Week 10: Health promotion program planning cont.
5.0(1)
5.0(1)
Card Sorting
1/41
Earn XP
Description and Tags
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
42 Terms
1
New cards
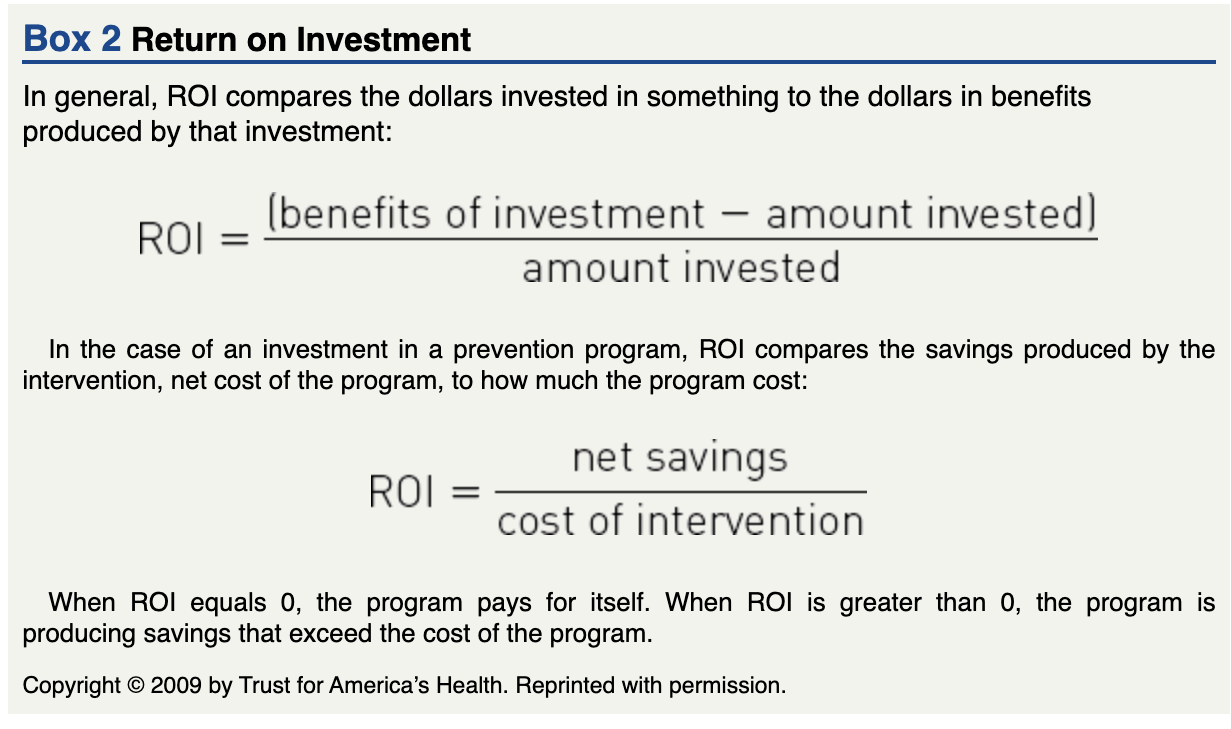
Return on investment (ROI)
measures cost of the program verses financial return of the program
*if ROI is 0, the program pays for itself, if higher than 0, the program will produce savings that exceed the cost of the program
*if ROI is 0, the program pays for itself, if higher than 0, the program will produce savings that exceed the cost of the program
2
New cards
The community guide
summarizes the findings from systematic reviews of public health interventions covering a variety of topics. The Community Guide is an essential planning tool for several reasons:
- uses a science based approach
- helps identify appropriate interventions for behaviour change, DP, and environmental change
- identifies suffiencent evidence
- complements science and rationale associated with healthy people
- uses a science based approach
- helps identify appropriate interventions for behaviour change, DP, and environmental change
- identifies suffiencent evidence
- complements science and rationale associated with healthy people
3
New cards
social math
“the practice of translating statistics and other data so they become interesting to the journalist and meaningful to the audience”
eg. breaking the numbers down by time
- what does the amount look like over a year? hour? minute?
eg. breaking the numbers down by time
- what does the amount look like over a year? hour? minute?
4
New cards
Planning parameters
There are several questions to which committee members should have answers before they become too deeply involved in the planning process.
5
New cards
capacity
the individual, organizational, and community resources, such as leadership, relationships, operations, structures, infrastructure, politics, and systems, to name a few, that can enable a community to take action
- community capacity = characteristics of a community
Capacity building = activities that enhance the resources of individuals, organizations and communities to improve their effectiveness to act
- community capacity = characteristics of a community
Capacity building = activities that enhance the resources of individuals, organizations and communities to improve their effectiveness to act
6
New cards
single step or cross sectional surveys
point in time
eg.
online surveys, mail surveys, face-to-face interviews or telephone interviews
- the information provided will be self report data
- limitations = bias
eg.
online surveys, mail surveys, face-to-face interviews or telephone interviews
- the information provided will be self report data
- limitations = bias
7
New cards
Opinion leaders
individuals who are well-respected in a community and who can accurately represent the views of the priority population. These leaders are:
Discriminating users of media, data, and activity that are community-related
Demographically similar to the priority group
Knowledgeable about community issues and concerns
Early adopters of innovative behaviour
Active in persuading others to become involved in innovative behaviour
Discriminating users of media, data, and activity that are community-related
Demographically similar to the priority group
Knowledgeable about community issues and concerns
Early adopters of innovative behaviour
Active in persuading others to become involved in innovative behaviour
8
New cards
key informants
individuals with unique knowledge about a particular topic.
eg.
- a person who has had a specific problem like losing weight and being able to talk about the barriers of such an experience
*can be subject to bias
eg.
- a person who has had a specific problem like losing weight and being able to talk about the barriers of such an experience
*can be subject to bias
9
New cards
multistep survey
those collecting the data contact respondents who will provide the data on more than one occasion.
1. send out broad survey
2. taking into account the 1st survey, a second more specific survey is sent out
1. send out broad survey
2. taking into account the 1st survey, a second more specific survey is sent out
10
New cards
nominal group process
- highly structured process in which a few
- knowledgeable representatives of the priority population (5 to 7 people) are asked to qualify and quantify specific needs.
- those invited to participate are asked to record their responses to a question without discussing it among themselves.
- knowledgeable representatives of the priority population (5 to 7 people) are asked to qualify and quantify specific needs.
- those invited to participate are asked to record their responses to a question without discussing it among themselves.
11
New cards
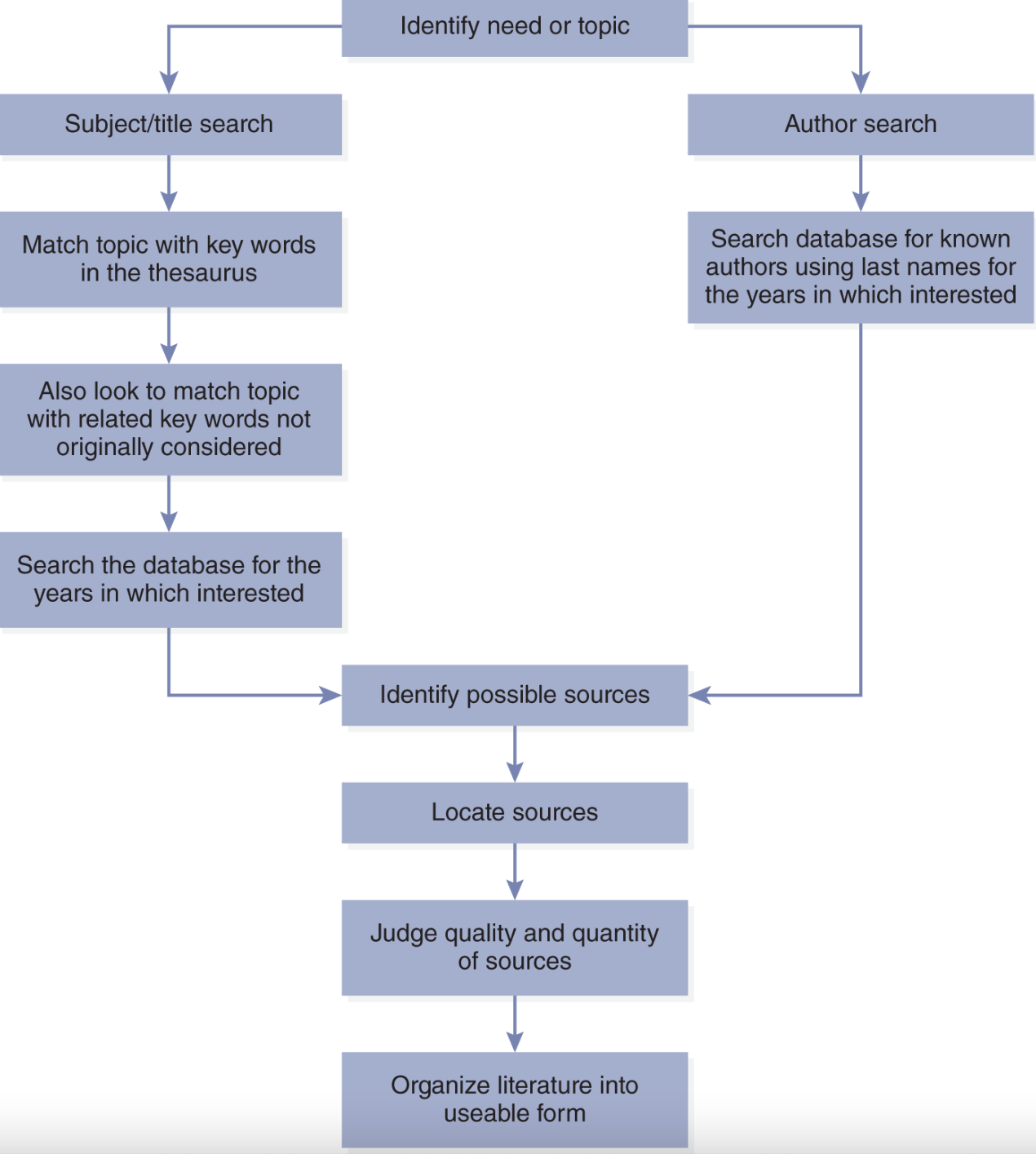
steps for conducting a literature search
12
New cards
health impact assessment
an approach that can help to identify and consider the potential or actual health impacts of a proposal on a population.
*can affect needs assessment
*can affect needs assessment
13
New cards
Health Impact assessment: 6 steps
1. screening
2. scoping
3. assessment
4. recommendations
5. reporting
6. monitoring and evaluation
2. scoping
3. assessment
4. recommendations
5. reporting
6. monitoring and evaluation
14
New cards
needs assesment: 6 steps
1. determining the process and scope
2. gathering data
3. Analyze data
4. Identify risk factors
5. Identify program focus
6. validating prioritized needs
2. gathering data
3. Analyze data
4. Identify risk factors
5. Identify program focus
6. validating prioritized needs
15
New cards
1. Determining the process and scope
what is the goal?
how extensive will the needs assessment be?
what will the planning committee gain?
time? resources? planning? funding?
participatory action research
*this step must not be minimized
how extensive will the needs assessment be?
what will the planning committee gain?
time? resources? planning? funding?
participatory action research
*this step must not be minimized
16
New cards
2. Gathering Data
- relevant data
- secondary data is recommended since easiest and cheapest to obtain (must be quantitative)
- then fill in the gaps with primary data (must be qualitative)
- figure out best methods for gathering primary data
- secondary data is recommended since easiest and cheapest to obtain (must be quantitative)
- then fill in the gaps with primary data (must be qualitative)
- figure out best methods for gathering primary data
17
New cards
3. Analyze the data
- may be most difficult step to complete
- use the first stages of PRECEDE-PROCEED
- set priorities - Basic Priority Rating model
- use the first stages of PRECEDE-PROCEED
- set priorities - Basic Priority Rating model
18
New cards
4. Identify risk factors linked to the health problem
- parallel to second phase of PRECEDE-PROCEED
- genetic, behavioural, environmental risk factors?
- once risk factors are identified, they must be prioritized
- genetic, behavioural, environmental risk factors?
- once risk factors are identified, they must be prioritized
19
New cards
5. Identifying Program focus
- Similar to third phase of PRECEDE-PROCEED
- identify the factors that have a direct impact on the risk factors
- networking
- identify the factors that have a direct impact on the risk factors
- networking
20
New cards
6. Validating Prioritized needs
- double checking
- focus groups with priority population to determine their reaction to the proposed need
- focus groups with priority population to determine their reaction to the proposed need
21
New cards
Interventions
the planned actions that are designed to prevent disease or injury or promote health in the priority population.
eg.
provide an incentive by stating that all employees seen wearing their safety belts would receive a $10 bonus in their next pay check.
eg.
provide an incentive by stating that all employees seen wearing their safety belts would receive a $10 bonus in their next pay check.
22
New cards
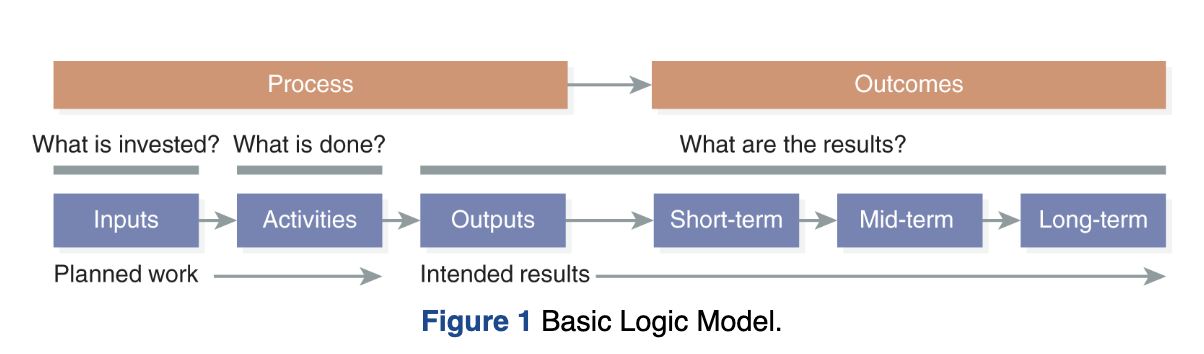
logic model
a logic model is a road map (Goldman & Schmalz, 2006) showing the connections among the key components of a program.
also called: a theory of change
also called: a theory of change
23
New cards
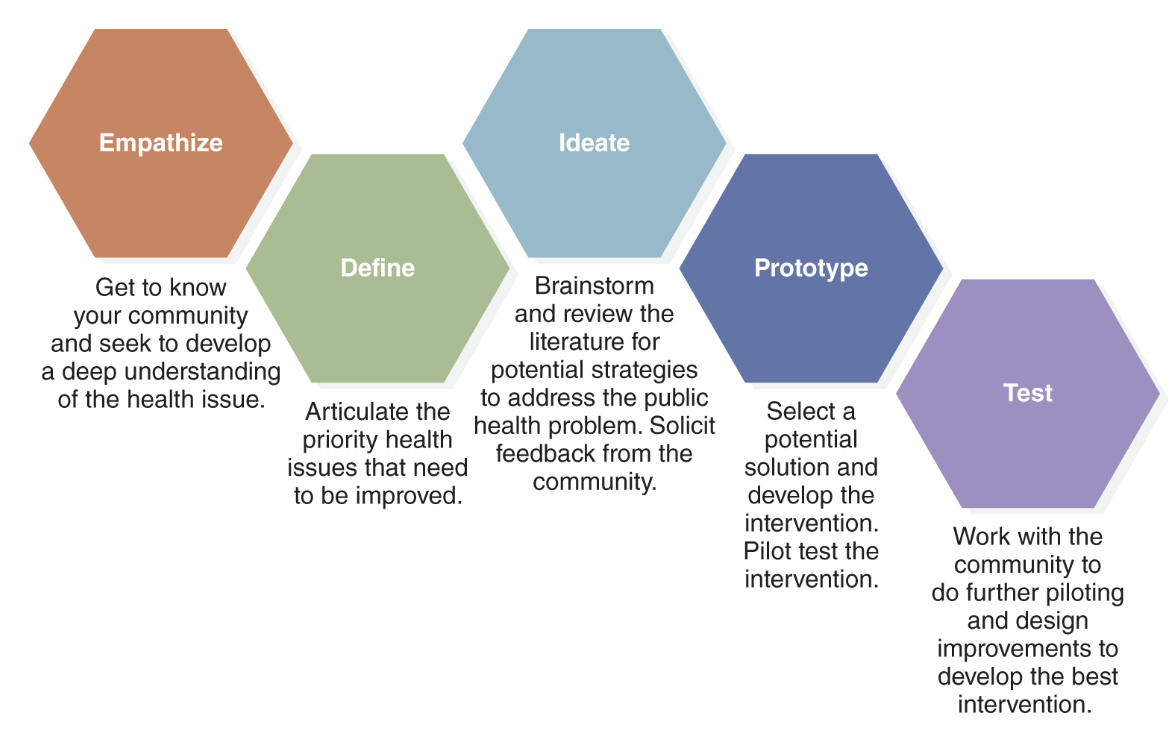
5 steps of Design thinking and intervention planning
1. Empathize
- get to know community, develop understanding of the issue
2. Define
- articulate the priority health issues
3. Ideate
- brainstorm and review literature for potential strategies
4. Prototype
- select a potential solution and develop the intervention
- pilot test
5. test
- work with community to design and improve the best intervention
- get to know community, develop understanding of the issue
2. Define
- articulate the priority health issues
3. Ideate
- brainstorm and review literature for potential strategies
4. Prototype
- select a potential solution and develop the intervention
- pilot test
5. test
- work with community to design and improve the best intervention
24
New cards
6 groups of intervention strategies
1. Health communication
- highest penetration rate lol
- health promotion programs
- Motivational interviewing
2. Health education
- theory and evidence based information
- no clear line between health communication and education
3. Health policy/enforcement
- orders, laws, policies
- made by authoritative person or organization
4. Environmental change
- providing opportunities, support to develop healthier behaviours
- removing environmental barriers
5. Health-related community service
- tests, treatments, care
- offered in variety of settings (clinics, pharmacies, stores)
6. Health advocacy and community mobilization
- community advocacy
- lobbying
- highest penetration rate lol
- health promotion programs
- Motivational interviewing
2. Health education
- theory and evidence based information
- no clear line between health communication and education
3. Health policy/enforcement
- orders, laws, policies
- made by authoritative person or organization
4. Environmental change
- providing opportunities, support to develop healthier behaviours
- removing environmental barriers
5. Health-related community service
- tests, treatments, care
- offered in variety of settings (clinics, pharmacies, stores)
6. Health advocacy and community mobilization
- community advocacy
- lobbying
25
New cards
where do we spend most of our healthcare dollars?
treatment and 'never ending ever-elusive' search for cures
26
New cards
T/F? our medical system falls under the population strategy
false, 95% of our medical system falls under the clinical strategy
5% is population
5% is population
27
New cards
the prevention paradox
unless we focus on people who are low or moderate risk, we will fail to reach the majority of people that will eventually develop a disease like cancer, obesity, heart disease
28
New cards
high risk strategies (Micro)
- individuals deemed at high risk to develop a certain disease are targeted to receive the health intervention
- High risk strategies have the ability to prevent disease in a small number of highly susceptible individuals, but no ability to prevent disease in large numbers of low risk people
eg. screening for gum cancer in individuals who chew tobacco
- High risk strategies have the ability to prevent disease in a small number of highly susceptible individuals, but no ability to prevent disease in large numbers of low risk people
eg. screening for gum cancer in individuals who chew tobacco
29
New cards
advantages of high risk strategies
- motivation of both practitioners and patients/ clients
- financial sensibility (using limited resources on those who need it)
- benefits are favourable
- financial sensibility (using limited resources on those who need it)
- benefits are favourable
30
New cards
disadvantages of high risk strategies
- medicalization of prevention (sense of feeling like a patient requiring treatment instead of they healthy individual they though they were
- challenges and costs of interventions
- ideal is very hard to achieve
- temporary results
- limited potential for individuals and population
- Behavioural insufficiencies
*large numbers of people with low risk produce higher incidence rates than a smaller group with low risk
- challenges and costs of interventions
- ideal is very hard to achieve
- temporary results
- limited potential for individuals and population
- Behavioural insufficiencies
*large numbers of people with low risk produce higher incidence rates than a smaller group with low risk
31
New cards
A _____ number of people at a small risk may give rise to more cases of disease than the _____number who are at high risk
large
small
small
32
New cards
Population-based strategies (macro)
- targets entire population
- purpose = decrease disease incidents and reduce overall level of risk
- factors intended to change behaviours & practices of the population
eg. COVID-19 mask mandates
- purpose = decrease disease incidents and reduce overall level of risk
- factors intended to change behaviours & practices of the population
eg. COVID-19 mask mandates
33
New cards
advantages of population based strategies
- radical = attempts to find the ROOT cause of disease and eradicate it
- powerful - changes the exposure risk for the entire population = powerful potential for health gains
- behaviourally appropriate = working with social norms
eg. smoking indoors
- powerful - changes the exposure risk for the entire population = powerful potential for health gains
- behaviourally appropriate = working with social norms
eg. smoking indoors
34
New cards
limitations of population based strategies
- individual benefits are minimal
- lack of motivation for population
- minimal benefits experienced by each individual may not
outweigh the small risk
eg. fake fat
-> olestra in potato chips
- lack of motivation for population
- minimal benefits experienced by each individual may not
outweigh the small risk
eg. fake fat
-> olestra in potato chips
35
New cards
circumstances for adopting population-based strategies
- when the health risk has permeated the entire population
- when, on a population-scale, benefits are outstanding but on an individual level, benefits are minimal
- when the only way to deliver intervention is through population strategies
eg. vitamin rich foods
- whenever the need is to impact as many people as possible
eg. smoking bylaws
- when, on a population-scale, benefits are outstanding but on an individual level, benefits are minimal
- when the only way to deliver intervention is through population strategies
eg. vitamin rich foods
- whenever the need is to impact as many people as possible
eg. smoking bylaws
36
New cards
MI: If at the end.... happened....
1st tool of effective behaviour change - find out what they want
allows for:
- client to consider their goal
- client buy in
- expectation management
- engages client
- cultivates 'partner' relationship
allows for:
- client to consider their goal
- client buy in
- expectation management
- engages client
- cultivates 'partner' relationship
37
New cards
MI lecture definition
"a client centered counselling style that helps people to resolve and restore their ambivalence regarding behaviour change"
(can be seen as scary to clients)
better definition:
"arranging conversations so people talk to themselves into change based on their own values and interests"
(can be seen as scary to clients)
better definition:
"arranging conversations so people talk to themselves into change based on their own values and interests"
38
New cards
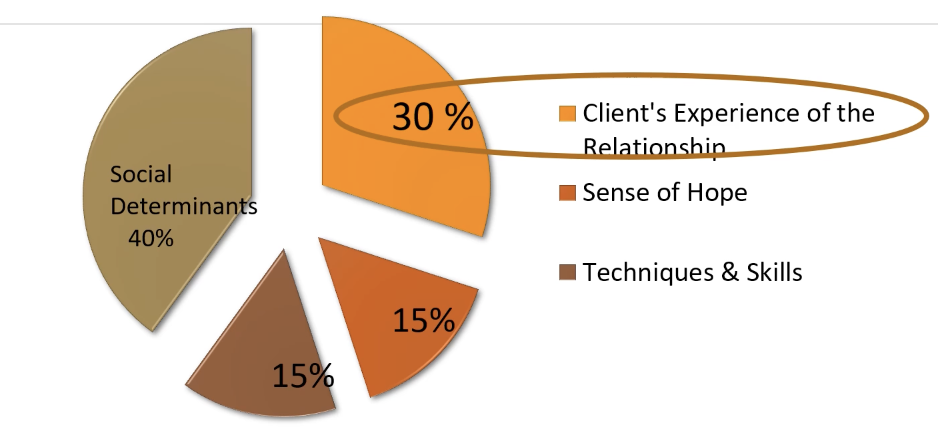
ENGAGING - Critical importance of relationship with you in manifesting positive change
39
New cards
the importance of: What is important?...
- taps into clients values
- why WE want them to change is irrelevant
- finding their desire to change
- responsibility shifts from practitioner to client
- more effective for client
eg. what is important to you about having a healthy heart?
- why WE want them to change is irrelevant
- finding their desire to change
- responsibility shifts from practitioner to client
- more effective for client
eg. what is important to you about having a healthy heart?
40
New cards
the advice challenge
*AVOID UNSOLICITED ADVICE
- ask permission before giving advice
- ask permission before giving advice
41
New cards
4 qualities of empathy
1. perspective taking
2. staying out of judgement
3. recognizing emotion
4. communicating that emotion
2. staying out of judgement
3. recognizing emotion
4. communicating that emotion
42
New cards
The Michelangelo belief
- Michelangelo carved his statue from an uggo mountain
- the capacity and potential for change is within every person
- masterpiece is within us
- the capacity and potential for change is within every person
- masterpiece is within us