Endocrine Glands
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
51 Terms
Characteristics of Endocrine Glands.
→ release hormones into the blood via their secretory cells
have no secretory ducts
found in gut, thymus, heart, kidneys, testis & ovaries
What is the origin of Endocrine cells?
Epithelial
organized into cords or clusters
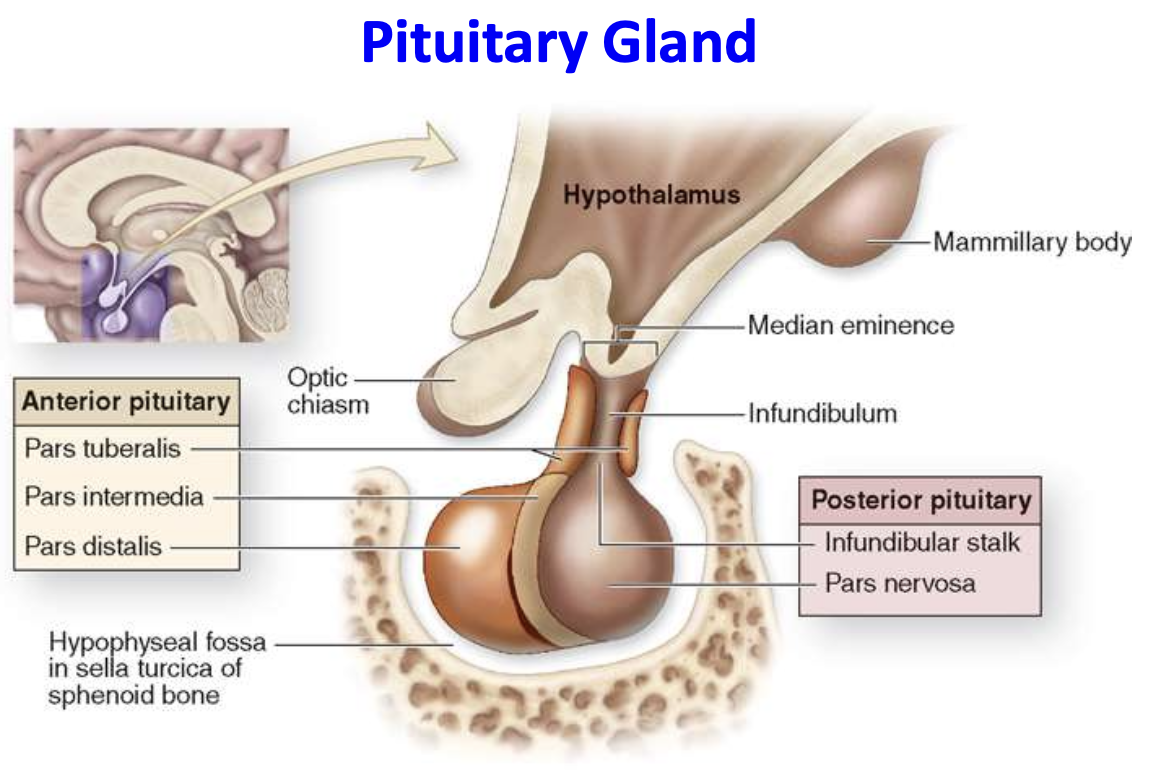
Parts of the Pituitary gland.
1) Posterior (neurohypophysis) - made of nervosa
directly attached to the hypothalamus via infundibular stalk
2) Anterior (adenohypophysis) - made of glandular pars tuberalis, intermedia, distalis
Where is the pituitary gland located?
fossa of sella turcica (part of sphenoid bone)
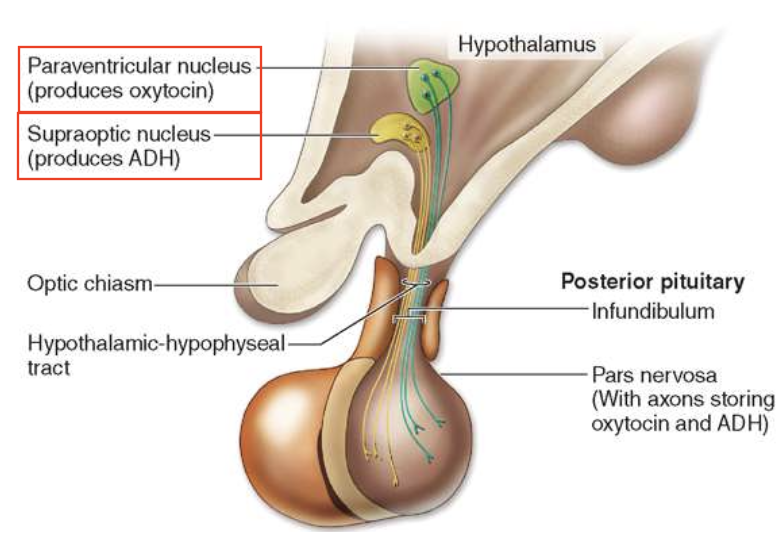
Describe the course of the Hypothalamic-Hypophyseal Tract. What do axons of this tract carry?
1) Axons extend from the hypothalamic supraoptic & paraventricular nuclei (PVN)
carry peptide hormones
PVN = oxytocin
supraoptic = ADH/vassopressin
2) Course through the infundibulum
3) Enter pars nervosa of the posterior pituitary
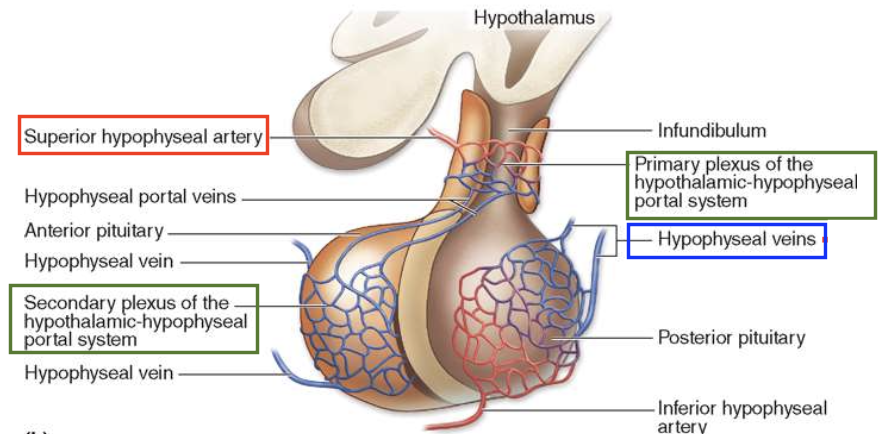
Describe Hypothalamic-Hypophyseal portal system.
Blood from the superior hypophyseal artery has 2 capillary networks:
Primary plexus - surrounds the infundibulum & median eminence
Second plexus - found throughout the pars distalis
→ Networks are connected by hypophyseal portal vein
What are the Parenchymal cells of the pars distalis are subdivided into?
1) Acidophils
2) Basophils
3) Chromophobes (poorly stained cytoplasm)
How are cords of acidophils and basophils arranged in the pars distalis?
distribution and number vary by region
closely associated with the second capillary plexus
What do the cytoplasms of all chromophil (somatotropic) cells have?
well-developed Golgi
euchromatic nuclei
cytoplasm (filled with secretory granules)
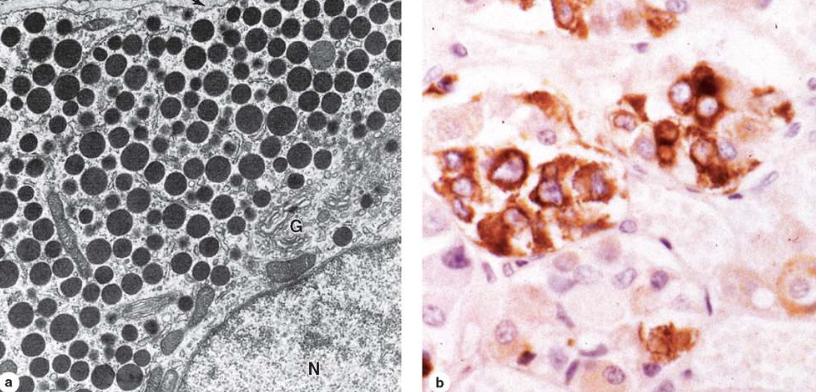
How are specific chromophils best identified?
Immunohistochemistry — with antibodies against their hormone products
1er antibody that binds to the protein of interest
2er binds to 1er and becomes fluorescent
List the 6 major tropic hormones the Anterior Pituitary secretes. What part of Anterior Pituitary secretes this?
Pars distalis secretes:
TSH
FSH
LH
GH
ACTH
Prolactin
How is the release of anterior pituitary (pars distalis) hormones regulated?
by hypothalamic factors carried by the hypothalamic-hypophyseal blood supply
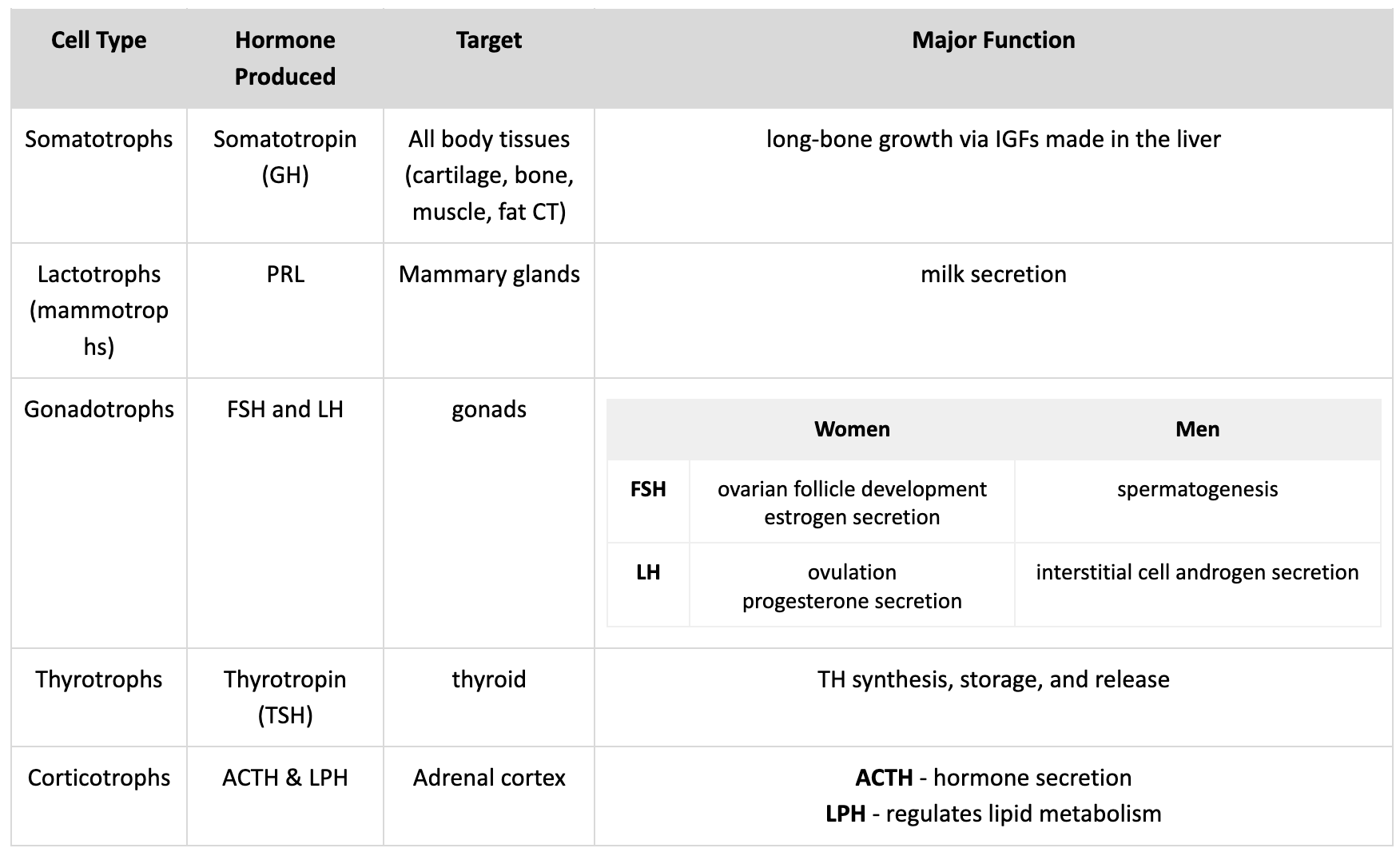
For the Anterior Pituitary, list the:
Cell types
Major hormones produced
Target
Function
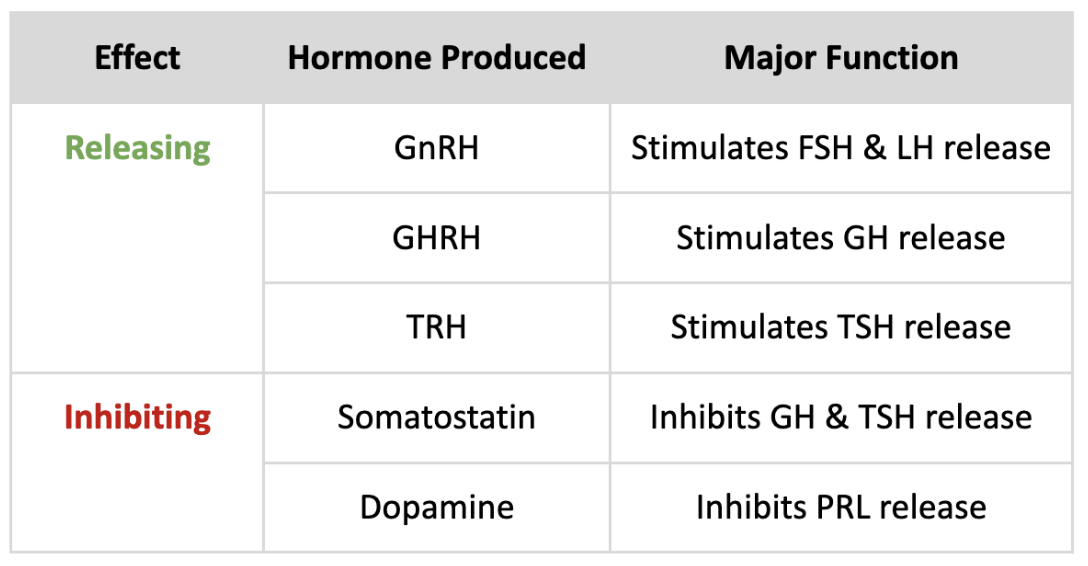
For the Hypothalamus, list the:
Major hormones produced
Effect on Anterior Pituitary hormones
(-) feedback loops affecting anterior pituitary secretion
Stimulus (e.g., ↓ body temp) causes the hypothalamus to secrete TRH
Thyrotropic cells in the anterior pituitary release TSH
TSH stimulates follicular cells of the thyroid gland to release TH
TH stimulates target cells to ↑ metabolic activities → ↑ body temp
Hypothalamus detects ↑ body temp and inhibits TRH secretion
TH also blocks TRH receptors on the thyrotropic cells→ inhibiting TSH synthesis and release
All this dampens TH production in thyroid
Characteristics of Pars Intermedia (anterior pituitary).
between pars distalis (PD) and pars nervosa (PN)
some of its basophilic cells can invade PN
contains remnants of the embryonic hypophyseal pouch which appear as “colloid-filled cysts” of diff size
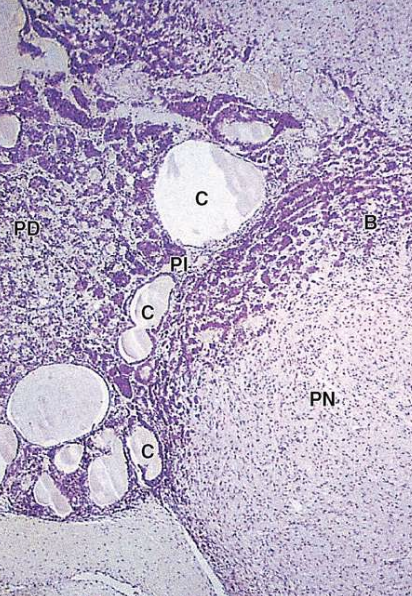
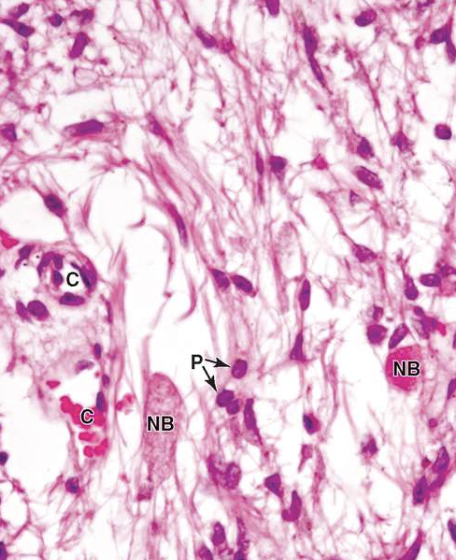
Characteristics of Pars Nervosa (posterior pituitary).
- has modified neural tissues containing unmyelinated axons
axons are supported/covered by pituicytes (glia cells)
axons run from the supraoptic and PVN
- has swellings - “neurosecretory (Herring) bodies”
oxytocin or vasopressin is released from Herring bodies upon neural stimulation
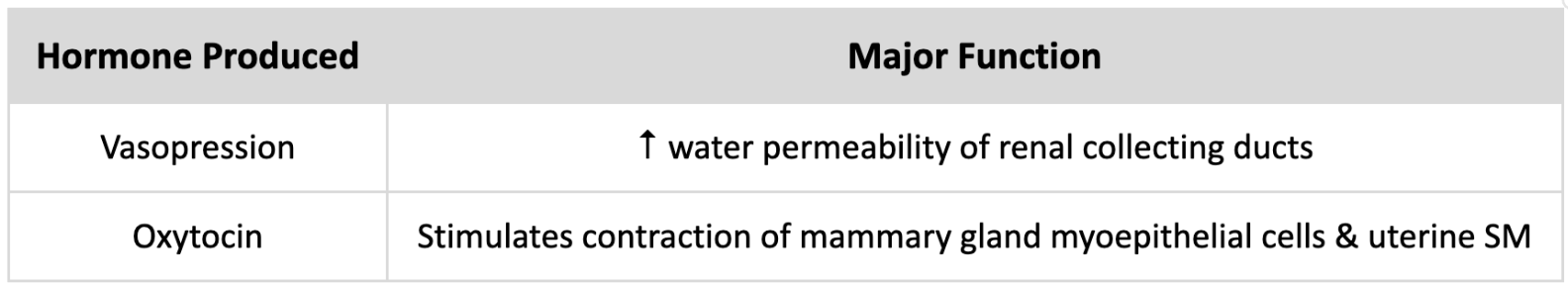
For the Posterior Pituitary, list the hormones it releases and functions. Note: It doesn’t PRODUCE these hormones.
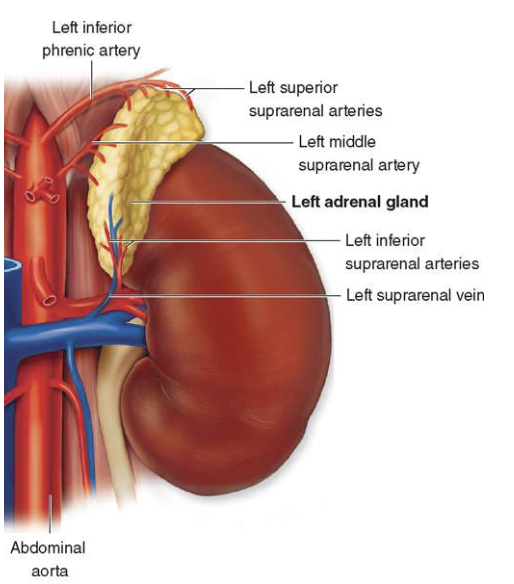
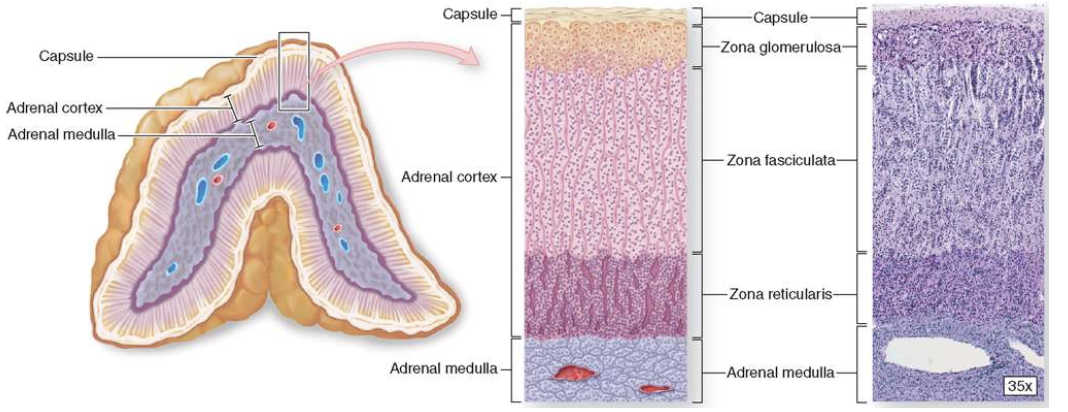
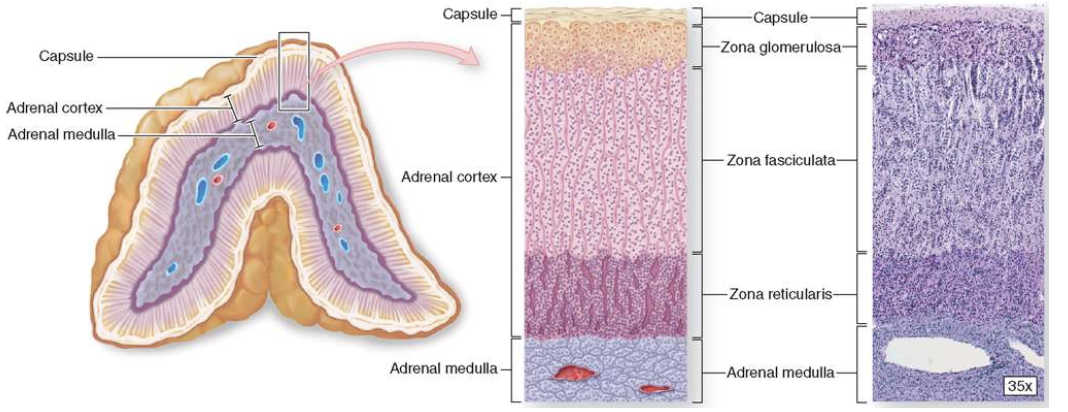
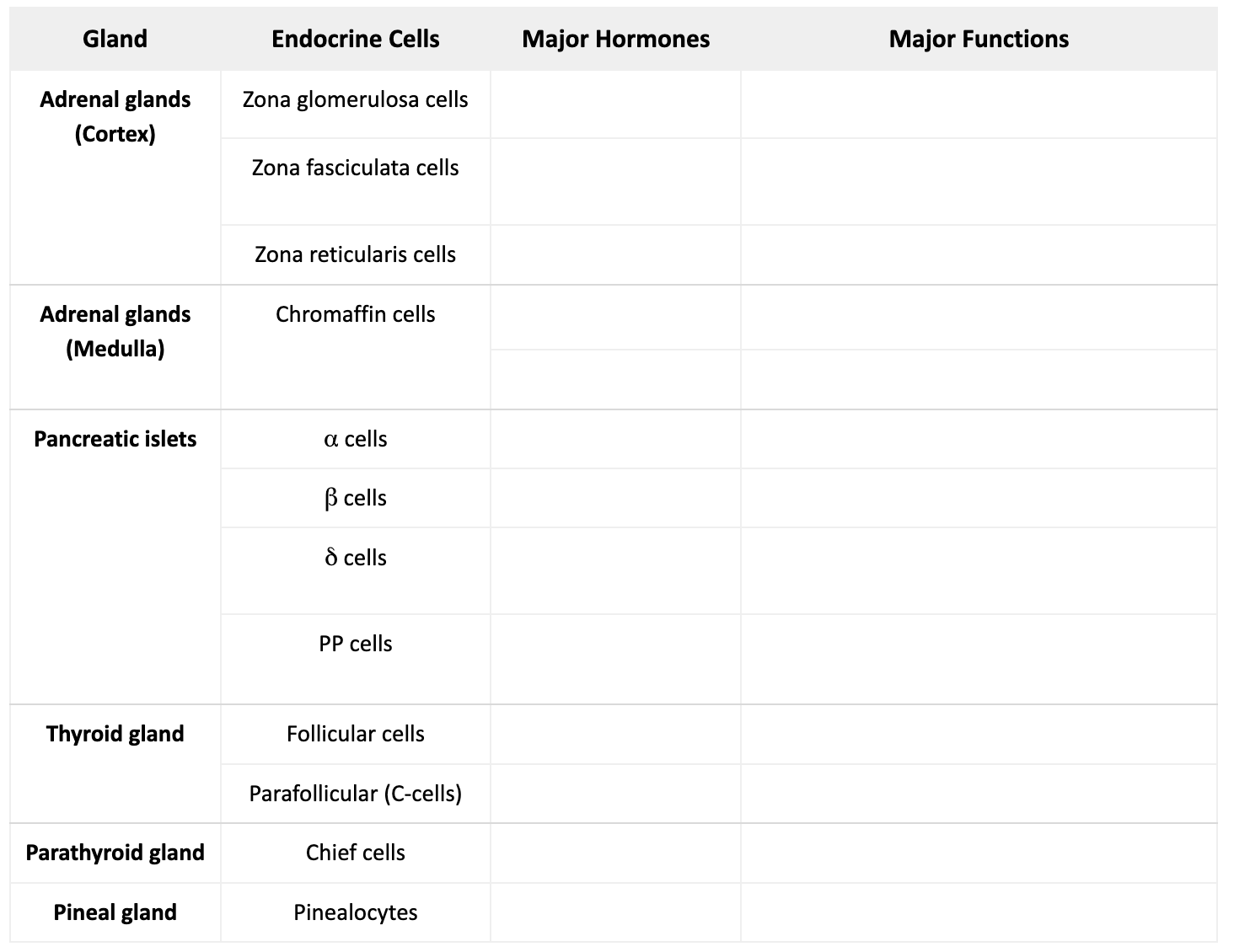
What does each Adrenal gland consist of?
Outer cortex
Inner medulla
Characteristics of Adrenal Cortex. (Hint: Mention function, origin and location)
Function: make steroid hormones
Origin: mesoderm
Location: lies inside the capsule and surrounds the innermost adrenal medulla
Characteristics of Adrenalocytes (Adrenal Cortex cells).
Lipid droplets/cholesterol esters (steroid hormone pre-cursors)
lots of SER for steroid hormone synthesis
Mitochondria with tubular and vesicular cristae
has Autophagosomes which remove mitochondria and SER during periods of inactivity in steroid synthesis
Euchromatic nuclei (indicates active transcription)
has Golgi, RER, and lysosomes
The steroid-secreting cells of the adrenal cortex are arranged into 3 concentric layers. What are they?
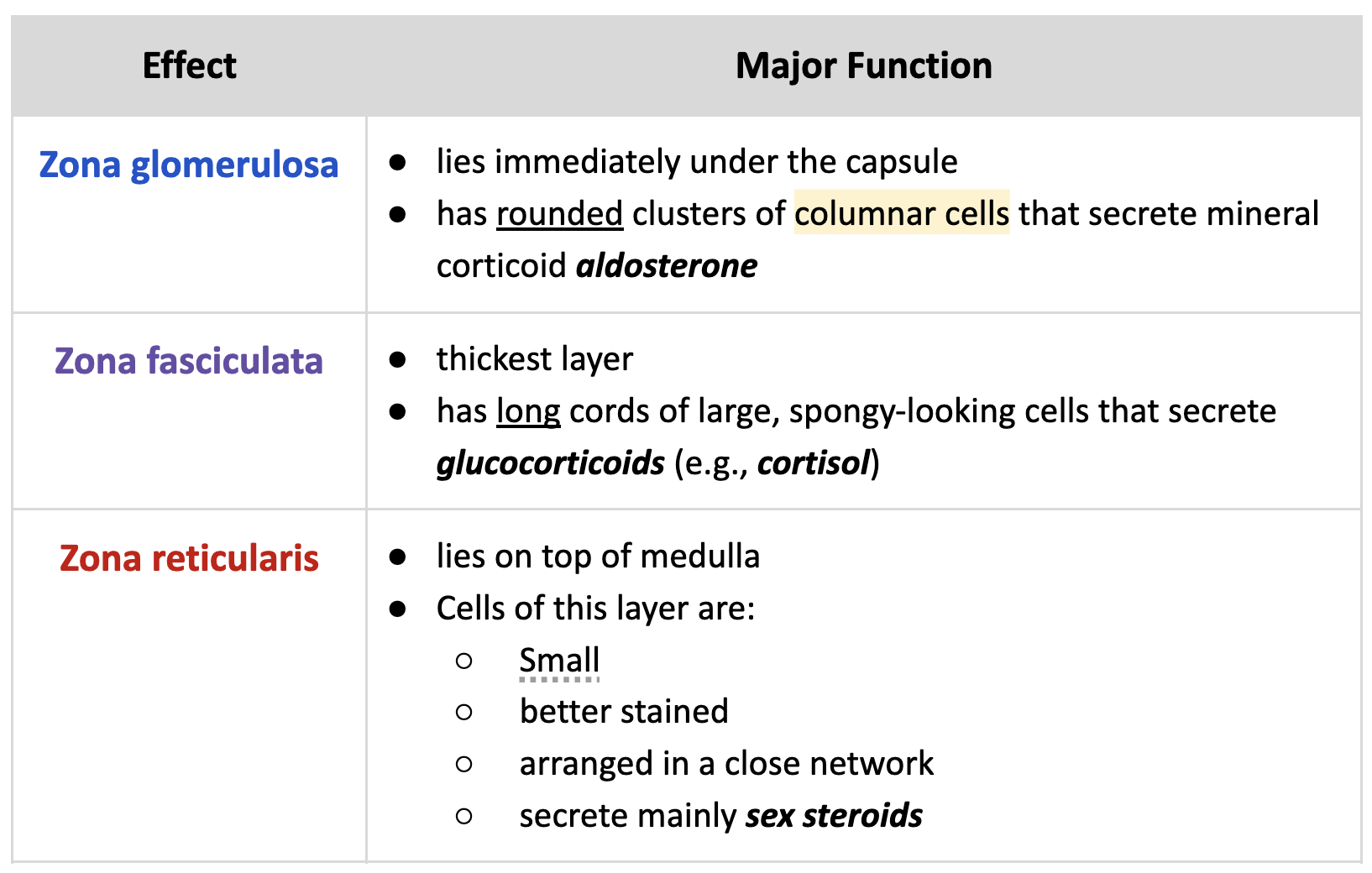
Characteristics of Medulla. (Hint: Mention function and location)
Function: makes Eph and NE via chromaffin cells
Origin: Embryonic neural crest cells
What are the characteristics of cells in the adrenal medulla (chromaffin cells)?
look like SNS neurons
large, pale-staining cells with cytoplasmic granules
arranged in cords interspersed with wide capillaries for vascularization
How are the NE cells vs Eph cells different?
NE cells are more e- dense than Eph cells due to chromogranins binding the catecholamines
What are adrenal glands (cortex & medulla) supplied and vascularized with?
Supply: suprarenal artery and vein
Vascularized: fenestrated sinusoidal capillaries
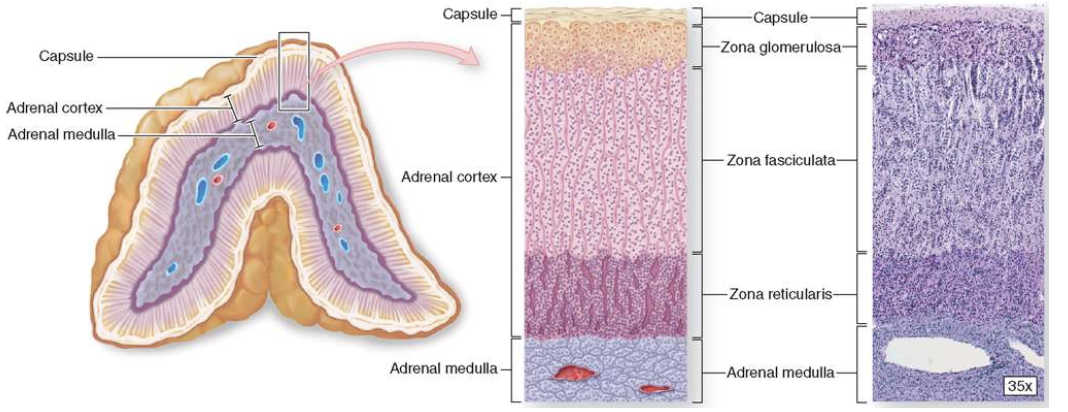
Characteristics of Pancreatic Islets (Islets of Langerhans).
→ clumped masses of pale-staining endocrine cells embedded in the exocrine acinar tissue of the pancreas
Note: Pancreas has 2 regions (exocrine and endocrine)
exocrine portion surrounds the islets
Describe the vascular system in the Islets of Langerhans.
Arterioles enter each islet → branch into fenestrated capillaries (allows communication b/w islets)
Capillaries merge and exit the islet as efferent capillaries
This vascular system allow islet hormones to regulate the secretion of neighboring islet cells and acini
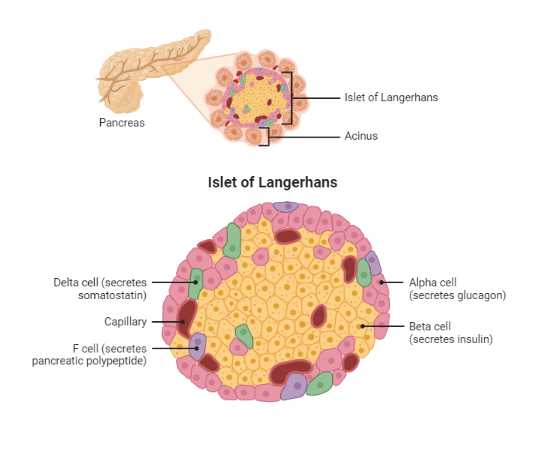
What does the modified aldehyde fuchsin stain reveal about the cells in the Islets of Langerhans?
Peripheral α cells stain deep brownish purple
Central β cells stain brownish orange
Reticulin CT along the islet capsule & capillaries stains green
List the 4 main islet cells.
α cells
β cells
δ cells
PP cells
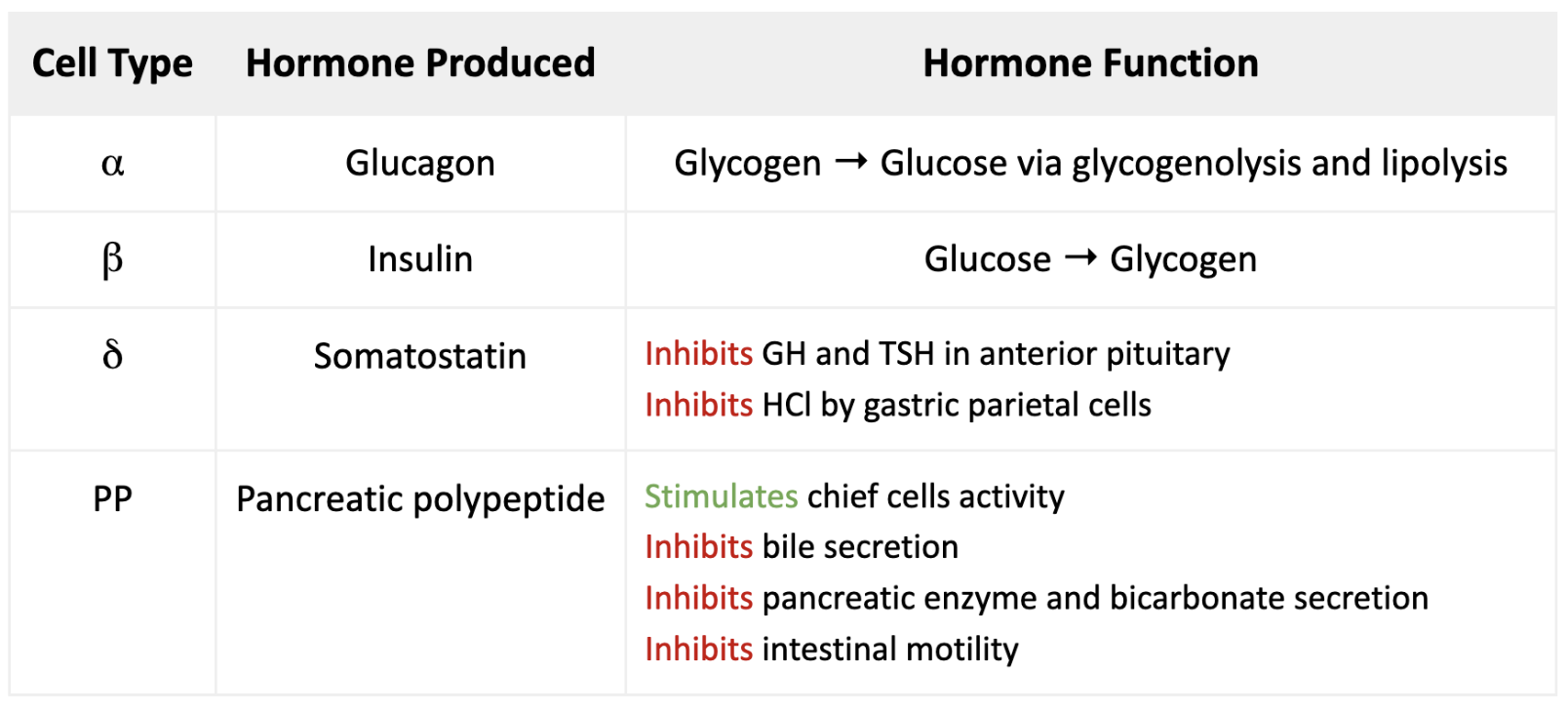
What hormone does each islet cell produce? What’s the function of these hormones?
Characteristics of Thyroid gland.
butterfly shaped
has a thin capsule
highly vascular
has a septa which allows larger blood vessels, lymphatics, and nerves to enter the gland
its parenchyma has diff colloid-filled epithelial follicles of various sizes
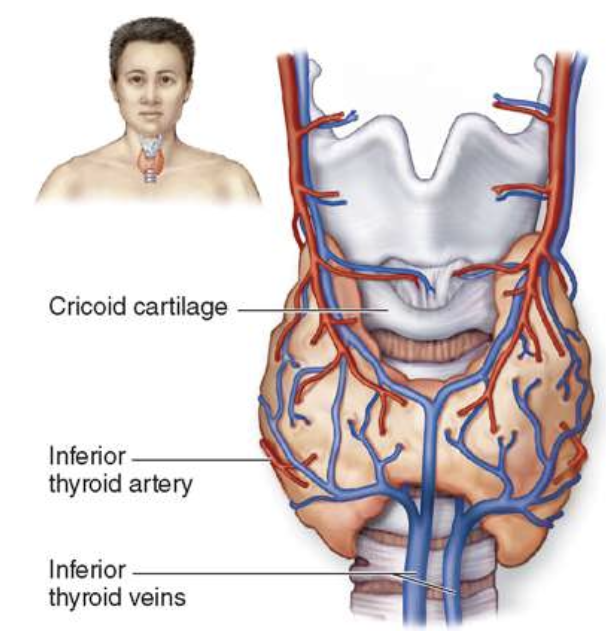
List the 2 anatomical landmarks of the Thyroid gland.
Surrounds the anterior surface of the trachea
Located just below the larynx
Characteristics of Thyrocytes (T-cells).
small
darker
secrete thyroglobulin into the colloid of follicle cells via their microvilli and pseudopodia
Characteristics of Thyroid Follicular Cells (thyrocytes).
→ secrete thyroglobulins (precursors for T3 and T4)
form a single layer of cells around the filled with colloid (gel), which mainly contains “thyroglobulin”
cell height - squamous to low columnar

Characteristics of Parafollicular Cells (C-cells).
→ pale and larger cells that secrete calcitonin
cytoplasm contains secretory granules (with calcitonin) and a large Golgi
Found:
as individual cells or clusters outside the follicles
inside the BM of the follicle, but don’t contact the colloid in the lumen

Characteristics of Parathyroid gland.
→ 4 small nodules embedded in the capsule on the posterior surface of the thyroid gland
nodules are divided into lobes via septa (check image)
has densely packed cords of small, functional principal/chief cells which secrete PTH
What do the principal cells of the parathyroid gland have?
Round central nuclei
Pale-staining cytoplasm
What happens to the Parathyroid as it ages?
Older glands: larger, acidophilic, and nonfunctional oxyphil cells
oxyphil cells may occur singly or in clumps of varying sizes as the gland ages
Young glands: mainly functional principal cells
How does PTH and Calcitronin compare?
PTH = ↑ blood Ca2+ levels
Calcitonin = ↓ blood Ca2+ levels
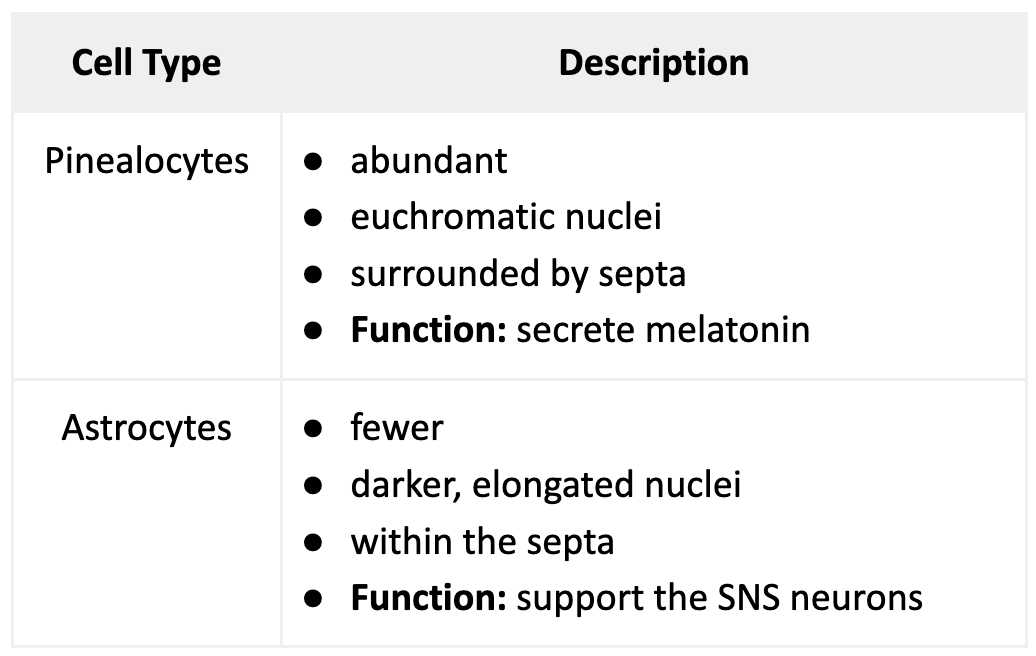
Characteristics of the cells found in the Pineal gland.
What marks the presence of the Pineal gland?
extracellular mineral deposit called “Corpus arenaceum”
Describe the pathway of Melatonin release.
When it’s dark the photoreceptive neurons indirectly send signals to the unmyelinated SNS neurons
SNS neurons run along the pineal septa and transmit the signal to the pinealocytes
Pinealocytes secrete melatonin
What do levels of the circulating melatonin determine?
Diurnal rhythms of hormone release
Physiologic activities throughout the body
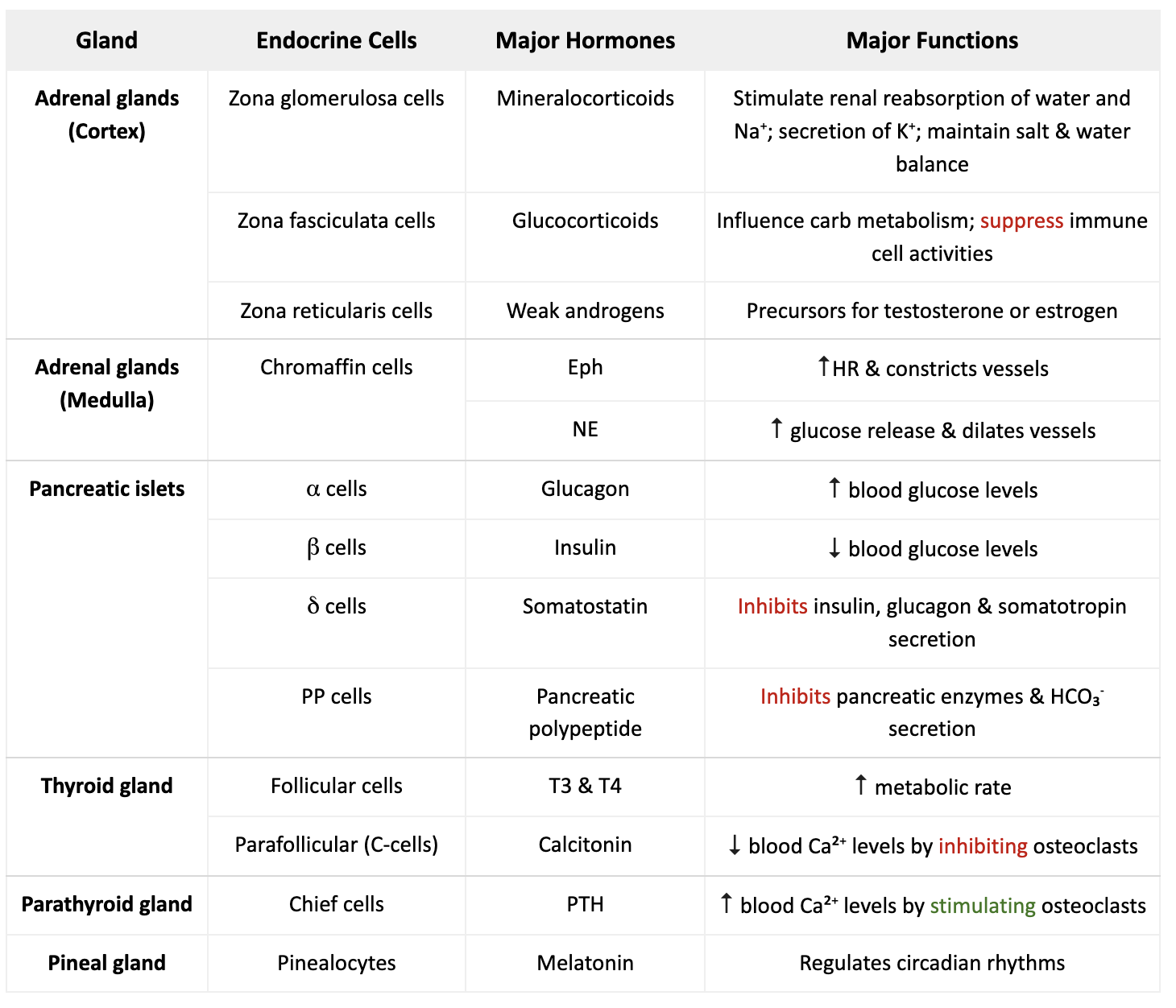
Fill out this table.
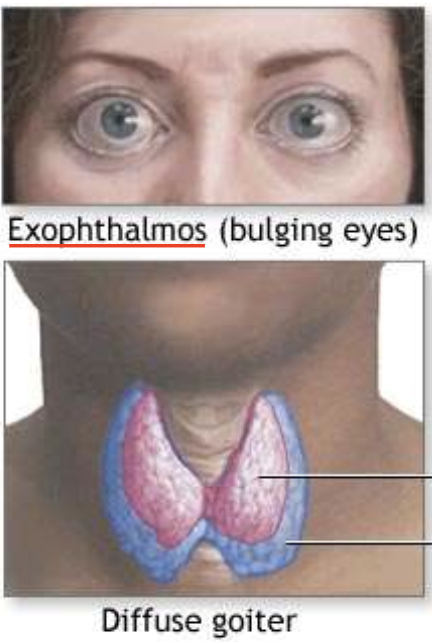
What is Hyperthyroidism?
→ too much thyroid production causing enlarged thyroid (diffuse goiter)
common cause = Grave’s disease
Symptoms: exophthalmus (bulging eyes)
What is T2D characterized by?
→ lack of sensitivity of target organs to insulin
body releases normal or high insulin, but insulin receptors don’t respond → insulin resistance
over time β-cell mass declines → ↓ insulin secretion
What is T2D mainly influenced by?
Genetics
Aging
Obesity
↓ insulin sensitivity
What is the major underlying defect of T2D?
Obesity
List 4 classic signs in a patient with diabetes for over 10 yrs.
Retinopathy
Neuropathy
Nephropathy
Cataracts