Biomechanics Final SG - Davis portion
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
Leading causes of amputation
1 in ____ people in the US have one or more amputations.
Most occur in patients how old?
Leading causes? (3)
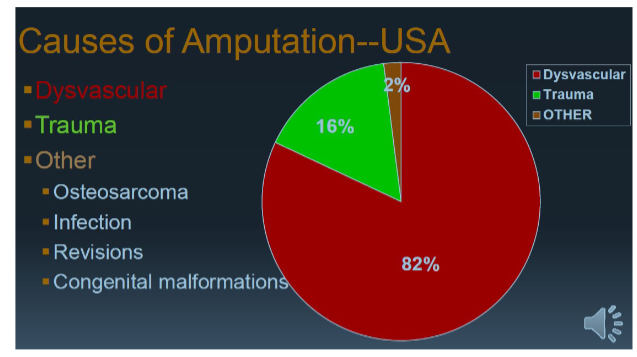
Leading Causes of Amputation
1 in 200 people in the US have one or more amputations
Most occur in patients 60 years-old and over
Causes:
Complications of diabetes and PVD (82%)
Trauma (16%) - young male population
Tumors & Congenital Malformation (2% each)
Causes of amputation in the USA pie chart: Fill in the blank
(Just a visual for the previous slide, Davis didn’t really go over it much)
Amputation terms
Trans
Disarticulation
Partial
Sound limb
Residual limb
Trans: When amputation crosses the axis of the long bone
EX: TTA transtibial amputation; TFA transfemoral amputation, TRA transradial amputation, THA transhumeral amputation
Disarticulation: When amputation is between long bones, through center of a joint
EX: Knee disartic → amputation of the knee but still keeping femoral condyles
Partial: Amputation of foot distal to ankle joint and of the hand distal to the wrist joint
Sound limb: Intact limb, healthy limb
Residual limb: The stump limb
Proper nomenclature for the Lower Limb (ISO)
For the following what is the proper naming for each
Ankle disarticulation
Below knee amputation BKA
Knee disarticulation
Above knee amputation AKA
Hip disarticulation
Transpelvic amputation
(Will be using abbreviations inside the test questions (the “right way” and the “wrong” way) just know if its its below knee, trans tibial, whatever the case is.) Probably best to just understand and focus on other cards)
Ankle (Syme) Disarticulation
All bones distal to the mortise joint
Transtibial Amputation (previous BKA)
Conventional, ETRL procedure (bony bridge between tib and fib). Takes a bit of healthy bone and puts it wire between 2 joints. This procedure delays prosthetic fitting.
Knee Disarticulation
amputation of the knee but still keeping femoral condyles
Transfemoral Amputation (previous AKA)
Ideal length is about 4 inches or 10 cm. Proximal to knee joint, allows femoral condyles to be excised with enough room to accommodate prosthetic knees.
Hip Disarticulation
removes the entire leg through the hip joint
Transpelvic Amputation
Removes the leg, hip joint, and portion of the pelvis
Proper Nomenclature for the Upper Limb (ISO)
Wrist Disarticulation
below elbow amputation
Elbow Disarticulation
above elbow amputation
Shoulder Disarticulation
Forequarter Amputation
(Same as previous slide)
Wrist Disarticulation
Transradial Amputation (previous below elbow)
Elbow Disarticulation
Transhumeral Amputation (previous above elbow)
Shoulder Disarticulation
Forequarter Amputation
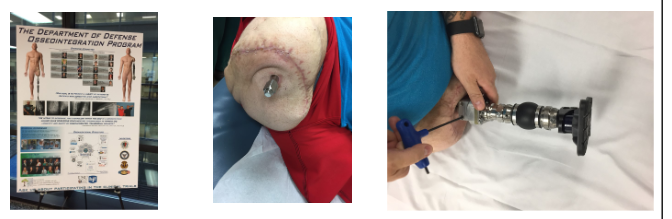
Osseointegration
What is it?
What are the two steps?
Attachment of prosthesis directly to the body
2 step surgery
Implant placement within the end of the bone
Placement of external protruding connector
Possible way of the future for prosthesis
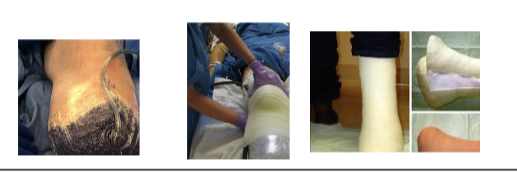
Postoperative compression dressing help with? (4) How long can it be used for post surgery?
Control Edema
Shape the limb
Protection of the residual limb
Fosters healing
May be used for weeks after surgery
Shrinkers
For TTA and TFA, the advantage of using a shrinker sock compared to wrapping methods are? What about for semirigid and rigid dressing?
Positive effects with use of volume management?
Why you would use a shrinker vs prosthetic sock?
Condie et al (1996) found that both TTA and TFA using a shrinker sock within 10 days after amputation demonstrated a significantly reduced time from amputation to prosthetic casting from those amputees using wrapping methods.
Moreover, TTA’s who received semirigid and rigid dressing demonstrated increased time until prosthetic casting
Positive effects with use of volume management: (7)
decrease edema
increase circulation
assist in shaping
provide skin protection
reduce redundant tissue problems
reduce phantom limb pain sensations
desensitize the residual limb (important for first 3 months)
Why would you use a shrinker vs prosthetic sock?
Shrinker: Wear it after surgery (When sutures are removed) to shape the limb and decrease levels of volume in preparation for a prosthetic. Also reduces inflammation. (Might need to wear it for the first couple of months and at night so it RL doesn’t swell)
Sock: To manage volume throughout the day as you wear the prosthetic. This is because the limb typically shrinks in size as the day goes on.
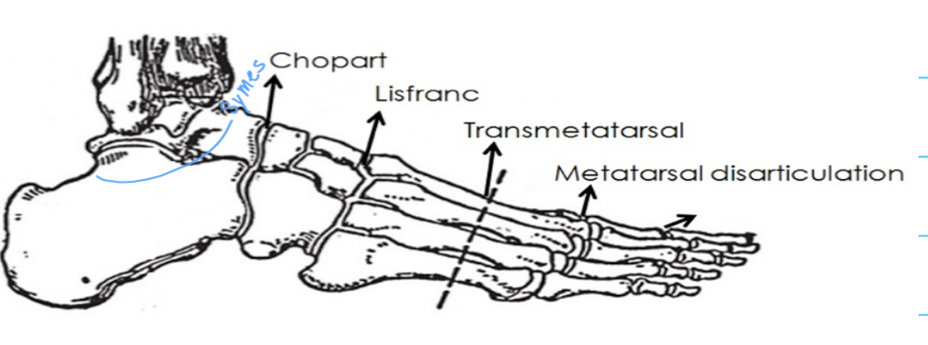
Partial foot amputation levels
Transmetatarsal
Lisfranc’s
Chopart
Symes
Transmetatarsal: through all metatarsals
Lisfranc’s (Tarsal-metatarsal): disarticulation of metatarsals
Chopart (Midtarsal): disarticulation of tarsal bones (Talus gets removed but most of calcaneus remains)
Symes: Removes a solid portion of talus AND a good chunk of the calcaneus)
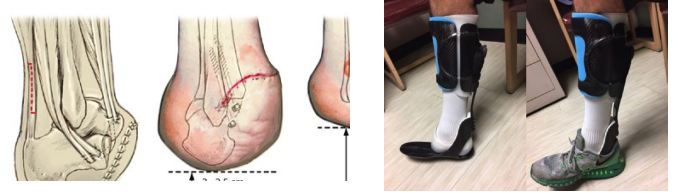
Syme’s Amputation
What is it? What bones are amputated?
For this amputation what is left?
What is attached to the distal tibia?
(Davis said focus more on this one than the others)
Ankle Disarticulation
All bones distal to the mortise joint. Removes a solid portion of talus AND a good chunk of the calcaneus.
Pt is left with right and left malleoli
Heel pad and inferior calc are attached to distal tibia
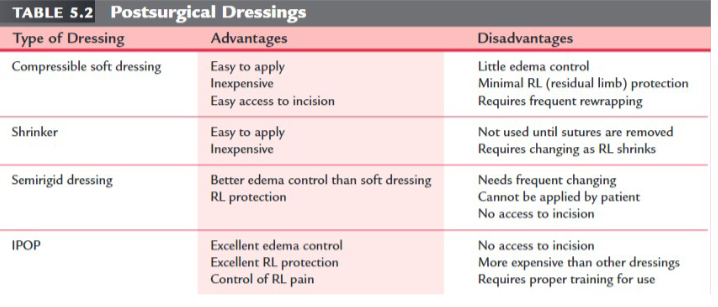
Post surgical dressing (Advantages and disadvantages)
Compressible soft dressing
Shrinker
Semirigid dressing
IPOP (Immediate Post-Operative Prosthesis)
Compressible soft dressing
Advantages:
Cheap
Easy to apply
Easy access to incision
Disadvantages:
Little edema control
Minimal RL protection
Requires frequent rewrapping
Shrinker
Advantages:
Cheap
Easy to apply
Disadvantages
Not used until sutures are removed
Requires changing as RL shrinks
Semirigid dressing
Advantages:
Better edema control than soft dressing
RL protection
Disadvantages:
No access to incision
Cannot be applied by patient
Needs frequent changing
IPOP
Advantages:
Excellent edema control
Excellent RL protection
Control of RL pain
Disadvantages:
No access to incision
More expensive than other dressings
Requires proper training for use
Phases of Amputee Rehab
What are the three phases? When does it take place and how long does each last?
Not so much worried about this but have a rough idea of what's happening in the healing phase vs the maturation phase)
Phases of Amputee Rehab
Healing
Immediately following surgery
Postoperative phase
Pre-prosthetic phase
Lasts up to 4–8 weeks
Maturation (Prosthetic phase)
Temporary prosthesis is given
Definitive prosthesis given when limb is stable
Gait training and prosthetic management
Around 4 to 6 months post surgery
Definitive
Long-term follow up
Learning to return to sport/return to work
The “K” levels: Medicare Functional Index
What are the 5 levels and what does each entail?
(VARIABLE CANDANCE - BIG IMPORTANT TERM)
K0 = not a potential user for ambulation or transfers / no feet allowed / no knees allowed. Insurance wont cover and pt will not get prothesis or socket.
K1 = a potential household ambulatory including minimal transfers / SACH or single-axis foot / single-axis knee or safety/lock (Given the most minimal foot and knee, pt only moves a bit around the house (barely active).
K2 = a potential limited community ambulatory / flexible keel foot / multi-axial foot / same knees as level 1. Pt is moving well at home and performs limited ambulation in community.
K3 = community ambulatory using variable cadence including therapeutic exercise or vocation / energy story feet / pneumatic and hydraulic knees. The sweet spot → pt will get approved. Can do everything such as play sport, go to work, etc)
K4 = high activity user who exceeds normal ambulation / all feet / all knees. Paralympian → running blades not covered by insurance usually sponsored
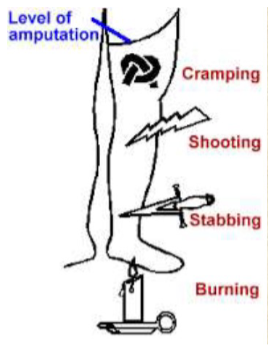
Phantom pain and sensation
Phantom pain is?
What do people that have had a limb remove sometimes report? This is know as?
Does this get better overtime without treatment?
Know differences between phantom pain, phantom limb sensation, and physical pain
Phantom pain is pain that feels like it's coming from a body part that's no longer there.
Most people who've had a limb removed report that it sometimes feels as if the amputated limb is still there. This painless phenomenon, known as phantom limb sensation
Phantom pain often gets better over time without treatment, for some patients managing phantom pain can be challenging.
Phantom pain and sensation - The specifics of each
Phantom sensation
Phantom pain
Residual limb pain
Know differences between phantom pain, phantom limb sensation, and physical pain
Phantom Sensation: A nonpainful sensation or awareness experienced that gives form to a body part with specific dimensions, weight or range of motion.
Phantom Pain: A painful sensation-experienced below the residual limb
Residual Limb Pain: Pain arising in the residual limb from a specific anatomical structure that can be identified.
Upper extremity surgeries PEDS
Surgery play a role in the management of children with? Associated with?
Reconstructions may be performed in infants to allow? What three professionals must work closely together?
Prosthetic fitting are generally ____ ____ dependent and have a variety of options. What are they? (4)
Families tend to prefer a ______ device that resembles what?
Benefits to early prosthetic fitting? (2)
Know what's going to be involved with UE surgeries especially with children, hinted on that.
Surgery plays a major role in the management of children with longitudinal upper arm or forearm deficiencies.
Associated with nonfunctional hands, polydactyl (extra fingers or toes), or other deformities.
Reconstructions may be performed in infants to allow for normal development in manual tasks
Surgeon, prosthetist, and PT/OT staff need to work closely together, making sure children are monitored throughout the developmental stages.
Prosthetic fitting are generally limb level dependent and have a variety of options.
Opposition, body powered, externally powered devices with hands, hooks with various shapes
Families tend to prefer terminal device that resembles a hand
Benefits to early prosthetic fitting
Encouraging bi manual tasks
Facilitating symmetric crawling
Lower extremity surgeries PEDS
Reconstruction surgery is often delayed for what reason?
Maintenance of long bone growth plates allows for?
Severe deformities that interfere with early fitting or with function require? What is important to prevent? What surgery can be done to provide the child with a functional residual limb?
Same thing as last slide, but also know different surgical processes for LE surgeries. BIG ONE TALKED ABOUT FOR TRANSTIBIAL IS? WHAT DOES IT DELAY?
Reconstructive surgery is often delayed to allow greatest amount of bone growth.
Maintenance of long bone growth plates allows for greatest development of limb length.
Severe deformities that interfere with early fitting or with function require early surgical intervention
It is important to prevent progressive deformities that may occur as a result of muscle and nerve imbalances.
Surgery to increase bone length using the Ilizarov technique can be successfully performed to provide the child with a functional residual limb.
BIG ONE TALKED ABOUT FOR TRANSTIBIAL IS ERTL PROCEDURE: Bony bridge between tib and fib
Takes a bit of healthy bone and puts wire between 2 joints
This procedure delays prosthetic fitting

Civilian statistics (For UE)
What is the total amount of amputees in the USA?
How many major amputations occur annually in the USA?
What age population does it tend to occur in?
95% occur below the?
Primary reason for amputation?
What percent of UE amputees do NOT wear a prosthesis?
Prevalence of UL amputation: Of the 5/100,000 UE amputations in the US
3.8/100,000 were _____ related.
1.3/100,000 were _____ related
<1/100,000 were ______ or ______ related.
total of 1.9–2.1 million amputees in the USA
185,000–200,000 major amputations occur annually in USA
Tends to occur in younger patients
95% occur below the elbow
Primarily due to trauma
50% of upper extremity amputees do not wear a prosthesis (Davis said this with emphasis)
Prevalence of UL amputation
Of the 5/100,000 UE amputations in the US
3.8/100,000 were trauma related.
1.3/100,000 were dysvascular related
<1/100,000 were congenital or cancer related.
UE classifications
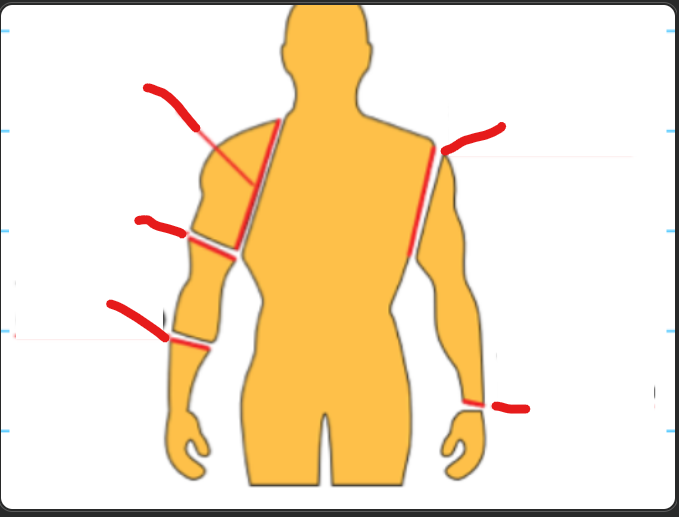
Partial hand
Wrist disarticulation
Transradial (below elbow)
Elbow disarticulation
Transhumeral (above elbow)
Shoulder disarticulation
Forequarter
six prosthetic options for UE
Body powered prosthesis
How does it work? Basic requirements?
Electrically powered prosthesis
How does it work?
Hybrid prosthesis
What is it?
Passive prosthesis
What is it used for?
What are the last two options?
Body powered prosthesis / cable operated
Body motion/strength is captured to operate terminal device (hook, hand, etc)
Basic Requirements: AROM, ability to generate force associated with those motions. Muscles are required to use it.
Electrically powered prosthesis
Electrical signal on the surface of the skin is used to communicate to the terminal device and power is supplied by an external battery
Hybrid prosthesis
Both body and electrical
Passive prosthesis
Cosmetic purposes
Activity specific prosthesis
Non-prosthetic user (SAID THIS ONE IS ON THERE FOR SURE, CANT FIND ANY INFO ON IT)
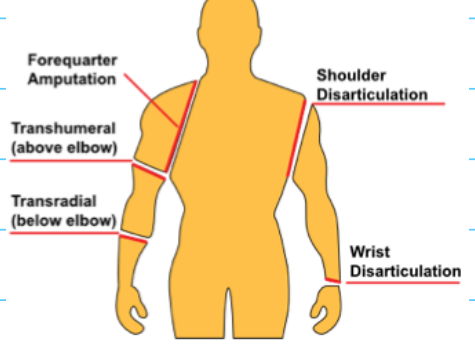
Body powered control system
For each what is the terminal device, elbow flexion, elbow lock:
Shoulder disarticulation
Transhumeral
Transradial
Most important motions for UE?
(Know this, already hinted on the test question given in class what movements would be needed)
Shoulder disarticulation
Terminal device: Biscapular abduction and latissimus dorsi
Elbow flexion: Biscpaular abduction and latissimus dorsi
Elbow lock: Scapular elevation
Transhumeral
Terminal device: Biscapular abduction and humeral flexion
Elbow flexion: Biscapular abduction and humeral flexion
Elbow lock: Shoulder depression and humeral abduction and extension
Transradial
Terminal device: Biscapular abduction and humeral flexion
Elbow flexion: NA
Elbow lock: NA
Most important motions for UE
Glenohumeral flexion
Shoulder elevation/depression
Scapular abduction (protraction)
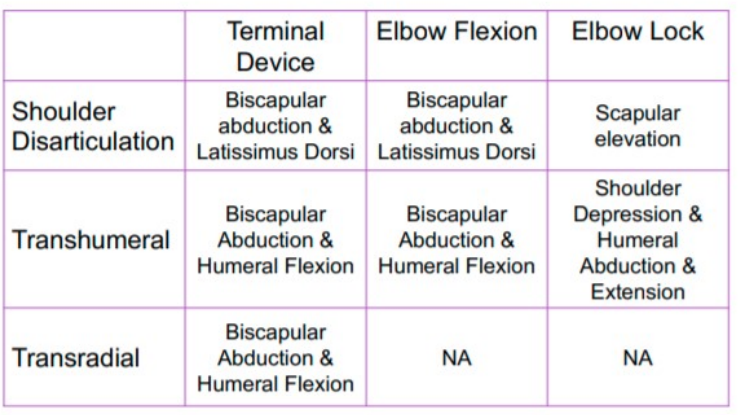
For the following picture label:
Ring or cross of post straps is near what spinal level and on what side?
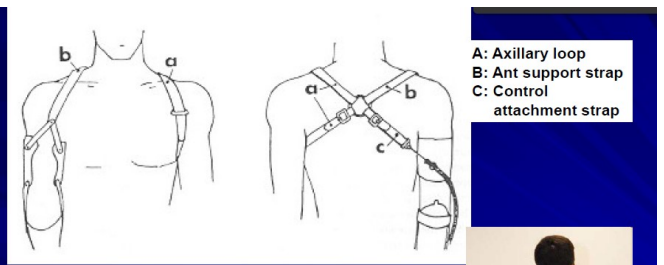
Ring or cross of post straps is near C7 on the sound side
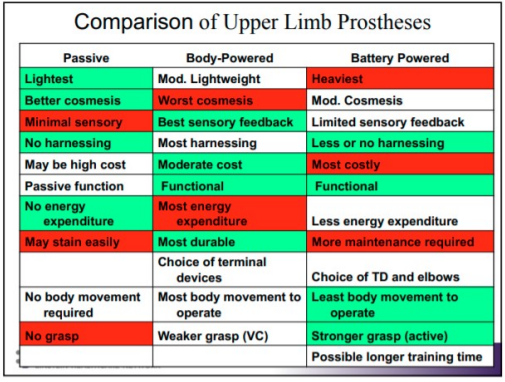
Upper extremity prosthetic comparisons
For the following (Passive, body-powered, battery powered) state its:
Weight level (Lightest, moderate, or heaviest)
Cosmesis (Better cosmesis, moderate cosmesis, or worst cosmesis)
Sensory (Best sensory feedback, limited sensory feedback, or minimal sensory)
Harnessing (Most harnessing, less or no harnessing, or no harnessing)
Function level (functional or passive)
Energy expenditure (No energy expenditure, less energy expenditure, or most energy expenditure)
Maintenance/durability level (Most durable, may stain easily, or most maintenance required)
Choice of terminal devices (choice of terminal devices or choice of terminal devices and elbows)
Movement required (No body movement required, least body movement to operate, or most body movement to operate)
grasp level (Stronger grasp (active), weaker grasp (VC), or no grasp)
Which one might have possible longer training time?
He didn’t really say much but I would know this
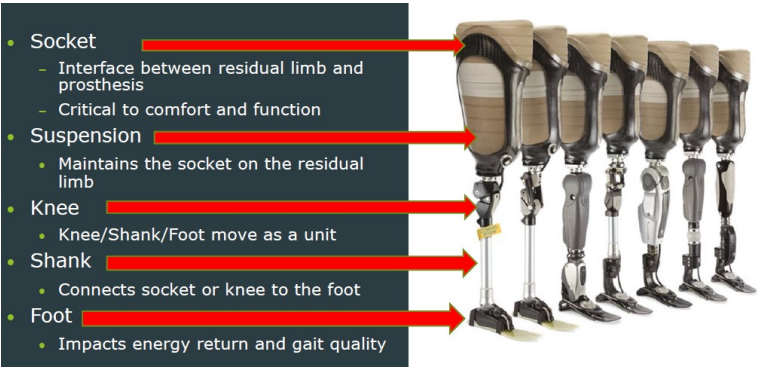
LE prosthetic - The components
What does each of the following do:
Socket (and what is it critical for)
Suspension
Knee
Shank (and what are its two types with differences)
Foot
The pylon is in the roughly the same area as? The foot ankle assembly is important for transtibial or transfemoral?
Socket
Interface between residual limb and prosthesis
Critical to comfort and function
Suspension
Maintains the socket on the residual limb (how they wear it without falling out)
Knee
Knee/Shank/Foot move as a unit
Shank
Connects socket or knee to the foot. Where the tib fib would be.
transmits forces and restores limb shape. Can be endo skeletal (internal skeleton supporting load. lighter and covered with cosmetic foam) or exoskeletal (hard laminate; outer structure provides support. Hallow and strong)
Foot
Impacts energy return and gait quality
the pylon (metal stick part) and the shank are in that rough same area, transfemoral is important in the foot ankle assembly
Types of prosthetic feet? (8)
Types of Prosthetic Feet
SACH
Single Axis (Anterior bumper limit dorsi 5-7 and posterior bumper limit plantar 15, no medial lateral)
Elastic keel
Multi-axial (keel is generally nonflexible, moveable ankle joint/multiple planes, may or may not have adjustable bumper)
Dynamic response
Hybrid
Microprocessor Ankles
Running Feet
more on individual ones in later card
Which foot is most appropriate? (Energy returns for the following)
SACH foot
Seattle foot
Flex foot
Human foot
SACH foot: 39% energy return
Seattle foot: 71% energy return
Flex foot: 89% energy return
Human foot: 246% energy return
Non-articulated foot/ankle assemblies
Have continuous ______ ______ from the _____ __ ____ _____ to the _____ __ ___ ______.
What is the solid ankle cushion heel (SACH) foot?
Articulated joint?
At heel strike, the heel wedge does what? Keel is made from?
Avantages? Disavantages?
Variations? (3)
Used by what K level patients?
Have continuous external surfaces from the sole of the foot to the shank of the prosthesis
Solid Ankle Cushion Heel (SACH) Foot:
A molded heel cushion made of a high-density foam rubber forms the foot and ankle into one component-cushion heel acts as a posterior bumper
No articulated joint
At heel strike, the heel wedge compresses to create a DF movement; keel is made of hardwood or aluminum
Advantages: inexpensive, light weight, durable, reliable, no moving parts, good absorption of ground reaction forces, more stability than single or multi-axis feet, child sizes available
Disadvantages: no adjustment on DF/PF, walking up hill is difficult, limited motion for active people, energy consuming, rigid
Variations: symes foot, sculptured toe foot, high heel for women
Used by limited or household ambulators (K1 level)

Tru-step foot or college park (didnt talk about this one)
What does it allow the pt to do? designed to mimic? First foot to do what? How does it decrease GRF and increase stability? What can be changed to provide correct resistance?
Elastic keel foot (didnt talk about this one)
Made form what type of material? Helps with what and has no what? Forefoot can do what? Remains ______ and _____ during standing and walking → a _____ response
Hybrid prosthetic feet (didnt talk about this one)
What material does it use and allows for what? Combination of what two things? Positive? Negative? Goal?
Dynamic response feet (KNOW THIS ONE FOR SURE, more on it next slide)
What does it do? Is there moving parts? Comes in? Allows for easier what due to the carbon fiber? Functions as what and when does it cushion, store energy, and return energy?
For single axis foot, anterior bumper and posterior bumper are?
Tru-step foot or college park
Allows pt to walk on dynamic surfaces
Designed to mimic anatomical foot and ankle
First foot to do 8 motions PF/DF, INV,EVR, ABD/ADD, SUP/PRO
3 part weight transfer system and shock absorbing heel to decrease GRF and increase stability.
3 bumpers can easily be changed to provide correct resistance
Elastic keel foot
Made of flexible material
Helps with push off movements → no moveable ankle joints
Forefoot can conform to uneven terrain, remains supportive and stable during standing and walking → dynamic response
Hybrid prosthetic feet
Using carbon fiber and allow certain moving parts
Combination of multi axis and dynamic response
+ would be accommodation to various surfaces
- would be increased weight cost and maintenance
goal: decrease cost and allow K2 level users to be able to get dynamic response foot
Dynamic response feet (more on another slide)
store (at heel strike) and release (at toe off) energy, no moving part
comes in different shapes and sizes for adults and peds
easier to walk, run → carbon fiber does all the work
Functions as a spring
cushion (at IC) → stores energy (through midstance) → return energy (pre swing)
Anterior bumper or stop (DF bumper)
Controls the amount and rate of dorsiflexion
Posterior bumper (PF bumper)
Controls the amount and rate of plantarflexion
Dynamic response feet
What does it do?
Functions as a? _____ at initial contact, ______ ______ through midstance and _____ _____ at pre-swing
Variation depend on?
Secured inside a?
Assists as a _____ _____ at midstance
Keel is made of?
Ankle joint mobility? What may it have?
Store and release energy
Function as a “spring”
Cushion at initial contact, store energy through mid-stance and return energy at pre-swing
Many variation depending upon length of the residual limb
Secured inside a cosmetic shell
Assist as a ankle rocker at midstance
Keel is made of a spring-like material
No moveable ankle joint
May have split toe design or urethane molded within keel

Below knee amputation (Amputation level: Transtibial)
What is it? Ideal length being from the?
Long transtibial is more than _____ of the tibial length.
Short transtibial is less than _____ of the tibial length. Just distal to the?
Advantages (Vs transfemoral) (3)
Energy expenditure (Unilateral and Bilateral)
Amputation Level: Transtibial: Below-knee amputation (BKA)
Resection through the tibia and fibula with the ideal length being from the proximal 1/3 to the middle of the limb
Long transtibial is more than 50% of the tibial length
Short transtibial is less than 20% of the tibial length
Just distal to the tibial tuberosity
Advantages (vs. transfemoral):
Mortality is lower
Better prospect for prosthetic rehab
Decreased phantom pain
Energy Expenditure:
Unilateral 10–20%
Bilateral 20–40%
Below knee amputation (Amputation level: Transtibial) continued:
Fibula is transected how much shorter than the tibia? Why?
If the fibula is transected the same length as the tibia, what can happen?
If the fibula is cut too short this results in?
What shape is ideal for prosthetic fitting techniques?
A bevel is placed on the _____ _____ _____. This is to minimize?
To avoid painful neuroma, what should be done?
Fibula is transected 1 to 2 cm shorter than the tibia to avoid distal fibula pain
If the fibula is transected at the same length as the tibia, the patient senses that the fibula is too long, which may cause pain over the distal fibula
If the fibula is cut too short this results in a more conical shape, rather than the desired cylindrical-shape residual limb
A cylindrical shape is better suited for total contact prosthetic fitting techniques
A bevel is placed on the anterior distal tibia to minimize tibial pain on weight bearing
To avoid a painful neuroma, a collection of axons and fibrous tissue, nerves should be identified, drawn down, severed and allowed to retract at least 3 to 5 cm away from the areas of weight-bearing pressure
Diagnostic test sockets (DTS) (Check socket)
Made with?
Assess fit both ______ and ______.
Ensures?
For transtibial:
Patients may be sent out with DTS on a?
Allows for what adjustments?
Helps ensure that the prothesis will?
Thermal plastic used with casting tech
Assess fit both statically and dynamically
Ensures proper fit and function of the prosthesis
Transtibial:
On a case-by-case scenario, patients may be sent out with DTS
Allows for custom socket adjustments
Helps ensure the laminated prosthesis will provide the patient with the best possible outcome.

Transtibial sockets
What are the types of TTA sockets?
He talked about this slide but didnt really say much but know
Types of TTA sockets
Plug Fit Socket
Patella Tendon Bearing Socket (PTB)
Supracondylar
Suprapatellar
Total Surface Bearing Socket (TSB)
Hybrid Sockets
didnt really talk much on this slide
Patella tendon bearing socket
This socket is the?
increases _____ or ____ _____ in the area of the patella tendon, ______ to the patella
Patellar tendon bar: what percent of weight is born here when standing and walking? contouring is? This allows for what two things?
most common
Increase contact or weight bearing in the area of the patella tendon, inferior to the patella
Patella tendon bar: 30% of the weight is born here when standing and walking
pressure related contouring
interfaces pressures in socket
Distributes pressure to RL
socket design for PTB
What does this prevent?
The top of the anterior wall bisects what?
The posterior wall trim line is (higher or lower) or?
What if the pt has too high of a post wall?
What direction of force does a posterior wall apply and why?
Why is it contoured?
The medial and lateral walls are slightly higher or lower than the anterior wall? Why?
Tibial flares still do what?
Pt with high medial and lateral walls typically have a what? Why?
prevents skin problems, choke syndrome, ulceration
The anterior wall = top of anterior wall bisects patella
The posterior wall = trim line higher or bisects patella tendon bar
If pt has too high post wall → decrease knee flexion and carbon fiver digging into back when firing
Applies an anterior directed force to maintain the patellar tendon on the PTB bar
Contoured to prevent increased pressure on the HS.
The medial and lateral walls slightly higher than the anterior wall adding stability.
Tibial flares still take weight
Pt with high med and lat walls = shorter RL for increased valgus/varus stability.
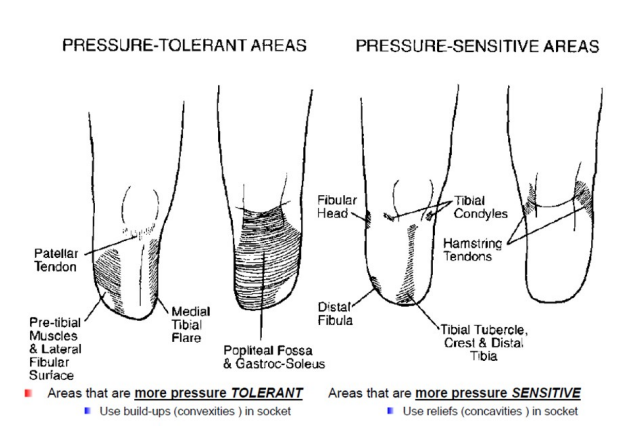
What are the pressure tolerant areas vs pressure sensitive areas of a transtibial amputee? What do pressure tolerant areas use compared to pressure sensitive areas?
Pressure tolerant: Use build-ups (convexities) in socket (presses into these areas)
Patellar tendon
Pre-tibial muscles and lateral fibular shaft/surface
Medial tibial flare
Popliteal fossa and gastroc soleus
Pressure sensitive: Use reliefs (concavities) in socket (pushes away from these areas)
Fibular head, distal fibula
tibial condyles
tibial tubercle, crest and distal tibia
Patella
hamstring tendons
Peroneal nerve
Areas that we can relief: pressure sensitive
Areas that can maintain pressure: pressure tolerant
Transtibial socket interface materials
What type of inserts are used for hard fit vs soft fit?
Silicone/gel liners are good for? three types?
Prosthetic socks (ply? accommodates? How much ply before pt needs a new prosthesis?)
Inside is made of? Sheaths are made of?
Hard Fit – no insert used
Soft Inserts: Pelite inserts
Silicone/Gel liners: Most widely used now, good cushion and pressure distribution, decreases shear, good for sensitive/adherent skin
Silicone Elastomers
Silicone Gels
Polyurethanes
Prosthetic socks
Ply (1 ply ~2 mm) add ply as day goes on
Accommodate limb volume changes
Once pt gets to 15 - 20 ply then its time for a new prosthesis
Flexible thermoplastic inner, Nylon sheaths

More on gel liners
Pt will be given how many at a time? Why? Is it covered by insurance?
When putting on a gel liner what are the three steps?
Signs of bacteria?
PT will be given 2 at a time (wear 1 while the other is getting cleaned), Covered by insurance
When putting on a gel liner:
Place inside/out and squeeze bottom
Make sure its not placed inward to avoid hickey
Mare sure limb reaches the end, then roll up liner
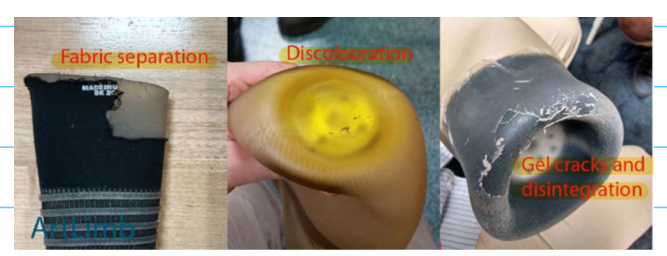
Signs of bacteria: Fabric separation, discoloration, gel cracks and disintegration
Transtibial socket suspension
What is suspension?
Types
Corset
How common? Seen is pts with long or short RLs? Used for?
Positives? Negatives?
Straps/Velcro cuff
Common for pt undergoing what changes (and what type of atheletes)
what does it look like?
positives? negatives?
Anatomical
For long or short RL and what type of instabilities?
Positives? Negatives?
Silicone suction suspension
Pin is attached to? Allows for?
Positives? Negatives?
Avoid if? What K levels is this for?
seal in liner
What type of system?
Each rink provides what?
Positives? Negatives?
external suspension sleeve (Nothing on this)
vacuum assisted socket system
How does this socket work? Increased _____ with decreased _____ on RL
Positives? Negatives?
didnt really talk about this slide but know
Suspension is the method by which the prosthesis is held on the residual limb
Types
Corset
Uncommon; seen with short RL. Used for knee stability and hypersensitive stages. Max med and lat support → unloads RL by 30%. Heavy, bulky, pistoning
Straps/Velcro Cuff
Supracondylar cuff. Common for pt undergoing increased leg volume changes (for triathletes). Inverted v strap with waist belt
+ easy to adjust, cheap, effective
- slight pistoning, not for short RL
Anatomical
PTB-SC & PTB SC/SP Socket. For short RL and ligamentous instability.
+ resists genu recurvatum
- kneeling difficulties, cosmetic appearance with sitting
Silicone suction suspension (3-S)
Pin attached to sleeve liner. Always volume fluctuations
+ increase cosmesis, decrease need for straps, decrease shear, decrease pistoning
- irritation from sleeve, costly, elongates distal tissues, increase sweat.
Avoid if neuromas present on distal RL. K2-K4
Seal-in liner
Vacuum system → hypobaric sealing membrane. Each ring provides increased suction/vacuum
+ decrease need for straps, prevent elongation of distal tissue, check for hypersensitivity
- irritation, costly, allows limited volume fluctuations with proximal ½ socks
External Suspension Sleeve
Vacuum assisted socket system (VASS)
Battery powered pulling air out of liner to make sure it stays on. Increase suction with decrease pressure on RL
+ increase RL volume control, decrease friction and pistoning, increase comfort
- heavy, costly, needs good hand function to turn on and off.
Transfemoral amputees - Above the knee amputation TFA:
The ideal length is ______ proximal to the _____ _____. What does this allow for?
Femoral length percentages for long, transfemoral, short transfemoral?
Advantages? Disadvantages?
Energy expenditure?
Surgical concerns?
Have a rough idea of transfemoral amputees, Know what disadvantages that can fall onto pt with short transfemoral amputees, Bilateral transfemoral amputees use?
Transfemoral Amputees
Above knee amputation (TFA): The ideal length is 8 cm proximal to the knee joint, which allows femoral condyles to be excised with adequate room to accommodate prosthetic knees
Long = more than 60% femoral length
Transfemoral = between 35%–60%
Short transfemoral = less than 35%
Advantages:
the healing rate is greater than more distal amputations, the residual limb in many cases is easier to fit
Disadvantages:
mortality is greater
more surgical complications
cut muscle bellies retract
muscle atrophy and loss of function
longer to shape the residual limb
rehab for prosthetic walking is less successful
Energy Expenditure:
Unilateral 60–70%
bilateral >200%
Surgical concerns:
Loss of adductor strength (ALABAM)
Adductor longus
Adductor brevis
Adductor Magnus
BILATERAL TRANSFEMORAL AMPUTEES USE STUBBIES!
Transfemoral socket design
Types
Bilateral TFA stubbies or shorties
This socket is very what? Pts have to learn how to?
Very challenging to learn what two things?
Lower to the ground = what?
Worn by using what?
What gait pattern do you need when wearing this?
Plug socket
Shape?
Tissue tends to displace which direction? Causes what type of rolls
Pressure distribution is?
Typically made from what?
How is it suspended?
The end bearing is very _____, causes what?
Quadrilateral socket
What does scarpas bulge do? Made for patients to? Involved with?
Posterior wall: flat slanting anterior for flexion of how many degrees? This puts what on a stretch and maintains what?
Medial brim: slightly higher or lower than the posterior brim? Does NOT press on what? Inward indentation near what muscle, pushing what what two directions for increased what?
Ischial Ramal containment socket
IC and CAT - CAM socket → what?
Anterior walls significantly reduces what? Why?
Hybrid socket
Mix of what two?
Marlo anatomical socket
Focuses on what?
Contained within socket without impeding what muscle?
Posterior trim line are below what?
Increase ROM with hip _____ ____ is ______
Elevated vacuum sockets (Brimless or sub ischial socket)
How many inches below the ischial trim lines?
Roll on liner contains what muscles?
Paired with what type of suspensions?
Positives? For pt with what three things?
Many sockets designs/used these days are a?
Types:
Bilateral TFA stubbies or shorties
Very functional, Pt learning how to walk
Very challenging to learn core activation and a balance
Lower to the ground = easier weight transfer
Worn by using their knee joints
Circumduction gait
Plug Socket
Larger at top, tapered to bottom
Tissue tends to displace upward - fleshy rolls
Poor pressure distribution
Typically made from carved wood
pelvic band and suspenders for suspension
poor ending bearing = increased tissue breakdown
Quadrilateral Socket
Scarpa bulge: maintains ischial tuberosity on ischial seat by providing counter pressure against post wall
Made for pt to stand and walk comfortably
Involved with pushing anterior to posterior
Posterior wall = flat slanting ant for flex of 15 degrees (glute and hamstrings on stretch. Maintains knee extension
Medial brim = slightly lower than post brim, not pressing on pubic ramus. Inward indentation near psoas, pushing anterior to posterior for increased stability and assurance
Ischial-Ramal Containment Socket
IC and CAT CAM socket → flexible inner brim with in solid outer frame
anterior wall = scarpas bulge is significantly reduced due to forces being applied medially and laterally
Hybrid Socket
Mix of both quadrilateral socket and ischial ramal containment socket
MAS Marlo anatomical socket
MAS design focuses on skeletal support with ischium and ramus contained within socket without impeding glute max.
Posterior trim line below gluteal fold
Increase ROM with hip ER is unrestricted.
Brimless (elevated vacuum sockets)
brimless or sub ischial socket. 2-4 inches below ischial trim lines
Roll on liner contains the add muscles
Paired with vacuum assisted suspensions
+ increase ROM and comfort
for higher level, longer RL, strong hip muscles
Many sockets designed/used these days are a combination of two types
Side by side comparisons of ischial containment design VS quadrilateral design
Ischium location
Shape
Indication
Which ones increase and decrease scarpas bulge? Which one has narrow medial and lateral dimensions and which one has narrow anterior and posterior dimensions?
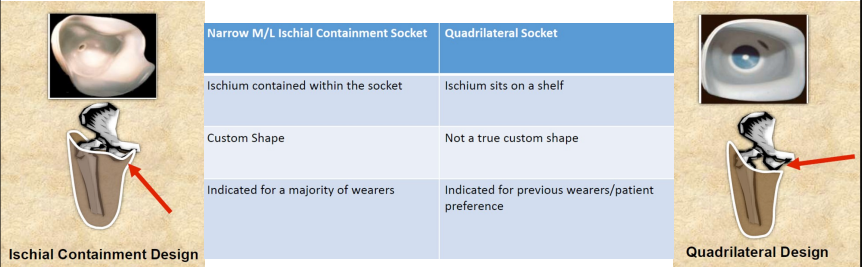
QS increases scarpas bulge
ICS has medial and lateral narrowed
QS as anterior posterior narrowed
TFA suspension systems
It is?
Bands?
Suspension is?
Traditional suction?
3-S silicone suction suspension is composed of what three things?
One of the three things is a big difference between transfemoral and transtibial, which one?. Used for _____ level trans_____ amputees
The vacuum is? Higher or lower levels?
TFA Suspension Systems
Anatomical
Bands: Silesian Band, Pelvic Band with external hip joint
Total Elastic Suspension
Traditional Suction: Pull in, Wet fit
3-S Silicone Suction Suspension
Pin Locking (Pin on distal end of liner)
Lanyard System (lower level transfemoral amputees. Big difference between transfemoral and transtibial is this system)
Seal-in Liner (suction/vacuum system)
Elevated Vacuum → higher levels

Prosthetic knees
Manual locking knee (single axis)
Knee of ____ ____. PAPA ROACH. How does it unlock and lock? What gait pattern will the pt adapt to?
For what K levels? ← KNOW THIS
Negatives?
Locks in what motions? Unlocks (manually) in what motion?
Weight activated stance control (single axis)
Temp depends on?
Swing control: swing control by what? Can add what motion assistance?
Stance control: (Low, moderate, or high) mechanical?
How does it work?
Polycentric Knees (Multi axis)
Usually the ____ prosthesis but is kept for?
Multi axis: What is it? No what?
Swing control: Assists what motion? Can have what add ons?
Stance control: (Low, moderate, or high) alignment?
How does it work?
Indications? K levels?
Negatives?
Fluid controlled knee (hydraulic)
Regulation of what phase by fluid filled cylinder.
Swing control is mechanical or muscular with resistance to what two motions?
Stance control is mechanical or muscular?
How does it work?
Indications? K levels?
What are the other two?
Types:
Manual lock single axis
knee of last resort. (Pt must go unlock it to sit, locks when they stand up. Circumduction gait)
weak and limited ambulator, K1 - K2
(-) abnormal gait, decreased cosmesis, cable failure, no ability to control knee
locks in ext, unlocks in flexion manually.
Weight-activated/stance control single axis
Temp depends on air chamber pressure
swing control; swing control by friction, can add ext assistance
stance control: mod mechanical
Works by mechanical friction brake activated in weight bearing 20 degrees ext. Brake sensitivity adjustable
Needs full unweighting for it to bend
Polycentric multi axis
Usually 1st prosthesis but is kept for back up
Multi axis: 4+ bar linkages (no hydraulics)
Swing control: ext assist or hydraulic add ons
Stance control: mod alignment
Works with 4 bar knee: knee bends → center of rotation moves and displaced posterior, increasing extension and increase stability. Axis shifts proximally to increase toe clearance
Indicated for needing increased stability due to short RL or weak hip ext. K1 - K2.
(-) heavy, costly, decrease cadence.
Gas/fluid control single axis
regulation of swing phase by fluid filled cylinder
swing control: mechanical with fix resistance and ext resistance
stance control: mechanical muscular
Works by valves opening and closing to adjust resistance
Indicated for active ambulators with variable cadence. K3 or higher (He said K2-K3) (sports participant)
Micro-processor
Constant friction

Manual locking knee (Repeat)
Indications? (4)
Disadvantages? (3)
Indications:
Knee of last resort
Weak patient, limited ambulator
No ability to control knee
K level 1–2
Disadvantages:
Abnormal gait
Poor cosmesis
Cable failure


Fluid controlled knee (hydraulic) (Repeat)
Joint axis?
Swing control?
Stance control?
Indications? (3)
Joint Axis: single
Swing Control: mechanical with flexion resistance and extension resistance
Stance Control: mechanical, muscular
Indications:
Active ambulator with variable cadence
Sports participation
K level 3 or higher

Gait deviations: what’s the cause
Patient causes? (8)
Prosthetic causes? (4)
Unilateral amputees usually have a midline shift towards what and increased what support? Why?
Shear occurs at what location and during what part of the gait cycle?
Decreased prosthetic stance time can be the result of what three things?
Patient causes
Strength issues
ROM restrictions
Volume fluctuations
Pain
Functional level
Habit/training
Balance
Confidence level
Prosthetic causes
Prosthetic fit
Pain in RL
Componentry (broken/loose)
Alignment issues
Unilateral amputees usually have a midline shift towards SL and increase DL support (due to fear of being on RL)
Shear occurs at the stump/socket and between ground and the foot at IC
decrease prosthetic stance time can be the result of pain, instability, or decreased prosthetic trust.
Prosthetic gait assessment
What do you do first?
90 to 95% of issues can be fixed by?
Too much ply can cause?
Too little ply can cause?
complete proper fitting first
90 - 95% issues can be fixed by putting sock ply
too much ply = pelvic asymmetry
too little ply = increase foot spins
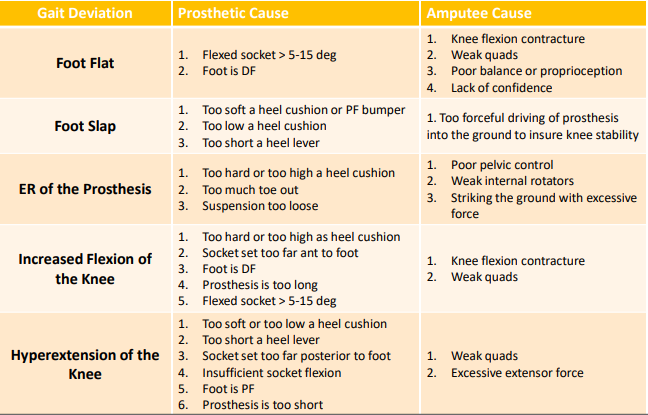
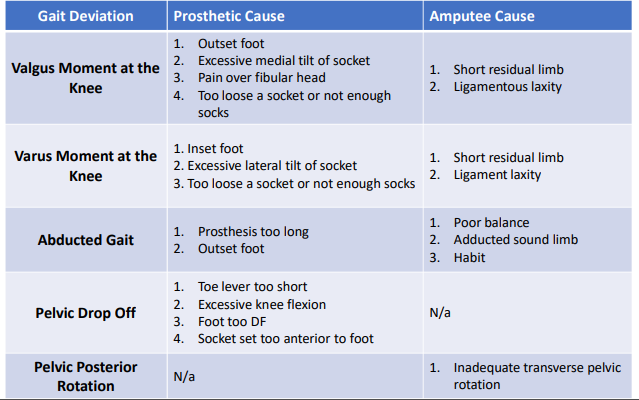
Amputee gait deviations: TTA weight acceptance (IC to LR) (Focus on highlights)
For the following, state the prosthetic cause and the amputee cause
Foot flat
Foot slap
ER of the prosthesis
Increased flexion of knee
Hyperextension of the knee
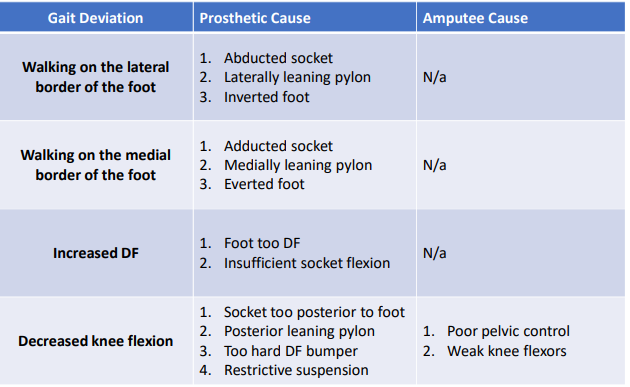
Amputee gait deviations: TTA single limb support (Mid-stance to TS) (No highlights)
For the following, state the prosthetic cause and the amputee cause
Walking on the lateral border of the foot
Walking on the medial border of the foot
Increased DF
Decreased Knee Flexion
Amputee gait deviations: TTA single limb support (Mid-stance to TS) (Focus on highlights)
For the following, state the prosthetic cause and the amputee cause
Valgus moment at the knee
Varus moment at the knee
Abducted gait
Pelvic drop off
Pelvic posterior rotation
Amputee gait deviations: TTA swing phase (Pre-swing to Terminal swing) (Focus on highlights)
For the following, state the prosthetic cause and the amputee cause
Pelvic rise
Decreased stride length on prosthetic side
Increased stride length on prosthetic side
Decreased toe clearance
Increased toe clearance
Lateral whip (heel goes out, TFA, TTA)
Medial whip (heel goes in, TFA, TTA)
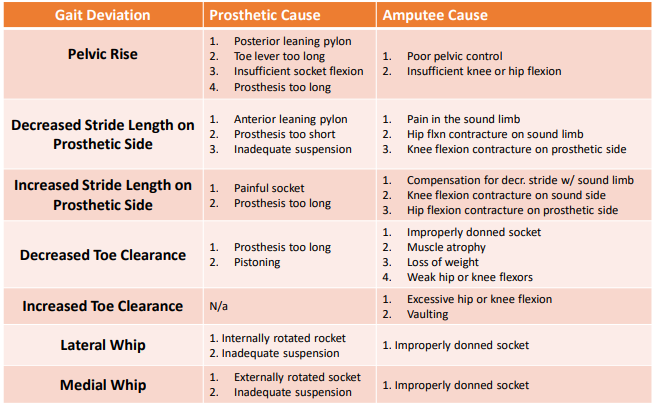
Amputee gait deviations: TTA sound limb and arm swing (Focus on highlights)
For the following, state the prosthetic cause and the amputee cause
Adducted limb
Vaulting
Uneven arm swing
Extended rotation
Increased stance time
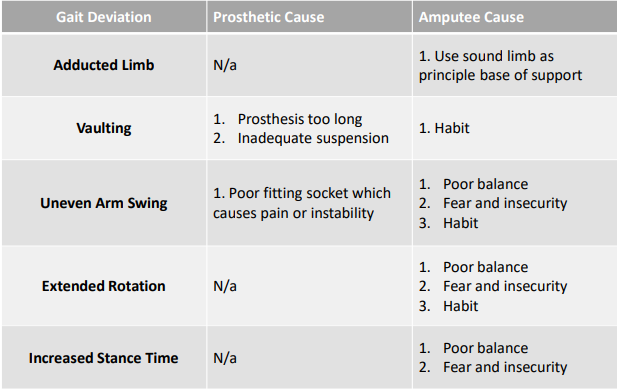
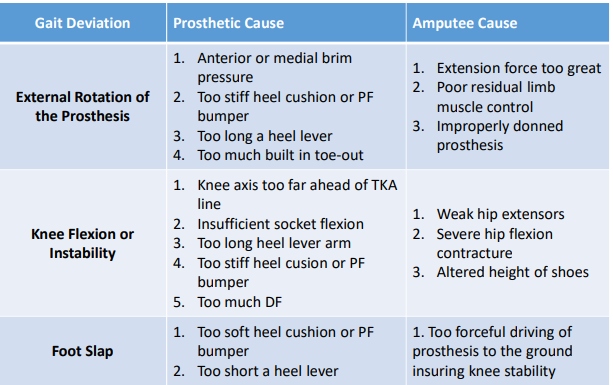
Amputee gait deviations: TFA weight acceptance phase (IC to IR) (No highlights)
For the following, state the prosthetic cause and the amputee cause
External rotation of prosthesis
Knee flexion or instability
Foot slap
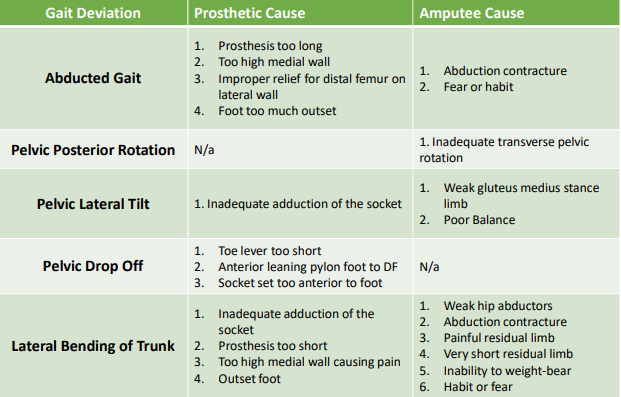
Amputee gait deviations: TFA single limb support (Mid stance to terminal stance) (Focus on highlights)
For the following, state the prosthetic cause and the amputee cause
Abducted gait
Pelvic posterior rotation
Pelvic lateral tilt
Pelvic drop off
Lateral bending of trunk
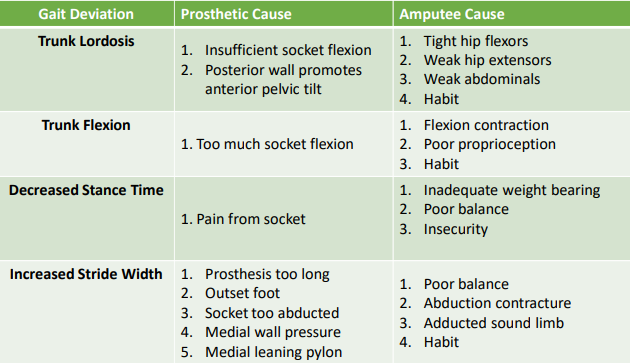
Amputee gait deviations: TFA single limb support (Mid stance to terminal stance) (Focus on highlights)
For the following, state the prosthetic cause and the amputee cause
Trunk lordosis
Trunk flexion
Decreased stance time
Increased stride width
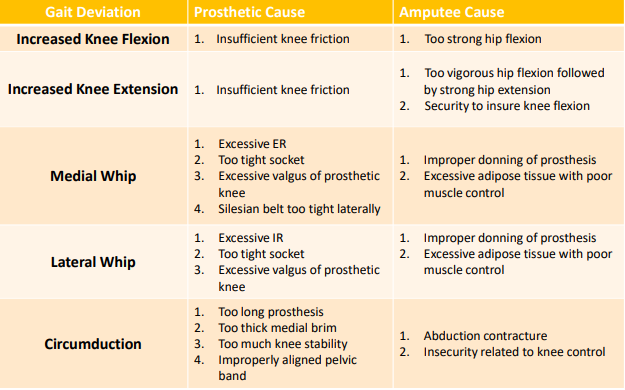
Amputee gait deviations: TFA (pre swing to terminal swing) (Focus on highlights)
For the following, state the prosthetic cause and the amputee cause
Increased knee flexion
Increased knee extension
Medial whip
Lateral whip
Circumduction TFA
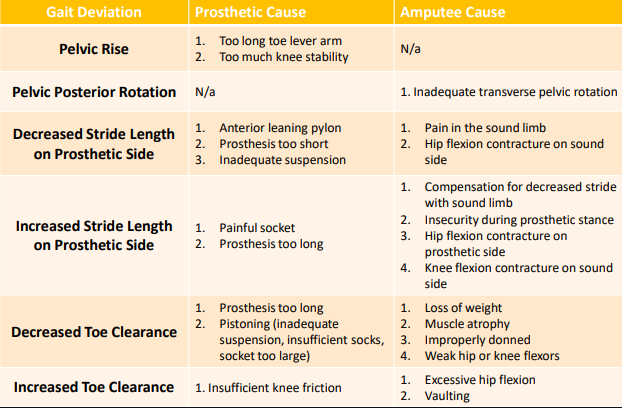
Amputee gait deviations: TFA (pre swing to terminal swing) (No highlights)
For the following, state the prosthetic cause and the amputee cause
Pelvic rise
Pelvic posterior rotation
Decreased stride length on prosthetic side
Increase stride length on prosthetic side
Decreased toe clearance
Increased toe clearance
Amputee running
Basic components of running? (Stride length, Stride frequency, Speed)
Five steps for learning basic running?
What can be seen with arm swing and trunk rotation in amputees, especially on the prosthetic side? Why?
Basic Component of Running
Stride Length = Distance covered with each stride
Stride Frequency = The number of strides taken within a given time
Speed = Stride Length X Stride Frequency
Five Steps for Learning Basic Running
Prosthetic Trust - reach out with prosthesis
Backward Extension - pull back with prosthesis
Sound Limb Stride - pull down and back with prosthesis, reach out with SL
Stride Symmetry - Relax and take equal strides
Arm Carriage - high hands and elbows
Arm swing and trunk rotation are decreased or absent in amputees especially on prosthetic side (for bracing)
Give away questions: Guaranteed on the test
1.A 78-year-old veteran with diabetes who sustained a transfemoral amputation in the Vietnam war presents for initial evaluation with difficulty walking. He is very short of breath and must stop to rest about every 200 feet. He feels that his current prosthesis is suddenly too heavy and too long and reported a low score in a satisfaction survey with the device. On initial examination you note he has 3 plus pitting edema on his sound foot. Management should initially begin with what?
A.A referral to the prosthetic service for a newer lighter and shorter prosthesis
B.Telling him he is just getting older and need to adjust to his changing body
C.A request for an electric scooter so that he doesn’t need to walk anymore
D.An evaluation and referral to his primary physician for the edematous foot
2. A dynamic response foot is typically made with a carbon fiber that can store and release energy at different points within the gait cycle. The J shape of a carbon foot would mimic which of the following gait functions?
A.A toe clearance during swing
B.A toe rocker during late stance
C.Multi-axial motion during stance phase
D.An ankle rocker at mid stance
D.An evaluation and referral to his primary physician for the edematous foot (Like 99% sure its this lol)
D.An ankle rocker at mid stance (Like 99% sure its this lol)
In class booklet questions
Which of the following is best described to be a K1 level prosthetic that requires the patient to manually unlock the knee to sit?
A. Microprocessor knee
B. Pneumatic knee
C. Manual locking knee
D. Hydraulic knee
Which of the following is an incorrect statement regarding prosthetic sockets?
A. The socket must hold the residual limb firmly to avoid pistoning
B. The Socket must provide the exact same pressure on all the areas of the RL
C. The socket must hold the RL comfortably to avoid irritation
D. The socket must be designed to support weight to allow for function of the limb
What is the term used when the wound site failed to develop sufficient strength to withstand forces placed upon it and the amputation site opens up?
A. Ulceration
B. Dehiscence
C. Revision
D. Verrucous Hyperplasia
Ideally, a prosthetic knee joint should provide
A. Stability in stance and swing phase control
B. Stability in stance but with free swing
C. Swing phase in control but with free stance
D. Locking stability in stance and in swing
Which part of the prosthetic foot plays the role of plantar flexors during eccentric control of DF from mid stance to terminal stance?
A. The axis
B. The heel
C. The keel
D. The sole
Socket for transfemoral amputees are typically aligned
A. In slight extension
B. In external rotation
C. In slight flexion
D. At neutral flexion/extension
Which statement about the upper extremity amputees is false?
A. High levels of these amputations occur in the younger population of patients
B. 50% of these amputees do not wear a prosthetic
C. 95% of these amputations are associated with below the elbow status
D. The majority of these amputations are due to congenital abnormalities or cancer
Clinically, the shortest a transtibial amputated RL can be and still allow for function in a typical fashion is
A. Immediately distal tot he tibial tuberosity
B. Immediately distal to the femoral condyles
C. 3 cm proximal to the tibial crest
D. 13 cm distal to the joint line
Which of the following amputations require the highest energy expenditure when using the appropriate prosthesis
A. Unilateral TF
B. Syme’s amputation
C. Unilateral TT
D. Chopart’s amputation
Swing phase gait deviations are commonly used as a method to
A. prevent the prosthetic toe from stubbing the ground
B. Compensate for poor alignment
C. Offset a painful limb or socket impingement
D. Maintain dynamic balance
What are the components of a prosthetic device for a patient with a Symes amputation?
A. Quadrilateral socket, knee, pylon, and foot
B. No prosthesis is needed, as this transmetatarsal amputation
C. PTB socket, pylon, and foot
D,. Socket and a foot with suspension built into the socket
Prosthetic feet that incorporate an energy storage and return mechanism are known as:
A. Single axis feet
B. Energy feet
C. Dynamic response feet
D. SACH feet
What is the stage of adjustment that allows relinquishment of false hopes and successful adaption of new roles based on realistic limitation and new potential?
A. Denial
B. Anger
C. Shock
D. Acceptance
The ischial containment socket for the transfemoral amputee:
A. Contains less of the residual limb than a quadrilateral socket
B. Provides better medio-lateral stability than a quadrilateral socket
C. Is rarely prescribed today, as a quad socket is preferred
D. Concentrates all weight bearing forces on the ischium
The most effective suspension is the one that provides:
A. Variable pistoning to adapt to different functional activities
B. Pistoning no greater than 1 inch
C. Pistoning no greater than ½ inch
D. No pistoning
C
B
B
A
C
C
D
A
A
A
D (i think)
C
D
B
D
Class A VS class B questions
Question 1:
Which of the following designs can BEST improve sitting comfort for your patient with TF amputation:
Hard plastic quad socket
Use of a plug fit type suspension
Hard carbon fiber containment socket with the patient adding sock ply
Flexible inner socket inside a supportive carbon fiber frame with posterior cutouts.
Question 2:
Successful fitting of the prosthesis is more likely to occur if?
The patient waits for the prosthesis long enough to get properly trained
The sound limb is in good status, and the results of the amputation are positive
The time the patient waits for the prosthesis is minimized
Both B & C are correct
Question 3:
The leading cause of amputation in the US is mostly associated with?
Trauma
Dysvascular/PVD/DM
Infection
Osteosarcoma
Question 4:
Your patient who is living with a TF amputation is walking by swinging the prosthesis in a wide outward arc. The MOST likely cause for this deviation is:
Patient insecurity.
A containment socket that properly encapsulates the ramus.
An exoskeletal prosthesis that is too short.
A socket that uses a lanyard suspension and fits well.
Question 5:
The IC socket for the transfemoral amputee?
Contains less of the RL that a quad socket
Provides better mediolateral stability than a quad socket
Concentrates all weight-bearing forces on the ischium
Is rarely prescribed today, as a quad socket is preferred
Question 6:
Prosthetic feet that incorporate an energy storage and return mechanism are known as?
SACH feet
Dynamic Response Feet
Single Axis feet
Energy feet
Question 7:
Swing phase gait deviations are commonly used as a method to:
Offset a painful limb or socket impingement
Compensate for poor alignment
Prevent the prosthetic toe from stubbing the ground
Maintain dynamic balance
Question 8:
Which of the following is a CORRECT statement regarding gel liners?
The liner should be a pulled on a sock to avoid air pockets
A liner does not contribute to suspending the prosthesis
One of the functions of a liner is to cushion the residual limb
Liners are not suitable for patients with sensitive skin
Question 9:
Which of the following statements regarding post-operative residual limb care is TRUE?
a) Control of residual limb edema results in decreased pain and enhances wound healing.
b) Knee and hip joints should be maintained in a flexed position when resting in bed.
c) Casts or rigid dressing are never used to protect the residual limb.
d) Activity and physical therapy should not be started until the wound is completely healed.
Question 10:
Ideally, a prosthetic knee joint should provide?
Stability in stance, and swing phase control
Stability in stance phase, but with free swing
Swing phase control, but with free stance
Locking stability in stance and in swing
Question 11:
Which of the following is an INCORRECT statement regarding prosthetic sockets?
The socket must be designed to support weight to allow for function of the limb
The socket must hold the RL comfortably to avoid irritation
The socket must provide exactly the same pressure on all areas of the RL
The socket must hold the RL firmly to avoid pistoning
Question 12:
What are the components of a prosthetic device for a patient with a Symes amputee?
The socket, and a foot with a suspension built into the socket with a medial window
PTB socket, pylon, and foot
No prosthesis is needed, as this a transmetatarsal amputation
Quad socket, knee, pylon, and foot
Question 13:
Which of the following area are RELIEF areas in the patellar tendon bearing (PTB) socket?
Head and shaft of the Fibula
Head of the Fibula and posterior soft tissue
Tibia Crest and Head of the Fibula
Patellar Tendon and Tibial Flares
Question 14:
The prosthetist might build a relief into a transtibial socket to accommodate pressure sensitive areas on the limb which could include:
The anterior tibialis muscle
The patellar tendon
The fibular head
The medial tibial condyle
Question 15:
You are observing the gait of a patient with a transtibial amputation. The patient demonstrates uneven step length. What is the most likely cause of this deviation?
The patient is fearful of bearing weight onto the prosthesis
The prosthetic knee axis is too medial
The patient’s hip flexors are weak
The socket is too adducted
Question 16:
Which part of the prosthetic foot plays the role of the plantarflexors during eccentric control of DF from midstance to terminal stance?
The heel
The keel
The axis
The sole
Question 17:
In a body-powered UE prosthesis for a transhumeral amputee, how does that patient typically control the terminal device?
Using implanted electrodes
Using scapular and humeral motions
Using trunk and cervical motions
The terminal device is not functional in a body-powered prosthesis
Question 18:
Which of the following statement is TRUE regarding bilateral amputations?
Bilateral amputations have the same prognosis as unilateral amputations
Bilateral amputations are extremely rare unless caused by trauma
Stubbies are energy-efficient choice for the initial gait in bilateral amputees
UE strengthening and trunk control are less important in the bilateral amputee
Question 19:
Which of these patients would be the WORST candidate for a prosthesis after lower extremity amputation?
The patient has diabetes and the residual limb is poorly shaped
The patient is elderly and has poor standing balance
The patient is unable to master gait training with crutches indep
The patient was wheelchair-bound for 2 years to amputation
Question 20: Final Question
Which statement about UE amputees is false?
The majority of these amputations are due to congenital abnormalities or cancer
95% of these amputations are associated with below the elbow status
50% of these amputees do not wear a prosthetic
High levels of these amputations occur in the younger age population of these patients
Flexible inner socket inside a supportive carbon fiber frame with posterior cutouts.
Both B & C are correct
Dysvascular/PVD/DM
Patient insecurity.
Provides better mediolateral stability than a quad socket
Dynamic Response Feet
Prevent the prosthetic toe from stubbing the ground
One of the functions of a liner is to cushion the residual limb
Control of residual limb edema results in decreased pain and enhances wound healing.
Stability in stance, and swing phase control
The socket must provide exactly the same pressure on all areas of the RL
The socket, and a foot with a suspension built into the socket with a medial window
Tibia Crest and Head of the Fibula
The fibular head
The patient is fearful of bearing weight onto the prosthesis
The keel
Using scapular and humeral motions
Stubbies are energy-efficient choice for the initial gait in bilateral amputees
The patient was wheelchair-bound for 2 years to amputation
The majority of these amputations are due to congenital abnormalities or cancer