Lesson 28 - Wound Management
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
123 Terms
What degrees of contamination apply to surgical wounds only?
1. clean
2. clean-contaminated
What degrees of contamination apply to surgical and traumatic wounds?
1. contaminated
2. infected (dirty)
What is a Class I/Clean wound?
1. uninfected operative wound with no inflammation that does not enter the respiratory, alimentary, genital, or uninfected urinary tract
2. no break in aseptic technique
What is a Class II/Clean-Contaminated wound?
operative wound in which the respiratory, alimentary, genital, or urinary tract are entered without unusual contamination
What is a Class III/Contaminated wound?
1. open, fresh, accidental wounds
2. operations with major breaks in sterile technique
3. operations with gross spillage from the GI tract
4. incisions with acute or no purulent inflammation
What is a Class IV/Dirty-Infected wound?
old traumatic wounds with retained devitalized tissue and those that involve existing clinical infection or perforated viscera
What are some examples of clean surgeries?
skin incision, mass removal, exploratory laparotomy, ovariohysterectomy, castration
What is the infection rate for clean surgeries?
0-6%
What are some examples of clean-contaminated procedures?
enterotomy, cholecystectomy, placement of a drain in an otherwise clean wound
What is the infection rate for clean-contaminated surgeries?
4.5-9%
What is the infection rate for contaminated wounds?
6-28%
What actions should you take with contaminated wounds?
1. Antibiotic prophylaxis
2. lavage
3. +/- debridement (wounds)
What traumatic wounds are considered contaminated?
<12 hours post-wounding
What traumatic wounds are considered infected (dirty)?
>12 hours post-injury or overtly infected
What actions should you take with infected (dirty) wounds?
1. Antibiotics
2. Lavage
3. debridement
4. drainage
5. +/- wet-dry bandages
What is the first step to approaching a traumatic wound?
initial patient assessment (ABCs)
What is the second step to approaching a traumatic wound?
wound assessment
What is the third step to approaching a traumatic wound?
wound cleansing and debridement
What is the fourth step to approaching a traumatic wound?
+/- surgical intervention
What is the fifth step to approaching a traumatic wound?
wound management plan
What should be determined in the wound assessment step?
1. type of wound
2. location, proximity to vital structures
3. degree of contamination
4. assess for trauma to deeper tissues (ex. fracture)
5. +/- culture & susceptibility of wound (consider macerated tissue culture)
What is the "golden period" of traumatic wounds?
first 6-8 hours between contamination at injury and bacterial infection (>105 bacteria per gram of tissue)
What decision does the golden rule impact?
decision to close the wound
What is the goal of wound cleansing?
reduce bacterial contamination and remove gross contaminants and necrotic debris from within the wound
How do you clean a wound?
1. Wide clip of hair around wound
2. Aseptically prepare area around wound
3. Lavage or irrigate wound with copious amounts of warmed solution
What is a trick for avoiding hair in the wound when clipping?
use aqueous sterile lubricant or oiled clipper blades
What can you use to lavage and irrigate a wound?
1. Saline (NaCl 0.9%, isotonic)
2. Lactated Ringers Solution (LRS, isotonic)
3. Tap water (hypotonic)
4. Dilute antiseptic solutions [CHX, P-I]
What kind of solution is ideal for wound lavage?
isotonic
When should chlorhexidine be used for lavage?
only early in wound management
What form of chlorhexidine is used for wound lavage?
solution formulation (not scrub) at an appropriate concentration for wounds
What antiseptics are used in wound management?
1.chlorhexidine 0.05% solution
2. povodone-iodine 0.1-1% solution
3. hydrogen peroxide
How does chlorhexidine work for wound management?
1. Synergistic antibacterial effect when combined with TrisEDTA
2. Residual activity (up to 48 hrs)
What can be resistant to chlorhexidine?
some strains of Pseudomonas spp.
How does povidone-iodine work for wound management?
1. Broad spectrum of activity
2. Free iodine inactivated by organic debris
3. No significant residual activity
How does hydrogen peroxide work for wound management?
1. Effective sporocide → use when possible exposure to Clostridium spores
2. Less effective antiseptic compared to CHX & P-I
3. Effervescent action dislodges bacteria & debris
What is a downside to using hydrogen peroxide for wound management?
cytotoxic especially to new capillaries
How should povidone-iodine be diluted?
the color of tea
What is true of all antiseptics at high concentrations and/or with prolonged use?
cytotoxic and can cause delayed wound healing
What is the goal of wound debridement?
remove non-viable tissue from wound
Which antiseptic should be used in a purulent or necrotic wound?
1. chlorhexidine
2. hydrogen peroxide
Which antiseptic should be used in a potential exposure to Clostridium tetani?
hydrogen peroxide
Which antiseptic should be used in a periorbital wound or surgical procedure?
povidone-iodine
Which antiseptic should be used in an orthopedic procedure?
1. povidone-iodine
2. chlorhexidine can be used but is not ideal
Why is chlorhexidine not ideal for orthopedic surgeries?
potential for pseudomonas resistance
Which antiseptic should be used in an abscess?
1. chlorhexidine
2. povidone-iodine but not ideal
3. hydrogen peroxide
Why is povidone-iodine contraindicated in abscesses?
inactivated in organic material
How can non-viable tissue affect wound healing?
1. Increase risk of infection (anaerobic bacteria)
2. Delay wound healing
What are some tips for successful wound debridement?
1. May use multiple methods of debridement for the same wound
2. Wounded tissue may take days to "declare" itself (~48 hours)
What are the methods for wound debridement?
1. surgical
2. mechanical
3. hydrodynamic
4. biosurgical
5. enzymatic
6. autolytic (moist)
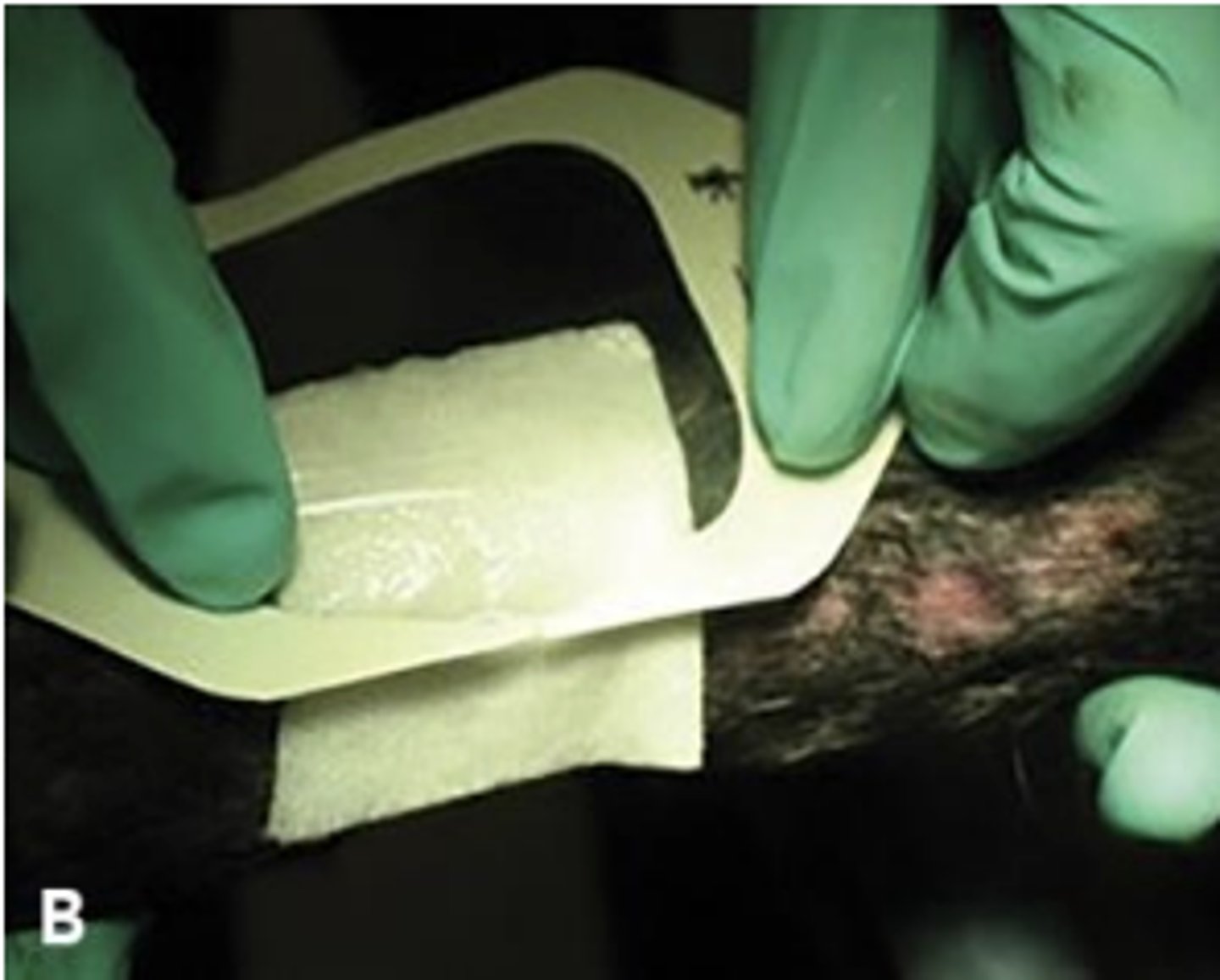
What is mechanical wound debridement?
wet-dry, dry-dry dressings and non-selective debridement
What is hydrodynamic wound debridement?
pressure irrigation
What is biosurgical wound debridement used for?
chronic, non-healing wounds
What is enzymatic wound debridement?
breaks down necrotic tissue and liquefies coagulum
What is autolytic (moist) wound debridement?
use hydrophilic, semi- or occlusive dressings

mechanical wound debridement

hydrodynamic wound debridement

biosurgical wound debridement
enzymatic wound debridement
autolytic wound debridement
How can surgical wound healing be classified?
stage of wound healing when the wound is closed
What does the type of wound healing depend on?
if the wound is closed or left to heal on its own
What type of wound closures heal with 1st intention?
1. primary closure
2. delayed primary closure
What type of wound closures heal with 2nd intention?
secondary closure
What phase of wound healing are primary and delayed primary closure wounds in?
inflammatory phase
What phase of wound healing are secondary closure wounds in?
repair phase (granulation tissue present)
What is primary closure of a wound?
wound repair within 24 hours of injury
What is primary closure indicated for?
1. clean surgical wound
2. contaminated traumatic wounds that are rendered clean
What is delayed primary closure?
wound repair within 5 days of injury before granulation tissue forms
What is delayed primary closure indicated for?
mild to moderately infected wounds (control infection before closing wound)
What is 2nd intention wound healing?
allow the body to heal the wound
What are the indications for 2nd intention wound healing?
1. wound too large to close surgically
2. affected area not amenable to surgery
3. heavily infected wound
4. surgical repair not an option (budget, anesthesia concerns, logistics)
What are the potential complications of 2nd intention wound healing?
potential complications: contracture, proud flesh (horses), delayed wound healing
What is secondary closure?
wound repair after granulation tissue formation
What are the steps to secondary closure?
1. "Freshen" wound edges
2. "Undermine" wound edges
3. Use tension relieving sutures and techniques if necessary
4. +/- place drain
What are the potential wound management plans?
1. Therapeutics
2. Bandages
3. Tetanus prevention (+/-)
4. Drains (+/-)
5. Skin grafting (+/-)
What are the different therapeutics you can use?
1. antibiotics (topical or systemic)
2. topical wound enhancers
3. analgesics like topical (lidocaine/bupivacaine), systemic (NSAIDs, opioids, gabapentin)
What are the benefits of moist wound healing?
1. Supports proliferation & migration of cells essential for wound healing processes
2. Supports production of cytokines & growth factors essential for wound healing
3. Prevents dehydration of wound bed & desiccation of cells critical to healing (fibroblasts, keratinocytes, inflammatory cells)
4. Prevents scab formation (scabs can trap unwanted bacteria and debris at wound site)
5. Allows for optimal balance in the stages of wound healing
6. Decreased pain (versus dry wounds which are irritated, more inflamed and have higher risk for infection)
7. Faster re-epithelialization
8. Reduced risk of infection (due to healthy balance of immune and other cells essential to wound healing)
9. Reduced scar formation
What are the layers of a modified robert jones bandage?
1. Contact (Primary) - also referred to as the wound dressing
2. Intermediate (Secondary)
3. Outer (Tertiary)
What are the functions of the contact (primary) layer of a wound dressing?
1. Debride (necrotic wounds)
2. Deliver topical medication
3. Absorb wound exudate
4. Protect granulation tissue (non-adherent only!)
What are the two basic types of contact (primary) layer of a wound dressing?
adherent and non-adherent
What are the indications for absorbent wound dressing?
open contaminated and infected wounds with exudate
What are the indications for adherent wound dressing?
necrotic wounds
What are the indications for non-adherent wound dressing?
1. ALL non-necrotic wounds particularly once granulation tissue has begun to form
2. Surgical wounds
What are the characteristics of an adherent layer?
1. Wicking action occurs as gauze dries and debris and exudate is absorbed into gauze
2. Wet dressings absorb faster than dry and have less wound dessication
3. Can use saline, hypertonic saline, 0.05% chlorhexidine
What is important about mechanical debridement?
non-selective and painful
What are the indications for using an adherent layer?
open wounds in need of debridement
What are some tips of successful contact layers?
1. discontinue as soon as debridement has been achieved
2. never use in the presence of granulation tissue
What kind of contact layer can be used in all wound types?
non-adherent
What is the function of non-adherent dressing?
help to retain moisture at wound site to promote moist wound healing
What will the frequency of dressing change depend on?
wound type and stage of wound healing
What is the function of the intermediate (secondary) layer?
1. Absorbent
2. Provides padding
3. Holds contact layer in place
4. Stabilizes & decreases movement (orthopedic bandage - depends on thickness of the layer)
What are the materials for an intermediate (secondary) layer?
1. cast padding
2. cotton wool wound
What is the function of the outer (tertiary) layer?
1. Protection
2. Stability
3. Holds other layers
How many layers are in the outer layer?
two (inner and outer)
What are the materials for an inner layer of the outer (tertiary) layer?
conforming bandage
What are the materials for an outer layer of the outer (tertiary) layer?
elastic adhesive tapes (Vetrap®, Elastikon®)
What is the order of most to least susceptible to tetanus?
equine, lamb, man > ruminants, swine > cat, dog
What is dead space?
abnormal space between tissue layers where blood and/or serum may accumulate
What are the techniques to manage dead space?
1. Suture obliteration
2. Compression bandage
3. Drainage
What are the indications for drains?
1. infection
2. dead space/seroma
3. body cavity effusions