Gastroenterology Esophagus
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
23 year old patient comes in with protrusion of the pharyngeal mucosa at the pharyngesophageal junction.
What condition do you expect?
How do you treat this condition?
Zenker Diverticulum
Treatment - Esophageal myotomy
Patient states that he experiences choking at night. You notice that there is a protrusion in the neck. The patient complains that they have had oropharyngeal dysphagia for years but didn't know what caused it. What do you suspect this condition is? How do you treat it?
Zenker Diverticulum
Treatment - Esophageal myotomy
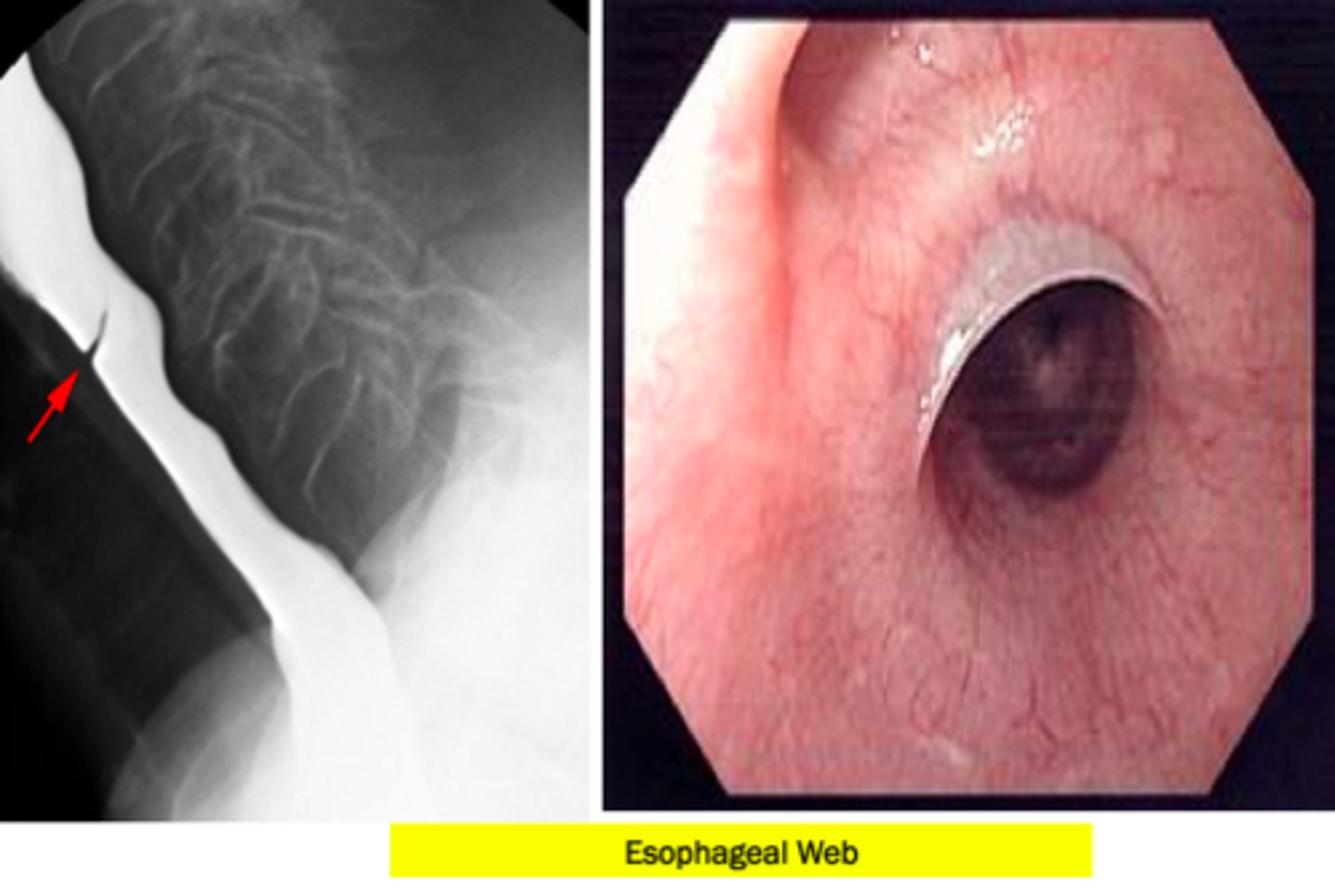
Your patient has iron deficiency anemia and complains of GERD-like symptoms and has difficulty swallowing. You perform a barium swallow and EGD. What is the treatment for this patient?
Esophageal dilation or electrosurgical incision and long term PPI therapy.
This patient has esophageal webs
What is the most common congenital esophageal anomaly?
Esophageal atresia
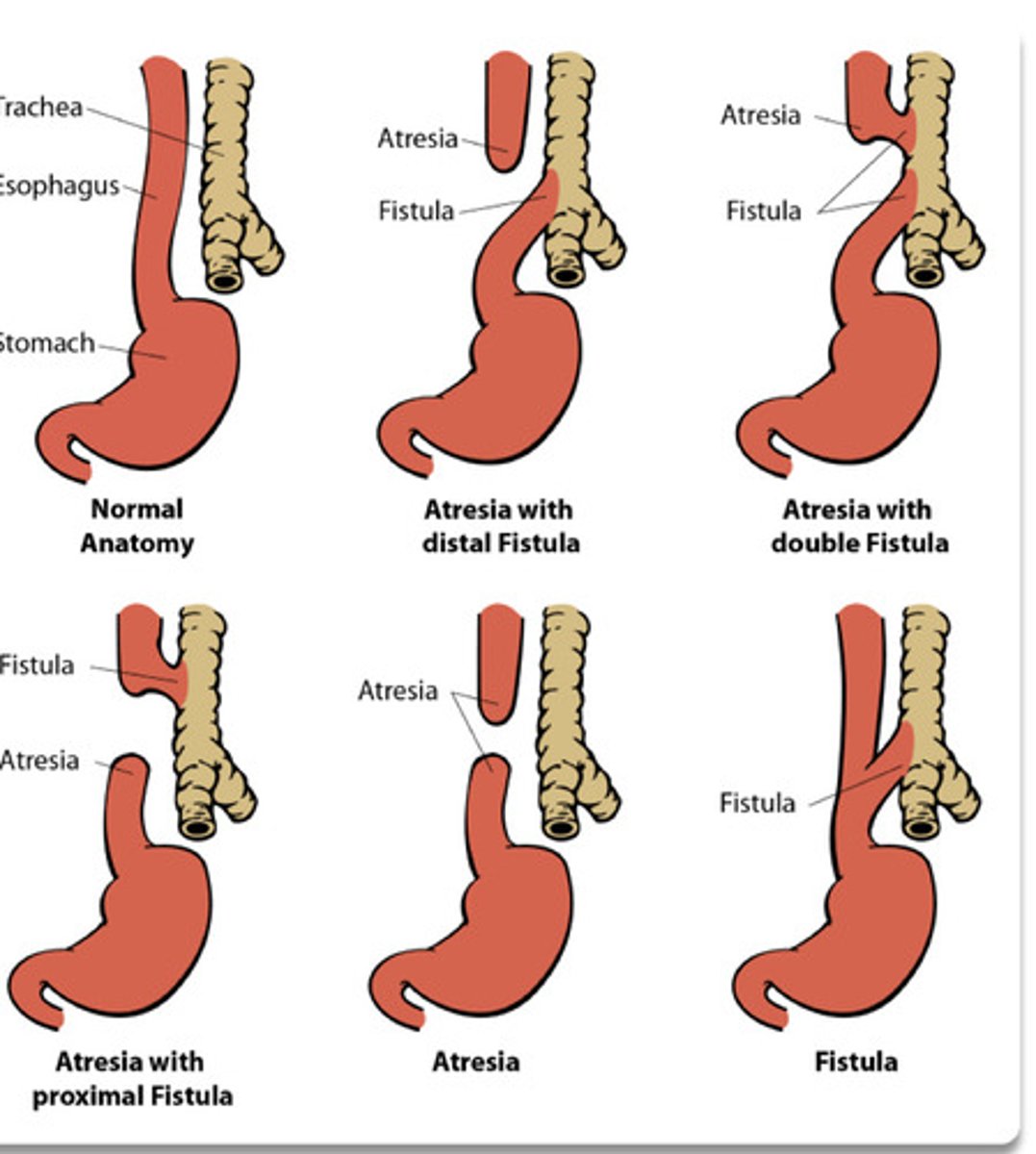
What is the most common tracheoesophageal fistula?
Distal
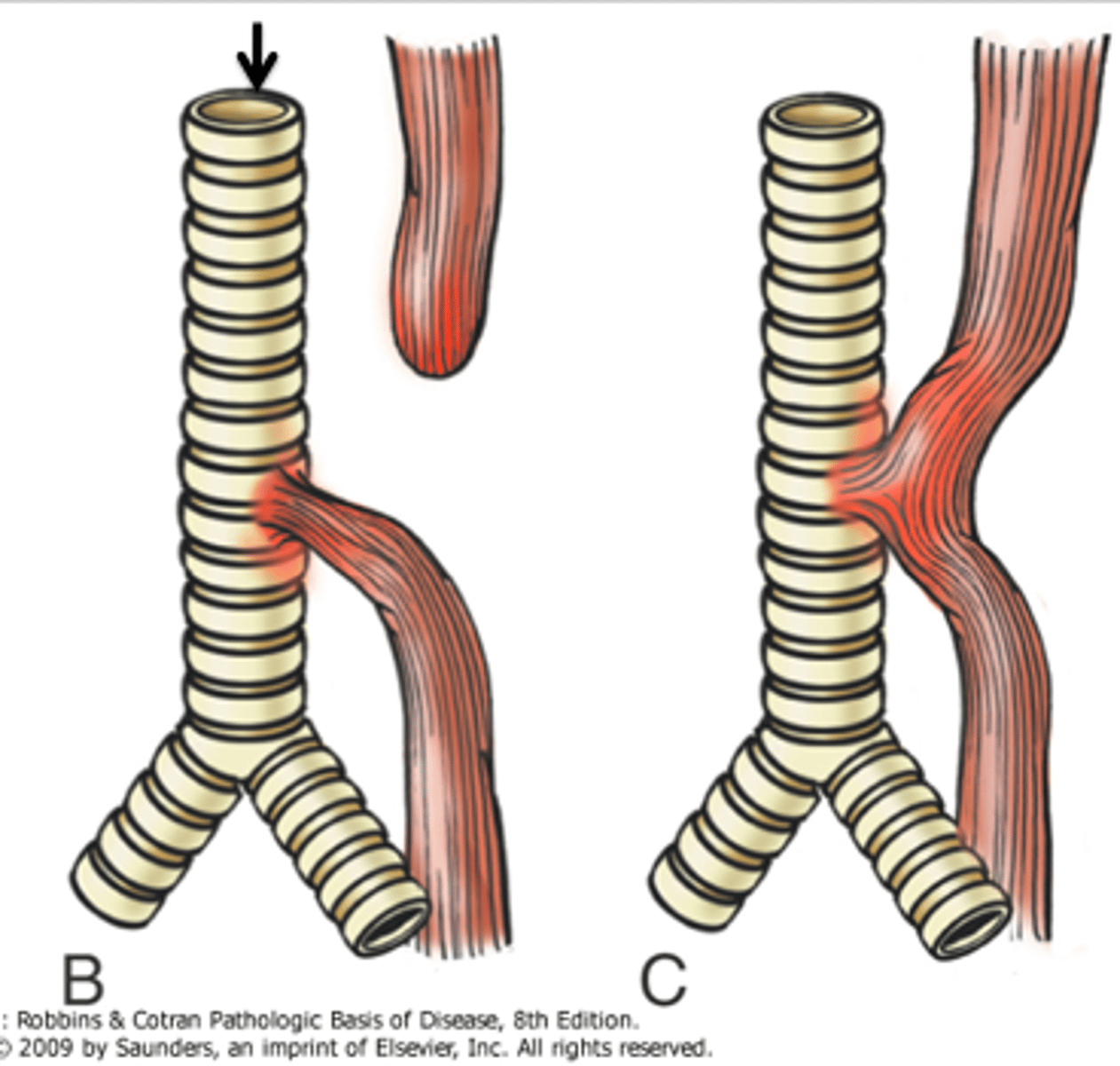
What is a complication of esophageal atresia?
Absent peristalsis
A person who has a loss of peristalsis in the distal two-thirds of the esophagus and impaired relaxation of the LES can be treated with ...
Botulinum toxin injection
Pneumatic dilation
Surgical heller cardiomyotomy
Peroral endoscopic myotomy (POEM)
This patient has achalasia
Your 50 year old patient complains of gradual onset of dysphagia for solid food and liquids. He said he gets regurgitation at night and feels discomfort after meals. His wife said he eats slower and lifts his neck when he eats. His wife has noticed a significant weight loss and is concerned for his health.
What test do you conduct first?
What test do you use to confirm your suspected diagnosis?
What is this patient's diagnosis
1.) First test is barium esophagram
2.) Manometry is gold standard for diagnostic confirmation. This is performed during endoscopy
3.) Achalasia
You conduct a barium swallow on a patient suffering from malnutrition and weight loss. Imaging displays a "bird's beak" appearance.
What do you diagnose this patient with?
Achalasia
What is the name of the esophageal wall ganglion cells that normally produce nitric oxide, leading to smooth muscle relaxation of the LES?
Auerbach's plexus
What causes diffuse esophageal spasms?
Abnormal esophageal contractions with normal LES relaxation.
25 year old male patient complains of intermittent and nonprogressive dysphagia of solid foods and liquids. He said it gets worse when he drinks hot tea or cold beer. He oftentimes feels chest pain.
What test do you order to further evaluate for dysmotility?
What do you see on this test?
What is your diagnosis?
How do you treat this patient?
1.) Barium esophagram
2.) Corkscrew esophagus or rosary bead esophagus
3.) Diffuse esophageal spasm
4.) Instruct the patient to eat slower and take smaller bites. Recommend drinking a warm liquid at the start of the meal to facilitate swallowing. You can also give your patient PPIs for 4-8 weeks
What are the 4 types of hiatal hernias?
•Type I = sliding hiatal hernia
•Types II, III and IV are all subtypes of paraesophageal hernias
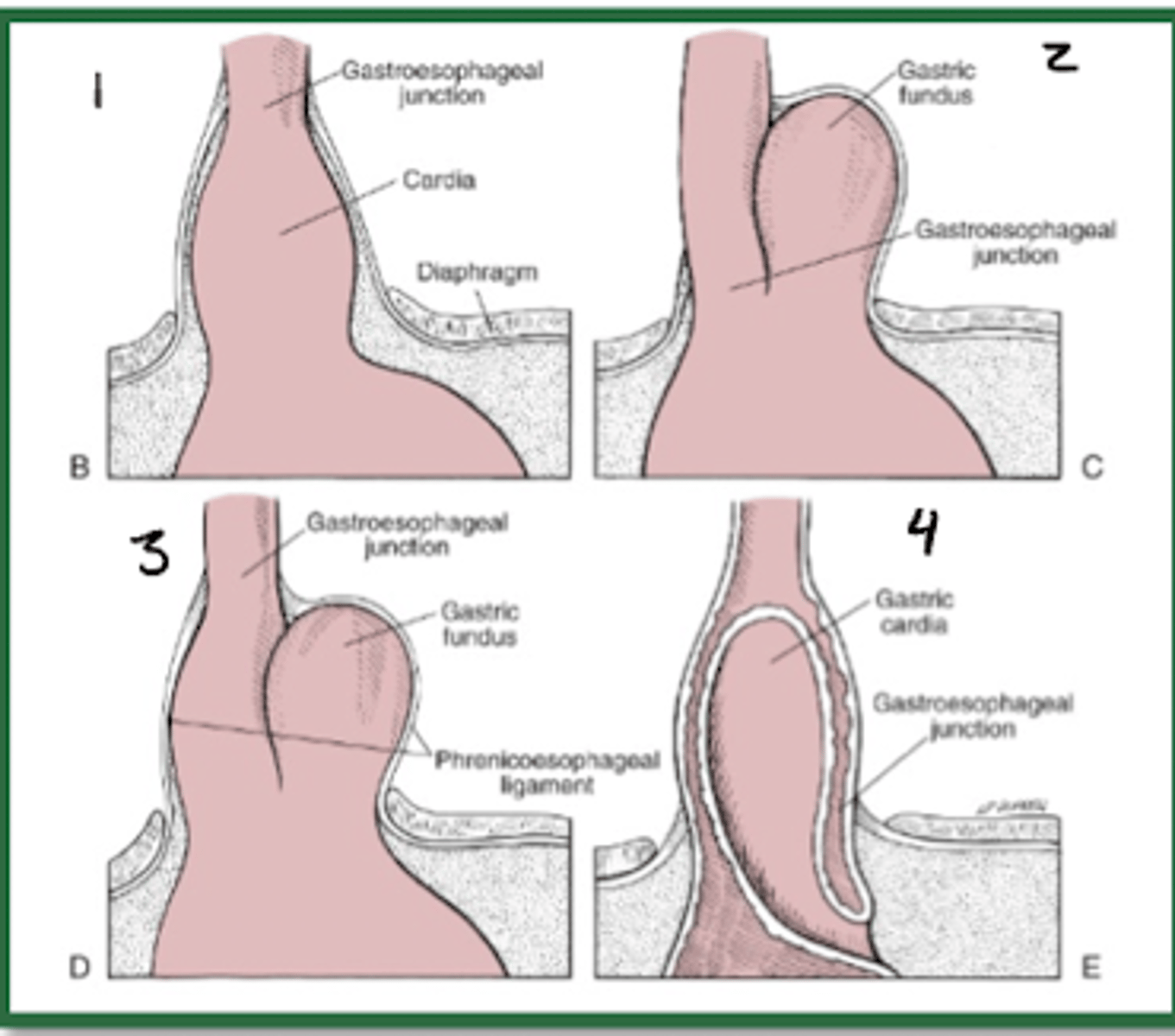
45 year old female patient presents with pain in the lower chest after eating. You notice hematemesis. She also appears to have dyspnea and pain on inspiration. You listen to her lungs and note decreased breath sounds. You listen to her abdomen and find bowel sounds on the left chest.
Note that while this patient had signs and symptoms patients are often asymptomatic.
What tests do you order to diagnose this patient?
What do you diagnose this patient with?
How do you treat this patient?
1.) Hiatal Hernia
2) CXR gastric air-fluid level behind cardiac shadow
Upper GI contrast radiography = cephalad displacement of the stomach
Endoscopy demonstrates herniation pattern depending on type
3.) asymptomatic patients don't require treatment. In this case, since the patient is symptomatic, the patient may require surgery through fundoplication techniques
Patient described having heartburn after laying down on the couch to watch TV after dinner. He complains of having heartburn daily and occasional regurgitation.
What tests do you order for this patient?
What is this patient's diagnosis?
How do you treat this patient?
1.) No Tests! Clinical diagnosis
2.) GERD
3.) Symptomatic relief, lifestyle modifications such as not laying down after eating, avoiding acidic food, lose weight. This patient may take antacids or H2 receptor antagonists as needed.
What are the red flag symptoms of GERD?
1.) Dysphagia
2.) Odynophagia
3.) Weight loss
4.) Iron deficiency anemia
5.) Bleeding
6.) vomiting
7.) GERD greater then 5 years
8.) Greater then 50
9.) Obese
10.) White race
11.) Male
12.) Tobacco use
13.) Family history
Patient is a 70 year old male suffering from heartburn for the past 5 years. His wife said he lost 25 pounds in two months. What test do you order?
Upper endoscopy!
This patient has multiple red flag symptoms. We need to visualize the type and extent of the tissue damage.
What tests can be conducted for patients who have multiple red flags, to diagnose GERD?
1.) Upper endoscopy
2.) pH/Impedance testing
3.) Esophageal manometry
What does esophageal manometry test for?
Motor function of esophagus and LES
What is the treatment for persistent/complicated GERD?
Initial - PPI daily
Long term - PPI PRN
Adam is a 45 year old male with severe GERD. Has been on PPIs for 5 years and is no longer willing to accept lifelong medial therapy.
What are two possible surgical treatments for Adam?
Fundoplication - adequate symptom relief and healing of esophagus in 85% of patients
Magnetic sphincter augmentation - symptomatic relief in 90% of patients and if hiatal hernia is less then 3 cm
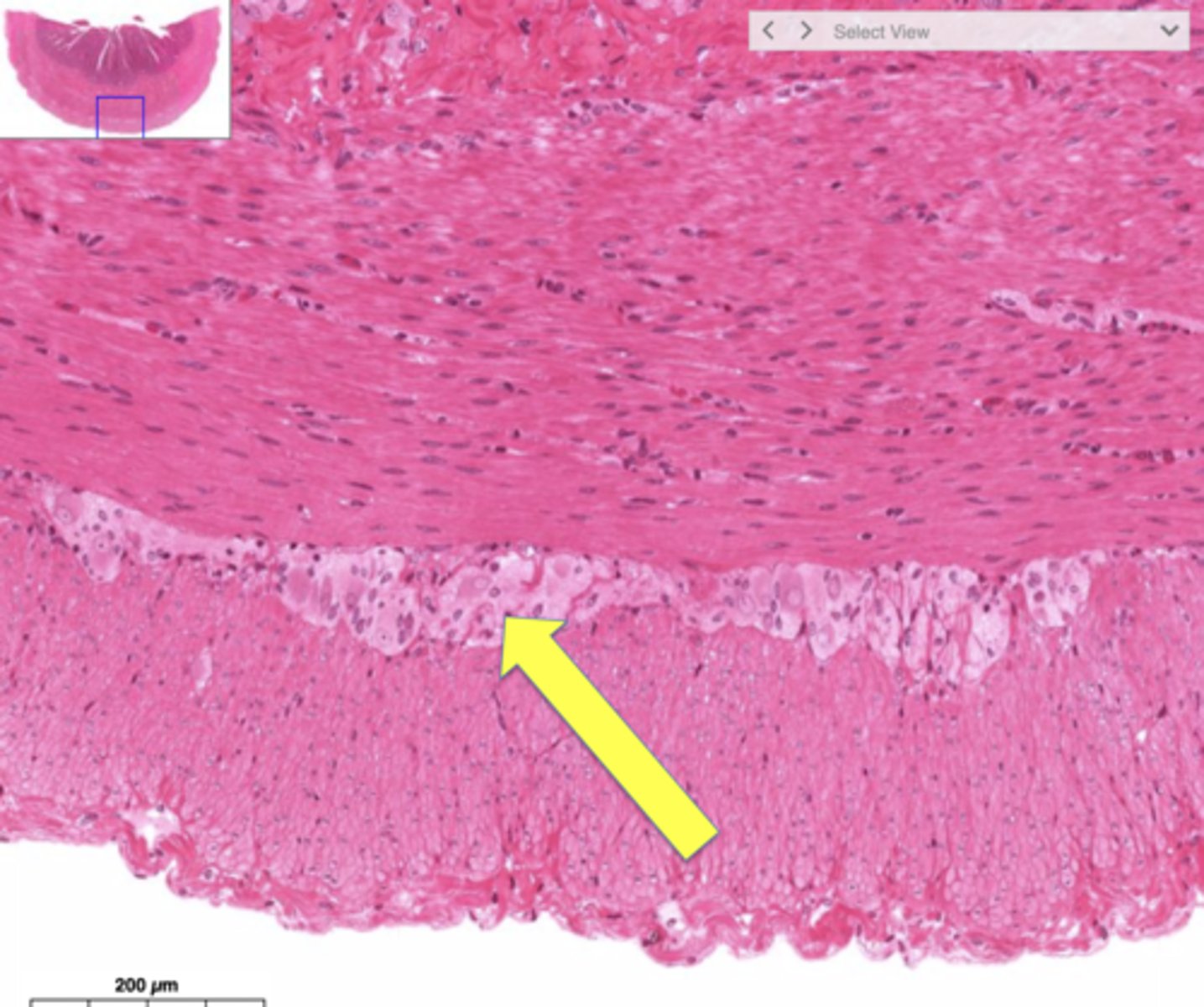
What is it called when an esophagus with normal squamous epithelium now has metaplastic columnar epithelium?
Barrett esophagus
What can result from an increased risk of dysplasia?
Esophageal adenocarcinoma
When should adults with GERD get screened for barrett's esophagus?
If there is one or more risk factors.
1.) GERD for greater then 5 yrs
2.) Greater then 50 years old
3.) Obese
4.) White race
5.) Male
6.) Tobacco use
7.) Family history
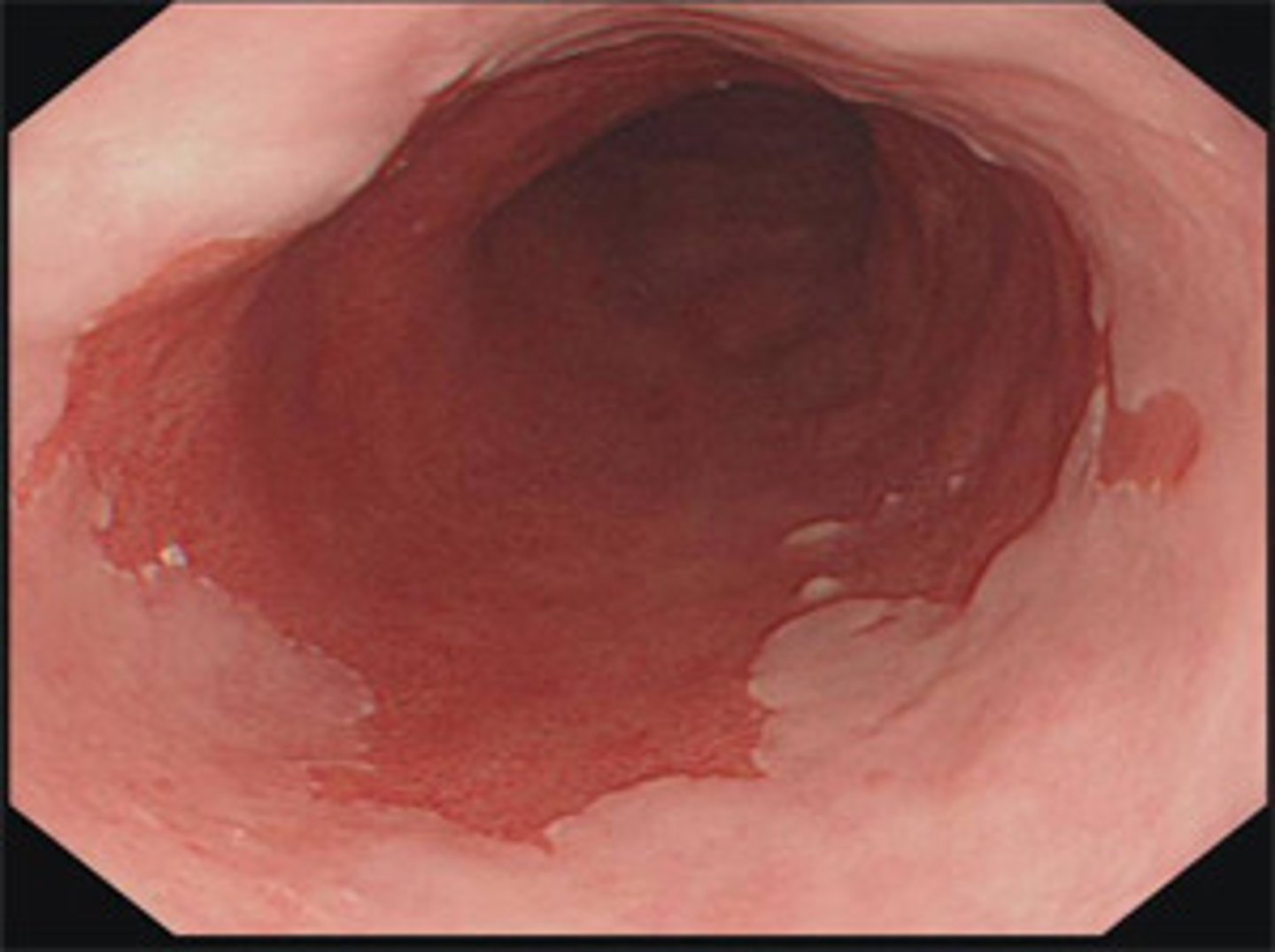
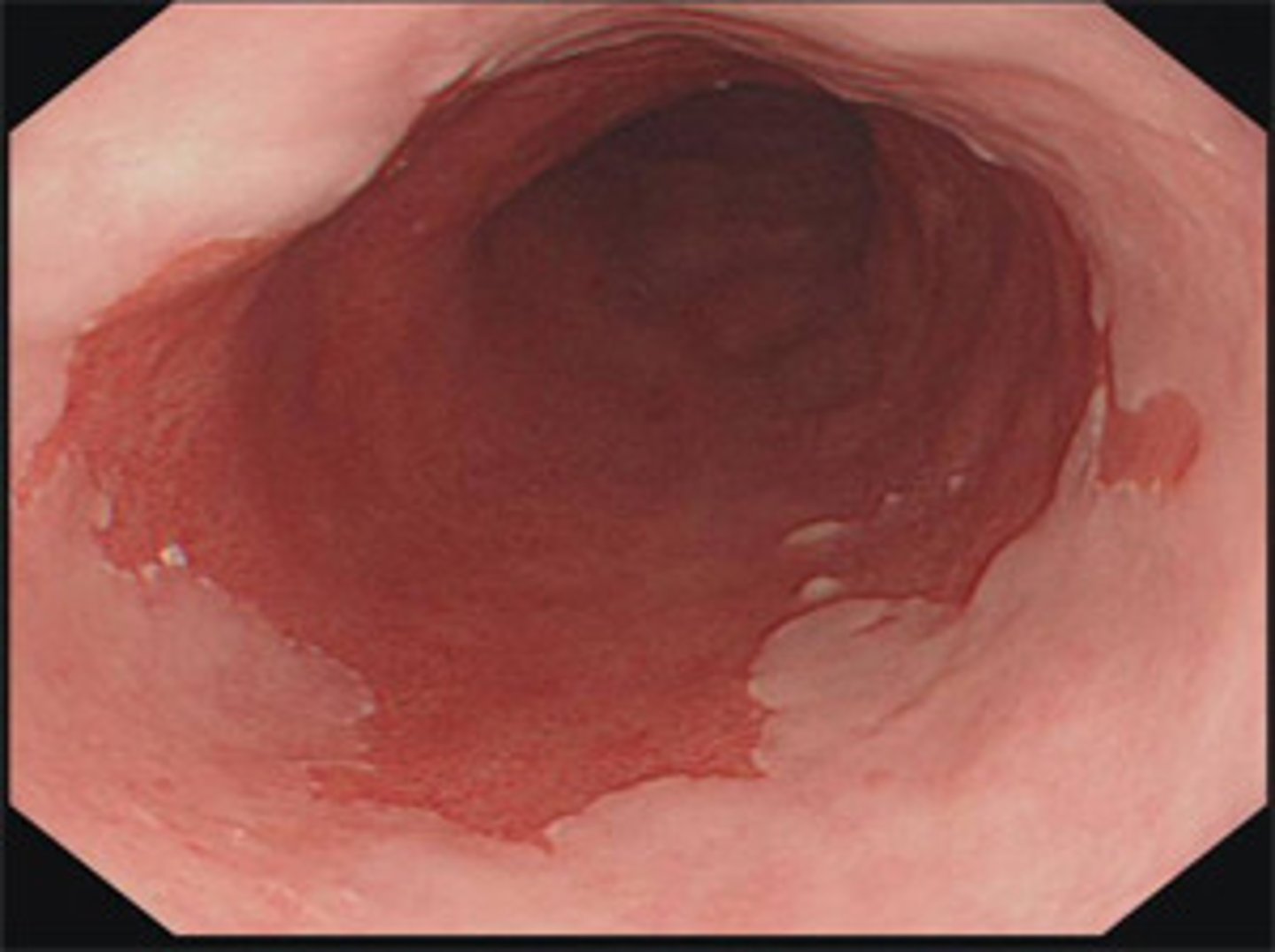
Jim is a 70 year old white man with GERD. He has had GERD for the past 6 years. You decide to screen him for Barrett's esophagus since he has two or more risk factors.
What test do you run?
What do you need to order to confirm the diagnosis?
What do you treat him with?
1.) Endoscopy
2.) Biopsy is needed for diagnosis
3.) Long-term PPIs once or twice daily to control reflux symptoms
In a patient with barrett's esophagus, how often should you perform an endoscopy if no dysplasia is present?
Every 3-5 years
Amy is a 51 year old woman with barrett's esophagus. She has high grade dysplasia and adenocarcinoma. What therapy should she undergo?
Endoscopic therapy
She needs to have an endoscopy every 3-6 months.
Richard a 65 year old man with Barrett's esophagus has low grade dysplasia. How often should he receive endoscopic therapy?
Every 6-12 months
Barrett's esophagus
What is this image of? It is salmon colored.
What percent of patients with esophagitis develop peptic strictures?
5%
April had GERD for 2 years, overtime she developed solid food dysphagia. An endoscopy with biopsy revealed that she has peptic stricture.
How do we treat this?
Balloon catheter dilation and long term PPI therapy to decrease likelihood of stricture recurrence.
Leo has been living with AIDs for 2 years. He constantly has odynophagia and dysphagia. You do an endoscopy with brushing and find yellow-white plaques on the esophagus that adhere to the mucosa.
How are you treating this?
Leo has infectious esophagitis caused by candida. You give him PO fluconazole for 14-21 days.
Angel is a 20 year old with CMV. She complains of odynophagia and dysphagia. You perform an endoscopy with biopsy and brushings to confirm your suspicion of infectious esophagitis.
What findings do you note?
How do you treat this?
1.) Shallow, superficial ulcerations
2.) IV ganciclovir --> Valganiciclovir orally, once symptoms resolve --> IV Foscarnet
Lily is a 15 year old teenager with HSV-1. Recently she came into the urgent care clinic because had pain and difficulty with swallowing. You diagnosed her with infectious esophagitis.
What test did you order to confirm this?
What clinical manifestations did you find?
What is the treatment?
1.) Endoscopy --> biopsy and brushings
2.) Multiple small, deep ulcerations
4.) PO acyclovir or Valacyclovir for 14-21 days
Your patient, a 33 year old veteran, complains of retrosternal chest pain, odynophagia, and dysphagia. You ask him when these symptoms started and he tells you every day about 3 hours after he takes his pills. He tells you that he takes ibuprofen orally daily for his back pain.
You order an endoscopy and you find that he has several shallow ulcers on his esophagus.
What is your diagnosis?
What is the treatment?
1.) Pill induced esophagitis
2.) Try non-NSAID treatment for his back pain such as cyclopbenzaprine (muscle relaxer).
Jeremy a 34 year old male has seasonal allergies. His current complaint is dysphagia of solid foods, heartburn, and chest pain.
What test do you order to confirm your suspected diagnosis?
What do you find?
What are some labs you could order?
Hint - You conduct a barium swallow and find small-caliber esophagus, tapered strictures, or concentric rings.
1.) Endoscopy with biopsy
2.) Edema, concentric rings, exudates, furrows, and strictures
3.) CBC to determine if eosinophils are elevated. Allergen specific IgE test.
Jeremy has esinophilic esophagitis
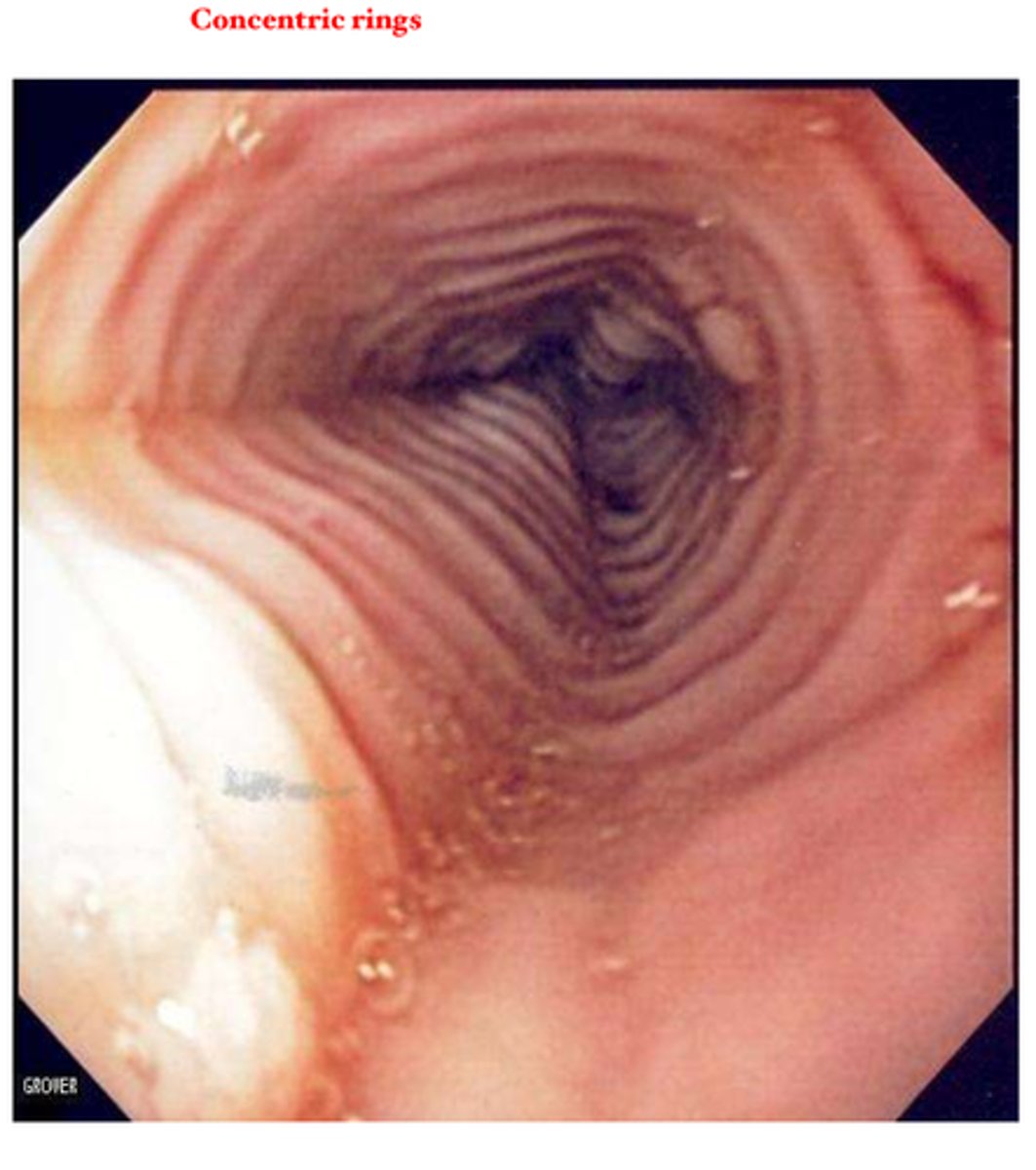
How do you treat eosinophilic esophagitis?
Proton pump inhibitor PO BID
Which radio sensitizing drugs increase your risk of radiation esophagitis?
Doxorubicin
Bleomycin
Cyclophosphamide
Cisplatin
What would you find on an endoscopy in a patient with radiation esophagitis?
Mucosa erythematous, edematous, friable.
Tissue changes and stricture may occur years after radiation exposure
How do you treat radiation esophagitis?
Supportive Care
- PPIs
- Dietary modification
Bailey, a 3 year old boy drank bleach. What type of esophagitis does he likely have? What is his treatment?
Corrosive esophagitis
- Caused due to ingestion of alkaline substances
- Supportive care, NO corticosteroids
Margot has a history of retching, for the past three days she has been vomiting blood. Turns out she has a partial thickness mucosal tear at the gastroesophageal junction.
What is the diagnosis?
How do you treat Margot's condition?
Mallory Weiss Syndrome
Resuscitate as need with fluids. Most cases resolve spontaneously
What are the risks of endoscopy, NGT placement, stricture site during endoscopic dilation?
Esophageal perforation
Lydia has odynophagia, dyspnea, sepsis, and her sternocleidomastoid muscle is tender to palpate. Where is the esophageal perforation located?
Cervical
Mark has epigastric pain with radiation to the shoulder, back pain, and inability to lie supine. Where is the location of the esophageal perforation?
Intra-abdominal
Carrie who has been forcefully vomiting all day is laying on the left lateral decubitus position and you auscultate over the precordium and hear Hamman's sign. There is a full thickness tear of the mucosal wall in Carrie's esophagus.
What do you suspect is Carrie's diagnosis?
How do you confirm this diagnosis?
What is the appropriate treatment?
1.) Thoracic Esophageal Perforation. Boerhaave's syndrome
2.) Gastrograffin and/or barium esophagography
3.) NGT for decompression, Broad spectrum antibiotics with prompt surgical drainage of fluid, debridement and repair in non-contained leaks.
What is the treatment for foreign bodies and food impaction?
Glucagon 1 mg IV for food bolus
What is a possible pharmacologic treatment for recurrent hiccups?
Chlorpromazine 25-50 mg
Which barrier level of the stomach is constantly regenerating?
Epithelial
Which layer of the stomach is involved in defense and repair and provides HCO3 and prostaglandins
Submucosal
Which layer of the stomach is the mucus bicarbonate-phospholipid barrier found in?
Pre-epithelial
What are the two main secretions that damage mucosa?
HCl and Pepsinogen
What decreases histamine?
Somatostatin
Kim is a 76 year old woman with discomfort centered in the upper abdomen. She has delayed gastric emptying and impaired accommodation of food. What test should we order for kim?
Since kim is over 60 we should order an endoscopy to confirm diagnosis of dyspepsia.
Amy is a 34 year old with discomfort centered in the abdomen with no apparent cause. Amy is in severe pain and she has been dealing with reoccurring vomiting for weeks. What test should we order to confirm diagnosis of dyspepsia.
We should order an endoscopy since Amy is experiencing alarming features.
Colin is an 18 year old with discomfort centered in the abdomen with no apparent cause. Colin drinks 1-2 beers a week. How should we treat Colin if he has a diagnosis of dyspepsia?
Patients under 60:
•Proton Pump Inhibitors (4 weeks)
•H. pylori testing
•Alcohol and caffeine reduction or cessation
•Postprandial symptoms tx with small, low-fat meals
What is the most common cause of gastropathy?
NSAIDs
Alcohol
Portal Hypertension
Medical/surgical stress
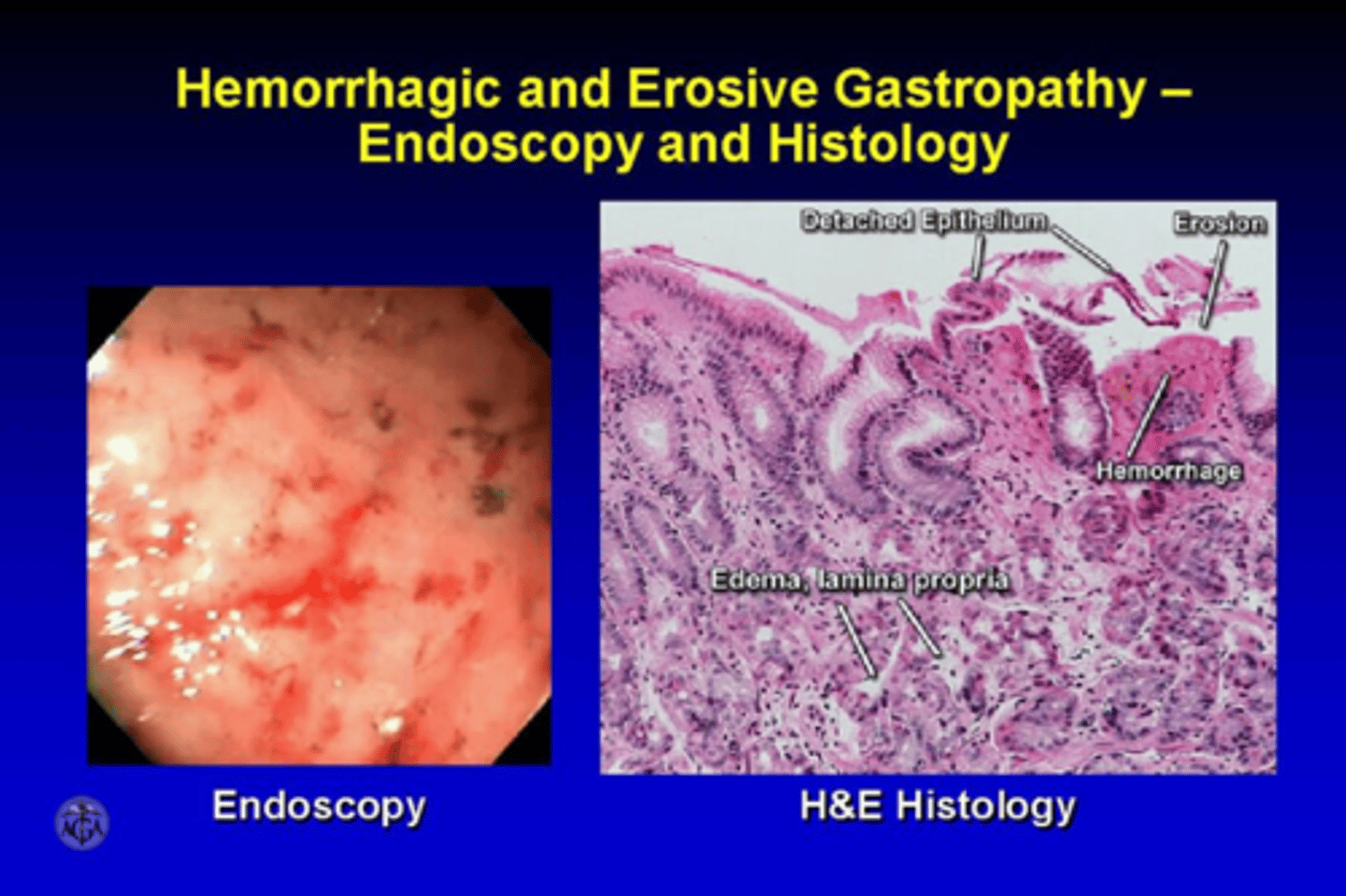
What are the signs and symptoms of Gastropathy?
Asymptomatic usually but may present with upper GI bleeding with hematemesis or melena
What is the most common clinical manifestation of erosive gastropathy?
Melena
25 year old male patient complains of intermittent and nonprogressive dysphagia of solid foods and liquids. He said it gets worse when he drinks hot tea or cold beer. He oftentimes feels chest pain.
What test do you order to further evaluate for dysmotility?
What do you diagnose the patient with?
1.) Barium esophagram
- you see corkscrew esophagus or rosary bead esophagus
2.) Patient has esophageal spasms
What is the most common clinical manifestation of erosive gastropathy?
Melena
Linda is an alcoholic and she also currently started taking ibuprofen for her neck pain. She comes into the ER with N/V and epigastric pain. Her BMI is below normal. She states she has vomited blood multiple times within the past week. She describes it to have a "coffee ground" appearance.
What tests do you order?
Endoscopy to see if Linda has errosive or hemorrhagic gastropathy.
You can also order a CBC and hemoccult.
Mary, a 56-year-old woman, has been in the intensive care unit (ICU) for the past 3 weeks due to complications from COVID-19 pneumonia. She was intubated and mechanically ventilated for 3 consecutive days during her admission. She remains critically ill but is currently hemodynamically stable.
Her most recent labs show a platelet count of 48,000/mm³, and her BMI is below normal. She has not had any episodes of overt bleeding, but nursing staff reports intermittent coffee ground material in her orogastric suction tubing.
What is Mary's diagnosis?
What treatment do you provide to Mary?
If bleeding occurs, what do you give?
1.) Stress-related gastropathy
2.) PPIs or H2RAs
3.) Continuous PPI infusion and Sucralfate suspension
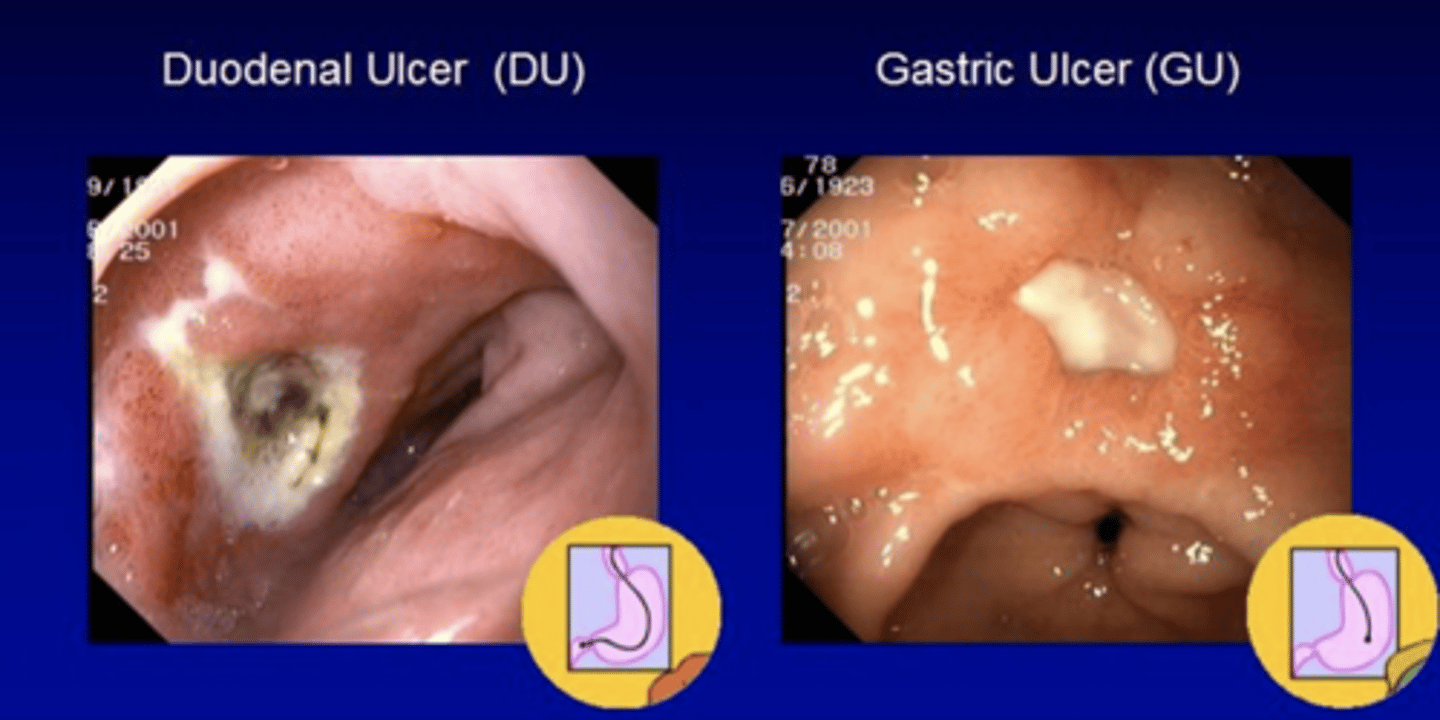
John, a 47-year-old man, presents to the clinic with a 3-month history of intermittent epigastric pain that worsens on an empty stomach and improves after eating. He describes the pain as "gnawing" and sometimes wakes up at night because of it. He has also experienced occasional nausea and bloating, but no vomiting or weight loss. He denies NSAID use or alcohol consumption. Patient is allergic to penicillin. Physical exam reveals mild tenderness in the epigastric region. You order a rapid urease test after conducting an endoscopy with biopsy. Test comes back positive for H. Pylori.
What clinical manifestations would you expect to find in the antrum?
What clinical manifestations would you expect to find in the gastric body?
How do you treat this patient?
You want to test 4 weeks after completion of therapy to see if the medication works and H. Pylori is eradicated. What test do you order?
1. Antrum: increased gastrin -> increased HCl production -> duodenal ulcer
2. Gastric Body: Can disrupt acid secretion and/or destroy acid-secreting cells --> Increased risk of gastric ulcers and gastric cancers
3.) Quadruple therapy for 14 days
PPI + Bismuth + Metronidazole + Tetracycline (Pylera)
4.) Urea Breath Test
How do you treat a patient with H. Pylori gastritis without a penicillin allergy.
PPI + Bismuth + Metronidazole + Tetracycline for 14 days (Pylera)
OR
PPI + Amoxicillin + Metronidazole + Clarithromycin
Kevin, a 52-year-old man, presents to the clinic with burning epigastric pain that has been occurring for the past 2 months. He describes it as a gnawing, dull, and hunger-like ache that often improves after eating, but returns 2 to 4 hours later. He also mentions that the pain sometimes wakes him up at night. Over the past week, he has noticed dark stools and mild fatigue. He denies NSAID use, but reports daily coffee and alcohol consumption. He has no known history of GI disease. His fecal occult blood test is positive.
1.) What tests do you order?
2.) What is the patient's diagnosis?
3.) How do you treat this patient?
1.) Endoscopy with biopsy.
2.) Peptic Ulcer --> Since symptoms improve after eating this is specifically a duodenal ulcer
3.) PPIs and H2RAs
- Mucosal defense agents such as bismuth sucralfate or misoprostol
If you have a patient with peptic ulcers but suspect perforation due to CBC showing anemia or leukocytosis. What scan would you order to further evaluate the patient?
Order an abdominal CT if perforation, penetration, or obstruction is suspected.
What is the most common cause of Upper GI bleeding?
Peptic Ulcer Disease
Severe PUD secondary to gastric acid hypersecretion due to unregulated gastrin release
Zollinger-Ellison Syndrome
Ryan, a 42-year-old man, presents to the clinic with recurrent episodes of upper abdominal pain and chronic diarrhea over the past 4 months. He has been treated twice for duodenal ulcers, but reports that the pain and diarrhea persist despite taking omeprazole daily. He denies NSAID use and has tested negative for H. pylori. He also notes unintentional weight loss and frequent diarrhea. An endoscopy reveals multiple ulcers. His secretin stimulation test is positive and fasting gastrin level is 1200pg/mL.
What is the treatment for this patient?
Ryan has Zollinger-Ellison Syndrome.
For symptom relieve he can receive PPIs. For a cure he needs surgical resection.
Hypertrophy and hyperplasia of the muscular layers of the pylorus --> leading to a functional outlet obstruction
Pyloric Stenosis
A 4-week-old male infant is brought to the pediatrician by his parents due to persistent vomiting. The vomiting began about 10 days ago and has become progressively worse. It is described as forceful and projectile, occurring shortly after feeds. The infant appears hungry after vomiting and wants to feed again. The parents have also noticed fewer wet diapers and some weight loss.
On physical exam, the infant appears mildly dehydrated. A firm, mobile "olive-shaped" mass is palpated in the right upper quadrant. No distention or tenderness is noted.
What tests should you order to further evaluate this infant?
What is the diagnosis?
What is the treatment?
1.) Ultrasound is most common test ordered.
UGI series will show string sign.
2.) Pyloric Stenosis
3.) Treatment
- Surgical
-Rehydration
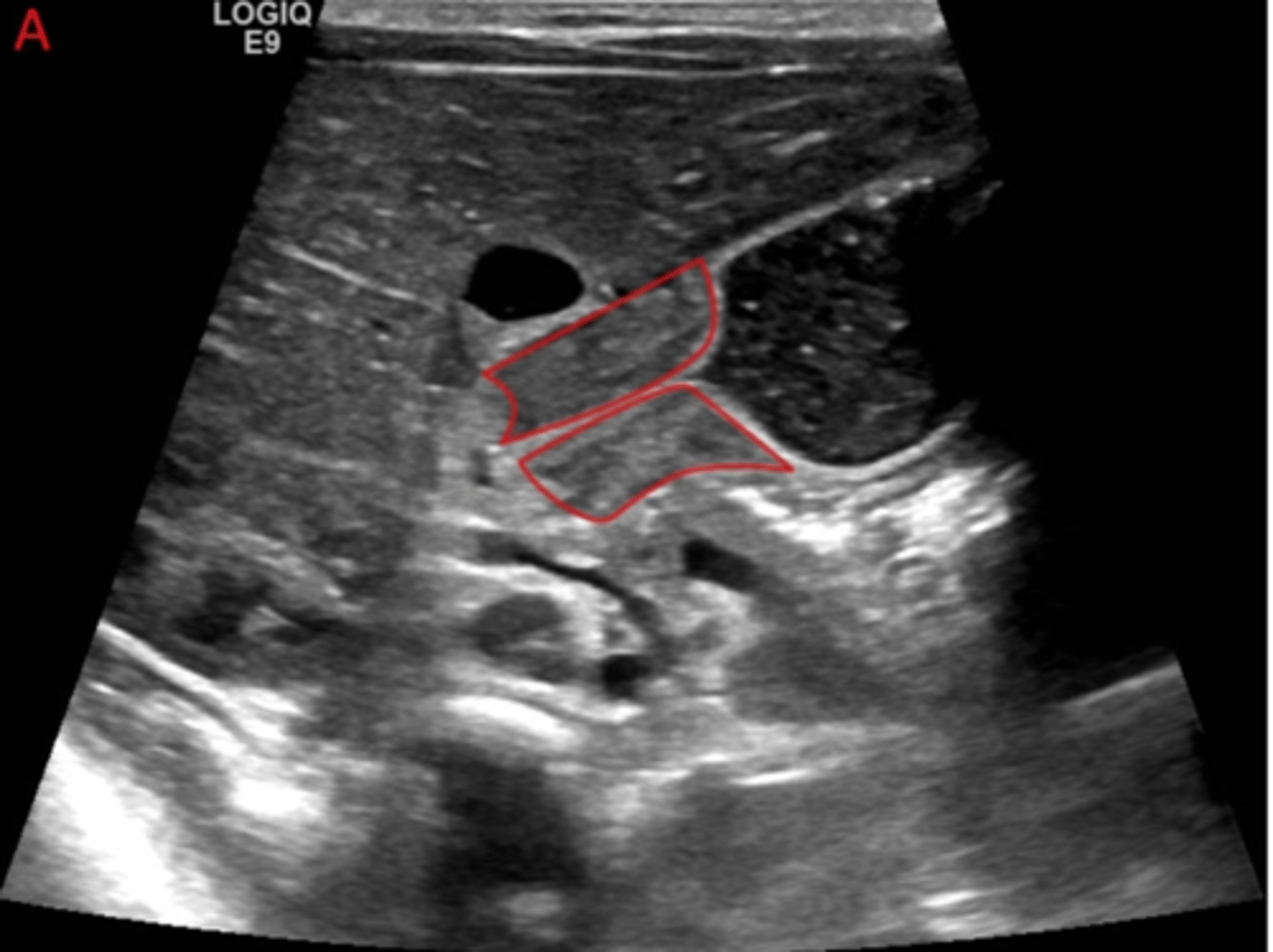
Most common cause of intestinal obstruction in infancy*
Pyloric Stenosis
Difficulty initiating swallow, pt points to upper cervical, nasopharyngeal regurgitation, aspiration, residual food sensation, coughing, choking, drooling, dysarthria
Oropharyngeal dysphagia
Difficulty swallowing a few seconds after initiation. Obstructed sensation suprasternal notch or retrosternal
Esophageal dysphagia
What is the most common obesity surgery?
Sleeve Gastrectomy
What are the benefits of Sleeve Gastrectomy compared with Roux en Y?
Lower risk of nutritional Deficiency
Which obesity surgery is best for those with type 2 DM?
by-pass/Roux en Y
Which obesity surgery is not reversible?
Sleeve Gastrectomy
Which obesity surgery is reversible?
By-pass
Which obesity surgery involves 15-20% total body weight loss at 1 year and is less invasive and reversible?
Laparoscopic adjustable gastric band