PSYC 2301 Final Exam
1/201
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
202 Terms
Factors that Influence symptoms
- Individual differences/personality
- Cultural differences
- Situational factors
- Stress
- Mood
Schema (illness representation)
A patients own beliefs about their illnesses; what they know about their disease/symptoms - helps them to explain.
Five components of illness schemas
- Identity (label)
- Consequences
- Causes
- Duration
- Cure
Models of illness
Most individuals have 3 models of illness:
- Acute illness
- Chronic illness
- Cyclic illness
Acute illness
Bacterial or viral, short duration.
E.g. standard cold or flu; lasts a couple of weeks and then it is gone.
Chronic illness
Multi-factorial, long duration. Usually have for life; no clear cure.
E.g. Diabetes
Cyclic illness
Alternating period of activity - being sick, and then being well, etc.
Interpretation of symptoms - additional influencers
- Lay referral network - input from friends, family, peers
- Internet - background info, lifestyle modification
Predictors of Health Service Users
- Age
- Gender
- Socio-economic status (SES)
- Culture
- Social psychological
Age
- Newborns use the system during birth
- Children/teens use it less (generally healthy)
- Late adulthood - health complications start; access of system increases
- Elderly - use the system the most
Gender
- Women use the system more than men
- Women give birth, are more prone to seeking help, more proactive, etc.
Socio-economic status (SES)
- High SES = less use of system, more use of specialists
- Low SeS = high use of system, less use of specialists
Culture
- Visible minorities use the system more; less use of specialists
- Ethnics made 4 + visits
- Linguistic barriers - seen a lot in Canada
- Perceived quality of care
Social Psychological
- Individual attitude/beliefs about symptoms and health care (if you think negatively about the system, you are most likely going to have a negative experience; negative thinking)
- Health belief model predictors:
1. Perceived threat to health - perception of severity influences help seeking
2. Belief of efficacy of intervention - knowing that there is a clear treatment will increase likeliness to seek help. Not knowing decreases likeliness.
Misuse of Health Services
Instances where the system is used incorrectly:
- Physical symptoms associated with emotional disturbances
- Symptoms triggered by psychological drivers
- Worried well individuals
- Somatacizers
- Secondary gains
Symptoms triggered by psychological drivers
o University students' disease
o Inappropriate assessment by patient (physician vs. specialist)
o Limited access - quicker/easier to see a doctor for physical health than a psychologist/psychotherapist for mental health
Worried well individuals
Individuals who place over emphasis on symptoms due to heightened self-care; use system a lot for small things.
Somatacizers
People who express symptoms after personal or emotional insult; expressing physical symptoms from overwhelming change in your life.
E.g. getting dumped and feeling like crap
Secondary gains
Downstream benefits arising form the illness, such as:
- Time off/rest
- Removal from responsibilities
- Medical (physical ability limited) vs. psychological symptoms (PTSD, resulting in reassignment for work)
Delay Behaviour
Patients live with one or more potentially serious symptoms without proper care.
- Delay = time between recognition and treatment.
Types of Delay Behaviour
Composed of several time periods:
- Appraisal delay
- Illness delay
- Behavioural delay
- Medical delay
- Treatment delay
- Provider delay
Appraisal delay
Symptom is serious.
- The time from noticing the symptom and believed it is serious.
Illness delay
Symptom implies an illness.
How long it takes you to believe that it is an actual illness.
Behavioural delay
Time between recognition and treatment.
How long it takes you to modify your behaviour and go to the doctor.
Medical delay
Time between appointment and treatment.
How long it takes you to see a professional.
- Out of your control, and is a problem with our system
Treatment delay
Occurs after primary visit due to:
- Curiosity being satisfied by the first visit
- Fear/alarm of symptoms/diagnosis
Provider delay
Occurs due to physician or treatment algorithm.
- If you need to do a bunch of things before you can start the treatment
- If the doctor needs to figure something out before providing treatment
Predictors of Delay Behaviour
- Elderly delay less
- Lack of regular physician
- Personal views/fears
- Frequency of symptom occurrence
- Personal safety assessment of symptom: highly visible, degree of pain, degree of change, incapacitating
Health Care Providers
- Phsyician
- Physician assistant
- Nurse practitioner
- Nurses
- Health educators/nutritionists
- Psychologists/psychotherapist
- Physiotherapists
- Social Workers
NOTE: Cannot limit conversation to only doctors.
Today's Patient
- Delivery of care can influence perceived cafe
- Patient consumerism - want to be more involved in decision making
- Internet is a resource
- Visits are brief & interrupted; disclosure is difficult
NOTE: Takes a doctor 17 seconds to make a diagnosis.
Structure of Health Care Delivery System
1. GP - primary providers: point of entry; gate keepers
2. Specialists - secondary providers
Disadvantages of Health Care Structure
- Requires a referral to see a specialist, which takes time
- Many people do not have a primary physician
Complimentary & Alternative Medicine (CAM)
Includes:
- Massage therapy
- Chiropractic care
- Acupuncture
- Homeopathy
Often layered on top of regular medical practice, creating a more holistic approach than just medicine alone.
Why Do People Use CAM
- Users tend to be female, middle-aged & highly educated with multiple chronic issues
- Higher SES scale - benefits and open-mindedness
- Gives people a sense of control
- Shorter wait times
- More commonly used by people with good jobs because it is covered (related to SES)
Changes in Philosophy
- More women working in field
- Physicians are no longer "God"
- Western practice influenced by Eastern medicine - vitamins, stretching, breathing, yoga, etc.
- Holistic approach (well-rounded; all-encompassing)
Holistic Approach
- Health is a positive state
- Healthy is not simply disease-free
- Health education, self-help and self-healing
Barriers to Care
- Poor communication
- Jargon
- Babytalk/elderspeak
- Nonperson treatment (depersonalization)
- Stereotyping (E.g. cultural, sexism, etc.)
Non-adherence
When the patient does not follow the prescribed treatment; this is very common.
Creative non-adherence
When patients modify and/or supplement prescribed treatment.
E.g. Forgetting to take a morning and lunch pill, and then taking 3 at bed time to even it out.
Causes of non-adherence
- Poor communication - explanation for treatment must be clear
- Perceived satisfaction - if they have a positive experience with the doctor, adherence is more likely
- Treatment regimen - complexity of treatment
- Type of treatment - high adherence for medical treatment; lower for vocational; lowest for social/psych treatment
Placebo Effect
Any medical procedure/agent that produces an effect in a patient because of its therapeutic intent and not its specific nature, whether chemical or physical
- Have been reported and used for centuries
Placebo effect process
- Non-active agent vehicle is given in place of a drug (e.g. tic tac)
- Patient reports a therapeutic effect
How does Placebo Effect work?
- Indirect physiological responses - knowing that you are actually getting a "pill" can lower stress & anxiety
- Possible release of endogenous opioids (fMRI data)
Factors that Influence Placebo Effect
- Interaction with health care provider/researcher
- Patient characteristics - optimist vs. pessimist; anxious = higher placebo effect
- Physical appearance/administration of placebo
Single-blind experiment
Experimenter knows who gets the placebo and who doe not.
Experimenter has potential to bias results.
Double-blind experiment
Experimenter and participants do not know who gets the placebo and who does not; gold standard because it eliminates bias.
Classifications of pain
- Acute pain
- Chronic pain
Acute pain
- Shorter duration; goes away with time
- Caused by soft tissue damage
- Infection
- Inflammation
Chronic pain
- Lasts longer; can be indefinite
- Linked with long-term illness or disease
- May have no apparent cause
- Can trigger other issues
- Difficult to assess & diagnose (can be subjective)
Types of Chronic pain
- Chronic benign
- Recurrent acute pain
- Chronic progressive
Chronic benign
- lasts for 6 + months
- Resistant to treatment/no treatment
- Things to do to mask symptoms, but thats it.
E.g. Lower back pain
Recurrent acute pain
Series of intermittent episodes; cyclical
E.g. Migraines, TMJ
Chronic progressive
- lasts for 6 + months
- Increasing severity; progressive
E.g. Rheumatoid arthritis
NOTE: To be considered chronic, you need to feel pain more often then not.
Why is pain difficult to study?
It is subjective, and canoe hard to pinpoint where the pain originates from.
Factors influencing Pain
- Cultural differences
- Gender
- Coping styles
Cultural differences
- Some cultures report pain sooner and more intensely
- Linked to cultural norms
E.g. Asian cultures do not mention it as much as Western cultures
Gender
- Women are more sensitive to pain - menstrual cycle contributes
- Differences in emotional processing of pain
- Men tend to internalize pain
Coping style
- Catastrophizing = heightened experience of pain
- Resilience & positive emotions = lowers experience of pain
Measuring pain
- Based on self-report
- Hard to measure; no gold standard of measurement
Common used tools:
- Verbal reports
- Pain behaviour
- BPS model
Verbal reports
- Experience and vocabulary
- McGill Pain Questionnaire
- Pain Catastrophizing Scale
Pain behaviour
Observable behaviours that arise from pain:
- Facial & audible expressions
- Distortions in posture and gait
- Negative affect (depressed, upset)
- Avoidance of activity
Nociception
The system that carries signals of damage and pain to the brain (internal process)
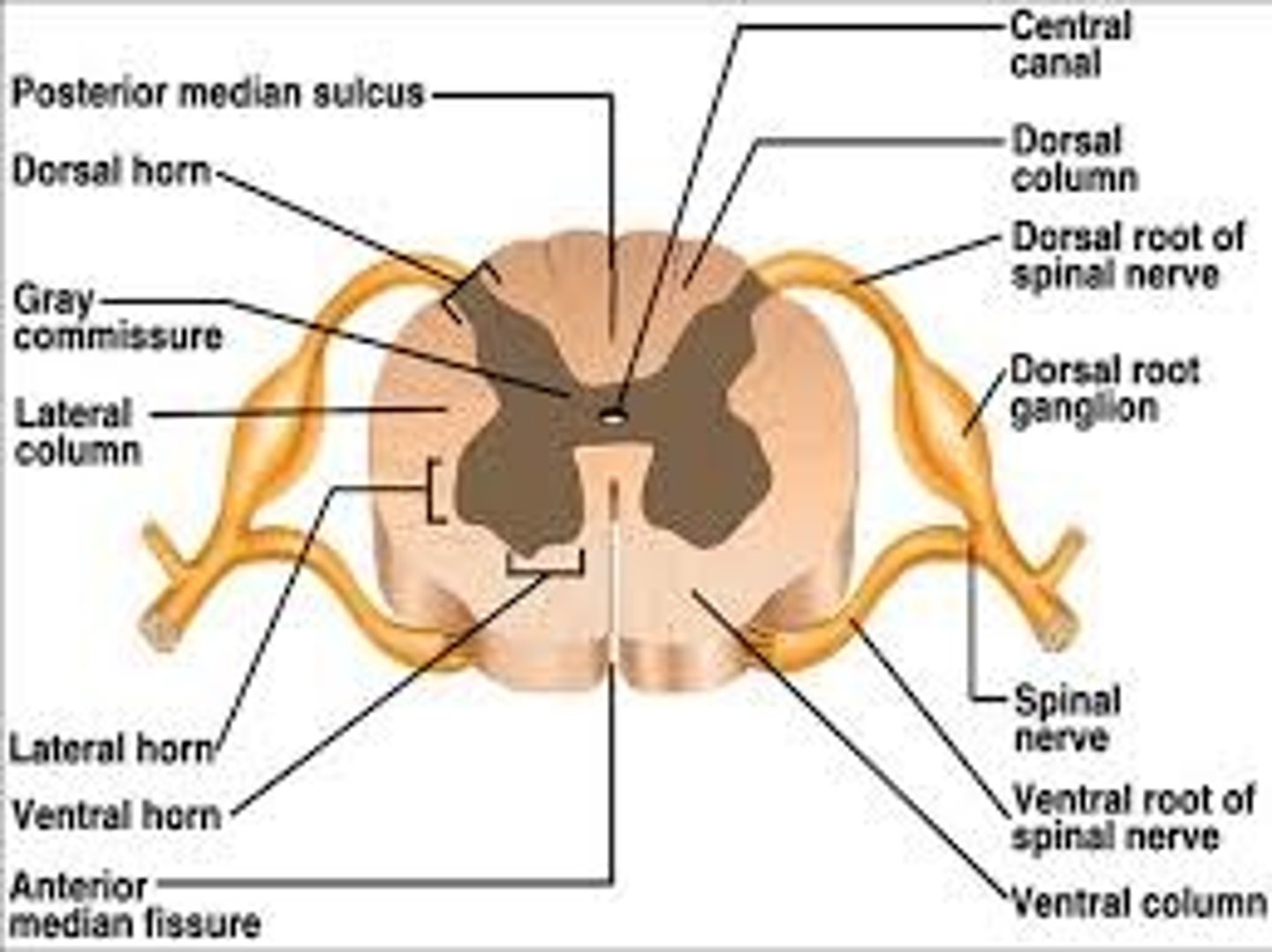
- Nociceptive neurons have cell bodies in the dorsal root ganglia
- Can detect mechanical, thermal and chemical stimuli
Polymodal nocicpetion
Ploy = more than one
Modal = method
There are multiple ways we can experience pain; they can happen simultaneously.
Nociception transmission
- Bidiretional axons synapse in dorsal horn of the spinal cord
- Signal travels to brain where it is processed
- Nociception occurs through several types of peripheral nerve fibres
Types of Peripheral Nerve Fibres
- A-delta fibre
- C-fibres
- A-beta fibres
A-delta fibre
- Small, myelinated fibres - fast (more myelination you have, the faster the signal)
- Transmit first pain and sharp pain rapidly
- Opens gate - allow us to experience pain
C-fibres
- Unmyelinated fibres (slower)
- Transmit secondary dull or aching pain
- Opens gate - allow us to experience pain
A-beta fibres
- Large diameter myelinated fibres (larger in size)
- Transmit information about vibration and position
- Supporting and changing what is happening around the experience of pain
- Closes gate - prevent us from experiencing pain
Traditional model of pain
- Suggested pain resulted form transmission of pain signals to the brain.
- Degree of pain was dictated by tissue damage
Pain Gate Theory
- Psychological factors contribute to experience of pain
- Open gate: experiencing pain; a-delta and c-fibres
- Closed gate: lessening pain; A-beta fibres
NOTE: Think of it like a dam.
Other factors that open/close gate
- Physical - extent of injury
- Emotional - anxiety/worry, tension, depression open gate; relaxation closes gate.
- Cognitive - Focus on pain, boredom open gate; involvement/interest in life activities close gate.
Weakness of Gate Control Theory
- Cannot explain phantom limb syndrome (PLS)
Neuromatrix
- Representation of a unified physical self
- Initially genetically determined
- Neurosignature can give rise to pain where a limb is no longer present
Pain Management
Body produced endogenous (from within) opioids to help deal with pain.
- Beta-endorphines - peptides that protect to the limbic system, brainstem
- Proenkephalin - peptides found in endocrine and CNS
- Prodynorphins - peptides in the gut, pituitary, brain
- Acute stress & physical activity reduce sensitivity to pain
Traditional Pain Management
- Pharmacological - medications
- Surgical - lesions of pain fibres in the brain
- Sensory techniques - counter-irritation (creating an "X" on a bug bite), massage, exercise
Psychologist Pain Management
- Biofeedback - understanding the symptoms from your body and planning accordingly
- Relaxation
- Hypnosis
- Acupuncture
- Distraction
Components of Chronic Pain
- Physiological
- Psychological
- Social
- Behavioural
NOTE: All are part of the BPS model
- Very individual experience
Pain & Personality
Chronic pain patients show elevated scores in:
- Hypochondria
- Hysteria
- Depression
AKA the neurotic triad
- Chronic pain associated with depression, anxiety and substance abuse
Chronic illness definition
- Long-lasting
- Long-term effect on body
- Range from relatively mild - severe
- Can be born with it, or can be developed
Factors of chronic illness
- Genetics (hereditary) - Alzheimer's, MS
- Environmental - cancer, asthma
- Lifestyle - CVD, HIV, gout
- Previous injury or prolonged strain
Most common in:
- Women
- Lower income
- Seniors
- Certain ethnic populations (Aboriginal)
Quality of Life
- Standard of health, happens and comfort experienced in someones life
- Different from standard of living
Standard of living = money, car, house, etc.
Helps determine psychological contribution:
- Depression
- Anxiety
- Distress
- Stress
NOTE: All are impacted by QOL, and visa versa
Components of Quality of Life
- Physical functioning
- Psychological status
- Social functioning
- Disease or treatment-related symptomology
QOL assessment
- Assessment tools can gauge QOL
- Gauge the extent to which normal life activities have been compromised
- Population norms can be established
- Allows for comparisons between countries
E.g. SF-36, and WHOQOL-BREF (BPS evaluation)
Evaluating QOL
QOL can fluctuate throughout a lifetime.
This is influenced by:
- Characteristics of the illness
- Acute changes in symptoms
- Age-related changes over time
- Culture
Why Study QOL
o Documentation or history
o Identify trends between illness and QOL factors
o Impact of treatment on QOL
o Comparative effectiveness between treatments
o Inform decision and policy makers
NOTE: If someone has multiple chronic disorders, you evaluate QOL based on all of the diseases combined.
Emotional Phases of Chronic Illness
1. Denial - may interfere with treatment
2. Anxiety - increased self-vigialenge; may hinder treatment
3. Depression - increases illness symptoms; increases with severity of illness.
Self-esteem
General evaluation of self-concept.
Self-concept
Stable set of belief's about one's qualities and attributes
NOTE: When your self-concept & reality do not align, this threatens your self-esteem
Composition of Self-Concept
Self-Concept is composed of:
- Physical self
- Achieving self
- Social self
- Private self
Physical self
- Body image (self-perception of physical look/function)
- Poor body image linked to low self-esteem, anxiety & depression
Achieving self
- Job/hobbies contribute to self-esteem/concept
- May be used as a motivator
Social self
- Social interaction helps with self-esteem
- Source of information and support
Private self
- Internal dialogue; helps you to work through things.
- Increased dependence on other can decrease experience of private self
- Loss of an unrealized dream
Active coping
May cause psychological distress
Avoidant coping
Less psychological distress, better overall outcomes
Physical rehabilitation goals
o Use your own body as much as possible
o Sense changes in the environment
o Learn new physical management skills - use your body in other ways
o Learn a necessary treatment regimen
o Learn how to control expenditure of energy
Benefit finding
Acknowledgement of the positive effects of chronic illness.
Positive Changes with Chronic Illness
- Re-evaluation of priorities
- Strengthening of priorities
- Strengthening of relationships
- Realization of one's abilities
- Lifestyle changes
NOTE: The type of disease you have can impact the changes you make.
Psychological Interventions for Chronic Illness
- Individual therapy (medical vs. psychotherapy) - talking about your problem
- Brief psychotherapeutic interventions
- Patient education - internet, expressive writing, self-education
- Relaxation, stress management, exercise
- Social support interventions (support group)
- Family support
Death in Infancy or Childhood
- Infant mortality is high
- Location and SES are contributors
- Sudden Infant Death Syndrome (SIDS) is the most common cause
- Other factors: accidents, cancer
NOTE: Children have a poor understanding of death until age 9 - 10