experience of friends/family/what's shown on media
What is outcome anxiety?
Fears of what the results of illness and treatment will be
What is procedural anxiety and what does this normally stem from?
fears about clinical procedures
inaccurate beliefs or fears about what is going to happen
What are some of the effects of anxiety and how can this be related to a clinical scenario?
-there are changes to the way in which the patient thinks and processes information eg. increased vigilance for threatening stimuli and threatening interpretations of ambiguous information
-an anxious patient's view of a clinical procedure is very different from the clinician's
Why is being depressed a common reaction to illness? (2)
illness restricts the opportunity for familiar and rewarding activities
where complete recovery is not certain, it threatens expectations about future sources of reward and fulfilment
Why do patients often feel angry?
due to the experience of disempowerment created by illness
How does anger often affect patients? (2)
patients usually direct their anger to whoever is available - clinicians and lay carers are often in the line of fire
many patients blame their illness on other people, including clinicians who they feel have failed to look after them → this impairs the clinician-patient relationship
How does illness impact a person's close relationships? (2)
people with illnesses may feel guilt about the effects of their illness on their carers
they may also feel unable to meet the expectations of others, including family and friends
Explain how self-blame can be both detrimental and beneficial
on the one hand it can lead to feelings of guilt or depression
it has also been shown than those who felt some responsibility for causing their illness in a study of recovering spinal cord injury patients, were better adjusted
List Mechanic and Volkart's triggers to consultation (4)
the frequency the illness occurs in given population
familiarity of the symptoms
predictability of the outcome of the illness
amount of threat and loss that is likely to result from the illness
What is a population-based approach?
focuses largely on health promotion activities and actions
What is an individual approach?
focuses on high-risk or affected individuals through direct interventions
Give an example of an individual approach
Weight reduction and preventing / delaying disease
(individual approach) what is meant by a secondary approach?
Secondary approach is to decrease mortality and prevalence of chronic complications in those who have already been diagnosed. Aims to identify high risk patients.
Give examples of population-based approaches (5)
-Governments "strengthen capacity for surveillance"
-Prevent and control disease by training healthcare professionals and analyse policies
-Focus on women of reproductive age (as risks of chronic diseases begins in uterus)
-Screening facilities to identify at risk individuals
-Walkways and bicycle paths near public transport to encourage daily physical activity
What is the WHO definition of epidemiology?
The study of distribution and determinants of health-related status or events (including disease)
The application of the study to control diseases and other health problems
In simple terms, what is epidemiology?
'how much' there is of a disease in the population, 'why' and 'what can be done about it'
What are the objectives of epidemiology? (5)
Identify the aetiology / cause of a disease and its relevant risk factors / transmission
Reduce mortality and morbidity
Determine extent of disease found in the community (critical for planning)
Evaluate existing and newly developed preventative and therapeutic measures
Provide foundation for delivering public policy
What is a numerator? + what is it in relation to epidemiology (3)
Upper part of a fraction
The feature which has been counted
Number of people who have developed the disease of interest
What is a denominator? + what is it in relation to epidemiology (3)
Lower part of a fraction, used to calculate a rate or ratio
The population from which the numerator was derived
Total number of people in the population at risk
What are the determinants of disease?
Physical, biological, cultural & social behaviour that influences health
What is the WHO definition of public health?
Art and science of preventing disease, prolonging life and promoting health through organised efforts of society
Give an example of a successful public health intervention (include some background)
Rapid increase in population of GB in 1800s
Caused overcrowding, poor housing and medical issues
First Public Health Act produced in 1848 leading to development of Board of Health
Towns appointed a Medical Officer of Health
1853 vaccination against smallpox made compulsory
1854 improvements in health hygiene introduced
1875 Public Health Act enforced laws about slum clearance, provision of sewers and clean water, and the removal of nuisances
What are the aims of public health?
Aim to reduce the amount of disease, premature death and discomfort and disability in the population
Describe the premise behind public health
Factors contributing to health problems are identified
Plans are drawn up to deal with them
What is incidence a measure of?
Disease risk
What is prevalence a measure of?
Disease burden
Define incidence
Number of new cases of a disease during a specific time period divided by the number of people at risk for that disease at that same period
Define prevalence
Number of infected people in the population divided by all the people in the population at specific point in time
How do you get the no. of new cases per 1000 population/no. Of new cases per 100 population
Multiply by 1000 / by 100
What is the difference between incidence and prevalence?
Prevalence also takes duration into account
What is the equation for prevalence
Prevalence = incidence x duration
How would prevalence be affected if the no. of people who die/are cured increases?
Prevalence decreases
How would prevalence be affected if fewer no. of people who die/are cured?
Prevalence increases
How do you calculate incidence?
(Number of new cases during specified period)/(Size of population at risk at the start of period)
Is prevalence a rate?
No!
What is deontology? (4)
Study of the nature of duty and obligation
Deontological ethics is the normative ethical theory that the morality of an action should be based upon whether that action itself is right or wrong upon a series of rules
Rather than based on the consequences of an action
Patient-centred, opposite to the society-centred utilitarian approach
What is consequential ethics? (2)
Anticipate likely results of an action and decide if its beneficial or harmful
Moral laws not involved
What is utilitarianism?
Looks at the greater good
What are virtue ethics? (3)
Person rather than action based
Looks at virtue / moral character of the person carrying out an action, rather than at ethical rules / duties / consequences of actions
Action is right if it is an action that a virtuous person would carry out in the samE circumstances
What is the hippocratic oath? (3)
Written by the greek physician Hippocrates
Sworn agreement made by physicians when they become doctors
Not a law but guiding principle for doctors
Outline the hippocratic oath (6)
Share knowledge with physicians that follow them
Do no harm
Doctors will not administer a deadly drug / tell someone else how to do so
Eg. conduct an abortion (this part has often been removed or rewritten in modern versions)
Being aware of their own limits
Not use their position to complete sexual acts or take advantage of their patients
Doctor-patient confidentiality
Relevance of the hippocratic oath today
Deemed the Oath as out of date for the purposes of modern medicine
New variants of the Oath are used
List the GMC ethical guidelines available (8)
Good medical practice
Confidentiality
Consent
Raising and acting on concerns
Leadership and management
Protecting young people
End of life care
Prescribing
Name and outline the first domain of good medical practice (4)
Knowledge, skills and performance
Develop and maintain your professional performance
Apply knowledge and experience to practice
Record your work clearly, accurately and legibly
Name and outline the second domain of good medical practice (4)
Safety and quality
Contribute to and comply with systems to protect patients
Responds to risks to safety
Risks posed by your health: if you know you have a serious condition that you could pass onto patients / if your judgement or performance could be affected by a condition or its treatment, consult a suitably qualified colleague + get immunised against common communicable diseases
Name and outline the third domain of good medical practice (6)
Communication and collaboration
Effective communication: listen to patients, give information in a way that they can understand, be readily accessible to patients and colleagues seeking info when on duty
Collaborating with colleagues: treat them fairly & respectfully
Teaching, training, supporting and assessing: be prepared to contribute to teaching and training doctors and students, be willing to take on a mentoring role for more junior doctors and other healthcare professionals
Continuity and coordination of care: contribute to the safe transfer of patients between healthcare providers and between health and social care providers
Establish and maintain relationships with patients: be polite, considerate + fair, work in partnership w/ patients sharing info they need to make decisions about their care
Name and outline the fourth domain of good medical practice (4)
Maintaining trust
Show respect for patients
Treat patients and colleagues fairly and w/o discrimination
Act w/ honesty and integrity
What is meant by medical professionalism?
Ensuring the well being of patients and to protect them from harm lies at the heart of medical professionalism
How can doctors maintain their medical professionalism?
Patients expect doctors to be technically competent, open and honest, and to show them respect
Demonstrating these qualities, doctors can earn the trust that makes their professional status possible
What should modern medical professionalism promote?
Actively promote engagement between doctors, patients, medical institutions and policy-makers
Outline the 4 pillars of medical ethics (4)
Autonomy
patient has ultimate control over whether they receive treatment or not
medical practitioners may not force treatment under normal circumstances
exception: when patients cannot be deemed able to reasonably make decisions for themselves
e.g. when detained under the Mental Capacity Act 2005
Beneficence:
having the best outcome for the patient in mind at all times
Non-maleficence
concise version of the Hippocratic oath
Do No Harm
Risk of an intervention should always be weighed up against the outcome of doing nothing at all
Justice
identifying whether or not an action is fair in society and within the realms of the law
What is the sick role?
Set of rights and obligations surrounding illness that could shape the behaviour of doctors and patients
Explain the importance of the sick role (2)
Provides temporary exemption from their ordinary role obligations
Provides the mechanism for returning people to health and therefore to their normal role performance
What is a potential problem with the sick role?
Sick role may become an attractive alternative to everyday pressures, providing a way of 'evading social responsibilities' and offering 'secondary gain' (interpersonal or social advantage attained by the patient as a consequence of the illness)
What are the rights and responsibilities of the sick role? (4)
Rights
exempted from normal social roles
e.g. work/family, is not responsible for their condition
Obligations
should try to get well
seek technically competent help
cooperate with medical professionals
What are the limitations of the sick role in modern society? (6)
now the unwell usually continue completely as normal in their jobs and social lives
less clear about who's responsible for adopting the sick role
patients will also be self-managing for most of their illness; requirement that they must seek + submit to medical care is looking unsound
instead of wanting to get better (impossible in many chronic diseases), patients are more concerned w/ avoiding the sick role completely
many illnesses e.g. arthritis, diabetes & asthma may never improve
sick role may be rejected for illnesses that are poorly defined or not widely accepted as valid e.g. chronic migraine
What is qualitative research? (2)
Application of logical, planned and thorough methods of collecting data and careful / thoughtful analysis
A way of doing research w/o counting because it doesn't set out to quantify or enumerate the social world or phenomena studied
Is qualitative research devoid of measurement or explanation?
-no, although qualitative research generally deals w/ speech, actions, and texts rather than numbers, you can analyse certain types of qualitative data quantitatively so qualitative analysis can offer profound and rich insights about aspects of health care and services that prove elusive to quantitative research
Give examples of qualitative approaches (2)
-if quantitative research asks 'how big is X or how many Xs are there?', qualitative research tackles questions such as 'what is X, and how do people's perceptions of X vary in different circumstances and why?'
-instead of counting the no. of suicides, which persumes that we already agree on the nature of suicide, the qualitative researcher many start by asking, 'what is suicide and how is it defined in this society?'
What is one of the key features of qualitative research?
Particularly suited to studying people in their day-to-day settings rather than in experimental or artificial ones
Outline the different qualitative methods of data collection (8)
-observing people in their own territory (non-participant observation)
-joining in (participant observation)
-talking to people (interviews, focus groups and informal chatting)
-reading what people have written (documentary analysis)
-examining objects, images and artefacts people create or use
-speech or behaviour can be collected using audio or video tapes
-textual analysis has been extended to include online conversations, forum threads and printed documents
-different qualitative methods can be combined to provide deeper insights
Outline the use of qualitative methods (5)
Insights provided by qual. research help to interpret/understand quan. data more fully
can be used independently to uncover social processes
especially valuable for understanding views and opinions
Eg. Morgan and Watkin's research on people's cultural beliefs on hypertension has helped to explain why rates of compliance w/prescribed medication vary significantly among and between white + afro-caribbean patients in south london
provides rich detail about life and behaviours inside healthcare settings
qual. methods are increasingly being used in studies of health service organisation and policy
What is a disadvantage of qualitative research?
Considerable skill is required by the researcher
What is a problem-focused approach to dealing with stress?
Targets the causes of stress in practical ways
Tackles problem or stressful situation
Give examples of problem-focused approaches (3)
problem-solving
time-management
instrumental social support
What are the advantages of a problem-focused approach? (2)
provides a long term solution
deals with root of the problem
When is a problem-focused approach not appropriate? (2)
in some cases i.e. death -> emotion-support is a better approach
doesn't work when it is beyond the person's control to remove the stress e.g. exams, work based stressors
What is an emotion-focused approach to dealing with stress? (2)
often called palliative coping
attempts to decrease emotional responses such as embarrassment, fear or depression
Give examples of emotion-focused approaches (6)
drugs that control emotion
prayer
meditation
drugs/alcohol
distraction
relaxation
What are the advantages of an emotion-focused approach? (2)
-can be an effective way of managing brief clinical challenges e.g. minor invasive procedures
-certain types of palliative coping are important in adjusting to the longer-term challenge of chronic disease e.g. seeing onself as better off than other people -> downward social comparison might help w/ emotional adjustment
What is a potential problem with an emotion-focused approach?
-can also include psychological defence mechanisms which can include potentially destructive responses such as venting frustration on other people or becoming angry w/ other people + can include denial
What is mortality rate?
-a measure of the frequency of death in a defined population during a specified interval
What must be specified in any mortality rate?
time must be specified in any mortality rate
Write down the calculation that would be required to determine the annual all-cause mortality rate per 1000 population
No. of deaths from all causes in 1 year/number of people in the population at mid year (because population changes over time) x 1000
Write down the calculation that would be required to determine the annual mortality rate per 1000 population for adults 30-40 years of age
No. of deaths from all causes in 1 year in adults 30-40 years of age/ no. of 30-40 year olds at mid year x1000
Write down the calculation that would be required for annual mortality rate per 1000 from heart disease
No. of deaths from heart disease/no. Of people in the population at mid year x1000
Write down the calculation that would be required for the annual mortality (per 1000 population) from heart disease in adults 30-40
No. of deaths from heart disease in people 30-40 in 1 year/no. Of 30-40 year olds at mid year x1000
What is case-fatality rate?
Proportion of people who have a disease and who are dying from it in a specified time period
What is case-fatality a measure of?
Disease severity
What would be the calculation for determining the case fatality rate in heart disease patients?
No. of deaths during a specific time period after heart disease onset or diagnosis/ no. of people with heart disease in that specific period
What can case-fatality be useful in measuring?
-the benefits of a new drug or intervention
What is a potential limitation of the numerator (case-fatality)?
-numerator should be restricted to deaths from that disease though it is not always easy to distinguish between deaths from that disease and other causes
What should ideally be used as the beginning of a specified time period and why is this not always feasible? (case-fatality)
-the date of disease onset should be the beginning of the specified time period but date of disease onset is often hard to standardise since many diseases develop insidiously (without symptoms) over a long period of time -> more often, the date of disease diagnosis is used
What is proportionate mortality?(2)
-provides a quick look at relative contribution of the different causes of death
-by itself, it is not a measure of risk -> you need to know total mortality rate
Write the calculation that would be used to determine the proportionate mortality of heart disease
No. of deaths from heart disease/total deaths x 100
Outline what a cohort study is (2)
-compare exposed and unexposed people
-we compare the incidence of disease in exposed and unexposed individuals
What are the advantages of carrying out a cohort study? (3)
desirable when the exposure of interest is rare
in a case-control study we are unlikely to identify a sufficient no. of exposed people when we are dealing with a rare exposure
incidence in both exposed and unexposed groups can be calculated so we can directly calculate relative risk
time sequence can be calculated
What are the disadvantages of carrying out a cohort study? (4)
-usually require large populations
-greater potential bias for assessing the outcome is present in comparison to case-control studies
-becomes impractical when the disease under study is rare
-high cost
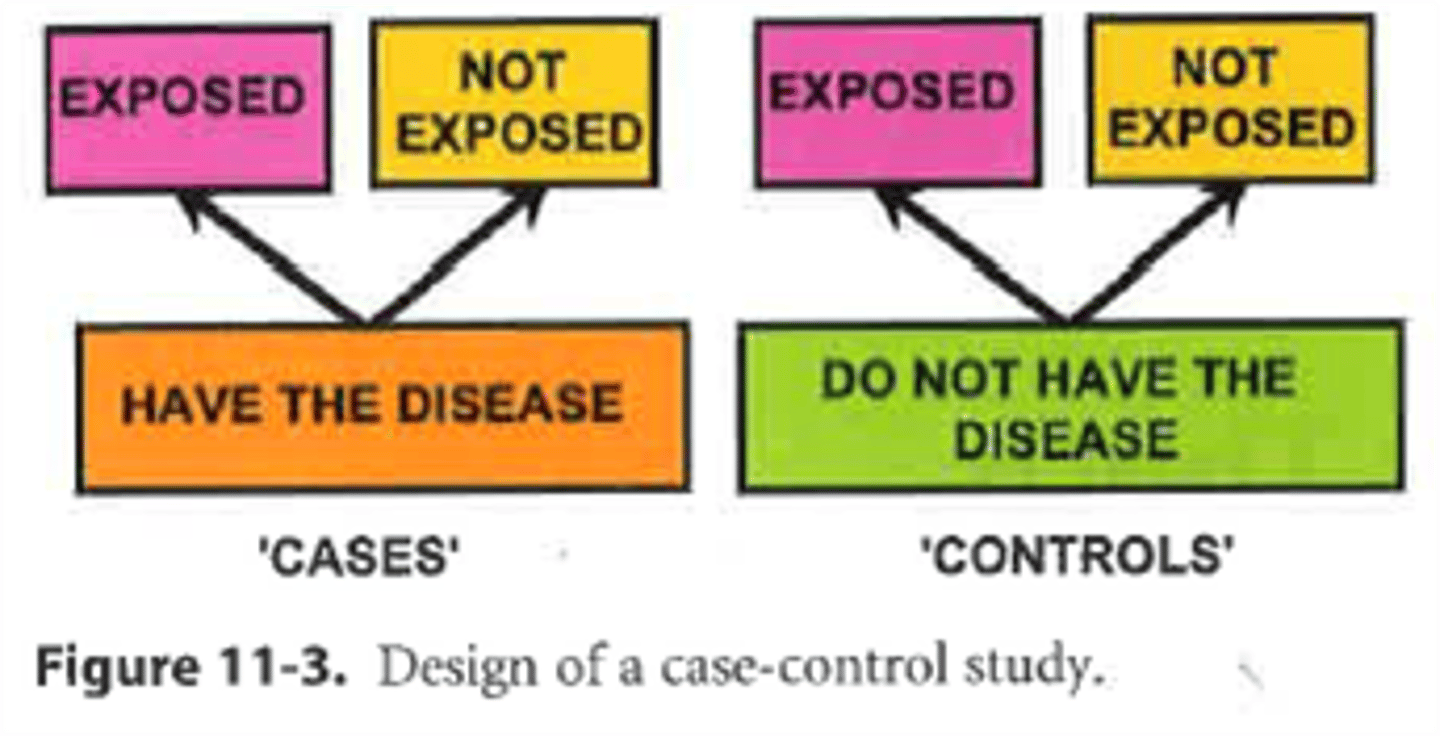
Outline what a case-control study is? (2)
-people with the disease (cases) and without the disease (controls) are compared
-we compare the proportions exposed in people with the disease and in people without the disease
What are the advantages of a case-control study? (4)
-relatively inexpensive
-require a relatively small no. of subjects for study
-desirable when disease occurrence is rare- if a cohort study were performed in such a circumstance, a tremendous no. of people would have to be followed to generate enough people with the disease for study
-we begin with cases and controls so we can study more than one possible etiologic factor and we can explore interactions among the factors