Introduction to Stress
1/56
There's no tags or description
Looks like no tags are added yet.
57 Terms
\
But there are many definitions, not just one
1) Shoplifting scenario
2) List best and worst personality traits
\
Three conditions: No audience, 1 person audience, 3 people present -- increased stress because increased feeling of being evaluated
Can predict things: Develop common cold twice as likely if you're stressed
Large number of daily hassles - 3x more chance than MLEs for developing depression
Reductions in immune function related to chronic stress Increase in immune function related to acute stress
What are the steps when we perceive stress as an evaluative process (Lazarus and Folkman)?
Step 1: Primary appraisal of the situation: is it threatening, challenging, etc?
Step 2: Secondary appraisal: Assess resources and choose a coping method
Step 3: Emotional focused coping: Manage emotional reaction
And/or
Problem focused coping: Deal directly with a stressor to decrease or eliminate it (best to help)
First response
Parasymp nervous system (releases acetycholine)
Parasympathetic withdrawal: Dry mouth, raised heart rate (tachicardia), slowed GI peristaltic)
Typically measured as heart rate variability
Sometimes, in rare cases, parasympathetic activated nervous system (disgust, blood phobia, fainting)
Sympathetic activation
Inhibits digestion, sweating, high heartbeat
Often measured with blood pressure, heart rate, norepiniphine in blood, salivary protein, skin conductance (sweating) pupil dilation
Second wave
(1) Hypothalamus: releases corticotrophin-releasing hormone (CHR);
(2) CHR: signals the pituitary gland to release adrenocorticotropic hormone (ACTH);
(3) ACTH: travels down to the adrenal glands where it prompts the release of cortisol.
(4) Cortisol: causes a number of changes that help deal with stress (increased blood sugar)
What is evidence against the body’s homeostasis theory by Cannon?
Body shows anticipatory reactions during stress, not just a reaction
The body often has multiple set-points: example: body temperature, different situations call for different set-points
During stress, homeostasis is sometimes actively disrupted (higher blood pressure)
What is allostasis and an allostatic load?
Allostasis: Health is state of responsiveness towards demands of the environment, more healthy than homeostasis
Definition: Maintaining physiological stability by adapting to demands
Allostatic load: A non-functional response to stress, or if you don't / can't adapt
Allostatic load (AL) represents the ‘wear and tear’ on the body after repeated allostatic responses
How can chronic stress affect the HPA-axis?
It can become dysregulated, leading to chronically elevated levels of cortisol.
impairment of the hippocampus decreases the reliability and accuracy of contextual memories, which may exacerbate more stress.
• Brief: influence on the function of the system, to which it is almost immune for a short period; this effect largely disappears when the stressor goes away, leading to increased sickness after.
• Chronic: negative impact on almost all aspects of the system; poorer immune function overall.
(2) Secondary appraisal: one’s resources and capacity to cope are evaluated
(3) Reappraisal: after a coping strategy is applied, a person reconsiders the stressor as being less or more stressful than originally thought (based on the effect of their coping)
\
(2) Cause of the illness: it is usually not possible to say whether an illness is the result of stress or other factors, as illnesses often have multiple causes and the role of stress varies between illnesses.
\
(3) Effects of stress: the effect of stress on health can be mediated by behavioral, emotional, or physical responses to stressors (people who are stressed will drink or smoke more).
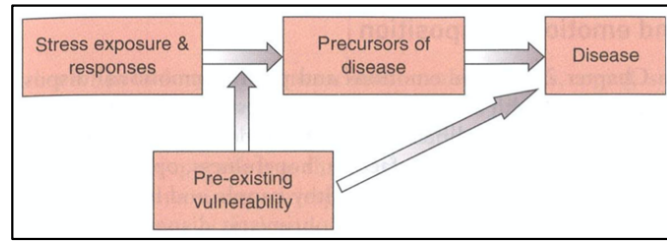
Vulnerability-stress model
= a model that summarizes how vulnerability factors interact with stressors to influence whether someone develops disease or not. It can be seen that pre-existing vulnerability influences disease both indirectly and directly
• Depersonalization = having an unfeeling, impersonal approach to others, cynicism, and a lack of engagement with the job or people.
• Reduced personal accomplishment = a poor sense of effectiveness, involvement and commitment, and poor belief in one’s ability to change or improve work patterns or environment.
(2) lack of control
(3) insufficient rewards
(4) absence of fairness
(5) value conflicts
(6) poor sense of community
(2) Threat & harm: stressful events are those that are harmful or threatening.
(3) Demands exceed resources: situations that demand more than there are resources result in stress.
(4) Interruption of goals: stressful events are those that interrupt major goals
\
For example, when someone losses his/her job he/she may be exposed to additional stressors (residential relocation, increased strain in the relationship which may lead to divorce)
\
Furthermore, employment difficulties, particularly becoming unemployed, are potent.
• **Periodicity**: random irregular events will hinder habituation, while continuous or predictable events promote it.
**• Biological processes:** many stressor-elicited changes may persist with the chronicity, while others may habituate over time.
**• After-effects:** even when an event is over, ensuing appraisal processes, affective responses, or stress-related physical effects can ‘prolong’ the impact of the event
\
These violations include expectations that occur ‘too early’ (death of a spouse early in the life course), but also those that occur ‘too late’ or not at all (not getting married, not getting promoted)
When measuring stress in the lab, what things are usually used as a marker of stress?
Anxiety levels, heart rate, adrenaline
What tests can be used to induce stress in the lab?
improvised speech
mental arithmetic
Intelligence test, etc.
Amplifying components:
time pressure
social evaluation
avoid punishment / obtain reward
What was found in the study where they gave people glucocorticoids like cortisol when doing exposure therapy?
They responded better to the exposure treatment (e.g. had less fear than treatment as usual). This could be because the glucocorticoids help the body with stressful situations, for example by increasing alertness
How do the SNS and HPA-axis affect the immune system?
The SNS increases immune system activity, while the HPA axis suppresses some immune activity through the production of cortisol.
In the experiment where people from individualist vs collectivist cultures were given either solicited or unsolicited support from a “mathematics major”?
• Participants from the collectivistic culture were less likely to ask for support and they also found the task more stressful when they had to ask for support instead of when they were given it.
• Participants from the individualistic culture rated the task as equally stressful regardless of the condition.
What 2 general approaches to stress management are there?
(1) those that focus on physical and mental relaxation (yoga, mindfulness)
(2) those that focus on cognition and behavior (psychoeducation, cognitive restructuring).
What 4 types of allostatic load are there?
(1) Frequent stress: the normal stress response is repeated frequently over time.
(2) Lack of adaptation: there is no adaptation to repeated stressors of the same type.
(3) Prolonged response: there is an inability to shut off allostatic responses after the stress is over.
(4) Hypo responsiveness: there are inadequate responses by some allostatic systems, which triggers compensatory increases in other systems.
Why does acute stress increase immune function, where chronic stress does not?
The immune system responds to pathogens with an acute-phase response as well as the formation of an immunologic memory.
Acute stress can have immune-enhancing effects, lasting for 3 to 5 days. Chronic stress can result in suppressed cellular immunity, which can lead to increased severity of the cold.
Hippocampal dysfunction
Stress-induced hippocampal dysfunction is a two-fold mechanism:
(1) Increased cortisol secretion: acute stress increases cortisol, which suppresses the mechanisms in the hippocampus that sub-serve short-term memory.
(2) Atrophy: repeated stress causes atrophy of dendrites of neurons in the hippocampus, which can result in those neurons being killed in the long-term.
What happened in the mta-analysis study where they measured acute vs chronic stress by S-IgA (a protein in saliva that protects us against viruses.) and immune function
A meta-analysis of studies measuring S-IgA during acute or chronic stress showed an increase in SIgA (better immune function) during acute stress, but a decrease in S-IgA (worse immune function) during chronic stress.
—> Acute stress can be beneficial for the immune system, but chronic stress can have negative effects.
S-IgA = a protein in saliva that protects us against viruses.