B6 CM repro Exam 5 (THE END)
1/346
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
347 Terms
primary infertility
•12 months of unprotected intercourse without successful pregnancy in women less than 35 years old
•6 months if over age 35
•Or need for 3rd party donor gametes
secondary infertility
infertility in woman who has given birth to a child
Fecundability
The probability of achieving pregnancy in one menstrual cycle
fecundity
the probability of achieving a live birth in one menstrual cycle
pre-testicular causes, testicular causes, post-testicular causes, sperm related factors
(foreman, factory, freeway)
male factors that may cause infertility
hypogonadotropic hypogonadism
endocrine disorder contributing to male infertility
primary testicular defects in spermatogenesis: hydrocele, varicocele
most common cause of male infertility
•testosterone (total and bioavailable)
•FSH and LH
•Estradiol, TSH, Prolactin
endocrine testing in assessment of male infertility
-pt has 2-5 days of ejaculatory abstinence, collect by masturbation at the office
-it needs to brought to lab within an hour
-two samples may be necessary due to inherent variability of spermatogenesis
how do you perform a semen analysis?
•Volume
•pH
•Concentration, count, motility and morphology
•Debris and agglutination
•Leukocyte count
•Immature germ cells
what do you look for in a semen analysis?
lower reference 1.5
what is a normal semen volume?
40%
reference range of total sperm motility?
Conc x volume x motility
how do you calculate sperm total motile count?
good
total motile count >40M is
10-40 M
what total motile count results in need for intrauterine insemination
<10 M
what total motile count results in need for IVF to obtain pregnancy?
•Quality / Quantity
•Menstrual cyclicity aka Ovulation
•General health / metabolism / preconception prep
egg abnormalities that may cause female infertility
•Fibroids / polyps / adhesions
•Anomalies
•Fallopian Tubes
•Endometriosis?
uterus abnormallites that may cause female infertility
age
30% until age 30
10% at 40
quality of eggs is based soley on
Unpredictable, variable, independent of age sometimes
-usually starts to drops off significantly at 37 y/o
what determines quantity of eggs?
ovulation induction
fertility method used to grow an egg
trigger shot
fertility method used to ovulate an egg
luteal support
fertility method used to implant an embryo
-hypergonadotropic hypogonadism ( menopause)
-eugonadotropic eugonadism (PCOS)
-hypo hypo ( athlete triad)
what are the 3 categories of ovulatory dysfunction
-previous cervical trauma via surgery can effect fertility, but less of a concern the more we learn
how does cervix factor into female fertility?
-hx of pelvic inflammatory disease
-endometriosis
-previous abdominal-pelvic surgery that may lead to pelvic adhesive disease
tubal abnormalities that may lead to female infertility
aneuploidy (meiotic nondysjunction)
most common cause of miscarriage
Anti-phospholipid syndrome
most common autoimmune cause of miscarriage
•Day 3 FSH and estradiol / Anti Müllerian hormone
•luteal phase progesterone levels to assess ovulatory function
•Thyroid stimulating hormone, Prolactin
•STI Screening
lab testing work up for female infertility
-treat underlying disorder!
ex: manage weight, tx hypothyroidism, tx hyperprolacinemia
best treatment for ovulatory disoredrs
clomiphene citrate
letrozole
metformin
drugs to treat ovulatory disorders by providing ovulation induction
clomiphene citrate
•Drug to tx ovulatory disorders
-Selective estrogen receptor modulator that competes for estrogen receptors at the hypothalamus and pituitary level
•Increases gonadotropin production from pituitary thus stimulates follicle production at the ovary
•Increased risk of twins, cysts, menopausal symptoms
pts with migraines with aura
contraindication of clomiphene citrate
letrozole
Rx for ovulatory disorders
-aromatase inhibitor to decrease peripheral estrogen
intrauterine insemination
in vitro fertilization
types of assisted reproductive technology (ART)
-assess for aneuploidy, monogenic disease, structural rearrangements (AMSR)
components of pre-implantation genetic screening (PGT)
premenstrual syndrome
A group of physical , mood related and behavioral changes that occur in a regular, cyclic relationship to the luteal phase of the menstrual cycle
•Interfere with some aspect of the patient's life.
-at least one affective and one somatic symptom
-has an identifiable dysfunction in social or economic performance
diagnostic criteria of pre-menstrual syndrome
•Depression
•Angry outbursts
•Irritability
•Anxiety
•Confusion
•Social withdrawal
affective behavioral symptoms of PMS
•Breast tenderness
•Abdominal Bloating
•Fatigue
•Headache
•Swelling of extremities
somatic symptoms of PMS
-mental disorder related to menstrual cycle
-specific set of at least 5 out of 11 possible symptoms with at least 1 core symptom
diagnostic criteria of premenstrual dysphoric disorder
luteal phase
during what menstrual phase does premenstrual dysphoric disorder symptoms occur?
•Mood swings, sudden sadness, increased sensitivity to rejection
•Anger, irritability
•Sense of hopelessness, depressed mood, self-critical thoughts
•Tension, anxiety, feeling on edge
list the core symptom options of premenstrual dysphoric disorder
•Aerobic exercise
•Stress reduction
•Calcium carbonate supplementation
•Magnesium supplementation
non-pharm treatments for PMDD
-NSAIDs
-ovulation suppression
-SSRI
Rx options for PMDD
•Combination oral contraceptive pills
•Drospirenone and ethinyl estradiol
ovulation suppression meds for PMDD
-increased risk of substance abuse, smoking
-decreased likelihood of attending prenatal visits
-chronic depression and/or anxiety
-increased complications of pregnancy
impacts of mood disorders on birthing pt
-increased likelihood of low birth weight and pre-term birth
-poor attachment to birthing person or primary caregiver
-increased dysregulation, irritability, crying, hypervigilance, low activity or tone
-increased level of stress hormones, including cortisol
impacts of maternal mood disorders on fetus
perinatal depression
the most common complication of childbirth
Anxiety Disorders
Life stress
History of depression
Lack of social or family support
Unintended pregnancy
Lower socioeconomic status
Lower educational level
Smoking and other substance use/abuse
Poor relationship quality
risk factors of perinatal depression during pregnancy
•Depression during pregnancy
•Anxiety during pregnancy
•Stressful life events during pregnancy or postpartum
•Traumatic or difficult birth experience
•Infant admission to NICU
•Lack of social or family support
•Previous history of depression
•Problems with breastfeeding
risk factors of perinatal depression post partum
recommended!
Grade B
USPSTF recommendation on screening for mood disorders in general adult population, including pregnant and postpartum women
ACOG recommends that clinicians screen ALL women at least once during the perinatal periodmfor symptoms of depression and anxiety using a standardized validated tool
ACOG recommendation for screening for mood disorders
Edinburgh postnatal depression scale
most common tool to screen for perinatal depression
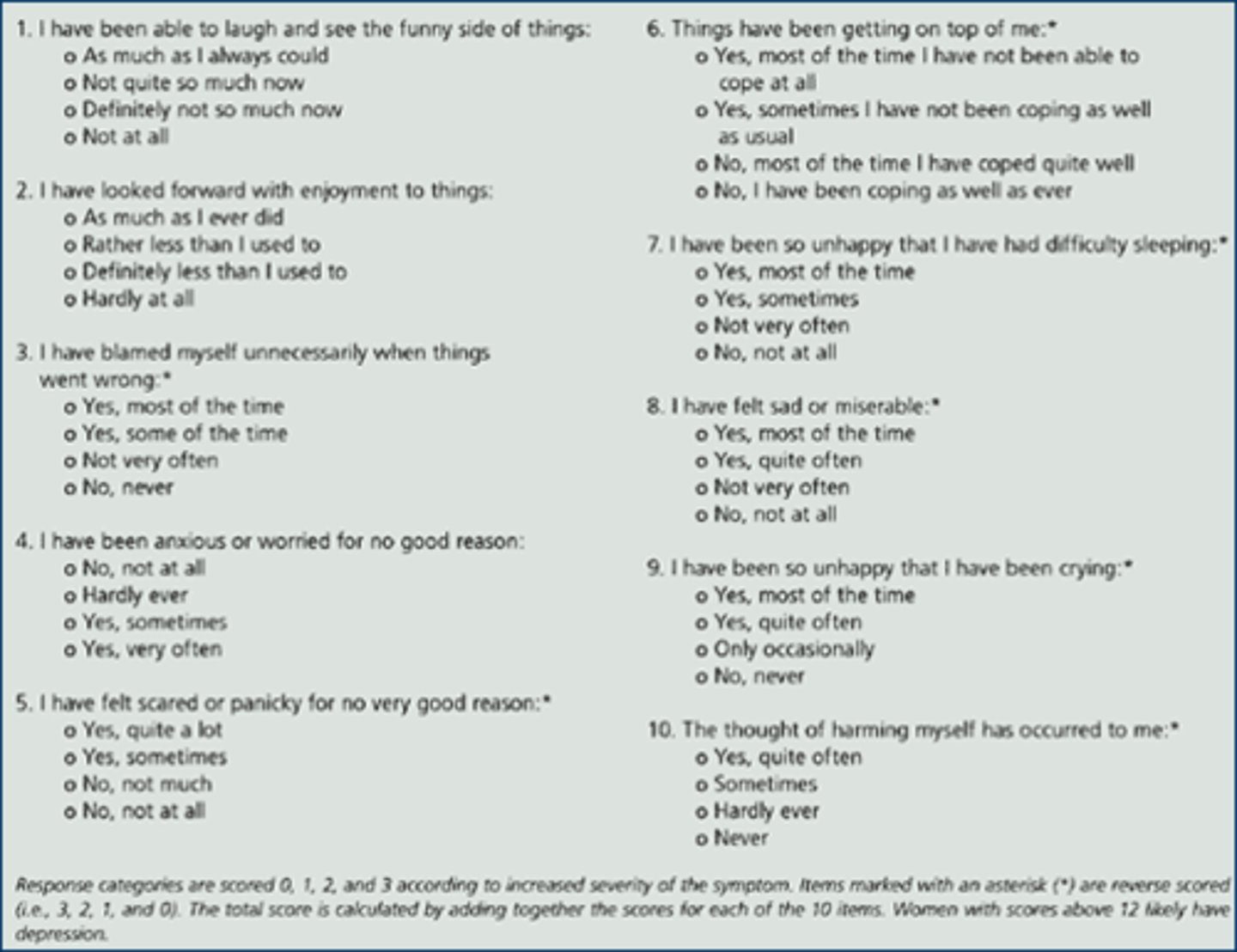
0-9= low depression symptoms
10-19= moderate depression symptoms
20-30= severe depression symptoms
score findings of EP depression scale
perinatal depression
major or minor depressive episode occuring during pregnancy or in the first 12 months after delivery
-at least 5 of listed DSM5 symptoms occuring most of the day or nearly every day
-must include depressed mood and or markedly diminished interest or ppleasure ina ll or almost all activities
criteria for major depressive episode
postpartum blues
mild transient depressive symptoms post partum
postpartum depression
depression after baby is born
postpartum psychosis
Most common in women with pre-existing disorders
•Treatment needs to occur quickly
•Can be a medical emergency
-presents 2-4 days postpartum
-resolution within 10 days
timing of postpartum blues
-presents at 2 weeks-12 months
-average duration 3-14 months
timing of postpartum depression
-presents 2-3 days postpartum
-average duration is variable
timing of postpartum psychosis
postpartum blues
postpartum symptoms: Mild insomnia, tearfulness, fatigue, irritability, poor concentration, depressed affect
postpartum depression
postpartum symptoms: Irritability, labile mood, difficulty falling asleep, phobias, anxiety symptoms worsen in the evening
postpartum psychosis
postpartum symptoms: Similar to organic brain syndrome: confusion, attention deficit, distractibility, clouded sensorium
none, self-limited
tx of postpartum blues
-personal or family hx of anxiety
-previous perinatal derpession or anxiety
-thyroid imbalance
risk factors for postpartum anxiety
postpartum OCD
post partum symptom:
•images are anxiety-based and not delusional; there is a very low likelihood that they will be acted upon
•Obsessions (intrusive thoughts or scary thoughts), which are persistent, repetitive thoughts or mental images related to the baby
•The thoughts are very upsetting and not something the person has experienced before.
postpartum OCD
postpartum symptoms:
• A sense of horror about the obsessions
• Fear of being left alone with the infant
• Hypervigilance in protecting the infant
• Those with the thoughts know their thoughts are bizarre and are very unlikely to ever act on them
•Delusions (often grandiose, but including paranoid)
•Impulsiveness, poor judgment, distractibility
•Grandiose thoughts, inflated sense of self-importance
•Severe cases: hallucinations & delusions
main symptoms of bipolar 1
-less severe than bipolar 1, no delusions
-anxiety, irritability
main symptoms of bipolar 2
usually triggered by trauma during the time leading up to, during delivery or shortly afterwards. It can effect up to 6-9 % of mothers. The trauma leaves the women feeling that either her life or the life of her baby is at risk.
PTSD following childbirth is usually triggered
3-14 days following birth
-within the 1st two weeks postpartum
when do symptoms of postpartum psychosis present?
•Rare compared to postpartum anxiety and depression
•Occurs in about every I or 2 out of 1.000 deliveries, or .1%-2% of births
prevalance of postpartum psychosis
ego-dystonic thoughts
Thoughts or impulses and behaviors that are felt to be distressing, unacceptable, or inconsistent with one's self concept.
-not indicative of psychosis
ego-syntonic thoughts
upsetting thoughts are compatible with your values and beliefs
- a sign of psychosis that should be assessed quickly
-personal or family hx of bipolar
-a previous psychotic episode -
MOST people will not harm themselves or others
risk factors of postpartum psychosis
SSRI: paroxetine, sertraline (amount secreted in breast milk is low)
initial treatment for postpartum mood disorders in breastfeeding pts
-SNRI: duloxetine, venlafaxine
-atypical antidepressant: buproprion, mirtazapine
-tricyclic: nortriptyline
treatments for postpartum mood disorders in breast feeding pts who are resistant to initial treatment
•use the general population treatment
•Start with SSRI's or restart previous therapy.
tx of postpartum mood disorders inn pts who are not breast feeding
domestic abuse (per department of justice)
felony or misdemeanor crimes of violence committed by a current or former spouse or intimate partner of the victim, by a person with whom the victim shares a child in common, by a person who is cohabitating with or has cohabitated with the victim as a spouse or intimate partner, by a person similarly situated to a spouse of the victim under the domestic or family violence laws of the jurisdiction receiving grant monies, or by any other person against an adult or youth victim who is protected from that person's acts under the domestic or family violence laws of the jurisdiction.
domestic abuse (per the state of louisiana)
the intentional use of force or violence committed by one household member or family member upon the person of another household member or family member.
psychological aggression
the use of verbal and non-verbal communication with the intent to harm another partner mentally or emotionally and/or to exert control over another partner
sexual coercioin
unwanted sexual penetration that occurs after a person iis pressured in a nonphysical way
unwanted sexual contact
unwanted sexual experiences involving touch but not sexual penetration, such as being kissed in a sexual way or having sexual body parts fonndled, groped, or grabbed
contact sexual violence
a combined measure that includes rape, beingn made to penetrate someone else, sexual coercion, and /or unwanted sexual contact
rape
being made to penetrate someone else (asked of males only)
sexual coercion
unwanted sexual contact
what are the 4 types of intimate partner violence?
unwanted sexual contact
what type of sexual violence is most common
college age women who do NOT attend college
what population of women are most likely to experience sexual violence?
college age men in college
what population of men are most likely to experience sexual violence?
of all victims under 18, 2/3 are ages 12-17
most common age range of children who are victims of sexual abuse
individual, relationships, community, societal
what are the 4 categories of risk factors for victimization
1. tensions building
2. incident
3. reconciliation
4. calm
what are the 4 components of the cycle of abuse
tensions building
what stage of abuse cycle?
-breakdown of communincation, becomes fearful and feels the need to placate abuser
-victim feels uneasy and a need to watch every move
incident
what stage of abuse cycle?
-any type of abuse occurs: physical, sexual, emotional
-threats, intimidation, blaming, arguing
reconciliation phase
what stage of abuse cycle?
-abuser apologizes for abuse, some beg forgiveness orr show sorrows
-abuser may promise it will never happen agian, blames victim for provoking the abuse or denies abuse occur
-minimizing, denying or claiming the abuse wasn't as bad as the victim claims
the calm
what stage of abuse cycle?
-before the tension starts again
-abuses slow or stop, abuser acts like the abuse never happened
-promises made during honeymoon stage may be met
-abuser gets gifts for victim
-victim believes or wants to believe the abuser will change
chronic pain, IBS, headaches, and MSK papin
somatic complaints associated with IPV
Health practitioners, including physicians, surgeons, physical therapists, dentists, residents, interns, hospital staff, podiatrists, chiropractors, nurses, nursing aides, dental hygienists, emergency medical technicians, paramedics, optometrists, medical examiners, or coroners.
who are mandatory reporters for children in the state of Louisiana?