Oral Mucosal Diseases- White and Red Conditions
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
why is oral mucosa pink?
-epithelium = non-vascular = white
-underlying CT = vascular = red
-white + red = pink
-areas of thicker epithelium = lighter pink/more white
-areas of thinner epithelium = darker pink/less white
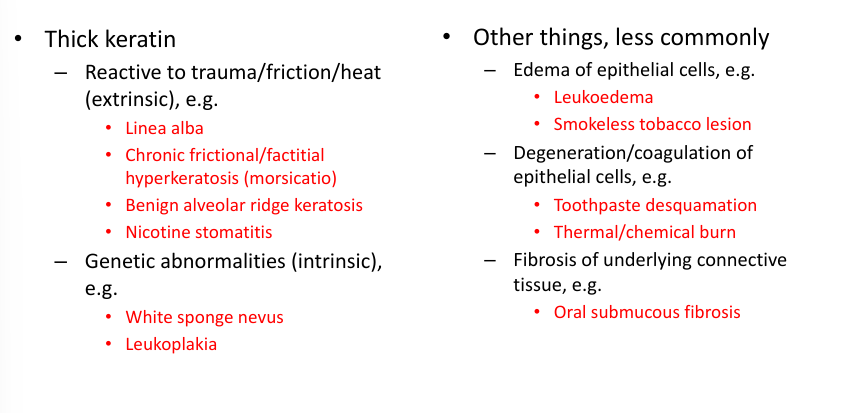
what makes lesions white?
-excess epithelium (hyperplasia, neoplasia, edema) and/or excess keratin (hyperkeratosis)
-thick keratin: reactive to trauma/friction/heat (“extrinsic etiology”), genetic abnormalities (“intrinsic etiology”)
-other things, less commonly: edema within epithelial cells, degeneration/coagulation of epithelial cells, fibrosis of underlying CT
keratin
-family of intermediate filament proteins present in epithelial cells (keratinocytes)
-cell level: key component of cytoskeleton
-organ level: barrier function
-54 functional keratin proteins
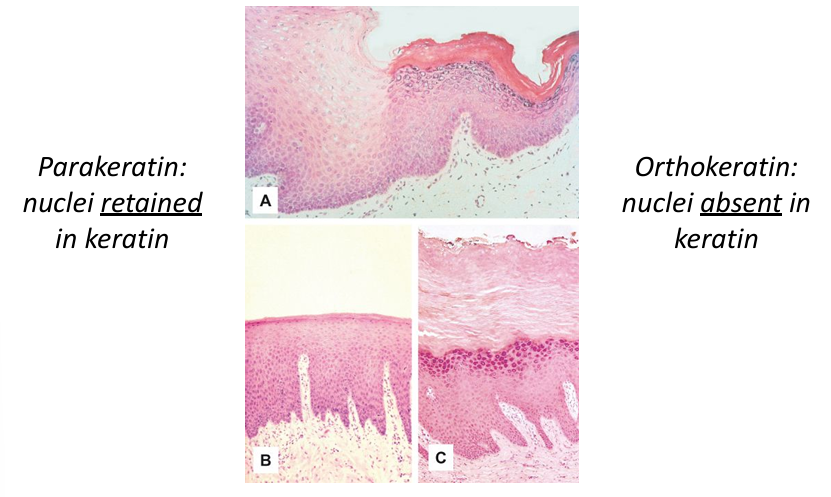
-orthokeratin and parakeratin: describes microscopic appearance of keratin
-dyskeratosis: abnormal intracellular keratinization
white v. yellow
-close but not the same
-ulcers are covered by a fibrin membrane and are tan/yellow- not white
what makes a lesion red?
-thinning of epithelium (atrophy)
-increased vascularity in lamina propria: during inflammation- vessels dilate to recruit more inflammatory cells, during tissue repair- angiogenesis (formation of new vessels) to form granulation tissue before maturation and organization of fibrous tissue
lesions that are both white and red
-acanthosis/hyperkeratosis (=white) + mucosal inflammation/granulation tissue formation (=red)
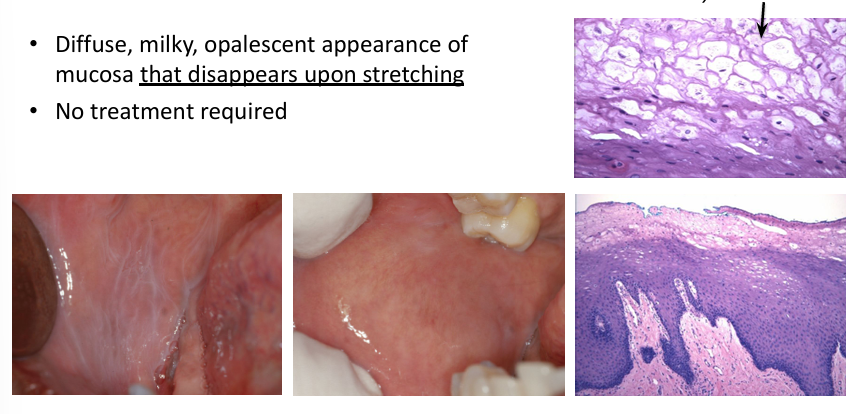
leukoedema
-diffuse, milky, opalescent appearance of mucosa that disappears upon stretching
-no treatment required
-diffuse, milky grayish-white surface with folds, wrinkles, or streaks
-does not rub off but disappears when stretched
-bilateral buccal mucosa: may extend onto lips, floor of mouth, palatopharyngeal tissue
leukoedema demographics
-any age, any sex
-may be more common in darker complexion
-more common and more severe in smokers, becomes less pronounced with cessation of smoking
-diagnosis made clinically: disappears when cheek is stretched
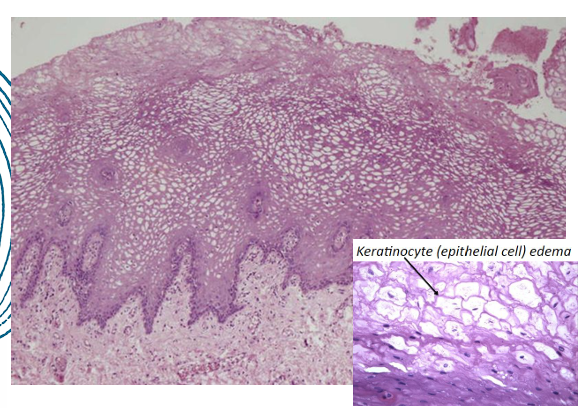
leukoedema histology
-acanthosis (thickened epithelium)
-parakeratosis (thickened parakeratin specifically)
-intracellular edema in the spinous layer
leukoedema diagnosis, treatment, significance
-diagnosis made clinically: disappears when cheek is stretched
-treatment: not required
-significance: important to distinguish from other white lesions, should be stretched to rule out any underlying lesions hiding under leukoedema
white sponge nevus
-diffuse thick corrugated or velvety white plaques
-bilateral buccal mucosa: sometimes also ventral tongue, labial mucosa, soft palate, alveolar mucosa, floor of mouth, rarely also extraoral (nasal, esophageal, laryngeal, anogenital mucosa)
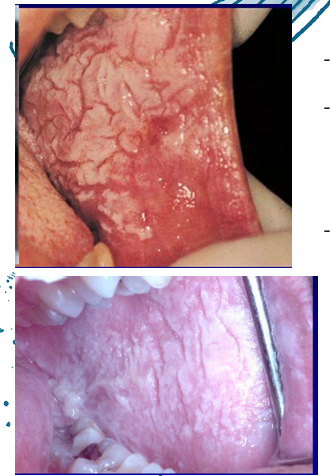
white sponge nevus histology
-acanthosis (thickened epithelium)
-parakeratosis (thickened parakeratin)
-intracellular edema in spinous layer
-perinuclear eosinophilic condensation in superficial cells (tonofilaments of mutated keratins)
white sponge nevus demographics
-autosomal dominant genetic disorder (genodermatosis) with high penetrance and variable expressivity
-defect in normal keratinization (keratins 4 and 13)
-age: usually birth/early childhood, may develop in adolescence
-no sex predilection
white sponge nevus diagnosis, treatment, prognosis
-dx: biopsy or cytology
-tx: not required
-prognosis: excellent
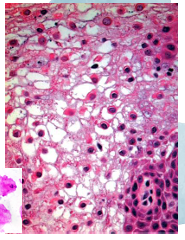
hereditary benign intraepithelial dyskeratosis
-diffuse thick corrugated or velvety white plaques of buccal and labial mucosa
-oral lesions can resemble white sponge nevus or leukoedema
-sometimes also floor of mouth, lateral tongue
-can have superimposed candidal infection (thrush)
-+thick opaque gelatinous plaques of conjunctivae adjacent to cornea- most prominent in spring, regress in summer/fall, when active → tearing, photophobia, itching of eyes, may leads to blindness
HBID demographics
-develops during childhood
-no sex predilection
-autosomal dominant genodermatosis
-primarily affects descendants of a triracial isolate (Native American, black, white) of people who originally lived in North Carolina
HBID histology
-acanthosis
-hyperparakeratosis
-dyskeratosis (dysregulated keratin production) in superficial epithelial cells
-dyskeratosis makes cells look like they are engulfed by adjacent cells → cell-within-a-cell appearance
HBID diagnosis and treatment
-dx: biopsy
-tx: not required, antifungal for superimposed thrush, refer to ophthalmologist for eye lesions- may require surgical excision but often recur
frictional keratosis
-chronic mechanical irritation that produces a white lesion with a roughened keratotic surface (similar to callous on the skin)
-no malignant transformation potential: linea alba, morsicatio, chronic irritation from broken and/or missing teeth, alveolar ridge keratosis involving the retromolar pad or crest of an edentulous alveolar ridge (caused by masticatory function or denture trauma)
-tx: smooth out sharp cusps (enameloplasty), biopsy to rule out dysplasia/SCC
linea alba
-white line
-hyperkeratosis of buccal mucosa (usually) along occlusal plane, usually bilateral:
-common consequence of frictional irritation or sucking trauma (from facial surfaces of teeth)
-not caused by dental problems
-may be scalloped
-dentulous areas only
-often more pronounced near posterior teeth
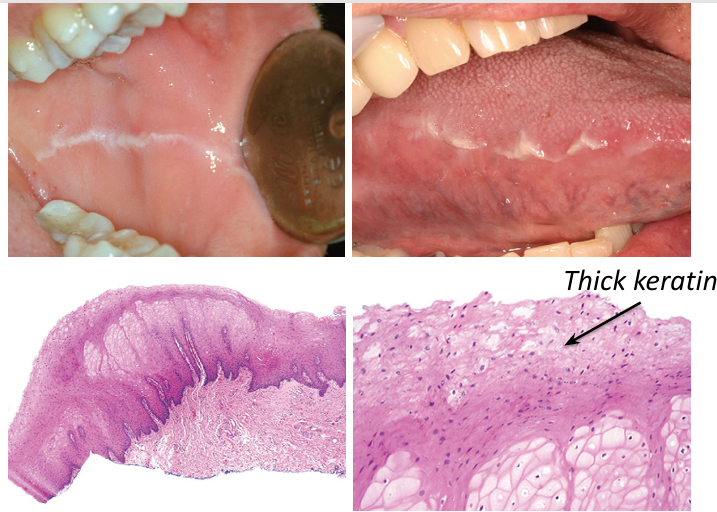
linea alba demographics, tx
-any age, any sex
-no tx necessary
-no malignant transformation potential
-may regress spontaneously
morsicatio (chronic frictional/factitial (bite) keratosis)
-chronic, chewing/nibbling-induced hyperkeratosis
-white papules and plaques with a shaggy irregular surface
-focal erosions or erythema, sometimes ulcerated
-patients may describe being able to remove shreds of white material
-generally poorly demarcated, diffuse borders
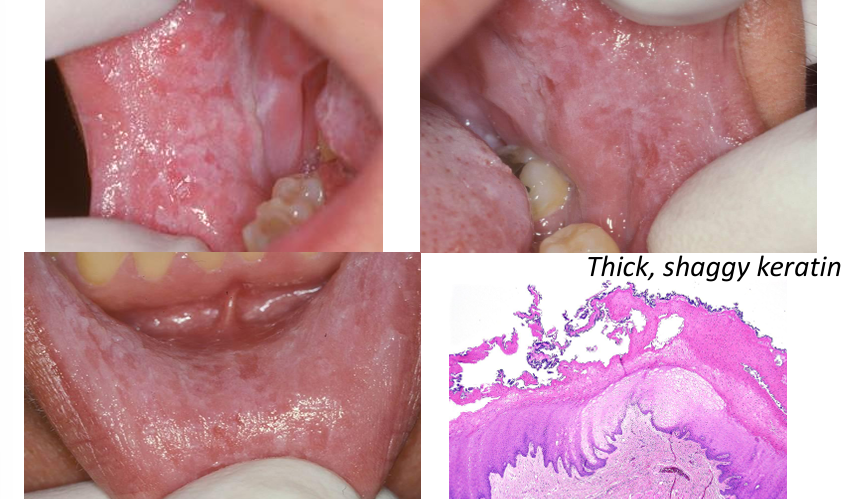
morsicatio demographics, tx
-occurs in 1-2% of population
-3x more common after age 35
-3x more common in females
-patient may or may not be aware of habit (parafunctional activity at night)
-no tx necessary, recommend to eliminate habit
-no malignant transformation potential
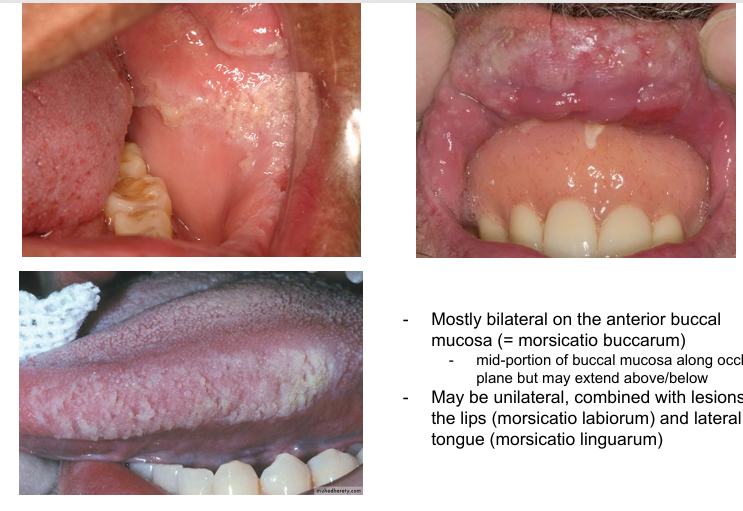
morsicatio location of lesions
-mostly bilateral on the anterior buccal mucosa (=morsicatio buccarum): mid-portion of buccal mucosa along occlusal plane but may extend above/below
-may be unilateral, combined with lesions of the lips (morsicatio labiorum) and lateral tongue (morsicatio linguarum)
morsicatio diagnosis
-diagnosis usually established clinically
-biopsy if not certain
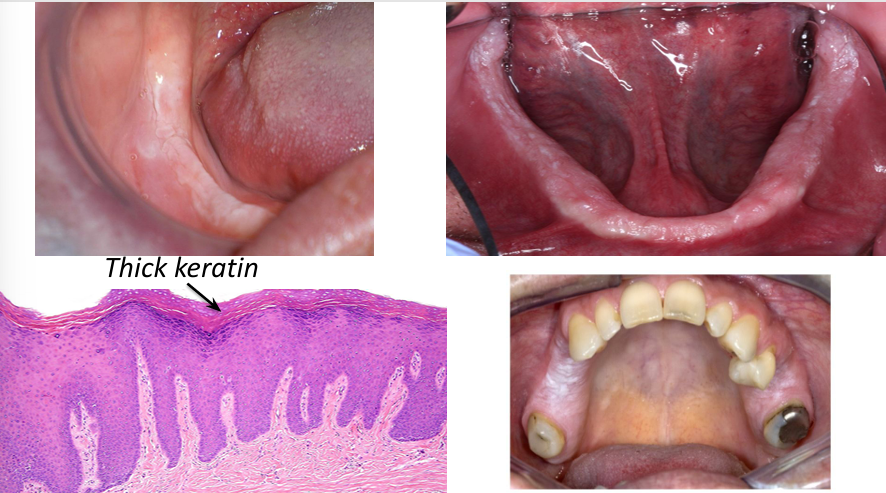
benign alveolar ridge keratosis (BARK)
-chronic, trauma-induced hyperkeratosis
-repetitive trauma of food bolus against: retromolar pad, crest of edentulous alveolar ridge
-generally poorly demarcated, diffuse borders
-no tx necessary once diagnosis established
-biopsy
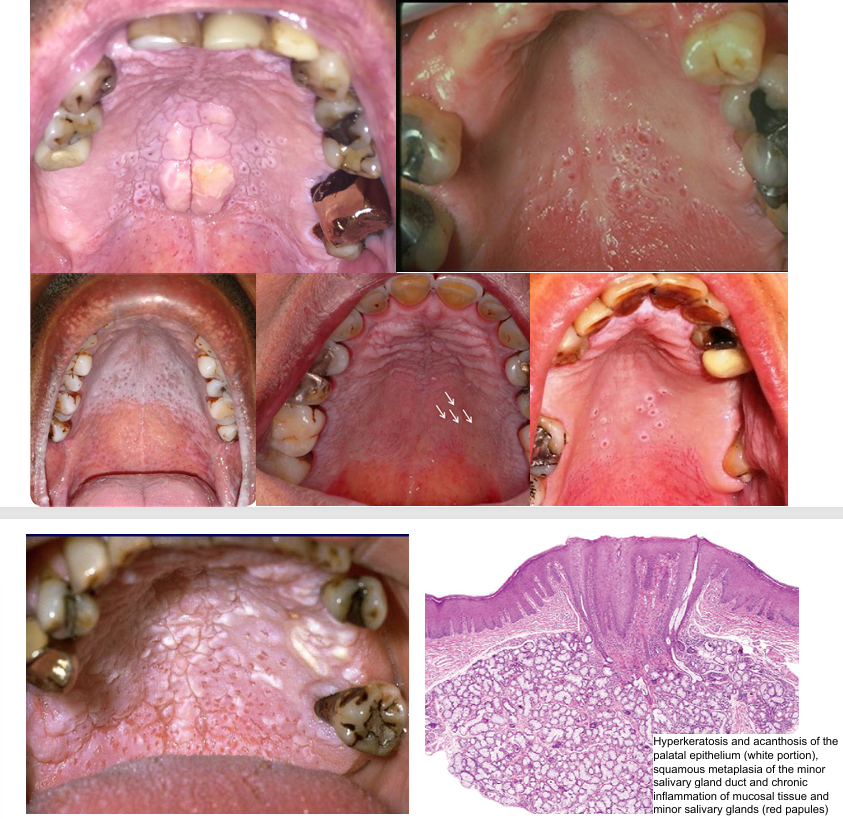
nicotinic stomatitis
-heat-induced hyperkeratosis of palatal mucosa (most often): pipe smokers, cigar smokers
-generalized hyperkeratosis with scattered, red, punctate papules: raised, red areas = inflamed orifices of salivary ducts
-not a premalignant condition, however tobacco users are at increased oral cancer risk in general
-treatment = smoking cessation, palate should return to normal within 1-2 weeks, if lesion persists >1 month upon habit cessation- BIOPSY to rule out dysplasia/SCC
nicotinic stomatitis demographics
-male predilection
-reverse smoking: reverse smoker’s palate
-hand-rolled cigarettes and cigars smoked with the lit end held within the mouth
-South America and Southeast Asia
-precancerous
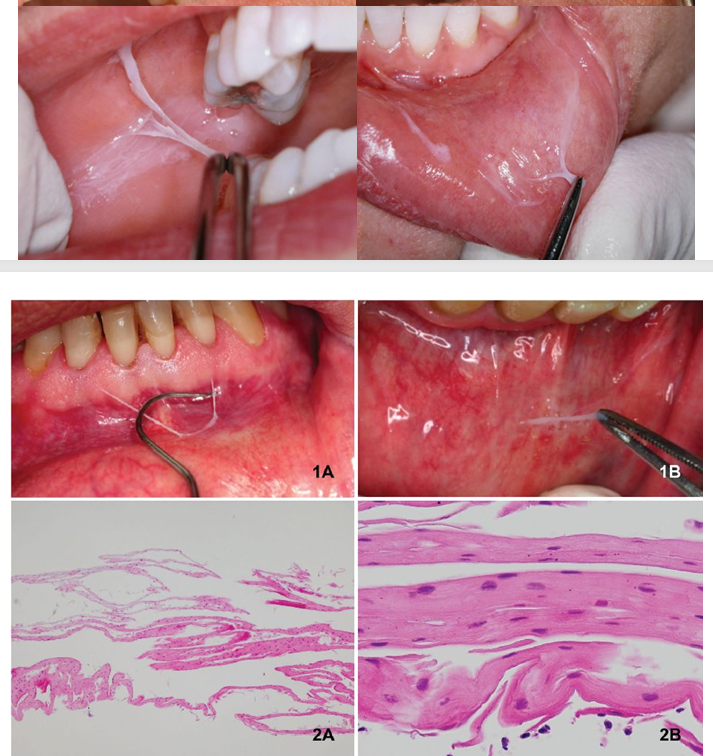
contact desquamation
-thready white fragments on top of (nonkeratinized) mucosa- easily peel off
-contact with irritants that are not strong enough to cause ulceration or necrosis- alcoholic mouth rinses, strong toothpastes
-no tx necessary
-may counsel pt to change products
thermal burn
-acute, heat-induced damage to oral mucosa: tender/sensitive, may be erythematous or covered by white/gray film
-resolves over 2-3 weeks
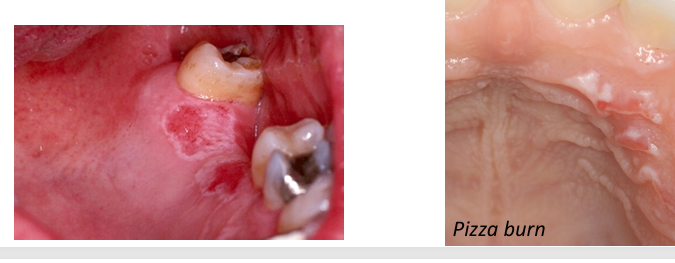
chemical burn (non-specific irritant contact stomatitis)
-white, necrotic plaque: variable erythema, may or may not be ulcerated
-history of exposure to caustic irritant: aspirin, topical anesthetic, hydrogen peroxide, formocresol, whitening strips
-management: removal of irritant, topical steroids as needed

coagulative necrosis
-type of cell death causing denaturation of intracellular proteins
-denatured lysosomal enzymes cannot degrade injured/dying cell
-cell outline of injured/dying cell preserved

plasma cell gingivitis
-allergic rxn to various allergens including components of chewing gum, herbal toothpaste, mint candy, peppers used for cooking, etc.
-rapid onset of sore mouth, intensified by dentrifices and hot/spicy foods
-entire gingiva becomes diffusely enlarged with bright erythema and loss of normal stippling
-edentulous areas exhibit less intense change
-topical placement of allergenic material → localized gingival and vestibular alteration

plasma cell gingivitis diagnosis and treatment
-dx: biopsy- plasma cell infiltrate in lamina propria, r/o neoplasm, find possible allergens- complete dietary history/records of everything taken orally, eliminate potential allergen and see if condition improves, allergy testing
-treatment: topical or systemic immunosuppressive medications if failed to identify the allergen (variable success), in spite of all evaluations and therapeutic interventions, some patients do not respond to treatment and no cause for disease can be identified
contact stomatitis
-hypersensitivity/allergic rxn to artificially flavored cinnamon products- rare to see a rxn to natural cinnamon
contact stomatitis clinical features
-white lesion with erythematous base
-diffuse (toothpaste) or localized (gum/candy)
-common to have pain or burning
-gingiva = most common with toothpaste use, resembles plasma cell gingivitis
-buccal mucosa/lateral tongue = most common with gum/candy use, resembles morsicatio or OHL
-usually diagnosed based on clinical appearance and use of cinnamon products
-biopsy can be used to rule out autoimmune/neoplastic processes

contact stomatitis treatment
-typically resolves within 1 week of stopping cinnamon
-if pt “relapses”, symptoms can return in 24 hours
lichenoid stomatitis
-etiology: hypersensitivity to dental metal undergoing corrosion, most commonly mercury (amalgam), nickel, gold, copper, silver, rare to react to resins (composites)
-clinical features: white/red lichen planus-like lesion near a dental metal restoration, typically asymptomatic, periodic erosions, does not migrate

lichenoid stomatitis diagnosis and treatment
-diagnosis: clinically and histologically very similar to lichen planus- requires correlation with clinical history/findings, biopsy to rule out dysplasia/carcinoma, patch testing- not always helpful
-treatment: start with recontouring the material, replace material with a non-metal
geographic tongue (benign migratory glossitis) etiology
-unknown- no relation to age, allergies, etc.
-common, 1-3% of population
-2:1 female predilection
geographic tongue clinical features
-well demarcated red areas surrounded by a slightly elevated yellow-white serpentine/scalloped border
-red zone = atrophic filiform papillae
-anterior 2/3 of tongue, tip and lateral borders, can happen ectopically too (buccal/labial mucosa, soft palate)
-multiple or solitary lesion(s)
-usually asymptomatic, but some patients experience burning sensation
-biopsy not indicated
-begins as small white patch, develops central erythematous atrophic zone, enlarges centrifugally

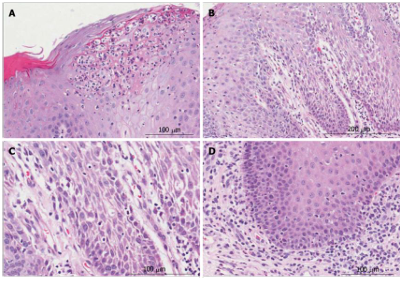
geographic tongue histology
-acanthosis, parakeratosis, inflammation in lamina propria
-neutrophils in spinous layer of epithelium = MUNRO abscess
-neutrophils are responsible for destruction of superficial portion of epithelium → atrophic, reddened mucosa
geographic tongue treatment
-none required
-appears quickly, heals within days or weeks, then develops elsewhere
-topical corticosteroids if burning sensation
-NO malignant transformation potential
hairy tongue
-keratin accumulation on dorsal tongue (filiform papillae)- either increased keratin production or decrease in normal desquamation of keratin → hair-like appearance
-may produce gagging sensation or bad taste
-coated tongue- same but no hair-like projections- may also cause oral malodor
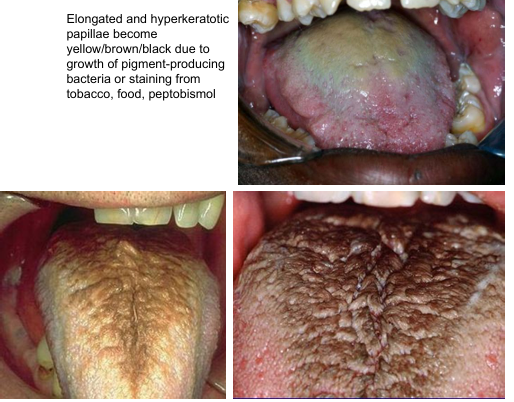
hairy tongue diagnosis and treatment
-biopsy not required
-no malignant transformation potential
-eliminate predisposing factors
-encourage oral hygiene
-gentle scraping/brushing, hydration
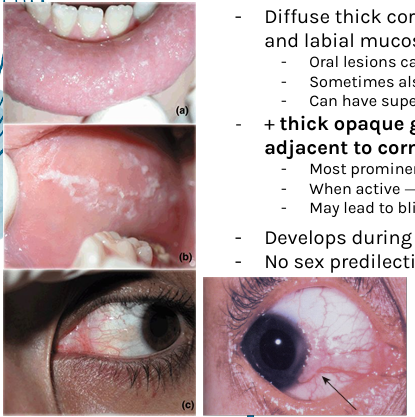
OHL
-EBV-induced white plaque on the lateral tongue in immunosuppressed individuals- not exclusive to HIV+
-faint white vertical streaks, do not rub off
-thickened, furrowed, shaggy keratin
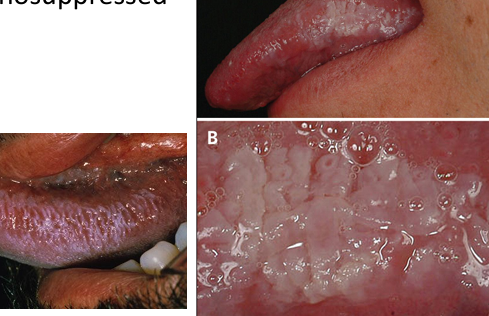
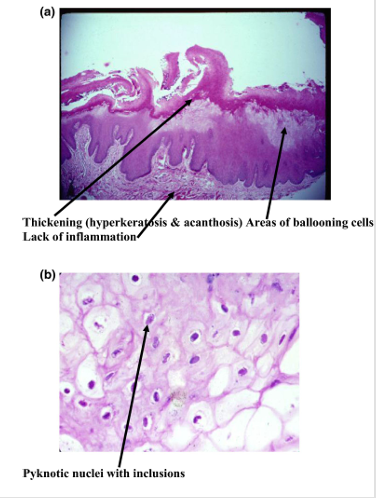
OHL histology
-hyperkeratosis with surface corrugations
-”balloon cells”- EBV infected epithelial cells in the upper spinous layer
-abundant clear cytoplasm + nuclear clearing and peripheral margination of chromatin (nuclear beading) due to extensive EBV replication that displaces chromatin to nuclear margin
OHL diagnosis and treatment
-dx: medical history, clinical presentation, biopsy + in-situ hybridization for EBV
-tx: not required, no malignant transformation
-can serve as indicator of level of immune suppression
oral candidiasis- 3 types
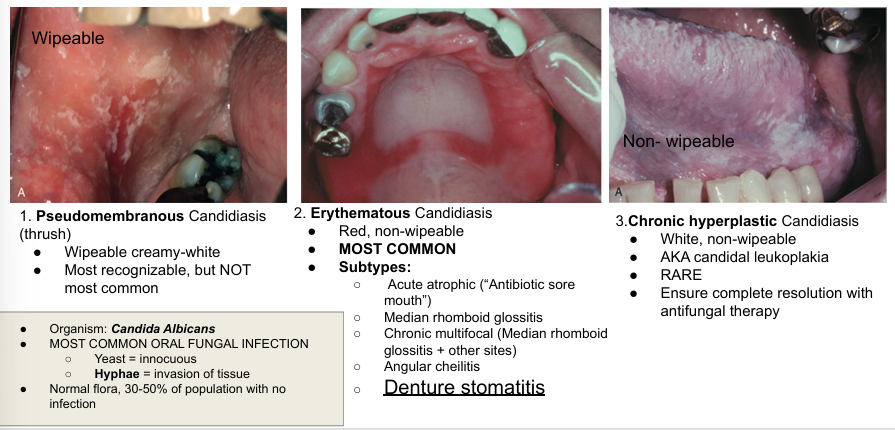
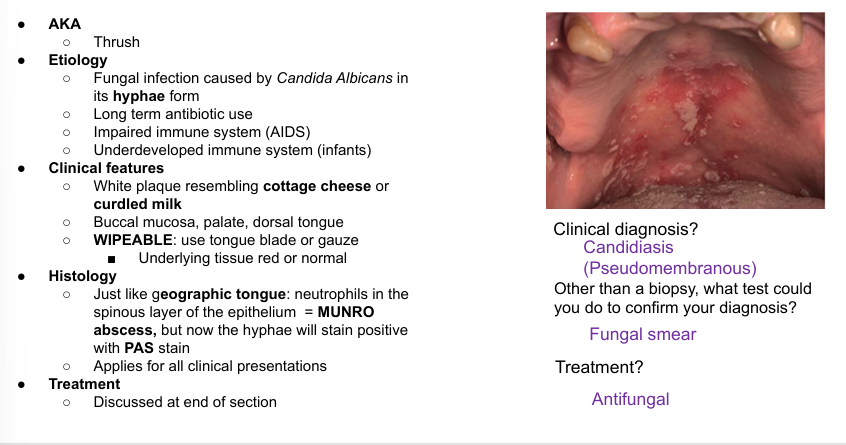
pseudomembranous candidiasis
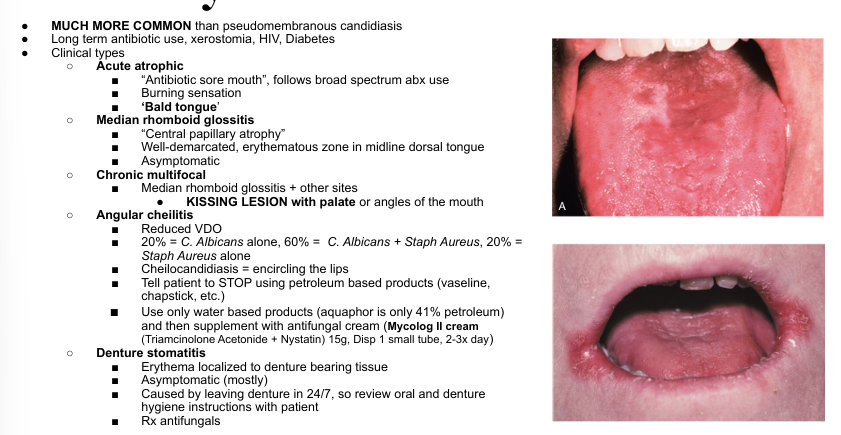
erythematous candidiasis
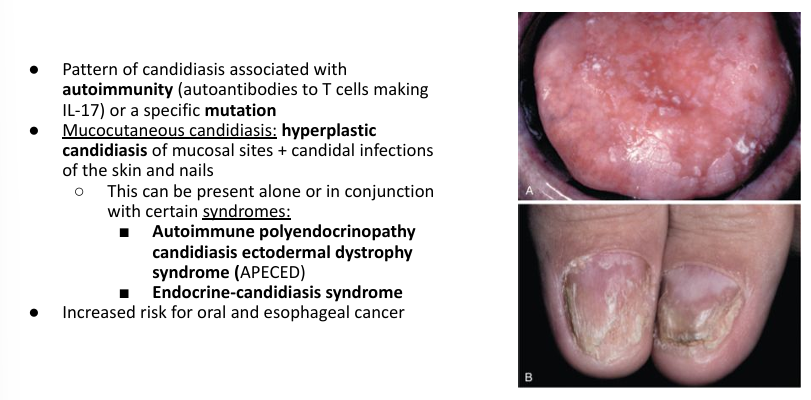
mucocutaneous candidiasis
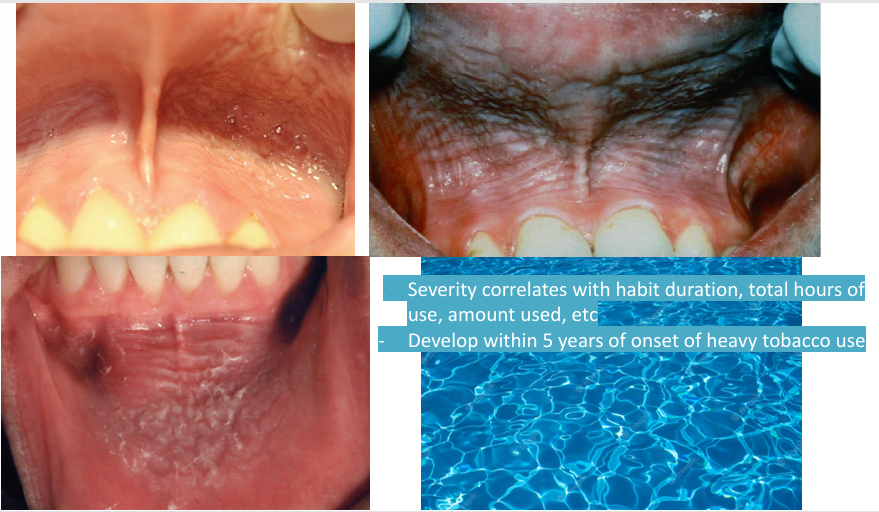
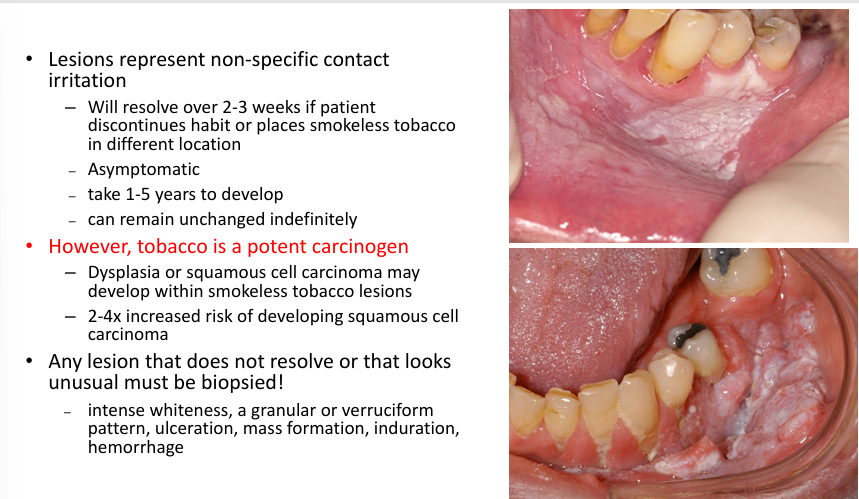
smokeless tobacco lesion
-epithelial alteration in response to repeated placement of smokeless tobacco, in vestibule- keratinocyte edema, hyperkeratosis (sometimes)
-clinical features: gray-white opalescent area, wrinkly appearance, gingival recession, staining of teeth
-similar change seen when other bulky materials held chronically in the vestibule
-stretching of mucosa reveals a distinct “pouch”- flaccid chronically stretched tissues
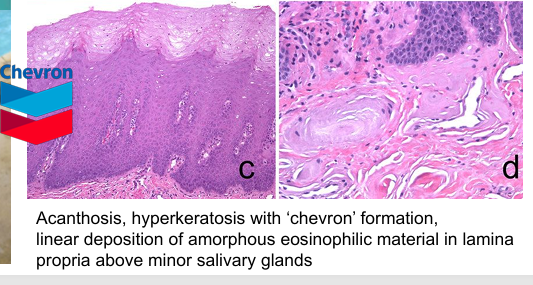
smokeless tobacco histology
other clinical presentations of smokeless tobacco- gingival recession
-painless loss of gingival tissue in area of tobacco contact (very common)
-destruction of the facial alveolar bone
-correlates with quantity of daily use and duration of use

smokeless tobacco lesions
smokeless tobacco use
-approximately 3-5% of adults use smokeless tobacco
-highest prevalence in young males in Southeastern and Midwestern states
-occasionally suggested at risk-reducing alternative to smoking
-smokeless tobacco (snuff) use: blood levels of nicotine metabolites similar to those seen in cigarette smokers, associated with increased risks of hypopharyngeal, esophageal, pancreatic, prostate, oral ccancer
-different formulations exist, of which dry snuff is associated with highest risk of oral cancer
smokeless tobacco lesion treatment
-no tx required
-alternating the tobacco-chewing sites reduces keratotic lesion
-habit cessation- normal mucosal appearance within 2 weeks, if lesion remains after 6 weeks without smokeless tobacco contact, biopsy is indicated
smokeless tobacco prognosis
-low malignant potential- risk of developing SCC less than that of cigarette smoking and alcohol abuse
-SCC develops after a long latency period of several decades
-lower risk with chewing tobacco and moist snuff and higher risk with dry snuff
-verrucous carcinoma may be associated with smokeless tobacco use
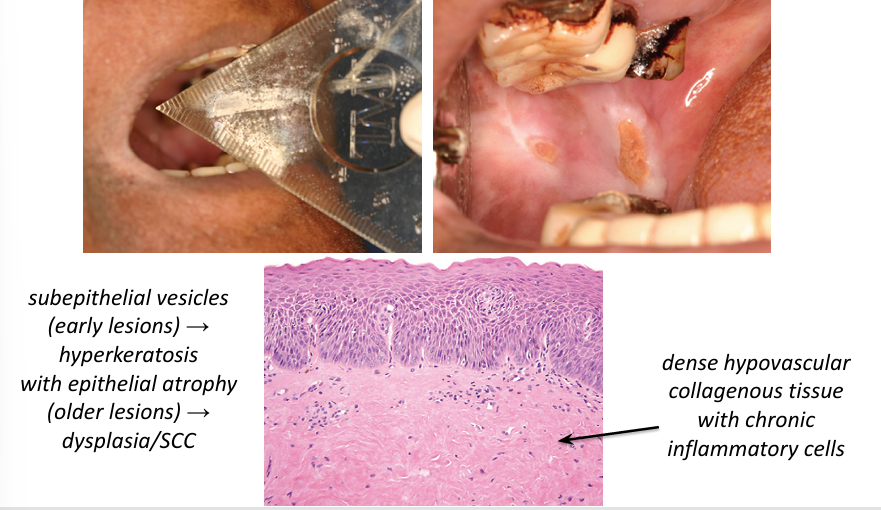
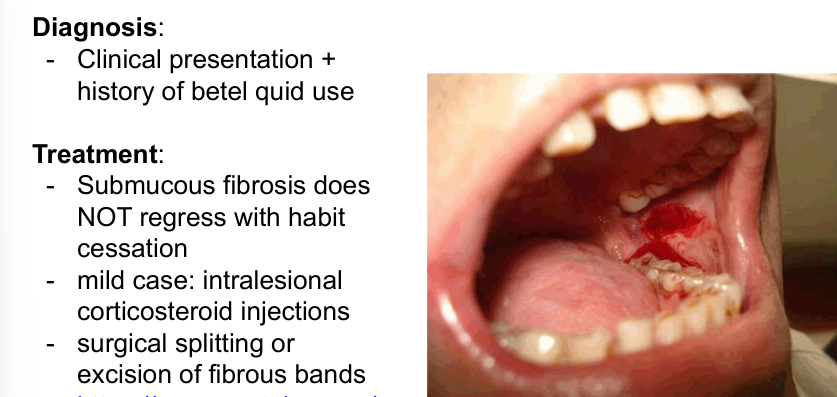
oral submucous fibrosis
-premalignant condition seen in 1-2% of areca nut and betel quid users- India, southeast Asia, Taiwan, NYC
-mucosa may appear white due to underlying fibrosis
-sometimes changes “better felt than seen”- “piano wire” feel
-patients report burning and increasing trismus
-progressive scarring/fibrosis limits mouth opening
-dysplasia may develop in long-standing lesions (7-13% of pts develop SCC)

oral submucous fibrosis clinical features
-mucosa develops blotchy, marble-like pallor and progressive stiffness of submucosal tissue
-most commonly affects buccal mucosa, retromolar area, soft palate
-palpable submucosal fibrous bands on the buccal mucosa, soft palate, labial mucosa
-extends to involve oropharynx, upper esophagus
-if tongue involved: becomes immobile, diminish in size, devoid of papillae
-white patch often noted- reflect epithelial change (most are hyperkeratosis, 10-15% epithelial dysplasia, 6% SCC)
oral submucous fibrosis dx and treatment
areca nut
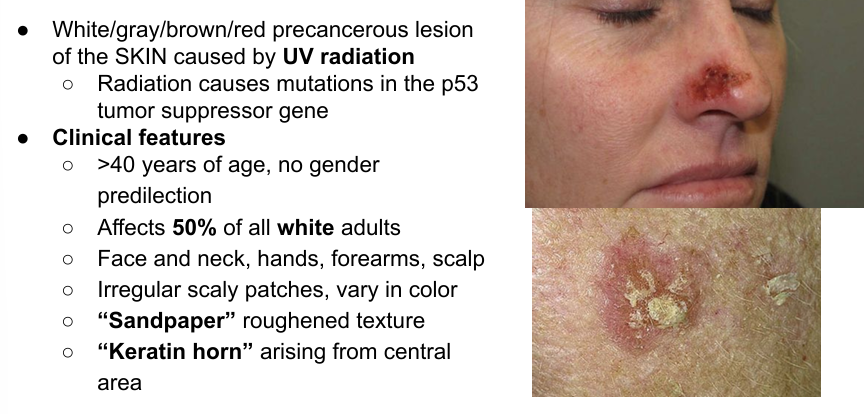
actinic keratosis
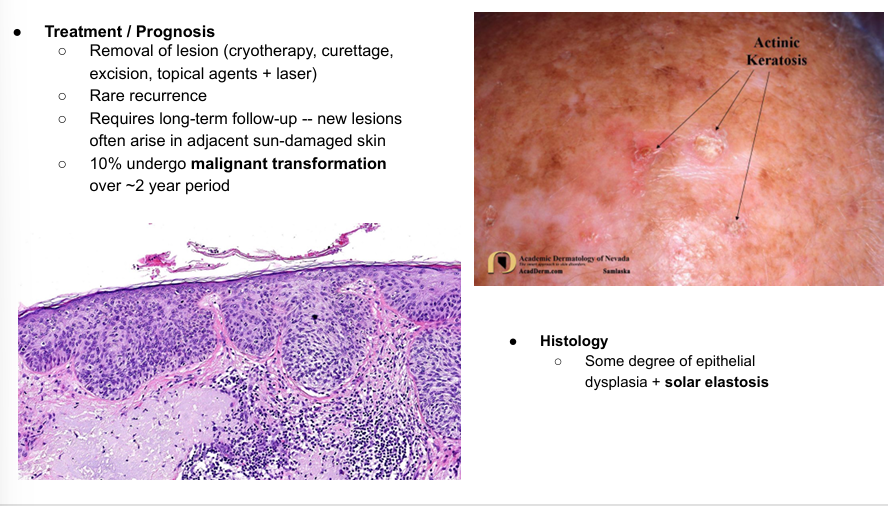
actinic keratosis tx/prognosis, histology
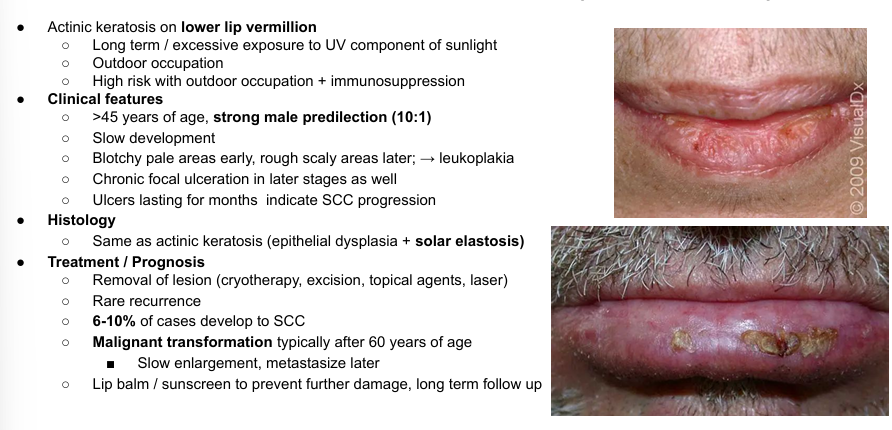
actinic cheilosis (cheilitis)
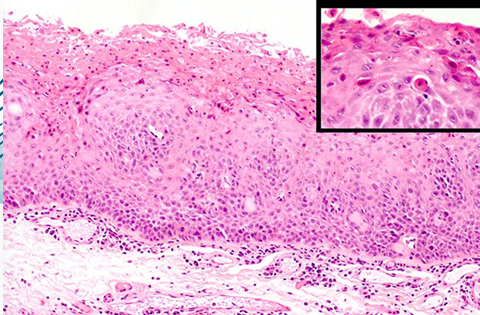
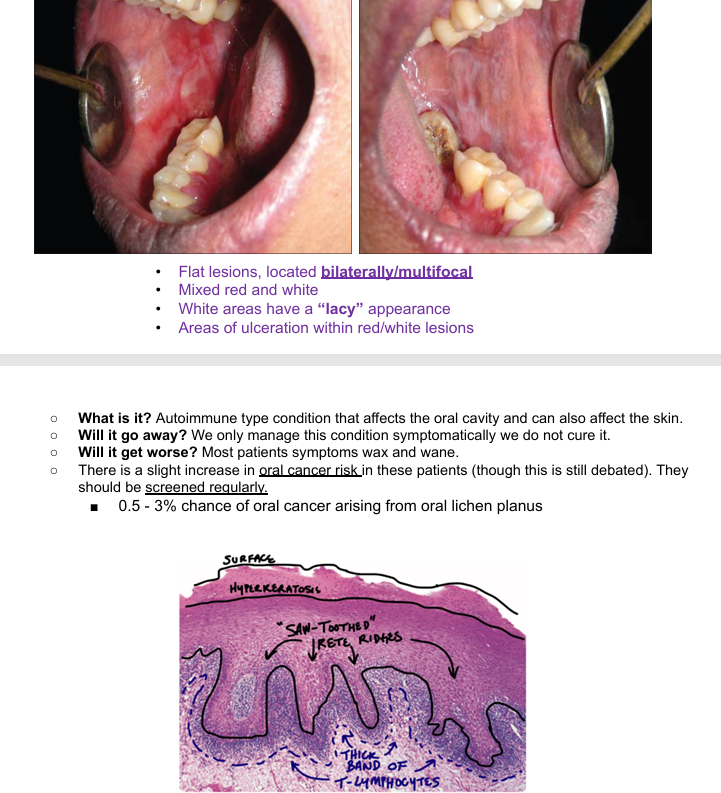
lichen planus
leukoplakia
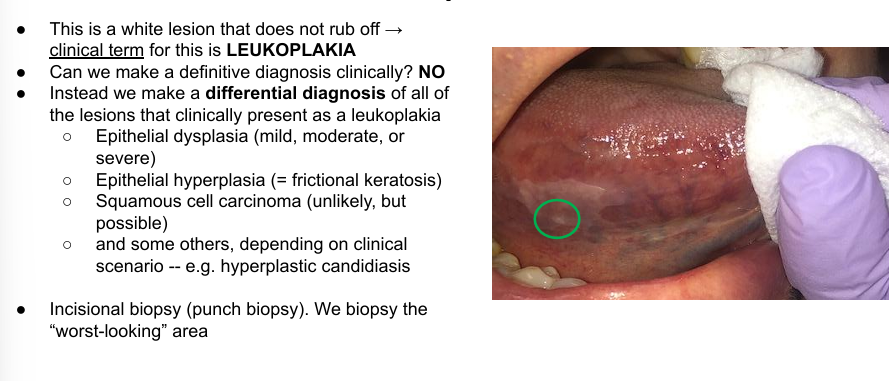
leukoplakia treatment/prognosis
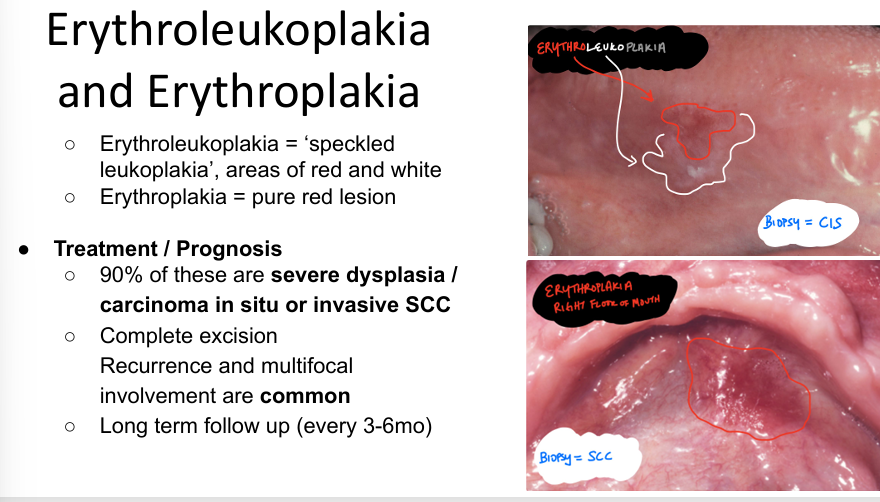
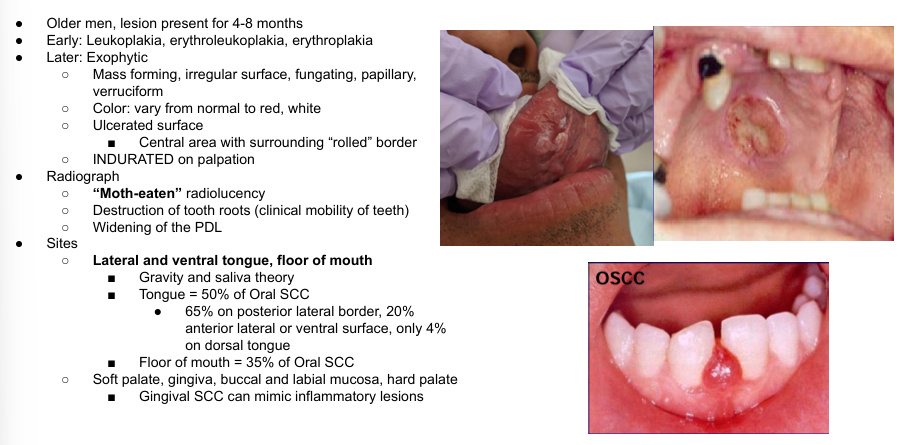
squamous cell carcinoma (SCC)
what makes a lesion white?