Digestive System Glands (LIVER HISTOLOGY)
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
What should a healthy liver look like on a macroscopic level?
- smooth
- consistent color
How large is the liver and how much does it weight?
The liver is the largest gland in the body: 1.5 kg
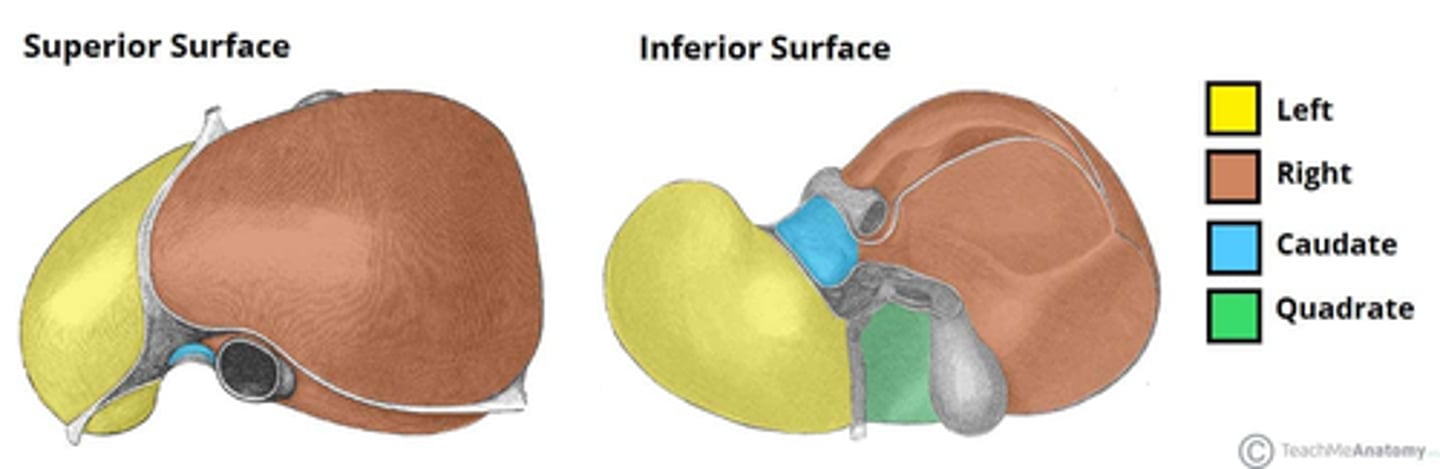
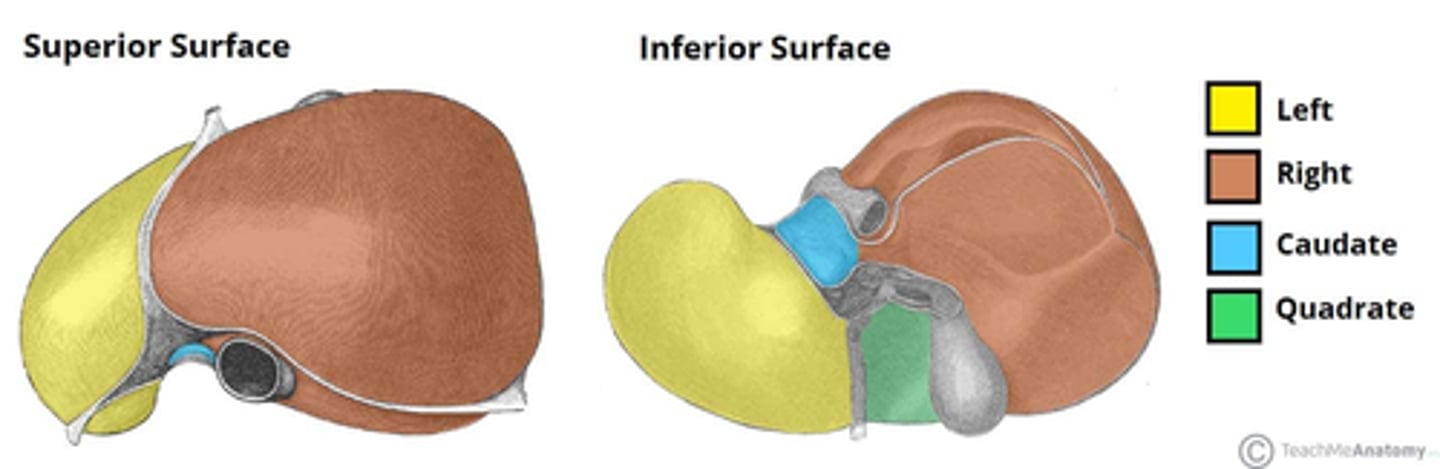
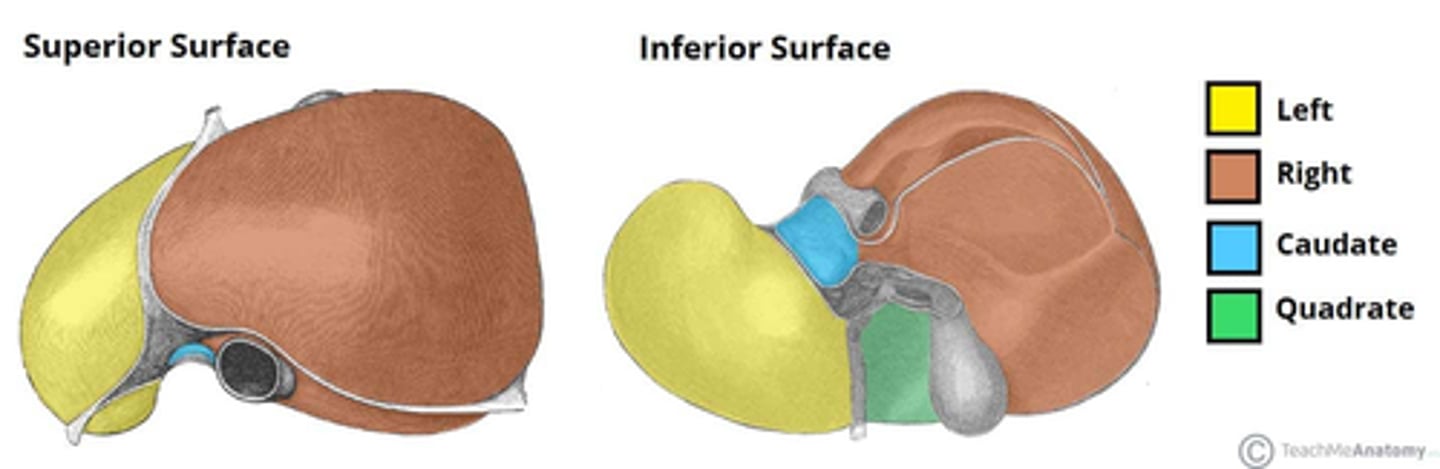
How is the liver structurally organized?
The liver is organized into four lobes:
1. right lobe
2 left lobe
3. caudate lobe
4. quadrate lobes
+ and several other lobules.
This structure is created by septa originating from the Glisson capsule.
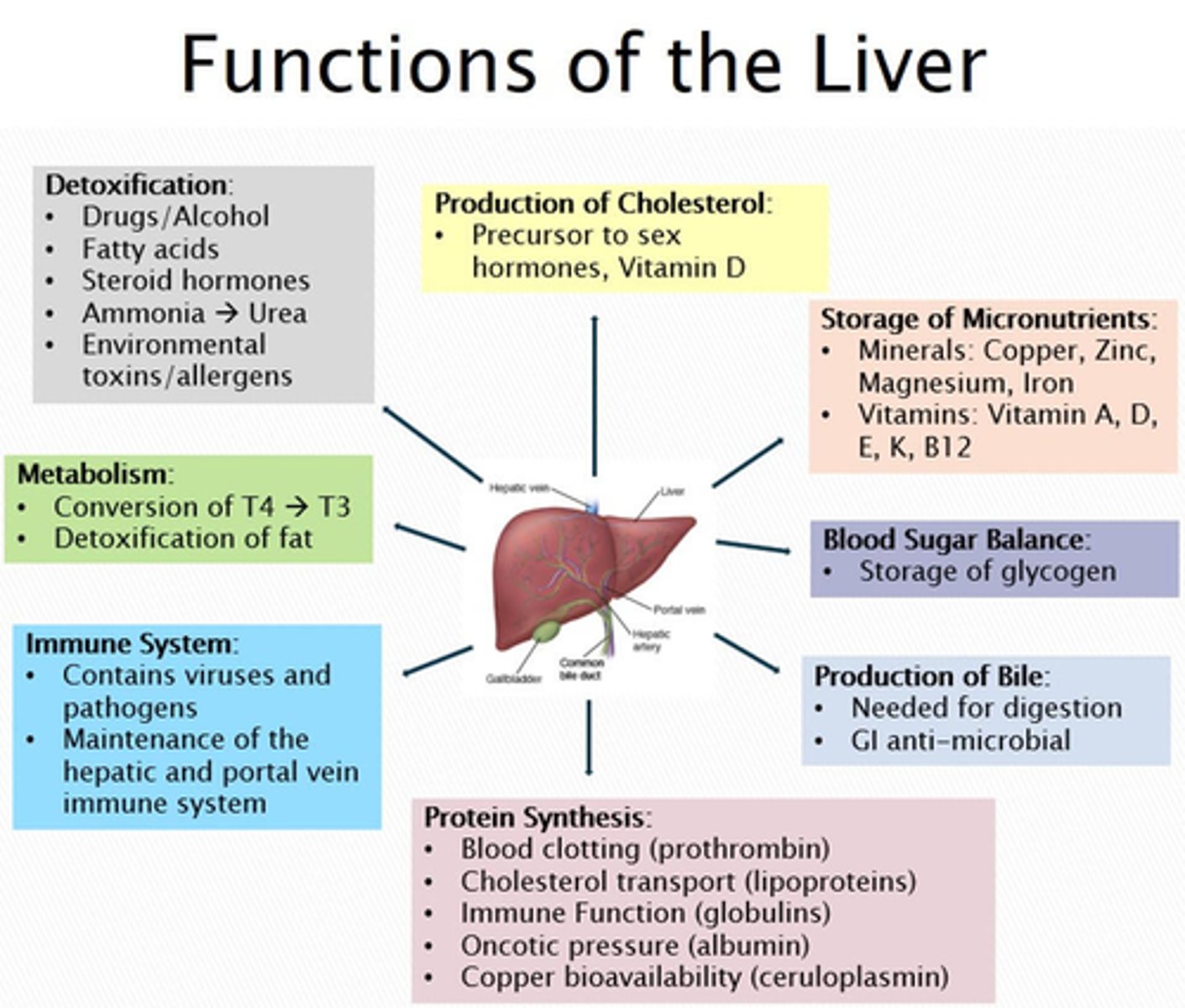
What is the primary function of the liver?
1. Production of bile
2. Synthesis of plasma proteins
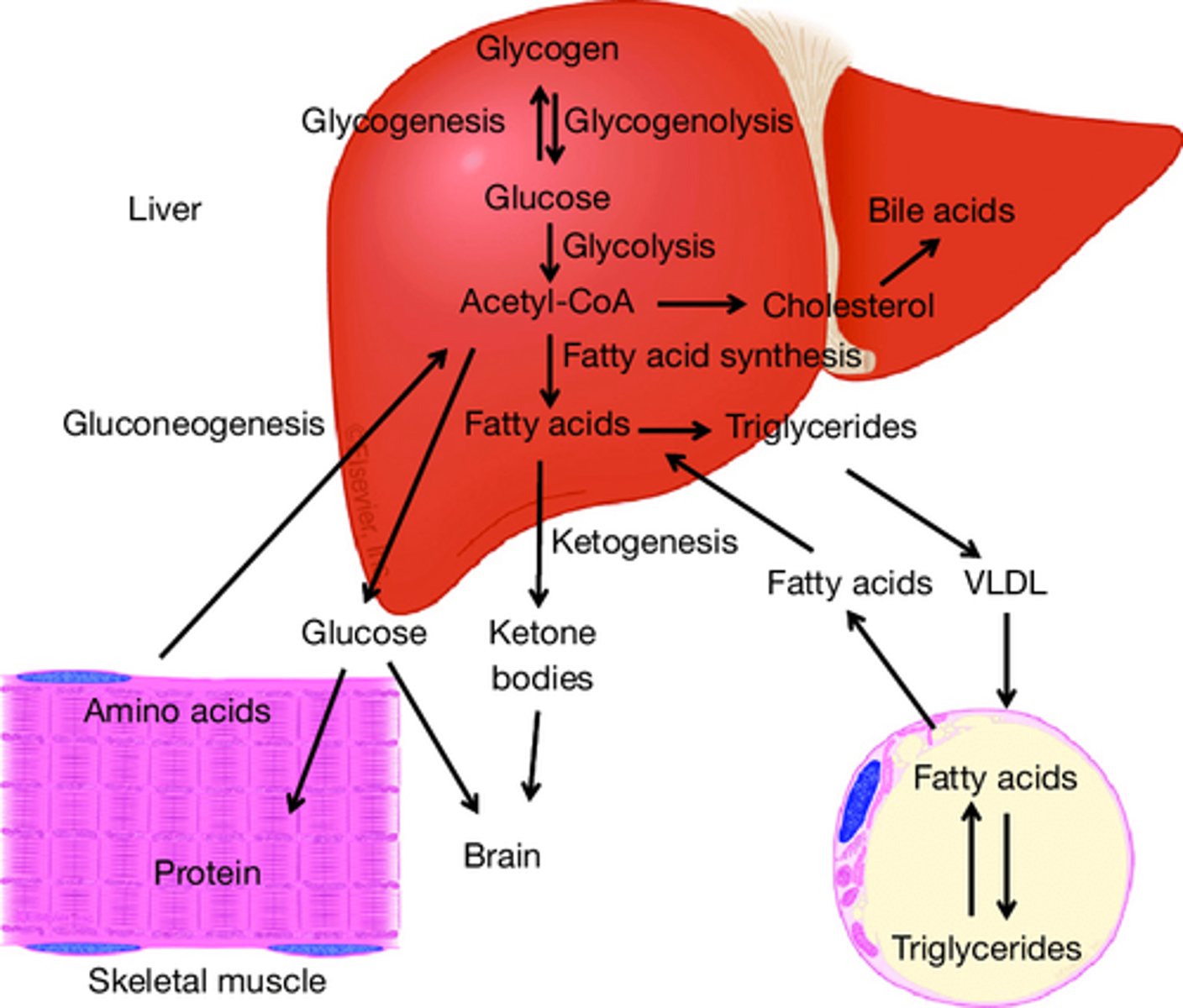
3. Metabolism of carbohydrates, fats, and proteins
4. Detoxification of various substances
5. Storage of nutrients, including vitamins and minerals
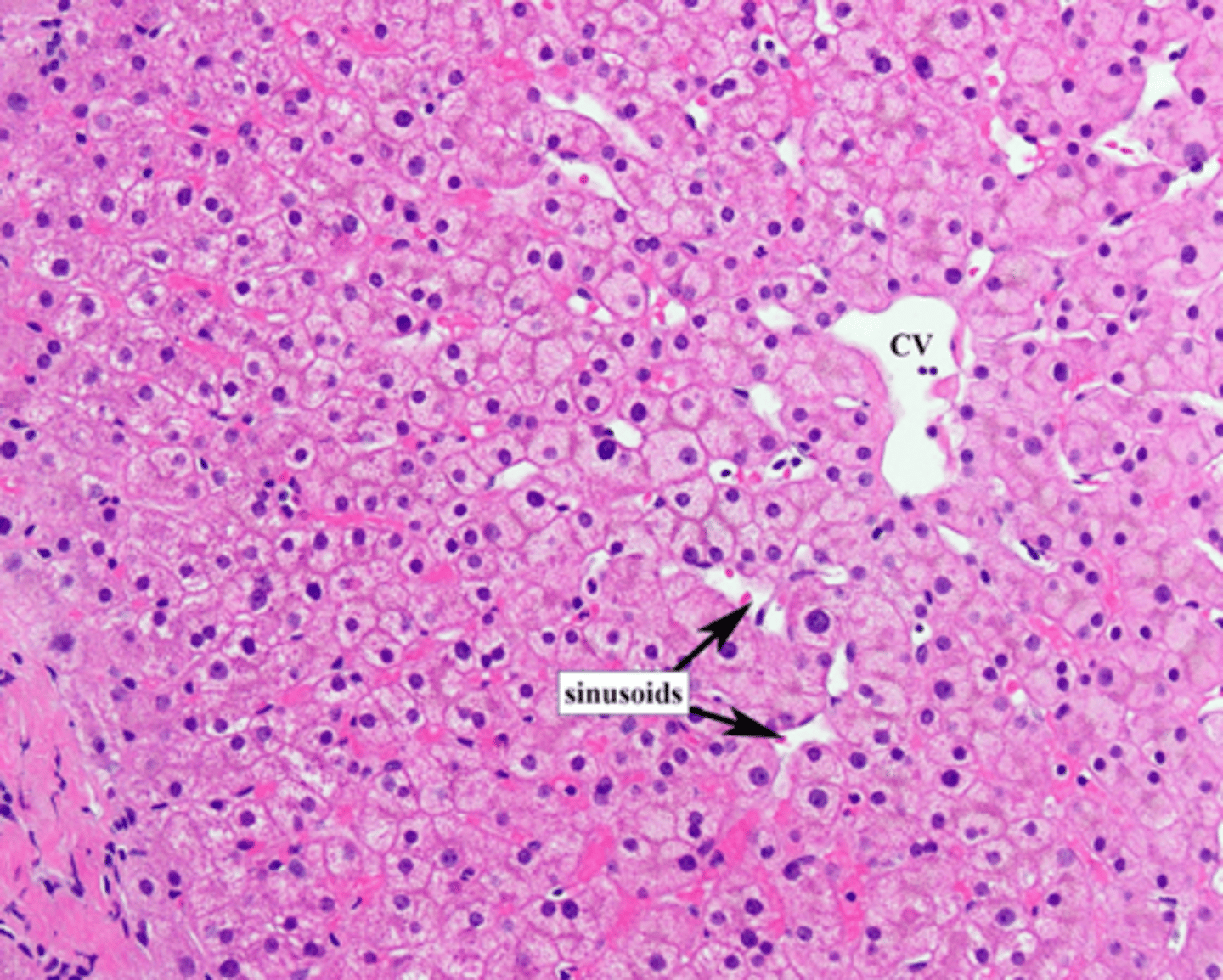
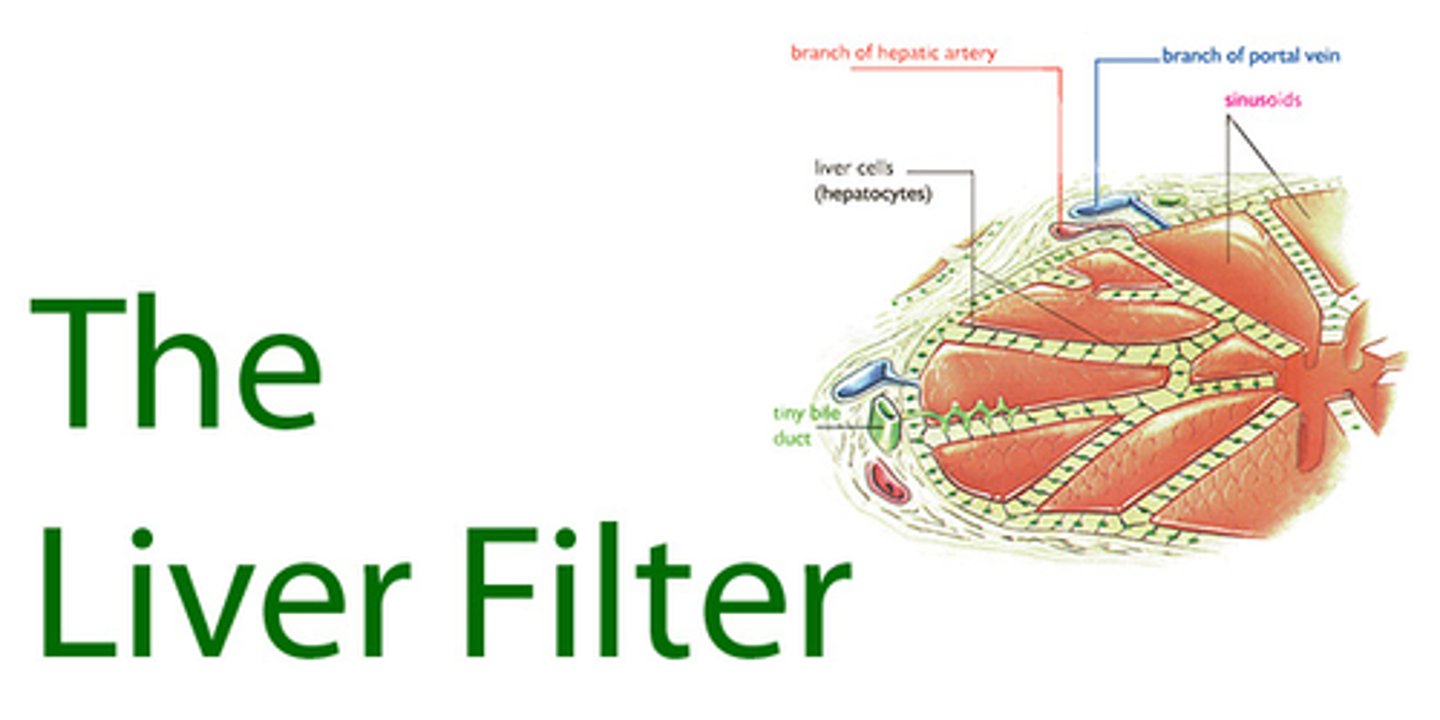
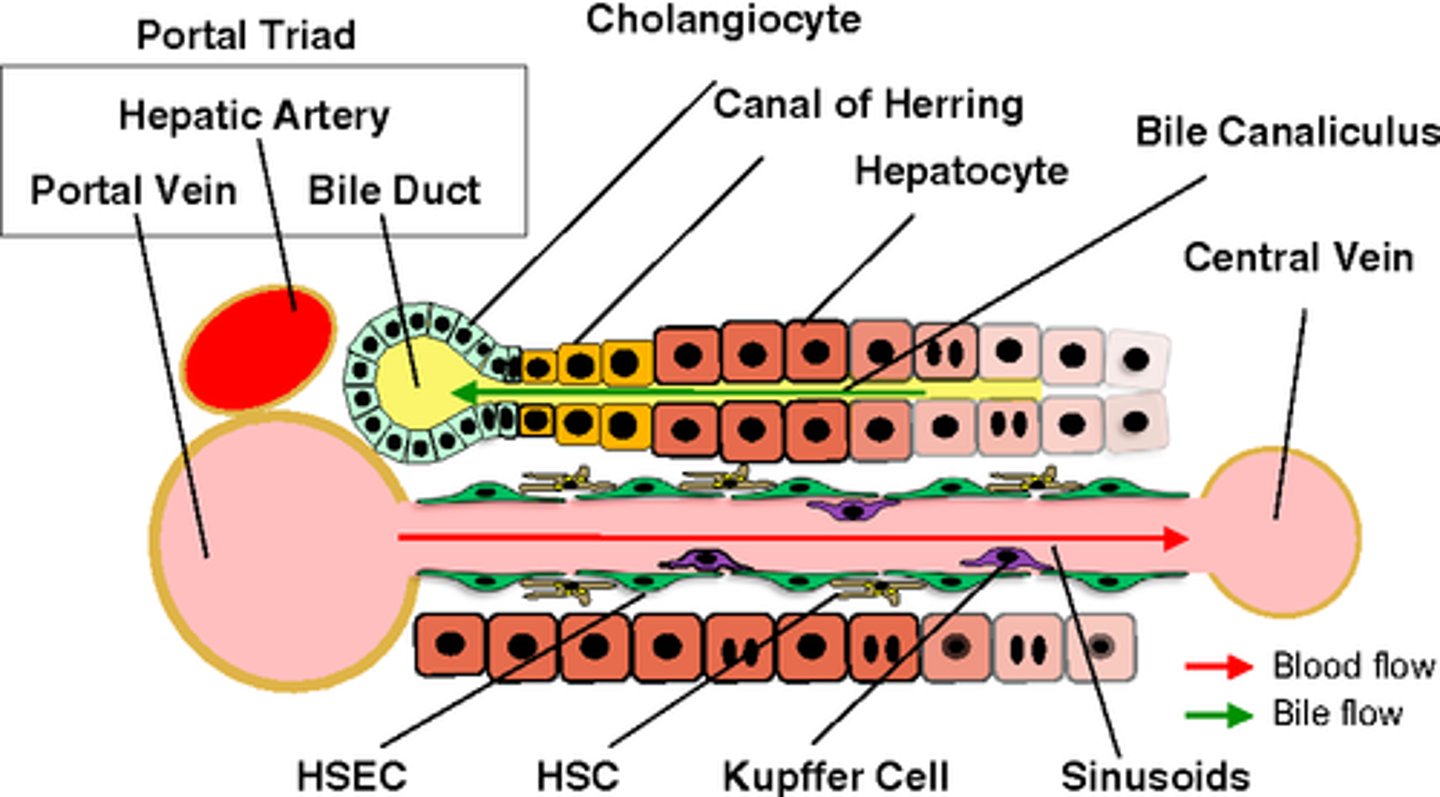
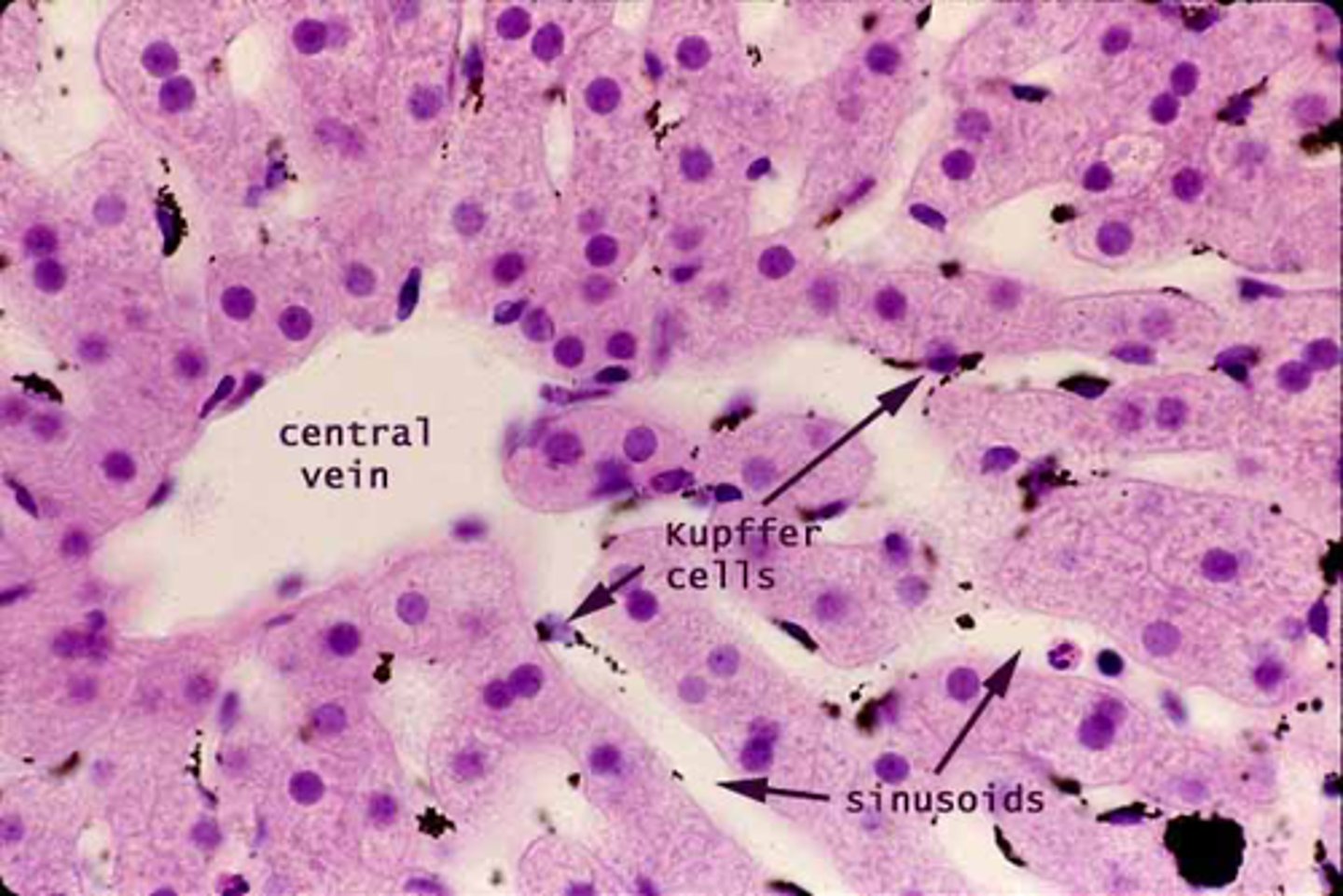
What are sinusoids in the liver?
specialized capillaries lined with fenestrated endothelial cells
the endothelial fenestrations the liver capillaries allow the transfer of small molecules and hence the function of filtration for hepatocytes

What does 'fenestrated' mean regarding liver sinusoids?
Fenestrated means the endothelial cells have small pores, facilitating filtration—an essential liver function.
Endothelial cells lining sinusoids have large fenestrations without diaphragm and lack basal lamina, allowing for efficient exchange between the blood and liver cells.
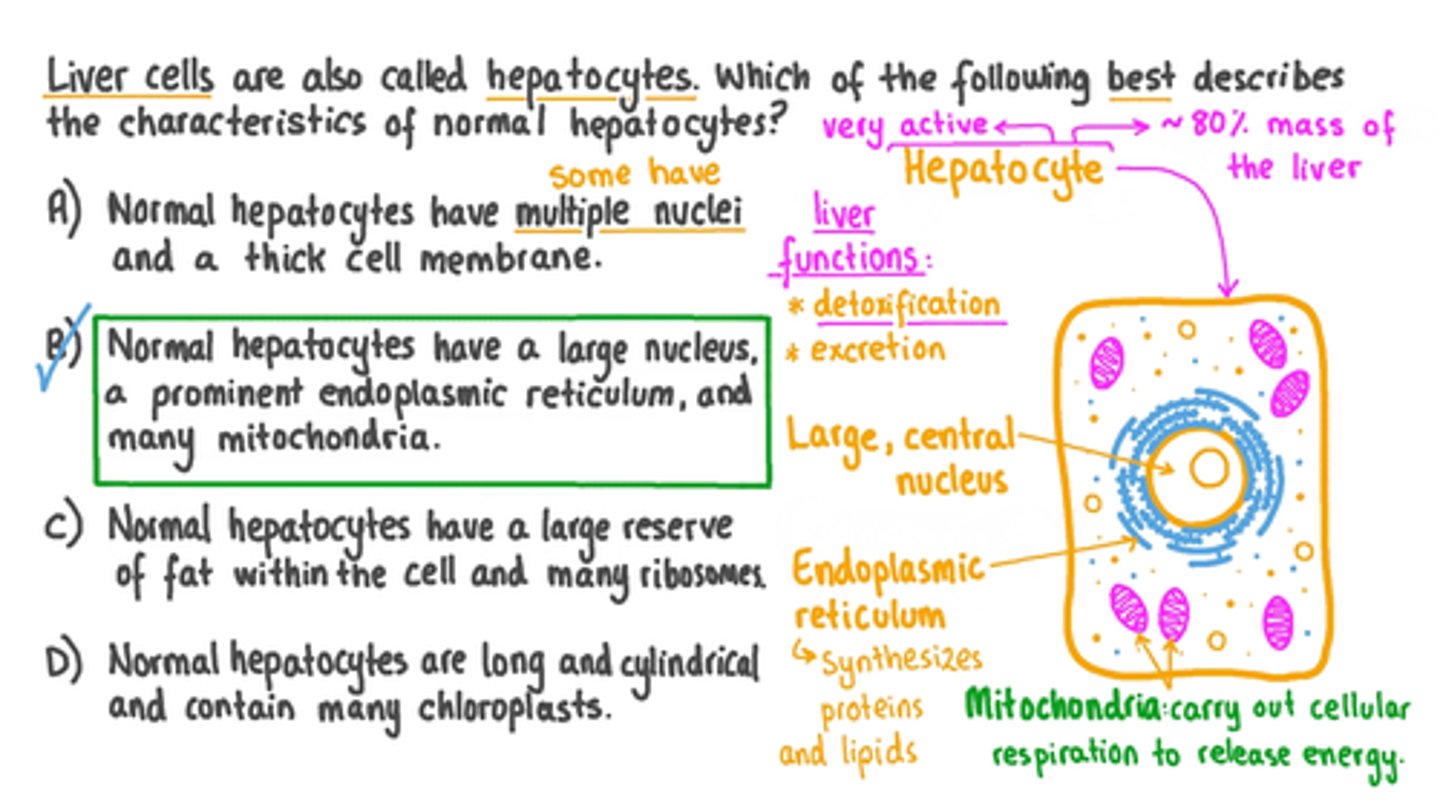
What are hepatocytes?
Hepatocytes are the functional cells of the liver, involved in processing substances in the blood.
What is the capsule of the liver?
The capsule is the outer surface of the liver composed of fibrous/connective tissue, covered by mesothelial cells from the peritoneum (liver: intraperitoneal).
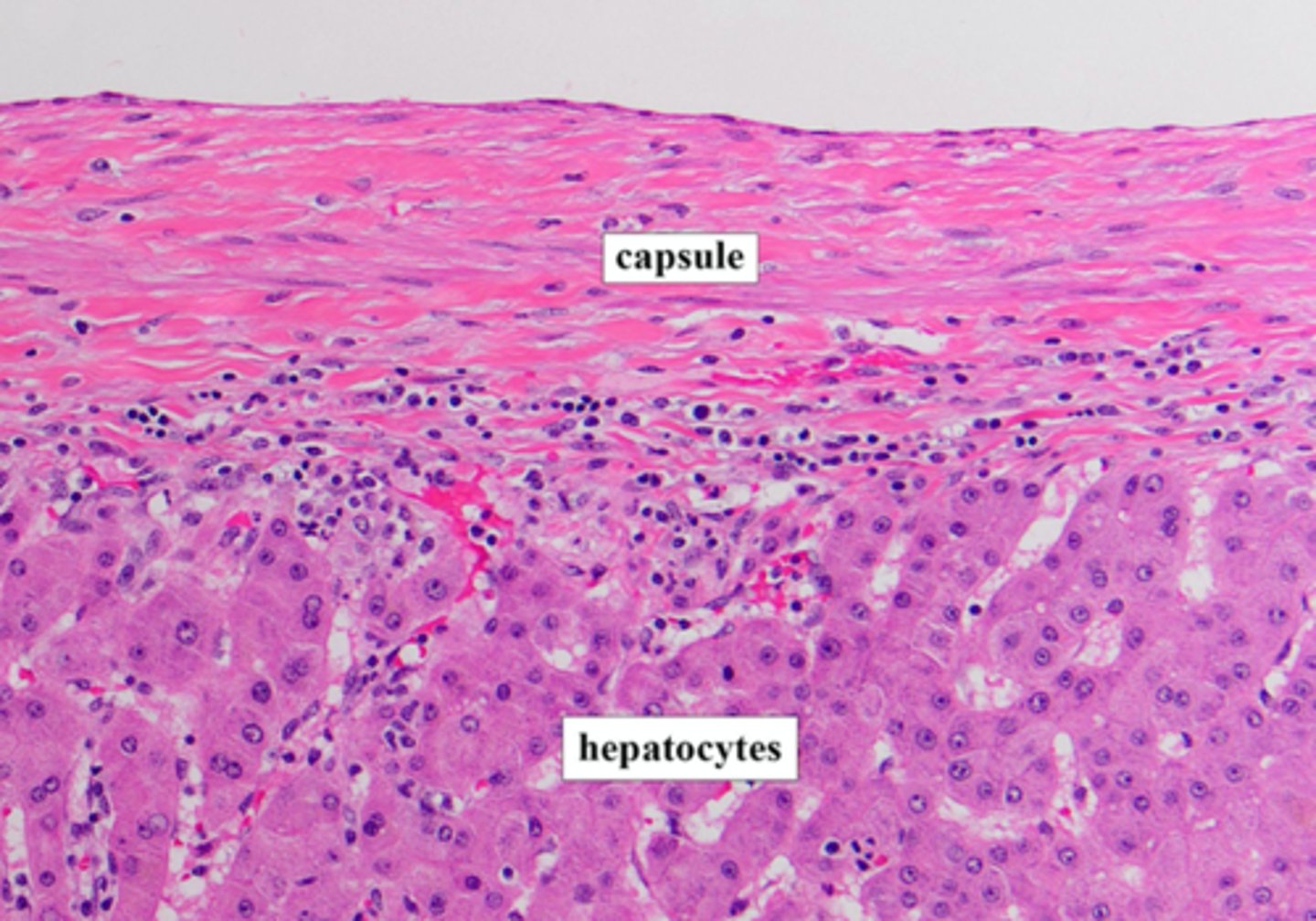
What cells cover the outermost surface of the liver?
The outermost surface (capsule) of the liver is covered by mesothelial cells that arise from the peritoneum.
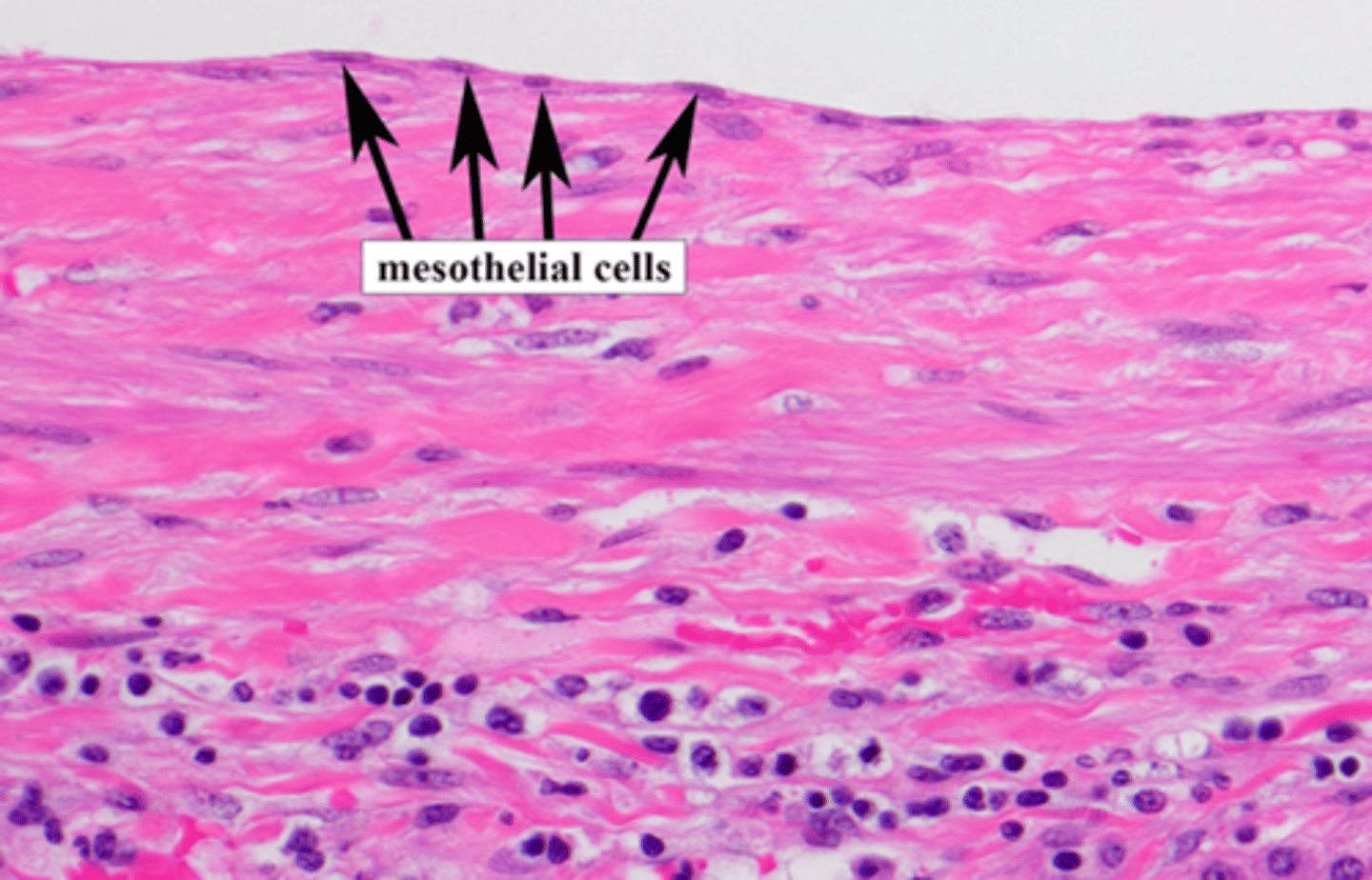
What is the name of the capsule which surrounds the liver and is covered by mesothelial cells (peritoneum)?
Glisson capsule
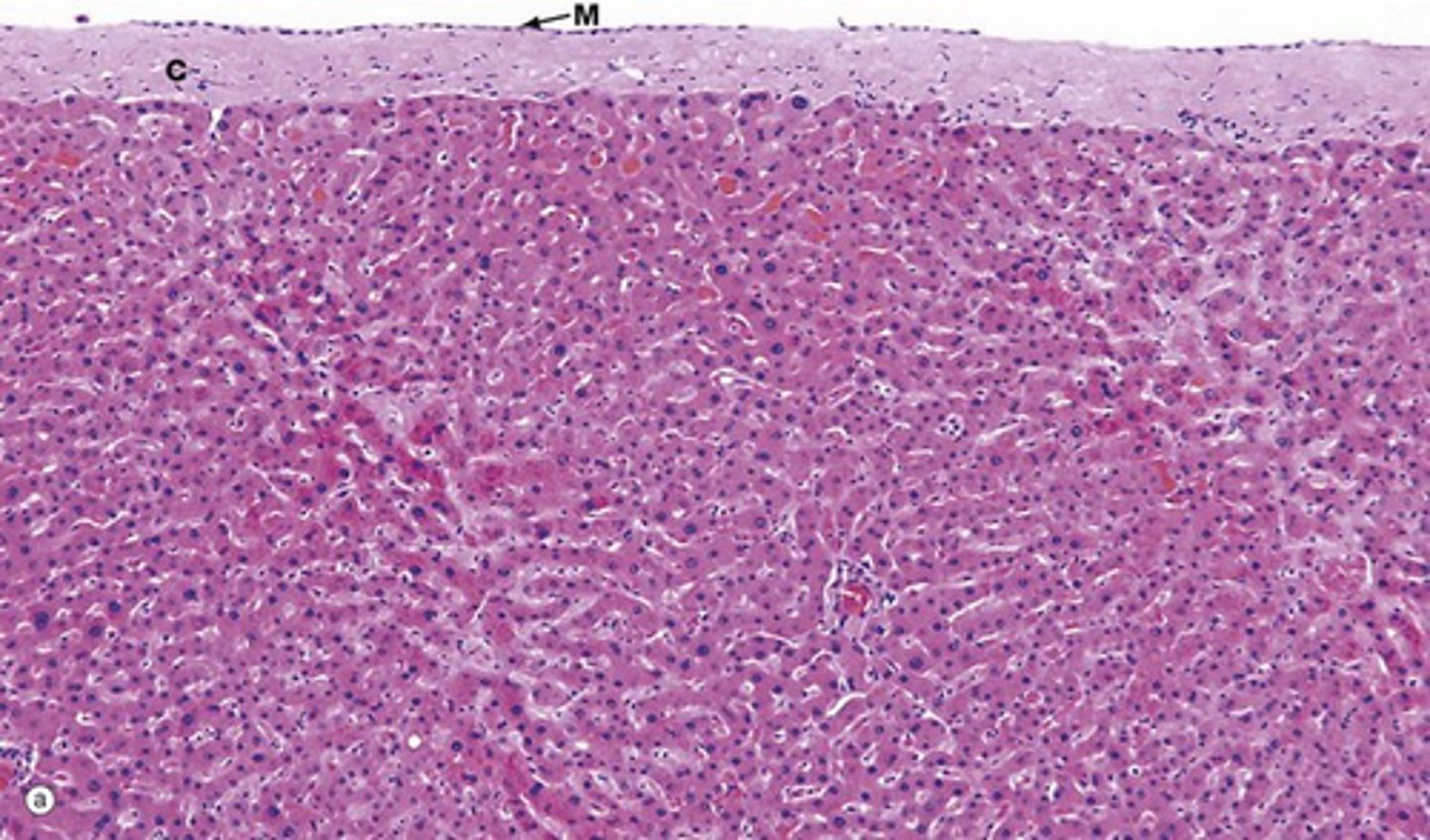
What is the parenchyma of the liver?
The Glisson capsule surrounds the liver parenchyma (bulk of liver), composed of hepatocytes.
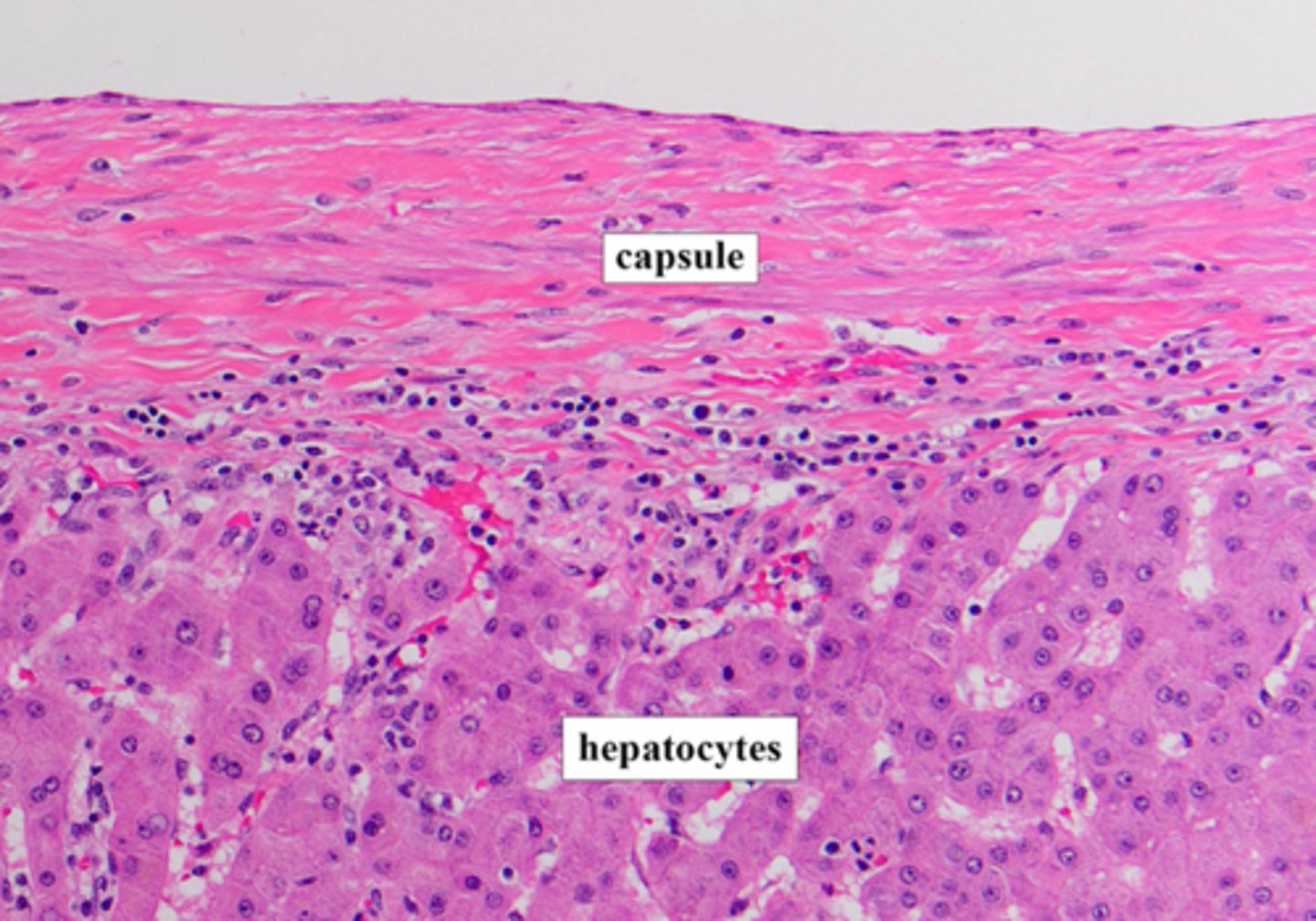
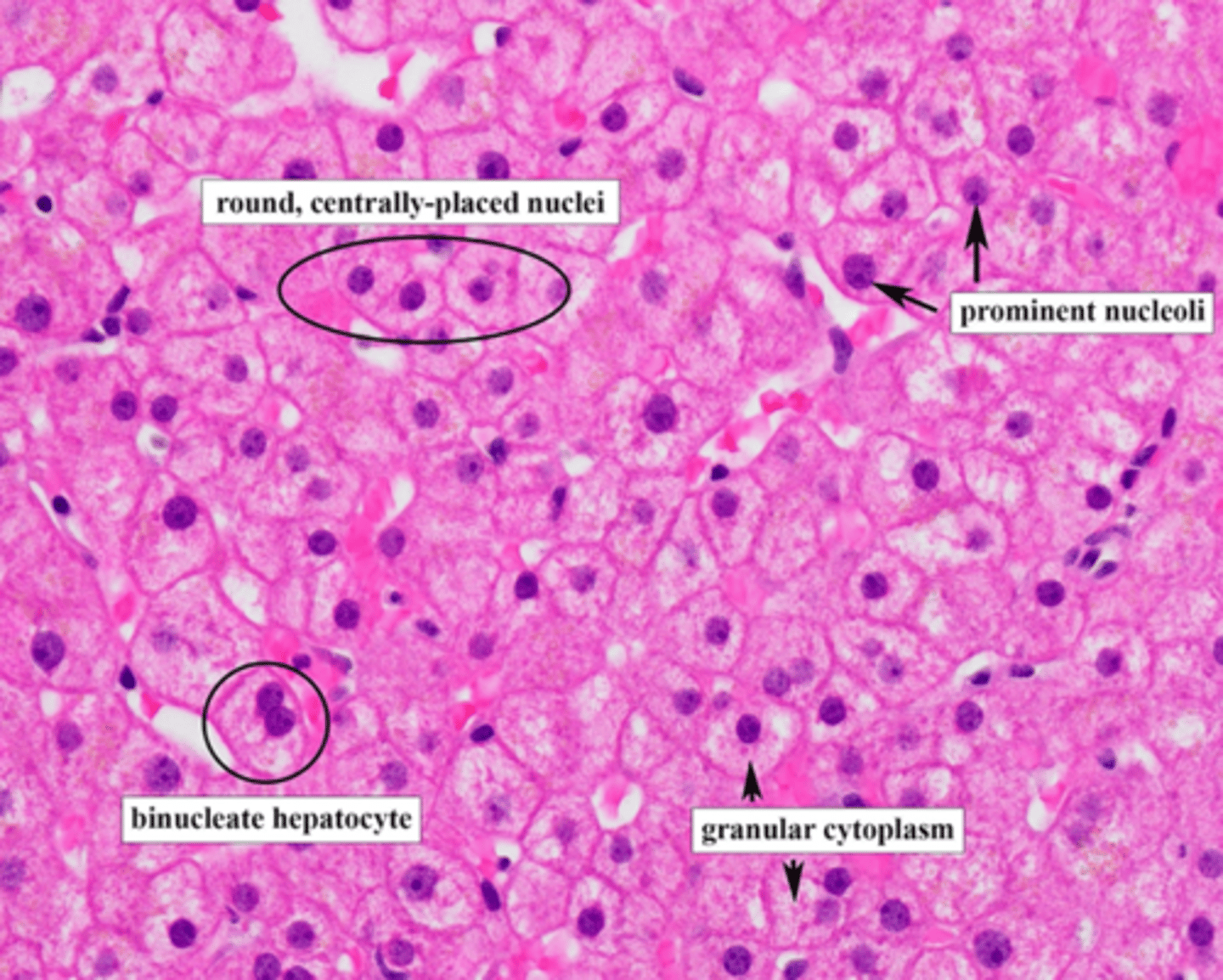
Describe hepatocytes:
1. large polygonal cells
2. eosinophilic cytoplasm (pink)
3. round nuclei

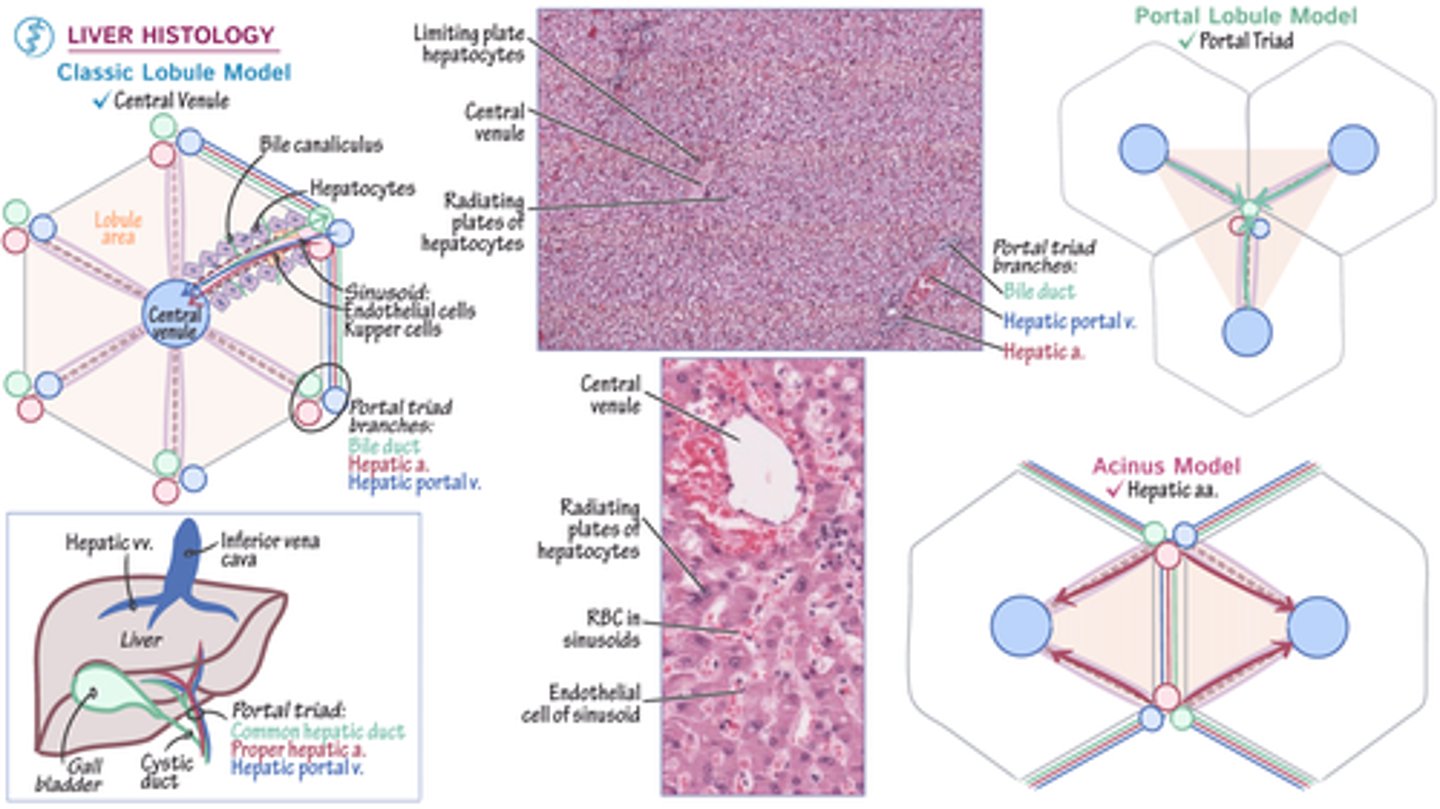
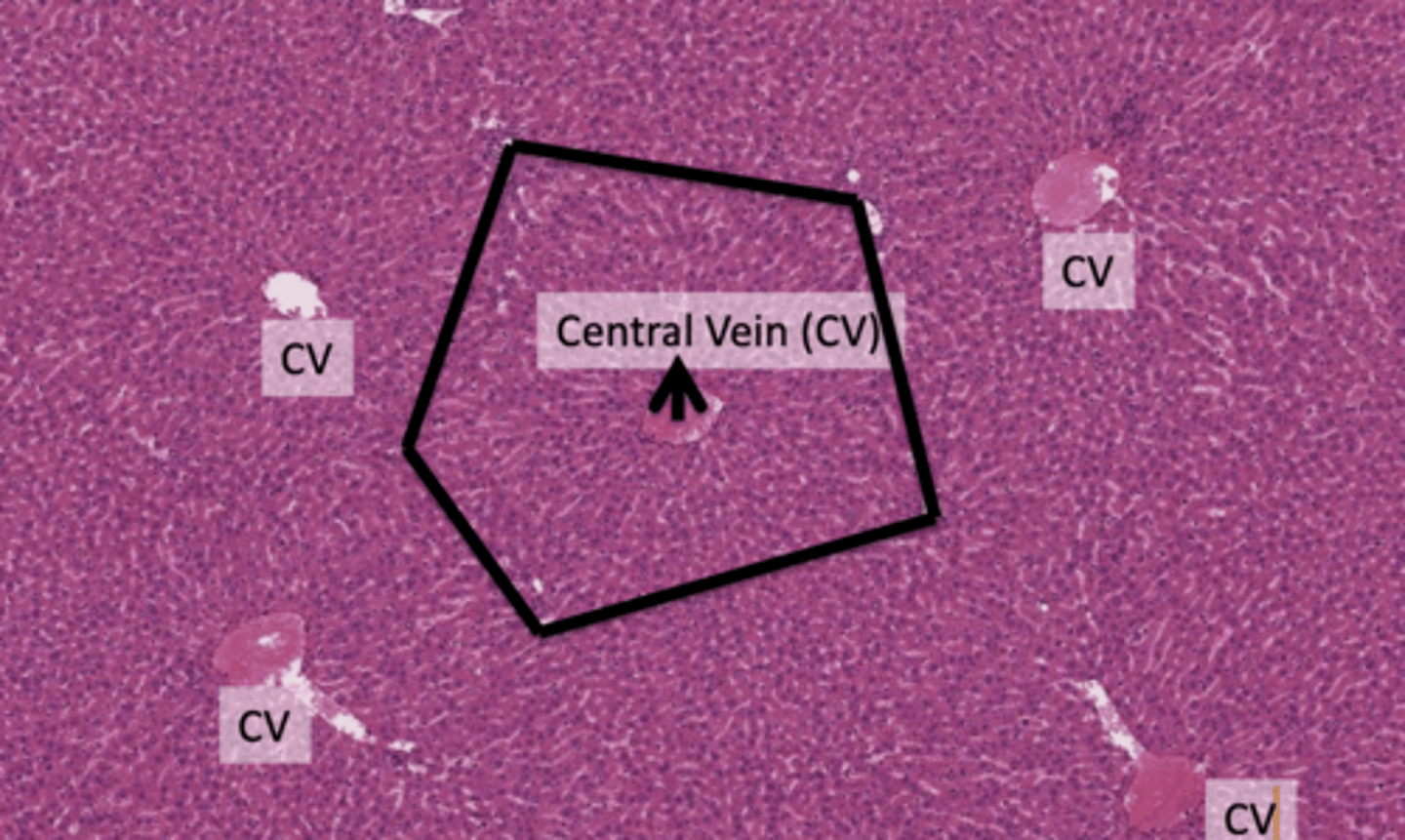
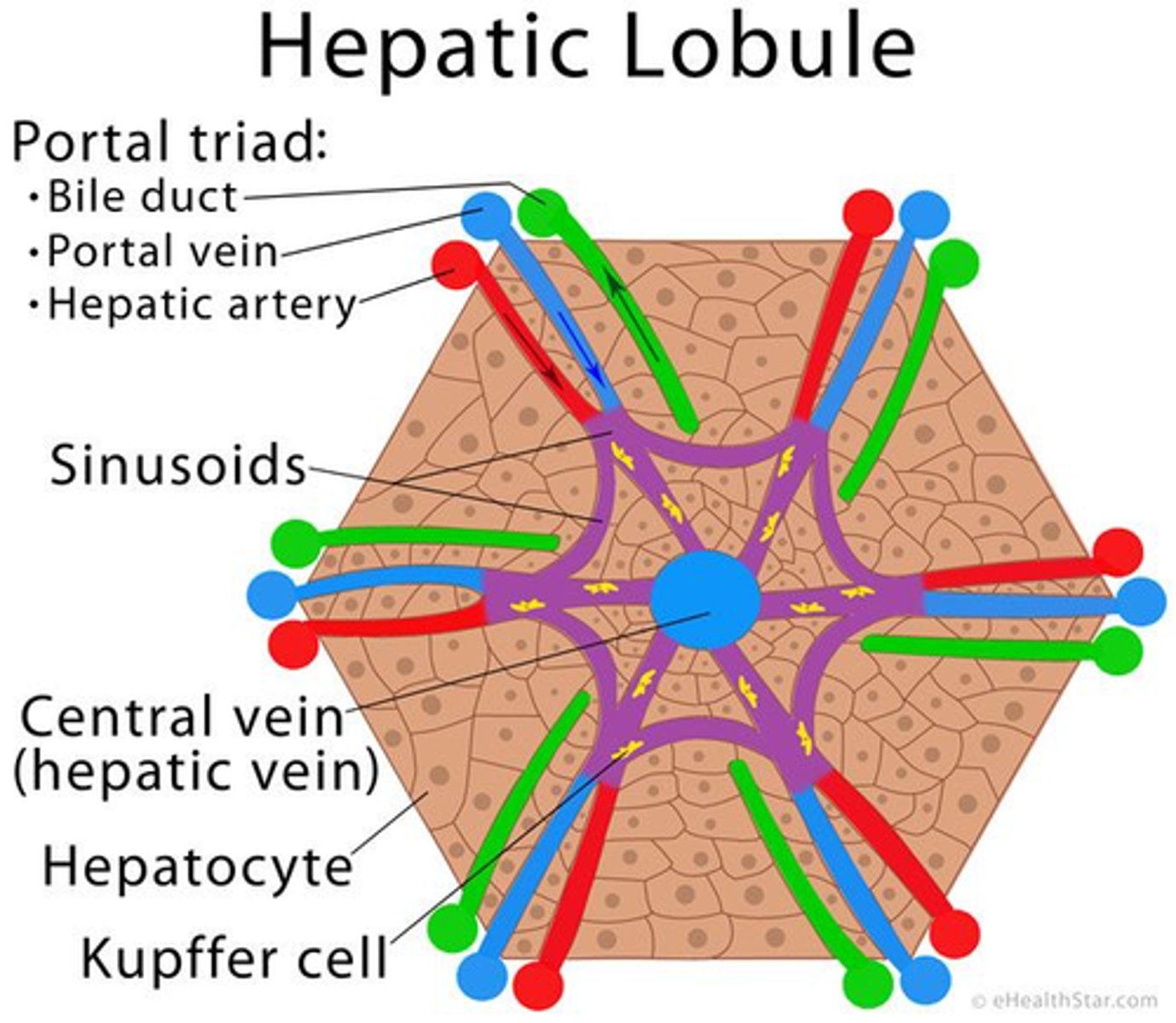
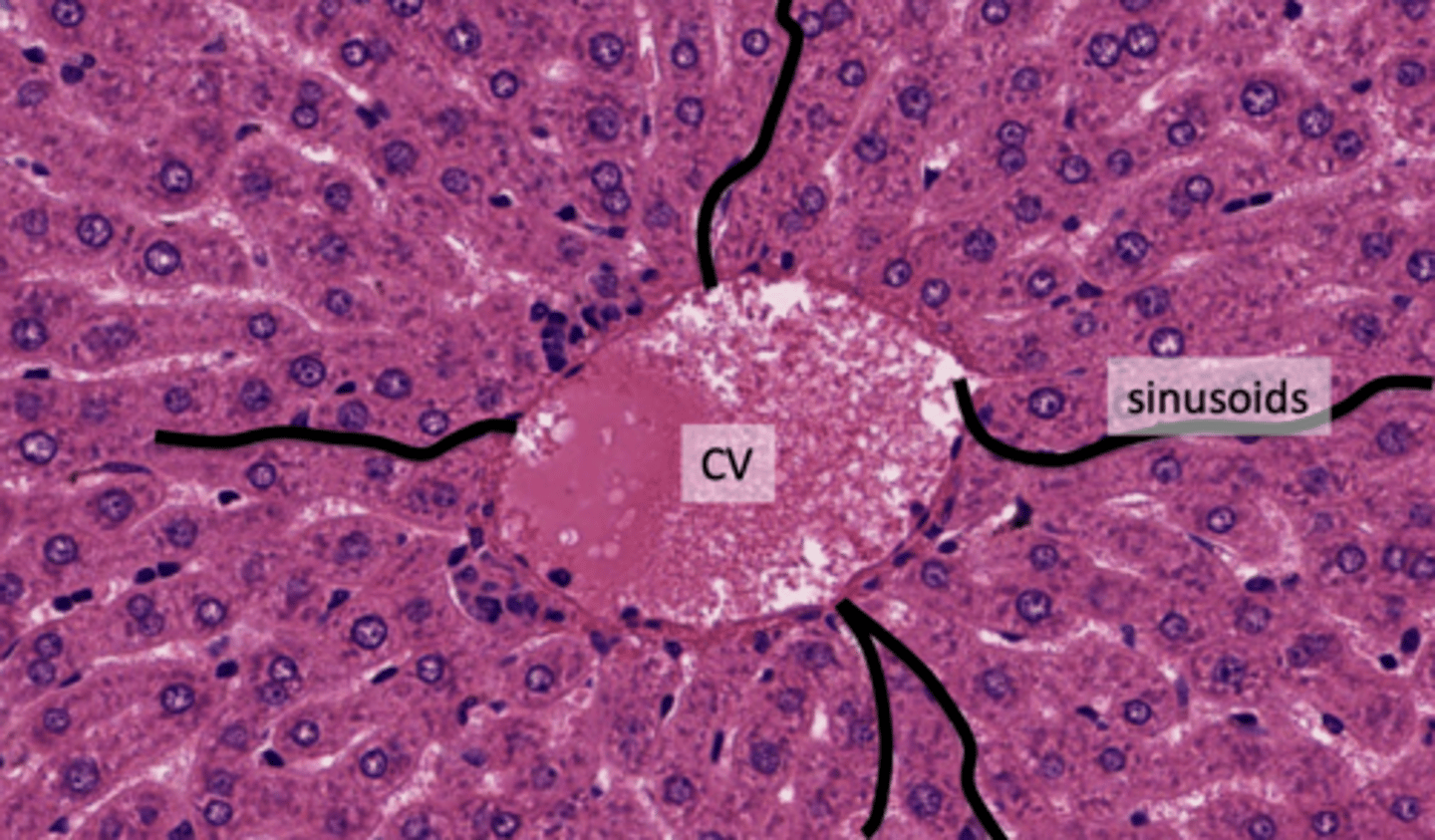
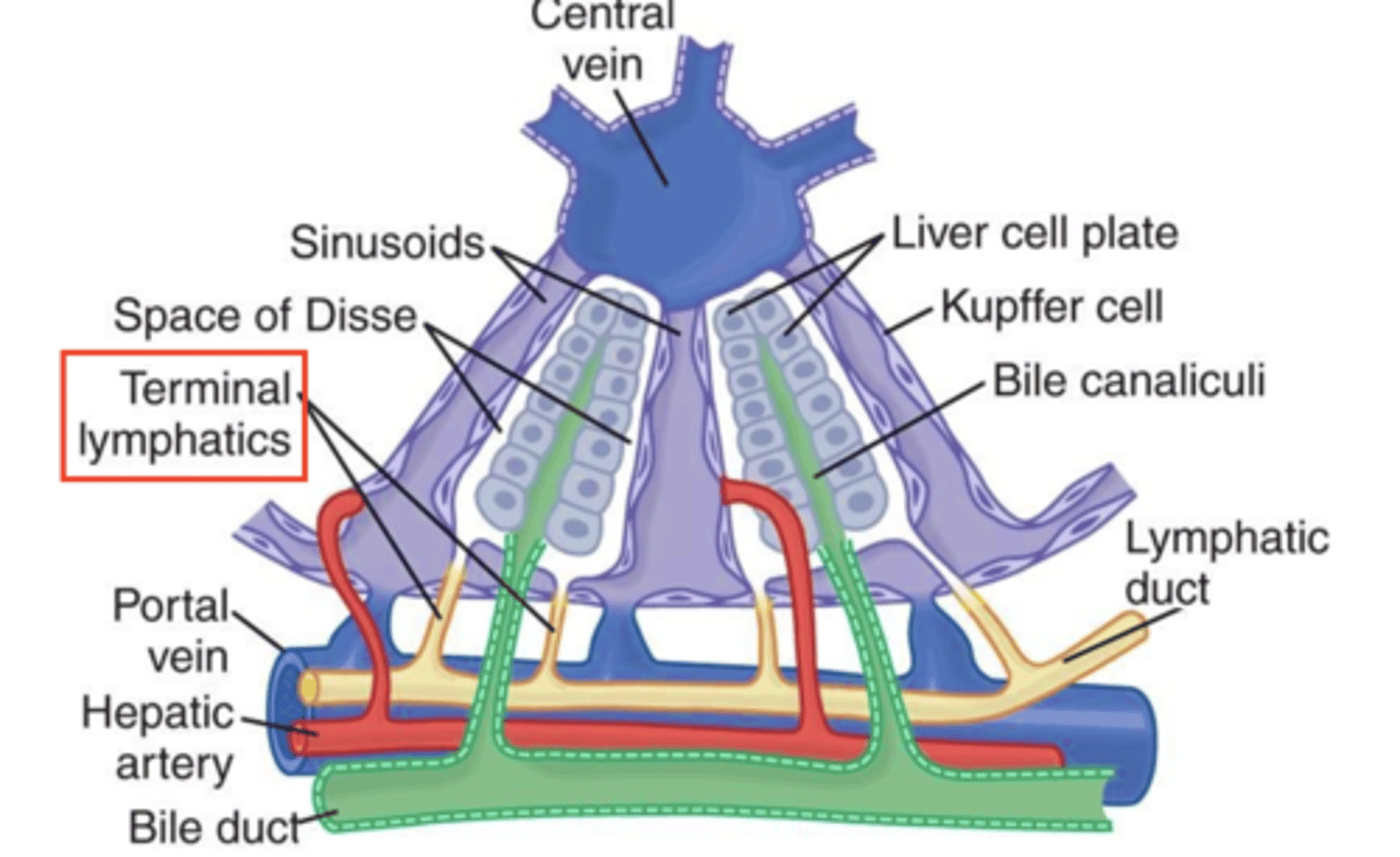
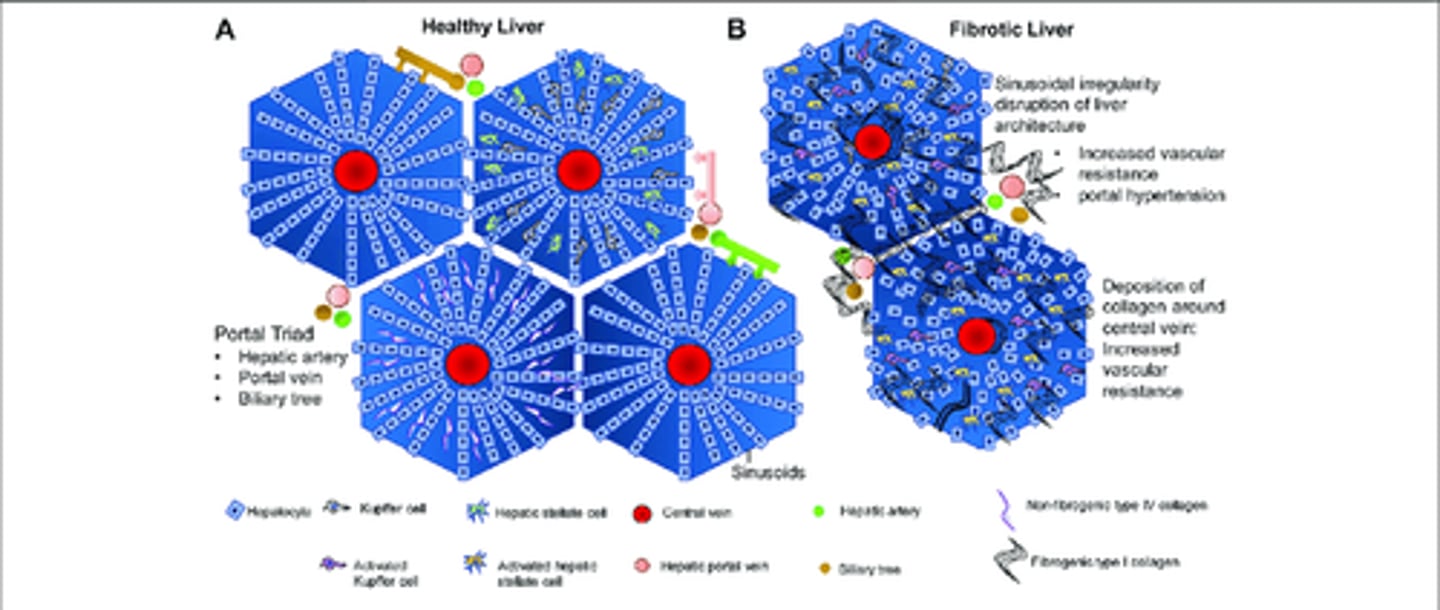
What is the classic liver lobule?
The classic liver lobule is a hexagonal mass of tissue primarily composed of plates of hepatocytes (liver cells), which radiate from the region of the central vein toward the periphery.
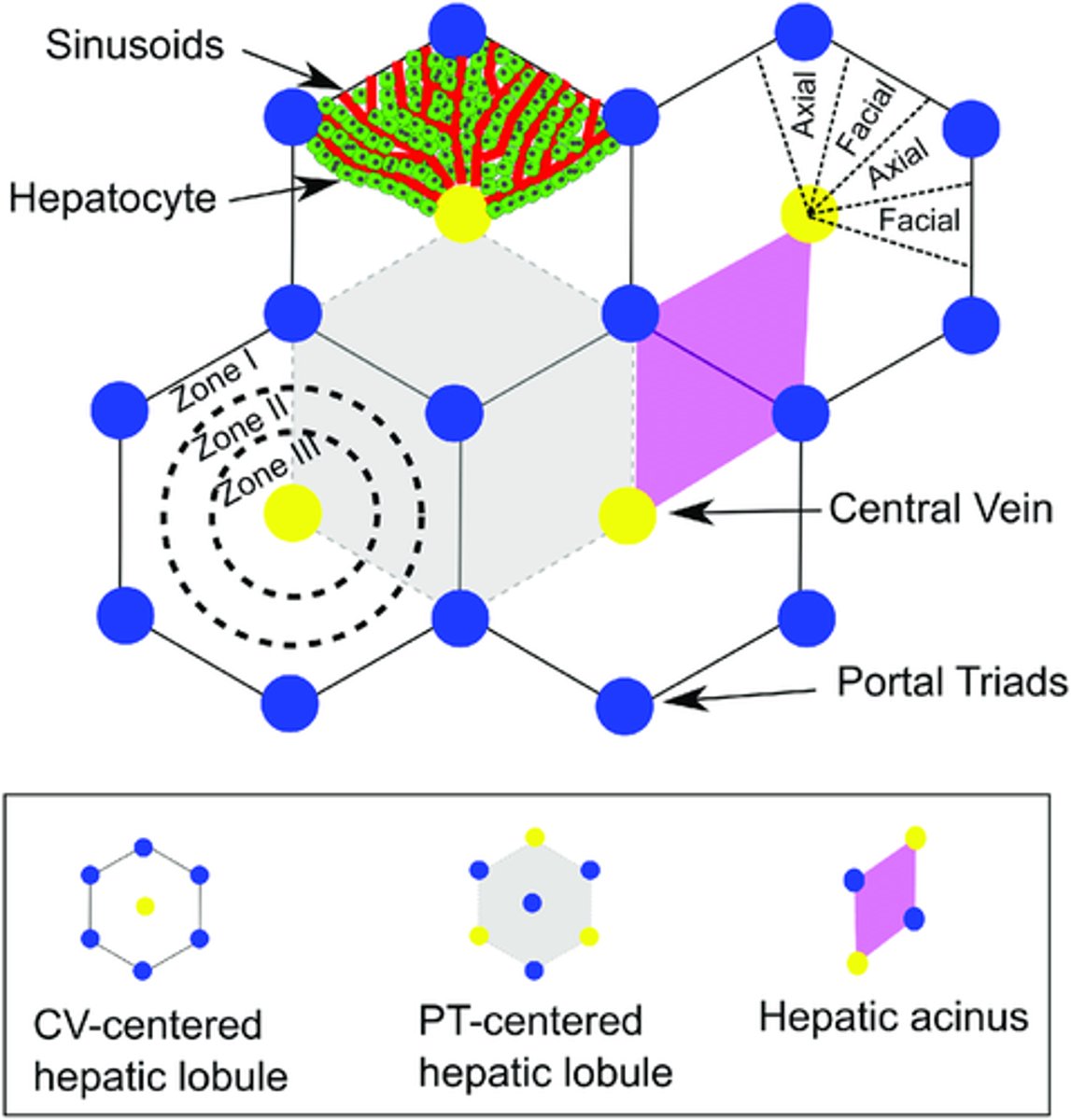
Describe the visual representation of the classic hepatic lobule?
1. Shape: Hexagonal
2. Center: Contains the Central Vein (CV)
3. Corners: Each corner of the hexagon is marked by a Portal Tract (PT).
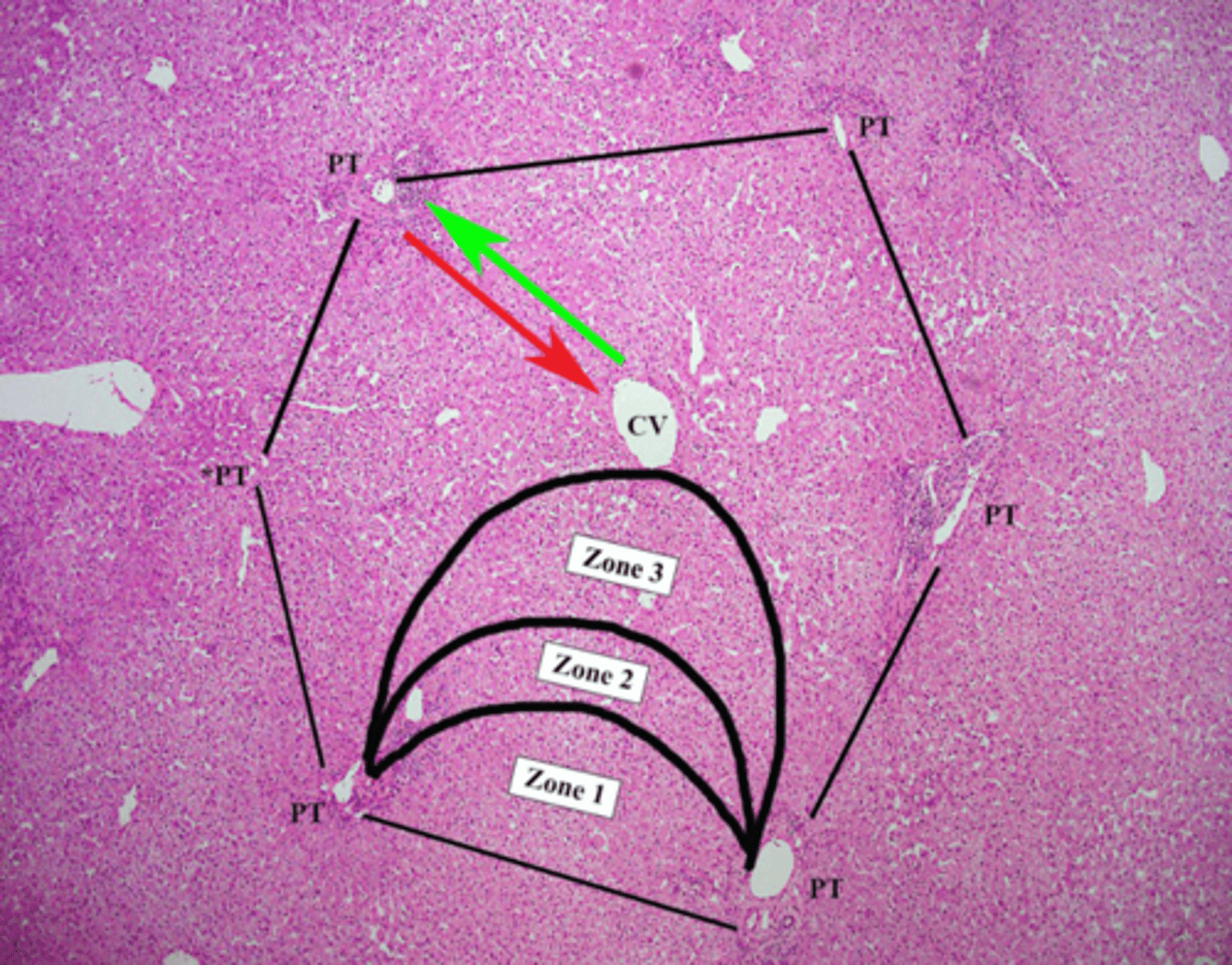
What are portal ducts (DTs)?
specialized regions within the liver where blood vessels, ducts, and other structures enter and exit.
They play a crucial role in the liver's functions, such as processing nutrients, detoxification, and producing important proteins.
What surrounds the portal areas in the liver lobule?
Limiting Plate:
cylindrical plate made up of modified hepatocytes, which surround the portal triads and have specialized roles related to them. (they are like the border of portal triads)
Hepatocyte plates are rows of liver cells metabolising, detoxifying, and producing bile.
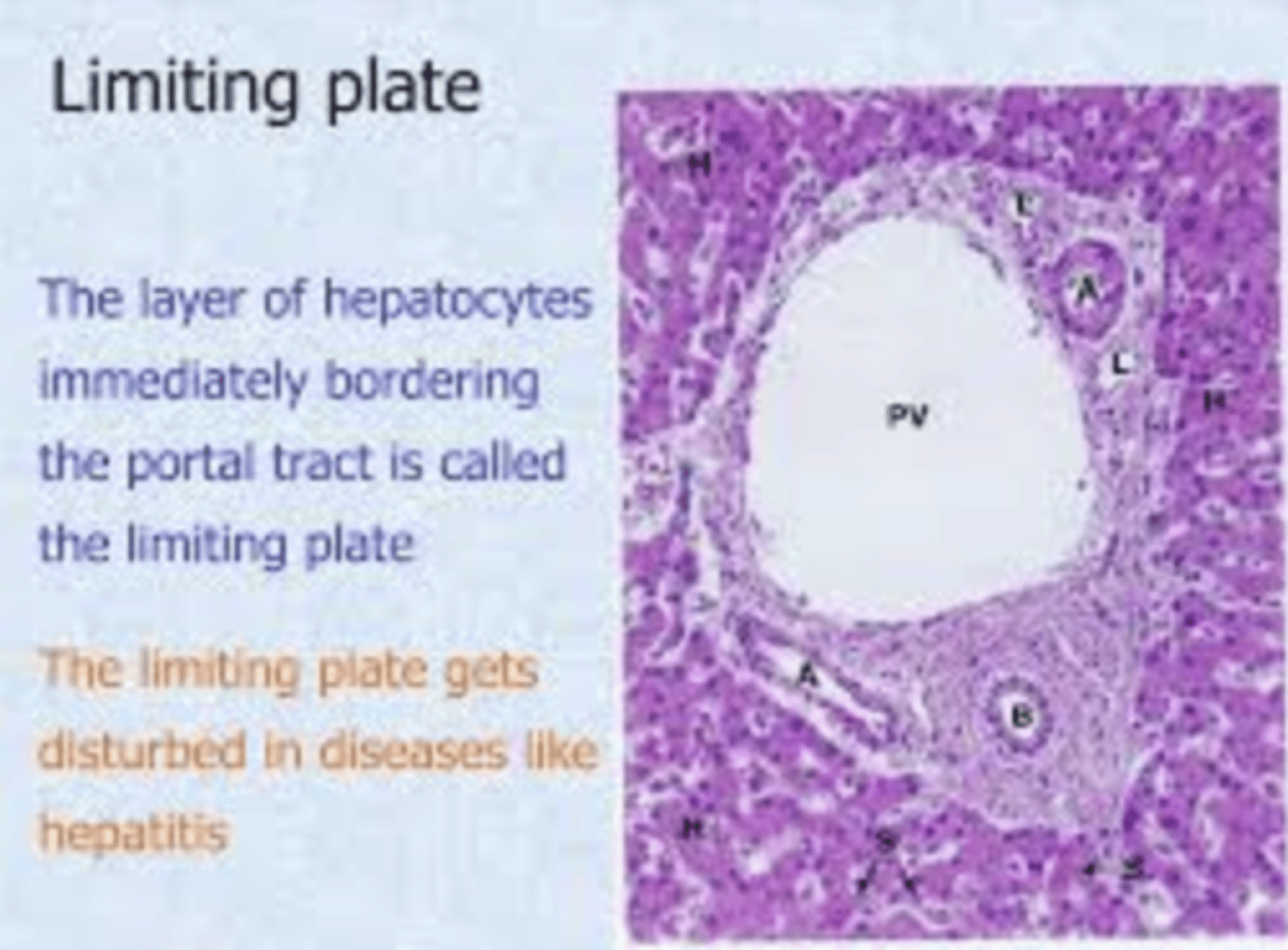
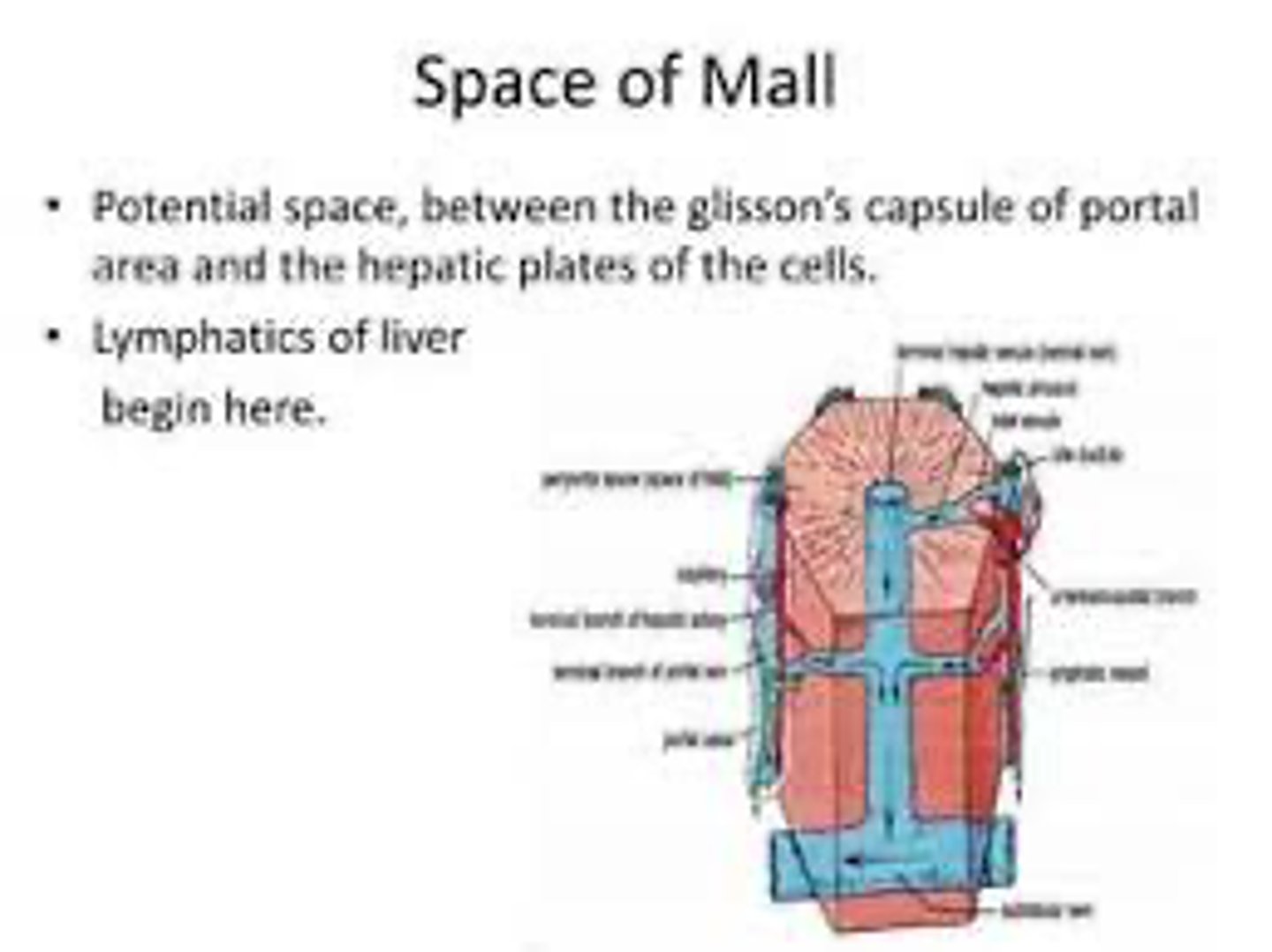
What is the space of mall and what does it surround?
Space of Mall:
region that separates the limiting plate (composed of modified hepatocytes) from the connective tissue (glissons capsule) in the portal area.
SEPARATES CONNECTIVE TISSUE (GLISSONS CAPSULE) FROM LIMITING PLATE
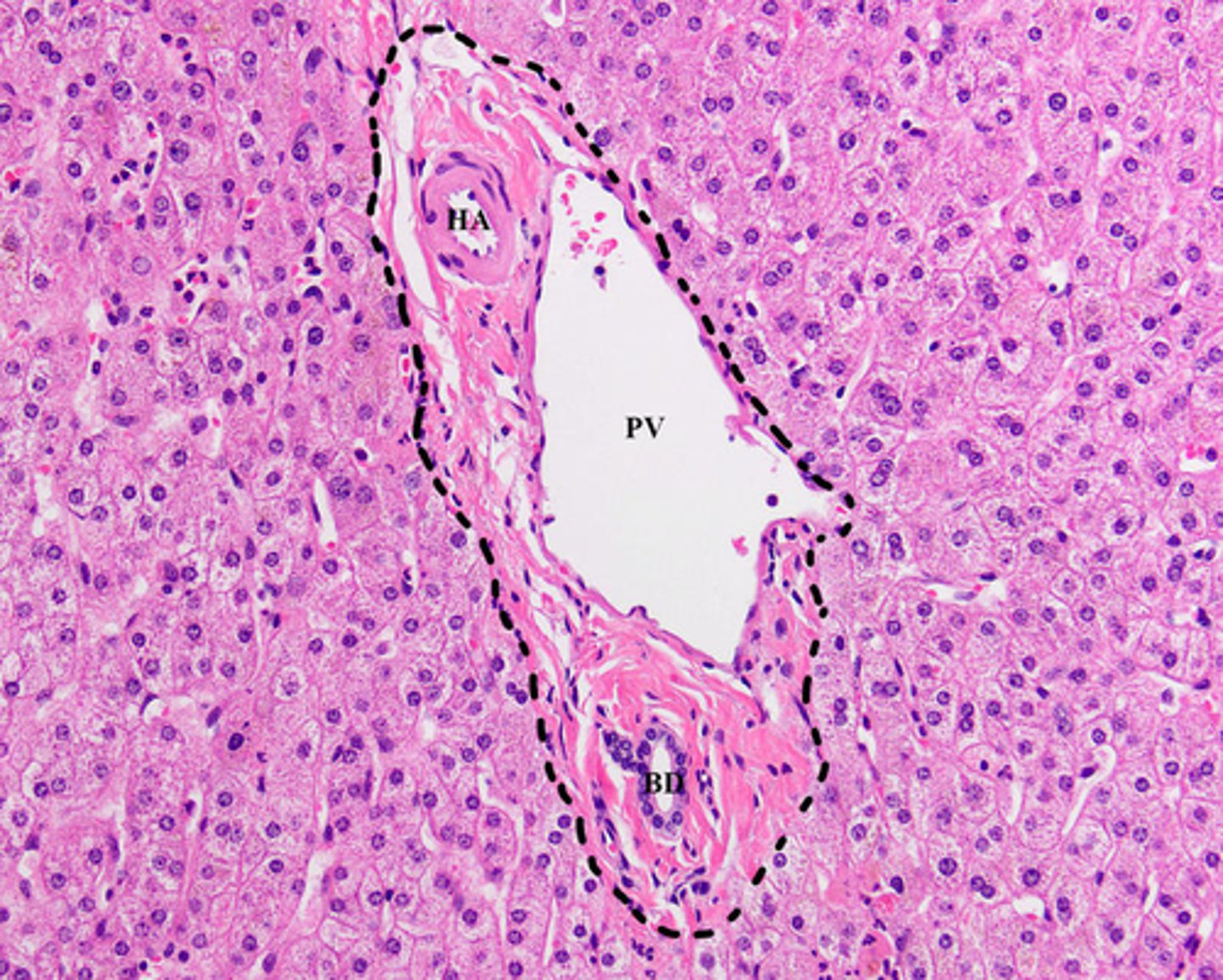
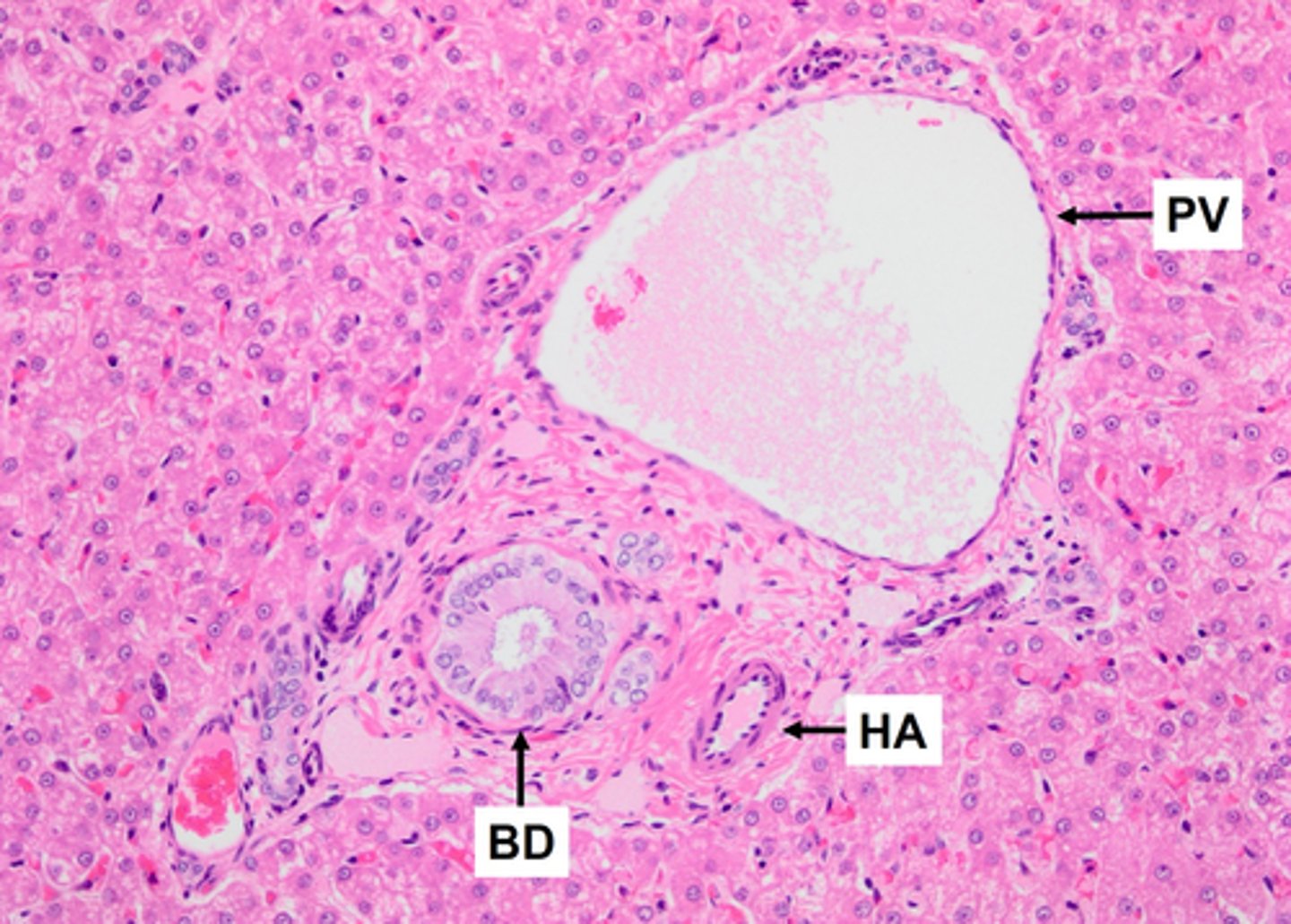
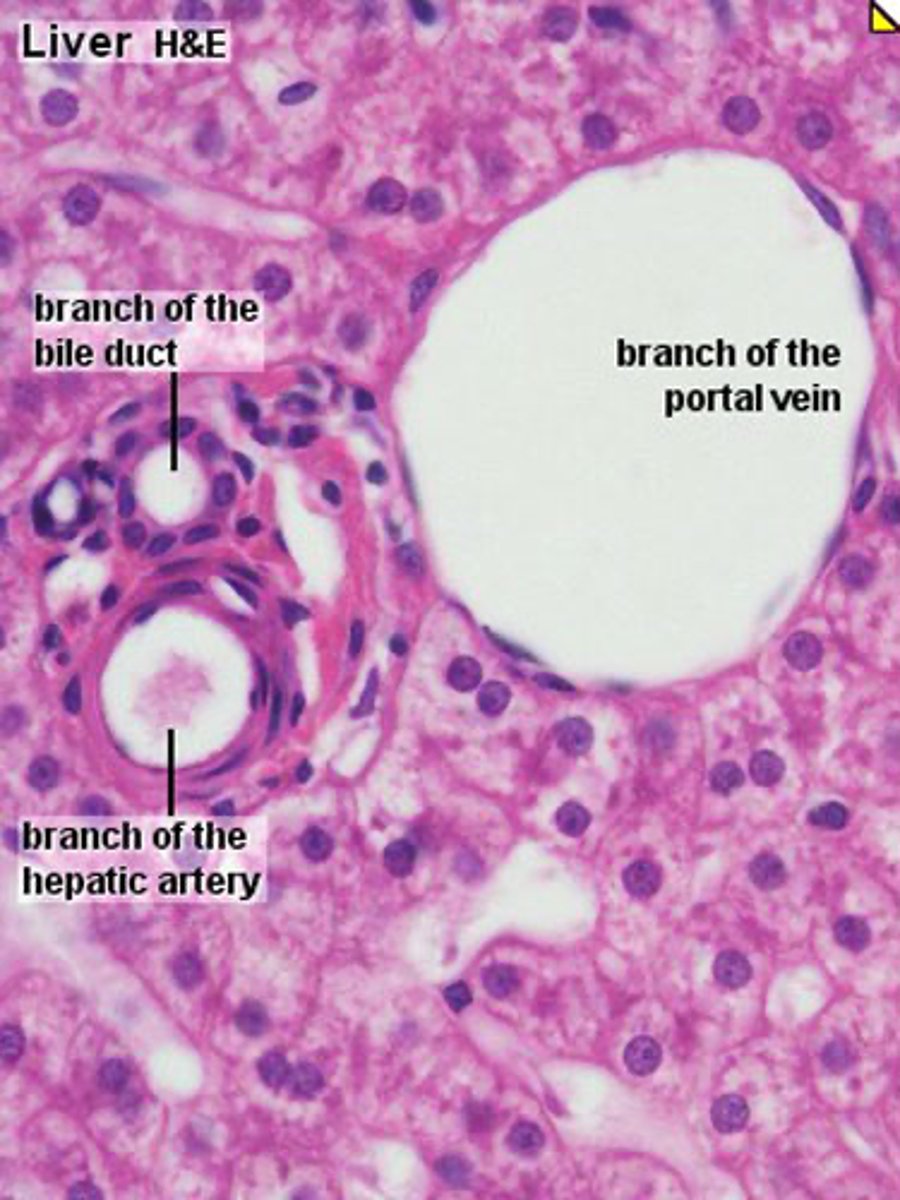
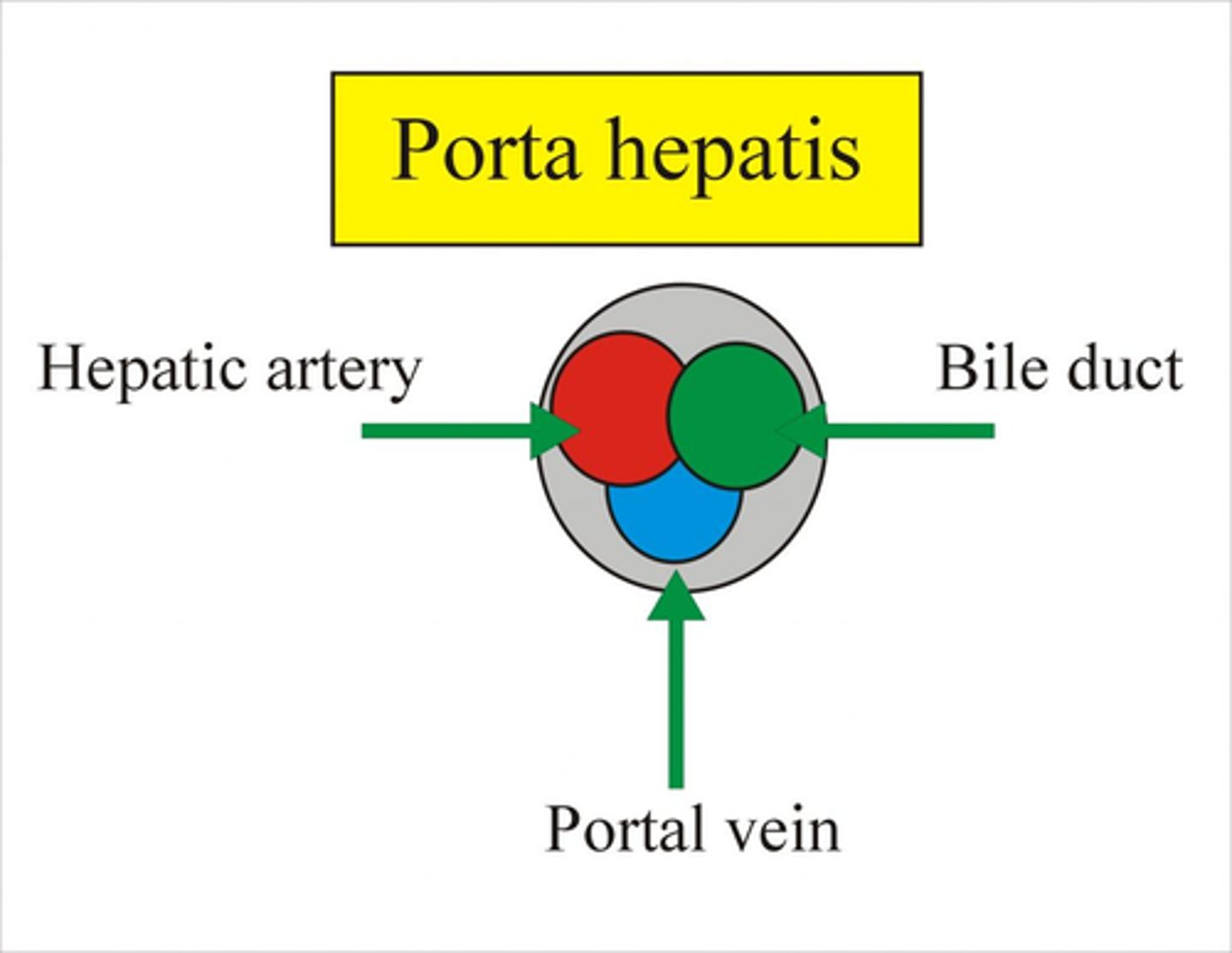
What are the components of the portal tract (triad/area/canal)?
regions of the connective tissue between lobules containing branches of:
- Hepatic Artery: Delivers oxygenated blood to the liver.
- Portal Vein: Carries nutrient-rich, deoxygenated blood from the digestive tract.
- Bile Duct: Transports bile produced by hepatocytes away from the liver.
What is the function of the Hepatic Artery?
Delivers oxygenated blood to the liver.
This is essential for supplying the liver with the oxygen needed for cellular metabolism and function.
What is the function of the Portal Vein?
Carries nutrient-rich, deoxygenated blood from the digestive tract to the liver.
This allows the liver to process nutrients, metabolize drugs, and detoxify substances.
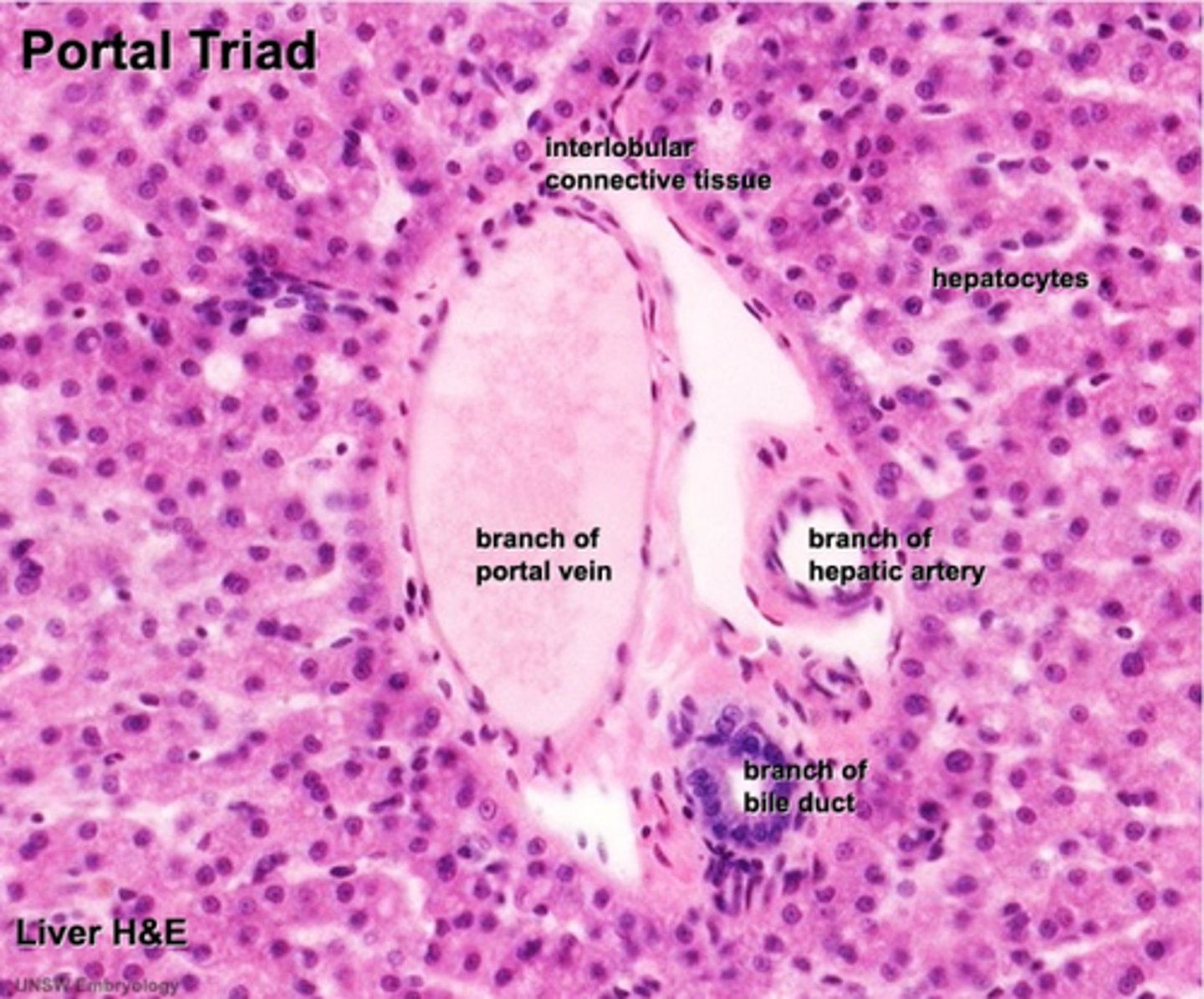
How does one histologically differentiate between the portal artery and vein?
artery: round
vein: irregular shape
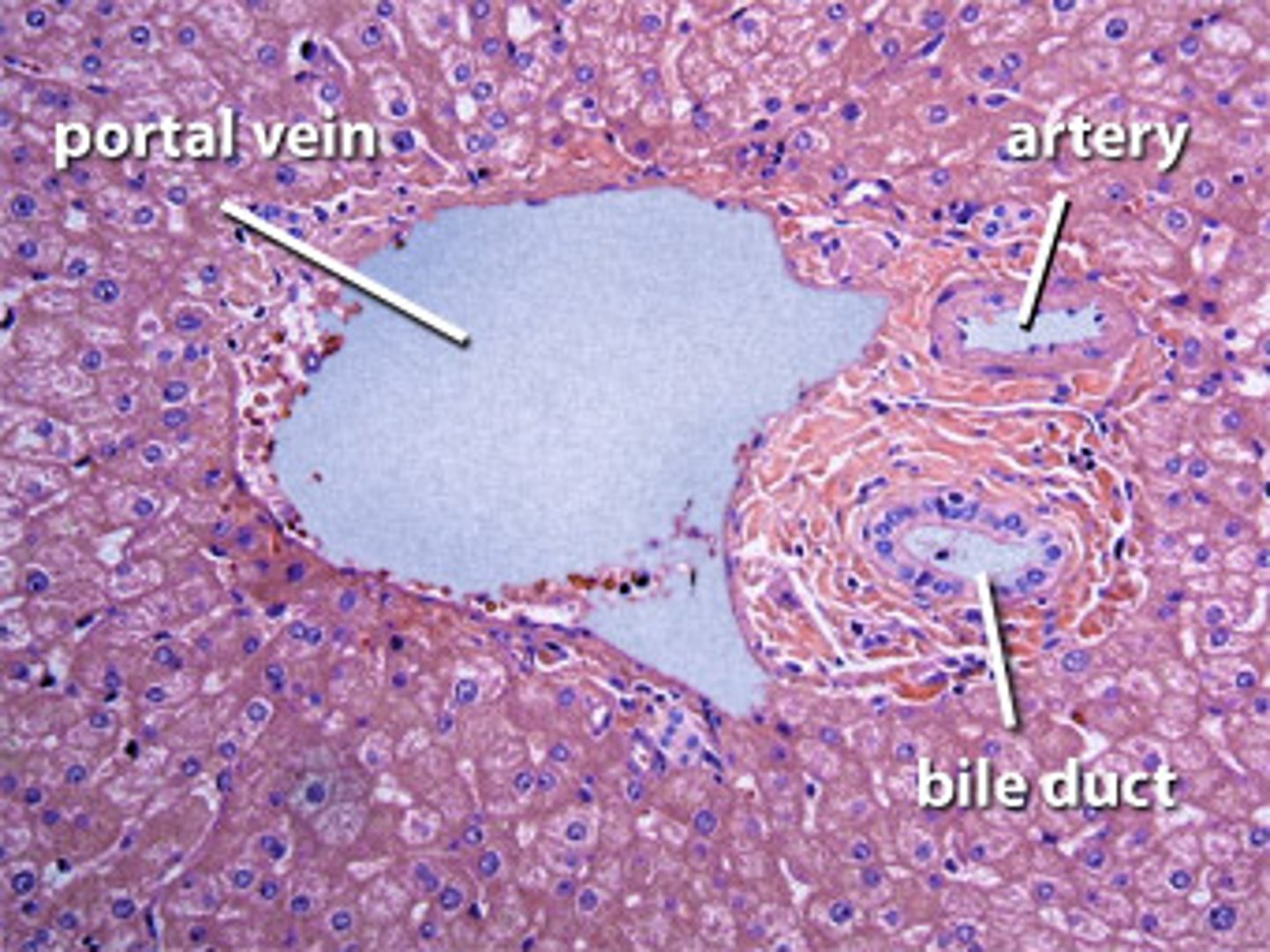
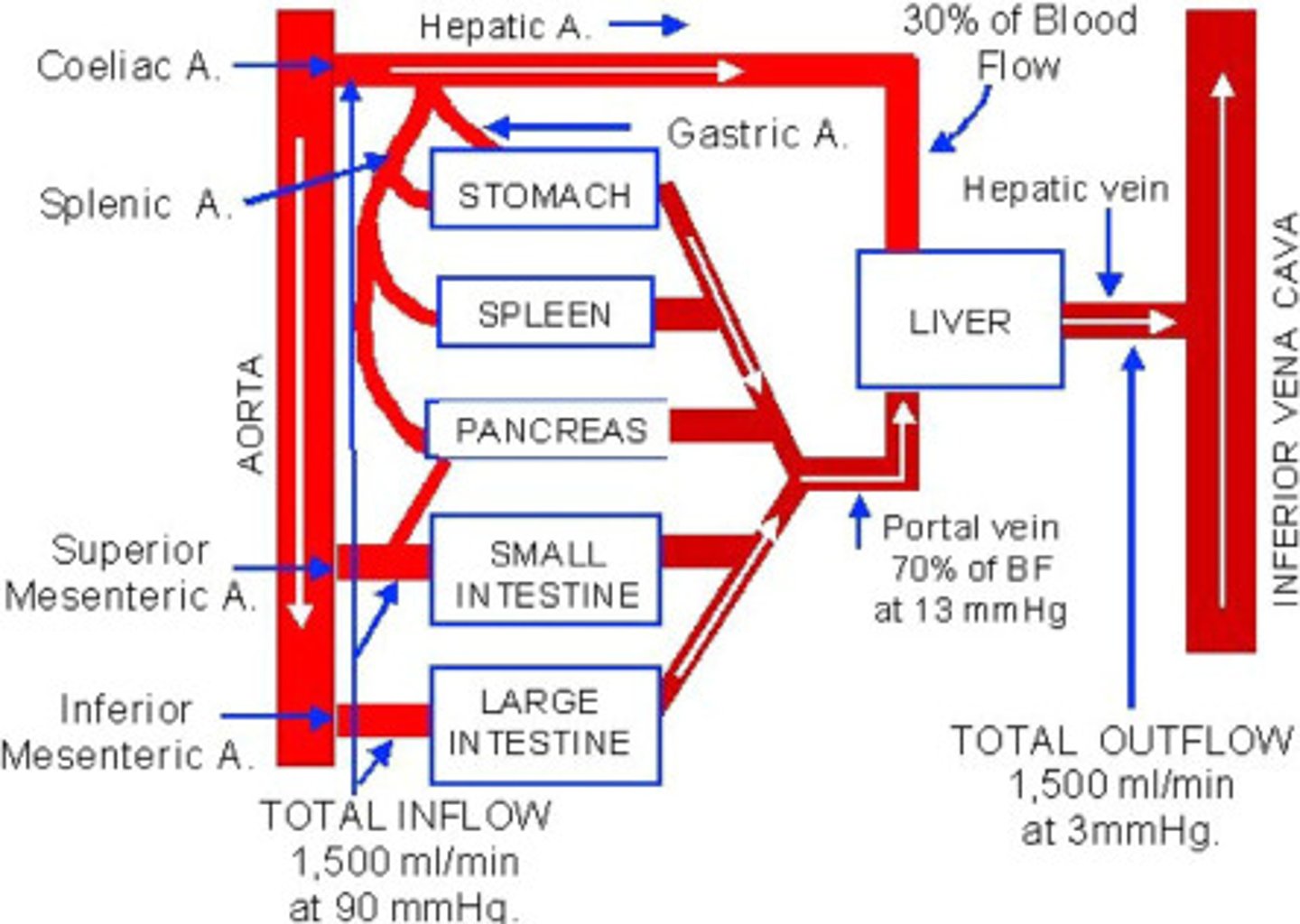
What percentage of the liver's blood supply comes from the portal vein and the hepatic artery?
portal vein: 70-80% (deox)
hepatic artery: 20-30% (ox)
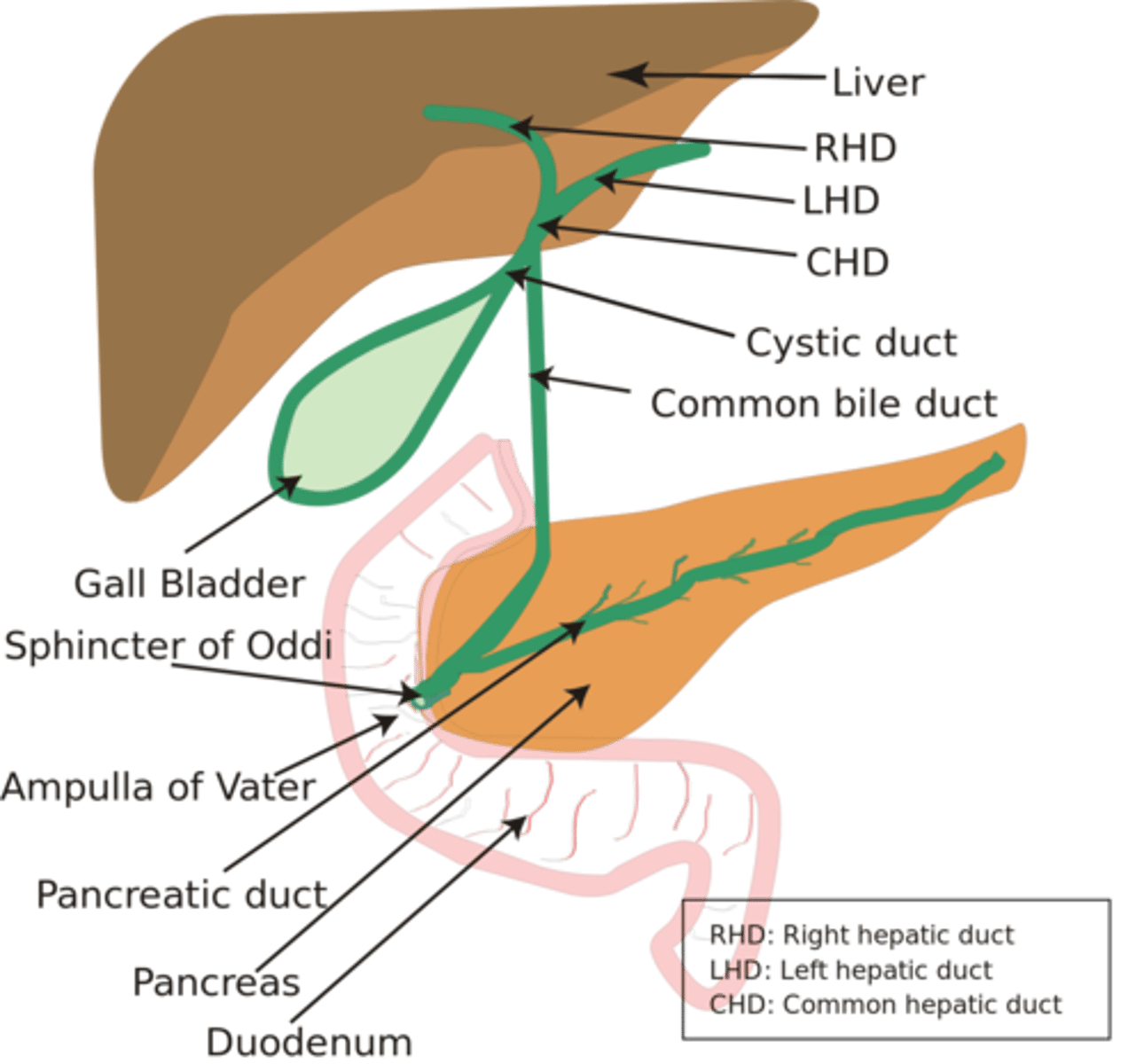
What is the function of the Bile Duct?
Transports bile produced by hepatocytes (drained into the bile duct within the portal areas) away from the liver into the gallbladder or directly to the small intestine (duodenum).
- gallbladder
- duodenum
Bile is crucial for the digestion and absorption of fats.
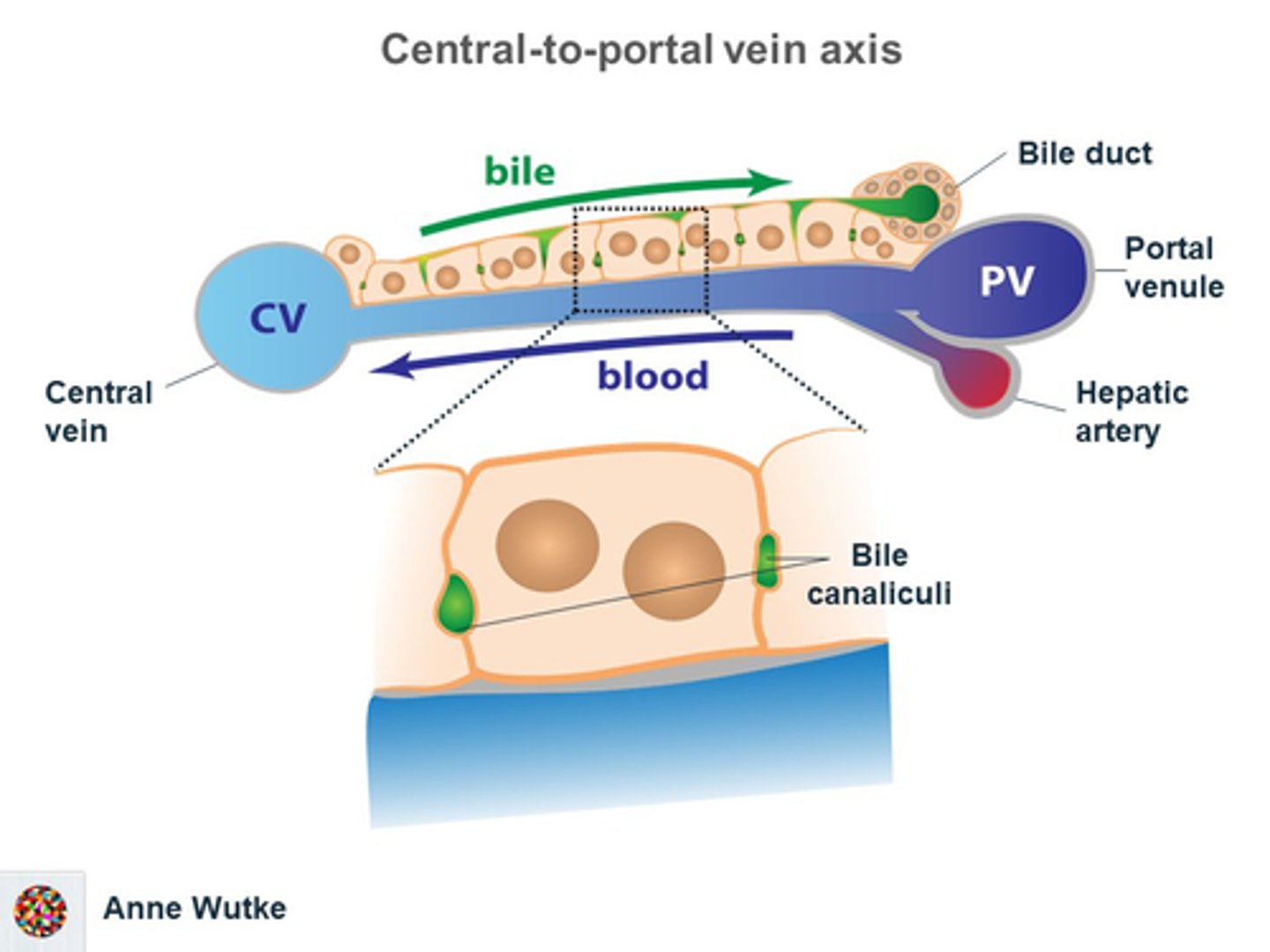
What do central veins in the liver do?
Central veins collect processed blood from the liver lobules and direct it towards the heart for systemic circulation.
it is situated at the center of the liver lobule and collects the processed blood from the sinusoids to transport it to the hepatic vein, and then to the inferior vena cava.
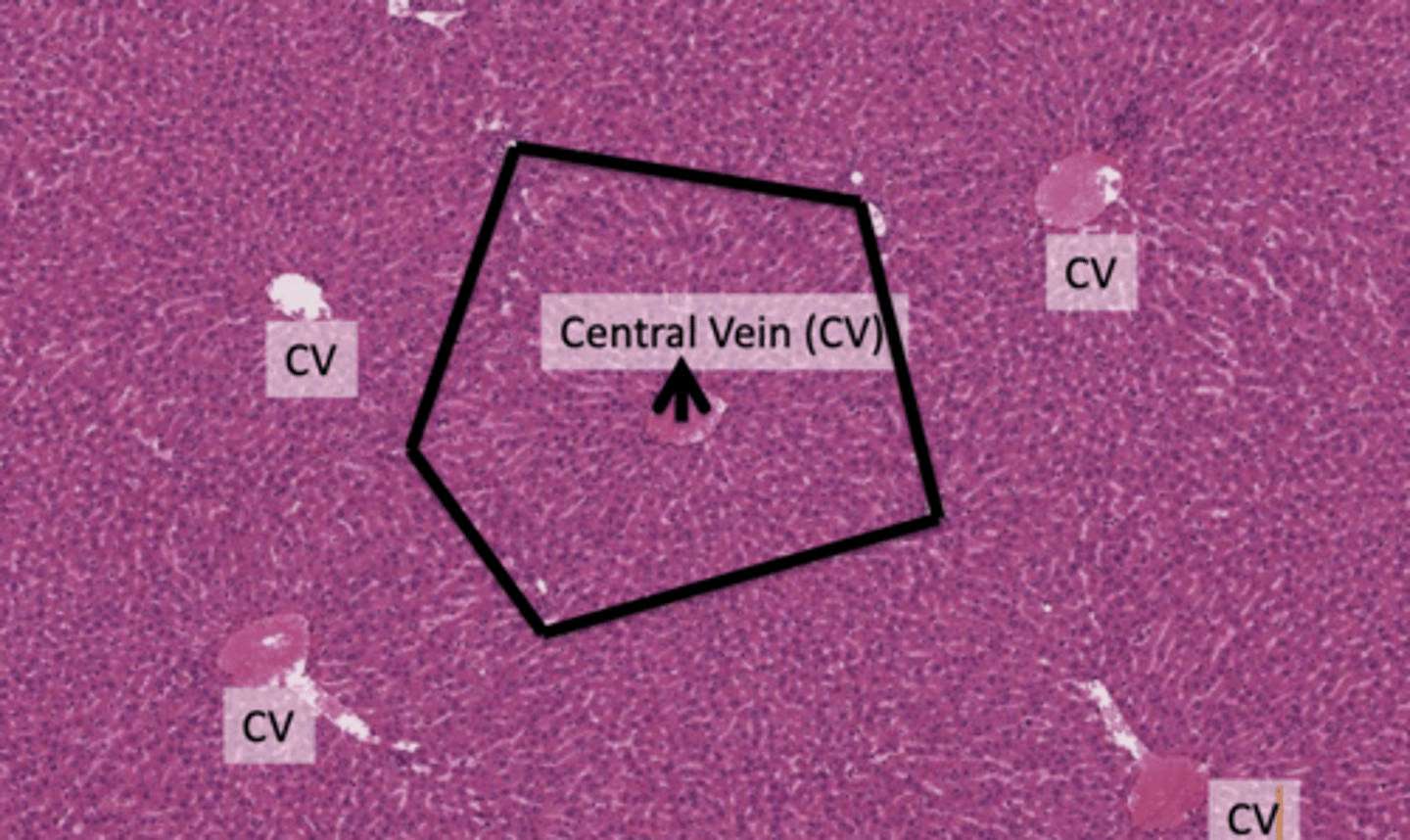
How does blood enter the Classic (Hepatic) Lobule?
Blood enters the lobule through the portal vein of the portal tracts positioned at the corners of the hexagonal lobule structure.
Blood flows from the portal tracts towards the central vein, passing through the liver parenchyma, which is rich in hepatocytes (liver cells).
BASICALLY BLOOD FLOWS THROUGH THE LIVER PARENCHYMA RICH IN HEPATOCYTES FROM THE PERIPHERY TO THE CENTRE
Outline how you would draw the blood flow from portal tracts to central vein:
1. Draw a Hexagon:Represent the shape of the liver lobule.
2. Mark the Corners: Place dots or small circles at each corner of the hexagon to indicate the location of the portal tracts.
3. Portal Tracts: At each corner dot, draw a small branching figure to symbolize the portal tracts. Label them "Portal Tract".
4. Add Arrows from Portal Tracts: From each portal tract, draw arrows inward, signifying the direction of blood flow towards the center of the hexagon.
5. Central Vein: In the center of the hexagon, draw a larger circle or cylinder and label it "Central Vein".
6. Arrows Toward Central Vein: The arrows from the portal tracts should converge at the central vein, illustrating the path of the blood flow.
7. Hepatocytes: Between the paths of the arrows, fill the space with dots or small cells to represent the hepatocytes through which the blood passes.
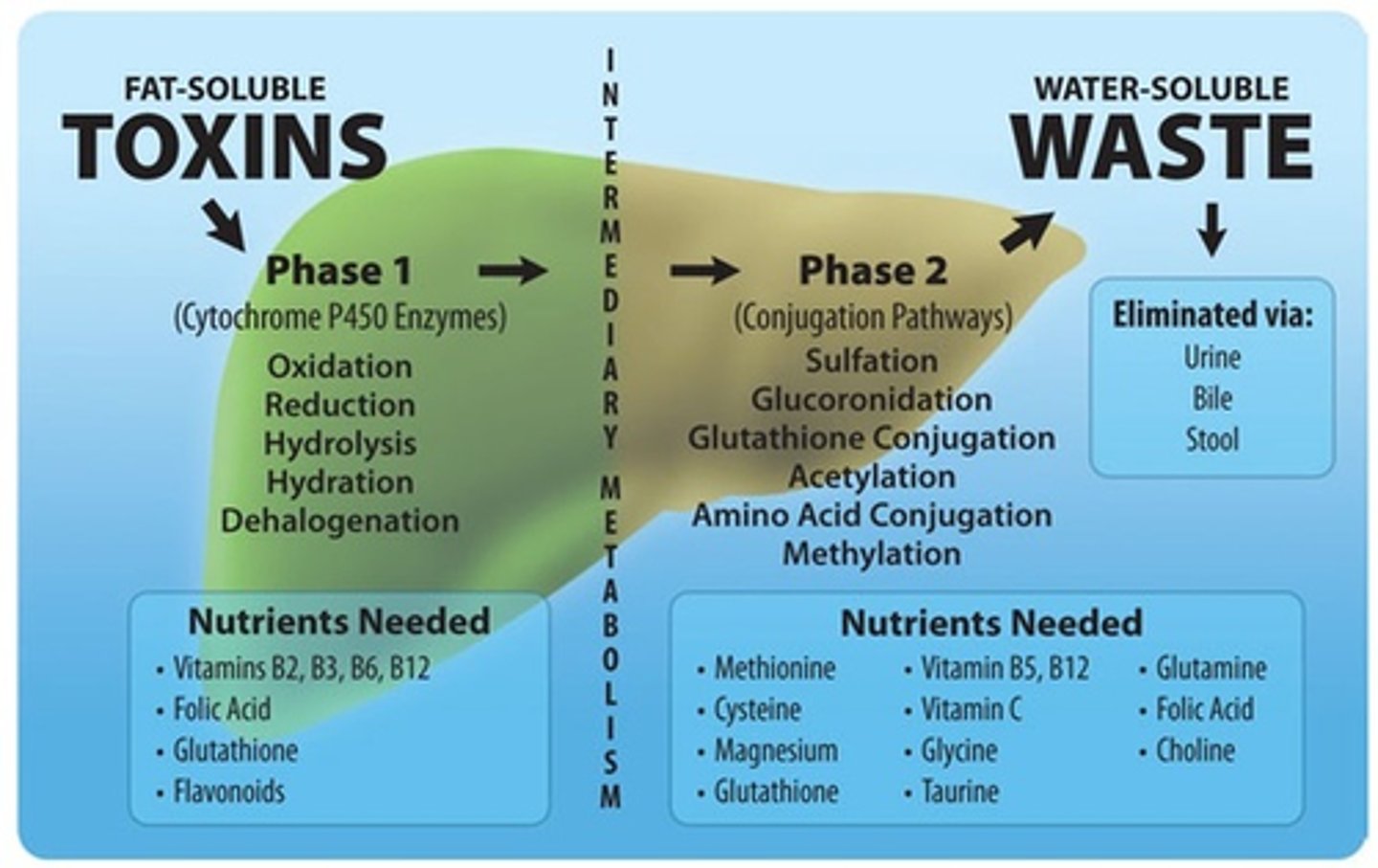
What detoxification function do hepatocytes perform?
Hepatocytes remove toxins from the blood, helping to cleanse it before it leaves the liver (filter).
SO REMEMBER THE TWO FUNCTIONS OF HEPATOCYTES ARE FILTERING AND THE PRODUCTION OF BILE
How do hepatocytes contribute to bile production?
Hepatocytes produce bile, which is collected by bile ducts and transported out of the lobule for digestion or storage.
SO REMEMBER THE TWO FUNCTIONS OF HEPATOCYTES ARE FILTERING AND THE PRODUCTION OF BILE
Describe the exit pathway of blood in the Classic (Hepatic) Lobule:
Central vein → sublobular veins → hepatic vein → inferior vena cava → general circulation
After processing, the blood collects in the central vein of the lobule (blood collects after being processed by hepatocytes), which drains into the hepatic vein and then into the inferior vena cava.
the hepatic vein is formed by the union of numerous sublobular veins that collect blood from the central vein
What is the function of liver sinusoids?
Liver sinusoids are capillaries that receive blood from the terminal branches of the hepatic artery and portal vein and deliver it to the central vein, facilitating the exchange of substances between the blood and hepatocytes.
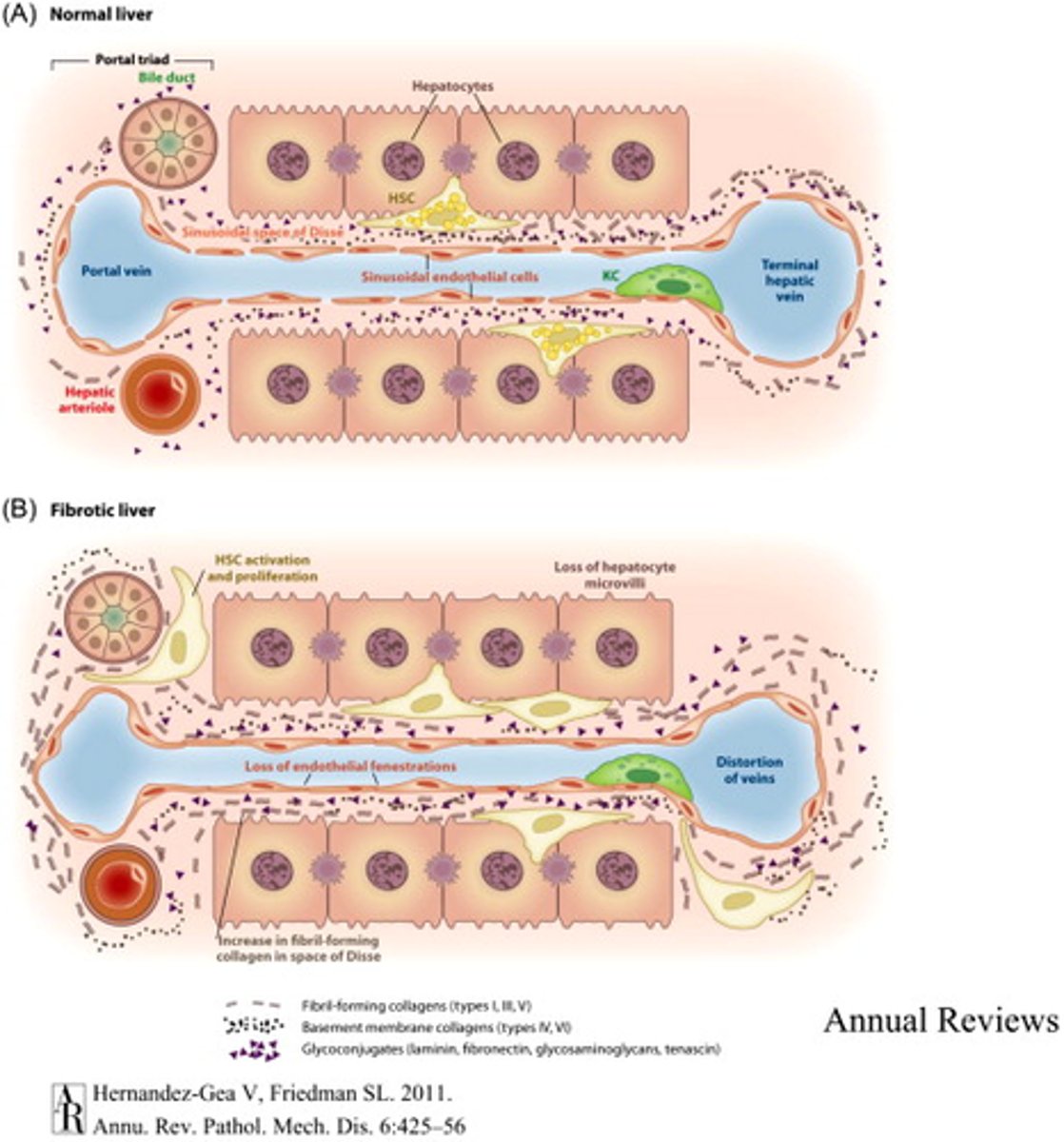
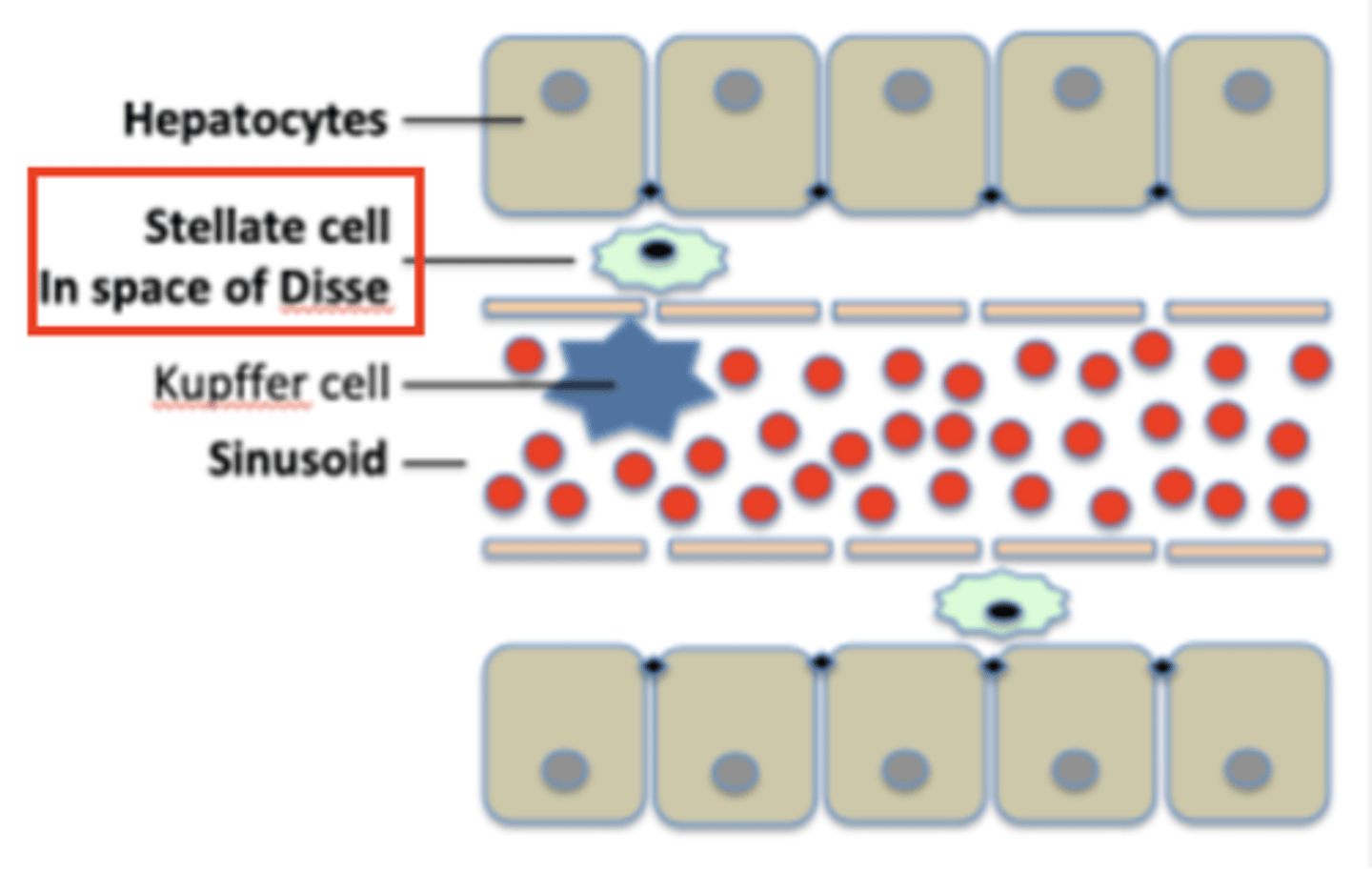
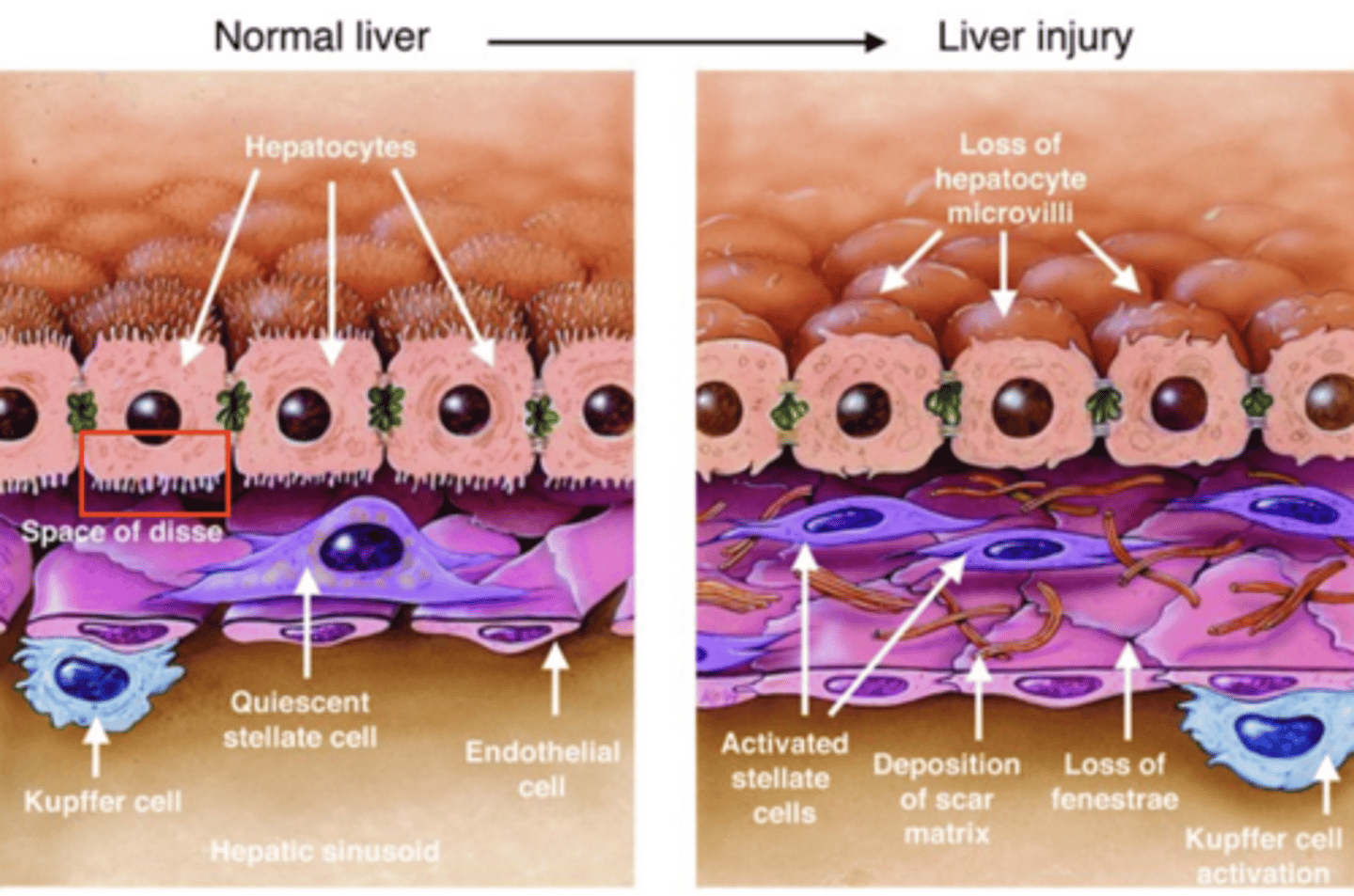
What is the perisinusoidal space, and what occurs there?
also known as the space of Disse:
area between the endothelium that surrounds the liver sinusoids (sinusoidal endothelium) and hepatocytes where exchange of materials takes place.
ITS A SUBENDOTHELIAL SPACE
give me another name of the perisinusoidal space:
SPACE OF DISSE
subendothelial space in the liver lobule between the sinusoidal lining and the hepatocytes.
hepatocytes do not directly contact the bloodstream; they exchange materials with the blood through the Space of Disse.
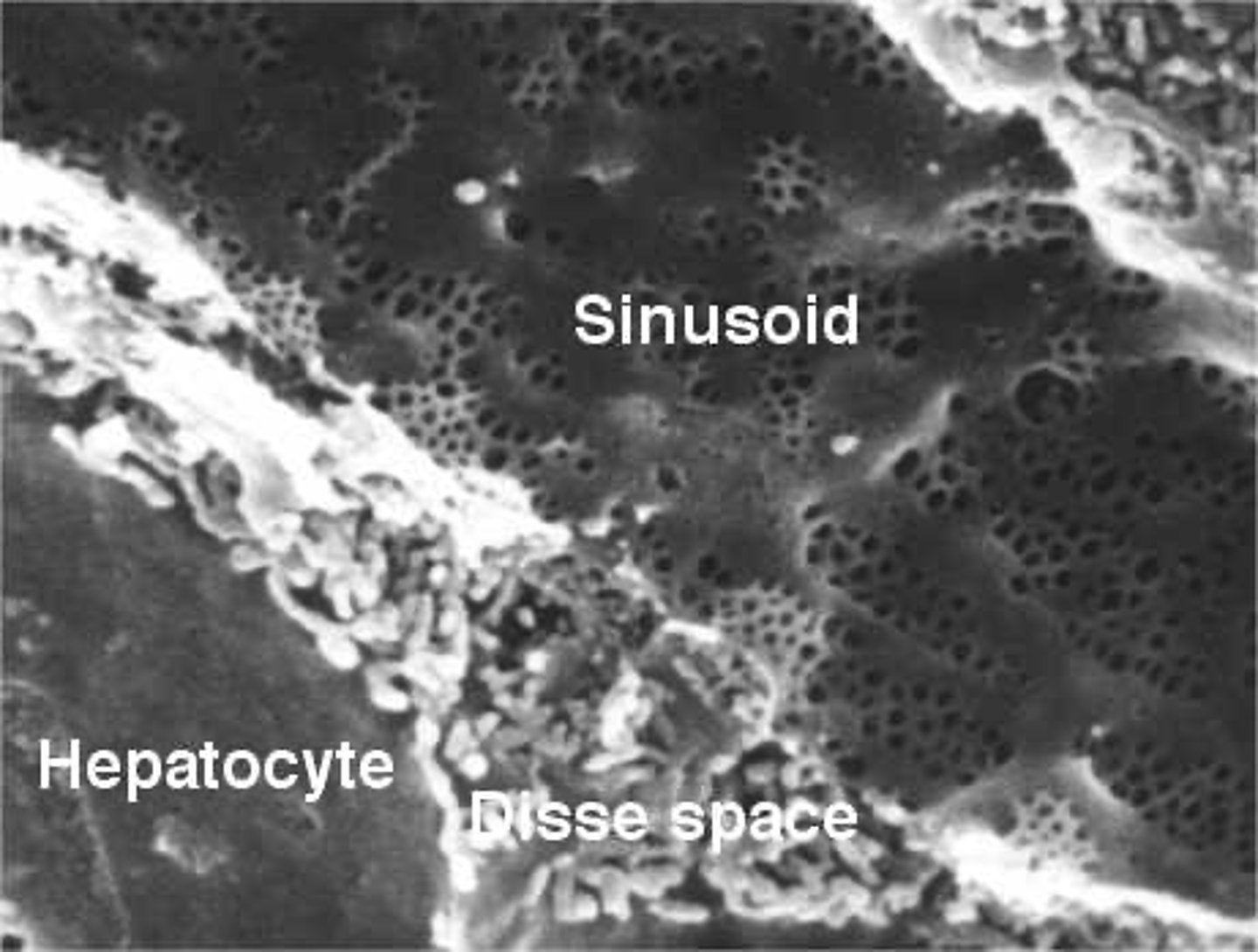
What features are present in the Space of Disse?
1. hepatocytes with short microvilli
2. reticular fibers: that maintain the architecture of the sinusoids
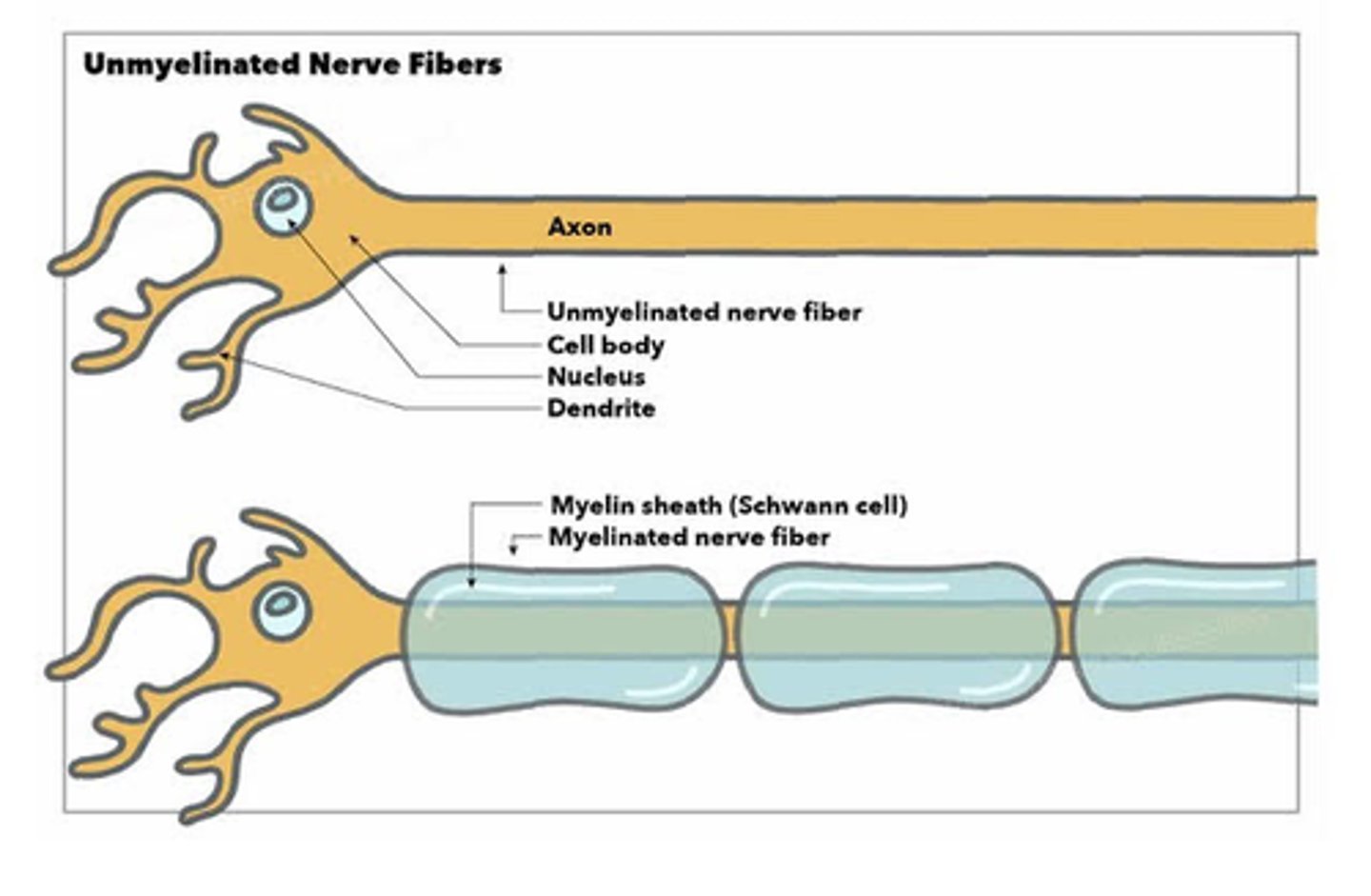
3. occasional non-myelinated nerve fibers
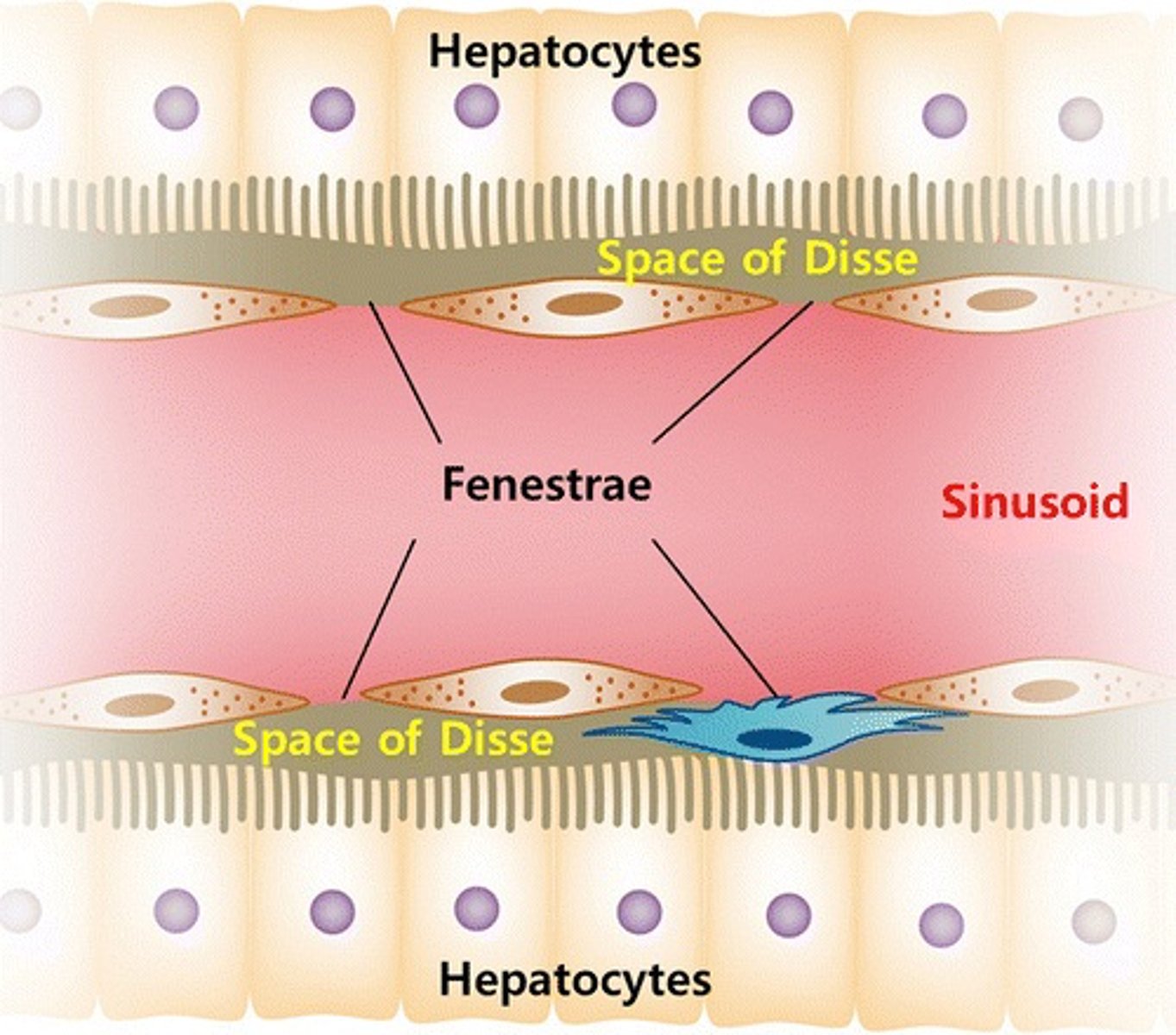
What is the role of hepatocyte microvilli in the Space of Disse?
increase the surface area for the exchange of metabolites between hepatocytes and the blood in the sinusoids.
What is the significance of nerve fibers in the Space of Disse?
Non-myelinated nerve fibers in the Space of Disse may play a role in regulating the functions of hepatocytes and the sinusoidal blood flow.
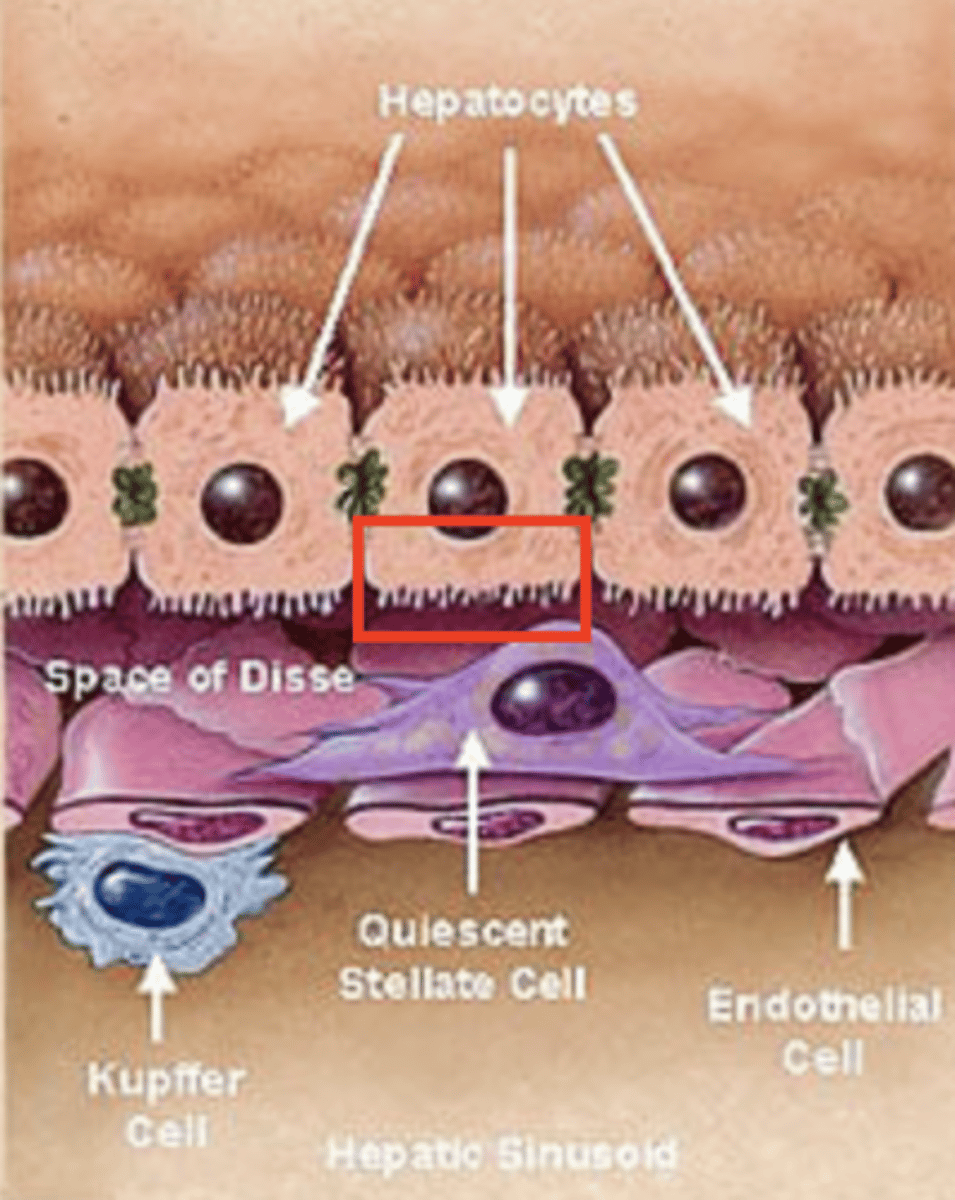
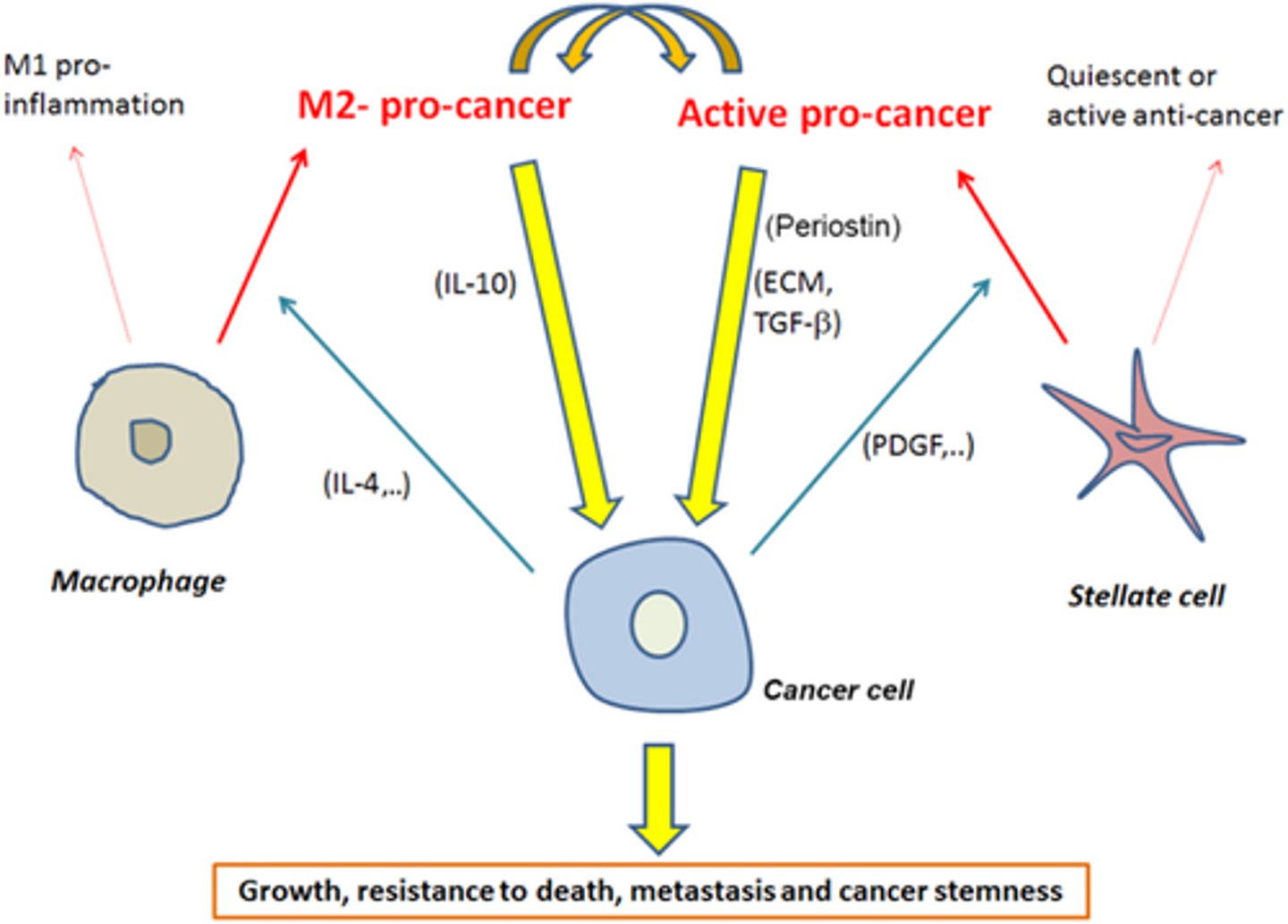
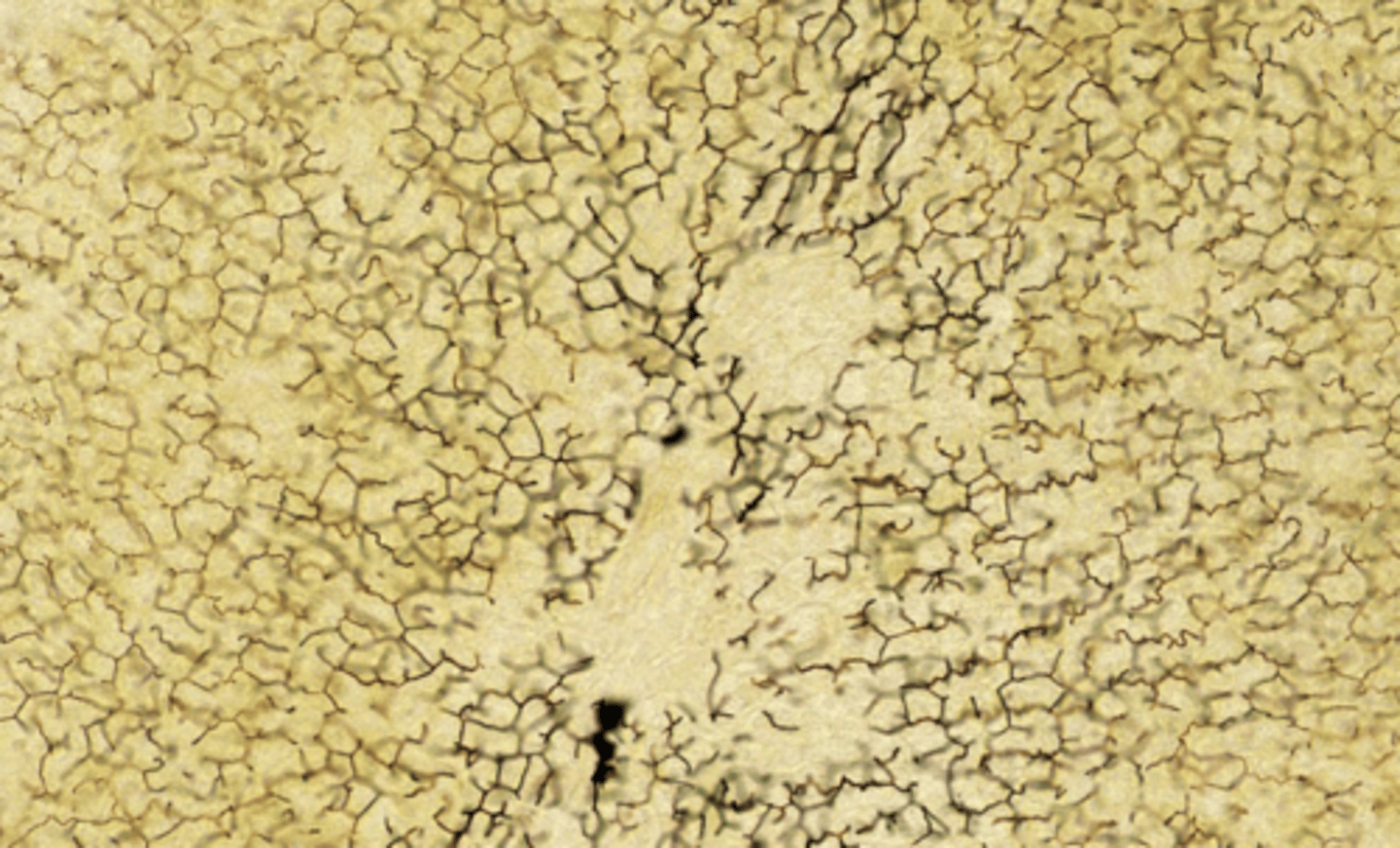
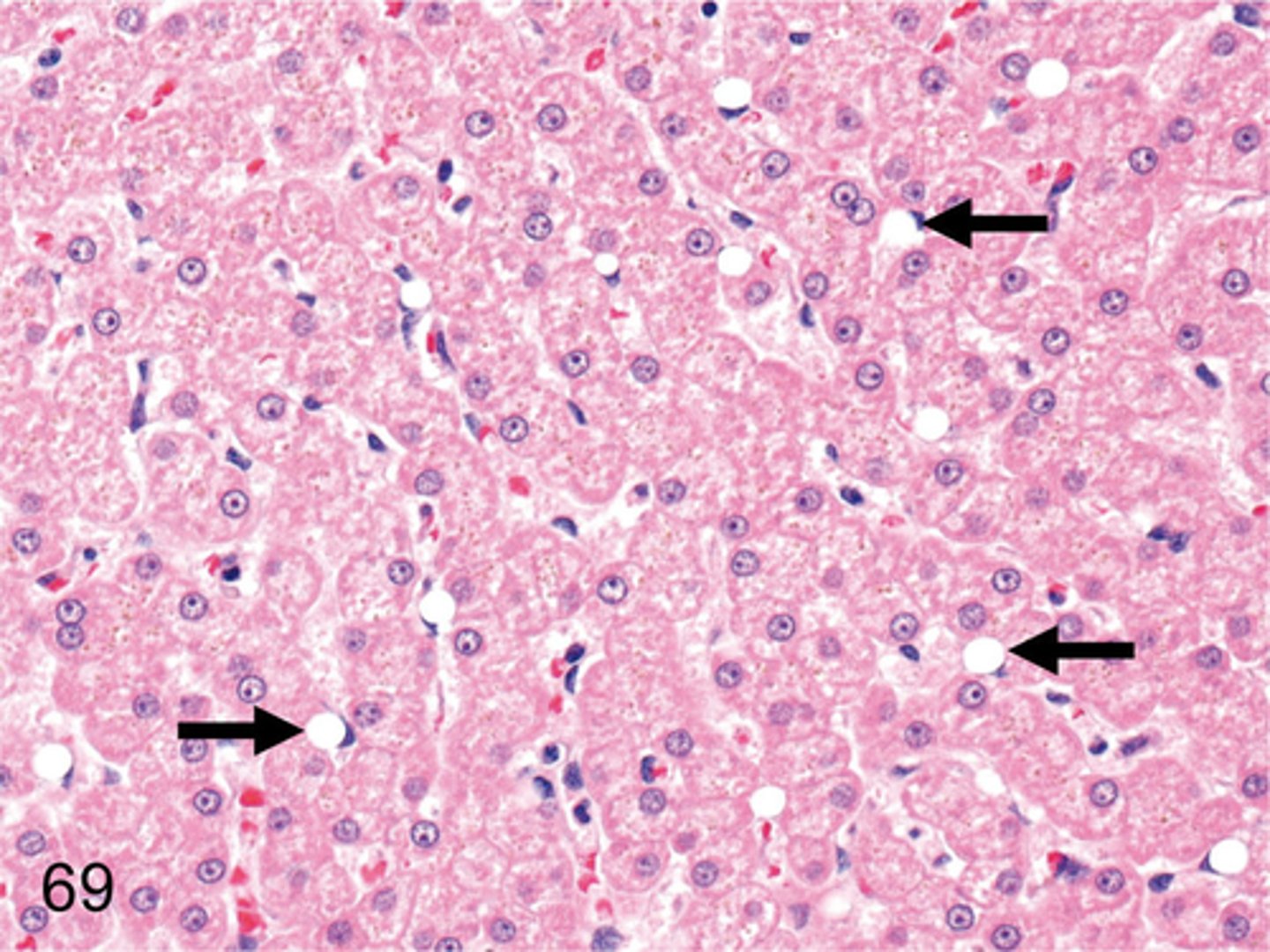
What are Kupffer cells and where do they originate?
Kupffer cells are specialized phagocytic cells found in the liver that originate from monocytes in the bloodstream.
THEY ARE BLACK DOTS, DARKER THAN HEPATOCYTES
Interspersed among the sinusoidal lining cells but form no junctions with them
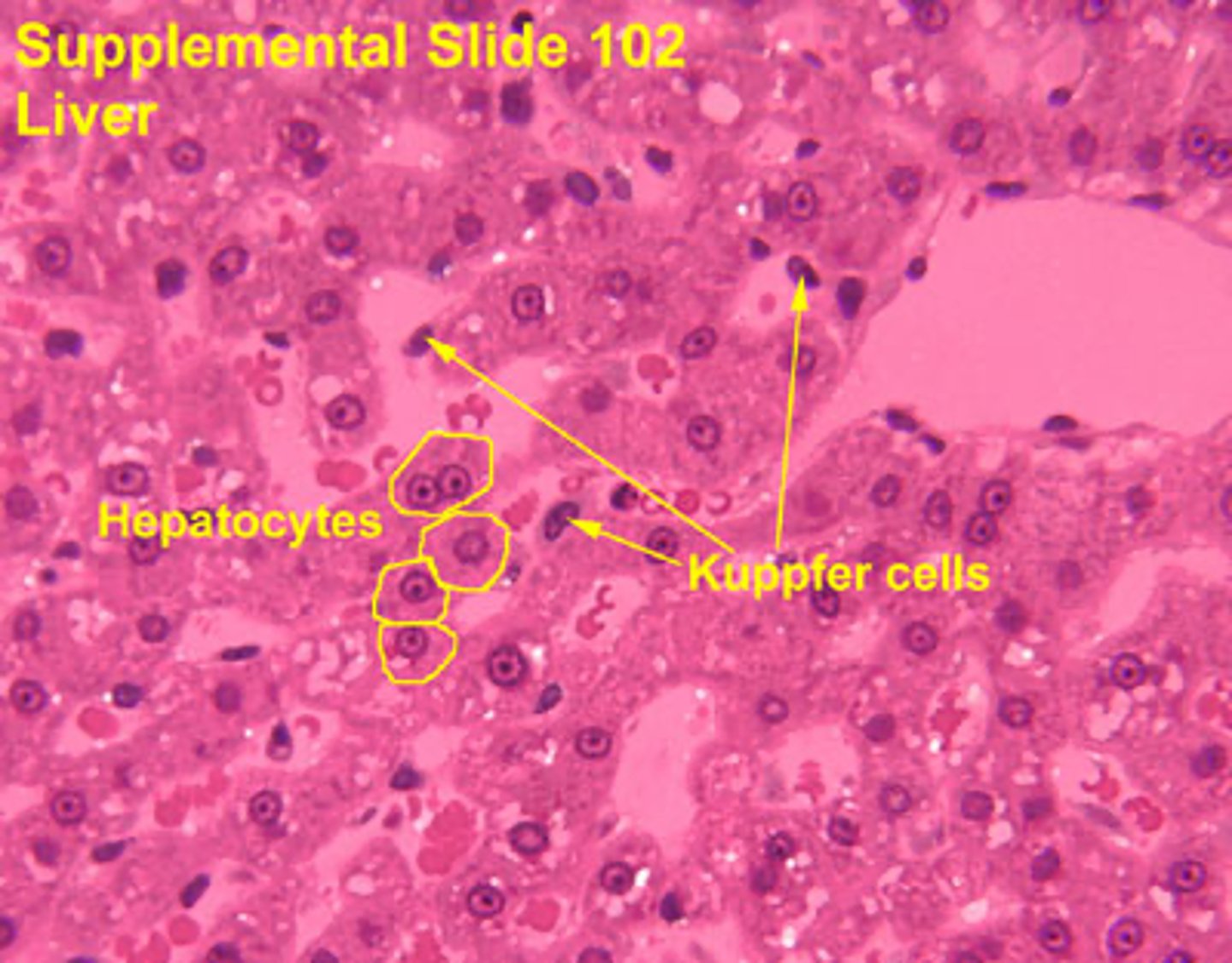
Kupffer cells function:
1. remove debris
2. remove old erythrocytes
3. remove cellular fragments from the bloodstream
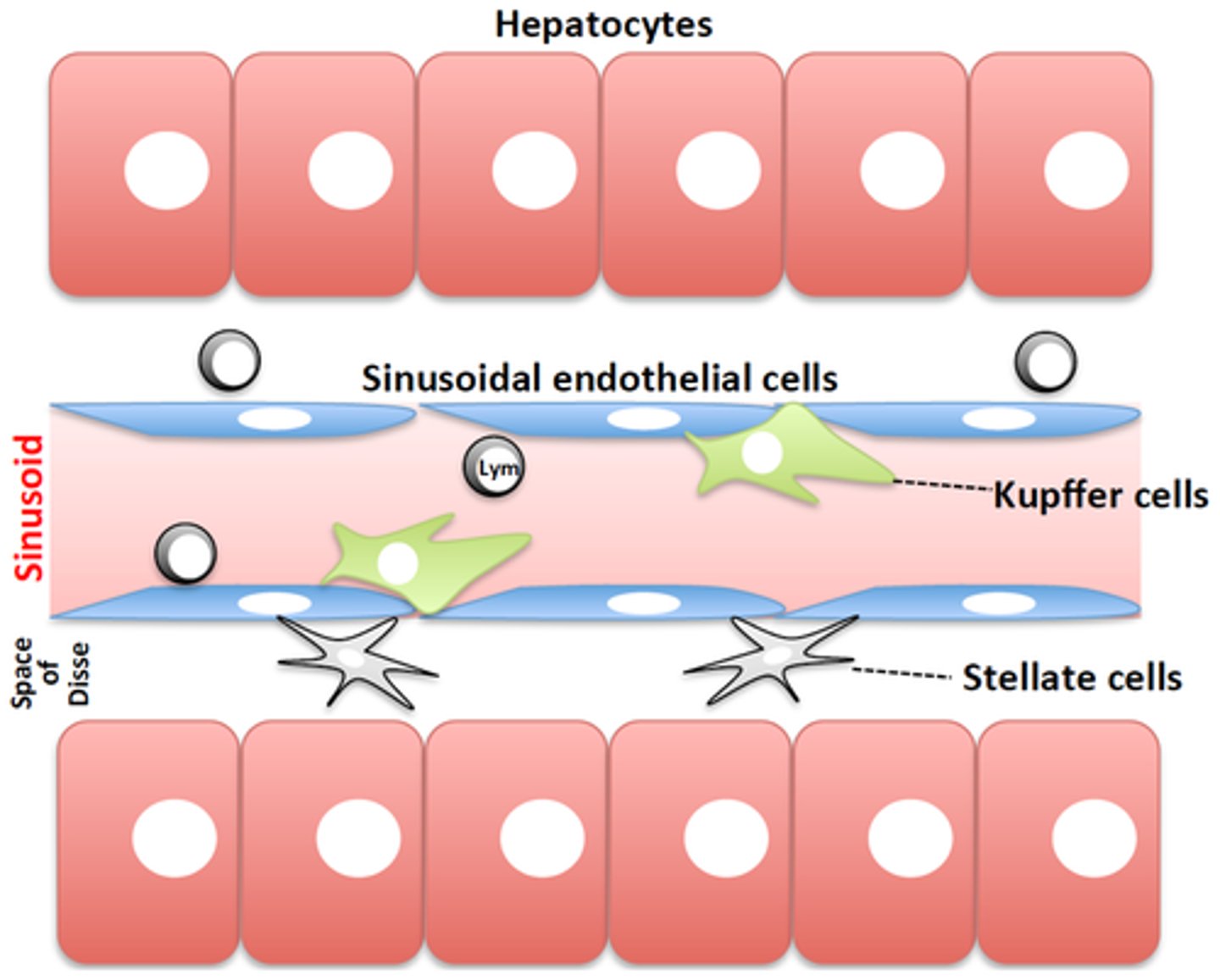
What are stellate macrophages in the liver?
Kupffer cells, are the liver's resident liver macrophages that remove pathogens, debris from the blood within the sinusoids.
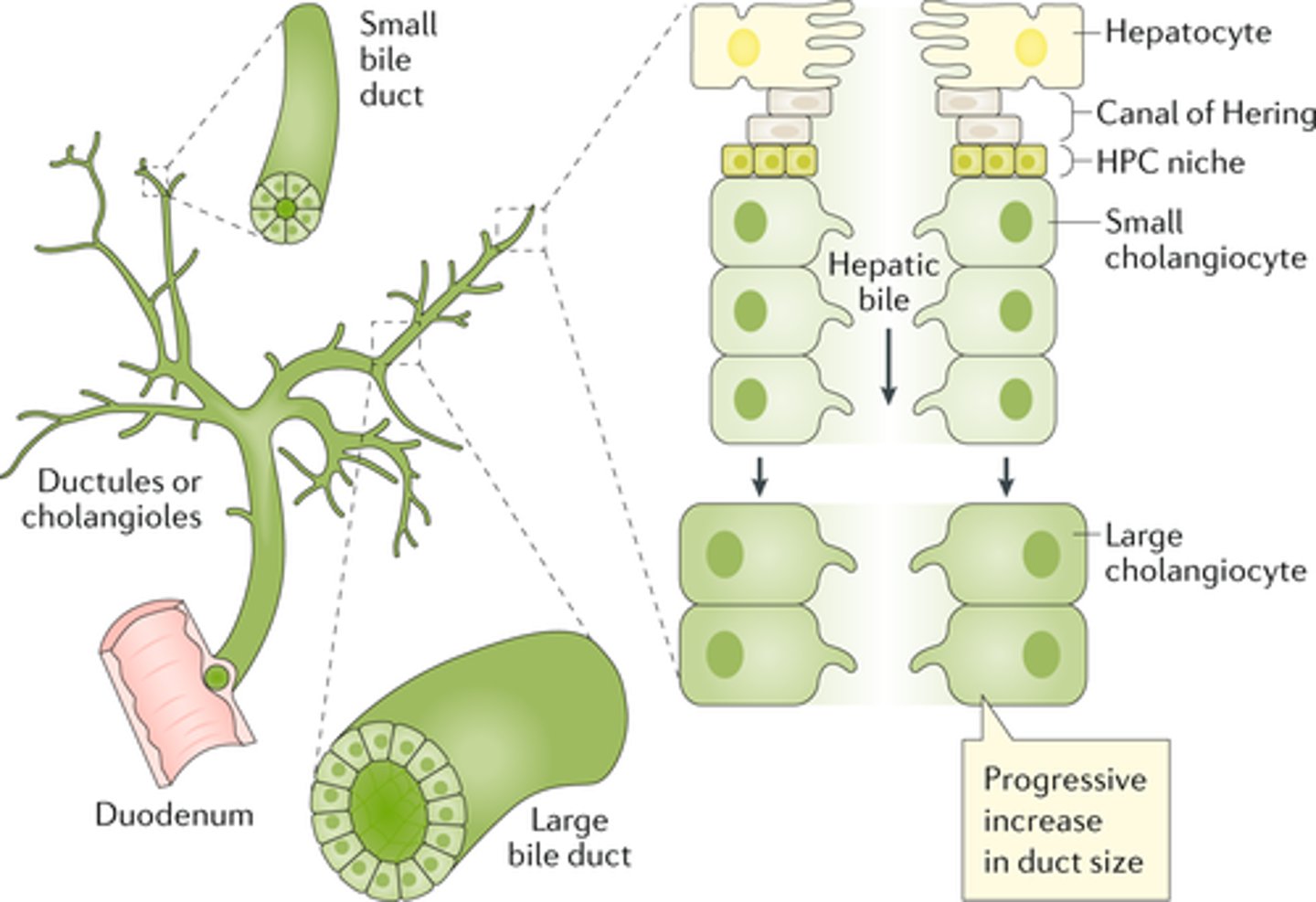
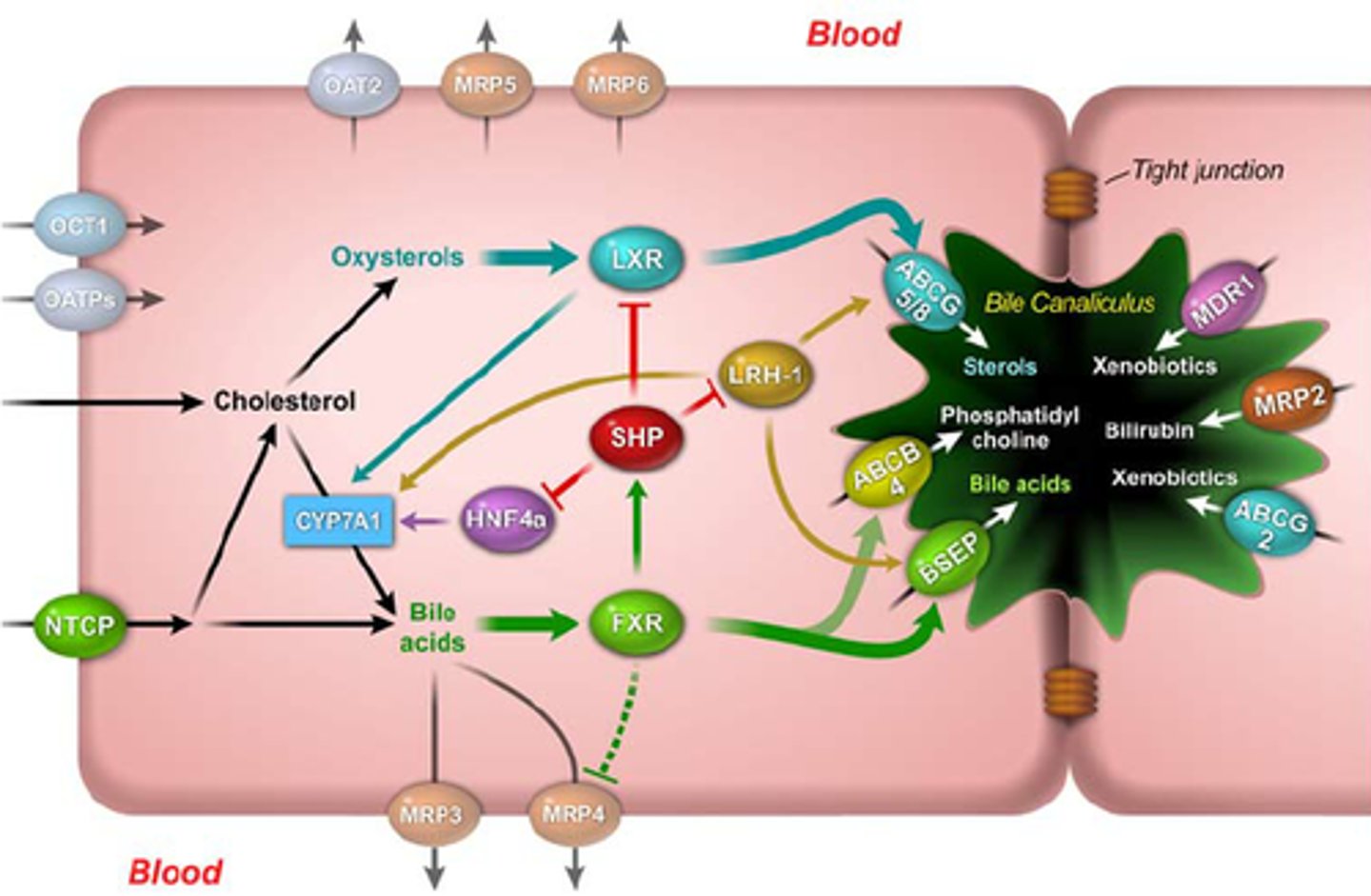
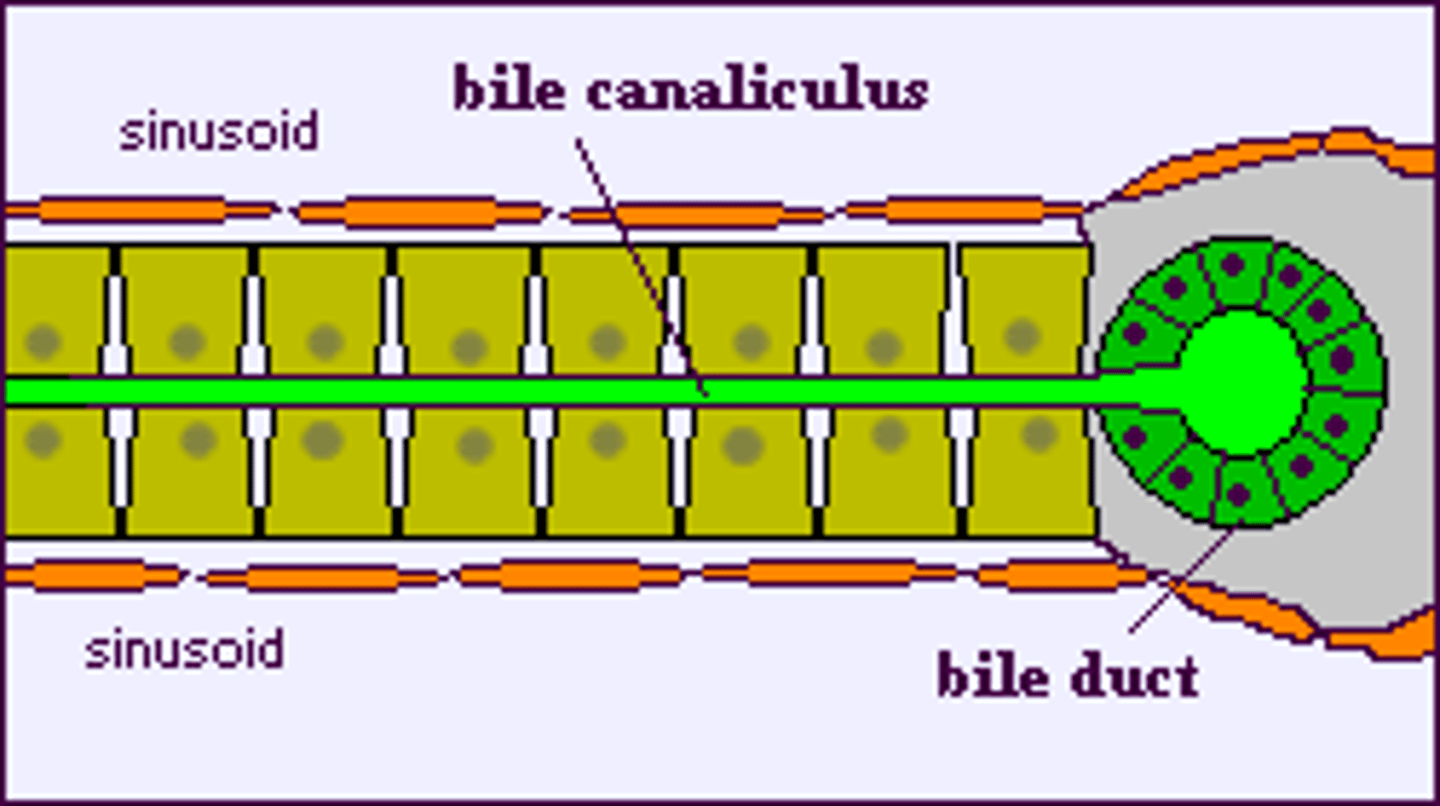
What are bile canaliculi?
ducts between hepatocytes (expanded intercellular spaces between adjacent hepatocytes) that collect and transport bile towards the bile ducts, AGAINTS THE DIRECTION OF BLOOD FLOW.
Bile flows toward the periphery of the classic liver lobule (opp direction of blood flow) and is transported by left and right hepatic ducts.
What is the function of the lymphatic system in the liver?
lymphatic ducts and terminal lymphatics, collects lymph from the space of Disse and carries it away from the liver.
What is the primary function of reticular fibers in the liver?
Reticular fibers are made up of type III collagen and provide a supporting framework (stroma) for the liver's cellular components (ex. hepatocytes).
helping maintain the organ's structural integrity (SPECIALLY OF SINUSOIDAL SPACE).
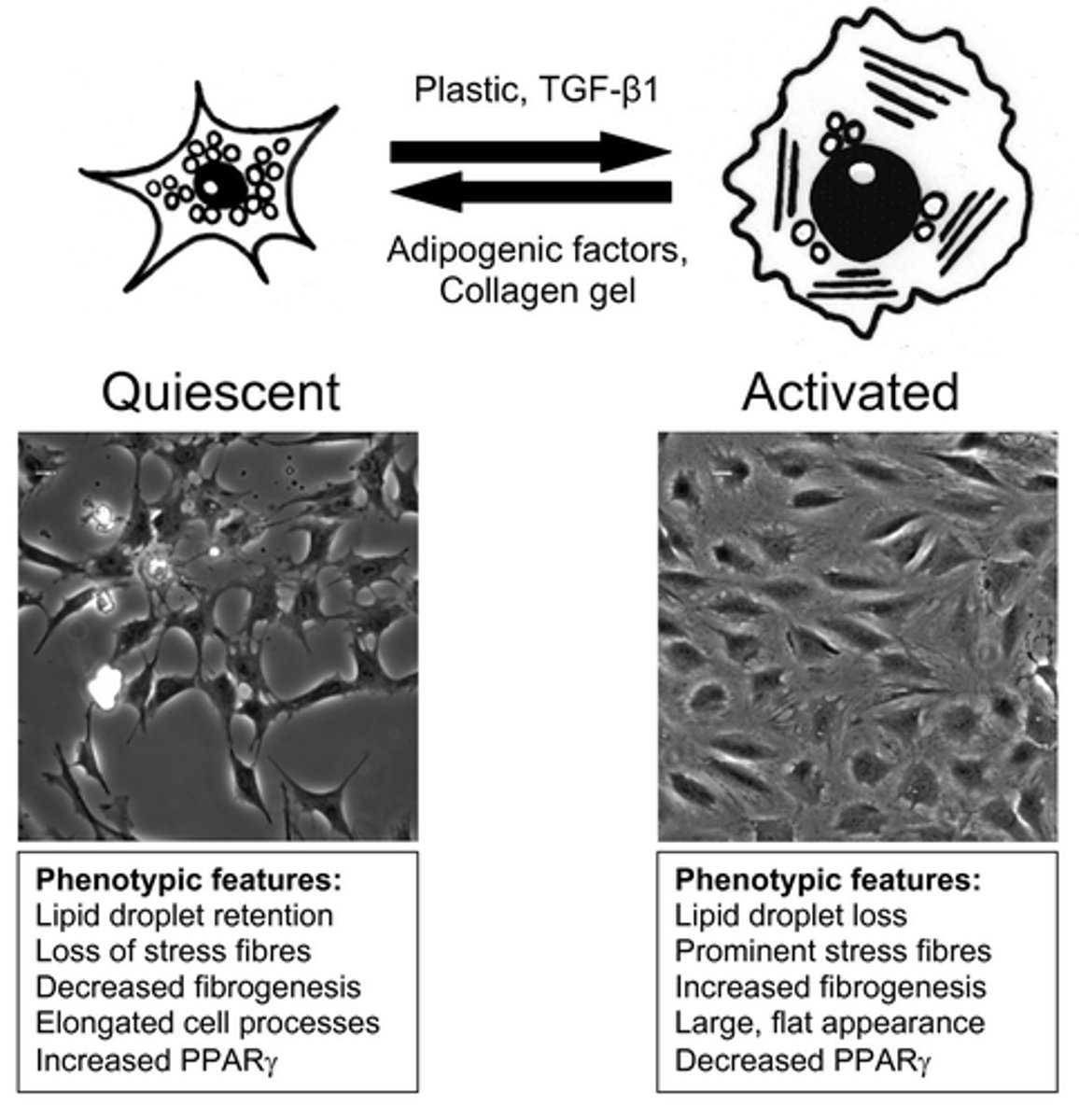
What are stellate cells and what do they store?
Stellate cells (Ito cells/perisinusoidal stellate cells), are fat-storing cells in the liver that preferentially store vitamin A.
What happens to stellate cells when the liver is compromised?
When the liver is compromised, stellate cells can activate, change phenotype and:
1. synthesise collagen, contributing to fibrosis
2. differentiate into myofibroblasts to control blood flow into sinusoid triads
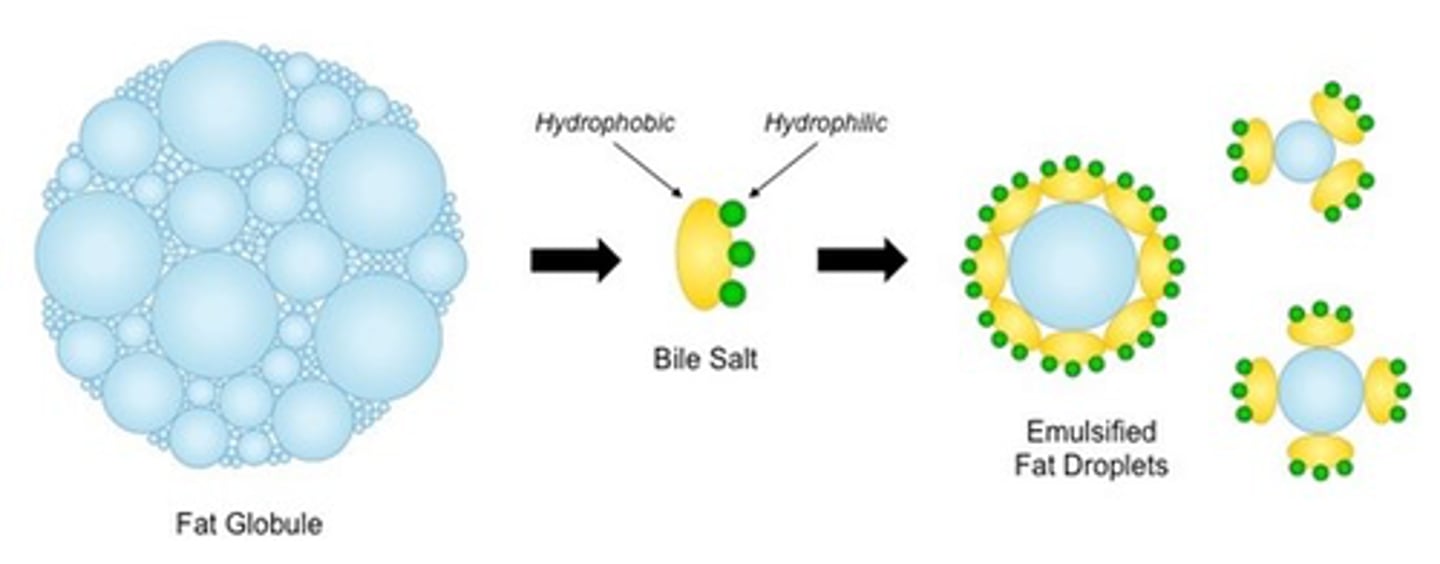
What is the primary function of bile acids in digestion?
Bile acids emulsify fats, which facilitates the breakdown and absorption of lipids in the small intestine.
By emulsifying fats into smaller droplets, bile acids increase the surface area for digestive enzymes to act upon
What percentage of bile acids are recirculated, and where does this occur?
90% of bile acids are recirculated.
This occurs in the enterohepatic circulation, where bile acids are reabsorbed from the intestines and returned to the liver.
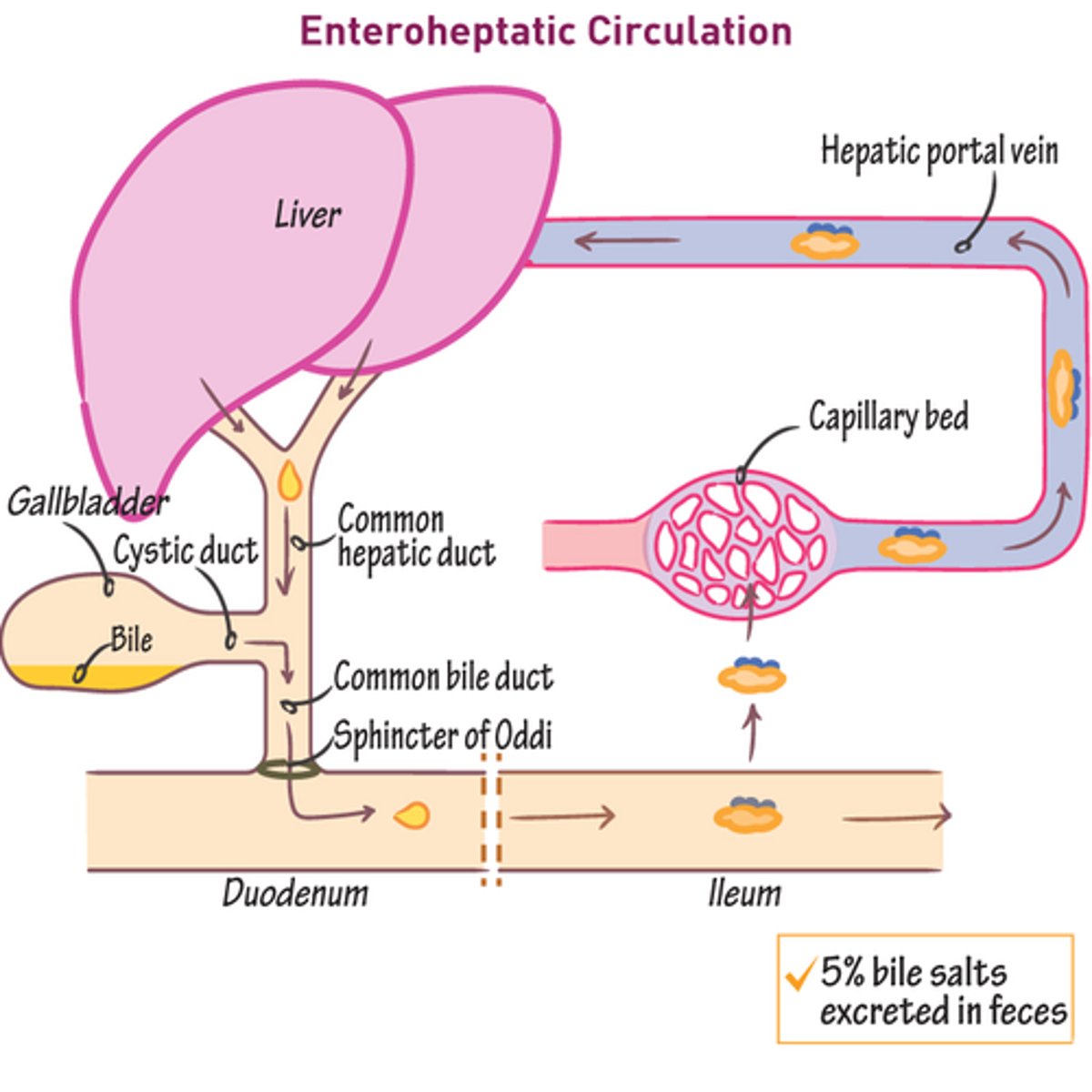
What happens to the remaining bile acids that are not recirculated?
The remaining 10% of bile acids are synthesized de novo (newly) in the liver to replace those lost in feces.
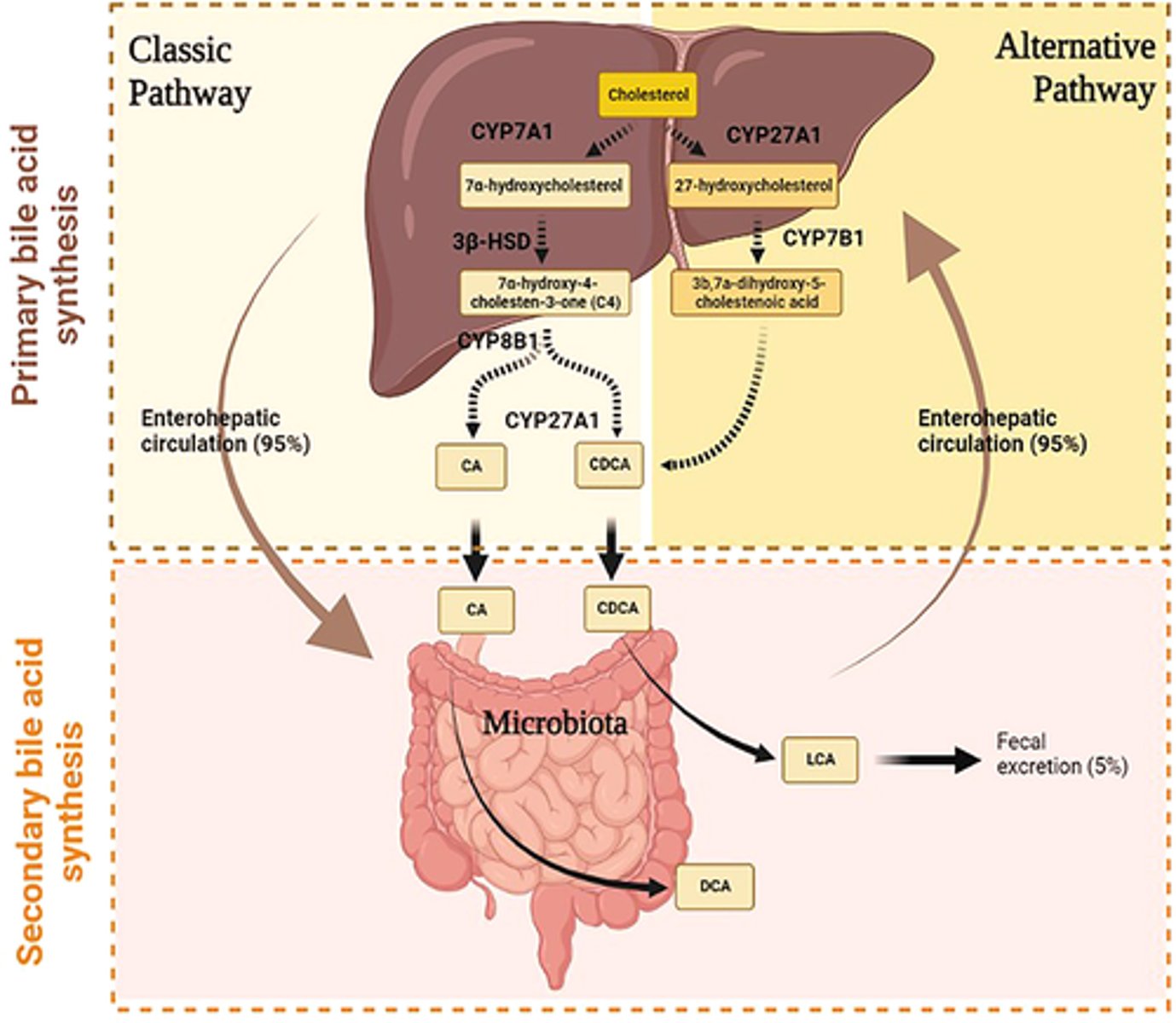
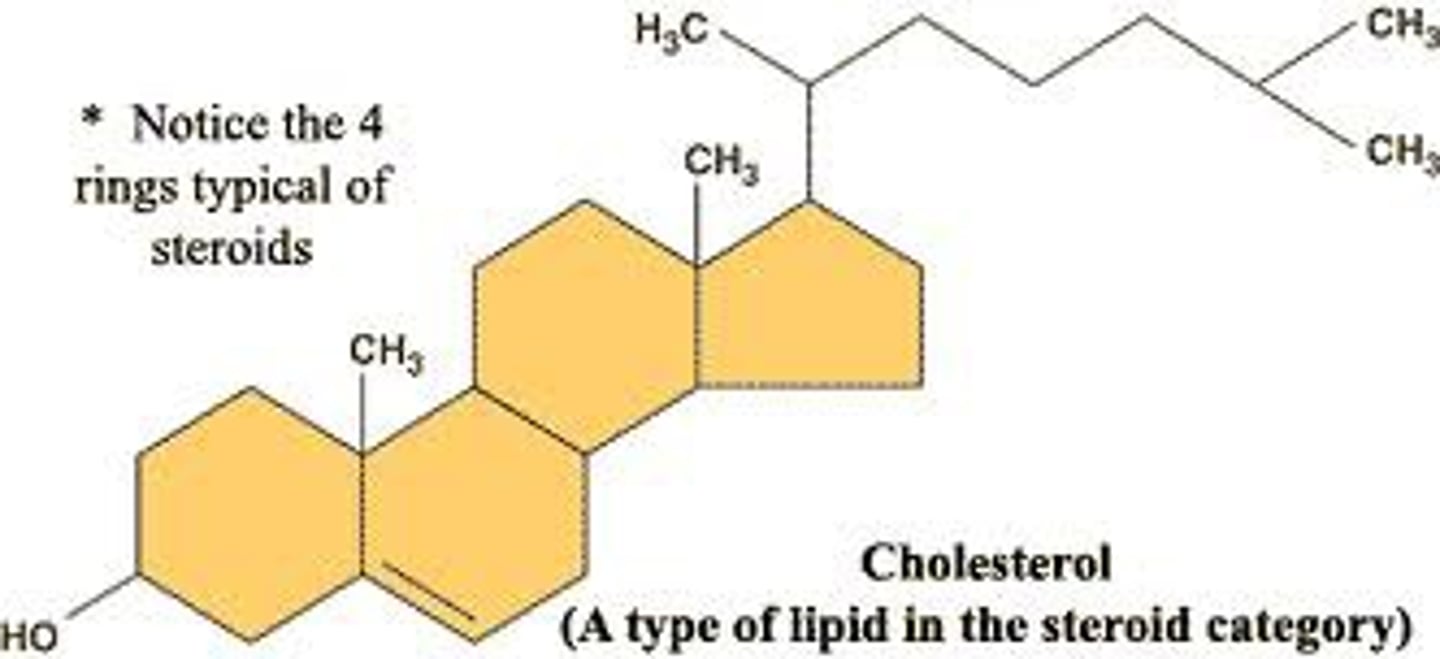
Where are bile acids synthesized, and from what molecule?
Bile acids are synthesized in the liver cells from cholesterol.
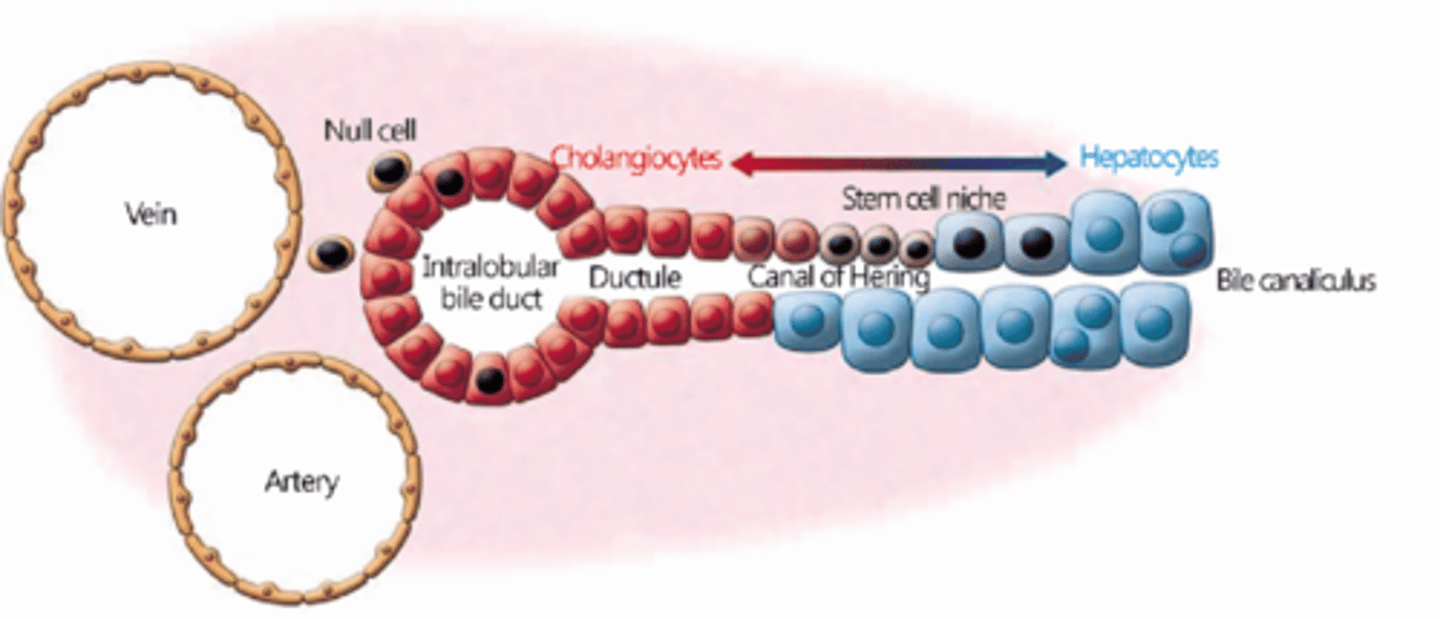
What is the role of bile canaliculi in bile flow?
Bile canaliculi receive the liver's exocrine secretion (bile) and carry it to the canals of Hering (bile ductules) at the very periphery of classic liver lobules.
Bile canaliculi are channels within the liver for bile flow. They are limited only by the plasma membranes of two adjacent hepatocytes (produce bile), which extend a small number of microvilli into their interiors to increase surface area for secretion and absorption.
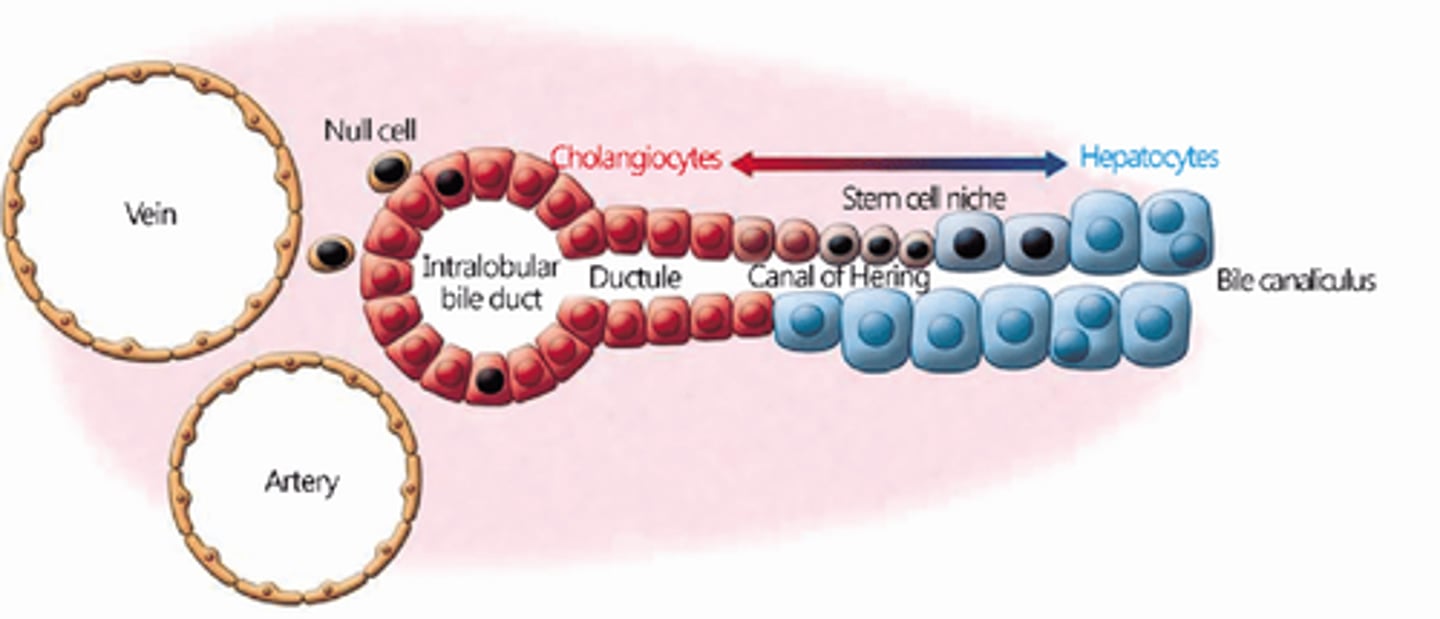
What composes the canals of Hering?
The canals of Hering are composed of modified hepatocytes and low cuboidal cholangiocytes (duct cells).
What do hepatocytes extend into bile canaliculi?
microvilli: increase the surface area within these channels.
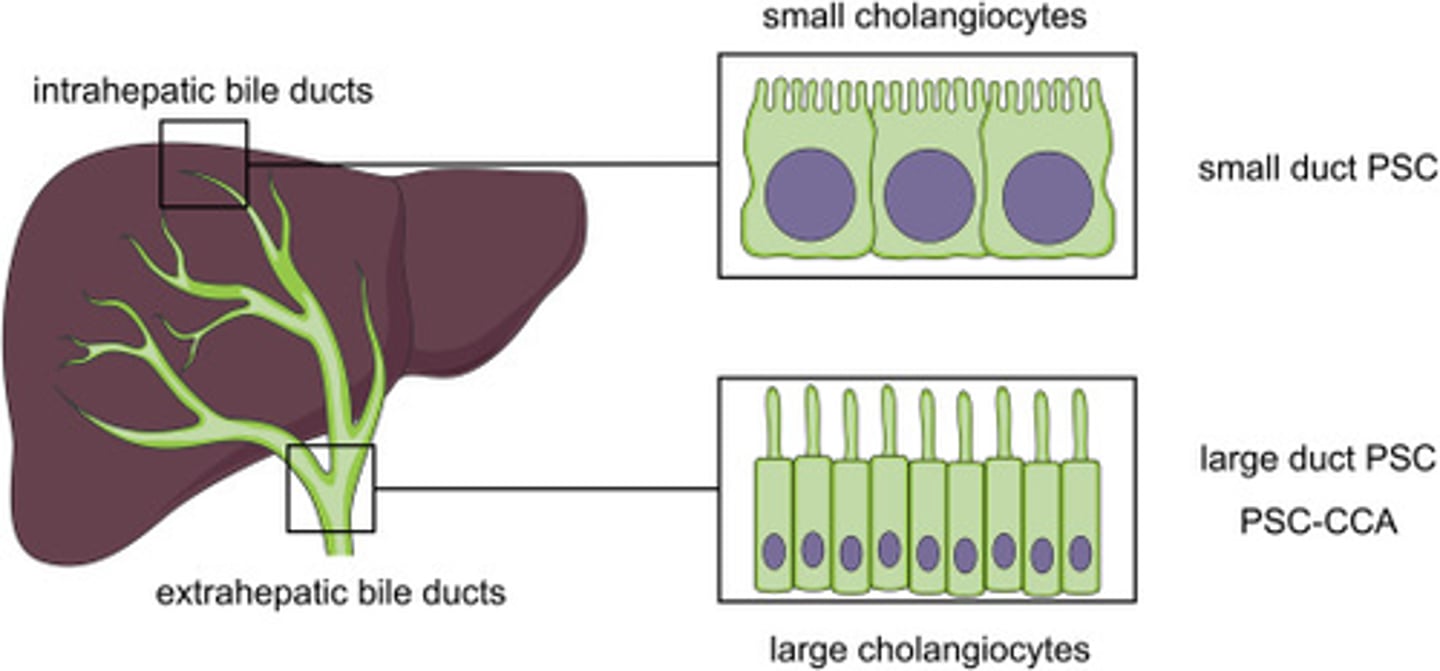
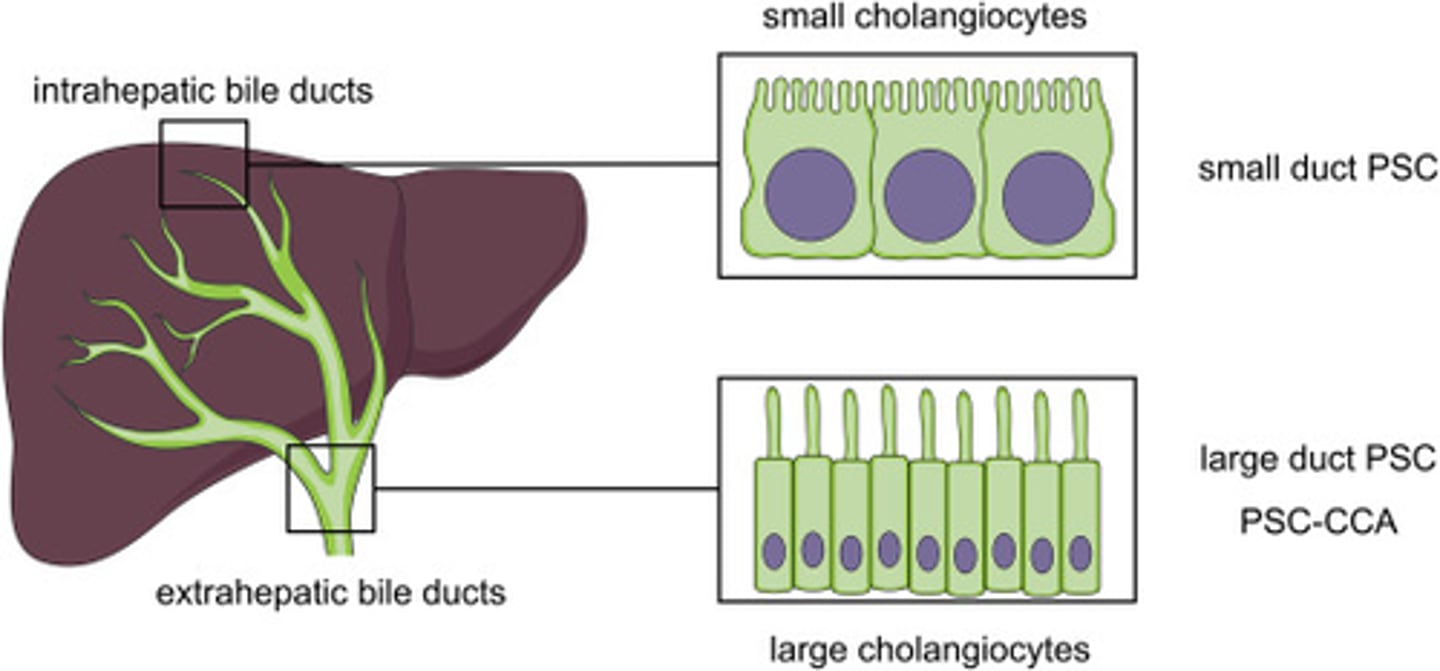
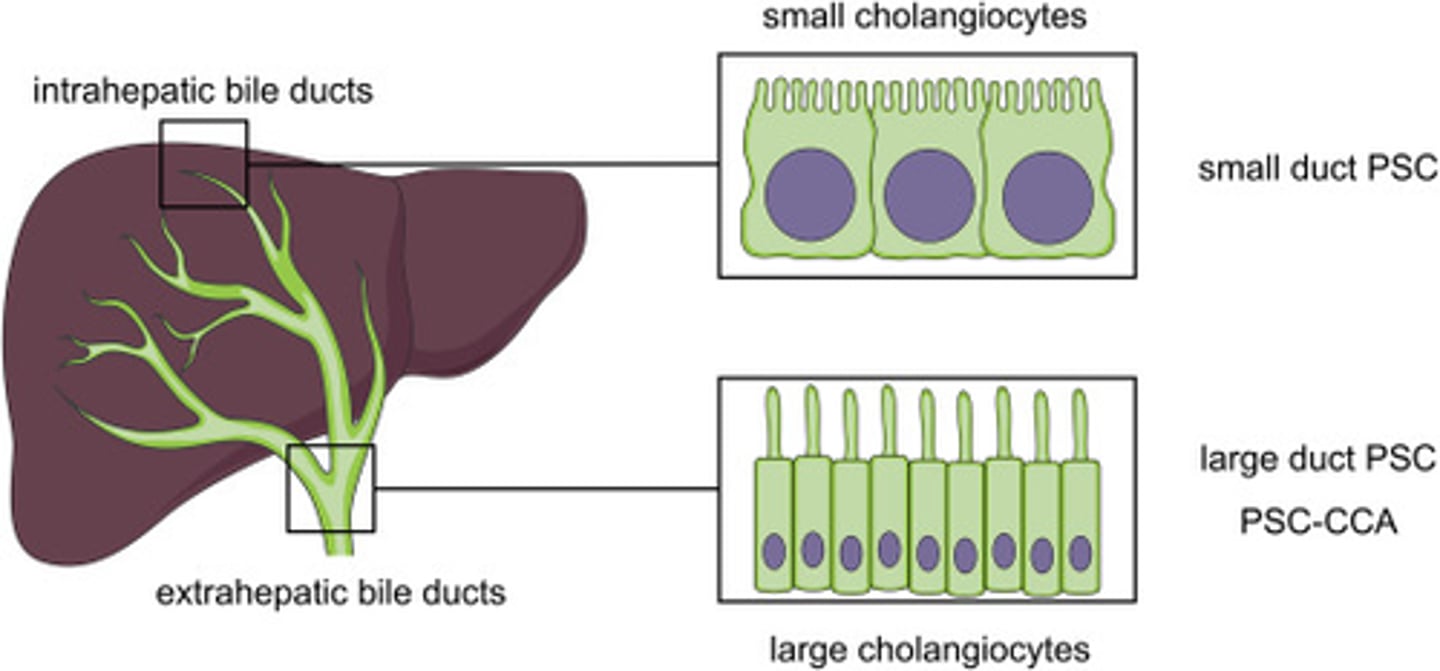
Where are bile ducts located and what are they composed of?
Bile ducts are located in the portal areas of the liver and are composed of a single layer of cuboidal shaped cholangiocytes.
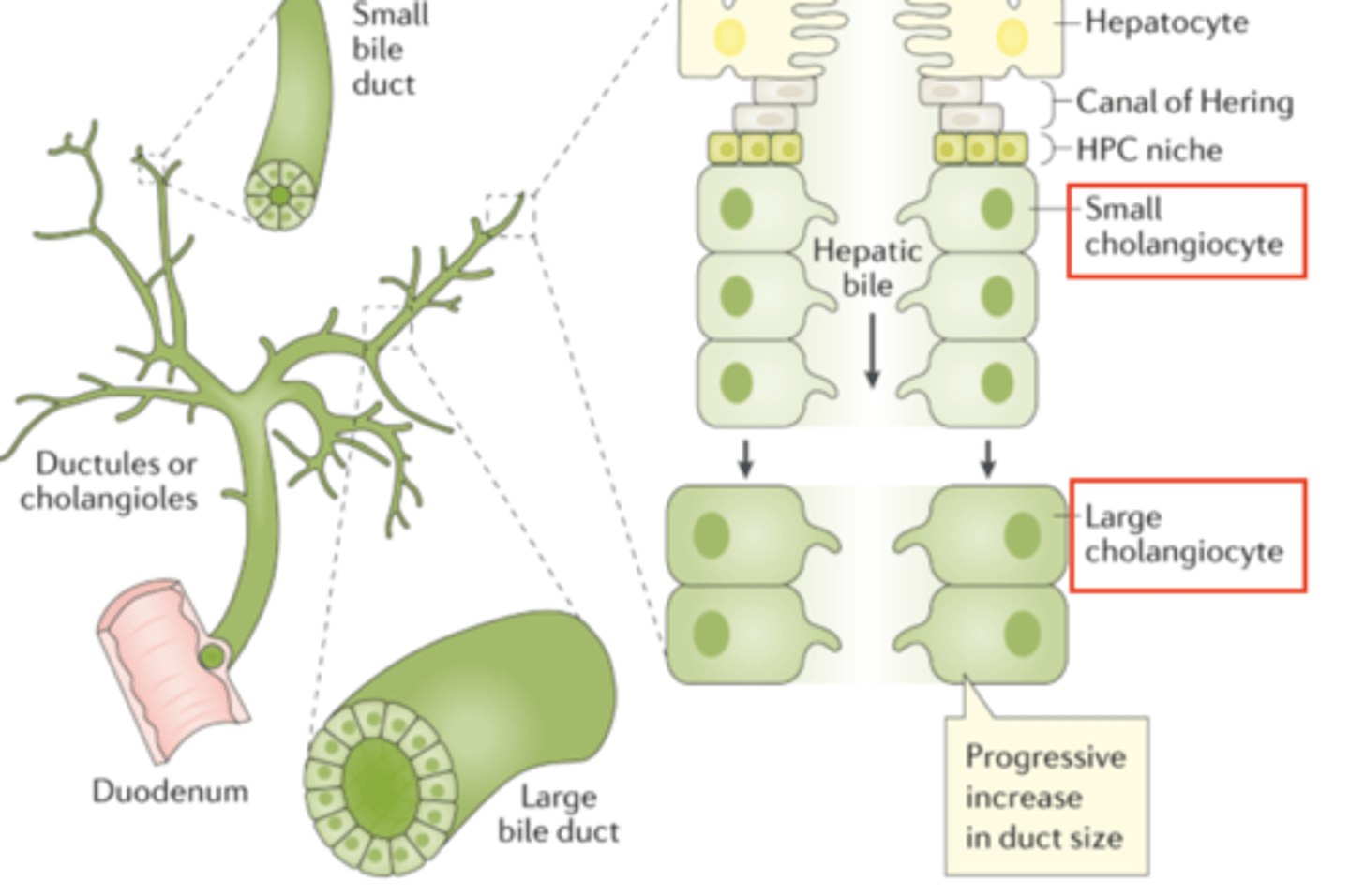
What is the structure and function of the apical surface of cholangiocytes?
The apical surface of each cholangiocyte faces the lumen of the bile duct and has numerous short microvilli (INCREASE SA) and a single long primary cilium.
THE SINGLE LONG PRIMARY CILIUM MOITORS THE BILE FLOW AND COMPOSITION WITHIN THE BILE DUCT
How do endothelial cells in bile ducts differ from cholangiocytes?
Endothelial cells are flat and never round like duct cells, which are cuboidal.
ENDOTHELIAL CELLS: FLAT
CHOLANGIOCYTES: CUBOIDAL
What do bile ducts receive and from where?
Bile ducts receive bile from the canals of Hering.
What happens to bile ducts after they receive bile?
After receiving bile, the bile ducts enlarge and fuse to form the hepatic ducts (have stratified epithelium of cholangiocytes, transport bile out of the liver at the porta hepatic)
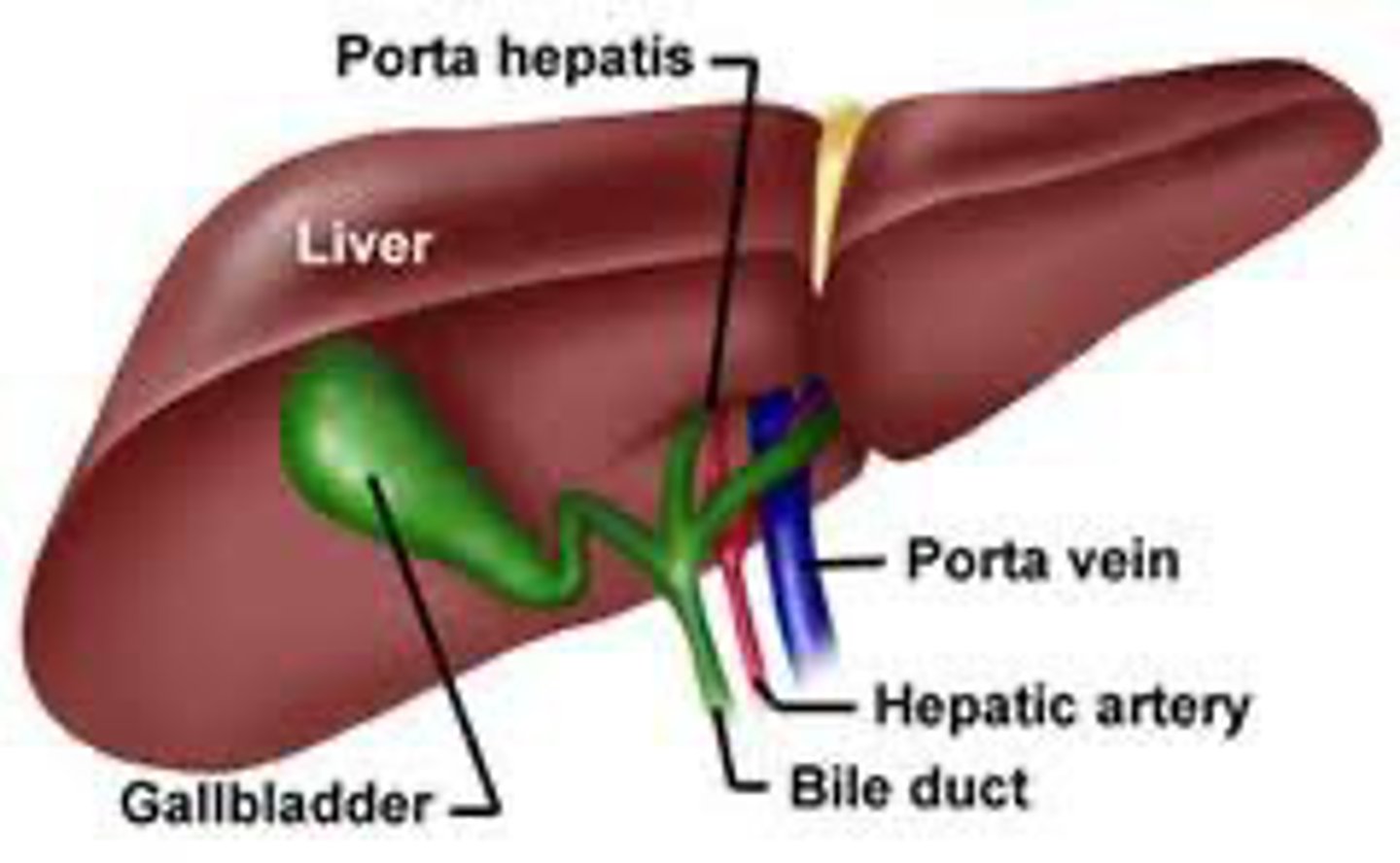
What kind of epithelium do the hepatic ducts have?
The hepatic ducts have a stratified epithelium of cholangiocytes.
REMEMBER: CHOLANGIOCYTES ARE CUBOIDAL NOT FLAT LIKE NORMAL EPITHELIUM
Where do the hepatic ducts transport bile to?
The hepatic ducts transport bile to the porta hepatis, where it leaves the liver.
What is the function of the right hepatic duct?
The right hepatic duct collects bile from the right lobe of the liver and is one of the two main ducts that drain bile out of the liver.
What is the function of the left hepatic duct?
The left hepatic duct collects bile from the left lobe of the liver and, along with the right hepatic duct, forms the common hepatic duct that drains bile out of the liver.
How is the common hepatic duct formed?
The common hepatic duct is formed by the convergence of the right and left hepatic ducts just outside the liver.
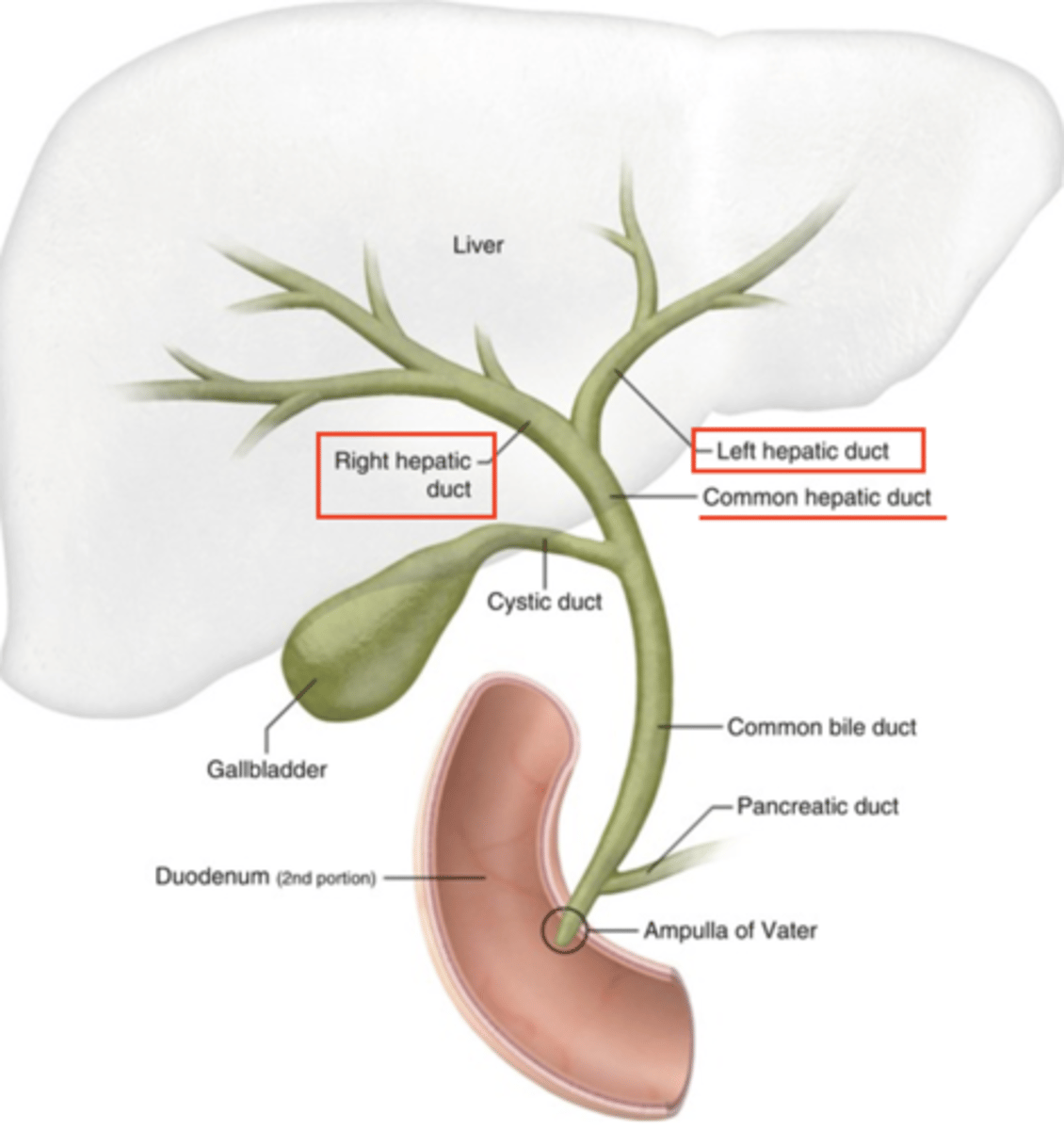
What does the common hepatic duct join to form the common bile duct?
The common hepatic duct joins with the cystic duct from the gallbladder to form the common bile duct.
common hepatic duct + cyst duct: common bile duct
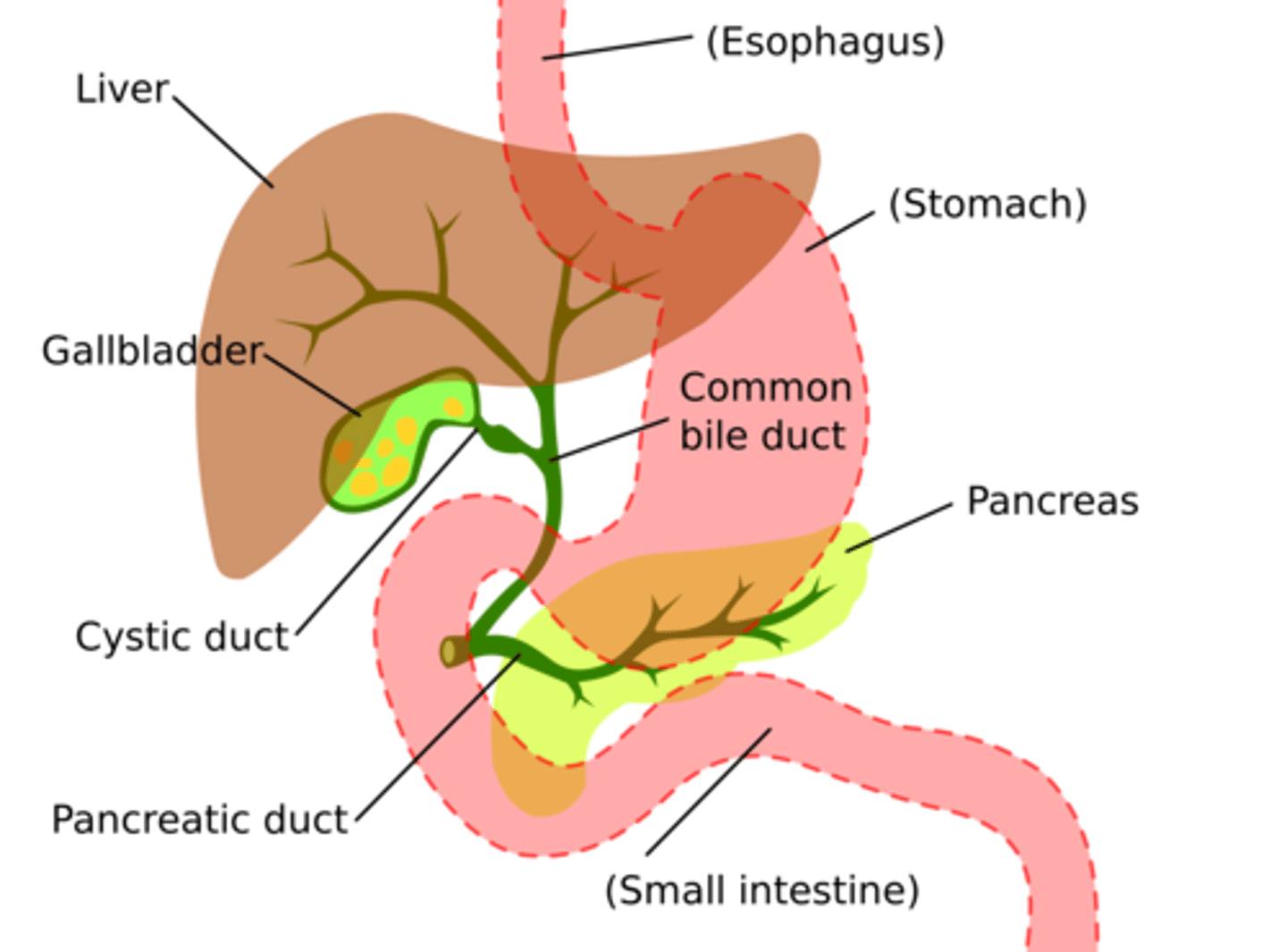
Where does the common bile duct release its contents?
The common bile duct releases bile into the duodenum of the small intestine at the ampulla of Vater, usually in conjunction with the release of pancreatic juices.
What is the Space of Moll?
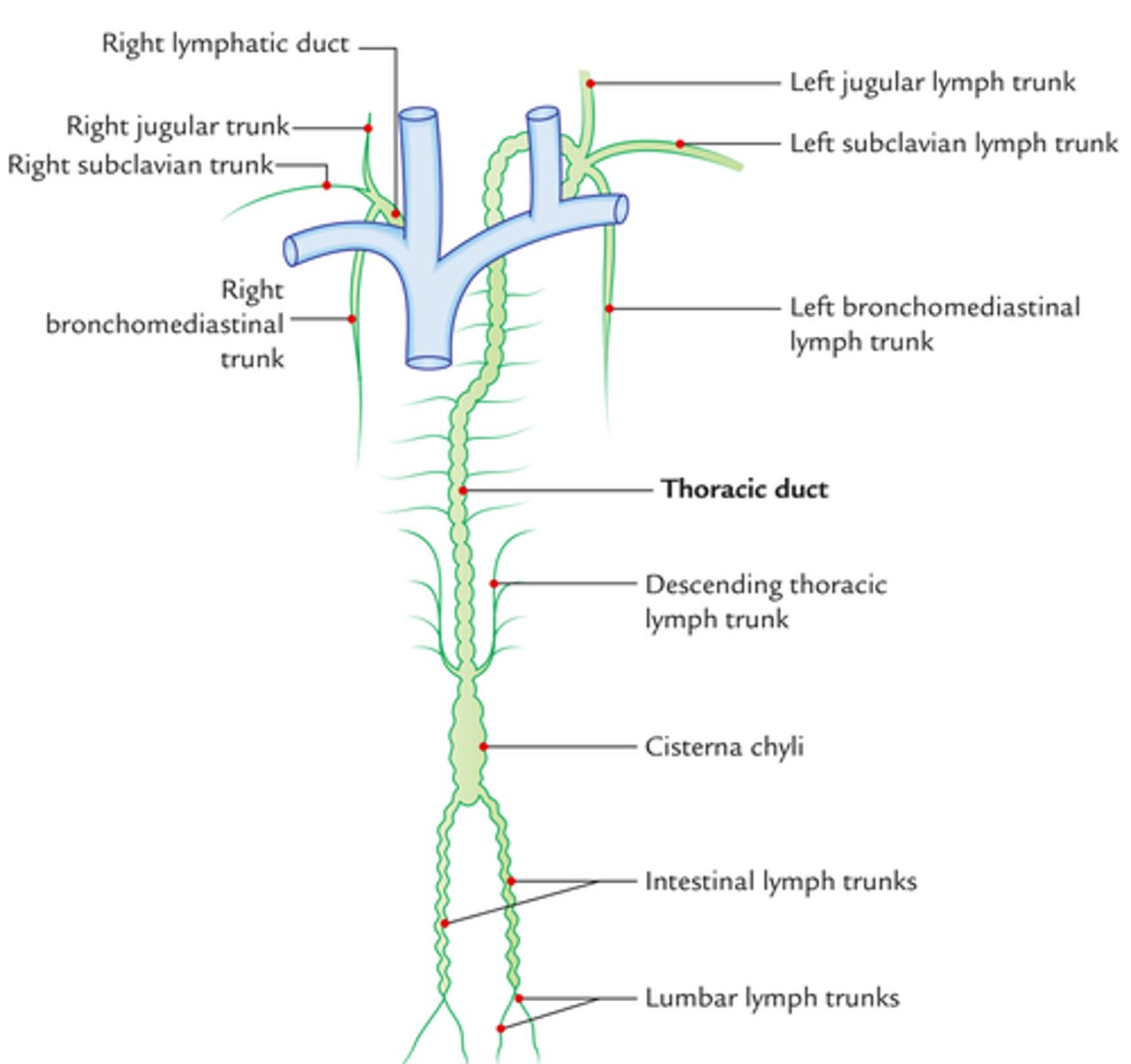
The Space of Moll refers to branches of the lymph vessels located in the portal areas of the liver.
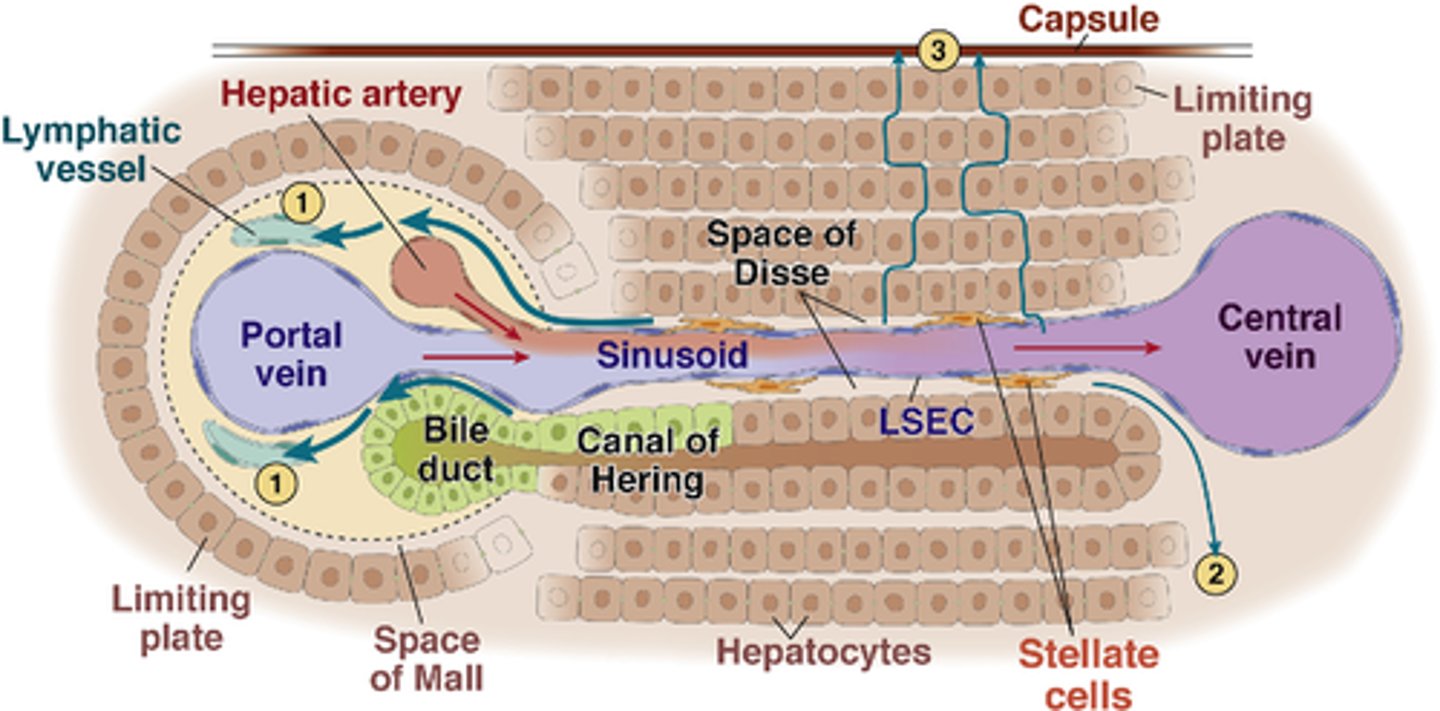
What happens to lymph vessels in the Space of Moll?
lymph vessels merge and increase in size, eventually forming one or two larger lymph vessels.
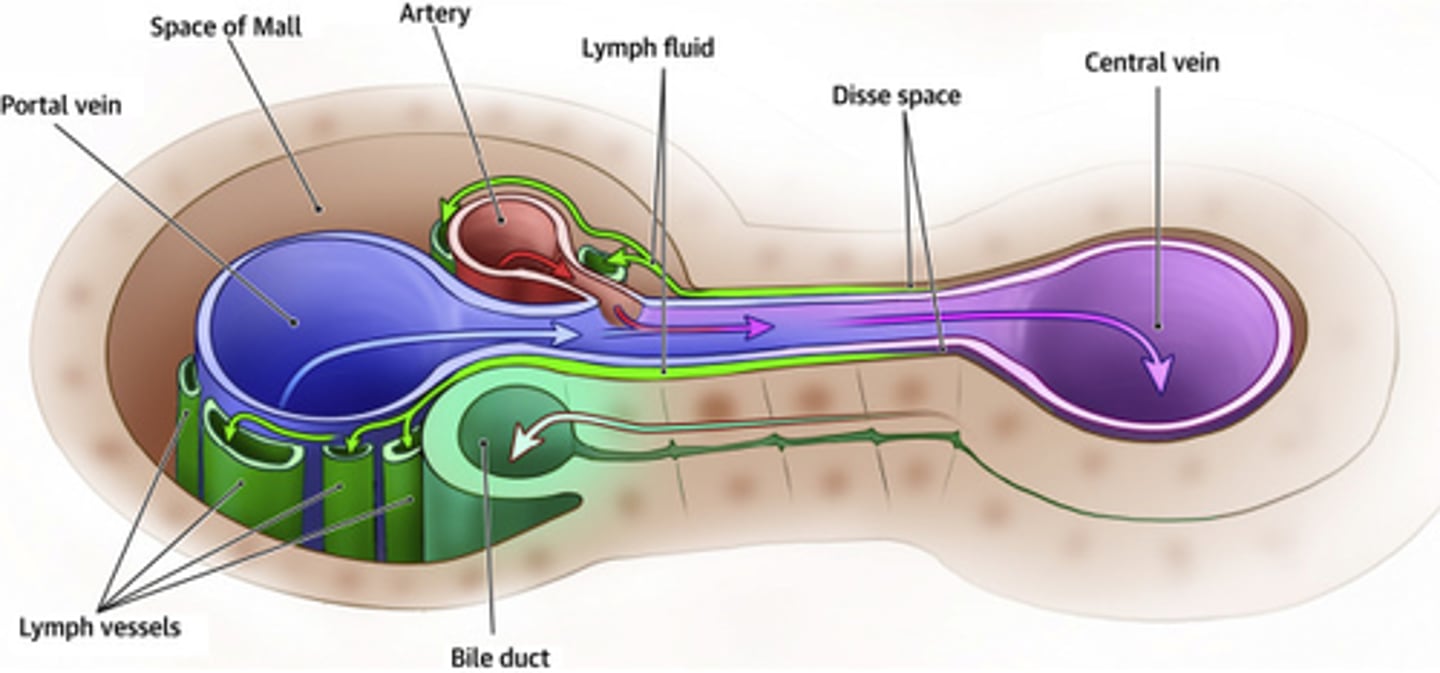
Where do the larger lymph vessels from the Space of Moll drain?
The larger lymph vessels from the Space of Moll join the thoracic duct: main lymphatic vessel that returns lymph into the blood vascular system.
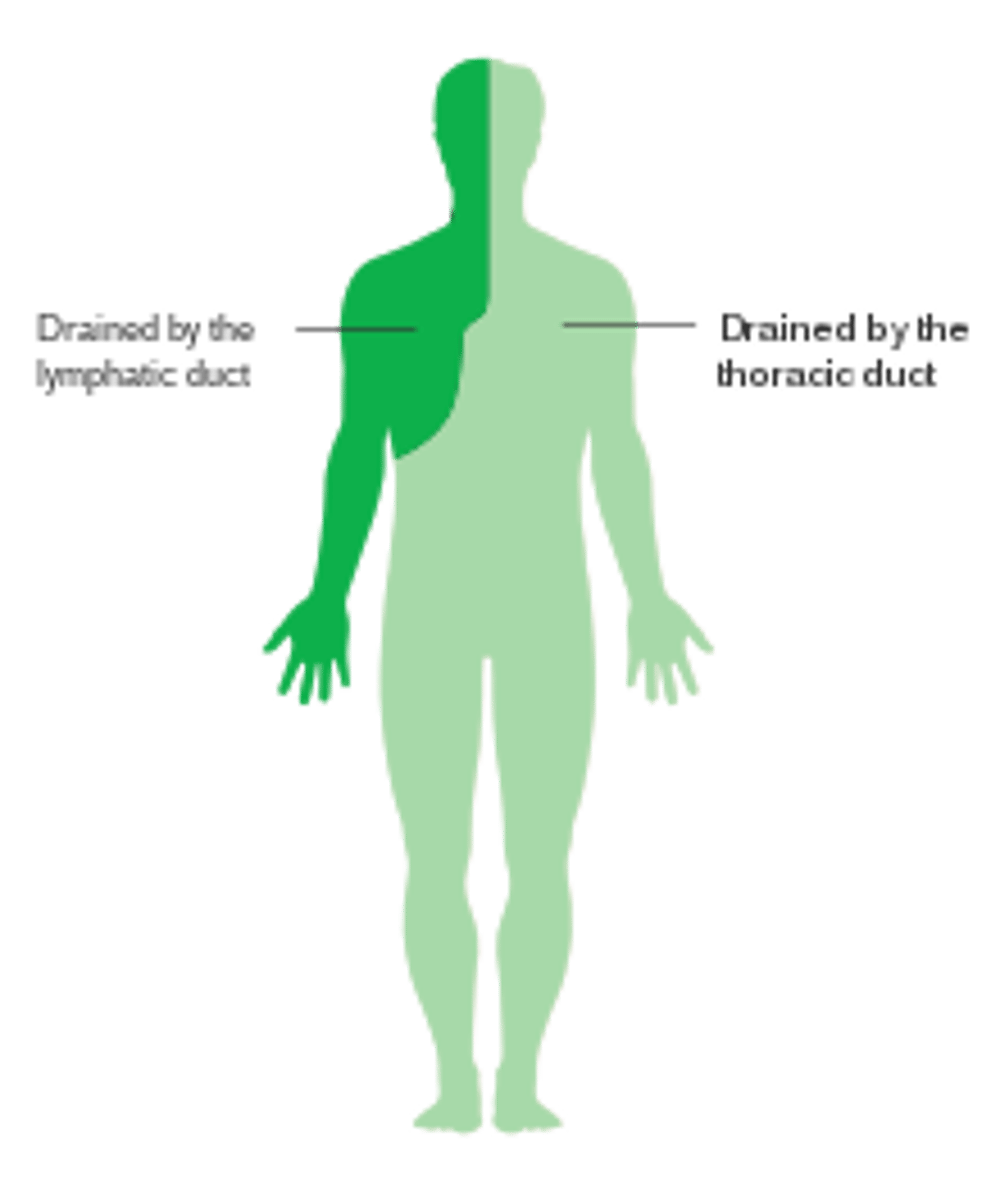
At what point does the thoracic duct return lymph into the blood vascular system?
The thoracic duct returns lymph to the blood vascular system at the junction of the left subclavian and left internal jugular veins.
What are the characteristics of hepatocytes?
1. Large polyhedral cells
2. Abundant rough endoplasmic reticulum (RER)
3. Abundant smooth endoplasmic reticulum (SER)
4. Numerous mitochondria
5. Numerous lysosomes
6. Numerous peroxisomes
7. Several Golgi complexes
8. Many lipid droplets
9. Many glycogen deposits
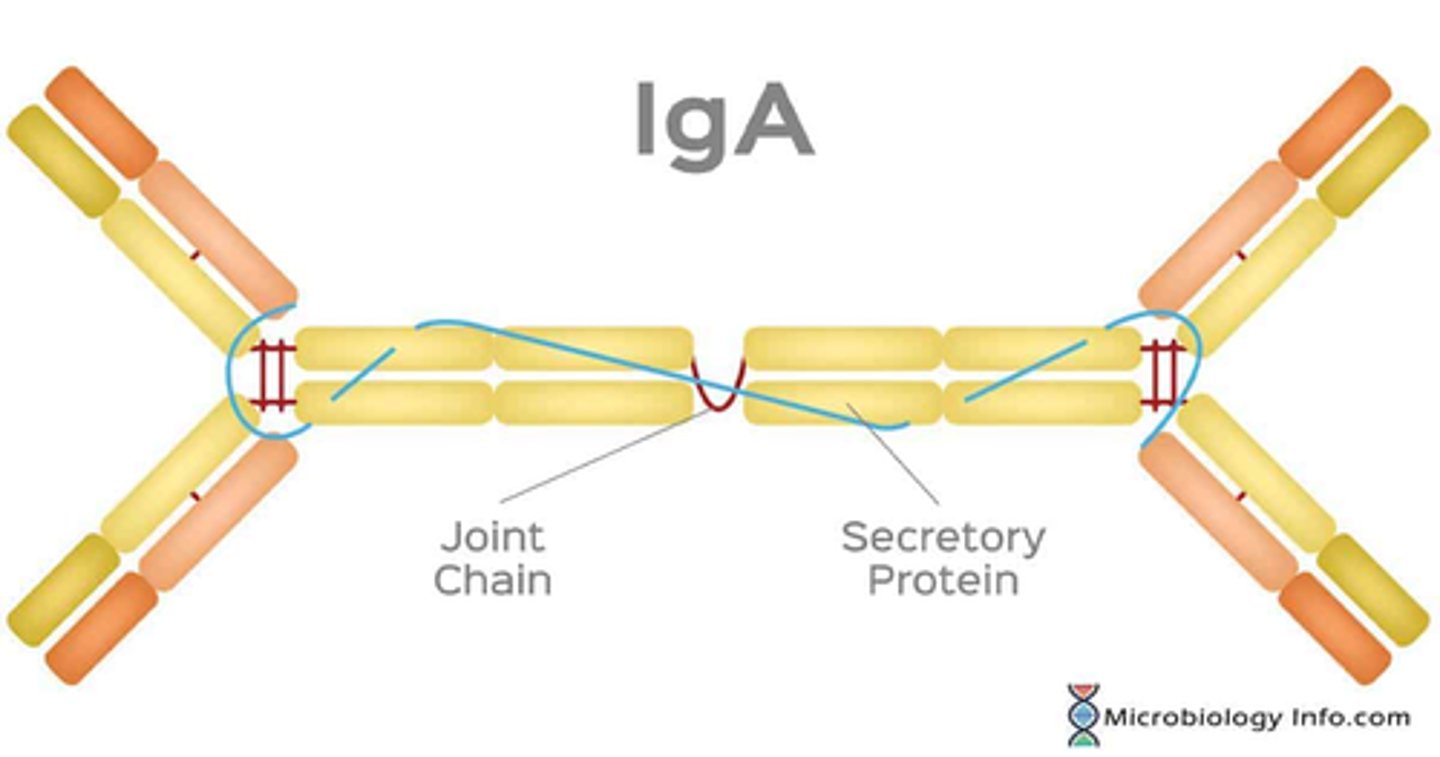
What is the function of IgA transfer in hepatocytes?
IgA transfer involves the uptake of IgA across the space of Disse and its release into bile canaliculi.
IgA is then transported through the hepatobiliary duct system to the intestine, where it plays a role in immunologic protection. This process is part of the enterohepatic circulation.
Do hepatocytes have a single nucleus?
Most hepatocytes have one round central nucleus, but approximately 25% of the cells are binucleated.
What is the function of Ito cells in the liver?
Ito cells, also known as hepatic stellate cells, are responsible for storing vitamin A within the liver.
What is the lifespan of hepatocytes?
5 months, after which they are replaced.

What cellular structures are prominently featured in hepatocytes?
1. endoplasmic reticulum (ER) (PRODUCTION)
2. mitochondria (M) (ENERGY FOR EXCHANGE)
3. bile canaliculi
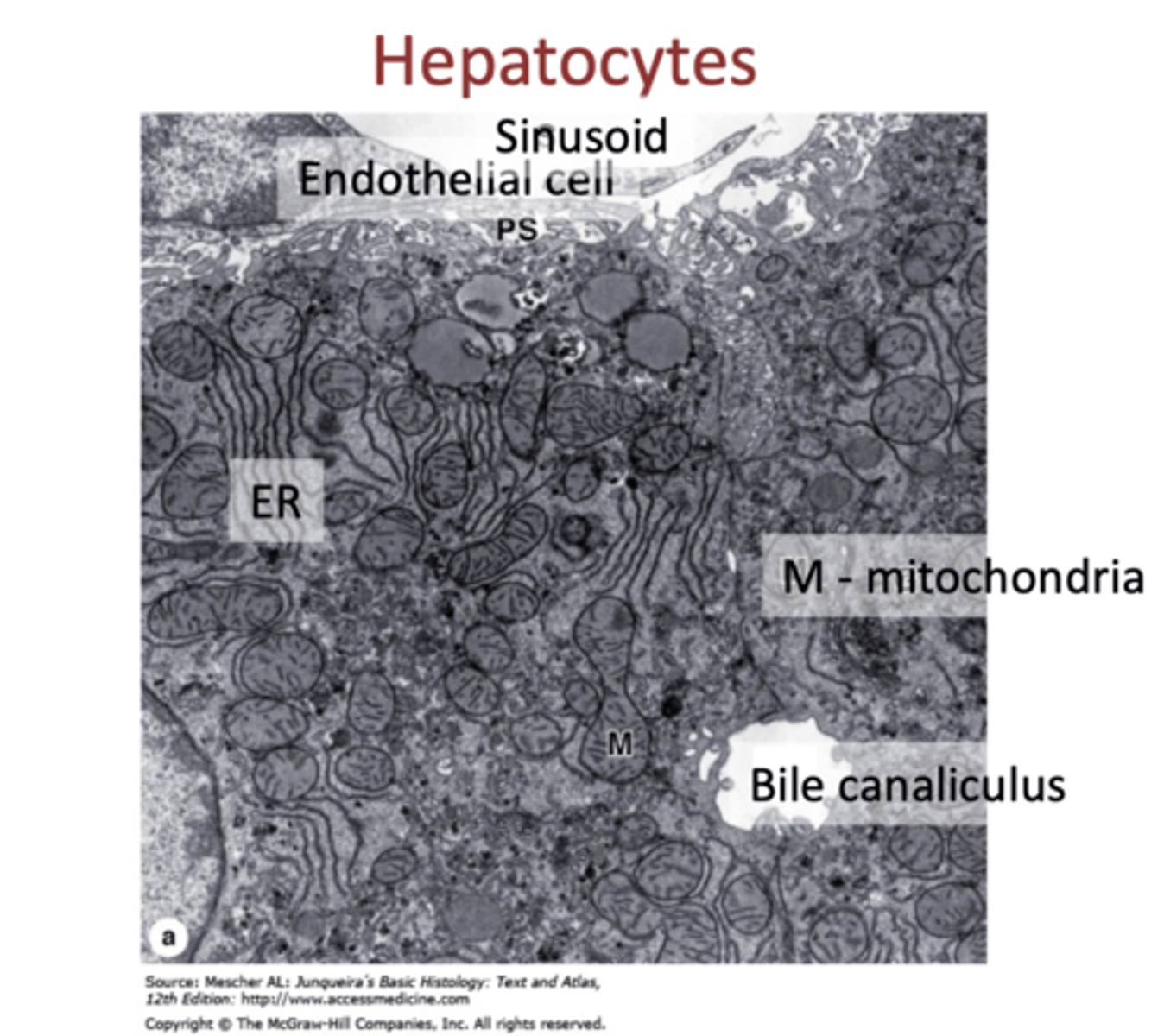
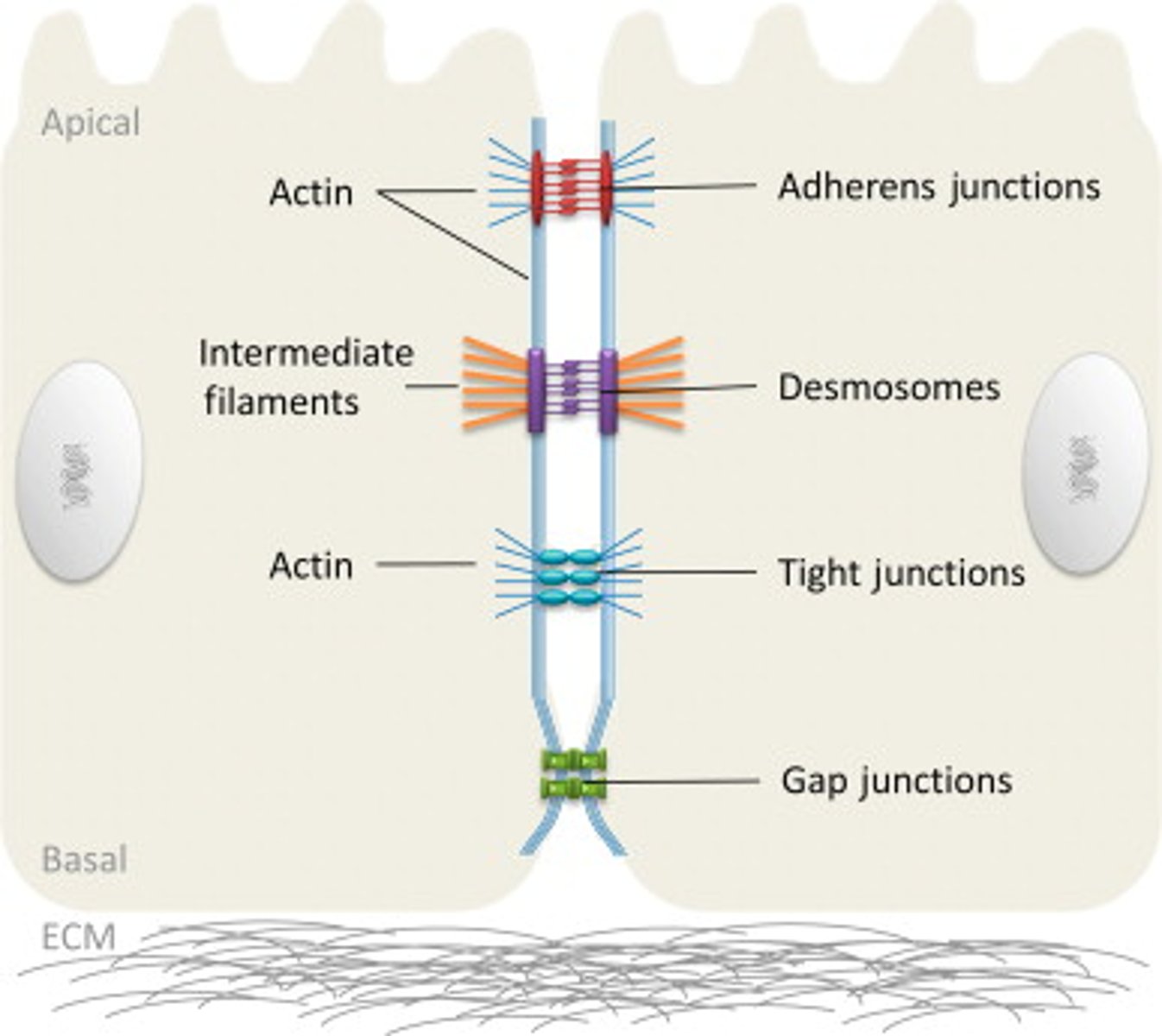
How are bile canaliculi sealed from the remaining intercellular space?
Bile canaliculi are sealed off from the remaining intercellular space by occluding junctions located on each side of each canaliculus.
What role do Kupffer cells play in the liver?
Kupffer cells are specialized macrophages located in the liver that phagocytose unwanted materials, such as bacteria and worn-out blood cells.
What does exocrine secretion by hepatocytes involve?
Exocrine secretion by hepatocytes involves producing and releasing bile, which contains bilirubin glucuronide, bile acids, cholesterol, lecithin, phospholipids, ions, IgA, and water.
1. Bilirubin glucuronide
2. Bile acids
3. Cholesterol
4. Lecithin
5. Phospholipids
6. Ions
7. Immunoglobulin A (IgA)
8. Water
What is the arrangement of hepatocytes in the liver?
Hepatocytes are arranged in interconnected plates, similar to the bricks of a wall, and are radially organized around the central vein of the liver lobule.
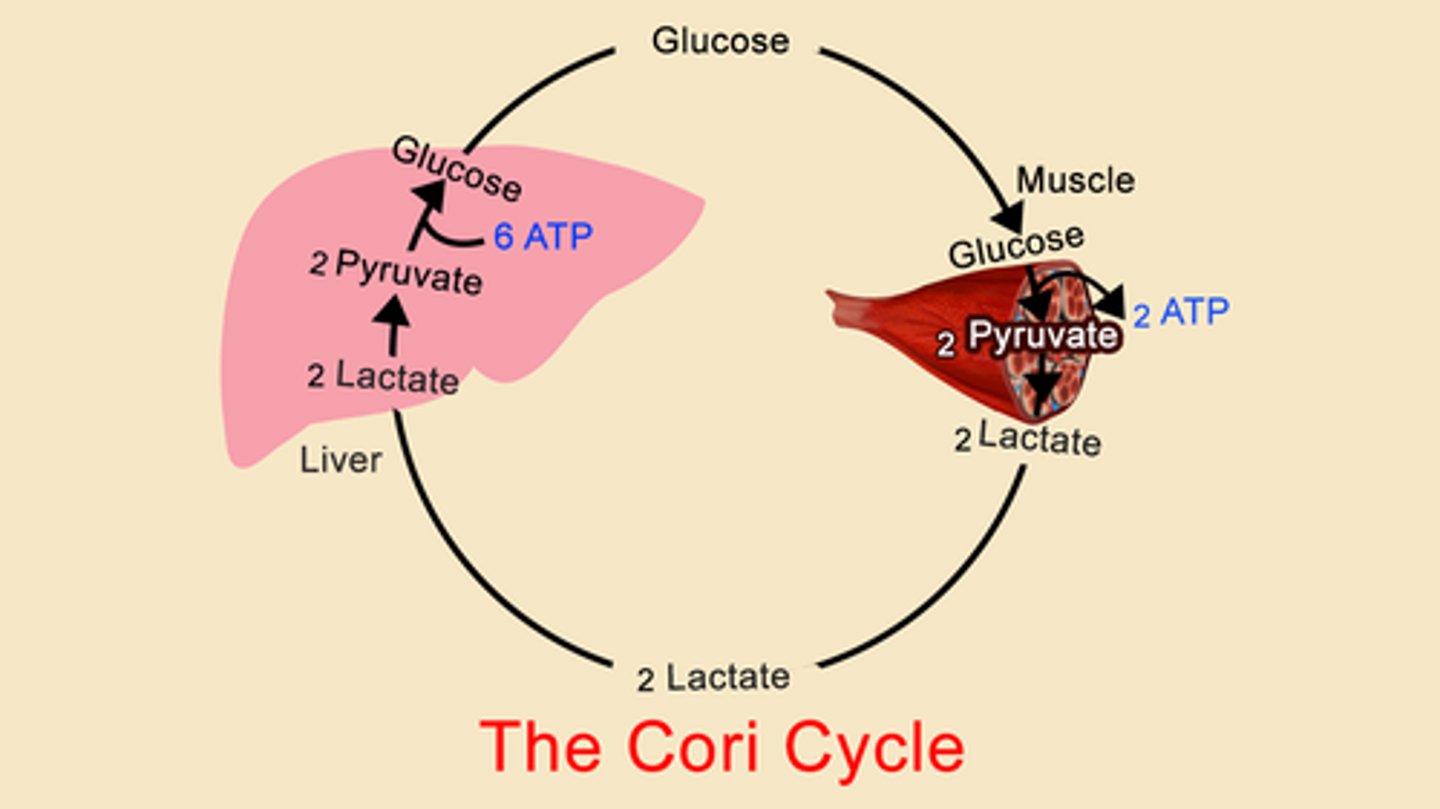
What is gluconeogenesis and where does it occur?
Gluconeogenesis is the conversion of amino acids and lipids into glucose, occurring in hepatocytes.
What does detoxification entail in hepatocytes?
Detoxification involves the inactivation of various substances such as drugs and toxins by enzymes in the microsomal mixed-function oxidase system, primarily occurring in the SER or in peroxisomes of hepatocytes.
What is the function of the bile canaliculus in hepatocytes?
collects bile secreted by hepatocytes
What is the role of hepatocytes in endocrine secretion?
produce and release plasma proteins:
1. prothrombin
2. fibrinogen
3. albumin
4. factor III
5. lipoproteins
also release nonessential amino acids.
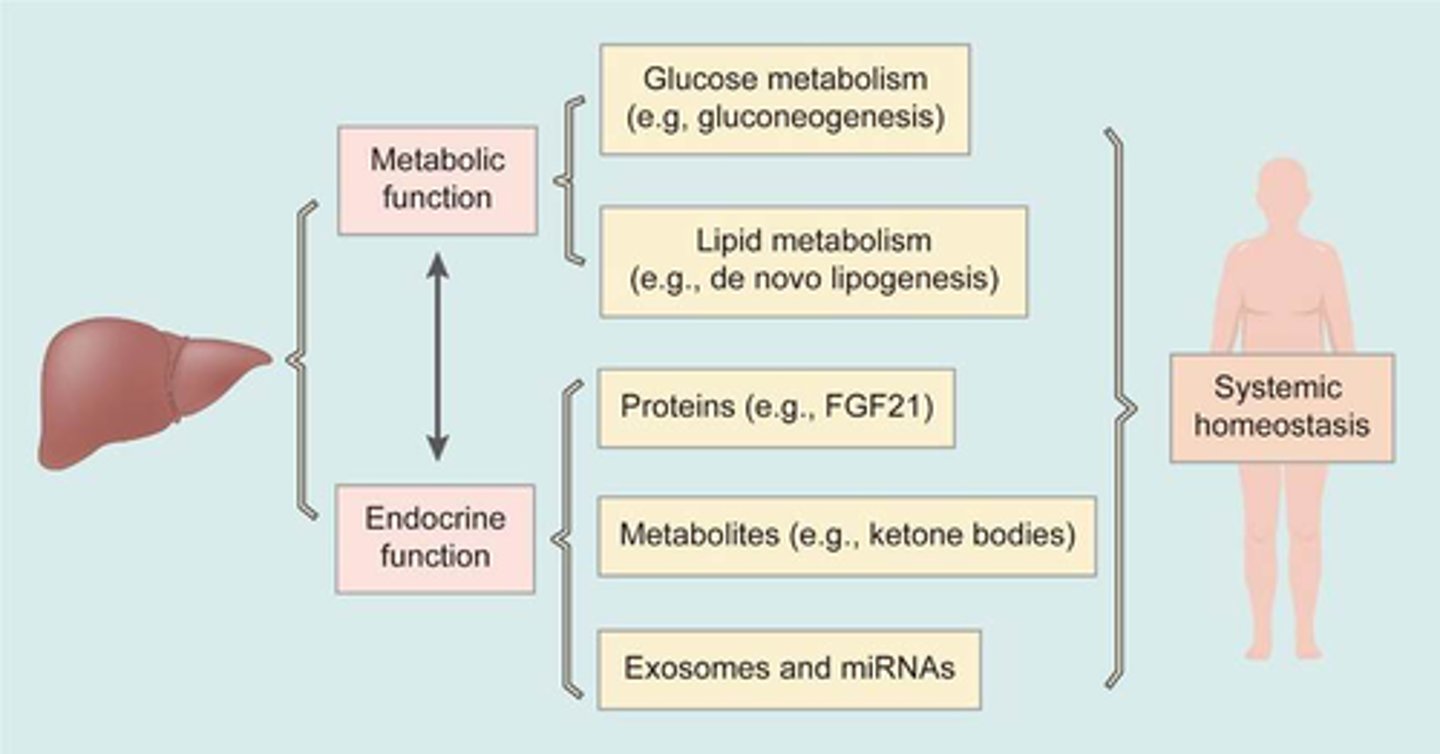
Where are metabolites stored in hepatocytes?
Metabolites are stored in the form of glycogen and triglycerides within hepatocytes.
1. glycogen
2. triglycerides
What other cellular feature is associated with hepatocytes and bile canaliculi?
In addition to microvilli, hepatocytes and bile canaliculi also have gap junctions that facilitate communication between cells.