Neuropsychology Exam 3
1/150
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
151 Terms
Three components of emotion
Behavioral – visible actions like facial expressions or body language.
Physiological – changes in the autonomic nervous system.
Experiential – internal, subjective experience and cognitive interpretation.
Behavioral
Facial expression (Paul Ekman)
Body language
Language
Our emotions are a big part of interpersonal interactions
What are Ekman’s six basic emotions?
Anger, Disgust, Fear, Surprise, Happiness, Sadness.
Physiological
Change in autonomic nervous system
Heart rate, respiration, sweating, pupil dilation — all help us respond to the environment.
Experiential - 2 aspects
Subjective quality – emotions “happen to us.”
Cognitive aspect – how we interpret, label, and regulate feelings.
James-Lange (Physiological theory)
Emotions are our “recognizing” a change in our autonomic arousal level.
We see a shark in the ocean, it causes our heart rate to climb, then we feel afraid
Cannon-Baird (Physiological theory)
Emotion feeling occurs before the physiological response.
Example: We feel fear → then HR increases.
Stage fright
Beta blockers stop physical arousal → people report less fear.
Supports James-Lange, but both theories are partially correct.
Schachter and Singer — Two factor Theory
Physiological Change
Cognitive Interpretation
Experiment
Cover Story — Vitamin (suproxin) on vision
Injected with .5cc of adrenaline or saline
2 groups
Informed - made aware of side effects > HR
Ignorant - no side effect info
Paired with angry or euphoric confederate
Measures self-report emotional state of subjects
Ignorant more intense than informed
Behavior Brain area
Patients with lesions in the brain stem (medulla) have been reported to have uncontrolled crying (behavioral emotions)
Not associated with “feeling” sad
Dissociation between brain areas that control behavior and the other components of emotion
Hypothalamus
Controls the push/pull of the autonomic nervous system
Sympathetic = action
Parasympathetic = calming
Control cardiovascular system
Regulates hormones, heart rate, breathing, sweating.
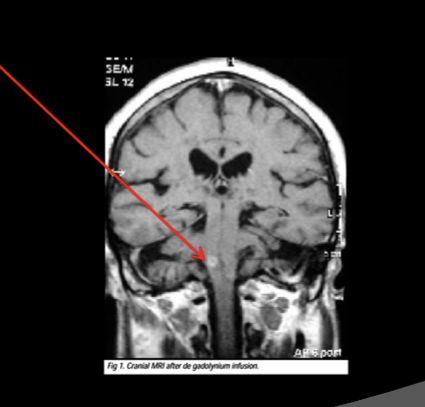
Amygdala
Made of several sub nuclei
Central nucleus
Lateral nucleus
Basal
Removal of any results in tameness
Stimulation results in fear response
Startle
Avoidance
LeDoux - Fear learning
Classical conditioning of fear response
Pair shock (UCS) with a ton (CS) and elicit freezing behavior (UCR)
Eventually CS alone elicits freezing (CR)
In some studies they recorded electrical activity from amygdala
In others they lesioned the amygdala
Fear Conditioning in Humans
Might underline anxiety disorders and PTSD
Initially neutral environment stimuli get repeatedly paired with stress producing events
Eventually these stimuli alone can cause stress response
Very resistant to extinction
Patient SM
Bilateral amygdala damage in late childhood due to Urbach-Withe disease
Rare genetic disorder
SM shows no behavioral or physiological evidence of fear
Shown fear including stimuli she only shows interest, curiosity, and excitement
Unable to reliably report or draw fearful facial expressions
Role of cortex in emotion
Interpretation of emotions
Judgements involving emotional information
Regulation of emotions
Role of cortex - laterality
RH appears to play a more important role in
LH damage results in more depression
RH damage more euphoria
RH damage
Problems judging facial expressions
Problems determining and expressing emotion in voice
A-prosodia
Problems with comprehending humor
Problems judging emotional situations (frontal lobes)
Orbitofrontal Cortex (OF)
Evidence suggests it has to do with translating personal consequences of behavior
Patiens with OF damage can verbalize consequences, but less likely to use this information
“ If I jump off the roof, I could break a leg”
Might involve connects with the anterior cingulate gyrus
Anterior cingulate involves in inhibitory control
Phineas Gage
Personality changes, less inhibited
Prefrontal Lobotomy
Jacobson’s chimp had fewer tantrums after frontal lobe removal
Moinz (neuropsychiatrist) convinced neurosurgeons to try on humans
Calmed patients and reduced compulsions
Schizophrenia
A serious mental disorder characterized by disoriented thoughts, delusions, hallucinations and other bizarre behavior.
1% of population - life long disorder
6 Schizophrenia diagnostics
Presence of critical symptoms — divided into:
Cognitive: delusions, hallucinations, thought disorder (incoherent speech)
Emotional: blunted or flat affect
Evidence of deterioration in functioning
Symptoms persist for at least 6 months
Any affective disorder must be secondary
Onset before age 45
Not due to an organic brain disorder
Postive schizophrenia symptoms
Hallucinations, Delusions, thought disorder
Negative schizophrenia symptoms
flat effect, lack of speech, Anhedonia (inability to pleasure)
what causes schizophrenia
overactive dopamine system
to many dopomaine receptors
Major neuromodulator in the brain
involved in movement, reward, cognitive functions (STM, working memory and attention)
Evidence for the role of Dopomaine
Neuroleptics (Haldol) is effective treatment for positive symptoms - block dopamine action
Dopamine Agonists (e.g., amphetamine) aggravates and mimic schizophrenia
Amphetamine psychosis
neuroleptics (Antipsychotics)
Drugs that block dopamine systems to reduce symptoms.
Affect both dopamine pathways; striatum involvement causes side effects.
Can lead to tardive dyskinesia — a movement disorder with repetitive muscle movements in the face, neck, arms, or legs due to too many dopamine receptors.
Anti-schizophrenic mediations
Clozapine doesn’t strongly affect D2 receptors (movement system).
Instead, it acts on D3 and D4 receptors in the limbic system and frontal lobes, helping control emotion and thought with fewer movement side effects.
what causes negative schizophrenia symptoms
Neurological damage (possible cause)
Glutamate hypothesis: underactive glutamate system in the cortex (NMDA receptor hypofunction) — since glutamate is the main fast-acting neurotransmitter in the cortex, low activity may lead to negative symptoms.
How do you get Schizophrenia
genetic hypothesis, environment hypothesis, combines effects
Diathesis-stress model
It explains how mental disorders develop through an interaction between:
Diathesis (vulnerability): a biological or genetic predisposition to a disorder.
Stress: environmental or life stressors that trigger the symptoms.
3 types of depression
Reactive
Endogenous/unipolar (major depressive disorder)
Bipolar -manic/depression
Reactive non-clinical depression
“normal” depression
response to life events
usually passes in relatively short time
Major depressive Disorder symptoms
Most typical symptoms:
Low mood
Inability to experience pleasure in past enjoyable activities
“Ruminating” over thoughts and feelings of worthlessness
Inappropriate guilt or regret
Helplessness or hopelessness
Other symptoms of depression:
Poor concentration
Withdrawl from being social
Reduces sex drive
Irritability
Insomnia or hypersomnia
Thoughts of suicide
Major depressive disorder (MDD)
cycles, episodes average 13 months
2-3 times more likely in women
7-20% of population
age usually around mid 20s
Major depressive disorder symptoms
40% generic
diathesis-stress model
MDD results from preexisting vulnerability which is activated by environmental stress
Bipolar - manic/depression
effects men and woman equally
Elation - delusions and grandiosity
average age: 30s
usually lasts 6 months - 8 months without medication
mania 2 months average
Types of Bipolar
Type 1 - cycles between mania and depression
Type II - cycle between depression and hypomania (less extreme mood elevation)
harder to diagnose
Cyclothymia Hypomania to mild depression
Bipolar Causes
Genetic
10 times more likely to have it if relative has it
Concordance is 70% in twins and 20% in fraternal (same if twins are together or apart)
some evidence is due to single dominant gene
Drug Treatment depression
Tricyclic antidepressants - effective in 70% unipolar
Prozac maybe even more
serotonin agonist, SSRI
Lithium carbonate - effective against mania in bipolar
psychedelic drugs (psilocybin)
ketamine
4 types of Anxiety disorders
generalized anxiety disorder (GAD)
Panic disorder - phobias
post-tramatic stress disorder (PTSD)
obsessive compulsive disorder (OCD)
Generalized Anxiety disorder (GAD)
• Excessive, ongoing worry and tension
• An unrealistic view of problems
• Restlessness or a feeling of being "edgy"
– Irritability
• Muscle tension
• Headaches
• Difficulty concentrating
• Longer than 6 months
Panic disorder
Characterized by sudden episodes of intense anxiety, fear, or terror.
Physical symptoms: heart palpitations, rapid breathing, dizziness.
With agoraphobia: fear of open or public places (can trigger attacks).
Without agoraphobia: panic occurs without a specific trigger.
Rates and causes of anxiety
2% rate men and women
Age: 35
Genetic factor
Higher rate in 1 st degree relatives (30%)
– Higher in monozygotic than dizygotic twins
• High comorbidity with Major Depressive Disorder
Caused by not enough or Blocked GABA receptors
Treatment Anxiety
Behavioral therapy
– Systematic desensitization
• Benzodiazepines (e.g., Valium)
– GABA agonist
– GABA is major inhibitory neurotransmitter
PTSD
Caused by experiencing or witnessing a traumatic event.
Involves recurrent dreams, memories, or flashbacks of the trauma.
Leads to avoidance of reminders, social withdrawal, and emotional numbness.
Also causes hypersensitivity to noise or movement and a heightened startle reflex.
what goes wrong in anxiety disorders?
The amygdala activates the hypothalamus, triggering the stress response.
The amygdala itself is activated by the cortex and learned associations (e.g., classical conditioning).
Overactive frontal cortex circuits may overstimulate the amygdala.
Benzodiazepines help by reducing frontal overactivity, which in turn reduces the stress response.
Disorders Arising from Damage/Disfunction
to the central nervous system
Cerebrovascular disorders
Traumatic brain injury (TBI)
Epilepsy
tumors
Headache
Degenerative
“other”
What are Cerebrovascular Disorders?
Among the most common causes of death and chronic illness in the Western world.
Caused by a disruption of blood flow to the brain (known as a stroke or Cerebral Vascular Accident – CVA).
Severity depends on the size of the affected blood vessel.
A Transient Ischemic Attack (TIA) is a temporary or mild stroke warning of possible future strokes.
Traumatic Brain Injuries (TBI)
Is the most common brain injury in people under 40
sport activities are the cause of 20% of TBI
higher chance of head trauma on males 15-30 years old
What does Traumatic Brain Injuries cause on the brain?
Immediate
Immediate injuries: contusion (bruising) where the brain hits the skull, hematoma (bleeding), and axonal tearing.
Secondary injuries: brain swelling (edema), glutamate excitotoxicity causing cell death, and blood-brain barrier disruption.
concussions - mild (TBI)
A mild traumatic brain injury (mTBI).
Glasgow Coma Scale (15-point test) checks eye, verbal, and motor responses — scores 13–15 = mTBI.
Neurological exam tests vision, hearing, reflexes, and strength.
Sport Concussion Assessment Tool (SCAT) evaluates:
Symptoms: headache, nausea, fogginess, irritability
Cognition: memory, concentration, orientation
Balance & coordination
Chronic Traumatic Encephalopathy (CTE)
A neurodegenerative disease caused by repeated head injuries.
Symptoms appear years later and affect behavior, mood, and thinking.
Considered a form of dementia.
Epilepsy
A brain disorder marked by recurrent seizures.
Two types:
Symptomatic seizures: have a known cause (e.g., TBI).
Idiopathic seizures: occur spontaneously with no clear cause.
Affects about 4–10 people per 1,000.
Epilepsy symptoms
Three main symptoms:
Aura: warning sign before a seizure
Loss of consciousness
Motor movements: body shaking or jerking
Diagnosis is confirmed with an EEG (electroencephalogram).
Seizure
The active component of epilepsy
manifested by a abnormal, excessive, and hypersynchronous electrical discharge of neurons in the brain.
two types - focal and generalized
Focal Seizures (partiel)
Begins in one place (a focus point) and spreads
Generalized Seizures
Affect both sides of the brain (bilaterally symmetrical).
Type: Grand mal (tonic-clonic) seizure.
Tonic stage (10–20 sec): muscles stiffen.
Clonic stage (1–3 min): rhythmic jerking movements.
Postictal phase: tiredness, confusion, soreness, headache, and no memory of the seizure.
Petit Mal (absence) seizure
A type of generalized seizure with loss of awareness.
Little or no movement — may blink, roll eyes, or stare blankly.
Person may stop speaking briefly (10–30 seconds).
Quick recovery afterward.
Most common in children.
Treatment for Epilepsy
Anticonvulsant drugs - Dilantin, phenobarbital, Carbamazepine (Carbatrol, Tegretol, others)
Surgery (especially in drug resistant cases)
Deep brain stimulation (DBS)
Tumors
A tumor is a mass of new tissue that grows independently of normal cells.
Benign tumors
Malignant tumors
Benign tumors
do not usually return after removal
Malignant tumors
Recur, grow progressively, and can be life-threatening.
Headaches: Migrane
Begins with an aura lasting 20–40 minutes (caused by vasoconstriction in the occipital cortex).
Followed by a headache due to vasodilation in the dura.
Pain is intense, often on one side of the head.
May include nausea and vomiting.
Degenerative CNS disease
Parkinson’s disease (PD)
Dementia
Alzheimer’s disease (AD)
Multiple Sclerosis (MS)
Huntington’s Disease
Parkinson’s Disease (PD)
A progressive central nervous system (CNS) disorder that mainly affects movement.
Early symptoms: tremors, muscle rigidity, slow movement, and walking difficulty.
Later symptoms: worsening movement issues and possible dementia.
Causes of Parkinson’s disease
Caused by the death of dopamine-producing cells in the substantia nigra.
Results from a mix of genetic and environmental factors.
15% have a close relative with the disease; 5–10% have a gene mutation.
About 60,000 new cases per year in the U.S.
Treatment for Parkinson’s Disease
Levodopa (L-DOPA): increases dopamine; often the first treatment.
Dopamine agonists: used when L-DOPA becomes less effective.
Deep Brain Stimulation (DBS): electrodes implanted in the thalamus can reduce symptoms in late-stage patients
Dementia
A progressive syndrome that impairs memory, thinking, and behavior.
Interferes with daily functioning and independence.
Other symptoms may include emotional problems, language difficulties, and low motivation.
Types of Dementia
Alzheimer’s (AD)
Frontal-temporal (FTD)
Lewy body (related to parkinson’s)
Vascular
Alzeimers’s Disease (AD)
A chronic, progressive neurodegenerative disease that worsens over time.
Causes 60–70% of all dementia cases.
Affects about 6.5 million people in the U.S.
Risk increases with age.
life expectancy 3-9 yrs
Always fatal no cure
Amnesic MCI
Frequently forgetting recent events
(important appointments, conversations, or social engagemnts)
Repetition: asking the same questions, telling the same stories
Misplacing items and being unable to find them
Getting lost in familiar places
Symptoms of Alzheimer’s
Early: trouble remembering recent events (mild cognitive impairment – MCI).
Later: worsening memory, language difficulties, disorientation, mood swings, loss of motivation, and poor self-care
Cause of Alzheimer
70% believed to be inherited
Likely many genes are involved
Increase risk in depression (MDD) And hypertension (high blood pressure)
Brain basis of Alzaimer’s
Brain pathology is associated with:
intracellular neurofibrillary tangles
Amyloid Plaques
Amyloid Hypothesis (Altzeimer’s)
Cause: Build-up of amyloid beta (Aβ) plaques outside brain cells
Gene: APP gene on chromosome 21 → extra copy in Down syndrome (trisomy 21) → early Alzheimer’s symptoms (~age 40)
Risk Factor: APOE4 form of Aβ → increases risk for early-onset AD (40s–50s)
Tau Hypothesis (Alzheimer’s)
Cause: Abnormal tau proteins trigger disease process
Effect: Tau proteins stick together → form neurofibrillary tangles inside neurons
Result:
Microtubules break down
Cytoskeleton collapses
Neuron’s transport system fails
Cycles (circadian Rhythms)
A pattern of cyclical body activities lasting about 24 hours
Physical, behavioral and internal biological changes.
What controls circadian rhythms
Controlled by two influences:
Environmental cues – mainly sunlight.
An internal clock (endogenous oscillator) in the brain.
The internal clock can free-run without light cues (e.g., in darkness).
With a regular light source, the clock becomes entrained (synced) to it.
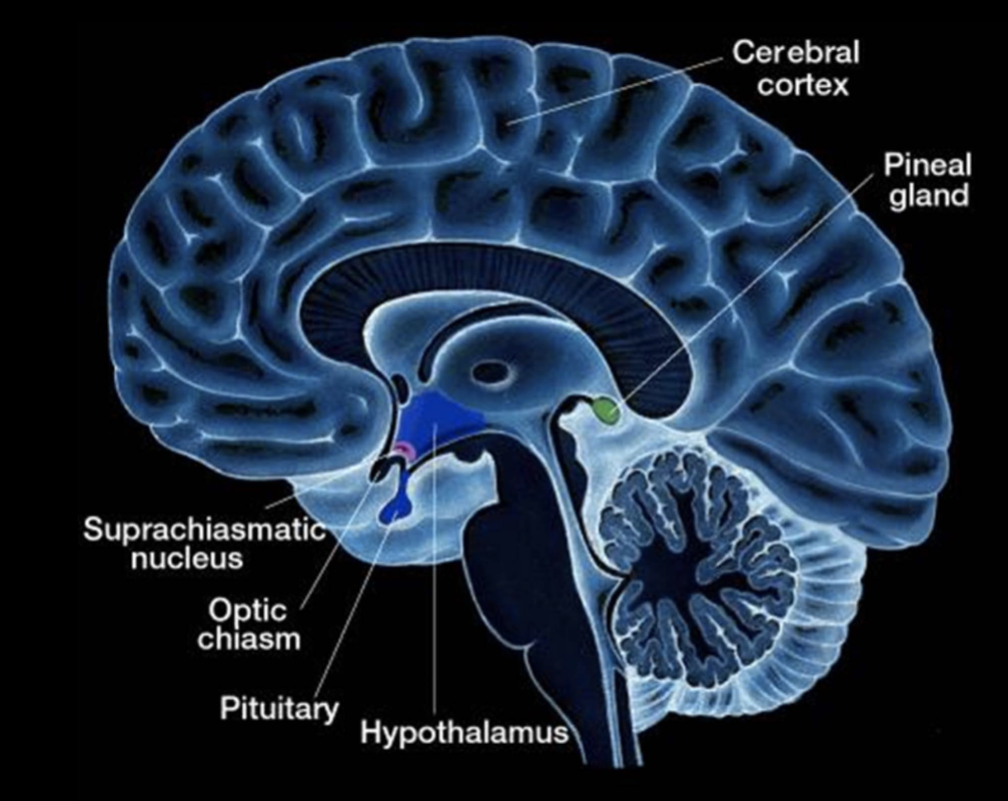
Special retinal ganglion cells (RGCs) send light signals to the suprachiasmatic nucleus (SCN) — a small area in the hypothalamus above the optic chiasm that regulates daily rhythms.
What are circadian rhythms for?
pacemakers of daily activity
arousal, metabolism, and hormonal activity
Suprachiasmatic nucleus (SCN)
The SCN has two parts: core and shell.
Core neurons receive input from M1 retinal ganglion cells (RGNs) that contain melanopsin, activated by light.
Light → activates M1 RGNs → activates core neurons → activates shell neurons.
Shell neurons hold the internal circadian clock.
This process allows external light to entrain (sync) our circadian rhythms.
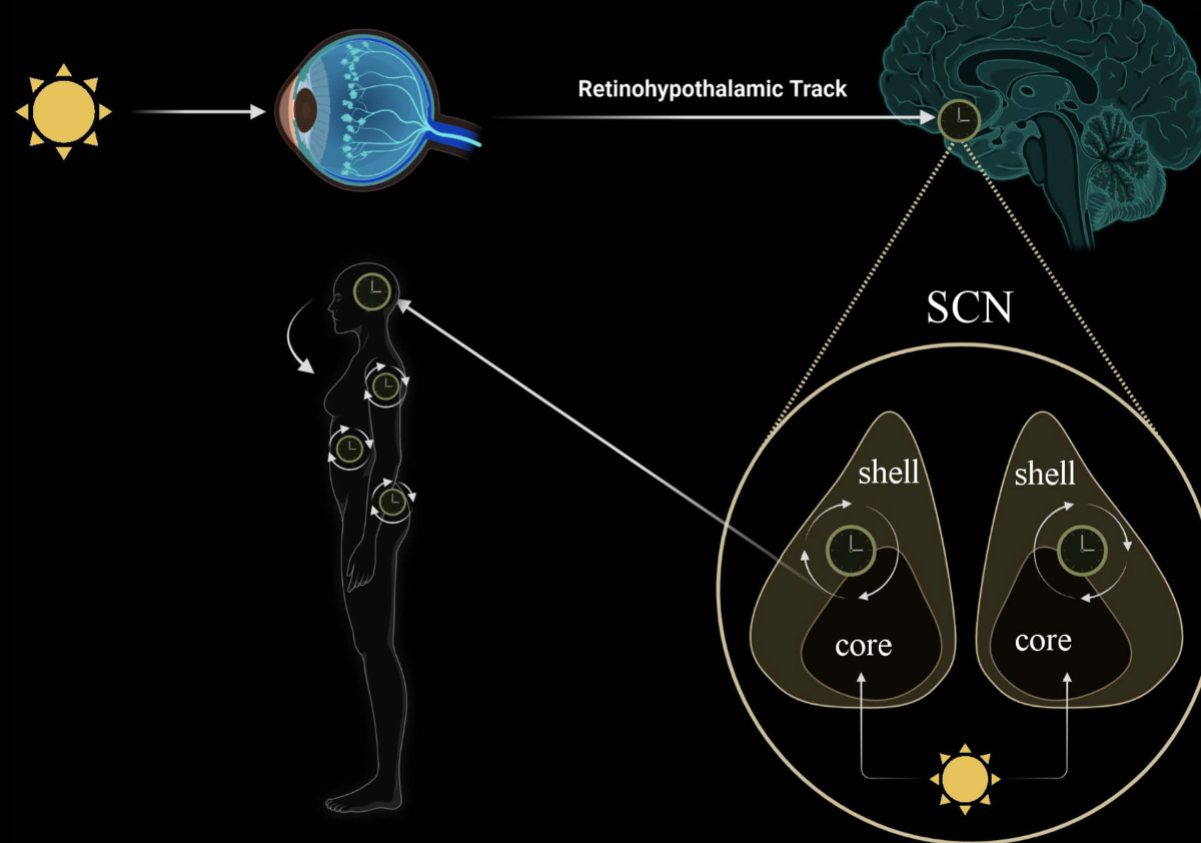
How does Suprachiasmatic nucleus(SCN) control sleep?
SCN shell neurons send signals to the pineal gland.
The pineal gland releases melatonin, a hormone that promotes drowsiness.
Melatonin helps regulate sleep and maintain circadian rhythms throughout the brain.
Why do we Sleep?
evolutionary or conservation theory
restorative theory
Evolutionary theory (sleep)
Sleep to conserve energy and for protection
Restorative theory (sleep)
Replenishes neurotransmitters.
Resets synaptic receptors to optimal sensitivity.
Enhances memory consolidation (strengthening of learned information).
What is sleep?
part of circadian cycle
state of altered consciousness
physiologically made of sequence of stages (stages defined as electroencephalogram EEG)
Four types of EEG
Defined by frequency
Beta - 13 to 20 Hz
Alpha - 8 to 12 Hz
Theta - 4 to 7 Hz
Delta - 1 to 4 Hz
Sleep spindles - 12 to 14 Hz
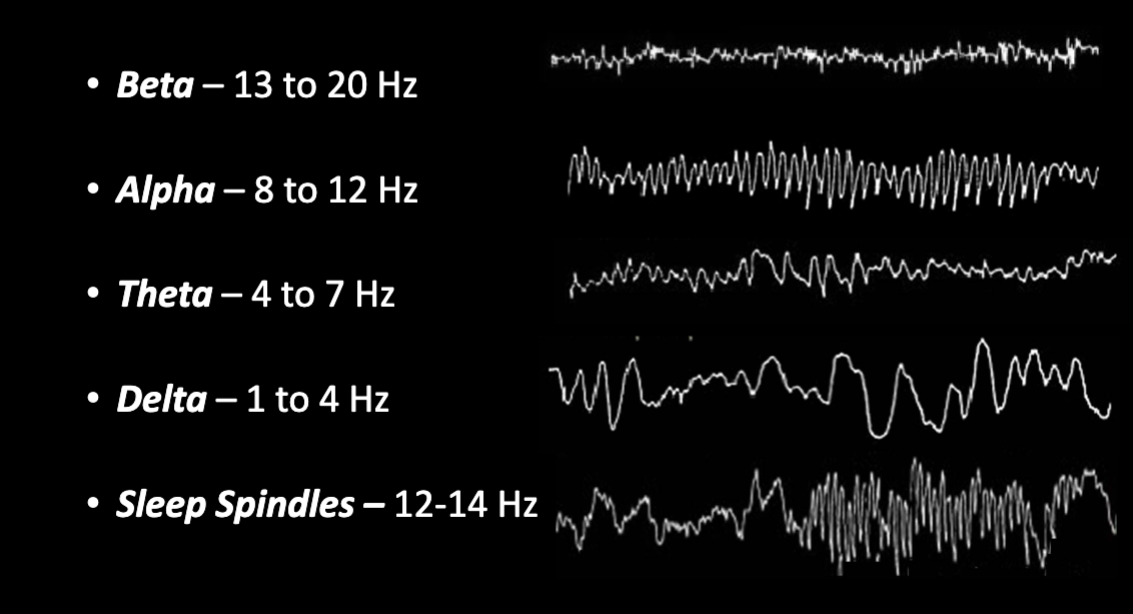
Sleep stages using EEG
Stage 1: wide awake to alpha
Stage 2: Alpha to Theta
Stage 3: Has both Theta and some Delta
Stage 4: Mostly Delta (slow wave sleep)
REM sleep
REM sleep
Period of brain arousal (paradoxical sleep)
Each episode last 10-20 minutes
Behaviorally characterized by rapid eye movement
What is REM sleep?
Most people awakened from REM report dreaming
dreaming can occur on other stages (but mostly REM)
REM is associated with paralysis of the body
What is dreaming?
Cortical activity during sleep
associated with images, ideas and emotions
may or may not remember after waking
more likely remember if awakened during REM
Dreams aren’t walking thoughts (frequently have bizarre quality)
Freud “Interpretation of dreams”
Dreams reflect the unconscious mind, showing hidden desires and anxieties, often from childhood.
Psychoanalysis uses dream interpretation to uncover repressed desires.
There is little scientific evidence supporting this theory
Dream theories
Dreams may reflect memory formation processes during sleep.
The prefrontal cortex (responsible for executive functions) is inactive during REM, which explains why dreams often seem bizarre or illogical.
Sleep Disorders
Since we spend about 25% of life asleep, many neuropsychological disorders affect sleep.
Two main categories:
Dyssomnias – problems with the amount, quality, or timing of sleep.
Parasomnias – abnormal behaviors or experiences during sleep.
Dyssomnia
A category of sleep problems characterized by a direct problem with the sleep process itself
Hypersomnia
Insomnia 2 types
Narcolepsy
Sleep apnea 2 types
Hypersomnia
sleeping too much or sleeping at inappropriate times.
Insomnia 2 types
Onset insomnia: problems getting to sleep
Maintenance insomnia: problems staying asleep
Can result in poor sleep hygiene, drugs and anxiety
Narcolepsy
A disorder causing excessive daytime sleepiness and sudden sleep episodes.
Episodes may be triggered by strong emotions.
The normal sequence of sleep stages is disrupted.
Sleep Apnea 2 types
Obstructive: caused by blockage of upper airway - reduction in blood oxygen
Central: problem in brain stem respiratory area that regulates breathing