10. ECG Interpretation: Conduction Blocks and Analysis
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
What is the function of the P wave on an ECG?
Atrial depolarization/contraction via SA node.
What does the PR Interval represent on an ECG?
Electrical flow from atria through AV node and HIS Bundle.
What does the QRS complex represent on an ECG?
Ventricular depolarization/contraction via Purkinje fibers.
What does the ST Segment represent on an ECG?
Electrical currents generated by repolarization of the ventricles.
What does the T wave represent on an ECG?
Ventricular repolarization/ relaxation.
What are the normal escape rhythm rates for the S.A. Node?
60-100 BPM.
What are the normal escape rhythm rates for the A.V. Node?
40-60 BPM.
What are the normal escape rhythm rates for the His Bundles?
25-40 BPM.
What are the normal escape rhythm rates for the Purkinje Fibres?
15-30 BPM.
What are the key parameters reviewed during EKG/Rhythm Interpretation?
Rhythm;
Rate;
P wave (ensure there is a p wave for every QRS, same morphology)
Intervals (P-R; QRS; QTc);
QRS;
ST segment;
T wave.
What is the normal rhythm for Normal Sinus Rhythm (NSR)?
Regular.
What is the normal rate range for Normal Sinus Rhythm (NSR)?
60-100 bpm.
What are the normal P wave findings in NSR?
Same morphology; One P wave for every QRS.
What is the normal duration of the PR Interval in seconds and small boxes?
0.12 - 0.20 seconds ( 3-5 small boxes).
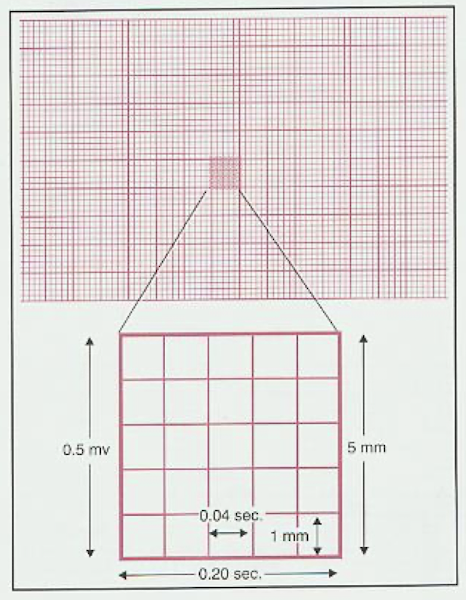
What is the normal duration of the QRS Complex in seconds and small boxes?
<0.12 seconds (less than 3 small boxes).
How is the QTc calculated and what is its normal duration?
QT/√r-r; Normally less than 440 msec.
What is the expected appearance of the ST Segment in NSR?
Isoelectric ( no significant ST elevation or depression).
What is the expected appearance of the T waves in NSR?
Normally positive in leads with positive QRS
Which lead is most commonly used for the rhythm strip?
Where is the rhythm strip usually displayed on a 12-lead EKG and why?
Lead II – aligns well with the heart’s normal depolarization vector and shows clear P waves and QRS complexes.
Bottom of the page – provides a longer, continuous view of the heart rhythm to detect arrhythmias, pauses, or conduction abnormalities. The top 12 leads show snapshots for morphology and axis analysis.
What is the definition of a conduction block?
Any obstruction or delay of the flow of electricity along the normal pathways of electrical conduction.
How is AV block defined and what is examined to diagnose it?
This term refers to any conduction block between the sinus node and the terminal Purkinje fibers; We examine the relationship between P wave and QRS complex.
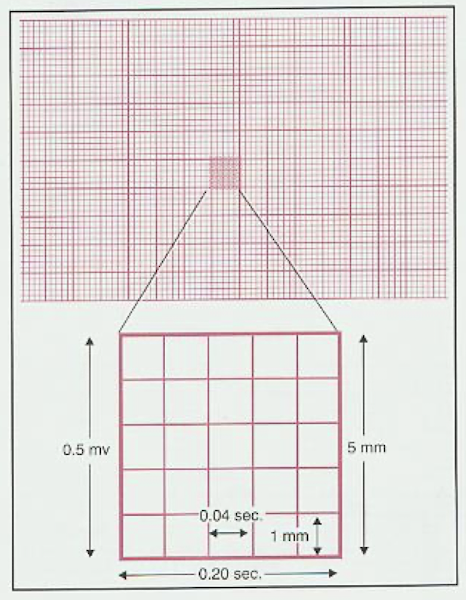
What characterizes a First-Degree AV Block?
There is consistent conduction through the AV node.
What characterizes a Second-Degree AV Block?
There is intermittent non-conduction through the AV node or Bundle of His.
What characterizes a Third-Degree AV Block?
There is NO conduction between the atria and ventricles ( complete AV dissociation).
What is a bundle branch block and what parameter is examined on the ECG?
Refers to a conduction block in the right or left ventricular bundle; We look at the width and configuration of the QRS complex.
What is the mechanism of conduction delay in First-Degree AV Block?
Delay of conduction through AV node or Bundle of His.
What is the key diagnostic feature for First-Degree AV Block on an ECG regarding the P and QRS relationship?
One P wave for every QRS complex.
What is the defining measurement for the PR Interval in First-Degree AV Block?
PR Interval greater than 0.20 seconds.

What measurement threshold, in small or large boxes, signifies a prolonged PR interval for First Degree AV Block?
Greater than 0.20 seconds ( 5 small blocks or one large block in horizontal plane

What are common causes of First-Degree AV Block?
Meds (digitalis; beta blockers; calcium channel blockers); inferior Ischemia; lyme disease.
Why does Second-Degree AV Block result in fewer QRS complexes than P waves?
Because some p waves fail to conduct you do not have a QRS complex for every p wave.
What are the two types of Second-Degree AV Block?
Mobitz Type I Second-Degree AV Block (Wenckebach); Mobitz Type II Second-Degree AV Block.
What is Mobitz Type I Second-Degree AV Block also known as?
Wenckebach.
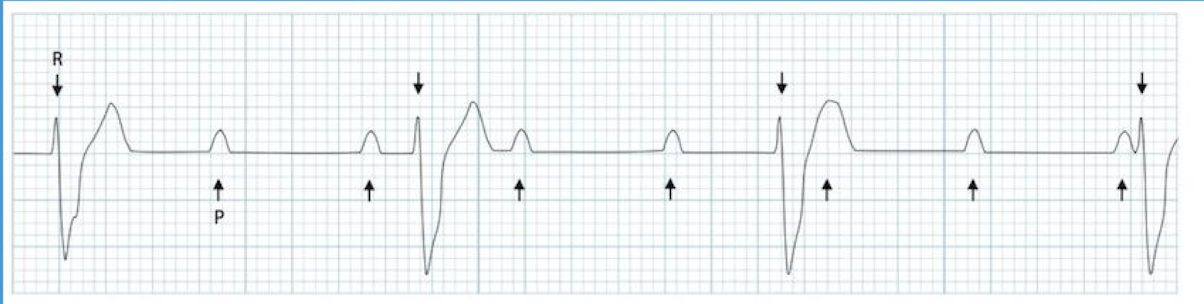
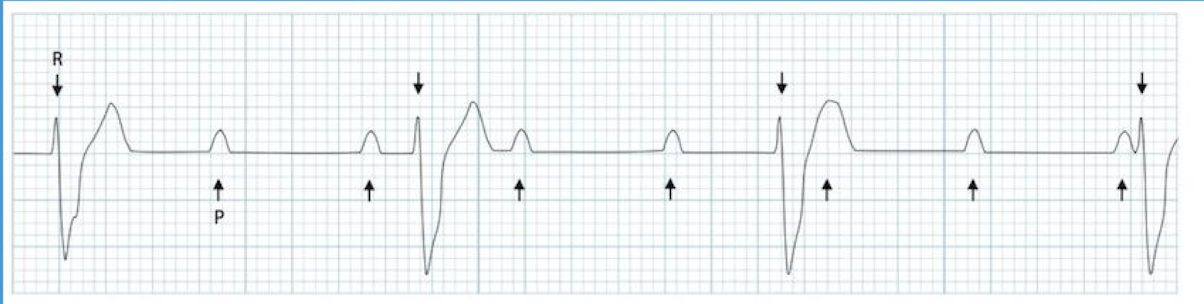
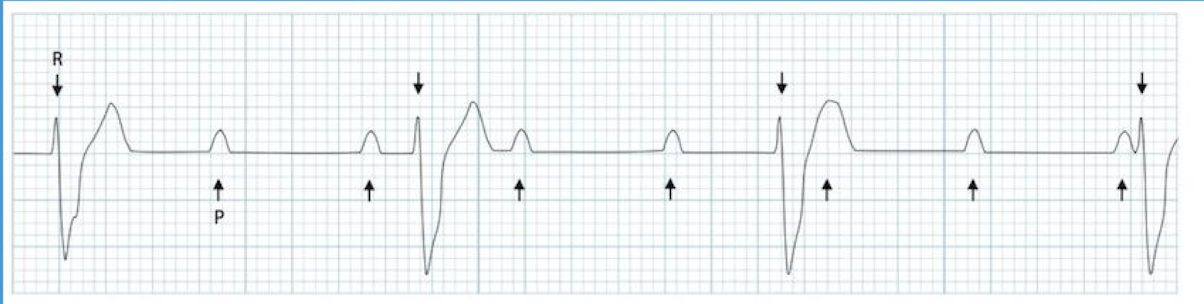
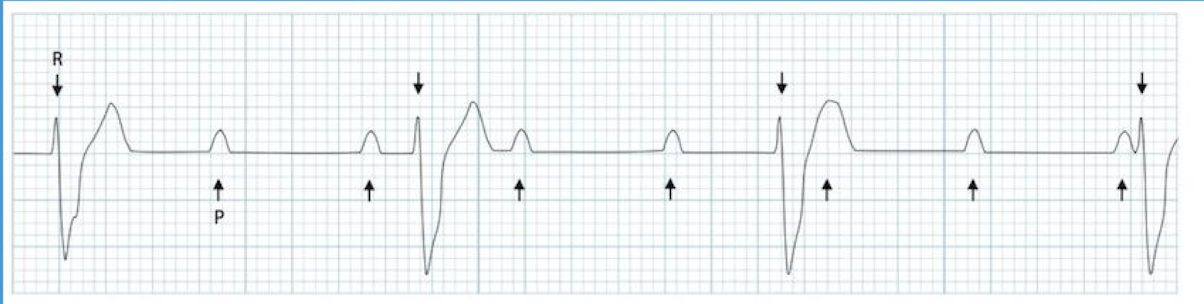
What is the underlying mechanism of conduction in Mobitz Type I Second-Degree AV Block (Wenckebach)?
Slowed conduction through the AV node.
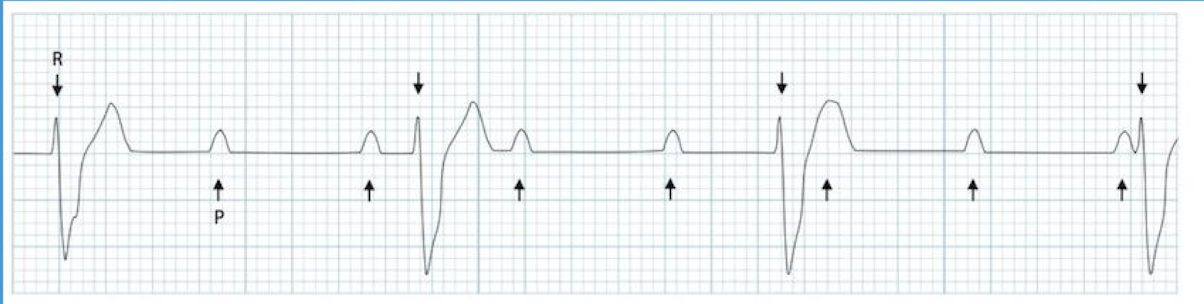
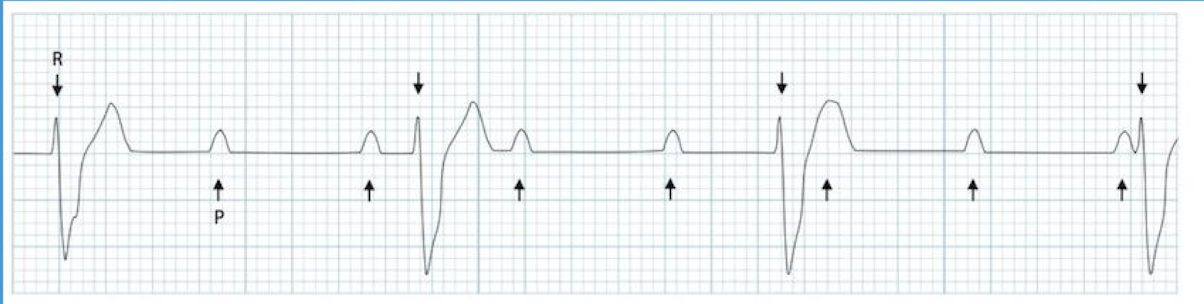
What happens to the PR interval and QRS complex in Mobitz Type I AV Block?
There is progressive lengthening of the PR interval until a QRS complex is dropped.

How often does the cycle repeat itself in Mobitz Type I Second-Degree AV Block?
Sequence repeats itself regularly.

How is the P wave/QRS complex relationship described in Mobitz Type I AV Block?
One for every QRS until one QRS drops.

In which specific population is Mobitz Type I Second-Degree AV Block often seen?
Common in athletes.


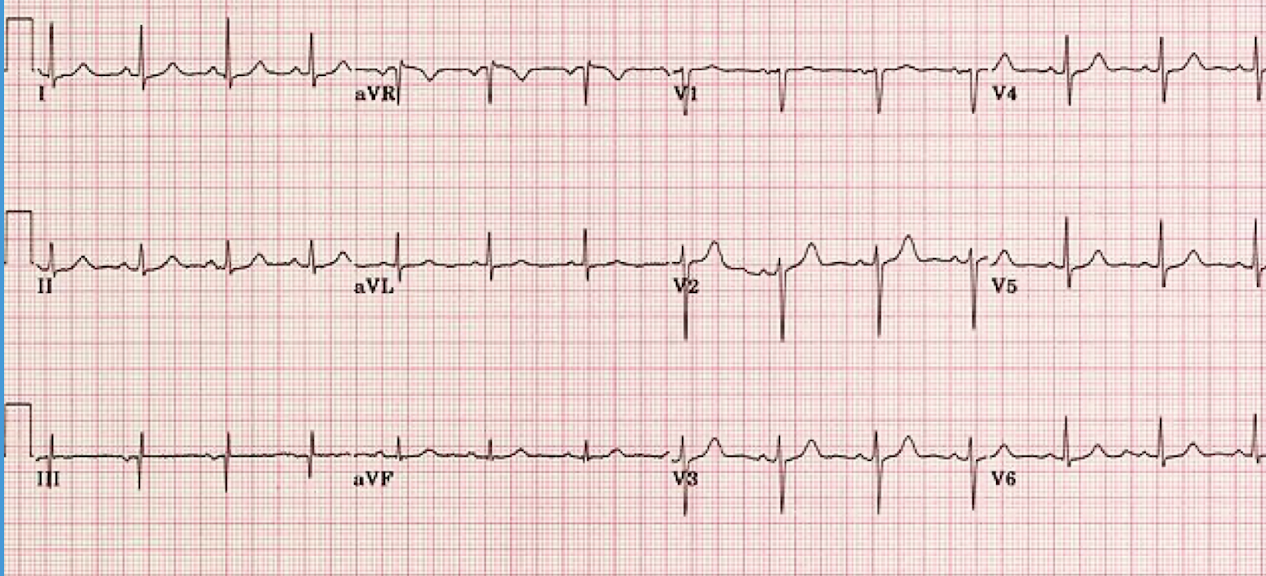
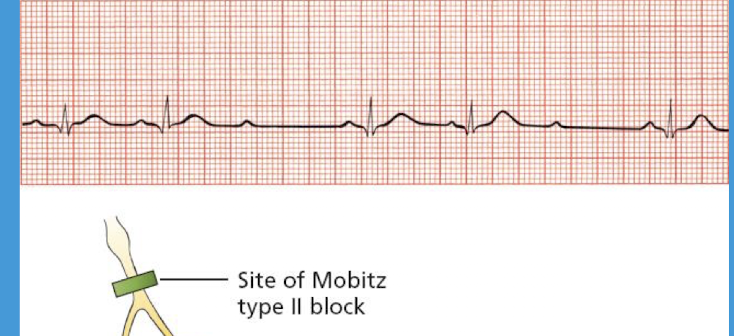
What is the usual site of slowed conduction in Mobitz Type II Second-Degree AV Block?
Usually due to slowed conduction below the AV node and in the Bundle of His.



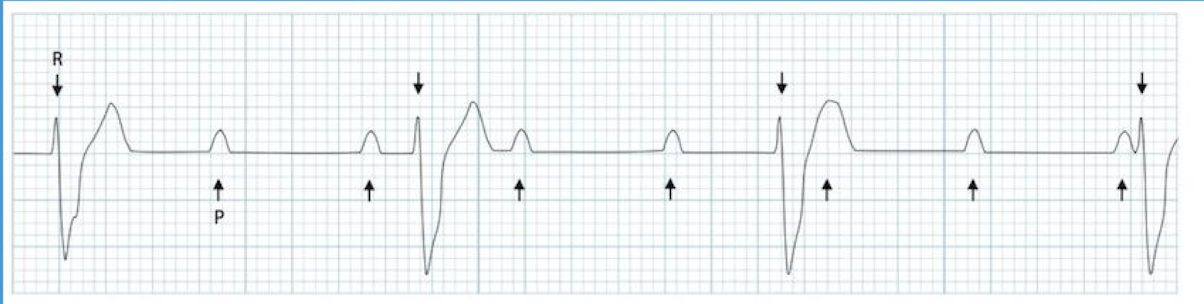
What happens to the PR Interval immediately before a dropped QRS complex in Mobitz Type II AV Block?
PR Interval stays the same before a dropped QRS complex.
How does the P wave to QRS complex ratio behave in Mobitz Type II AV Block?
Cycle repeats but the ratio of P waves to QRS complexes varies.
What is the expected QRS Interval measurement in Mobitz Type II Second-Degree AV Block?
>0.12 sec (Normal <0.12 sec or less than 3 small boxes).

Does the PR interval need to be prolonged in Mobitz Type II Second-Degree AV Block?
No; it does not need to be prolonged ( > 0.20).

What defining feature distinguishes Mobitz Type II on an EKG strip?
P-R interval is fixed with sudden drop of QRS.

What is the recommended treatment for symptomatic patients with Mobitz Type II Second-Degree AV Block?
PPM (Permanent Pacemaker).
What is Third-Degree AV Block also known as?
Complete Heart Block.
What is the main physiological feature of Third-Degree AV Block regarding electrical activity?
No conduction from atria to ventricles.
How is the relationship between P waves and QRS complexes described in Third-Degree AV Block?
Complete AV dissociation ( NO relationship between P and QRS complex).
How does the ventricular rate compare to the atrial rate in Third-Degree AV Block?
Ventricular rate is slower than the atrial rate.
What drives the ventricles in Third-Degree AV Block and what is the typical QRS appearance?
Ventricles are driven by a ventricular escape rhythm; Most QRS will be wide.
What is the typical ventricular rate finding in Third-Degree AV Block?
< 30 bpm.
What is the treatment for Third Degree AV Block?
PPM (Permanent Pacemaker).
What are the two key characteristics of the QRS complex during normal ventricular depolarization?
The QRS is narrow ( less than 0.12 seconds); and the axis is normal (between 0-90 degrees).
What is the physiological mechanism of Right Bundle Branch Block (RBBB)?
Conduction through the right bundle is obstructed which results in a delay in depolarization of the right ventricle.
What is the defining QRS width measurement for Right Bundle Branch Block?
QRS complex widened to greater than 0.12 seconds.
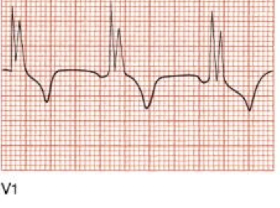
What specific QRS morphology is seen in leads V1 and V2 for RBBB?
RSR′ (rabbit ears) or a tall R wave in V1 and V2 with ST-segment depression and T-wave inversion.

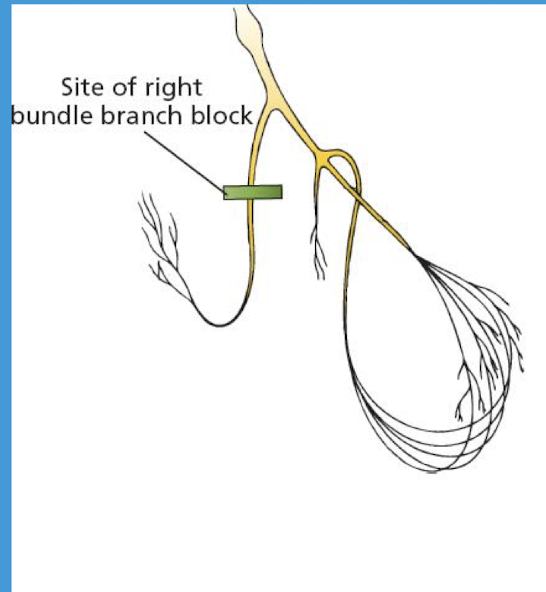
Where are reciprocal changes typically seen in a Right Bundle Branch Block?
V5; V6; I; and aVL.
What is the physiological mechanism of Left Bundle Branch Block (LBBB)?
Conduction through the left bundle is obstructed which results in a delay in depolarization of the left ventricle.
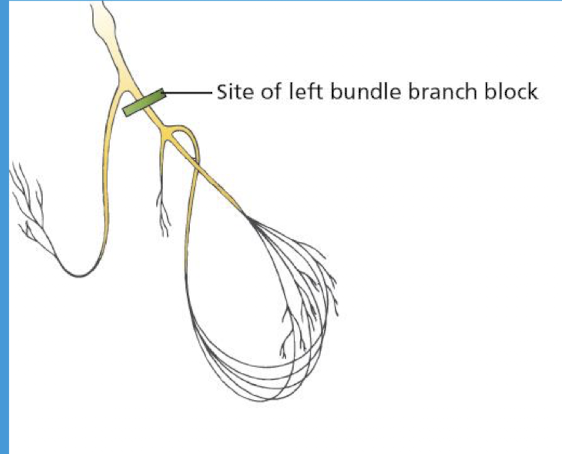
What is the defining QRS width measurement for Left Bundle Branch Block?
QRS complex widened to greater than 0.12 seconds.
What specific QRS morphology is seen in leads V5, V6, I, and aVL for LBBB?,
Broad or notched R wave with prolonged upstroke in leads V5; V6; I; and aVL; with ST-segment depression and T-wave inversion


Where are reciprocal changes typically seen in a Left Bundle Branch Block?
V1 and V2.
What axis deviation may be present in a Left Bundle Branch Block?
Left axis deviation may be present.
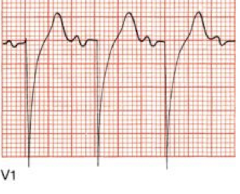
When trying to distinguish between LBBB and RBBB on an EKG, which lead is most useful and what should you look for?
Lead V1 is most useful.
RBBB: “Rabbit ears” (rSR’ pattern) in V1 — a small initial R, deep S, and tall terminal R’.
LBBB: Broad, deep S wave or inverted terminal R in V1 — often a wide, negative QRS without the classic “rabbit ears.”

