RCC 1002 Endo Midterm
1/233
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
234 Terms
Younger patients are more likely to need RCT. (T/F)
False, older
Microbial flora is a major determinant in the healing of exposed pulp. (T/F)
True, its absence means no devitalization, granulomas, or abscess (as seen in rodents)
What is the most common symptom that indicates a need for RCT?
Pain
- Sensitivity, discoloration, swelling, tenderness, etc. are other symptoms
- Can also be asymptomatic
Only a pulpal diagnosis is necessary prior to endodontic treatment. (T/F)
False, a pulpal and periapical diagnosis are both needed
______ should be removed prior to endodontic access.
Decay
RCTs can be performed without isolation, as long as all surfaces are disinfected. (T/F)
False, rubber dams are the standard of care and are required for treatment (asepsis, protects patient)
Access objectives include the following, in what order?
A. Locate all canal orifices
B. Remove all caries
C. Establish restorative margins
D. Remove all coronal pulp tissue
E. Completely unroof chamber
F. Achieve straight line access
B, C, E, D, A, F
Removal of unsupported tooth structure is unnecessary in RCT. (T/F)
False, must be removed, along with all defective restorations and caries
Mandibular anteriors are more likely to have 2 canals than maxillary anteriors. (T/F)
True, mandibular incisors 40% and canines 22% to have 2 canals
Maxillary lateral incisors have an apical _______ curvature, while the centrals have an apical ______ curvature.
Distal
Lingual
Evaluation criteria of the anterior access includes all of the following, except:
A. Pulp horns
B. Lingual shoulder removed
C. No overextension/gouging
D. Access cavity free of debris
E. Smooth flared walls
A, pulp horns should be removed
What teeth are wide B-L?
Maxillary centrals and mandibular canines
The first maxillary premolar is the only premolar where two canals are the majority. (T/F)
True
- Maxillary second have 50:50 for 1 and 2 canals
- Mandibular premolars have a 1 canal majority
Maxillary premolar have an ________ shaped access, while the mandibular have a __________ access.
1. Oval (wide B-L) or triangular (rare, 3 canals w/ base at buccal)
2. Oval (wide B-L), but more rounded
In a type II root configuration:
The root begins as two and joins as one towards the apex
Canal Root Configuration
Type 1: 1 canal and 1 foramina
Type 2: 2 canal and 1 apical foramina
Type 3: 2 canal and 2 apical foramina
Type 4: 1 canal and 2 apical formaina
What is an important anatomic consideration for maxillary premolars?
Mesial concavity at the CEJ which may allow for lateral perforation
Mandibular premolars are easy teeth for RCT. (T/F)
False, more complex than they appear
- Can have 1-3 roots that divide deep within root
In a first mandibular premolar, the access is positioned ___________.
Buccally (just short of B cusp tip)
- Have prominent buccal cusp and vestigial lingual cusp
In a second mandibular premolar, the access is positioned _______.
Centrally
What is the most often root canal treated tooth?
Mandibular 1st molars
Mandibular 1st molars typically have ____ roots with ____ canals.
2 roots, 3-4 canals
- Mesial root most often has 2 canals (MB and ML) and distal root may have 1 or 2 (D or DB and DL)
- 3 roots are possible (2.5-5.3%)
The shape of the access opening for mandibular 1st molars is:
Trapezoid (rhomboid, 4 canals) or triangular (3 canals)
C-shaped canals most commonly occur in ______ ______ molars and are most common in Asians.
Mandibular second
Mandibular second molars have _______ roots with _______ canals.
Usually 2 roots with 1-4 canals
- C-shaped (1 ribbon-shaped orifice, starting at MB and ending at distal aspect)
- 1 root is possible
What is the largest tooth and the tooth with the most complex anatomy?
Maxillary 1st molar
How many roots and canals are in maxillary 1st molars?
3 roots (P, MB, DB) and 4 canals (95%, MB, MB2, D, P)
In a maxillary 1st molar, the access is more _______ than centered.
Mesial
- Should preserve the oblique ridge
How does the technique for maxillary molars differ from mandibular?
It is easier and preferred to find the palatal canal first
Maxillary 2nd molars usually have 4 canals. (T/F)
False, 2-4 is possible but 3 is most common
- Same number of roots as 1st molar, but more narrow
In all maxillary molars, the palatal root curves buccally. (T/F)
True
What are the basic requirements for a good endodontic x-ray?
1. Tooth centered in film (minimizes distortion)
2. 3-5 mm of bone beyond apex of tooth (prevents misdiagnosis + incorrect file length)
3. No overlapping, foreshortened, or elongated images
Which of the following is the incorrect cone alignment for maxillary radiographs?
A. Right angle for canines
B. Right angle for incisors
C. Right angle for premolars
D. Right angle for routine molars
E. Mesial 20 degrees for 4 canals
C, mesial 20 degrees for premolars
The cone alignment for radiographs of the mandible is the same as that for the maxilla. (T/F)
False, only premolars are the same
- Mesial 20 degrees for canines
- Distal 20 degrees for all incisors and molars
When are intraoral radiographs recommended for endodontic treatment?
1. Evaluation of all patients
2. Immediate post-operative imaging
3. In absence of clinical signs + symptoms for evaluation of healing following nonsurgical + surgical endo treatment
When are limited FOV CBCTs recommended?
1. Diagnosis of patients with contradictory/nonspecific signs + symptoms
2. Clinical exam and 2-D radiograph are inconclusive in detecting vertical root fracture
3. Presurgical treatment planning to localize root apex + evaluate proximity to other structures
4. Surgical placement of implants
5. Dento-alveolar trauma, root fractures, luxation, and/or displacement of teeth + localized alveolar fractures
Detecting lesions with PA radiography alone was most difficult in:
1. Second molars
2. Roots in close proximity to maxillary sinus floor
When are CBCTs recommended?
1. Imaging for potential extra canals, complex morphology, and anomalies
2. Calcified canals
3. Non-healing previous endo treatment
4. Nonsurgical retreatment to assess endo treatment complications (ex. overextended obturation, localized perforations)
5. Localization, differentiation, and prognosis of external and internal resorption
Missed canals are easily identified by PAs. (T/F)
False, typically identified by CBCT
- CBCT also useful for identifying periapical lesions, root canal anatomy, bone + root fracture, resorption, perforations
The estimated WL is:
Radiographic WL (from reference point to apex) minus 0.5-1 mm (instrument short of apical constriction)
The minimal size file for taking a WL radiograph is _____.
#15
The reference point for the WL must be reproducible and the rubber stop must be perpendicular. (T/F)
First statement is true, second statement is false
- Rubber stop must be parallel
What is the initial apical file?
Largest file that would passively reach the WL
Which of the following is incorrect regarding the apex locator?
A. Less radiation
B. Takes a longer time to determine WL
C. Detects perforations
D. Accurate
E. Easy to use
F. Useful when the apex is not visible on the radiograph
B, time saver
To determine the WL using an apex ID, look at the ________ portion of the reading.
Green, this indicates the tip of file is in or very near to the apical constriction
- Red = file outside canal
The dental pulp is _______ _______ _______ that forms + supports dentin and forms the bulk of the tooth.
Loose connective tissue
The dentin and pulp have a __________ and __________ relationship.
Embryologic and functional
Pulp responds to dental injuries, only when it is directly stimulated. (T/F)
False, responds even when it is not directly stimulated
How does dentin influence the defense potential of the pulp?
Low compliance environment, limits room for pulp inflammation during healing
Predentin is unmineralized. (T/F)
True, organic matrix located between mineralized dentin and odontoblasts
Secondary dentin forms:
After root is fully developed
- Primary dentin forms during tooth development, ends when root formation is complete
- Both are physiological
_____________ dentin forms from odontoblast-like cells, following odontoblast death due to a strong stimulus.
Reparative
- Requires stem cells + new signals
In reactionary dentinogenesis, pre-existing odontoblasts from the tertiary dentin in response to a mild stimulus with upregulation of signals. (T/F)
True
The pulp cavity is the pulp tissue found in the crown of the tooth. (T/F)
False, the cavity is the entire central space in dentin found in both the root and crown (entire tooth)
- Pulp chamber is just in the crown
Coronal pulp is all of the following compared to radicular pulp, except:
A. More cellular
B. More fibrous
C. More vascular
B, it is less fibrous
Lateral (accessory) canals are smaller canals that extend from the main canal to ____________.
PDL
- Extend in vertical, horizontal, or lateral direction
The apical foramen is the apical termination of cleaning, shaping, and obturation. (T/F)
False, the apical constriction is the apical termination (WL stops here)
The distance from the major diameter (apical foramen) to the minor diameter (apical constriction) increases with age. (T/F)
True, due to cementum deposition
In a maxillary first molar, the isthmus is located:
4 mm from the apex in the MB root
- Also located in the mesial root of the mandibular molars
In what order does pulp dentinogenesis occur?
A. Development of enamel organ (bud, cap, and bell stages)
B. Synthesis of dentin matrix
C. Dental follicle
D. Odontoblast differentiation
E. Dental papilla
A, C, E, D, B
Structural organization of the pulp
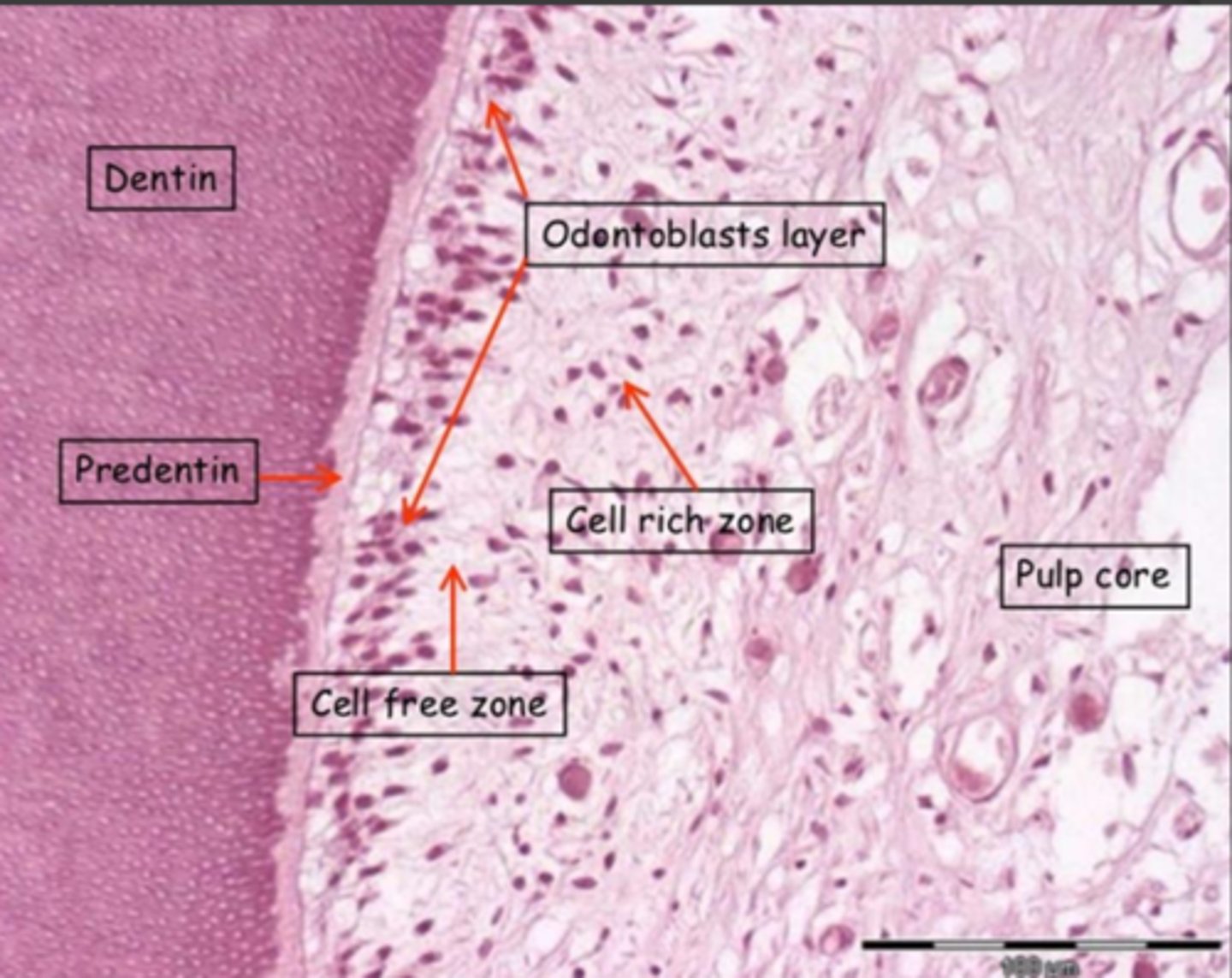
Which of the following is not a component of the odontoblast layer?
A. Processes of odontoblast cells
B. Cell bodies of odontoblasts
C. Dendritic cells
D. Nerve fibers + terminals
E. Capillaries
A, processes found in cell-free zone
What is present in the cell-free zone?
- Unmyelinated nerve fibers
- Capillaries
- Cell processes
Usually absent in radicular pulp
Cell-rich zone has a high concentration of:
Fibroblast-like cells and undifferentiated mesenchymal cells
- Also contains macrophages, lymphocytes, and dendritic cells
The cell-rich zone is more prominent in the coronal pulp. (T/F)
True
How does pulp change with age? Does it lose its vitality?
- Reduction in size, number of cells, NAV
- Increased fibrosis
Remains vital throughout life
Odontoblasts on the roof and floor of pulp chamber produce more dentin than adjacent walls. (T/F)
True, pulp chamber decreases in size towards crown (easier to perforate)
Pulpal calcifications in the coronal pulp is __________, while in the radicular pulp it is _______. This is a common occurence (at least 50% of all teeth).
1. Discrete (pulp stones)
2. Diffuse
Calcifications can hinder RCT
Pulp dentinogenesis involves three stages:
Bud (dentinogenesis), cap (amelogenesis), and bell (apposition)
The cap stage marks the onset of _______ _______.
Crown formation
Root formation starts at the ______ ______ stage.
Late bell
Stages of tooth development begins with the dental lamina and ends with a formed tooth. (T/F)
True
- Dentinal lamina -> ectoderm -> dental placode -> bud -> cap -> bell
Pulpal diagnosis is an easy process due to the tests currently available. (T/F)
False, can be asymptomatic and the tests have a poor ability to diagnose the pulp's condition.
If the cold test causes pain, pulpitis can be diagnosed. If it has no effect, it is likely necrosis or a calcified canal. (T/F)
True
- Need to establish baseline with normal tooth prior to testing
- If canal is calcified -> use EPT
The EPT is more reliable than the cold test and can be performed on dentin, enamel, and any restorations (including crowns). (T/F)
False, cold test is more reliable and can be performed on all of the areas listed. EPT cannot be performed on crowns.
Necrotic pulp reads ________ on an EPT test.
80
- Vital pulp is 1-79 (test cannot determine if vital pulp is healthy or has pulpitis)
What is the diagnostic triad?
1. Clinical exam (endo tests)
2. Radiographic evaluation
3. Reproduction of pain
________ _______ is the most convincing sign of irreversible pulpitis.
Spontaneous pain
With reversible pulpitis, a stimulus is required to evoke a _________ response of _______ duration. The response to thermal tests is _________.
1. Painful
2. Short (does not linger)
3. Hyper-responsive (slightly exaggerated)
Reversible pulpitis is inflamed tissue that requires RCT. (T/F)
False, heals with conservative therapy. Irreversible pulpitis requires RCT.
How can asymptomatic irreversible pulpitis be diagnosed without any signs/symptoms?
Clinically and radiographically, caries extend to the pulp
How can symptomatic irreversible pulpitis be diagnosed?
- Induced pain that is intense and remains after stimulus is removed (>10 seconds)
- History of spontaneous pain (constant or intermittent)
- Thermal test response is hyper-responsive + prolonged
In both reversible and irreversible pulpitis, the EPT is WNL. (T/F)
True (Necrotic is 80)
Necrosis has no response to thermal tests or EPT. (T/F)
True, also usually has history of spontaneous, prolonged, or provoked pain from irreversible pulpitis stage
- EPT = 80
What indicates a normal periradicular diagnosis?
No response to percussion + palpation, no mobility, no radiographic change
Normal apical tissues have an intact _________ and uniform _________ space.
Intact LD and uniform PDL space
How can asymptomatic apical periodontitis be diagnosed?
Radiographic evidence of periapical radiolucency, and may have a past history of pain
- Lesion w/ negative percussion
Symptomatic apical periodonitis has ______ pain that worsens with ______________.
Intense, mastication or percussion (extreme sensitivity, w/ or w/o palpation sensitivity and w/ or w/o lesion)
The thermal and EPT response for symptomatic apical periodontitis is _________.
Hyper-responsive or no response if pulp is necrotic
Symptomatic apical periodontitis presents radiographically as:
No radiographic changes (at first), thickened PDL at apex, or periapical radiolucency (not always)
The key characteristic of an acute apical abscess is:
Swelling
- Other factors include spontaneous pain, mobility, and percussion and palpation sensitivity
How does cellulitis differ from an abscess?
Diffuse, asymmetric swelling that cannot be drained
- Skin or mucosa is red, hot, and sensitive to touch
Abscess is localized collection of inflammatory material and can be drained
A chronic apical abscess presents with an associated ____________.
Sinus tract
- Gradual onset with intermittent discharge of pus
In a chronic apical abscess, swelling is present but a periapical radiolucency is not. (T/F)
False, swelling is absent and periapical radiolucency is present.
Does an apical abscess respond to a thermal test and EPT?
No, neither chronic or acute
Condensing osteitis is a _________ lesion with little or no discomfort.
Radiopaque
- Due to low grade chronic inflammation
- May or may not respond to thermal tests and EPT
Percussion and palpation responses are _____________ in chronic apical abscess and condensing osteitis.
Negative
Shaping enlarges the canal to facilitate __________.
Cleaning
- Also creates space for medication delivery + adequate geometry for obturation
Which of the following does cleaning not remove?
A. Infected dentin
B. Infected pulp
C. Necrotic tissue
D. Inflamed tissue
E. Debris
D
What is required to target microorganisms in less accessible (ex. accessory) canals and in biofilms?
Mechanical root canal preparation
- Must be done prior to irrigation
- If this bacteria remains -> apical periodontitis will not resolve