acute care medical/surgical management & discharge planning
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
in acute care, what is a PTs role regarding pain?
- to teach functional mobility with pain (not to alleviate)
*document pain every session and response to functional activities/interventions
oral agents - given for how much pain, how often, & how long they take to work
- mild --> severe pain
- intermittent or scheduled
- slowest to work (~20 mins)
IV agents - given for how much pain, how often, & how long they take to work
- moderate --> severe pain
- intermittent or break through doses
- work rapidly
patient controlled analgesia (via IV) & patient controlled epidural analgesia - given for how much pain & how often
- moderate --> severe pain
- can constant does or dependent on pt pushing a button
common side effects of strong analgesics
- dizziness/lightheadedness
- nausea
- drowsiness/sleepiness
- orthostatic hypotension
patient controlled epidural analgesia (PCEA) is associated with an increased risk for
orthostatic hypotension
true or false: PCA and PCEA can be disconnected for mobility
false
true or false: PTs cannot press the PCA/PCEA button for the patient
true
how does pain affect breathing after surgery?
- limited diaphragm descent
- limited bucket handle movement
- reliance on upper chest breathing
- cough suppression
- shallow breathing because of incision
what is the result of a breathing changes due to pain after surgery?
- retained secretions (and increased risk of atelectasis and infection)
- limited acitivty tolerance
the primary intervention of respiratory complications is
mobility
indications for airway clearance techniques
- impaired mucociliary transport
- excessive pulmonary secretions
- an ineffective or absent cough
*impaired airway clearance
what are simple forms of airway clearance?
- deep breathing
- coughing techniques
- mobility
safety considerations for airway clearance techniques
- should be performed at least 30 mins prior to or after meal/tube feeding
- optimize pain control prior to
- consider use of inhaled bronchodilators prior to intervention
- monitor vital signs throughout
- monitor patient tolerance and response to treatment
if a pt has shallow breathing, guarding, fear of pain with coughing (rib fx, surgery, chest tube) - what are PT priorities? what techniques should you use?
- PT priorities: improve ventilation, prevent atelectasis, making coughing tolerable
- techniques: incentive spirometer, splinted cough, diaphragmatic breathing, positioning/mobility
*pain control first, slow and controlled
how to use incentive spirometer?
long slow breath to get down to alveoli at bottom of lungs (usually 10x/hr)

what is a splinted cough?
pillow is used to apply gentle pressure to the painful area (surgical incision, rib fx)

what is diaphragmatic breathing?
facilitates outward motion of the abdominal wall while reducing upper rib cage motion during inspiration
*needs to be taught in multiple positions
if a pt can cough but it's ineffective, is fatigued, has poor technique, secretions not clearing - what are PT priorities? what techniques should you use?
- PT priorities: improve cough mechanics, reduce fatigue, mobilize secretions
- techniques: teach cough technique, huff cough/FET, ACBT
what are the stages of an effective cough?
1. large volume inhalation (trunk extension)
2. closure of glottis
3. contraction of abdominals (trunk flexion)
4. forceful expulsion of air
why is it important to do an inspiratory hold while doing stages of an effective cough/optimizing a cough?
because it builds pressure
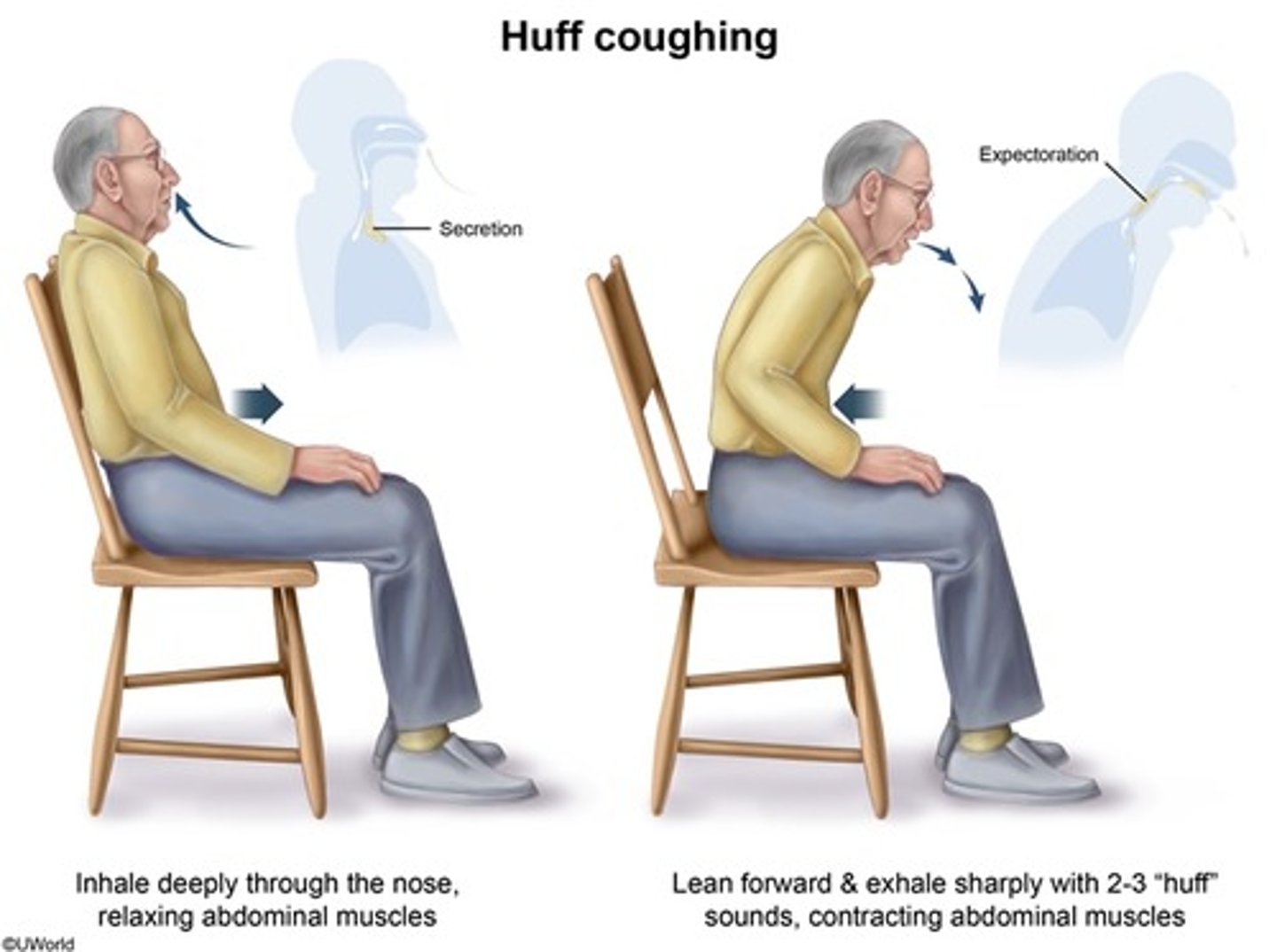
what are the benefits of a Huff Cough (forced expiratory technique/FET)
- less painful
- less fatiguing
- helps stabilize collapsible bronchiole walls
- air gets behind mucus
what is the active cycle of breathing (ACBT)
1. breathing control 5-10 seconds (relaxed)
2. 3-4 thoracic expansion exercises (deep breathing)
3. breathing control 5-10 seconds (relaxed)
4. 3-4 thoracic expansion exercises (deep breathing)
5. breathing control 5-10 seconds (relaxed)
6. 2 huff coughs
*repeat
if a pt has dyspnea (high RR, anxiety, poor breathing pattern, hypoxemia) - what are PT priorities? what techniques should you use?
- PT priorities: reduced WOB, improve efficiency, support activity tolerance
- techniques: pursed-lip breathing, diaphragmatic breathing, breathing control
SOB vs dyspnea
- SOB is an observation
- dyspnea is percieved difficulty of breathing (ask the pt)
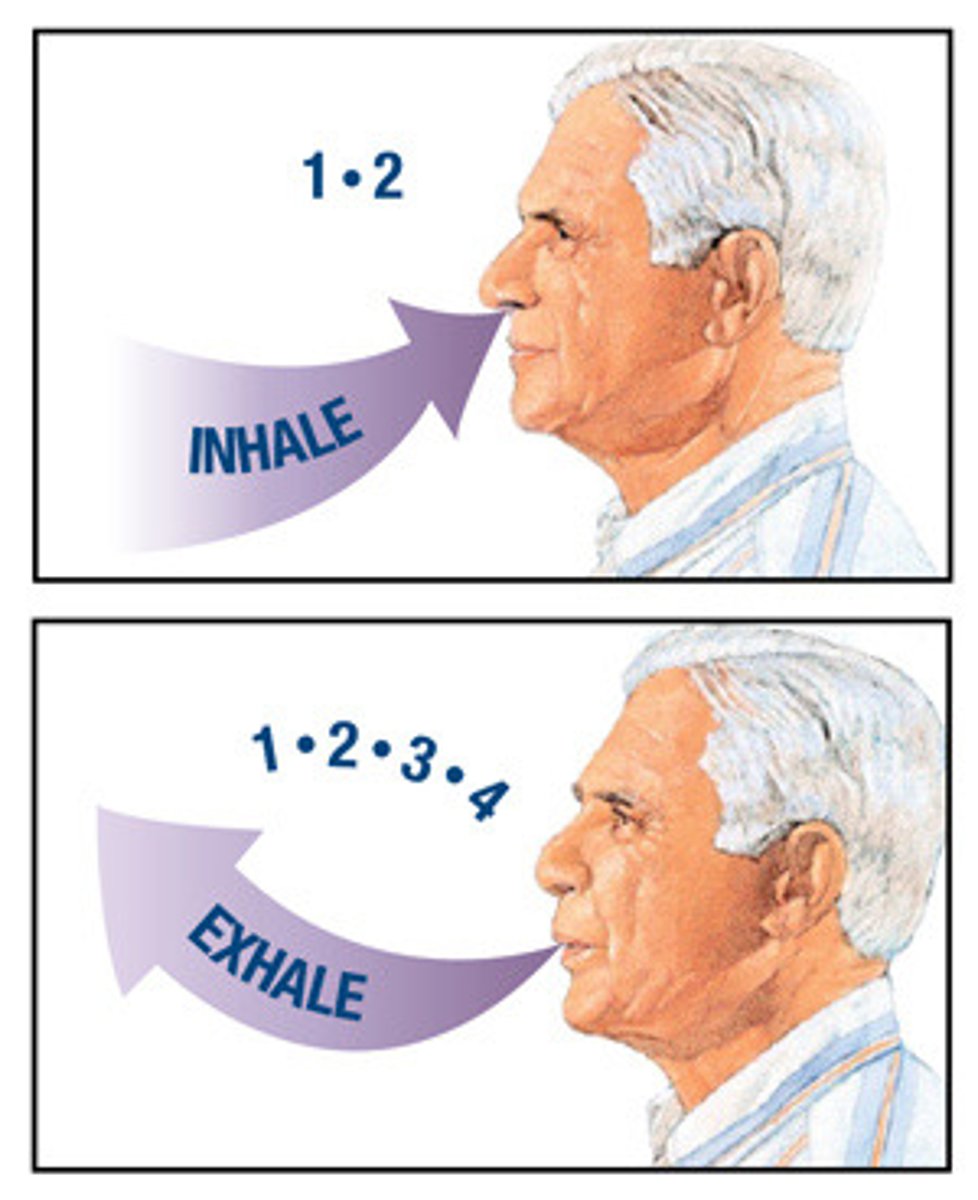
what is pursed-lip breathing?
***only used for dyspnea relief
- for every 1 second of inhalation, 2 seconds of exhalation
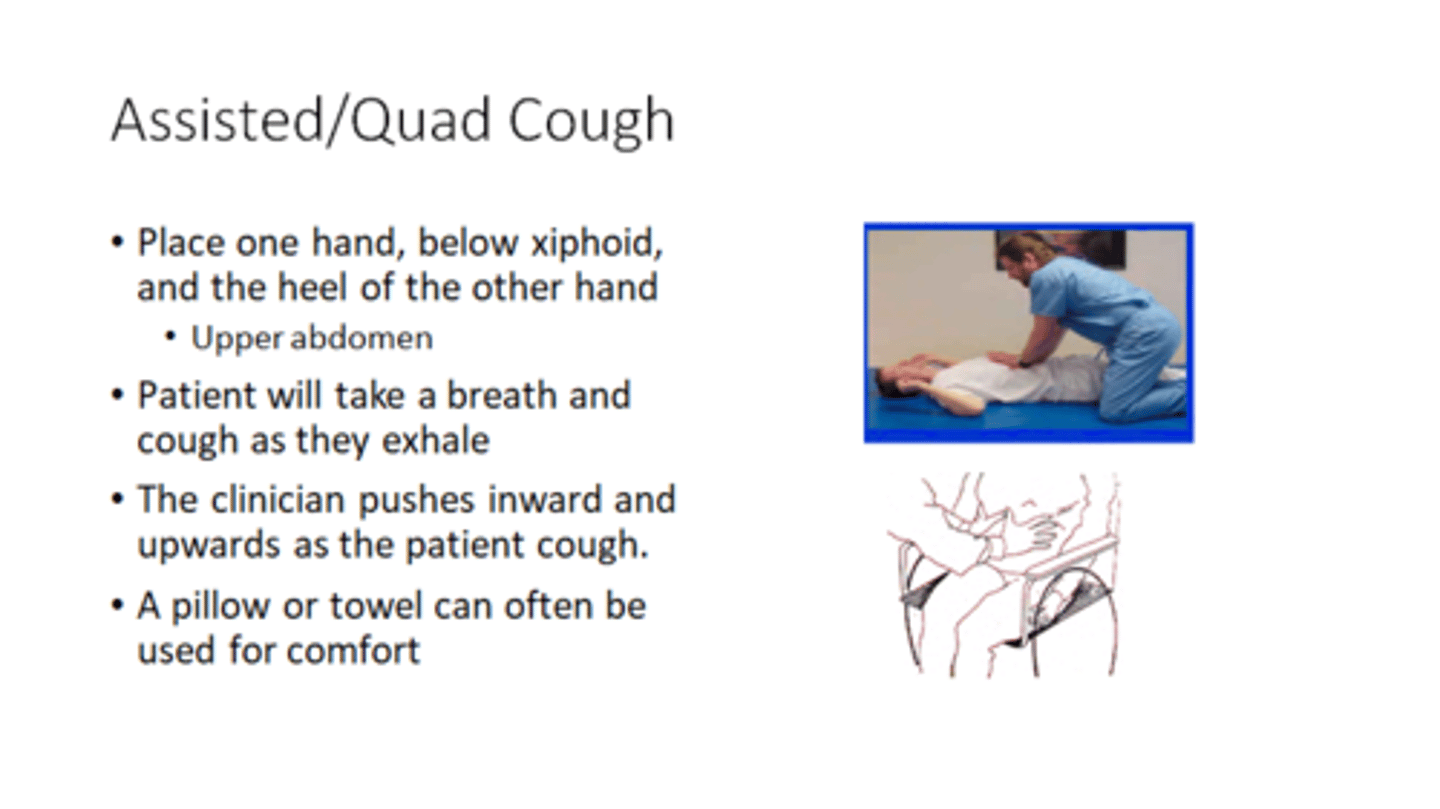
if a pt has weak/absent cough due to a neurological condition (SCI, ALS, prolonged vent use)- what are PT priorities? what techniques should you use?
- PT priorities: augment expiratory force, prevent secretion retention, reduce respiratory complications
- techniques: manually assisted cough, mechanically assisted cough
manually assisted cough
instruct the person to take a deep breath and deliver manual assistance as they cough
*timing of person and caregiver is key
mechanically assisted cough
devices that apply mechanical forces to the body or intermittent pressure changes to the airway to assist with coughing
risk factors for VTE formation
- Virchow's Triad (vascular stasis, endothelial injury, hypercoagulability)
- elevated risk for 5-6 weeks after surgery
complications of DVT
- PE
- post thrombotic syndrome (PTS)
what is PTS? sxs? long-term outcomes?
- permanent damage to valves in veins --> blood reflux
- chronic sxs: aching pain, intractable edema, limb heaviness, leg ulcers
- long-term outcomes: impaired functional mobility, poor QoL, increased healthcare costs
complications of PE
- death
- chronic thromboembolic pulmonary HTN (CTPH)
preventative measures of VTE
- LE exercises (prevent vascular stasis)
- ambulation
- hydration
- mechanical compression
- medication referral
UE DVT is associated with
cancer and use of PICC lines
signs and sxs of UE DVT
swelling, pain, edema, cyanosis, dilation of superficial veins
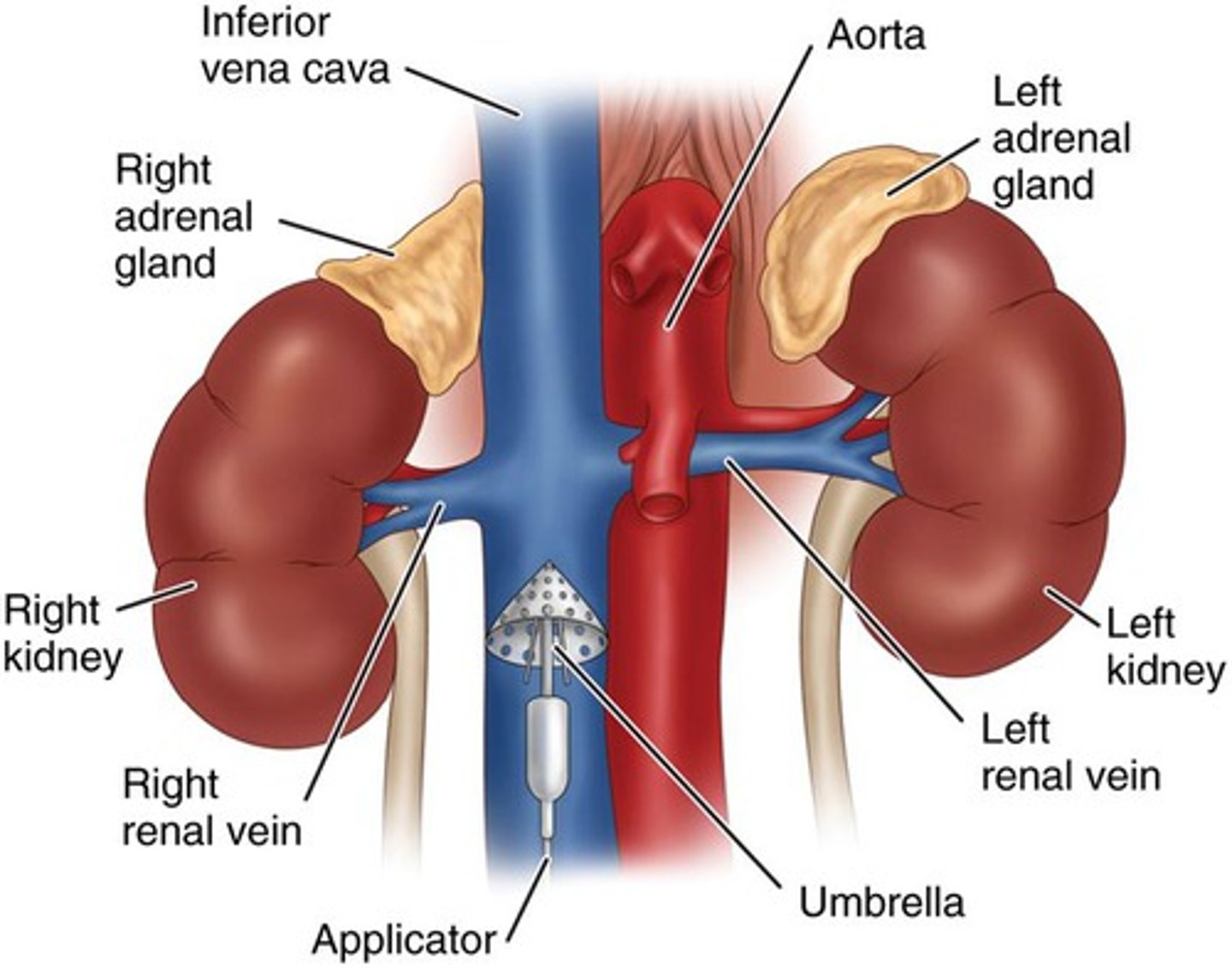
what are IVC filters?
- catch clots before they reach lungs
- used for people who can't be anticoagulated (oncology pts or if meds don't work)
when is compression use recommended?
- when a person is at high-risk
- sxs of PTS (pain and swelling) are present
ineffective discharge planning can increase risk of:
- falls
- readmissions
- caregiver burden
- institutionalization
PT, OT, SLP role in discharge? who has the ultimate decision?
- make recommendations
- pt, medical provider, insurance
PT-driven vs System-Driven discharge planning
PT-driven:*
- PLOF
- current functional status
- safety and fall risk
- ability to participate in therapy, learn, and carry over
- pt goals and preferences
- available assistance/support
System-driven:*
- insurance coverage and authorization
- facility acceptance criteria
- bed availability
- diagnosis-based coverage regulations
- LOS pressures
why are there discharge pressures from the hospital?
- hospitals are paid using diagnostic-related groups (DRGs)
- no matter how long pt stays, hospital gets a fixed rate
how does PT reduce hospital readmissions
- PT/OT during hospitalization
- early home-based PT
- when PT discharge recommendations are followed
what dischage destinations can PTs recommend?
- home
- inpatient/acute rehab
- SNF
pt can go home w/o services if
they're at PLOF and have no new need for assistance
pt can go home with OP PT if
- pt is not at PLOF
- has no new need for assistance
- can leave the home safely
pt can go home with home PT if
- pt is not at their PLOF
- either has no new need for assistance or has need for assistance with help available
- is homebound
what does it mean for someone to be homebound
- require the assistance of another person or an AD to leave the home
- OR leaving home is contraindicated or unsafe
- leaving the home requires considerable and taxing effort
(exceptions made for medical appts, religious services, special occasions)
t/f: the fact that nobody is able to drive the pt to OP PT is a reason that qualifies them as homebound
false