Anxiety disorders and anxiolytics
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
56 Terms
Define anxiety
A normal physiological response to threatening situations. This serves as a protective function. It becomes pathological when non-threatening stimuli are more likely to be interpreted as threatening stimuli.
Describe the prevalence of anxiety in the UK
Around 8 million people in UK have anxiety. It is the 2nd most common neurological condition after headache in the UK.
What are the different types of anxiety disorder?
1. Simple/ specific phobias e.g. arachnophobia, agoraphobia, claustrophobia
2. Social phobia/ social anxiety disorder (SAD)
3. Panic disorder (PD) (often in response to trigger, heart thumping out of chest feeling)
3. Post traumatic stress disorder (PTSD) e.g. flashbacks to a memory
4. Generalised anxiety disorder. Diffuse vague worries of things in the future.
5. Obsessive compulsive disorder. Anxiety drives the compulsive disorder.
6. Premenstrual dysphoric disorder - this can be considered an anxiety disorder or mood disorder. This is associated with the menstrual cycle.
What is the most common anxiety disorder?
Generalised anxiety disorder
What are the DMS criteria for general anxiety disorder?
It must have the features of:
- Excessive anxiety and worry most days of the week at least for 6 months
- Patient cannot control feeling of worry
It should also include 3 of the following symptoms:
- restlessness
- fatigue
- trouble concentrating
- irritability
- muscle tension
- sleep problems
What conditions are common in patients with generalised anxiety disorder?
1. Other anxiety disorders
- Phobias
- Panic disorder
- PTSD
2. Depression
3. Substance abuse
Name core features of anxiety disorders
- Negative cognition
- Physiology
- Avoidance
What are the main features of panic disorder?
Experience panic attacks
"might die"
What are the main features of social anxiety disorder?
Blushing, speech
Embarassment
What are the main features of generalised anxiety disorder?
Worry, tension
Future threat
What are the main features of post traumatic stress disorder?
Flashbacks to known trigger where they "will die"
What is negative cognition?
When a person has a bias to interpret unthreatening situations as threatening or negative.
Negative cognition is often reinforced of memories. For example, a negative association with a person/ object to an unpleasant situation.
What are psychological symptoms of anxiety controlled by?
Activation of the autonomic nervous system (fight or flight)
What are examples of psychological symptoms of anxiety?
- Racing heart
- Palpitations
- Restlessness
- Sweating
- Increased blood pressure
What are defence/ avoidant behaviours controlled by?
Activation of the amine pathways (noradrenaline, 5-HT)
Describe the normal response to threats
1. Threatening stimulus causes a stress/ fear response which is both learnt and innate.
The innate response includes:
- Autonomic activation - fight or flight response
- Negative emotions (aggression, anger)
- Defence and avoidance behaviours
- Arousal and alertness (increased vigilance)
Hypothalamus results in corticosteroid secretion (leading to metabolic effects)
Outline signal transmission of the innate fear response
- Sensory information is received from triggering stimulus (e.g. seeing a spider)
- Signal travels to the thalamus (sensory relay station)
- The thalamus connects to the amygdala (fear centre of the brain)
- Amygdala activates HPA (hypothalamus pituitary axis) via the hypothalamus - body ready for fight or flight
This triggers amine neurotransmitters (which are associated with alertness, attention and vigilance) and periaqueductal grey (which is associated with defence and avoidance behaviour).
What does the activation of the hypothalamus pituitary axis (HPA) result in?
- Release of cortisol and adrenaline
- Autonomic activation: fight or flight
Describe brain area involved in the "learnt" fear response
The prefrontal cortex provides information. This integrates emotions into decision making alongside the hippocampus which sees whether the brain recognises the stimulus.
What is the "alive, alert, awake" neurotransmitter?
Noradrenaline
What is the cause of anxiety disorders?
We are not too sure what causes anxiety disorders.
It could relate to abnormal regulation in brain areas involved in fear. For example:
- Could be underactivity of 5-HT system
- Could be overactivity of NA system
- Could be disruption in level of GABA inhibition
- Genetics and environmental factors
How may there be disruption in GABA inhibition resulting in anxiety disorders?
- Reduced expression of GABAa receptors
- Reduced function/regulation of GABAa receptors by benzodiazepines
- Reduced function/regulation of GABAa receptors by neurosteroids
What are the different treatment types for anxiety disorders?
1. Pharmacotherapy
2. Psychological interventions (low intervention = self help; high intensity interventions = CBT)
What are the different medical treatments for anxiety disorders?
- Beta blockers
- Benzodiazepines
- Antidepressants
- Buspirone (partial agonists at 5HTa receptors)
Describe the stepped-care approach to generalised anxiety disorder (GAD)
Step 1 - low level of intervention
- This is for all known and suspected presentations of GAD
Step 2 - diagnosis of GAD and education
- Here, low intensity psychological interventions are tried ( individual guided self-help and
psychoeducational groups)
Step 3 - GAD with marked functional impairment -> drug treatment or of a high-intensity psychological intervention (CBT/applied relaxation
Step 4 - more complex drug treatment and/or psychological treatment regimens
Describe the use of beta blockers for treatment of generalised anxiety disorder
Beta blockers treat autonomic symptoms of anxiety. They will slow down heart rate.
Describe the use of propranolol for anxiety disorders
Propranolol has been used for treating specific phobias.
In Amsterdam some people have been cured of their fear of spiders using propranolol
This is because propranolol also works on memory and can cause people to forget they're scared of spiders.
Now it is being investigated to see if it can be used for the treatment of PTSD.
Describe GABA-a receptors
Ligand-gated ion channel
5 subunits (pentameric): usually 2 alphas, 2 beta, one gamma sub-unit
It is a Cl- channel
GABA binds to GABA-a receptor.
It has 2 GABA binding sites, both alpha-beta interfaces.
Where does GABA bind?
Agonist binding site
It is between the alpha and beta subunits (alpha beta interface)
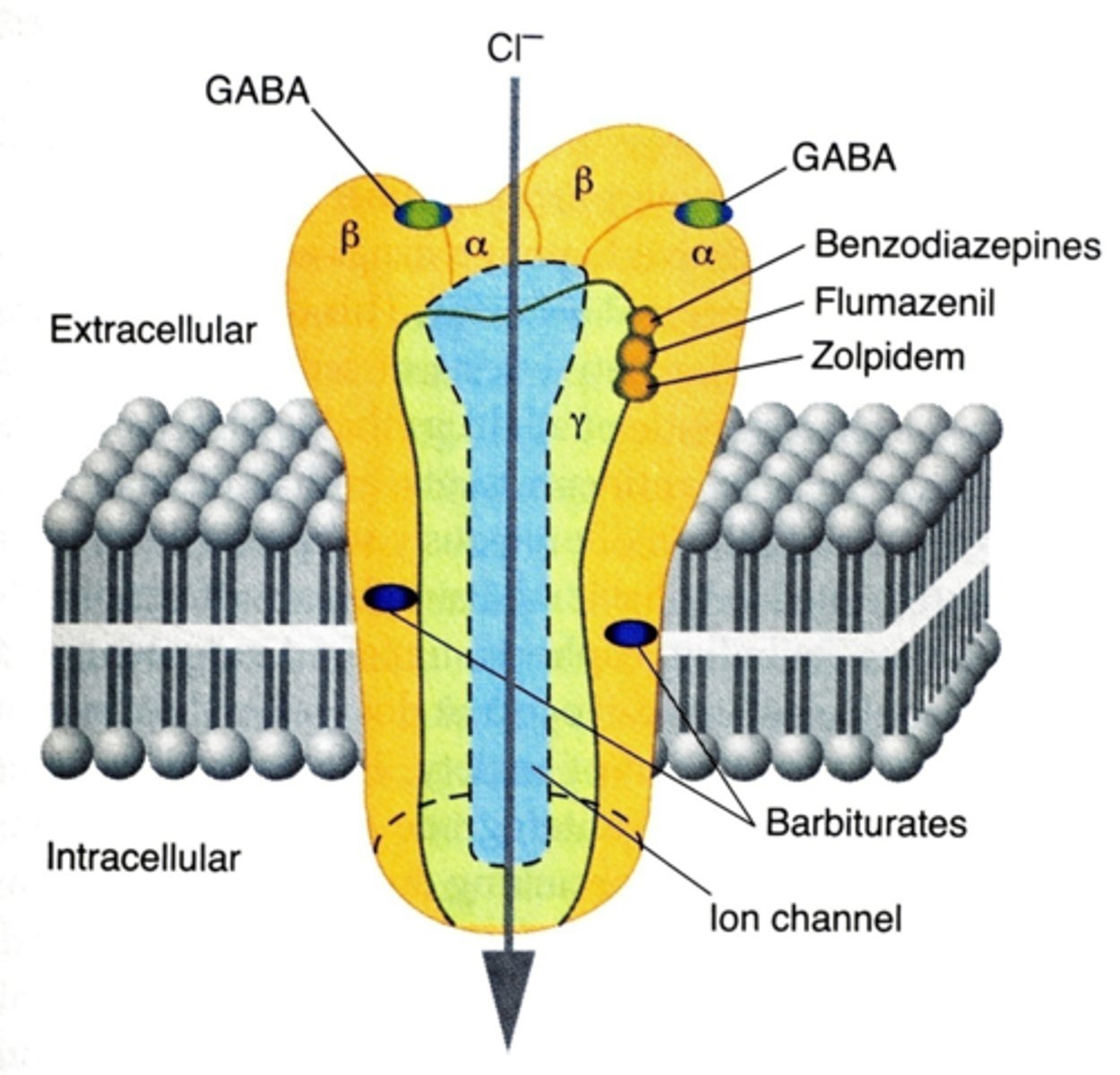
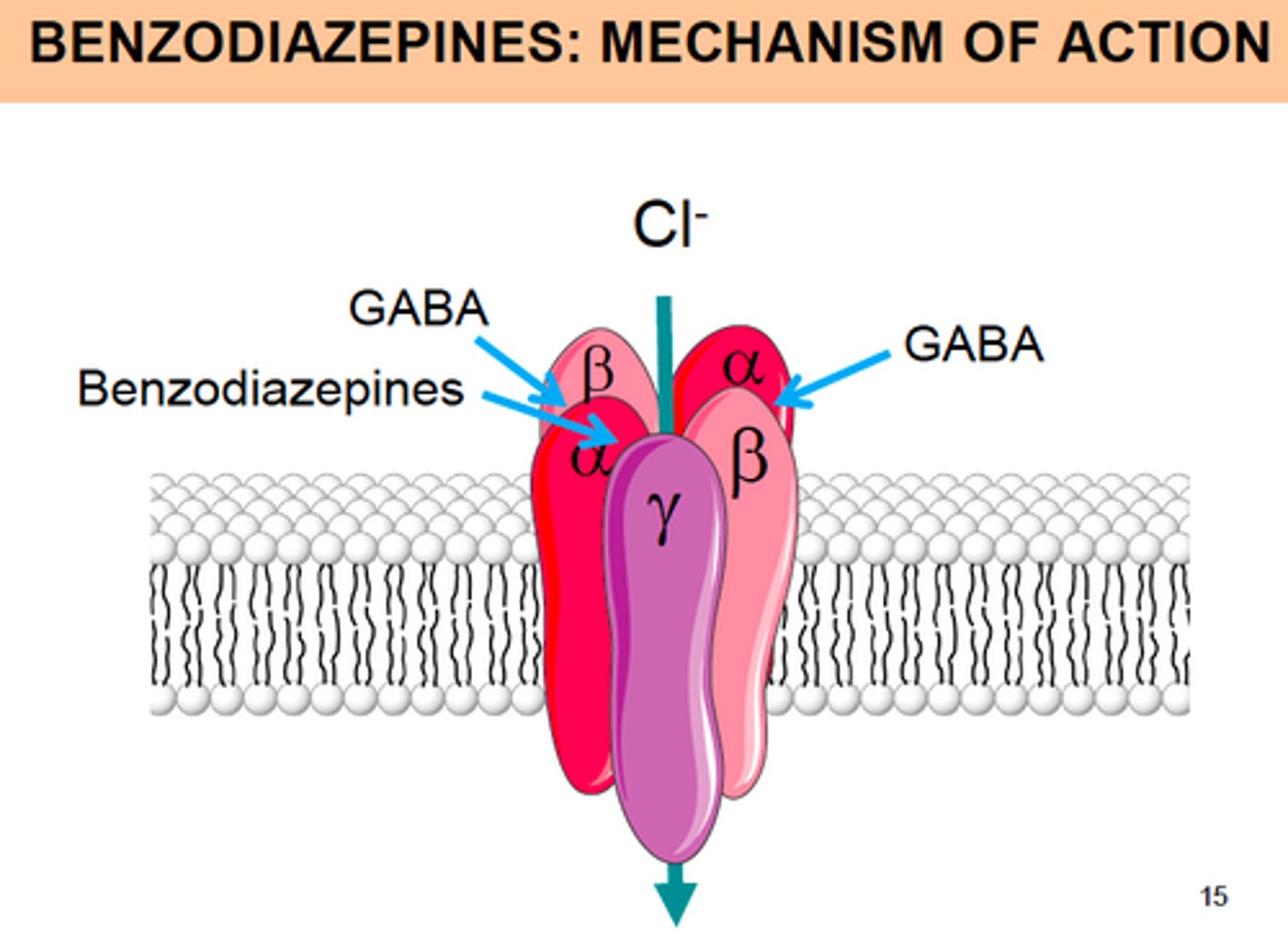
Where do benzodiazepines bind?
An allosteric site on GABA-a receptor.
It is between the alpha and gamma subunit (alpha gamma interface)
What are the different types of benzodiazepines?
1. Benzodiazepine agonist
2. Benzodiazepine antagonist
3. Benzodiazepine inverse agonist
What is a benzodiazepine agonist?
It is a positive allosteric modulator.
Benzodiazepines which increase the flow of Cl- through the GAGA-a receptor. This increases the inhibitory effect of GABA channel.
Benzodiazepines agonists have 100% intrinsic efficacy.
What is a benzodiazepine antagonist?
Benzodiazepines which stops the flow of Cl- through the GAGA-a receptor.
These do not activate the receptor.
Benzodiazepines agonists have 0% intrinsic efficacy.
What is a benzodiazepine inverse agonist?
It is a negative allosteric modulation. These reduce the flow of Cl- through the GABA-a channel. This decreases the inhibitory effect of GABA channel.
What is the mechanism of action of benzodiazepines?
They are positive allosteric modulators. They increase the flow of Cl- through the GABA-a channel.
They are benzodiazepine agonists.
Describe the structure of benzodiazepines
There is a benzene ring which has different R groups attached to it.
What do the R groups of the benzene ring control?
1. The infinity of the benzodiazepine to bind the receptor
2. The intrinsic efficacy of benzodiazepine to produce a functional effect
Give examples of benzodiazepines
Diazepam
Flunitrazepam
Clonazepam
Midazolam (partial agonist)
What is the role of midazolam?
It is used as a pre-operation sedative
What is the use of negative allosteric modulators of the GABA-a receptor?
They are used for seizure generation models.
They turn down inhibition through the GABA channel, meaning there is increased excitation.
Examples include beta carboline compounds.
What is rohypnol?
The date rape drug
It is benzodiazepine agonist.
It is particularly dangerous as it can be "undetectable" as it is colourless and odourless
What are some negative effects of benzodiazepines?
- Memory loss (but can be useful in pre-op e.g. midazolam)
- Sedation (e.g. date rape drug)
- Could have abuse potential (some people develop tolerance or physical dependence with long term use of benzodiazepines)
- Could be addictive
- Withdrawal symptoms
Give examples of benzodiazepine withdrawal symptoms
- Irritability
- Cognitive impairment
- Insomnia
- Dysphoria
- Hypersensitive to light/sound
How long should people be on benzodiazepines?
It should be a short term treatment.
It should be given for maximum 2 weeks.
This is due to its withdrawal effects
Give examples of anxiolytic benzodiazepines
Diazepam, lorazepam
Give examples of hypnotic benzodiazepines
Nitrazepam, flurazepam, temazepam
What are the different sub-classes of benzodiazepines?
1. 2-keto drugs
2. 3-OH drugs
3. Triazolo drugs
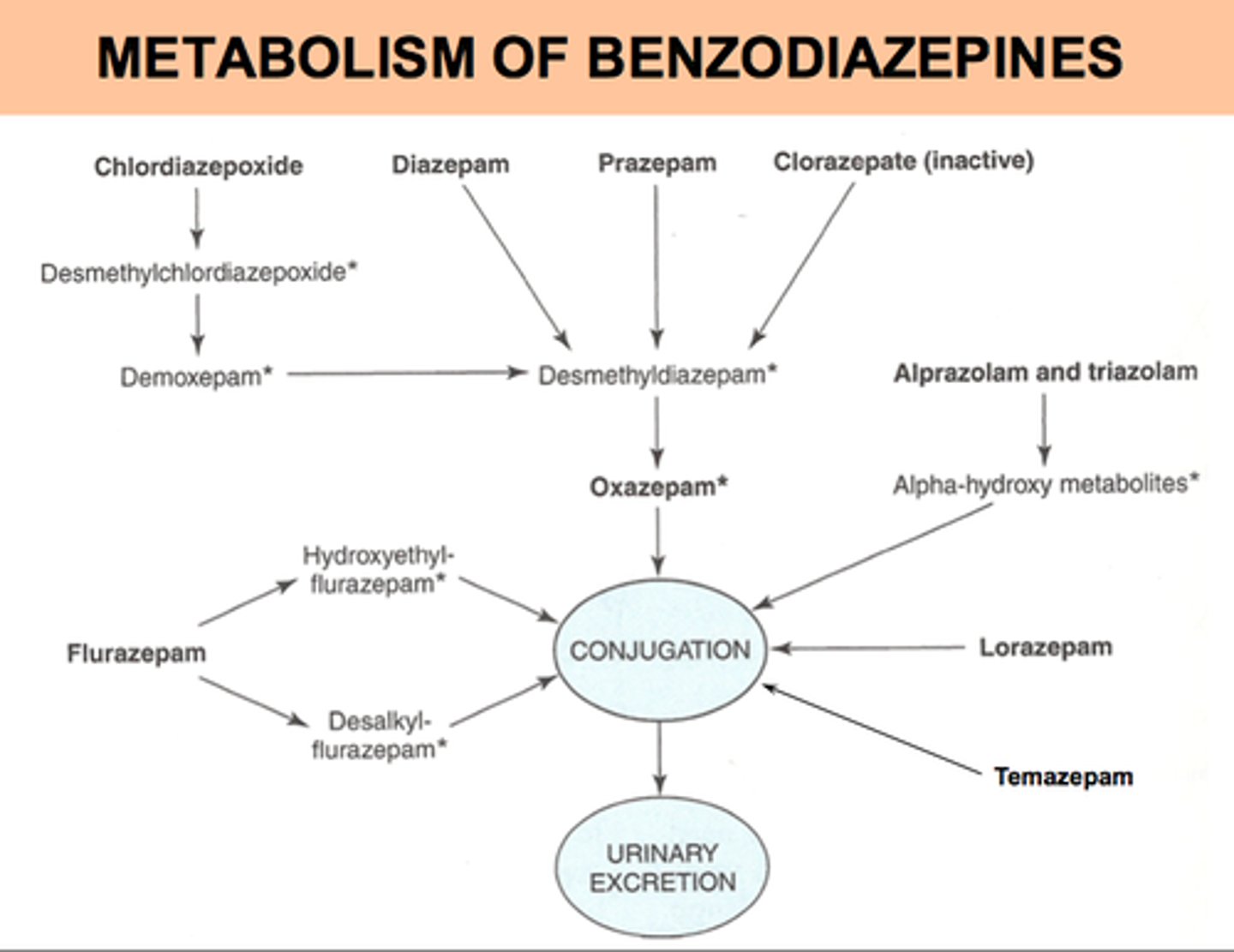
Describe metabolism and half-life of benzodiazepines
- 2-keto drugs are oxidised in the liver and has active metabolites which increase its half life. Diazepam has a long half-life (40 hours). Therefore, it has more CNS depression.
- 3-hydroxy groups have a shorter half-life e.g. lorazepam around 14 hour half-life. It is glucuronidated.
- Triazolo drugs are oxidised and have a shorter half-life.
With a shorter half-life, the drug is cleared quicker so patients do not have "hangover" or withdrawal symptoms the next day.
Give examples of 2-keto benzodiazepines
Diazepam, chlordiazepoxide, clorazepate
Give examples of 2-hydroxy benzodiazepines
Lorazepam, oxazepam
Give an example of triazolo benzodiazepine
Alprazolam
What are the first choice benzodiazepines?
Alprazolam and lorazepam
How should benzodiazepines be stopped?
They should be tapered off.
What is a benefit of newer benzodiazepines?
They are safer in overdose compared to barbiturates
What are side effects of benzodiazepine overdose?
Sedation, ataxia (poor muscle control), slurred speech
Why shouldn't alcohol be taken with benzodiazepines?
Alcohol is a depressant.
It Is an allosteric modulator of GABA. It is a positive allosteric modulator. Consequently, it has an additive effect and increases inhibitory effects of GABA-a receptor.
It interacts with dopamine, opioid and 5-HT receptors as well.