HSS1100 Immunology - Lectures 8, 9, 10
0.0(0)
Card Sorting
1/240
Earn XP
Last updated 4:09 PM on 12/13/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
241 Terms
1
New cards
What are the general characteristics of viruses?
- Grow only in living cells;
- Possess only one type of nucleic acid (either DNA or RNA);
- Multiply by separate synthesis of nucleic acid and protein that are then assembled to form virus particles;
- Viruses DO NOT DIVIDE;
- Do not have their own metabolism;
- Vary in size from 10-300 nm.
- Possess only one type of nucleic acid (either DNA or RNA);
- Multiply by separate synthesis of nucleic acid and protein that are then assembled to form virus particles;
- Viruses DO NOT DIVIDE;
- Do not have their own metabolism;
- Vary in size from 10-300 nm.
2
New cards
What are the basic structural components of virions?
1. Nucleic acid core: carries the genetic code;
2. Protein coat: protects the core and carries the antigens.
Some protein coats (capsids) contain carbohydrates or lipids.
3
New cards
What are the three methods by which viruses can be grown?
1. Cell cultures;
2. Embryonated eggs;
3. Living animals.
NOT ALL VIRUSES GROW IN ALL THREE.
2. Embryonated eggs;
3. Living animals.
NOT ALL VIRUSES GROW IN ALL THREE.
4
New cards
What are the 5 general steps of replication?
1. Adsorption;
2. Penetration and uncoating;
3. Synthesis of nucleic acid and protein;
4. Assembly-Maturation;
5. Release.
2. Penetration and uncoating;
3. Synthesis of nucleic acid and protein;
4. Assembly-Maturation;
5. Release.
5
New cards
What occurs during the adsorption step of viral replication?
Viruses adsorb to receptors on the cell surface.
6
New cards
What occurs during the penetration and uncoating step of viral replication?
The virus enters the cell, the protein coat is lost and the nucleic acid is release.
The nucleic acid becomes undetectable (eclipse).
The nucleic acid becomes undetectable (eclipse).
7
New cards
What occurs during the synthesis of nucleic acid and protein step of viral replication?
The viral nucleic acid redirects the cell metabolism to produce viral protein and nucleic acid.
8
New cards
What occurs during the assembly-maturation step of viral replication?
Viral components are assembled to form mature (infective) virus particles.
9
New cards
What occurs during the release step of viral replication?
Newly formed virus particles are released by either lysis (destruction) of the cell or budding through the cell membrane.
10
New cards
What is the golden rule for detection of viruses in a laboratory?
The golden rule is that viruses DIE OUT QUICKLY in clinical specimens. They must be examined and inoculated in the laboratory within hours after collection.
Use viral transport media and courier services, no room for the postal services. DO NOT FREEZE but keep refrigerated.
Use viral transport media and courier services, no room for the postal services. DO NOT FREEZE but keep refrigerated.
11
New cards
What are the two main approaches for viral diagnosis?
1. Detection of viruses in clinical specimens.
2. Detection of the immune reactions triggered by the virus in the patient (i.e., detection of antibodies in the patient's blood.
2. Detection of the immune reactions triggered by the virus in the patient (i.e., detection of antibodies in the patient's blood.
12
New cards
What are the steps for detection of viruses in clinical specimens?
1. Visualization by electron microscopy, high magnification required.
2. Effects after inoculation into the cell cultures require time to wait for multiplication.
3. Direct detection of viral antigens in clinical specimens themselves by immunological methods.
2. Effects after inoculation into the cell cultures require time to wait for multiplication.
3. Direct detection of viral antigens in clinical specimens themselves by immunological methods.
13
New cards
What are the effects that occur after inoculation of virus into a cell culture?
- Cytopathic effect (visible modification of infected cells).
- Hemagglutination (some cells agglutinate red blood cells).
- Immunofluorescence and other serological methods reveal the presence of viral antigenic material (even when there is no visible damage by multiplying virus).
- Hemagglutination (some cells agglutinate red blood cells).
- Immunofluorescence and other serological methods reveal the presence of viral antigenic material (even when there is no visible damage by multiplying virus).
14
New cards
What are the steps for detecting the immune reactions triggered in a patient's immune system by a virus?
1. Presence or absence of antibody against a given virus (immunity tests).
2. Rise in antibody or high antibody titer against a given virus (evidence that the virus caused a viral illness, diagnostic tests).
2. Rise in antibody or high antibody titer against a given virus (evidence that the virus caused a viral illness, diagnostic tests).
15
New cards
What are respiratory viruses?
A group of viruses which are found mainly in the respiratory tract and produce respiratory tract diseases.
They belong to different virus families.
They belong to different virus families.
16
New cards
What five virus groups are included in the respiratory virus category?
1. Influenza viruses;
2. Parainfluenza viruses;
3. Respiratory syncytial viruses;
4. Rhinoviruses;
5. Coronaviruses.
2. Parainfluenza viruses;
3. Respiratory syncytial viruses;
4. Rhinoviruses;
5. Coronaviruses.
17
New cards
What are the two main types of influenza virus?
- Influenza A (MAJOR EPIDEMICS);
- Influenza B (milder diseases);
- Influenza B (milder diseases);
18
New cards
What are the general characteristics of influenza viruses?
- Grow easily in certain cell cultures;
- Produce a haemagglutinin.
- Nucleic acid made of separate but connected segments (high frequency of recombination);
- Antigenic variability explains reappearance of new types of influenza that cause "pandemics".
- Produce a haemagglutinin.
- Nucleic acid made of separate but connected segments (high frequency of recombination);
- Antigenic variability explains reappearance of new types of influenza that cause "pandemics".
19
New cards
What are the clinical symptoms of influenza?
- Acute febrile illness with variable respiratory symptoms.
- Extreme age groups are sensitive to both disease and complications.
- Extreme age groups are sensitive to both disease and complications.
20
New cards
What are the two methods for diagnosing influenza?
1. Throat washing (naso-pharyngeal aspirate);
2. Serum samples.
2. Serum samples.
21
New cards
What is throat washing (naso-pharyngeal aspirate)? How is it used to diagnose influenza?
Taken within 3 days after onset and inoculated immediately in cell cultures. If delayed, use transport medium.
22
New cards
How are serum samples used to diagnose influenza?
Two blood samples (acute and convalescent phase) taken at 2-3 weeks interval are investigated for antibodies. Acute sample needs to be collected as soon as onset.
23
New cards
What is serum?
The liquid portion (containing antibodies) of whole blood when cells are removed. If the only test possible is detection of specific IgG or total antibody, then paired sera are required.
Sera is taken 14-21 days apart and tested at the same time. A rise in amount of antibody indicates a current infection. A significant rise or decrease or seroconversion in titer indicates a current infection.
Sera is taken 14-21 days apart and tested at the same time. A rise in amount of antibody indicates a current infection. A significant rise or decrease or seroconversion in titer indicates a current infection.
24
New cards
How is influenza infection prevented?
- Vaccines against both types are available, but use is hampered by antigenic changes.
- Antibodies against one strain protect only partially or not at all against new strains.
- Vaccines are administered to high risk groups (elderly, heart diseases, health workers).
- Some antiviral drugs (amantidine) are available but are only active against type A.
- Antibodies against one strain protect only partially or not at all against new strains.
- Vaccines are administered to high risk groups (elderly, heart diseases, health workers).
- Some antiviral drugs (amantidine) are available but are only active against type A.
25
New cards
What are the main characteristics of parainfluenza viruses?
- Frequent in infants and small children.
- Cause respiratory disease that may result in serious complications.
- Cause Laryngotracheobronchitis (croup), bronchiolitis, and bronchopneumonia.
No vaccine available.
- Cause respiratory disease that may result in serious complications.
- Cause Laryngotracheobronchitis (croup), bronchiolitis, and bronchopneumonia.
No vaccine available.
26
New cards
What are the main characteristics for respiratory syncytial virus?
- Major respiratory pathogen in children under 2 years.
- Bronchiolitis and pneumonia can occasionally be fatal.
- Can cause epidemics;
- NO VACCINE available;
- Antiviral treatment with ribavizine.
- Bronchiolitis and pneumonia can occasionally be fatal.
- Can cause epidemics;
- NO VACCINE available;
- Antiviral treatment with ribavizine.
27
New cards
What are the main characteristics of rhinoviruses?
- Main cause of the common cold;
- Over 100 different serological types with no cross immunity;
- Repeated infections are common.
- Over 100 different serological types with no cross immunity;
- Repeated infections are common.
28
New cards
What are the main characteristics of coronaviruses?
A virus causing coronavirus disease 2019 (COVID-19) discovered in 2020 in Wuhan china.
Spreads from infected person to person through:
- Close contact;
- Respiratory droplets;
- Contaminated surfaces;
- Touching objects (fomites);
- Common greetings.
Spreads from infected person to person through:
- Close contact;
- Respiratory droplets;
- Contaminated surfaces;
- Touching objects (fomites);
- Common greetings.
29
New cards
How do laboratories detect respiratory viruses?
1. Fastest approach is direct detection of viral antigens by immunofluorescence or other immunological methods (combined with inoculation in cells).
2. Clinical specimens, by order of decreasing usefulness:
- Naso-pharyngeal aspirates;
- Throat washings;
- Throat and nasal swabs.
3. Chances of detecting the virus decrease rapidly after a few days illness.
2. Clinical specimens, by order of decreasing usefulness:
- Naso-pharyngeal aspirates;
- Throat washings;
- Throat and nasal swabs.
3. Chances of detecting the virus decrease rapidly after a few days illness.
30
New cards
How are respiratory viruses serologically diagnosed?
- Less useful and usually retrospective.
- Dates of paired sera in relation to illness are important for the lab.
- Labs test for series of respiratory agents, since symptoms are rarely typical for a given virus.
- Dates of paired sera in relation to illness are important for the lab.
- Labs test for series of respiratory agents, since symptoms are rarely typical for a given virus.
31
New cards
What are some public health measures for respiratory viruses?
1. Detection of circulating strains and antigenic make-up influenza strains in the community.
2. Decide if amantadine is useful (active against influenza A only).
3. Restricting admissions/ closing of nursing homes, hospitals, etc...
2. Decide if amantadine is useful (active against influenza A only).
3. Restricting admissions/ closing of nursing homes, hospitals, etc...
32
New cards
What are some methods of managing patients with respiratory viruses?
1. Cohorting in pediatric facilities for RSV and croup.
2. Restrictive use of antivirals (amantadine for influenza A, ribavirine for RSV).
3. Special care for debilitated patients.
2. Restrictive use of antivirals (amantadine for influenza A, ribavirine for RSV).
3. Special care for debilitated patients.
33
New cards
What viruses are included in the enteric virus category?
1. Polioviruses;
2. Coxsackieviruses;
3. Echoviruses.
2. Coxsackieviruses;
3. Echoviruses.
34
New cards
What are enteroviruses?
Viruses that multiply mainly in the gastro-intestinal tract, but, as a rule, DO NOT CAUSE GASTRO-ENTERITIS.
They can reach other organs as a results of viremia (virus in blood) and cause severe damage. Usually causes damage in the central nervous system.
They can reach other organs as a results of viremia (virus in blood) and cause severe damage. Usually causes damage in the central nervous system.
35
New cards
What are the common characteristics of enteroviruses?
- Infection acquired through the respiratory tract (naso-pharynx) and/or gastro-intestinal tract.
- Infection with enteroviruses is 95% inapparent (multiples up to 5-6 weeks without symptoms.
- Infection causes minor illness in 4-5% of cases (fever, pharyngitis).
- Infection causes major illness in
- Infection with enteroviruses is 95% inapparent (multiples up to 5-6 weeks without symptoms.
- Infection causes minor illness in 4-5% of cases (fever, pharyngitis).
- Infection causes major illness in
36
New cards
What are the types of poliovirus?
There are three immunological types of polioviruses:
- Type 1;
- Type 2;
- Type 3.
Man is the only natural host for poliovirus.
- Type 1;
- Type 2;
- Type 3.
Man is the only natural host for poliovirus.
37
New cards
How are polioviruses diagnosed clinically?
1. Isolation of virus from stool specimens (in stools after 5-6 weeks), CSF, pericardial fluid, after inoculation in cell cultures.
2. Serology:
- Two specimens (acute and convalescent phase) are necessary.
- Acute specimen immediately after onset.
- Convalescent specimen 2-3 weeks later is usually collected.
2. Serology:
- Two specimens (acute and convalescent phase) are necessary.
- Acute specimen immediately after onset.
- Convalescent specimen 2-3 weeks later is usually collected.
38
New cards
What is the epidemiology of poliovirus infections?
The most important factor that favours the spread of the disease is the large number of INAPPARENT infections.
People infected with enteroviruses show no sign of disease, but spread the virus to other susceptible persons.
People infected with enteroviruses show no sign of disease, but spread the virus to other susceptible persons.
39
New cards
How is poliovirus infection prevented?
Two types of highly effective vaccines are used:
1. Killed (inactivated) polio vaccine - SALK, trivalent.
2. Live attenuated polio vaccine - SABIN, trivalent.
1. Killed (inactivated) polio vaccine - SALK, trivalent.
2. Live attenuated polio vaccine - SABIN, trivalent.
40
New cards
What are the characteristics of the Salk, killed polio vaccine?
- Does not produce local immunity (IgA) in the GI tract.
- The virus can still multiply in GI tract and spread in the community.
- Vaccine is superseded by the live attenuated vaccine.
- Killed vaccine is used in immunocompromised individuals and adults with no previous immunizations against poliomyelitis.
- The virus can still multiply in GI tract and spread in the community.
- Vaccine is superseded by the live attenuated vaccine.
- Killed vaccine is used in immunocompromised individuals and adults with no previous immunizations against poliomyelitis.
41
New cards
What are the characteristics of the Sabin, live attenuated polio vaccine?
- Easy to administer by mouth;
- Produces IgA and IgG antibodies;
- Produces GI tract resistance to infections;
- Prevents wild spread of virus in the community.
- Should not be administered to immunocompromised patients or adults who have never been vaccinated against polio before.
- Produces IgA and IgG antibodies;
- Produces GI tract resistance to infections;
- Prevents wild spread of virus in the community.
- Should not be administered to immunocompromised patients or adults who have never been vaccinated against polio before.
42
New cards
What are the two types of Coxsackieviruses?
Type A - several types;
Type B - several types.
Type B - several types.
43
New cards
What are the clinical symptoms of the Coxsackieviruses?
* Aseptic meningitis (Group A, B);
* Herpangina and hand-foot-mouth disease (group A);
* Minor respiratory illness (Group B);
* Pleurodynia, pericarditis and myocarditis (group B).
* Herpangina and hand-foot-mouth disease (group A);
* Minor respiratory illness (Group B);
* Pleurodynia, pericarditis and myocarditis (group B).
44
New cards
What is the epidemiology of Coxsackieviruses?
- Seasonal variation (summer and fall);
- Prevalent type varies every few years.
- Prevalent type varies every few years.
45
New cards
How are Coxsackieviruses diagnosed?
Most group A coxsackieviruses can be isolated only by mouse inoculation.
Other diagnostic methods include:
1. Isolation of virus from stool specimens (in stools after 5-6 weeks), CSF, pericardial fluid, after inoculation in cell cultures.
2. Serology:
- Two specimens (acute and convalescent phase) are necessary.
- Acute specimen immediately after onset.
- Convalescent specimen 2-3 weeks later is usually collected.
Other diagnostic methods include:
1. Isolation of virus from stool specimens (in stools after 5-6 weeks), CSF, pericardial fluid, after inoculation in cell cultures.
2. Serology:
- Two specimens (acute and convalescent phase) are necessary.
- Acute specimen immediately after onset.
- Convalescent specimen 2-3 weeks later is usually collected.
46
New cards
What are the preventative methods for Coxsackieviruses?
None, there are no vaccines or preventative measures for Coxsackieviruses.
47
New cards
What are echoviruses and their general characteristics?
ECHO = Enteric cytopathic human orphan viruses.
Named because, when first isolated in cell cultures, no relation to disease was evidence.
There are several types of viruses.
Named because, when first isolated in cell cultures, no relation to disease was evidence.
There are several types of viruses.
48
New cards
What are the clinical symptoms of echoviruses?
- Minor respiratory illness.
- Aseptic meningitis.
- Aseptic meningitis.
49
New cards
How are echoviruses diagnosed in the laboratory?
1. Isolation of virus from stool specimens (in stools after 5-6 weeks), CSF, pericardial fluid, after inoculation in cell cultures.
2. Serology:
- Two specimens (acute and convalescent phase) are necessary.
- Acute specimen immediately after onset.
- Convalescent specimen 2-3 weeks later is usually collected.
2. Serology:
- Two specimens (acute and convalescent phase) are necessary.
- Acute specimen immediately after onset.
- Convalescent specimen 2-3 weeks later is usually collected.
50
New cards
What are the preventative methods for echoviruses?
None, there are no vaccines or preventative measures.
51
New cards
What are four examples of viruses that causing diarrhea?
1. Rotavirus;
2. Norovirus;
3. Adenovirus;
4. Calici- and astroviruses
2. Norovirus;
3. Adenovirus;
4. Calici- and astroviruses
52
New cards
What are Rotaviruses and their general characteristics?
A virus causing epidemics of diarrhea of infants, during winter months. The virus multiplies in the small intestine, producing a loss of fluids and electrolytes.
Transient malabsorption of fats and sugars.
Transient malabsorption of fats and sugars.
53
New cards
What are the clinical symptoms of rotavirus infection?
- Acute gastroenteritis in infants and young children (6mo - 2 years).
- Diarrhea;
- Vomiting;
- Fever;
- Dehydration.
Rotaviruses are found in enormous numbers in stool, diapers, on hands, surfaces, and are HIGHLY INFECTIOUS.
- Diarrhea;
- Vomiting;
- Fever;
- Dehydration.
Rotaviruses are found in enormous numbers in stool, diapers, on hands, surfaces, and are HIGHLY INFECTIOUS.
54
New cards
How is a rotavirus infection diagnosed?
- Identification of virus present in stools by electron microscopy or immunological techniques.
- Cell cultures have no practical value;
- Examine stools within 3 days.
- Cell cultures have no practical value;
- Examine stools within 3 days.
55
New cards
What is the epidemiology of rotavirus infections?
Short incubation period: 2-3 days.
Transmission from infants with explosive diarrhea by the fecal-oral route, via aerosols and fomites.
Nosocomial outbreaks occur in nurseries, day care centers and children's hospitals.
Most older children and adults are immune.
Transmission from infants with explosive diarrhea by the fecal-oral route, via aerosols and fomites.
Nosocomial outbreaks occur in nurseries, day care centers and children's hospitals.
Most older children and adults are immune.
56
New cards
What are preventive measures for rotavirus infections?
Treat at home when possible.
In hospitals:
- Rapid viral diagnosis;
- Proper isolation procedures;
- Strict adherence to hand washing and gowning procedures to prevent nosocomial infections.
- Early discharge from hospitals;
- VACCINE.
In hospitals:
- Rapid viral diagnosis;
- Proper isolation procedures;
- Strict adherence to hand washing and gowning procedures to prevent nosocomial infections.
- Early discharge from hospitals;
- VACCINE.
57
New cards
What are the general characteristics of norovirus infections?
Noroviruses are the cause of outbreaks of gastroenteritis in older children and adults, in any season.
58
New cards
How are norovirus infections diagnosed?
Diagnosis is important in nursing homes, hospitals to differentiate it from bacteria gastroenteritis. Diagnosis is arrived at by first excluding a bacterial cause.
59
New cards
What is the epidemiology of a norovirus infection?
Similar to rotavirus, but just as contagious.
Fecal-oral route of transmission; foodborne outbreaks have been reported from water, and shell-fish.
Acquisition of immunity is slower than rotavirus, hence disease in older age groups.
Fecal-oral route of transmission; foodborne outbreaks have been reported from water, and shell-fish.
Acquisition of immunity is slower than rotavirus, hence disease in older age groups.
60
New cards
How are norovirus infections prevented?
No vaccine.
Treat at home when possible.
In hospitals:
- Rapid viral diagnosis;
- Proper isolation procedures;
- Strict adherence to hand washing and gowning procedures to prevent nosocomial infections.
- Early discharge from hospitals;
PROBLEM:
- Isolation and cohorting is more difficult and complicated by the presence of cases among staff.
Treat at home when possible.
In hospitals:
- Rapid viral diagnosis;
- Proper isolation procedures;
- Strict adherence to hand washing and gowning procedures to prevent nosocomial infections.
- Early discharge from hospitals;
PROBLEM:
- Isolation and cohorting is more difficult and complicated by the presence of cases among staff.
61
New cards
What are the general characteristics of adenoviruses?
- Some types cause gastroenteritis in young children;
- The types causing gastroenteritis cannot be cultivated in cell cultures;
- Diagnosed by ELECTRON MICROSCOPY and Immunology methods.
- The types causing gastroenteritis cannot be cultivated in cell cultures;
- Diagnosed by ELECTRON MICROSCOPY and Immunology methods.
62
New cards
What are the general characteristics of Calici- and astroviruses?
- Poorly characterized viruses causing sporadic gastroenteritis in infants and children;
- Diagnosed by ELECTRON MICROSCOPY.
- Transmission by the fecal-oral route.
- Diagnosed by ELECTRON MICROSCOPY.
- Transmission by the fecal-oral route.
63
New cards
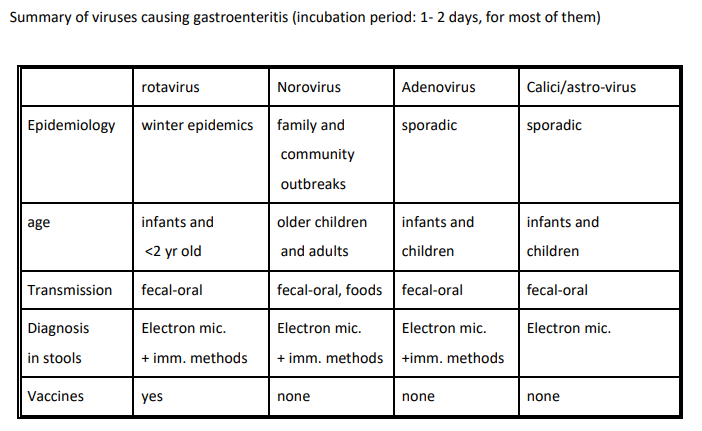
Provide a general summary of the viruses causing gastroenteritis in terms of epidemiology, age, transmission, diagnosis, and vaccines.
64
New cards
What is the practical importance of rapid laboratory diagnosis of gastroenteritis viruses?
- Rotavirus and norovirus are extremely contagious;
- Isolate and/or cohort ASAP;
- Laboratory not useful for "clearing out" patients (in contract to bacterial gastroenteritis).
- Isolate and/or cohort ASAP;
- Laboratory not useful for "clearing out" patients (in contract to bacterial gastroenteritis).
65
New cards
What are the five viruses that cause Exanthems (rashes)?
1. Measles;
2. Rubella (German Measles);
3. Varicella (chickenpox);
4. Herpes simplex virus (HSV);
5. Papilloma viruses.
2. Rubella (German Measles);
3. Varicella (chickenpox);
4. Herpes simplex virus (HSV);
5. Papilloma viruses.
66
New cards
What are the common epidemiological features of viruses causing exanthams (rashes)?
1) Humans are the SOLE reservoir;
2) They are HIGHLY contagious.
2) They are HIGHLY contagious.
67
New cards
What are the clinical symptoms of measles infection?
- Nasal and ocular catarrh (redness) preceding the rash;
- High fever;
- Koplik spots;
- Rash appears behind the ears, forehead, and around the nostrils (spread to the whole body);
- Natural disease produces lifelong immunity.
- High fever;
- Koplik spots;
- Rash appears behind the ears, forehead, and around the nostrils (spread to the whole body);
- Natural disease produces lifelong immunity.
68
New cards
What are the complications associated with measles infection?
- Secondary bacterial infections (e.g., broncho-pneumonia, otitis);
- Encephalitis;
- Sclerosing panencephalitis (SSPE);
- Exacerbation of tuberculosis and leukemias.
- Encephalitis;
- Sclerosing panencephalitis (SSPE);
- Exacerbation of tuberculosis and leukemias.
69
New cards
How is measles diagnosed?
Serological diagnosis of suspected cases and determination of immune status of contacts.
70
New cards
Why is laboratory diagnosis of measles important?
1. Allows to detect the first index case of a potential epidemic;
2. Allows to detect which individuals are immune.
2. Allows to detect which individuals are immune.
71
New cards
How are suspected measles cases serologically determined?
The demonstration of IgM antibody against measles in a single blood specimen or of a rising antibody titer against measles (IgG) in paired blood samples.
OR
Demonstration of circulating measles specific antibody (IgG) in close contacts.
OR
Demonstration of circulating measles specific antibody (IgG) in close contacts.
72
New cards
What are the two methods for which we prevent measles infections?
1) Immunoglobulin treatment administered within 5 days of contact with a measles case (suppresses or attenuates the disease).
2) Live attenuated vaccination, administered after 12 months of age.
GIVEN AS MMR (Measles, Mumps, Rubella vaccine).
2) Live attenuated vaccination, administered after 12 months of age.
GIVEN AS MMR (Measles, Mumps, Rubella vaccine).
73
New cards
What are the general characteristics of Rubella (German Measles)?
Causes mild disease, but is extremely dangerous in non-immune pregnant women because it can produce BIRTH DEFECTS in the offspring.
74
New cards
What are the clinical symptoms of rubella?
- Similar to measles but milder;
- Causes enlargement of cervical, retro-auricular (behind ears), and sub-occipital lymph nodes;
- Results in lifelong immunity.
PARTICULARLY DANGEROUS IN THE FIRST TRIMESTER IN SUSCEPTIBLE PREGNANT WOMEN.
After the third trimester, the risk is lower, but damage can still be traced up to the 6th month.
- Causes enlargement of cervical, retro-auricular (behind ears), and sub-occipital lymph nodes;
- Results in lifelong immunity.
PARTICULARLY DANGEROUS IN THE FIRST TRIMESTER IN SUSCEPTIBLE PREGNANT WOMEN.
After the third trimester, the risk is lower, but damage can still be traced up to the 6th month.
75
New cards
What are the risks to the fetus from contracting rubella at each trimester?
1st Trimester (0-4 weeks):
- 50%
2nd Trimester (5-8 weeks):
- 20%
3rd Trimester (9-12 weeks):
- 7%
After the third trimester, the risk is lower, but damage can still be traced up to the 6th month.
- 50%
2nd Trimester (5-8 weeks):
- 20%
3rd Trimester (9-12 weeks):
- 7%
After the third trimester, the risk is lower, but damage can still be traced up to the 6th month.
76
New cards
What are the principal birth defects associated with rubella?
Generalized:
- Abortion;
- Early death of newborn.
Localized:
- Cataracts (infection at 6th week);
- Deafness (infection at 9th week);
- Hear defects (infection from 5-10th week).
Others:
- Low birth weight;
- Cleft palate;
- Dental abnormalities;
- Mental deficiency.
- Abortion;
- Early death of newborn.
Localized:
- Cataracts (infection at 6th week);
- Deafness (infection at 9th week);
- Hear defects (infection from 5-10th week).
Others:
- Low birth weight;
- Cleft palate;
- Dental abnormalities;
- Mental deficiency.
77
New cards
How long do congenital rubella cases last?
Virus can persist up to 18 months in urine and therefore presents a hazard for susceptible personnel and family contacts.
78
New cards
What is the epidemiology of rubella infections?
Pre-vaccine era:
- Cases occurred in school-age children;
- Winter and spring;
- Major epidemics every 7-10 years;
- Lifelong immunity in 80% of young adults.
NOW:
- 60% of cases are in those 15 years+;
- Symptoms cannot be atypical.
- Cases occurred in school-age children;
- Winter and spring;
- Major epidemics every 7-10 years;
- Lifelong immunity in 80% of young adults.
NOW:
- 60% of cases are in those 15 years+;
- Symptoms cannot be atypical.
79
New cards
How are rubella cases diagnosed?
By serological methods:
1. Suspected cases (acquired or congenital) -- detection of rubella specific IgM antibody or rising antibody titer against rubella in paired sera.
2. Immunity status -- detecting of circulating antibody against rubella (IgG) in single serum).
Several methods have now replaced the old hemagglutination inhibition test (HAI).
1. Suspected cases (acquired or congenital) -- detection of rubella specific IgM antibody or rising antibody titer against rubella in paired sera.
2. Immunity status -- detecting of circulating antibody against rubella (IgG) in single serum).
Several methods have now replaced the old hemagglutination inhibition test (HAI).
80
New cards
Why is it important for laboratory diagnosis of rubella?
Atypical cases may spread to susceptible pregnant women and trigger an epidemic.
- Confirmation of cases during early pregnancy allows informed decisions concerning abortion.
- Confirmation of a case in a newborn can prevent spread to non-immune nurses who are pregnant.
- Determination of immune status of contacts is important.
- Confirmation of cases during early pregnancy allows informed decisions concerning abortion.
- Confirmation of a case in a newborn can prevent spread to non-immune nurses who are pregnant.
- Determination of immune status of contacts is important.
81
New cards
How is rubella infection prevented?
1. Check the immune status of women in child-bearing age (presence of IgG antibody to indicate immunity).
2. Diagnosis of congenital rubella syndrome in hospitals (Risk to non-immune staff).
3. Rubella serology screening in women and men starting work in hospitals, clinics, etc...
4. Vaccination of the non-immune with LIVE ATTENUATED vaccines.
5. Strict isolation of congenital rubella cases in hospital.
2. Diagnosis of congenital rubella syndrome in hospitals (Risk to non-immune staff).
3. Rubella serology screening in women and men starting work in hospitals, clinics, etc...
4. Vaccination of the non-immune with LIVE ATTENUATED vaccines.
5. Strict isolation of congenital rubella cases in hospital.
82
New cards
What are the vaccination policies of rubella?
Vaccinate with live attenuated vaccine:
1. Vaccination of babies (MMR) after 12 months.
2. Vaccination of pre-pubertal girls, if not immune.
3. Vaccination in the post-partum, if not immune.
4. Vaccination of hospital personnel, women and men, if not immune.
Immunity induced by the live vaccines appears to be long-lasting.
1. Vaccination of babies (MMR) after 12 months.
2. Vaccination of pre-pubertal girls, if not immune.
3. Vaccination in the post-partum, if not immune.
4. Vaccination of hospital personnel, women and men, if not immune.
Immunity induced by the live vaccines appears to be long-lasting.
83
New cards
What is Varicella (chickenpox) caused by?
It is caused by the varicella/zoster virus (VZV), a member of the herpes group.
84
New cards
What are the clinical symptoms of varicella?
- Mild childhood febrile illness with characteristic vesicular rash;
- Successive crops of fresh vesicles appear within 3-4 days after the onset of the rash;
- Papule, vesicles, and crusts are present.
- Successive crops of fresh vesicles appear within 3-4 days after the onset of the rash;
- Papule, vesicles, and crusts are present.
85
New cards
What are complications associated with varicella infection?
* In non-immune adults, pneumonia can be fatal;
* Chickenpox can be transmitted to the newborn if infection occurs close to the end of pregnancy.
* Shingles (Herpes Zoster)
* Chickenpox can be transmitted to the newborn if infection occurs close to the end of pregnancy.
* Shingles (Herpes Zoster)
86
New cards
What is Shingles (Herpes Zoster)?
A limited rash, along the traject of one nerve (often intercostal) accompanied by pain. The disease is mainly found in adults and represents a late recurrence of latent varicella infection in the partially immune.
Cases of zoster may be at the origin of outbreaks of varicella.
Cases of zoster may be at the origin of outbreaks of varicella.
87
New cards
How is varicella infection diagnosed?
Identification of viral particles in vesicles or pustules by electron microscopy or immunological methods, followed by cell cultures.
88
New cards
How is varicella infection prevented?
- Vaccination;
- Detection of susceptible individuals in hospital personnel by serology;
- Passive immunization with zoster immuno-globulins (ZIG);
- Treatment with antivirals.
- Detection of susceptible individuals in hospital personnel by serology;
- Passive immunization with zoster immuno-globulins (ZIG);
- Treatment with antivirals.
89
New cards
What is Herpes Simplex virus (HSV)?
A widely dissemination virus and infections that occur in early childhood, most often inapparent. After initial infection, the virus may persist as a latent infection with reapparance of lesions (clusters of vesicles) "cold sores" triggered by factors like:
- Fever;
- Exposure to the sun;
- Change in temperatures.
The spread of infection is difficult to control because of the high percent of inapparent infection and because it can be transmitted sexually.
- Fever;
- Exposure to the sun;
- Change in temperatures.
The spread of infection is difficult to control because of the high percent of inapparent infection and because it can be transmitted sexually.
90
New cards
What are the two types of herpes simplex virus?
- Type 1 (HSV1);
- Type 2 (HSV2).
- Type 2 (HSV2).
91
New cards
What is type 1 herpes simplex virus?
Primarily associated with oral and ocular lesions and transmitted through oral and respiratory secretions: "cold sores".
Type 1 can also be transmitted sexually, but some protection is afforded by previous Type 1 infections.
Type 1 can also be transmitted sexually, but some protection is afforded by previous Type 1 infections.
92
New cards
What is type 2 herpes simplex virus?
Herpes genitalis -- Associated with genital tract and transmitted mainly venereally. Infection in females can be transmitted to newborns.
Type 1 can also be transmitted sexually, but some protection is afforded by previous Type 1 infections.
Type 1 can also be transmitted sexually, but some protection is afforded by previous Type 1 infections.
93
New cards
What is recurrent herpes? Which type of HSV does it occur with?
Occurs with both types of herpes simplex virus, and usually in the same region(s) as the primary lesion.
94
New cards
How is herpes simplex virus diagnosed?
1. Identification of virus particles by EM or immunological methods in clinical specimens.
2. Virus grows easily in cell cultures (usually within 24-48 hours);
3. Serology of very little use.
2. Virus grows easily in cell cultures (usually within 24-48 hours);
3. Serology of very little use.
95
New cards
What are the clinical symptoms apart from cold sores associated with herpes simplex virus?
- Genital infections;
- Herpetic encephalitis;
- Neonatal herpes;
- Herpetic whitlow;
- Corneal and conjunctival infection;
- Relationship to carcinoma of the cervix (unproven).
- Herpetic encephalitis;
- Neonatal herpes;
- Herpetic whitlow;
- Corneal and conjunctival infection;
- Relationship to carcinoma of the cervix (unproven).
96
New cards
What are genital infections associated with HSV?
Primary infections that cause recurrences in both sexes.
97
New cards
What is herpetic encephalitis?
Encephalitis in young adults as a result of a latent herpetic infection since the primary infection in childhood.
Rare but very serious, affects the nervous system.
Rare but very serious, affects the nervous system.
98
New cards
What is neonatal herpes?
Usually acquired during the passage in the birth canal from an asymptomatic mother affected with either type 1 or type 2 herpes.
Difficult to prevent. Severity varies from a few vesicles to a fulminant generalized infection.
- Death or severe sequelae.
Difficult to prevent. Severity varies from a few vesicles to a fulminant generalized infection.
- Death or severe sequelae.
99
New cards
What is herpetic whitlow?
Herpetic infection affecting the fingers, occupation hazard of health care personnel.
Leads to nosocomial infections of newborns in nurseries.
Leads to nosocomial infections of newborns in nurseries.
100
New cards
What are corneal and conjunctival infections caused by HSV?
Infections that lead to ulceration of the cornea and blindness.