Lower Urinary System
1/125
Earn XP
Description and Tags
UT 302 - Abdomen 1
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
126 Terms
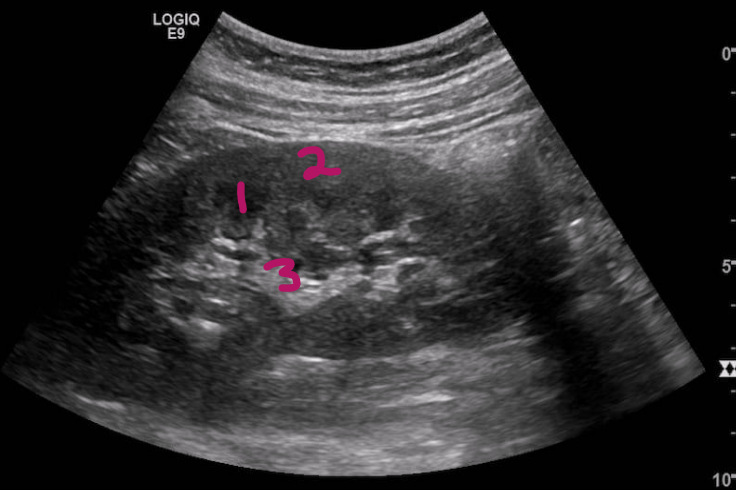
Label this image
Renal cortex
Renal medulla (pyramids)
Renal sinus
During early embryology of urogenital system, kidneys develop in 3 successive waves from cranial to caudal:
Pronephros
Mesonephros
Metanephros
What is the pronephros?
Early in 4th embryologic week
A transitory nonfunctioning kidney at this stage
What is the mesonephros?
Late in 4th week
Mid kidney provides partial function while the permanent kidney develops
What is the metanephros?
5th week
Third most inferior part of kidneys becomes permanent kidneys
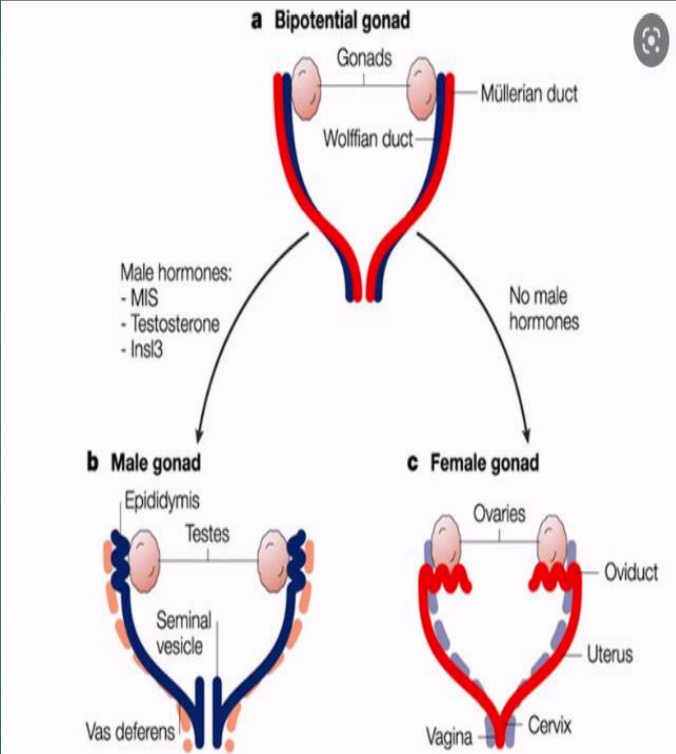
The ___ duct (from the first phase) becomes the ___ duct that helps form the genitalia
pronephric; mesonephric
In males, the ___ duct is called the ___ duct
mesonephric; Wolffian
The Wolffian duct eventually becomes the …
epididymis, vas deferens, and the ejaculatory duct
In females, the ___ duct is called the ___ duct
mesonephric; Mullerian
The Mullerian duct eventually becomes the …
uterus and vagina
What are some of the common indications for urinary bladder point-of-care ultrasound (POCUS) examination?
Bladder volume estimation
Bladder mass
Bladder outlet obstruction
Hematuria
Hydronephrosis
Anuria
Flank or pelvic pain
Confirm proper placement of Foley catheter
What transducer is ideal for scanning the bladder?
The low frequency curvilinear transducer is ideal for scanning the bladder (BL)
Can use the phased array low frequency transducer if the curvilinear transducer is not available
What are some lab value indicators of urinary system disease?
Hematuria
Blood urea nitrogen (BUN)
2-8 mg/dL
Serum creatinine
0.5 to 1.2 mg/dL
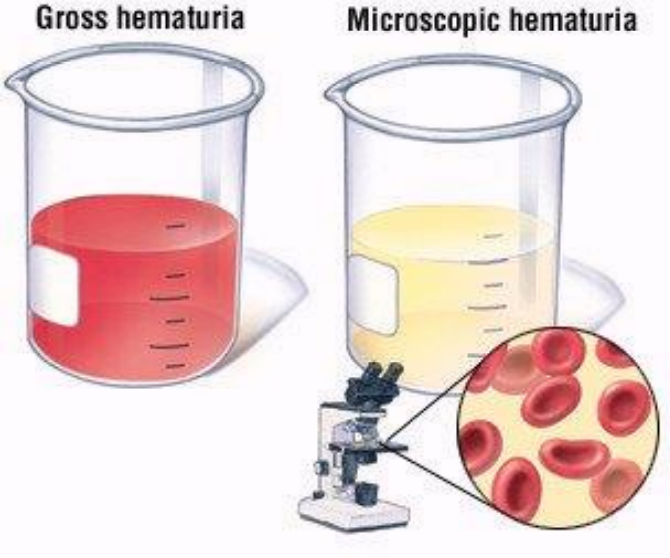
What is hematuria?
More than two to three blood cells per high-powered field are seen
The presence of red blood cells in the urine
Can be microscopic or macroscopic
The underlying cause can be located in the kidneys, ureters, bladder or urethra
Kidneys, urethra, and bladder can be visualized by US
What is the most common cause of hematuria?
Renal calculi (kidney stones)
What are the symptoms of renal calculi?
Severe colic pain
When they are at the ureteropelvic junction (UPJ), ureterovesical junction (UVJ), or in the bladder
Pain
Nausea
Vomiting
Fever and chills
From associated infection, hematuria, dysuria, bacteriuria and /or leukocytosis
What is the color of normal, healthy urine?
Pale straw or transparent yellow color
What urine color suggests mild dehydration?
Darker yellow or honey-colored
What urine color suggests liver problems or severe dehydration?
Darker, brownish color
What urine color may suggest blood in the urine?
Pinkish or red
Kidneys are part of the ___ urinary system
upper
The ureters, bladder, and urethra are part of the ___ urinary system
lower
What structures play important roles in transporting, storing, and eliminating urine?
Ureters
Bladder
Urethra
What structures are conduits in the process of eliminating urine?
Pelvic ureter
Urethra
What is the primary function of the bladder?
Functions as a temporary reservoir for urine storage as the kidneys produce urine and it flows down the ureter
T/F: normal pelvic ureters, abdominal ureters, and the urethra are not usually seen on an ultrasound
True
When can structures that are not normally visualized on US actually be seen?
When there is coexisting pathologic conditions
Example: kidney stone blocking urine in the ureter
T/F: a urine-filled bladder is hard to see on US
False
Describe the anatomy of the urinary bladder
Hollow, smooth, musculomembranous, collapsible sac
Lined with a mucous membrane of transitional epithelium that allows for expansion
Mucous membrane lining contains rugae or folds
Capable of considerable distention
When bladder is empty, membrane appears folded or wrinkled
Normally, bladder is a round-edged tetrahedron
Has 1 superior, 1 posterior, and 2 inferior surfaces
Where is the bladder located?
Anatomically between ureter and urethra
In the retroperitoneum on the pelvic floor just posterior to pubic symphysis
Where are the two ureteral orifices located in the bladder?
In the body on the posteroinferior portion of the trigone
Where is the urethral orifice located in the bladder?
In the neck of bladder and in the most inferior region
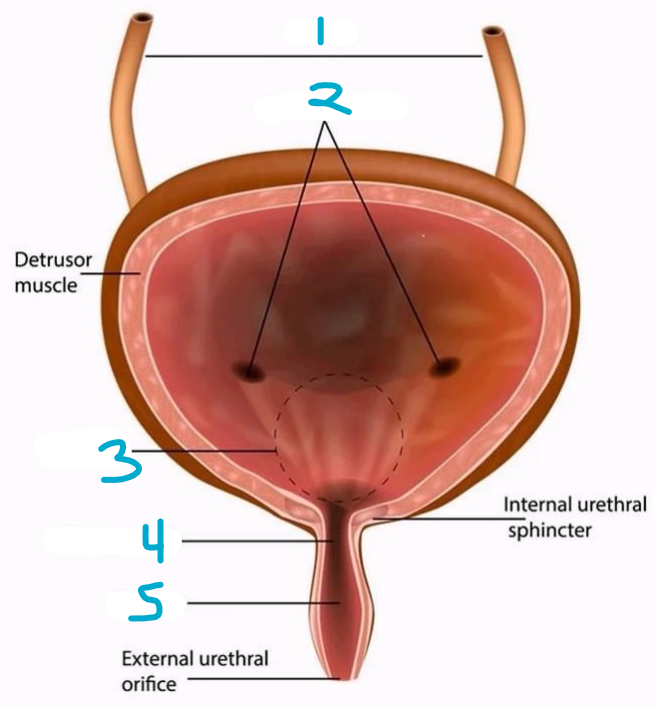
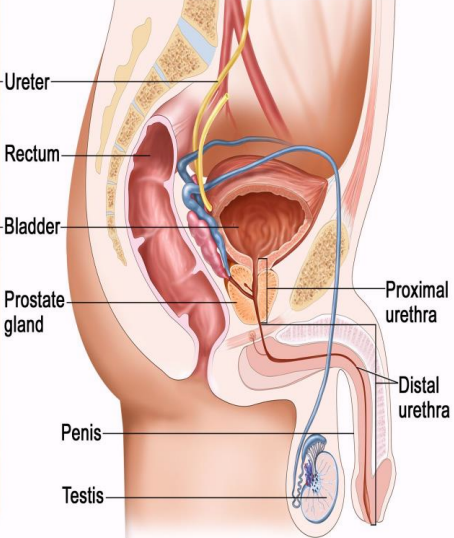
Label the image
Ureters
Ureteric orifices
Trigone
Bladder neck
Urethra
Describe the anatomy of the trigone
Triangular
No rugae
Attached to muscular coat
3 openings
2 ureters
1 urethra
Why is it important for sonographers to recognize the bladder anatomy, including size, shape and appearance?
Because it helps the sonographer identify congenital anomalies of the bladder, pathologies and abnormalities in the surrounding anatomy
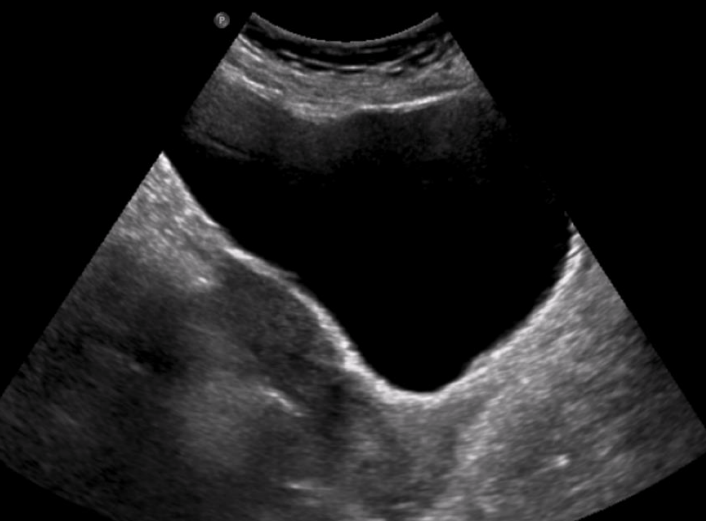
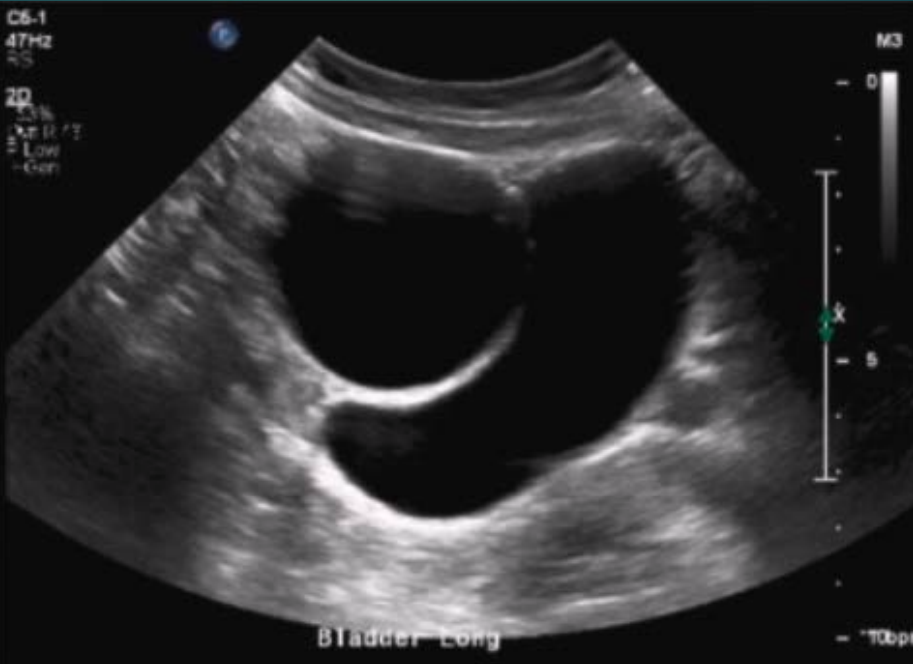
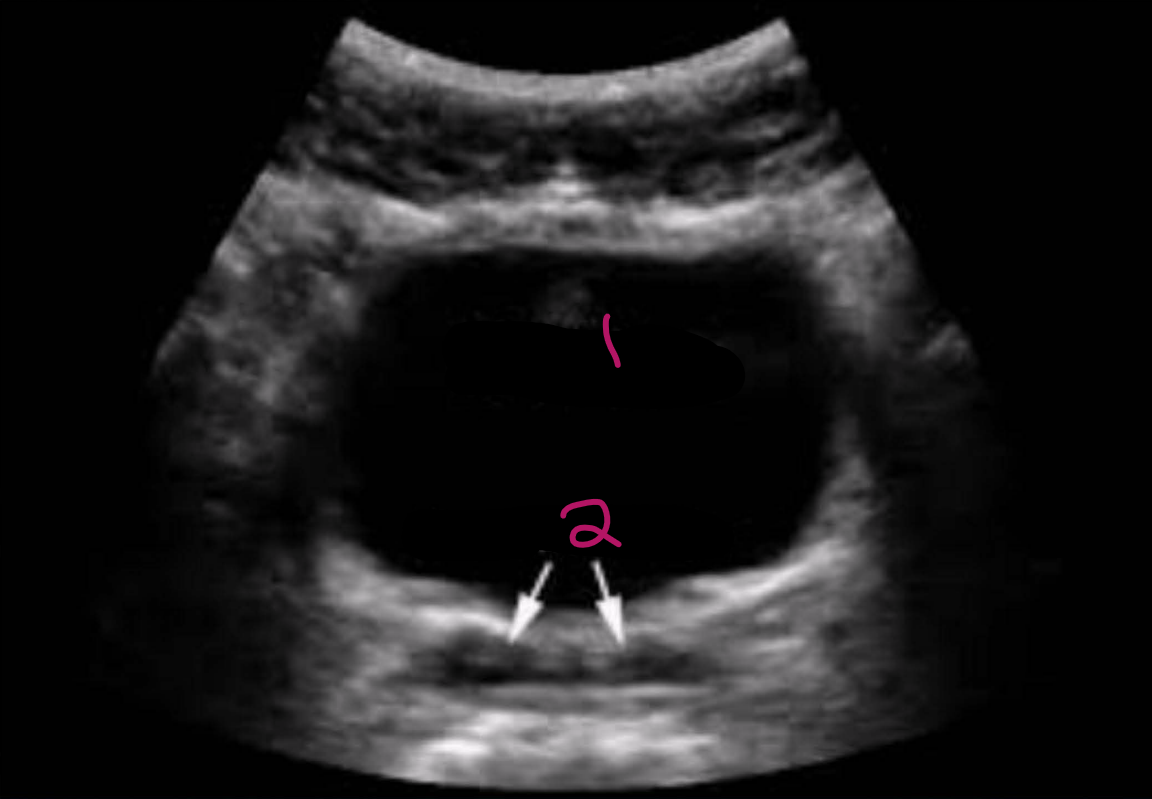
Is this a trans or long image of the bladder?
Long (triangular appearance)
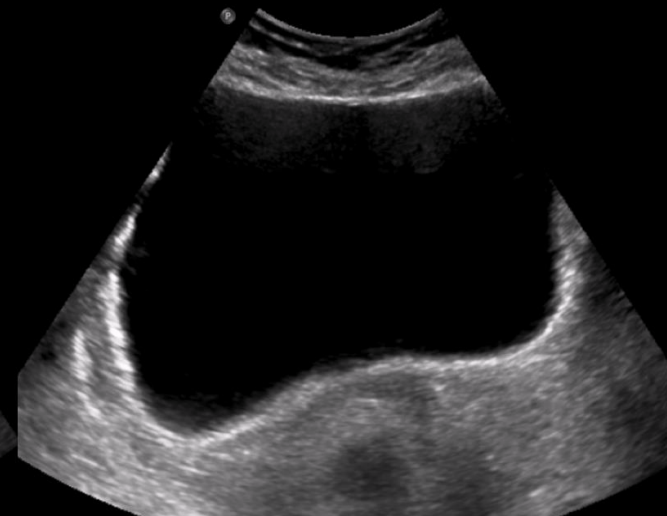
Is this a trans or long image of the bladder?
Trans (rectangular appearance)
T/F: a full bladder also provides an excellent acoustic window to view the uterus and other pelvic organs
True
Small intestine coils lie adjacent to the ___ surface of bladder and are displaced ___ as the bladder enlarges
superior; posteriorly
The lower abdomen may visibly bulge with ___ of the bladder (acute/chronic urinary retention)
overdistention
At what volume of fluid is the adult bladder considered to be moderately full?
500 mL ~ 1 pint (but can hold almost double if neccessary)
What is the upper limit of normal for bladder wall thickness when the bladder is distended?
3 mm
What is the upper limit of normal for bladder wall thickness when the bladder is empty?
5 mm
Infants have a proportionally ___ bladder wall
thicker
Describe the anatomy of the ureters
Slender tubes that convey urine from kidneys to bladder
From the renal pelvis, ureters descend in retroperitoneum and course obliquely through posteroinferior bladder wall
Each ureter is a continuation of the renal pelvis
Continually contracts and relaxes, forcing urine downward in to the bladder about every 10-15 secs
What is the average ureter length?
30 cm
What is the average ureter diameter?
6 mm
How do the ureters prevent backflow of urine into the kidneys?
As bladder fills, the pressure increases causing upper and lower walls of terminal portions of ureter to become closely applied to each other to act as valves to prevent regurgitation of urine from bladder
When bladder is distended, the openings of ureters are about ___ apart, and the distance between them is 2.5 cm when the bladder is empty and contracted
5 cm
Where can the ureters become constricted?
At the junction at renal pelvis (ureteropelvic junction - UPJ)
As they cross the iliac vessels
At the junction with bladder (ureterovesical junction - UVJ)
Normally, the ureters are not seen on an ultrasound after they leave the renal pelvis until …
their entrance into the bladder
How do the ureteric orifices appear on US?
Two small bumps on the posterior aspect of the bladder on either side of midline
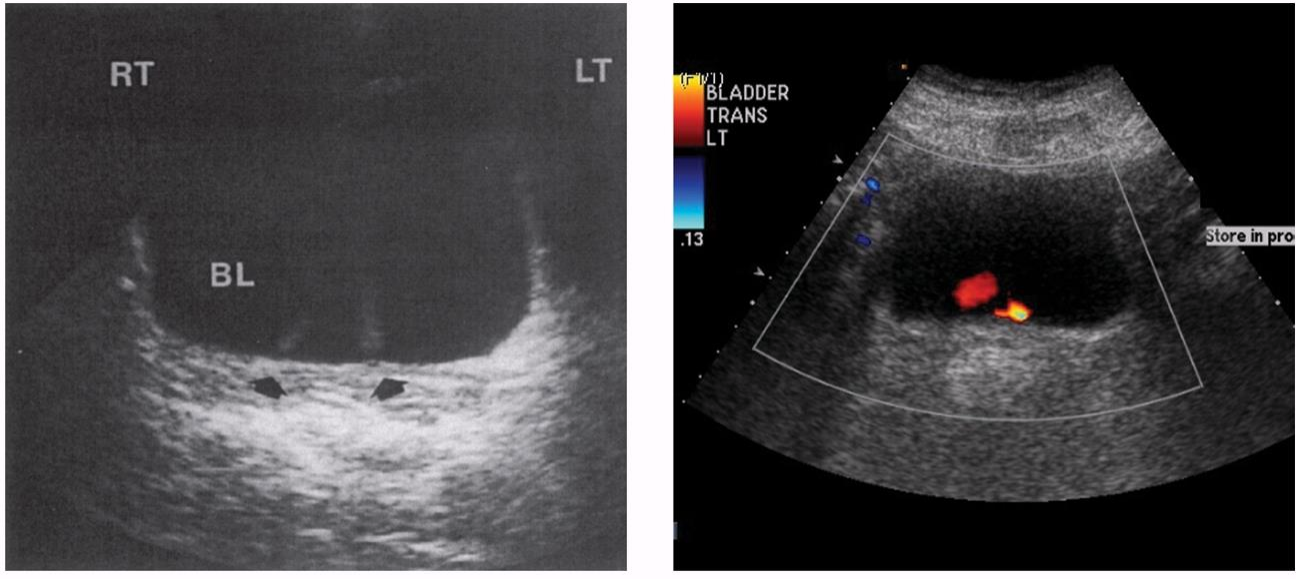
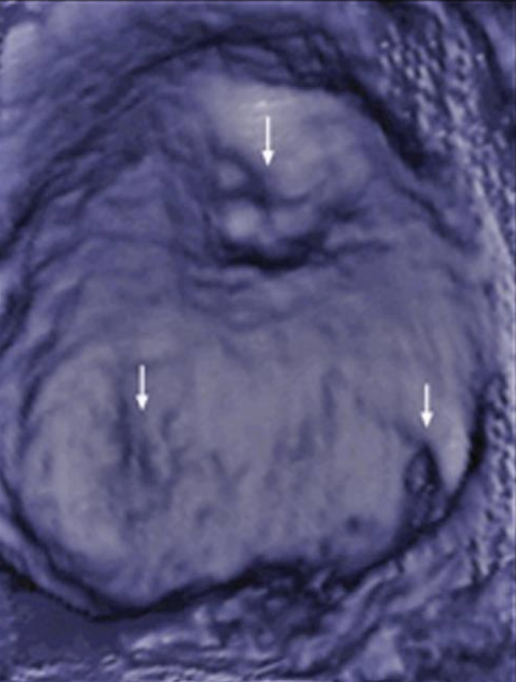
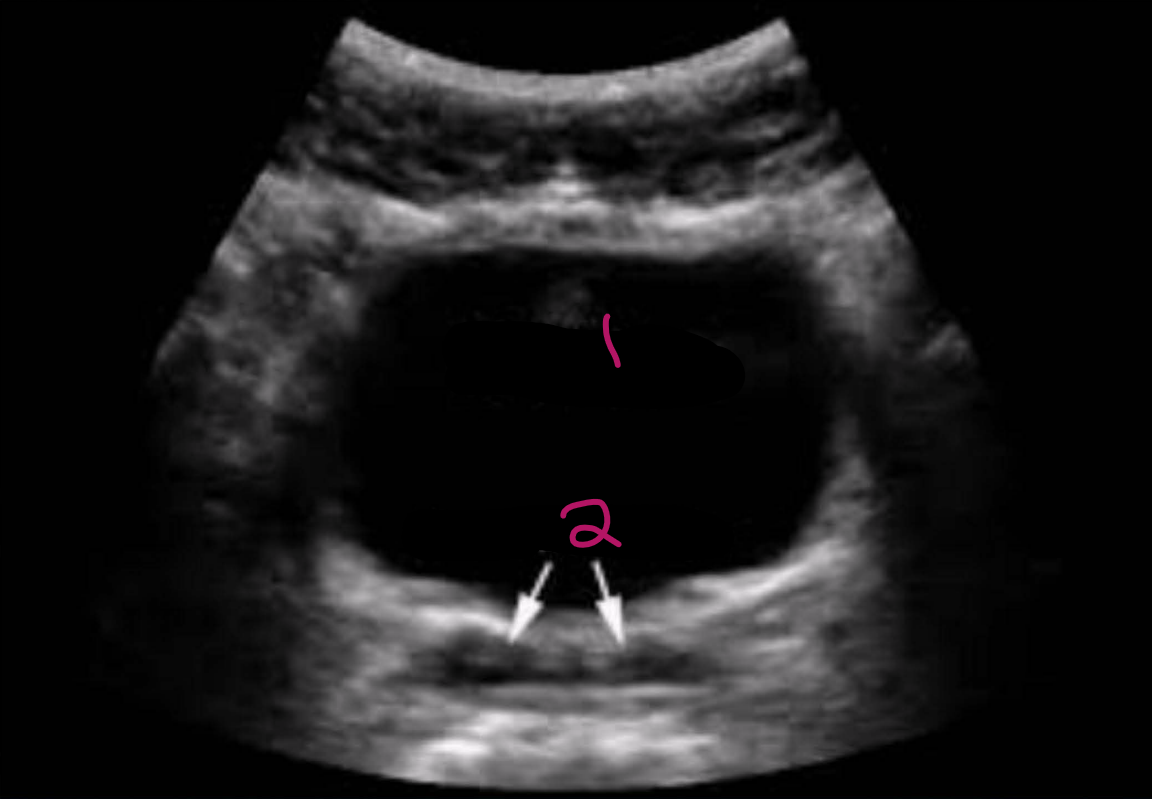
Describe these images
Left: simultaneous jets of low-intensity echoes (arrows) are visualized entering urinary bladder (BL)
Right: color Doppler demonstrates both right and left ureteral jets on transverse image on a male patient
What happens to the bladder during urination?
The bladder muscles contract and sphincter opens to allow urine to flow through the urethra
How long is the male urethra?
20 cm (travels through the penis and caries both semen and urine)
How long is the female urethra?
4 cm
What is the urachus?
Embryonic tract formed as bladder descends into true pelvis
Usually obliterates by birth, if it doesn't it creates a channel between bladder and umbilicus

Where is the bladder located in a fetus?
At the umbilicus
Communicates with the allantois (extension of cloacae/urogenital sinus)
What are the types of urachal variants?
Completely patent urachus
Urachal cyst
Urachal sinus
Urachal diverticulum
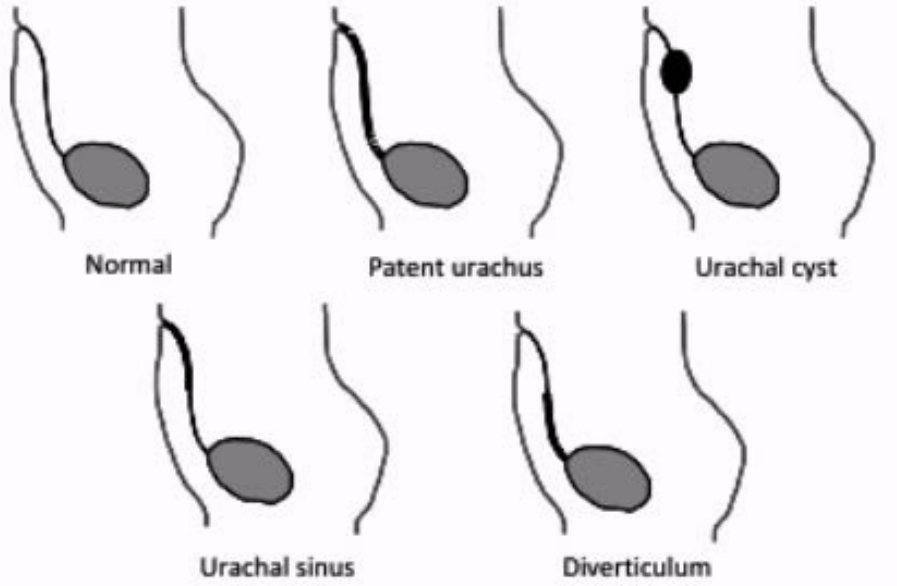
What is a completely patent urachus?
About 50% of cases
Both ends remain open, causing urine to leak from the umbilicus
What is a urachal cyst?
About 30% of cases
Both ends close off, and a cyst forms in the middle
What is a urachal sinus?
About 15% of cases
Closes at bladder end but not umbilicus

What is a urachal diverticulum?
About 5% of cases
Closes at umbilicus but remains patent at bladder

What is micturition?
Mechanism for voiding urine
What are the steps of micturition?
Starts with involuntary and voluntary nerve impulses
When volume of urine exceeds 200 to 400 mL, stretch receptors trigger transmission of impulses to lower portion of spinal cord
Initiates conscious desire to expel urine and a subconscious, micturition reflex
Combination of voluntary relaxation of external bladder sphincter muscle, reflex contraction of linear smooth muscle fibers along urethra
Contraction of detrusor muscle squeezes urine out of bladder
What is incontinence?
Involuntary emptying of bladder
Results from aging or trauma to any parts of nervous system by cerebral hemorrhage or cord injury
What is retention?
The inability to empty bladder even though bladder contains an excessive amount of urine
Catheterization may be used to relieve discomfort accompanying retention
30% of patients who are routinely catheterized eventually develop a ___ posteriorly at bladder neck from catheter trauma
“ledge”
Why is it bad to develop a “ledge”?
Makes voiding difficult
Considerably complicates catheterization process
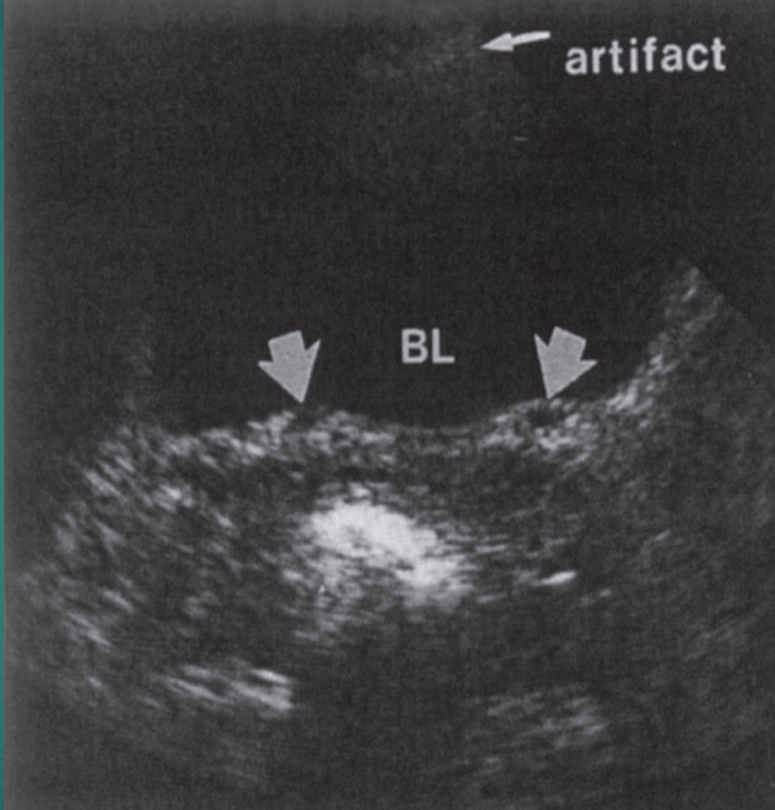
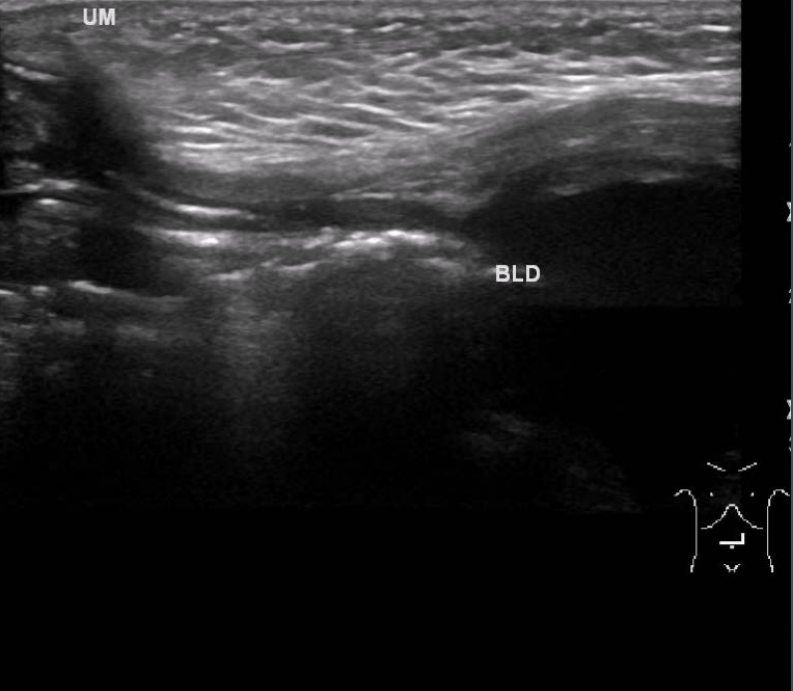
How does a Foley catheter appear on US?
The catheter appears anechoic, with an echogenic exterior

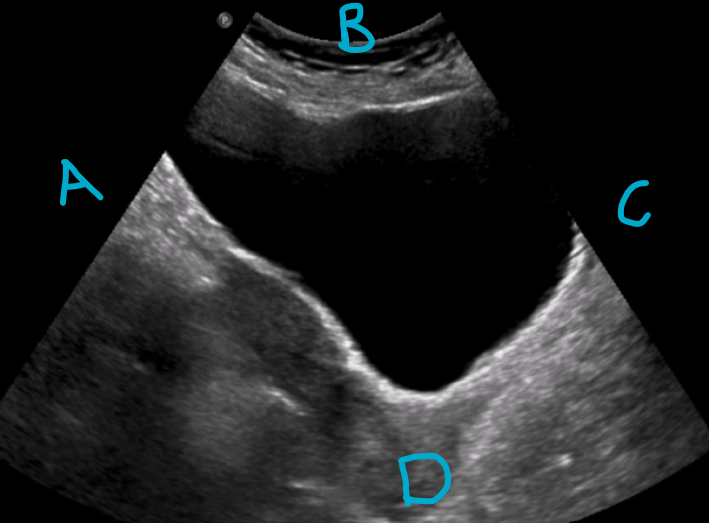
Label the directions in this image
A - superior
B - anterior
C - inferior
D - posterior
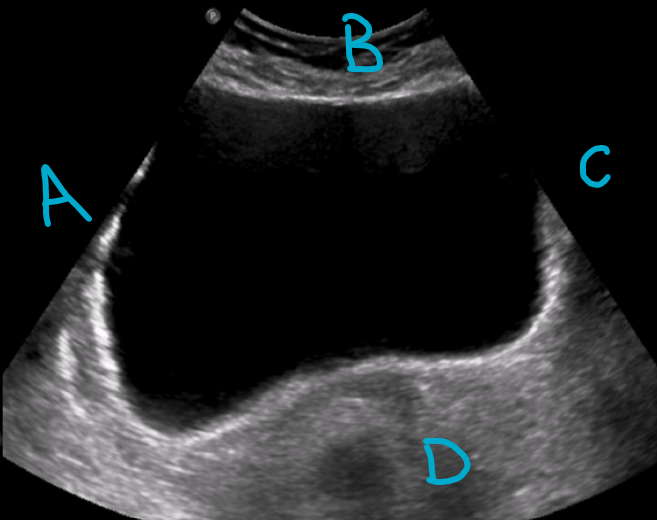
Label the directions in this image
A - right
B - anterior
C - left
D - posterior
How should patients prepare for a bladder ultrasound?
It is important for patients to properly prepare in order to better visualize the bladder with a transabdominal approach
Bladder distention is absolutely essential to optimal visualization of bladder, bladder wall, and related anatomy
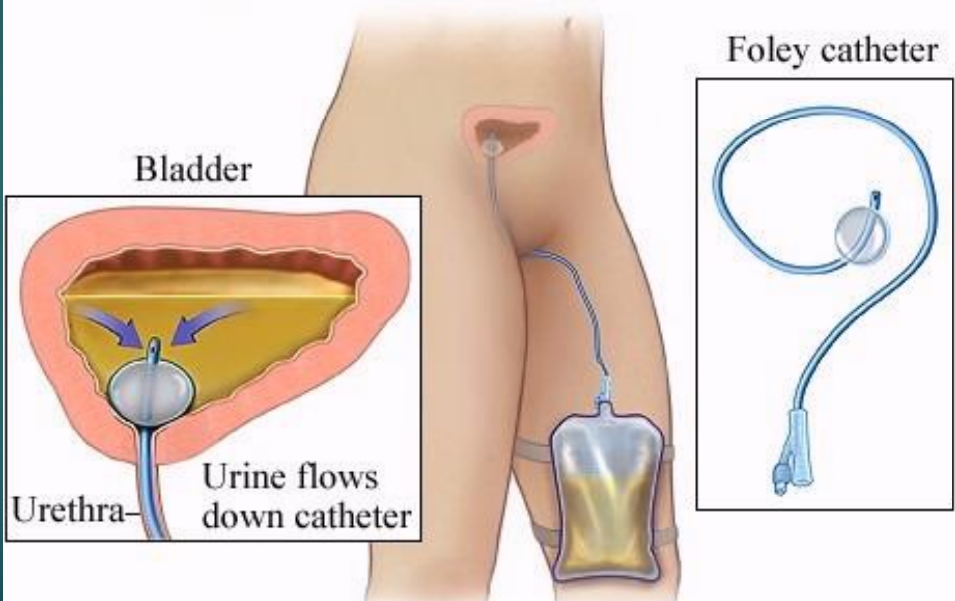
What are the three methods that can be used for bladder filling?
Instruct patient to drink 16 ounces of water 1 hour before exam and not to void until exam is completed
Instruct patient not to void before examination
Catheterizing patient and instilling fluid into bladder through a Foley catheter
What are some techniques for scanning the bladder?
Most widely used approach to scan the urinary bladder is transabdominal method
Patient is usually examined in supine position
May be necessary to position the patient in LPO/RPO or RLD/LLD to better demonstrate bladder wall abnormalities, movement of debris or calculi to dependent bladder wall, or bladder tumors
To lesser extent, endovaginal, endorectal, and transperineal methods may be used for lower urinary tract
Not necessary to restrict diet or use catheters or enemas to reduce intestinal contents or air
Scan in both longitudinal and transverse planes transabdominally
May scan in longitudinal and coronal planes endovaginally and transperineally
What role do Foley catheters play in bladder US examination?
Foley catheters are not routinely inserted for bladder filling unless it is a medical emergency
Many studies show catheter insertion may introduce infectious contaminants into body
Foley catheter balloon appears as round cystic structure in filled bladder and may cast shadows in areas of interest
What sonographic purpose does a fully distended bladder serve?
Cystic reference in abdominopelvic anatomy
Pushes adjacent bowel and gas out of field of view
Provides “window” to identify pelvic anatomy
Facilitates identification of dilated ureters
What pelvic structures should be routinely imaged in males?
Bladder
Seminal vesicles
Prostate
Rectum
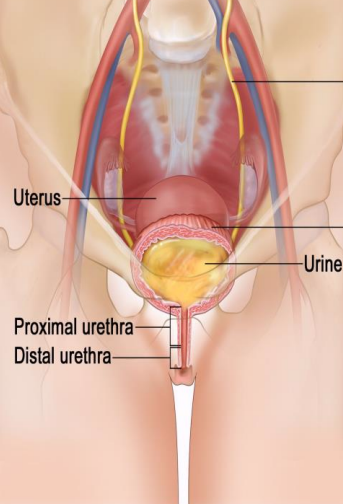
What pelvic structures should be routinely imaged in females?
Vagina
Bladder
Uterus
Ovaries
Adnexa
Rectum
T/F: disease processes in pelvic structures can involve or mimic those of other closely related anatomy
True
What are some considerations for scanning the bladder?
Knowledge of pelvic anatomy, genitourinary tract, gastrointestinal tract, pelvic vasculature, and pelvic musculature are important
Transducer selection should take into consideration body habitus and exam objectives
Select highest frequency transducer possible to make sure penetration is adequate to visualize posterior aspect of areas of interest
Equipment instrumentation includes harmonics, speckle reduction, spatial compounding, and computerized techniques to aid elimination of artifact echoes
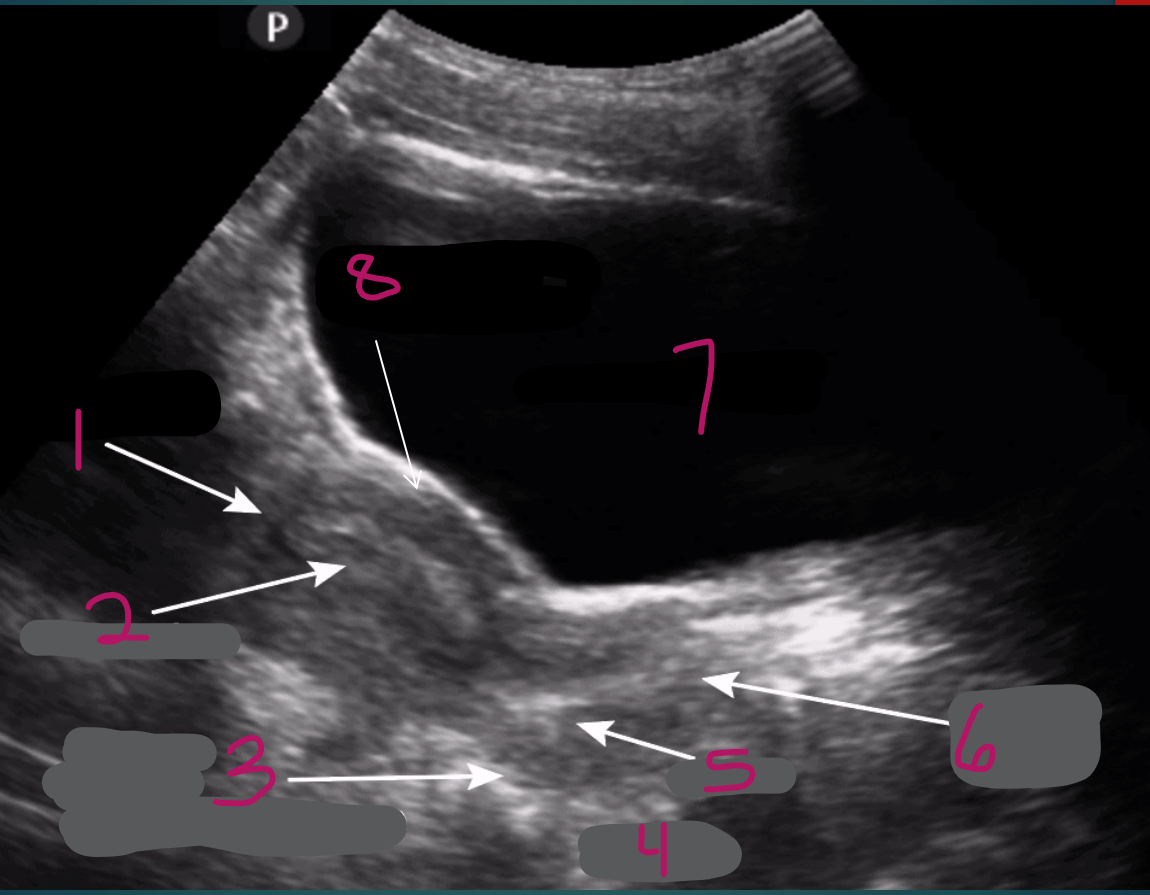
1
Fundus of uterus
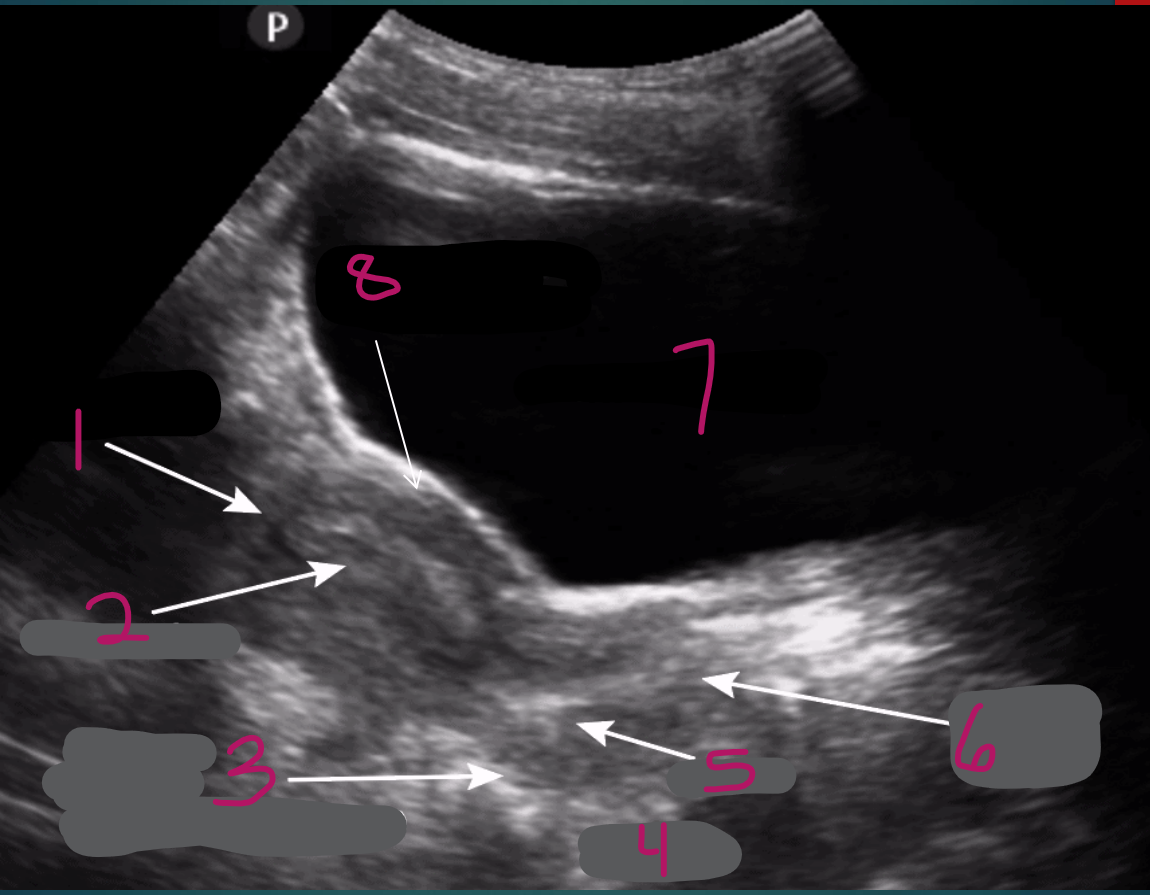
2
Endometrium of uterus
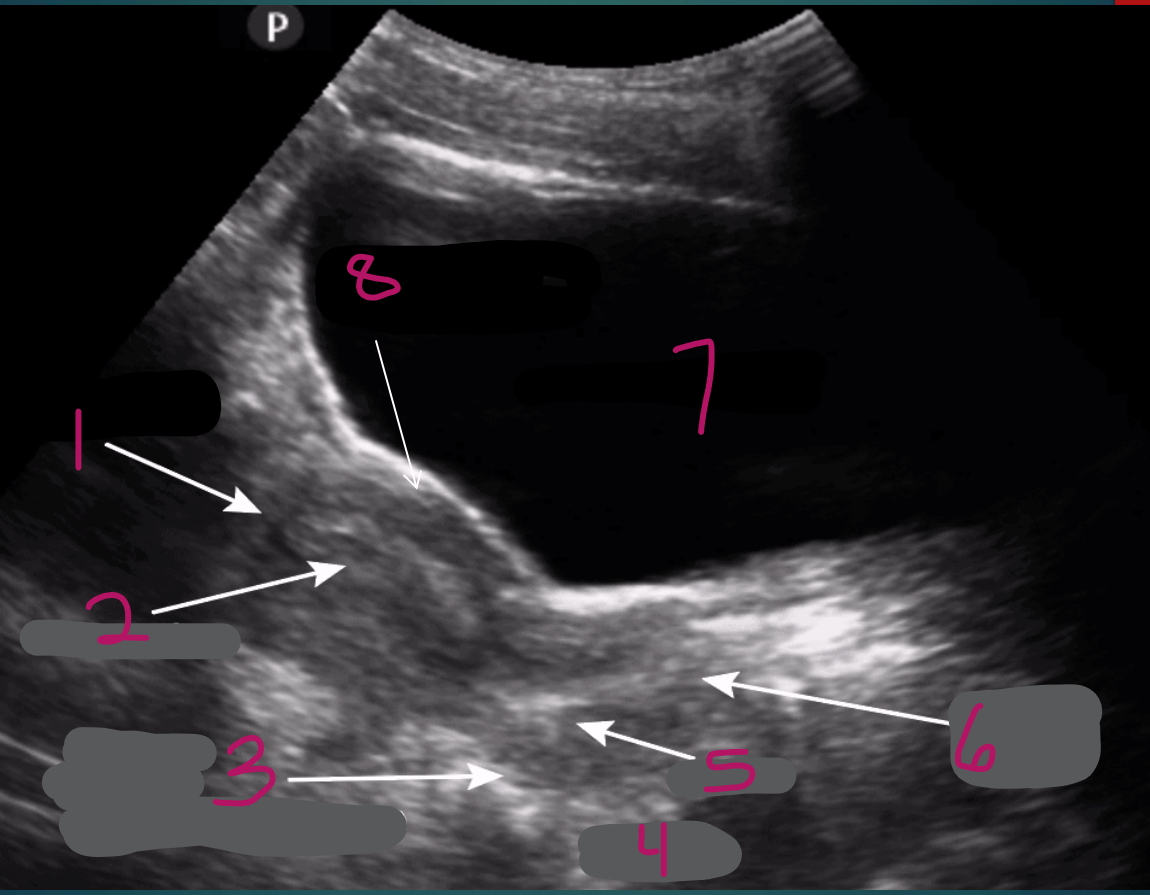
3
Pouch of Douglas (posterior cul-de-sac)
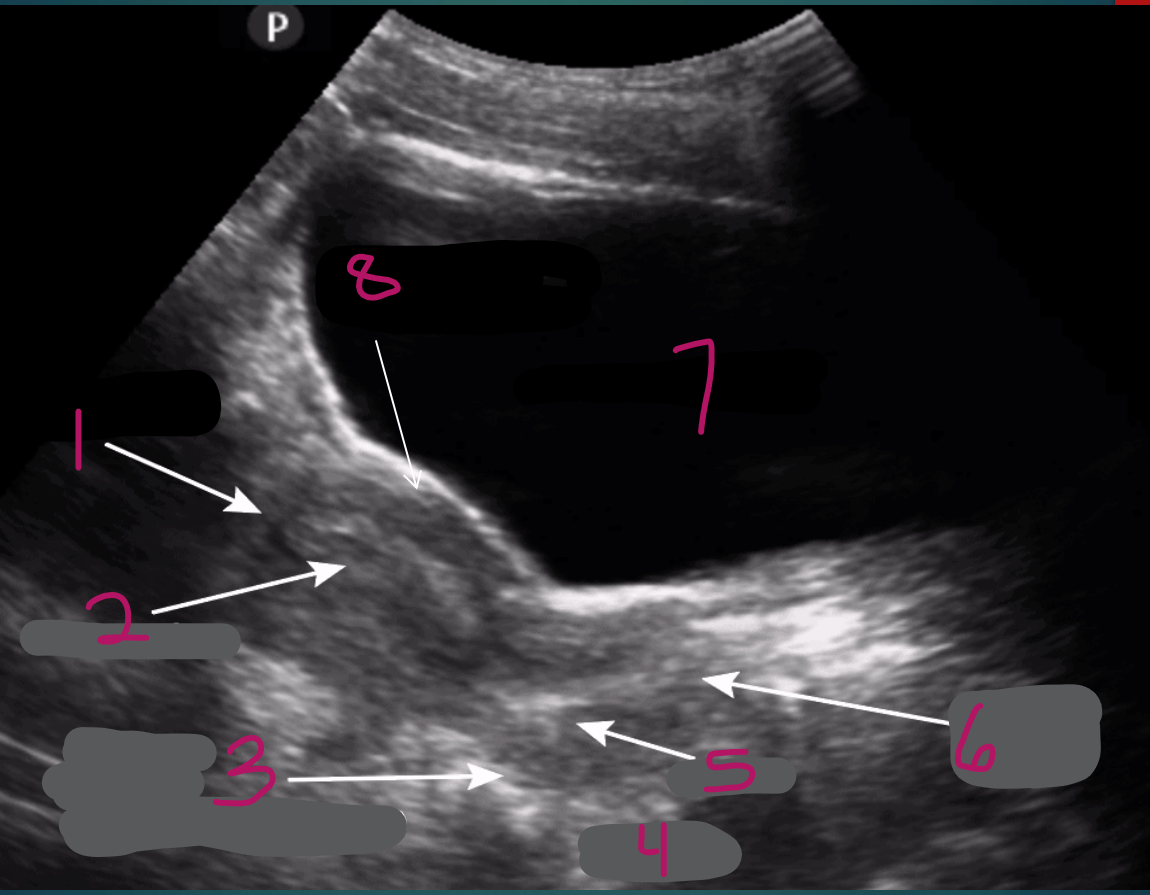
4
Rectum
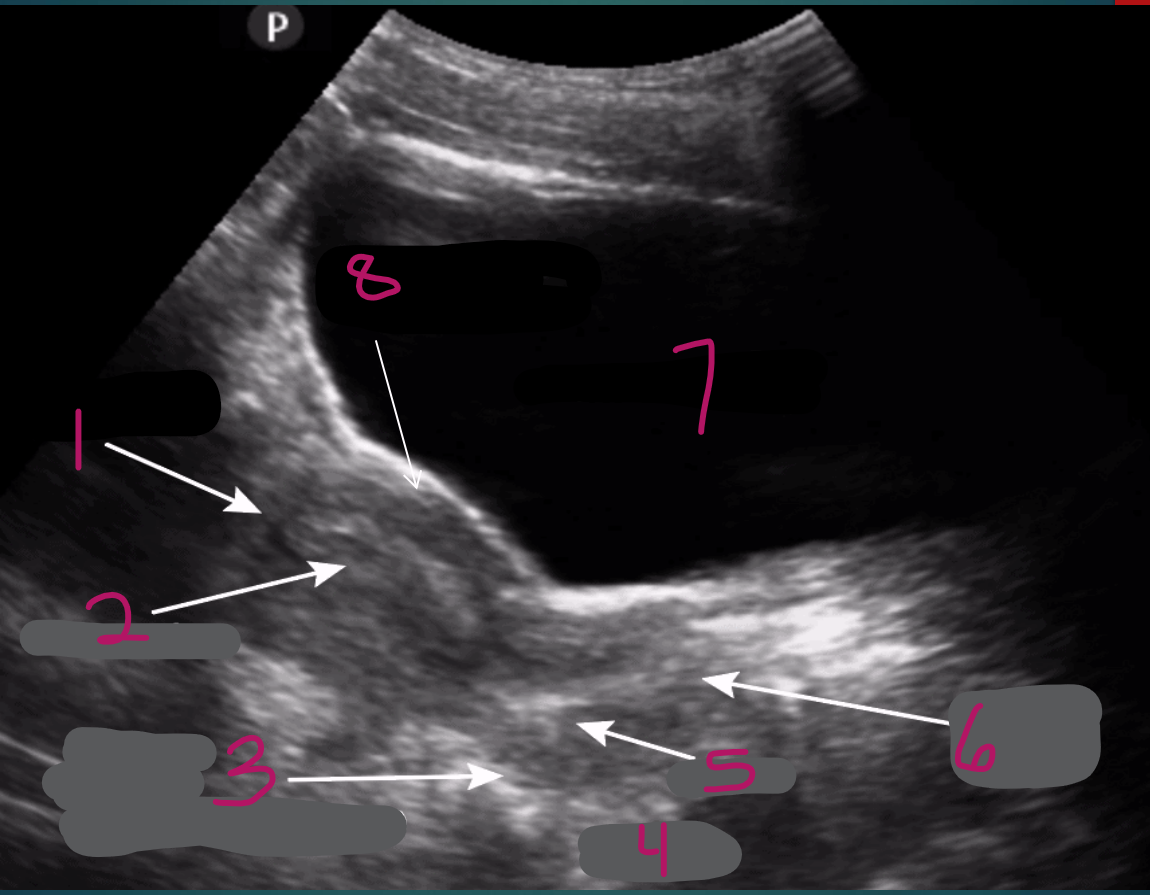
5
Cervix
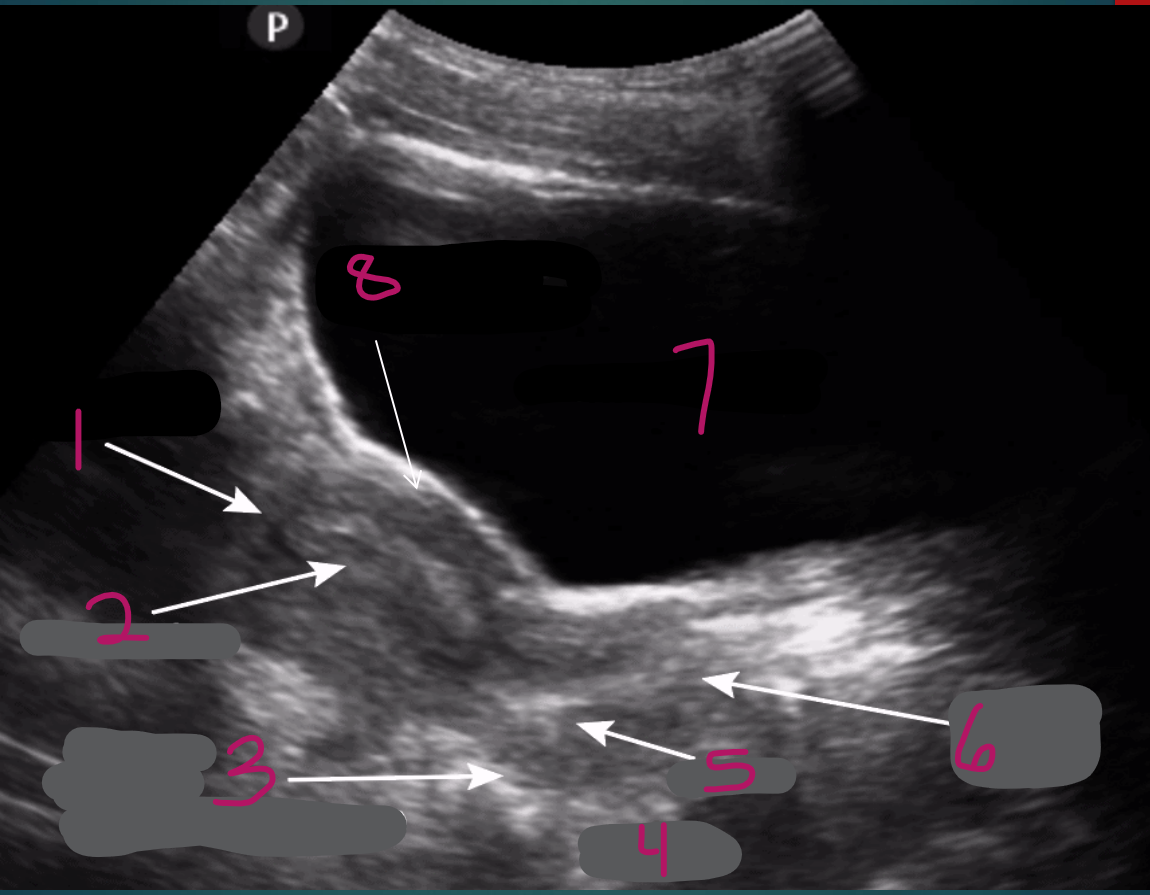
6
Vaginal stripe
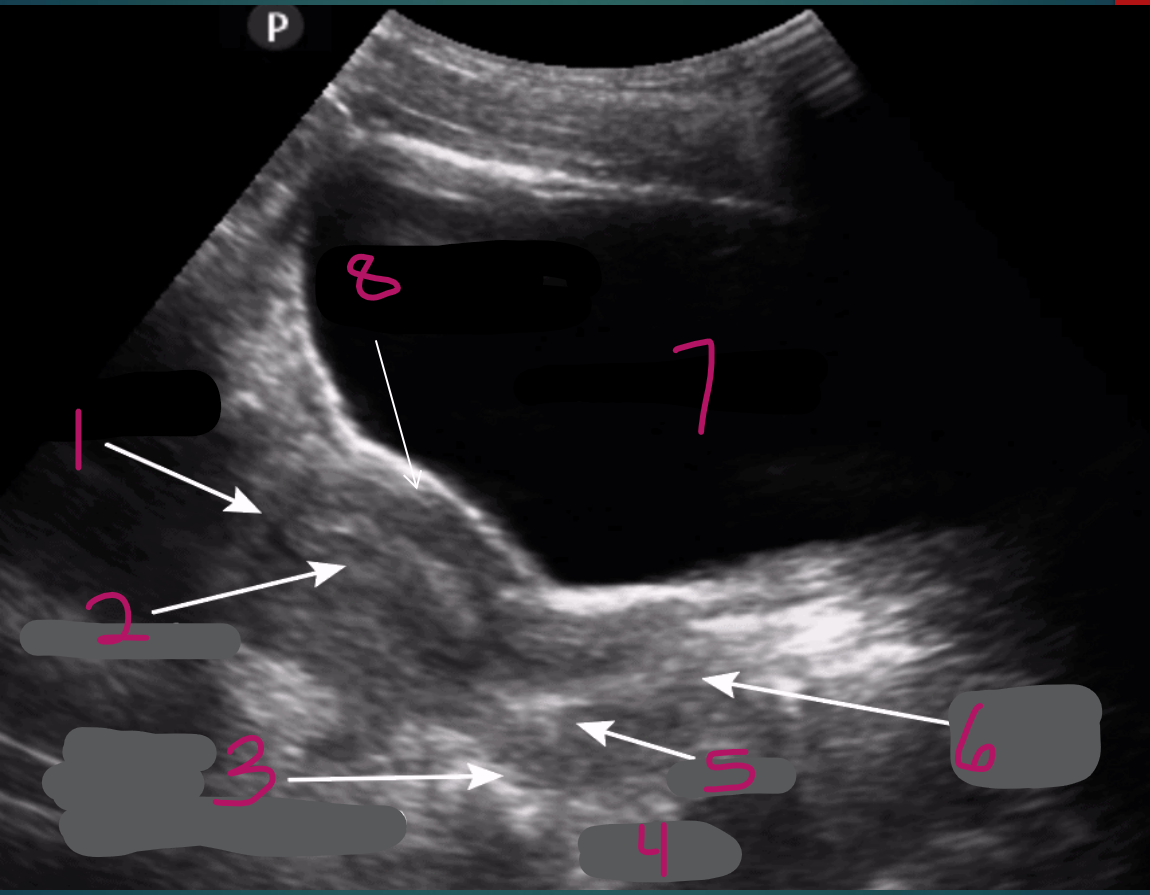
7
Full bladder
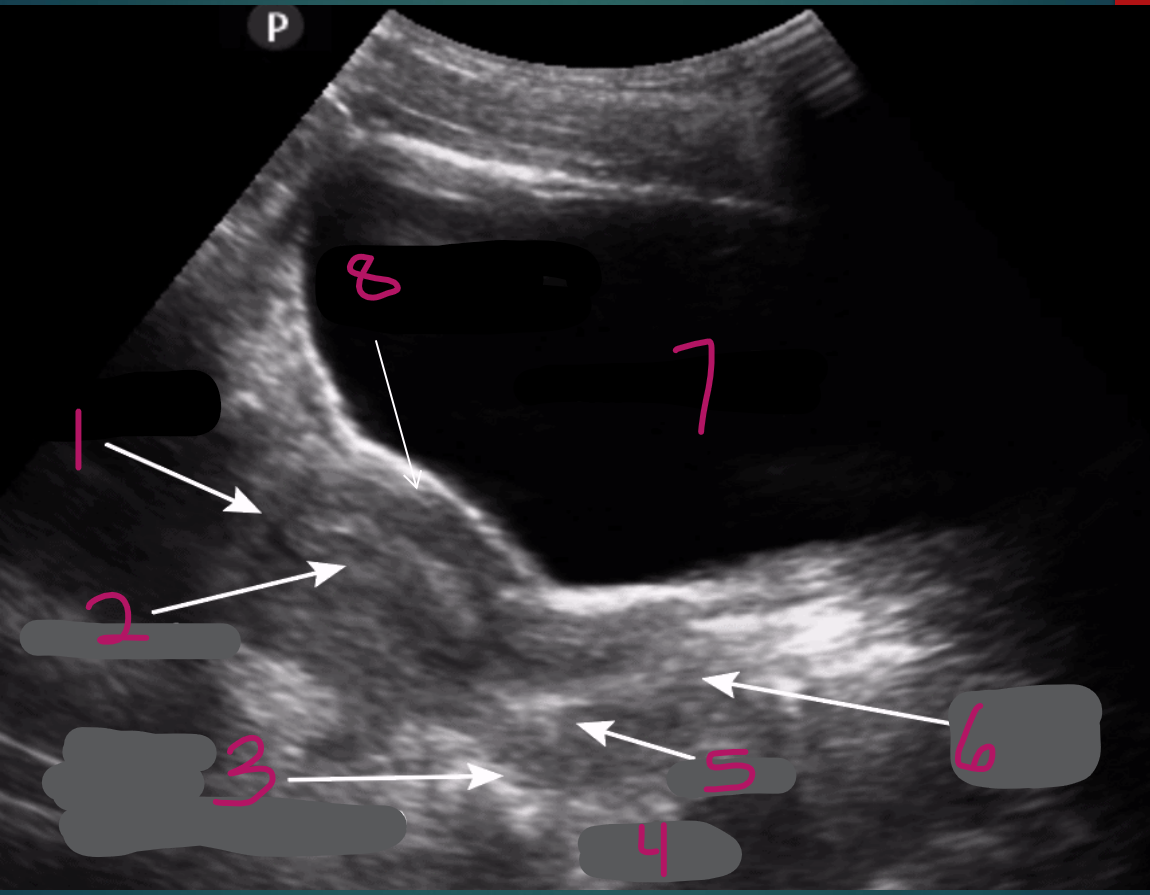
8
Vesicouterine pouch (anterior cul-de-sac)
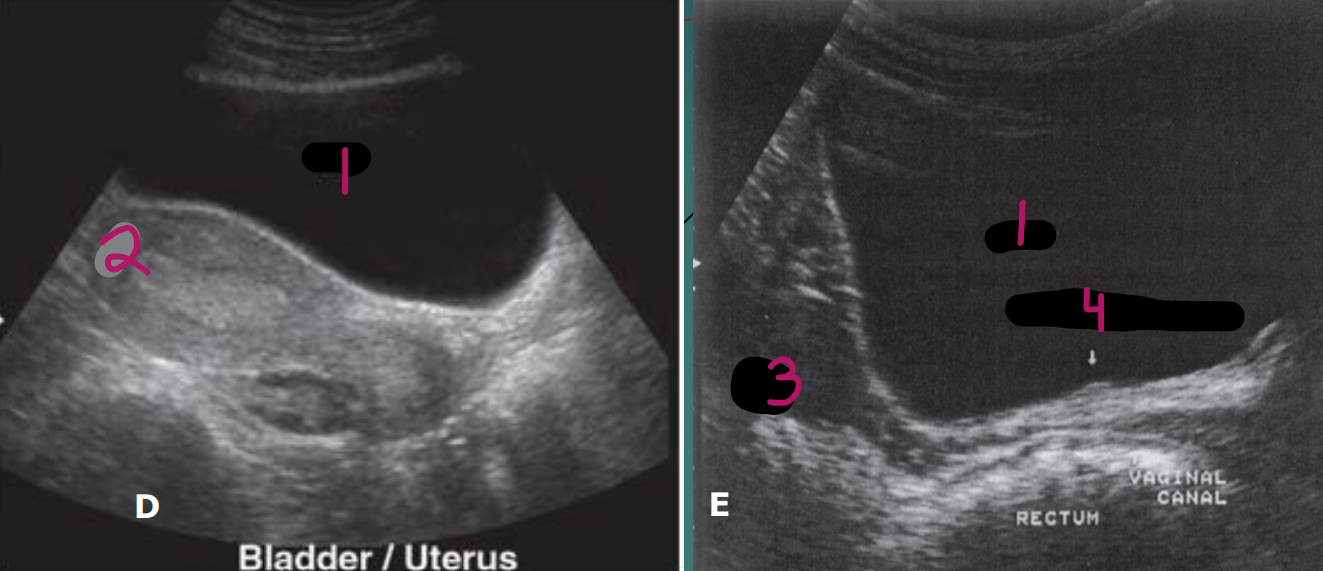
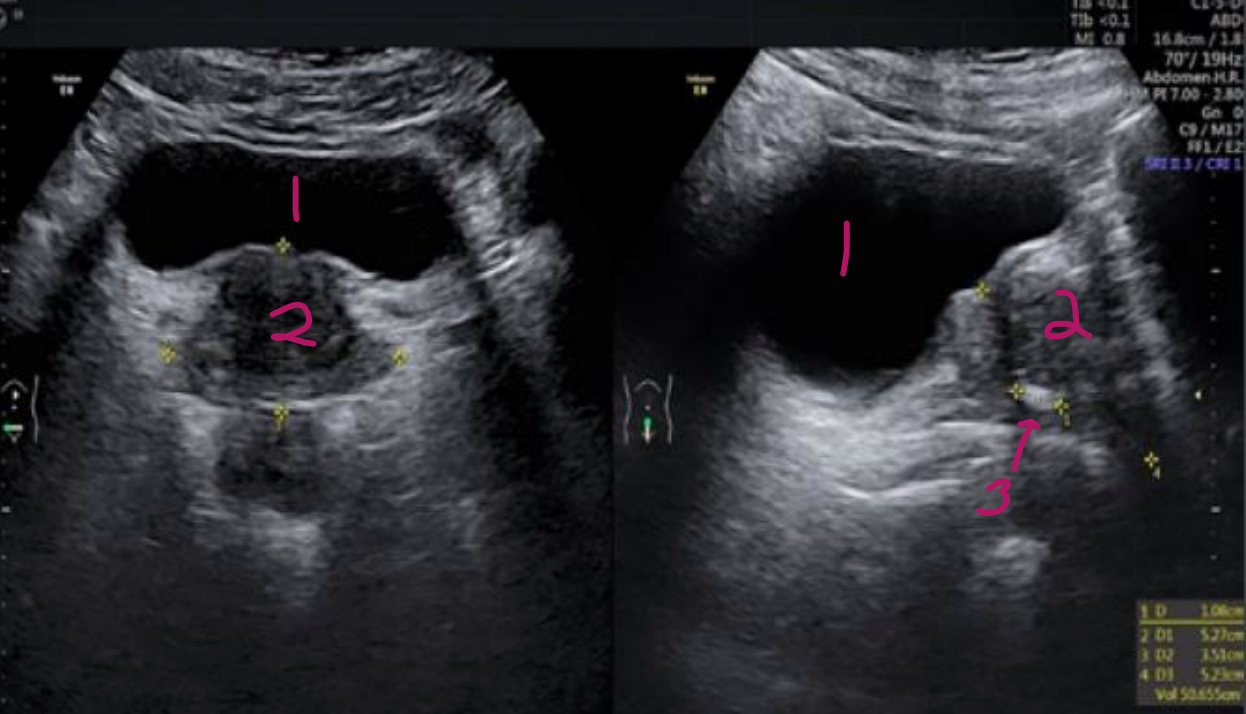
1
Bladder
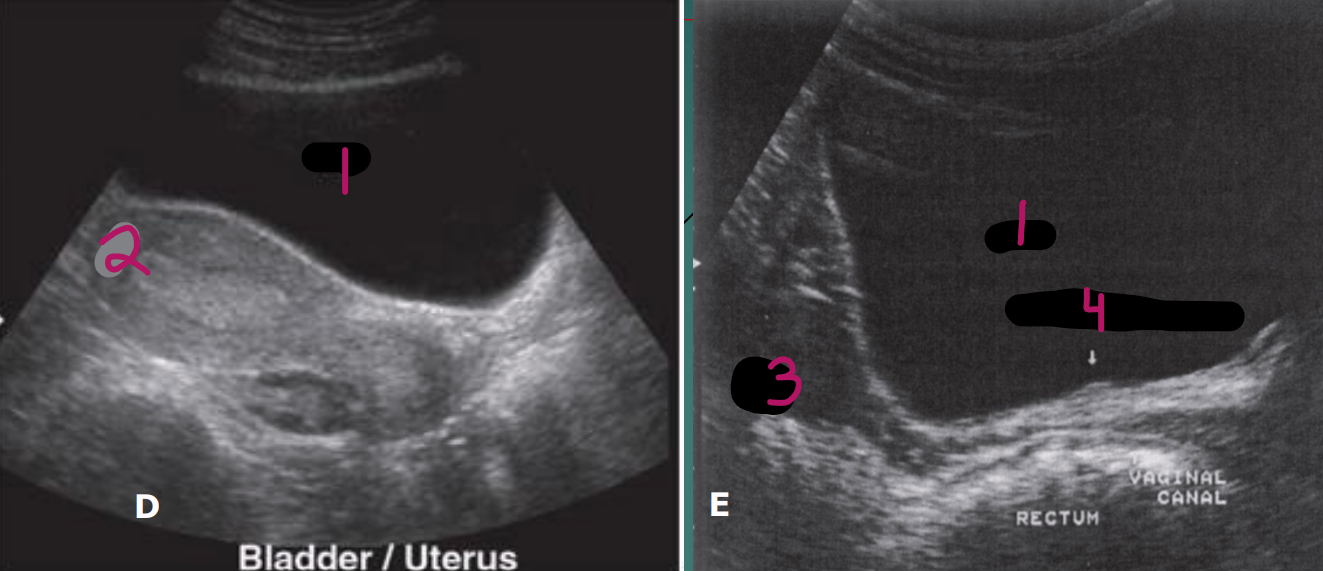
2
Uterus
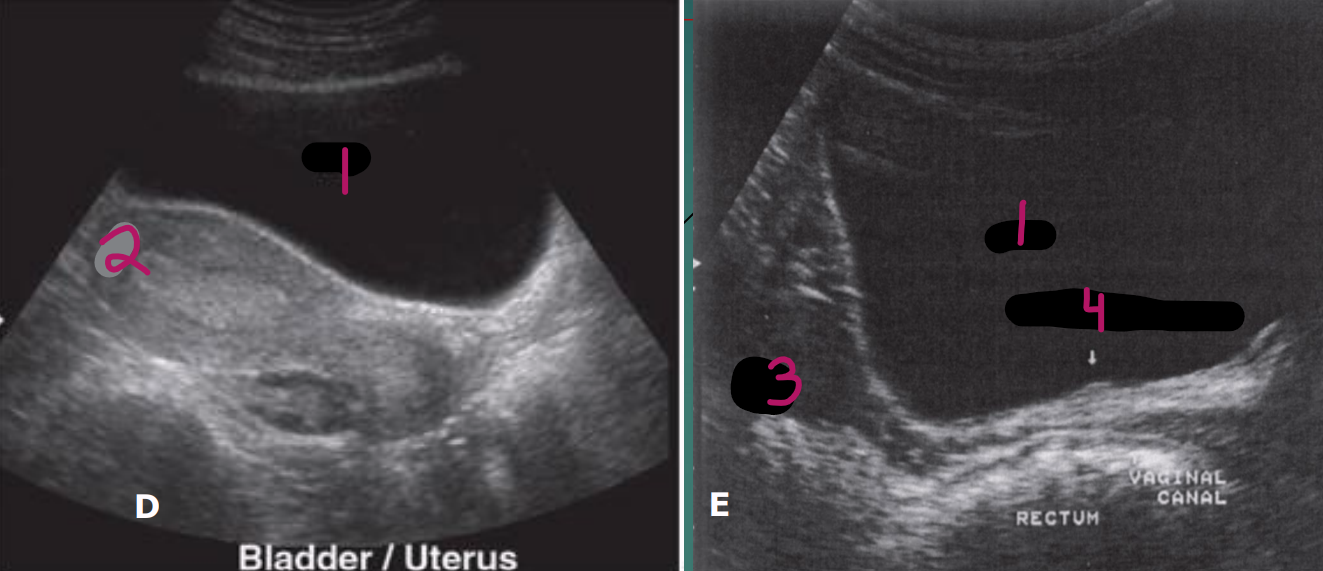
3
Ovary
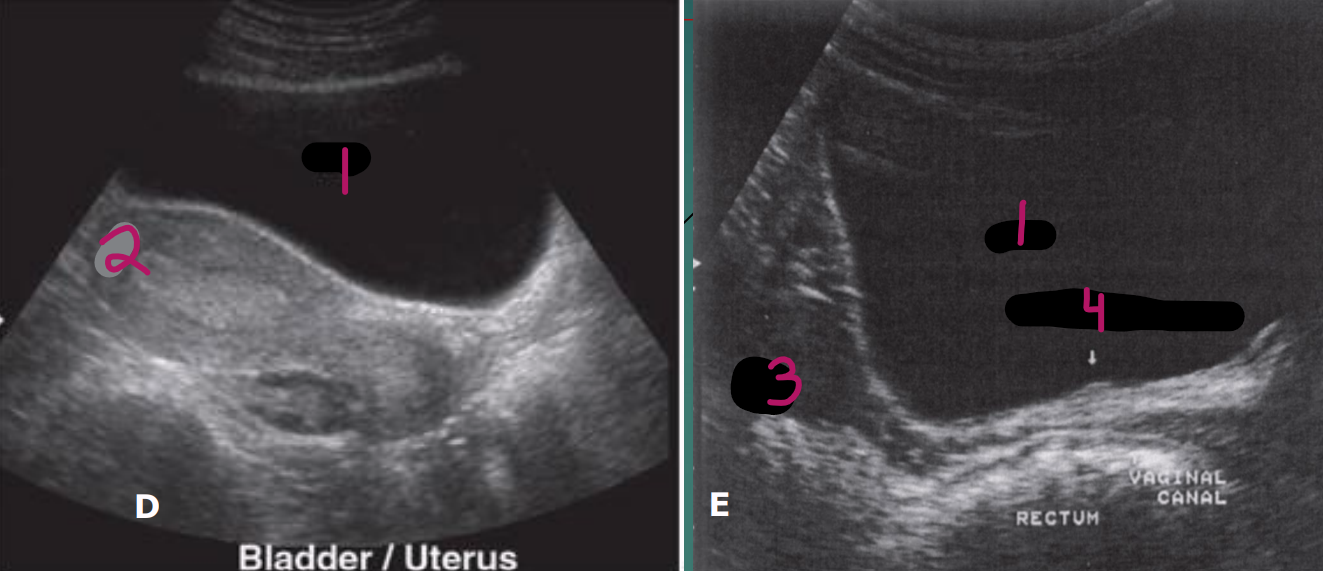
4
Right ureteral orifice
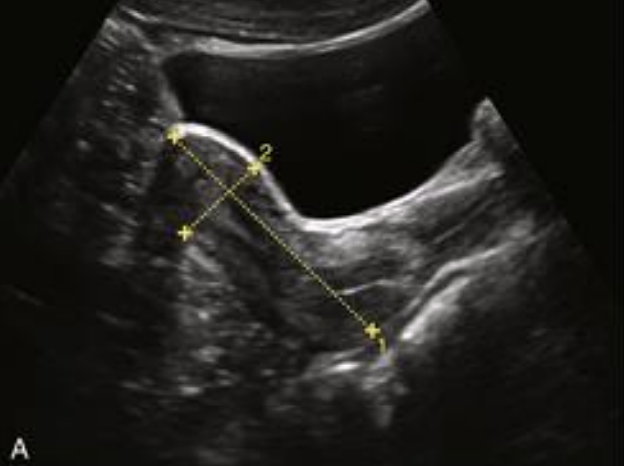
What is shown in this image?
Long image of uterus and bladder

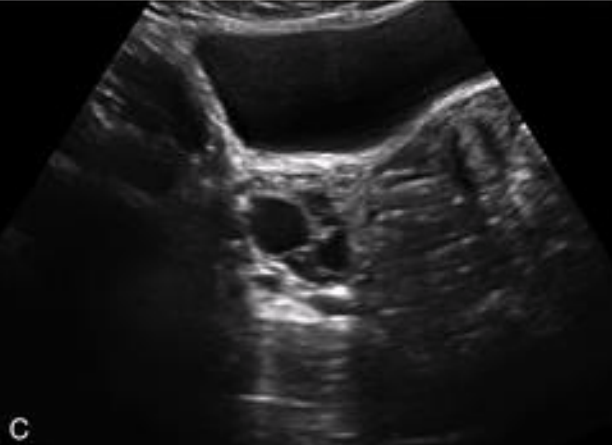
What is shown in this image?
Trans image of uterus and bladder
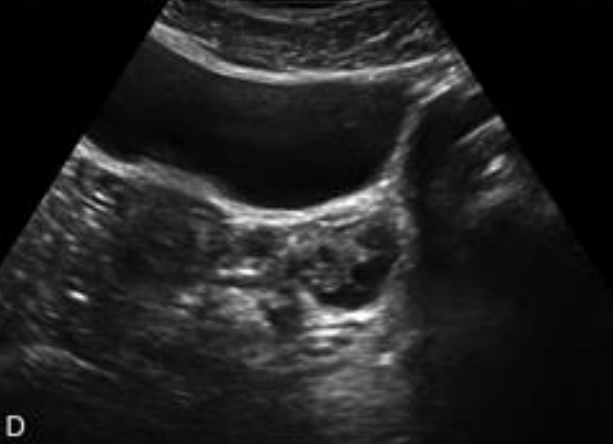
What is shown in this image?
Trans image of right ovary and bladder
What is shown in this image?
Trans image of left ovary and bladder
1
Bladder
2
Seminal vesicles
1
Bladder