BIO20: IMMUNE AND EXCRETORY SYSTEM
1/117
Earn XP
Description and Tags
Immune system and Excretory system.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
118 Terms
Pros and Cons of Xenotransplants
✅ Pros of Xenotransplants
Solves Organ Shortage Crisis
There’s a major shortage of human donor organs. Xenotransplants (especially from pigs) could help meet demand.
Readily Available Supply
Animals like pigs can be bred specifically to supply organs, providing a steady, scalable source.
Shorter Waiting Times
Patients wouldn’t need to wait months or years on transplant lists.
Medical Advancements
Research into xenotransplants leads to improvements in immunosuppressive therapy, genetic engineering, and organ preservation techniques.
❌ Cons of Xenotransplants
Immune Rejection
The human immune system strongly reacts to foreign animal tissues (hyperacute rejection), requiring strong immunosuppressants.
Risk of Zoonotic Diseases
There’s a risk that animal viruses (like porcine endogenous retroviruses, PERVs) could transfer to humans.
Ethical Concerns
Ethical issues include animal welfare, genetic modification, and the acceptability of using animals in this way.
Shorter Graft Survival
Even with suppression, xenografts often fail sooner than human transplants due to incompatibilities.
High Cost and Technical Complexity
Developing safe and viable xenotransplants is expensive and technically challenging.
Plasma
The liquid component of blood that carries cells nutrients, hormones, and waste products.
Erythrocytes (Red blood cells)
A blood cell that carries oxygen using hemoglobin. Has no nucleus.
Anemia
A condition where there’s a deficiency of red blood cells or hemoglobin, leading to reduced oxygen delivery.
Leukocyte (White blood cell)
A white blood cell that is involved in defending the body against infections and foreign substances.
Platelets
Cell fragments in blood that help with clotting. Prevents us from bleeding out.
Thrombus
A blood clot that forms in a vessel and stays there. (Forms when blood flow is stagnant/blood vessel wall is damaged, etc.)
Embolus
A clot or other substance that travels through the bloodstream and can block a vessel. (Piece of thrombus that travels through the bloodstream.)
Blood types
Categories (A,B,AB,O) based on specific antigens on red blood cells.
Antigen
A molecule on the surface of cells that triggers an immune response.
Antibodies
Proteins produced by the immune system that bind to specific antigens.
Rhesus Factor
An additional antigen (positive/negative) on red blood cells important for blood compatibility.
Agglutination
Clumping of red blood cells due to incompatible blood types interacting.
Immune System
Organs and processes of the body that provide resistance to infection and toxins.
All blood cells are produced in the BONE MARROW.
Blood is a type of tissue (Fluid tissue)
STEM CELLS of the BONE MARROW give rise to BLOOD CELLS.
Components of blood
An average person has about 5 litres of blood.
55% plasma, less than 1% white blood cells, 45% red blood cells.
What is plasma composed of?
90% water with these compounds suspended or dissolved: blood proteins, nutrients, minerals, waste products, and dissolved gases.
3 types of proteins in the blood
Albumins: For osmotic balance
Globulins: Antibodies, immunity
Fibrinogens: Blood clotting
Role of Erythrocytes
Primary function is to transport oxygen from the lungs → tissues
Contain hemoglobin, increasing the availability of blood to carry oxygen.
There are 280 million hemoglobin molecules in one red blood cell!
Structure of the red blood cell (What is it composed of?)
NO NUCLEUS: Allows for more room for hemoglobin, thus increasing the amount of oxygen and CO2 each red blood cell can carry.
BICONCAVE DISCS: Gives a large surface area to volume ratio. This means that there is a lot of membrane over which gas exchange can occur.
How does a Erythrocyte’s small size make it perform more efficiently?
They are small enough to squeeze through capillaries. This slows down the flow of red blood cells, making gas exchange in the capillaries more efficient bc the red blood cells are there longer.
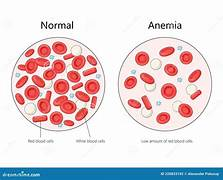
Normal blood vs Anemia
Anemia: Deficiency in hemoglobin or red blood cells. (Decreased oxygen delivery to tissues, low energy levels.)
Possible causes: Hemorrhage (Physical injury), dietary deficiency of iron.
How does blood clotting work?
Blood clots form when a blood vessel is damaged, platelets are activated to create a ‘plug’ to stop bleeding. The protein ‘Thromboplastin’ is released from platelets to start this process.
Damaged blood vessel → Formation of platelet plug → Development of clot
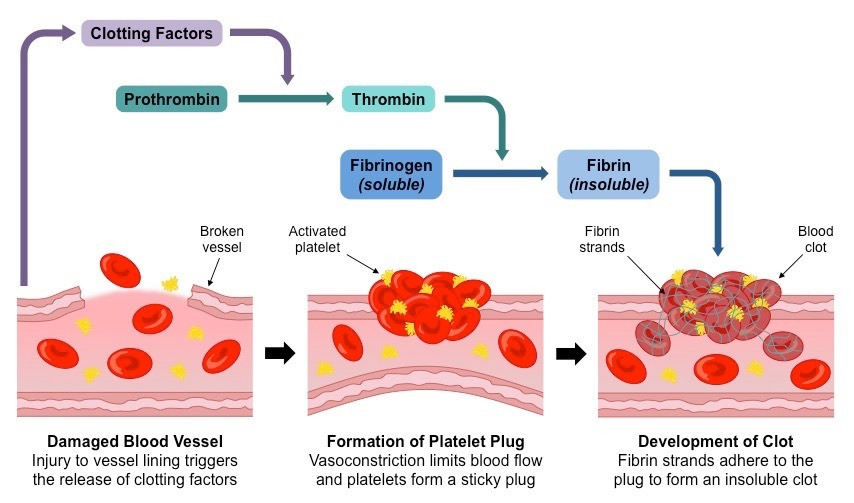
Thrombocytes (Platelets)
Function: Blood clotting (prevents entry of bacteria and further loss of blood, and allows the wound to heal.)
Platelets are small cell fragments consisting of cytoplasm surrounded by the cell surface membrane.
Do NOT contain a nucleus.
How can blood clotting be harmful?
Although blood clotting preserves life, it can also result in life-threatening situations.
The embolus (a fragment of blood clot) can become stuck in another vital organ because it is carried by the circulatory system.

Antigen
A substance that stimulates the reformation of an antibody. (Foreign Substance)
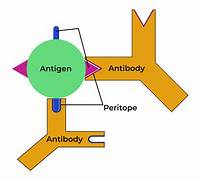
Antibody
The protective protein produced by the immune system in response to the presence of a foreign substance.
Antibodies recognize and latch onto antigens in order to remove them from the body.
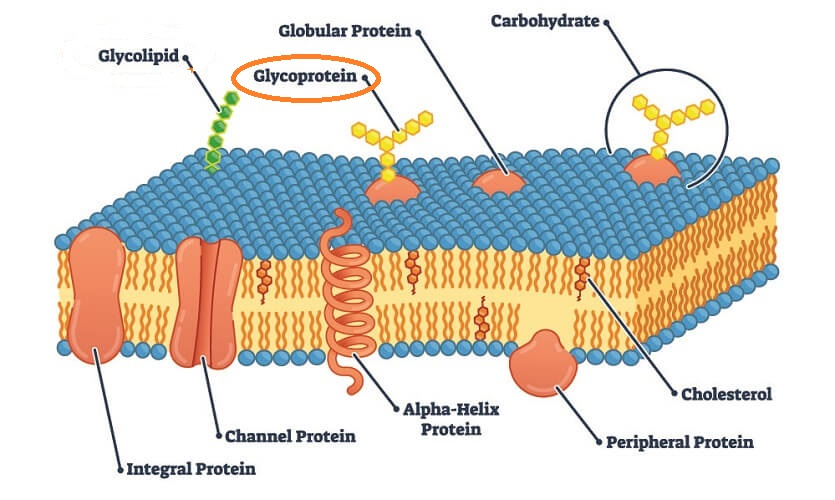
Glycoprotein makers
The membrane surface of the red blood cells may contain different types of glycoprotein makers.
Glycoprotein markers are proteins on the surface of cells that have attached sugar chains (glycans). These structures help the immune system recognize and differentiate self vs. non-self cells.
Important in immune recognition, cell communication, and blood typing (e.g., ABO groups).
Act as antigens—if foreign, they trigger an immune response.
Used by the body to detect pathogens, infected cells, or transplanted tissues.
What are the 4 human blood types?
These glycoprotein makers act as antigens. For each antigen there is a corresponding antibody. Ppl do NOT produce the antibody that attack their own antigens on their red blood cells.
A: A maker
B: B maker
AB: Both A and B maker
O: None
Blood type AB does NOT produce any antibodies.
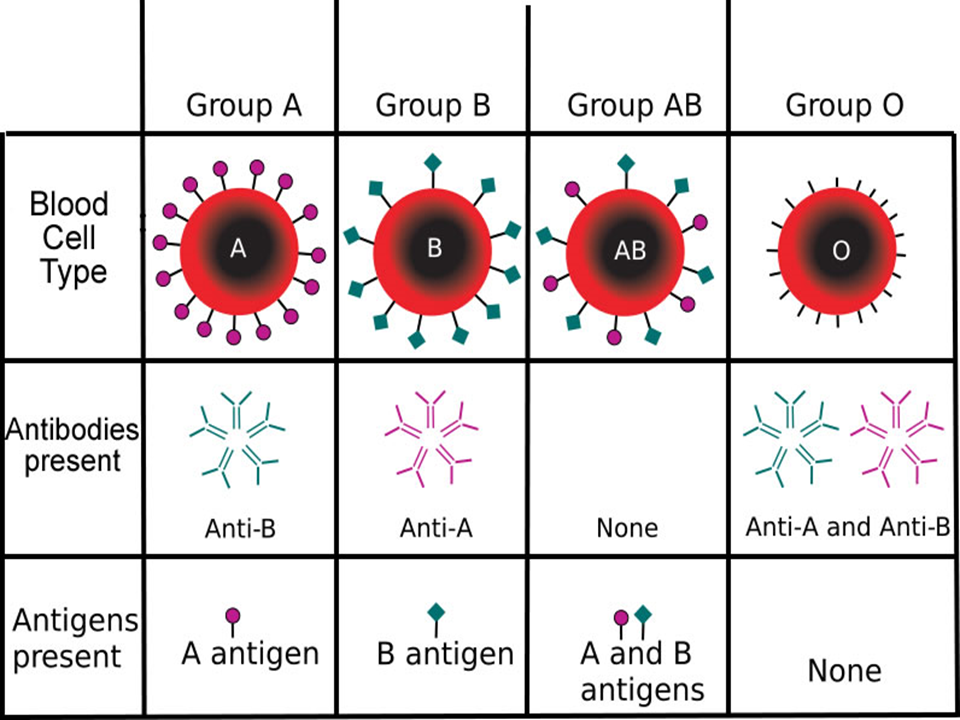
Which blood type has no antibodies and which blood type has no antigens?
No antibodies: AB (Universal acceptor (+))
No antigens: O (Universal donor (-))
What would happen if an individual with blood type O received blood that was type A?
They would experience a severe immune reaction because their anti-A antibodies attack the foreign A antigens, destroying the donor red blood cells. This causes life-threatening complications like kidney failure and requires emergency treatment. (Type O can only receive type O blood.)
Agglutination
Clumping of the blood cells caused by antigens and antibodies.
When blood of an incompatible type is transfused, the red blood cells of the donated blood AGGLUTINATE.
Type O are universal donors, type AB are universal recipients.
Rhesus Factor
A type of antigen
Positive (+): You have the Rh factor
Negative (-): You do not have the Rh factor
It is another source of blood incompatibility.
Ppl who are Rh- CAN donate blood to Rh+ individuals, but should NOT RECEIVE Rh+ blood.
Erythroblastosis Fetalis
Rh+ babies and Rh- mothers
Rh- woman with Rh+ fetus → cells from Rh+ fetus enter woman’s bloodstream → Woman becomes sensitised, antibodies (O) form to fight Rh+ blood cells. → In the next Rh+ pregnancy, maternal antibodies attack the fetal red blood cells.
Phagocytosis
process where cells engulf (eat ) and digest pathogens/debris.
Macrophage
A large immune cell that performs phagocytosis and activates other immune responses.
Pus
Thick fluid of dead white blood cells, bacteria, and tissue debris at infection sites.
Inflammatory response
Body’s reaction to injury/infection (redness, heat, swelling) to isolate and heal damage.
Complement protein
proteins in blood that help antibodies clear pathogens (lysis, tagging, inflamation)
T cell
Immune cell (Lymphocyte) that targets infected/cancerous cells (Adaptive immunity)
B cell
Immune cell that PRODUCES antibodies against pathogens.
Receptor sites
Protein structures on cells that bind specific molecules (ie. Antigens, hormones) (Ie2. A B cell’s receptor binds to a virus’s antigen → triggers antibody production.)
Helper T cell
Coordinates immune response by activating B cells, Killer T cells, and macrophages.
Killer T cell
Destroys infected/cancerous cells directly.
Memory B cell
“Remembers” past infections for faster antibody production upon re-exposure.
Pathogens
Innfectious agent “germ” that causes illness.
Living: parasites, protozoa, fungi, prokaryotes.
Non-living: Virus, prion
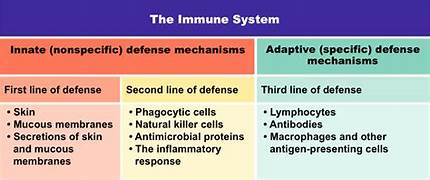
Non-specific line of defence? (Hint: Body has 3 lines of defenses)
Non-Specific (Innate Defences):
SURFACE BARRIERS that prevent the ENTRY of pathogens in the body.
First Line of Defence:
Physical defenses (Skin as a protective barrier against pathogens, respiratory tract with mucus to flush out bacteria and dust)
Chemical defenses (Skin’s acidic secretions, tears and saliva that secrete antimicrobial enzymes, and stomach that has acids and enzymes to destroy microbes in food.)
Second Line:
When a pathogen enters the body, this line of defence is triggered.
Phagocytosis occurs
Inflammatory response
1. At fist sign of injury, chemical signals are released by the foreign invader.
2. Chemical signals trigger an inflammatory response.
3. NEUTROPHILS engulf and digest the microbes. Remaining fragments of protein, dead white blood cells, abd the digested invader are called PUS.
Fever: Body’s system-wide resposne to infection.
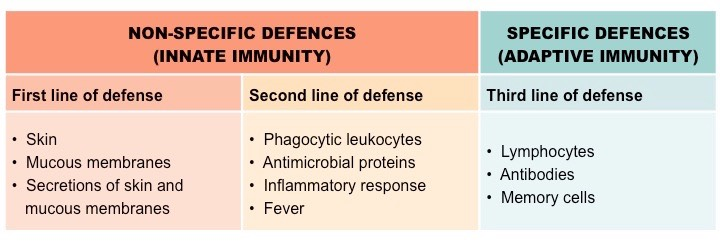
Specific line of defence?
Binding of the antibodies to antigens inactivates antigens by:
Neutralization (blocks viral binding sites; coats bacteria
Precipitation of dissolved antigens
Aggulation of microbes → Enhances → Phagocytosis
Activation of the complement system → lysis (cell bursting)
Adaptive (Specific) defense mechanism
Think of the lymph node (Storing the b and t cells) as a army barracks filled with soldiers that are waiting for an enemy that they are SPECIFICALLY trained to fight.
Neutrophils (Hint: Leukocyte)
Leukocyte = white blood cell
Part of the innate immune system (Non-specific)
Phagocytic – they engulf and digest pathogens like bacteria and fungi.
Short-lived (a few hours to days).
Die after attacking invaders – their remains form pus.
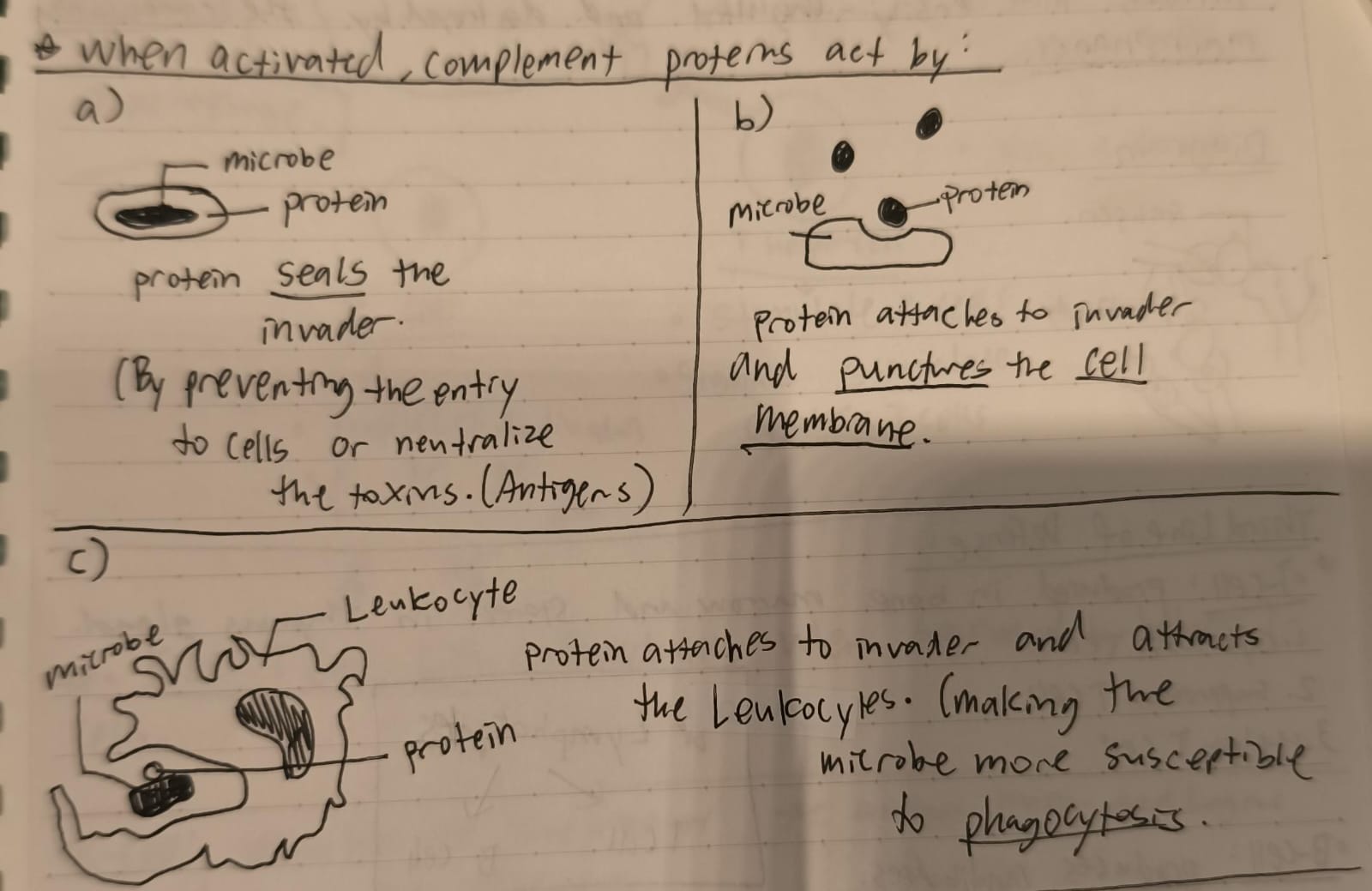
Complement proteins
The presence of pathogens activates these antimicrobial proteins.
Under normal conditions, these proteins are inactive in the circulatory system.
When activated, the proteins serve as messengers and initiate attacks on pathogens.
How do complement proteins work?
Protein SEALS the invader by preventing the entry to cells or neutralize the toxins (Antigens).
Protein attaches to invader and punxtures the cell membrane.
Protein attaches to invader and attacks the Leukocytes (Making the microbe more susceptible to phagocytosis.)
Lymphocytes (Hint: Leukocytes → Phagocytes + Lymphocytes)
White blood cells that produces antibodies.
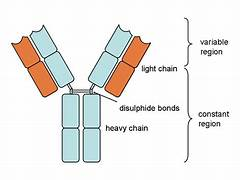
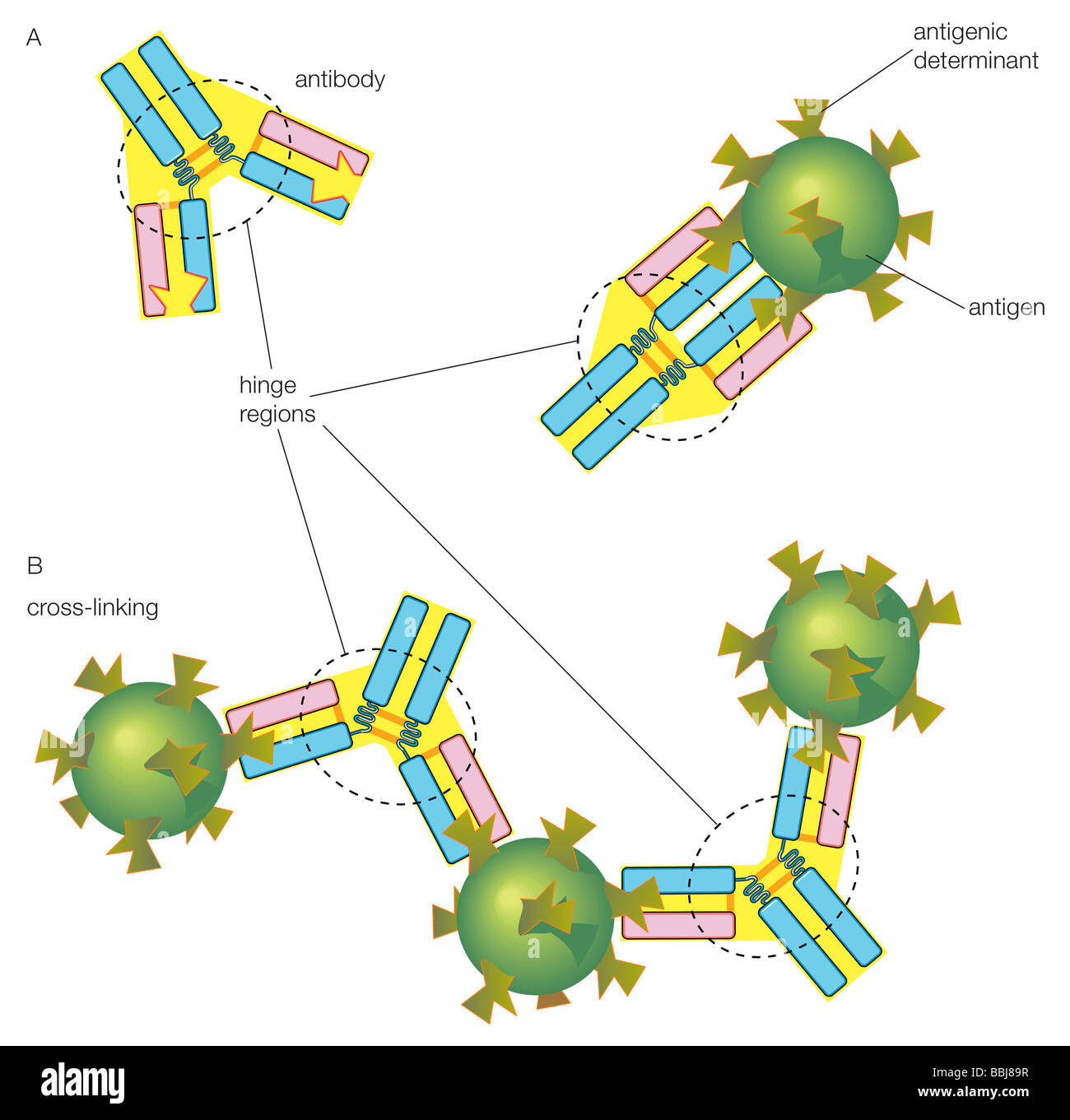
Antibodies
Y shaped proteins that recognize and bind to antigens (foreign substances).
Antibody-Antigen Complex
Each antibody attaches only to its complementary maker.
It is larger, more conspicuous, and therefore, more easily engulfed and destroyed by the circulating MACROPHAGES (Performs phagocytosis).
3 types of T cells
Cytotoxic T cell
Suppressor T cell
Helper T cell (Seek out intruders and signal an attack by messaging to B-cells.)
-Lymphocytes → T cells + B cells
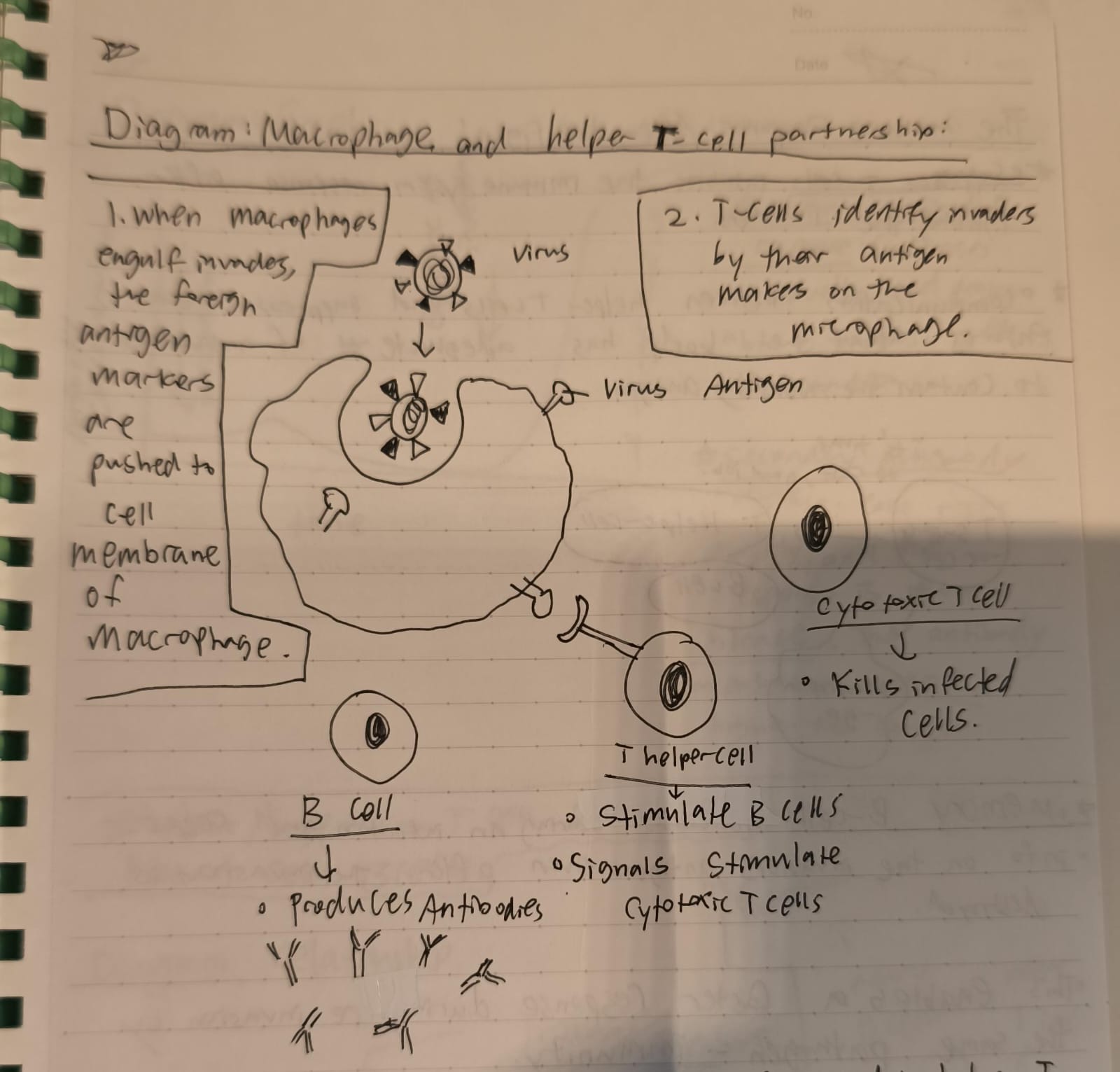
The relationship between B-cells and T-cells
When macrophages engulf invaders, the foreign antigen makers and pushed into the cell membrane of the macrophage.
T-cells help identify invaders by their antigen makers ON the microphage (DIFFERENT FROM MACROPHAGES. They’re SMALLER phagocytes, such as Neutrophils. They are short-lived and innate.)
Killer T-cells kill infected cells when SIGNALED by the helper T-cells.
Suppressor T-cell
Inhibits the immune system response AFTER fighting the invaders.
It communicates to the helper T-cells, B-cells, and Macrophages telling them that it’s time to rest
Also, communication between helper T-cells and suppressor T-cells ensure that the body has adequate # of antibodies to contain the invading antigen.
They are also the reason for our tolerance of our own antibodies
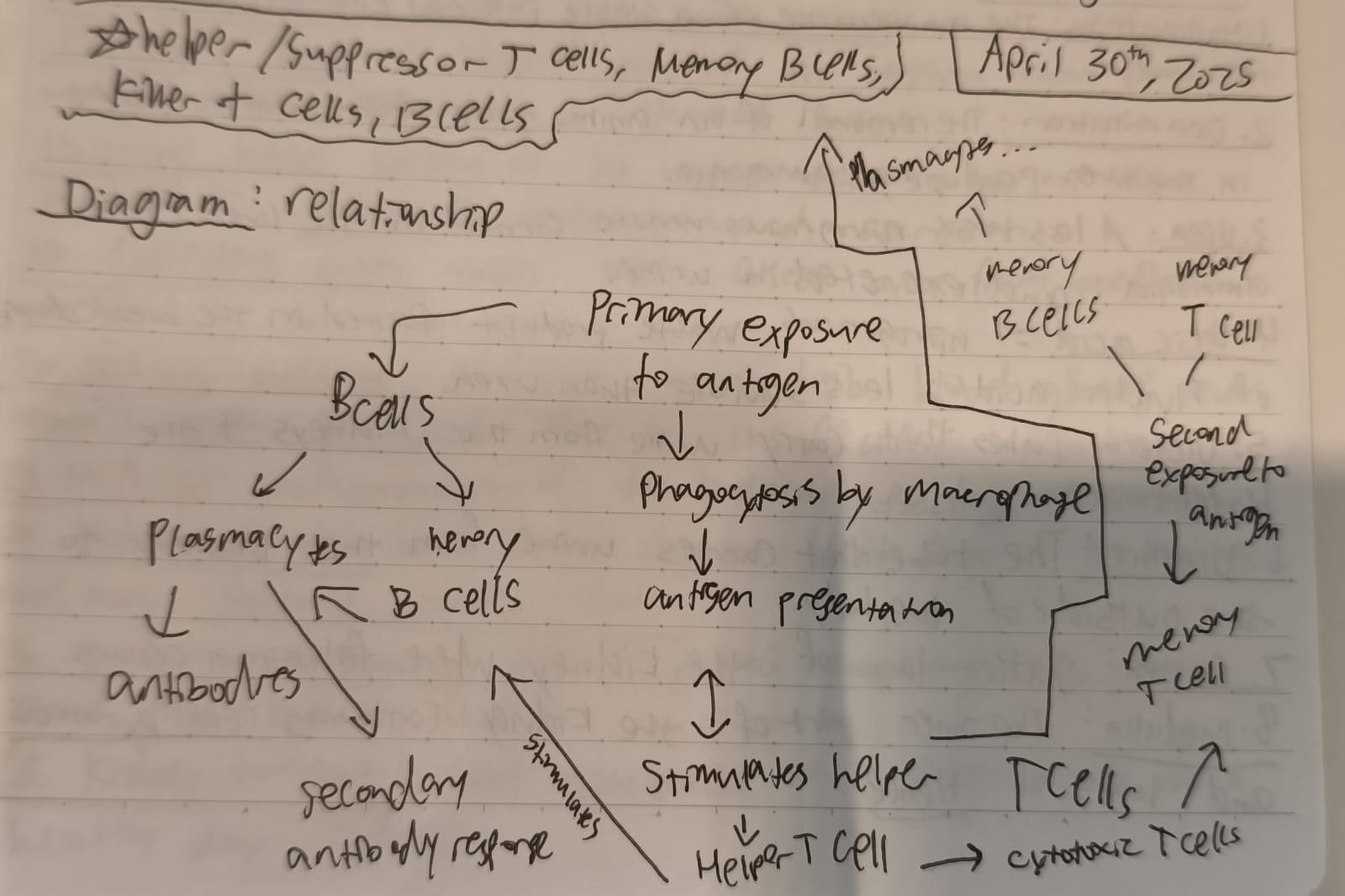
Memory B-cell
Generated during an infection and keeps info on the invaders antigens even after the invasion is destroyed.
Enables a faster response next time by the same pathogen. (Immunity)
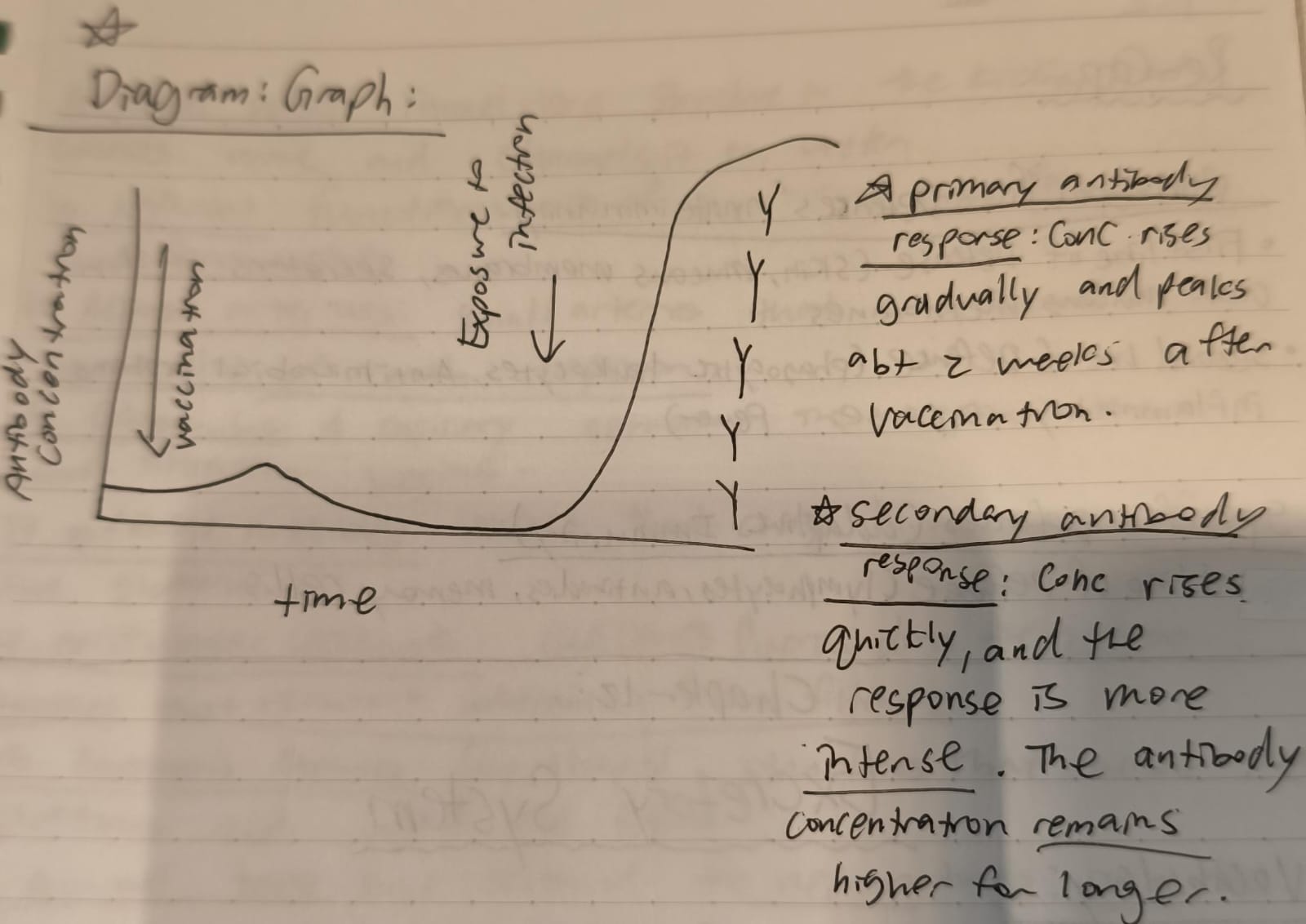
Primary and secondary antibody response:
Primary antibody response: Concentration rises gradually and peaks abt 2 weeks after vaccination.
Secondary antibody response: Concentration rises quickly, and the response is more INTENSE. The antibody concentration remains higher for longer.
Which line(s) of defence are in the nonspecific defences or specific defences?
Non-specific: 1st and 2nd line
Specific: 3rd line
Homeostasis
The maintenance of a stable internal environment in the body
Deamination
The removal of an amino group from amino acids in the liver producing ammonia.
Urea
A less toxic nitrogenous waste formed in the liver from ammonia and excreted in urine.
Ureic acid
A nitrogenous waste product formed in the breakdown of nucleic acids; less soluble than urea.
Urea vs Ureic acid
Urea is the primary, highly soluble nitrogenous waste excreted in urine and sweat, while uric acid is a less soluble purine metabolite excreted only in urine, with potential to form harmful crystals if accumulated.
Ureters
Tubes that carry urine from the kidneys to the bladder
Urethra
The tube that carries urine from the bladder to the outside of the body.
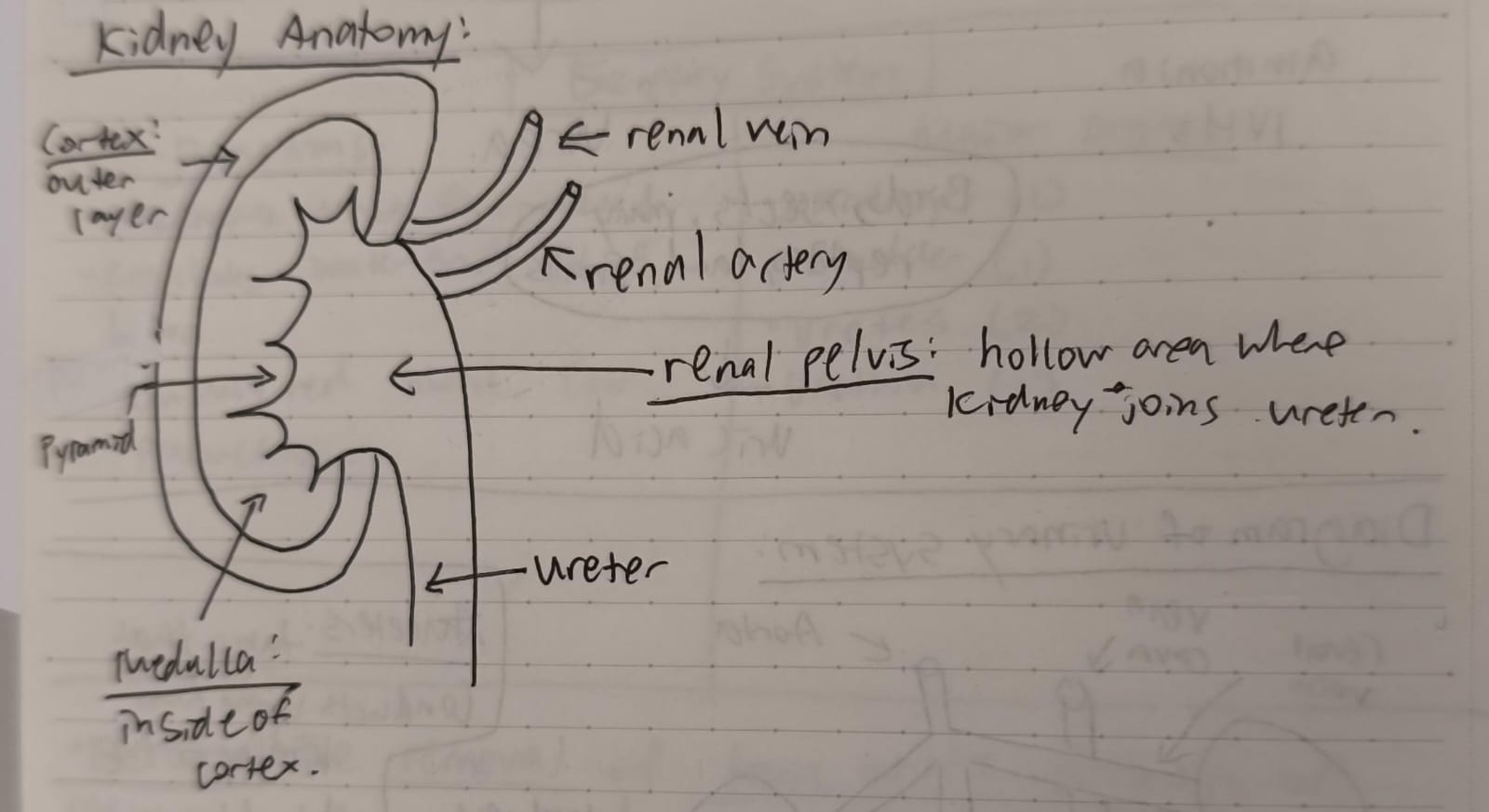
Cortex
Outer layer of the kidney where filtration occurs.
Medulla
The inner part of the kidney containing renal pyramids and loops of Henle.
Renal Pelvis
Funnel-like structure in the kidney, that collects urine and channels it to ureter.
Nephrons
Functional units of the kidney that filter blood and form urine.
Afferent Arterioles
Small arteries that bring blood to the glomerulus of each nephron.
Glomerulus
A capillary network in the nephron where blood filtration begins.
Efferent Arterioles
Vessels that carry blood away from the glomerulus.
Peritubular Capillaries
Capillaries surrounding the nephron tubules that reabsorb substances from filtrate.
Bourman’s Capsules
Cup shaped structures that encase the glomerulus and collect the filtrate.
Proximal Tubule
First section of the nephron tubule where the MOST reabsorption of nutrients and water occurs.
Loop of Henle
U-shaped part of the nephron that concentrates urine by absorbing water and salts.
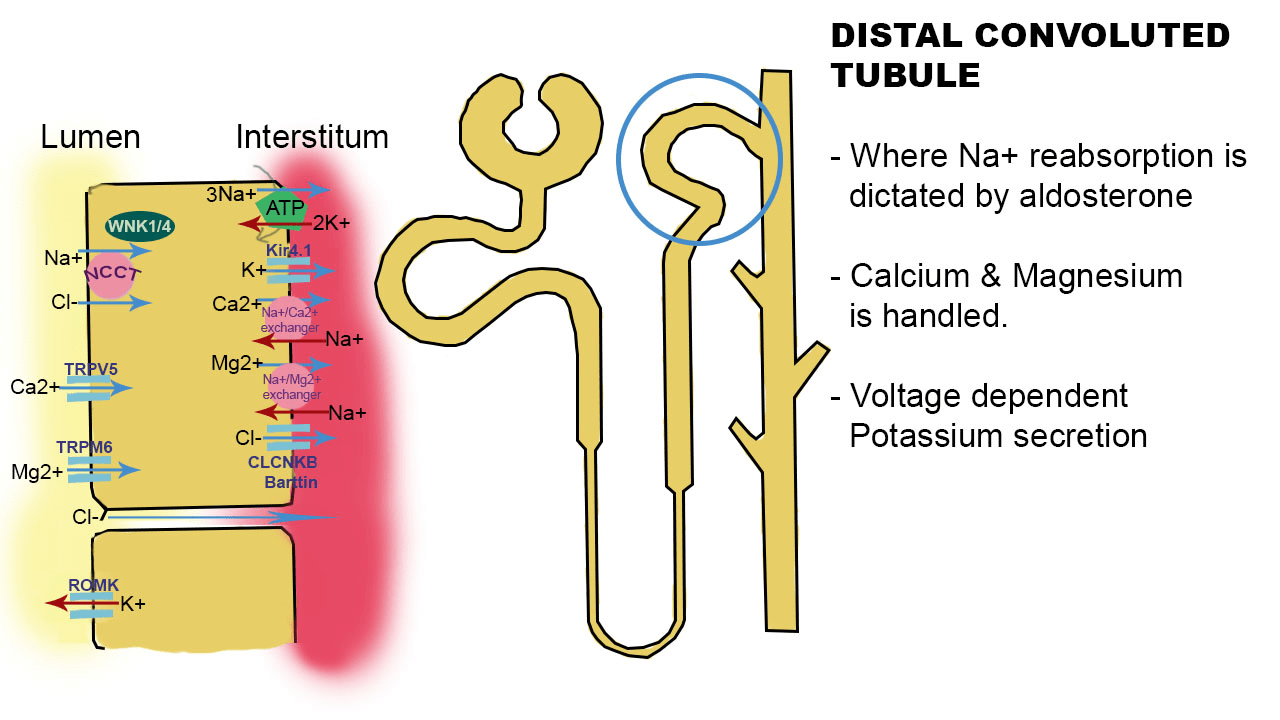
Distal Tubule
Section of the nephron after the loop of Henle involved in selective reabsorption and secretion.
Collecting Ducts
Tubes that collect urine from nephrons transport it to renal pelvis.
Diabetes Mellitus
Disease where high blood glucose levels result in glucose in urine due to insufficient insulin.
Nephritis
Inflammation of the kidneys, affecting filtration
Kidney Stones
Hard mineral deposits that form in the kidney and may obstruct urinary flow.
Dialysis Technology
Medical process that artificially filters blood when kidneys fail.
Kidney Transplant
Surgical replacement of a diseased kidney with a healthy donor kidney.
Major organs of the excretory system
Kidneys
Bladder
Ureters (2)
Urethra (1)
Functions of the excretory system
Removes waste from blood
Regulates water and PH of blood
Controls red blood cell production
Excretion
The removal of toxic waste products of metabolism from the body.
Ammonia (Origin and organ of excretion)
Origin: Deamination of amino acids by the liver
Organ of excretion: Kidneys
Urea (Origin and organ of excretion)
Origin: Deamination of amino acids by liver, ammonia is combined with CO2.
Organ: Kidneys, skin (Small amounts)
Uric Acid (Origin and organ of excretion)
Origin: Product of breakdown of nucleic acids; DNA
Organ: Kidneys
3 different kinds of nitrogenous wastes (Hint: What do animals and humans excrete?)
Most aquatic animals (Fishes) → Ammonia NH3
Mammals, amphibians, sharks, some bony fishes → Urea
Birds, insects, many reptiles, land snails → Uric acid
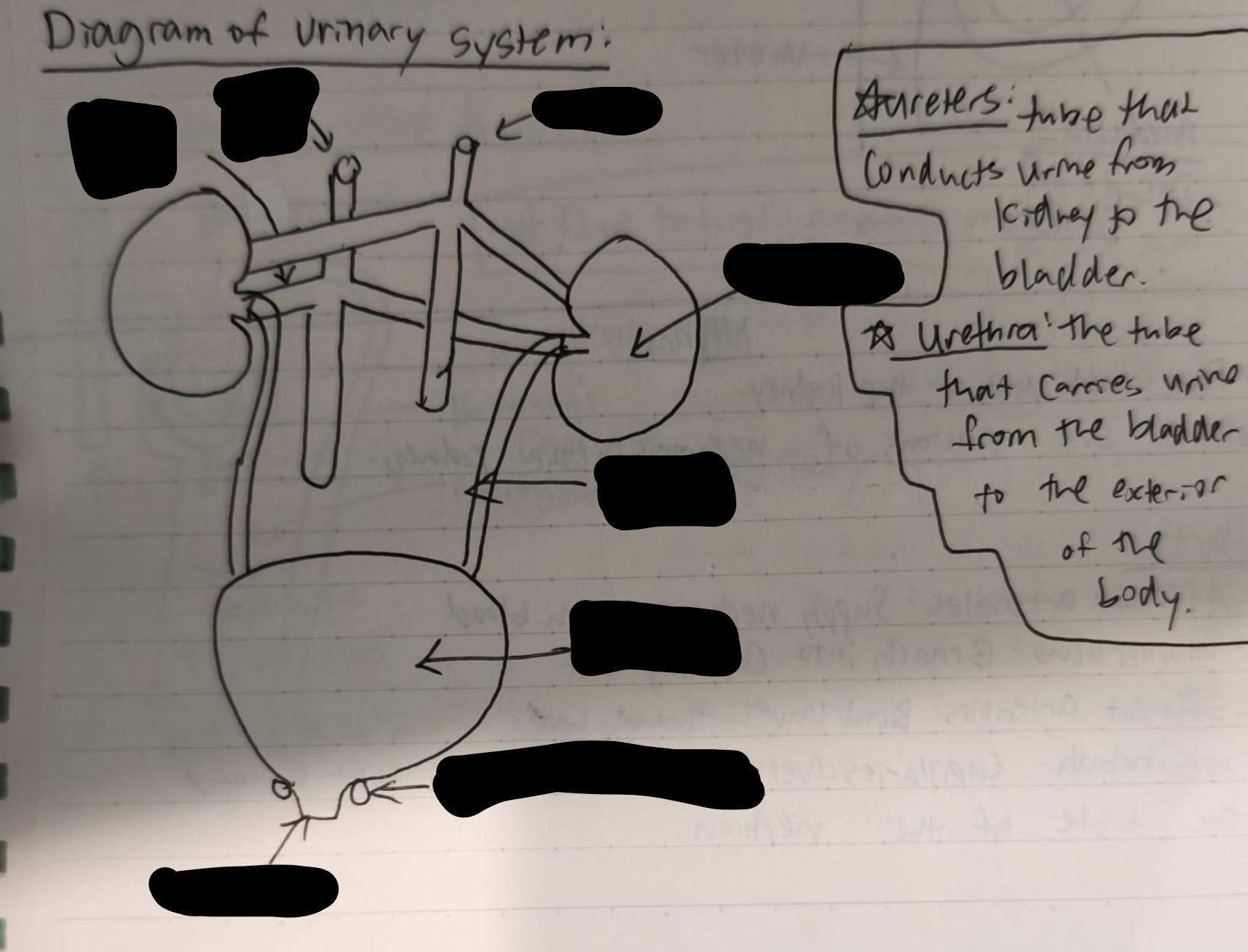
Label the urinary system
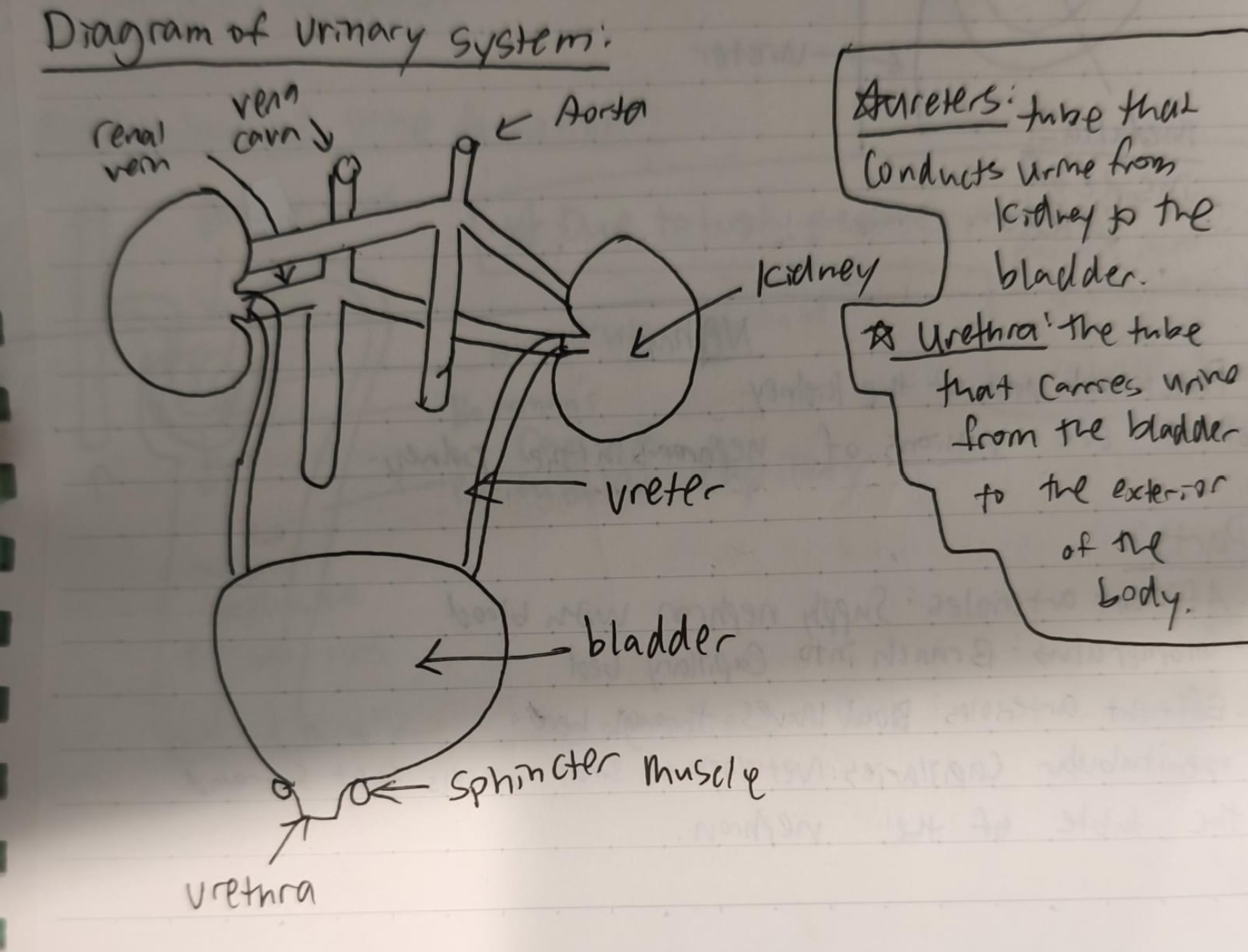
Ureters vs Urethra
Ureters: Tube that conducts urine from kidney to the bladder.
Urethra: The tube that carries urine from the bladder to the exterior of the body.
Function of the collecting ducts
Converge at the pelvis of the kidney, pouring their contents into the ureter, which carries the urine to the urinary bladder for temporary storage.
Parts of a nephron
Bowman’s capsule
Proximal tubule
Loop of Henle
Distal tubule
Collecting ducts
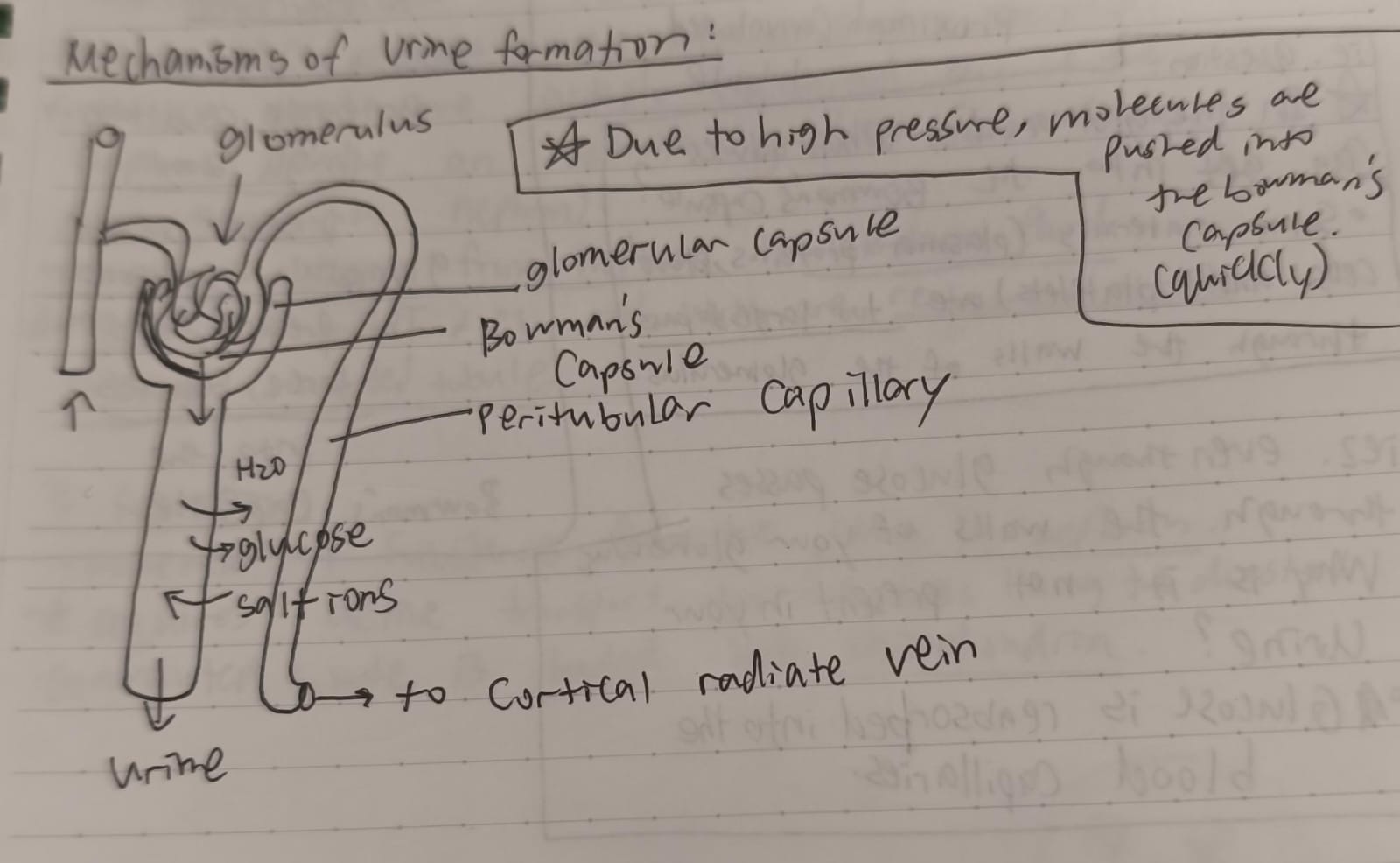
3 renal processes
Glomerular filtration (ultrafiltration) (Due to high blood pressure, molecules are pushed)
Tubular reabsorption (Selective reabsorption) (Water + glucose)
Tubular secretion
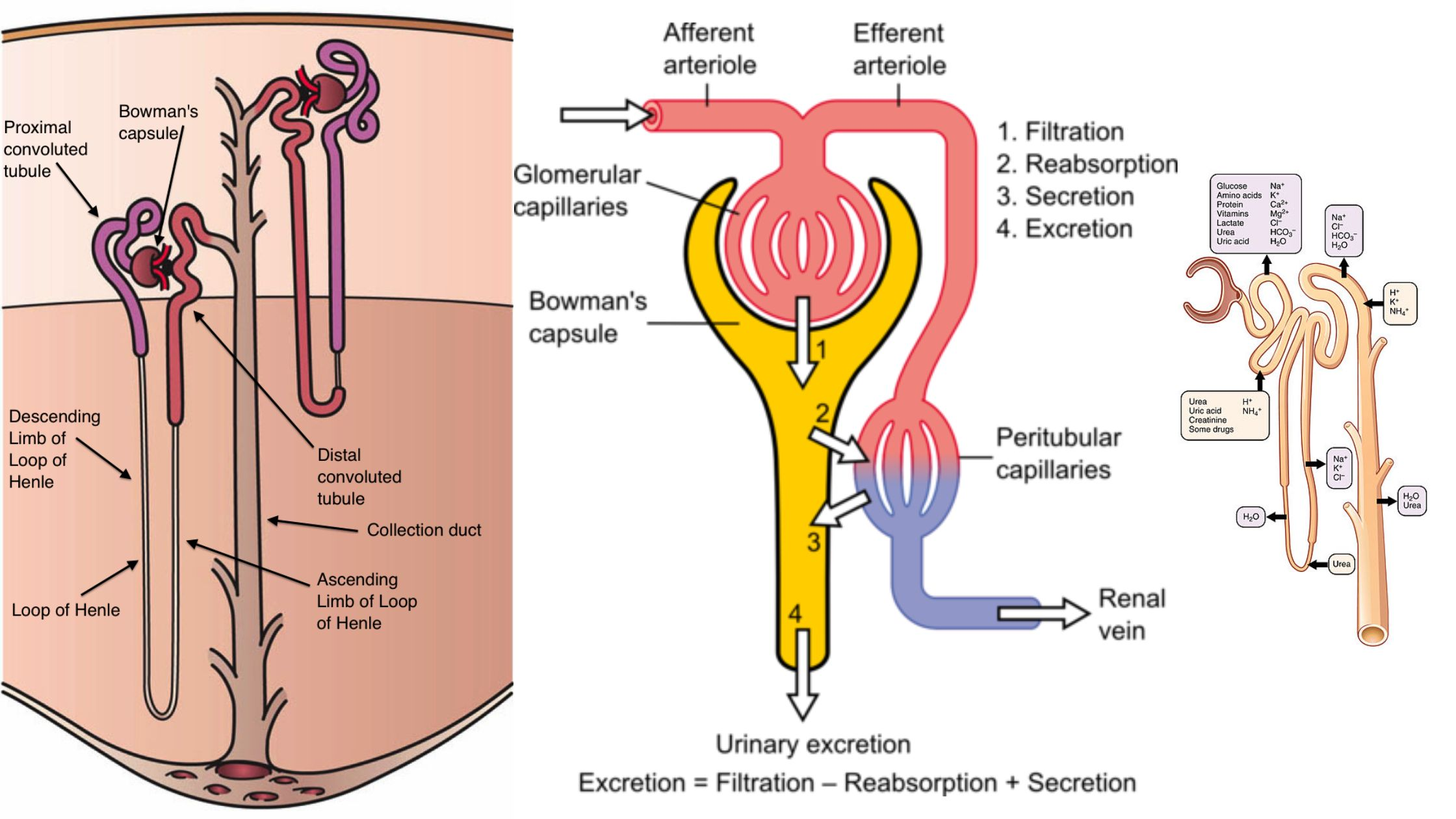
Blood flow through the nephrons
Blood enters the nephron via the afferent arteriole.
It flows into the glomerulus, a capillary tuft where filtration occurs under high pressure.
Filtered blood exits the glomerulus through the efferent arteriole.
The efferent arteriole branches into the peritubular capillaries (and vasa recta in juxtamedullary nephrons) surrounding the nephron tubules.
These capillaries facilitate reabsorption and secretion between blood and tubular fluid.
Finally, blood from the peritubular capillaries drains into the venous system via arcuate veins and ultimately leaves the kidney through the renal vein.
Kidney
Kidney: Bean-shaped organs located on either side of the spine.
The right kidney is slightly lower than the left kidney to make space for the liver.
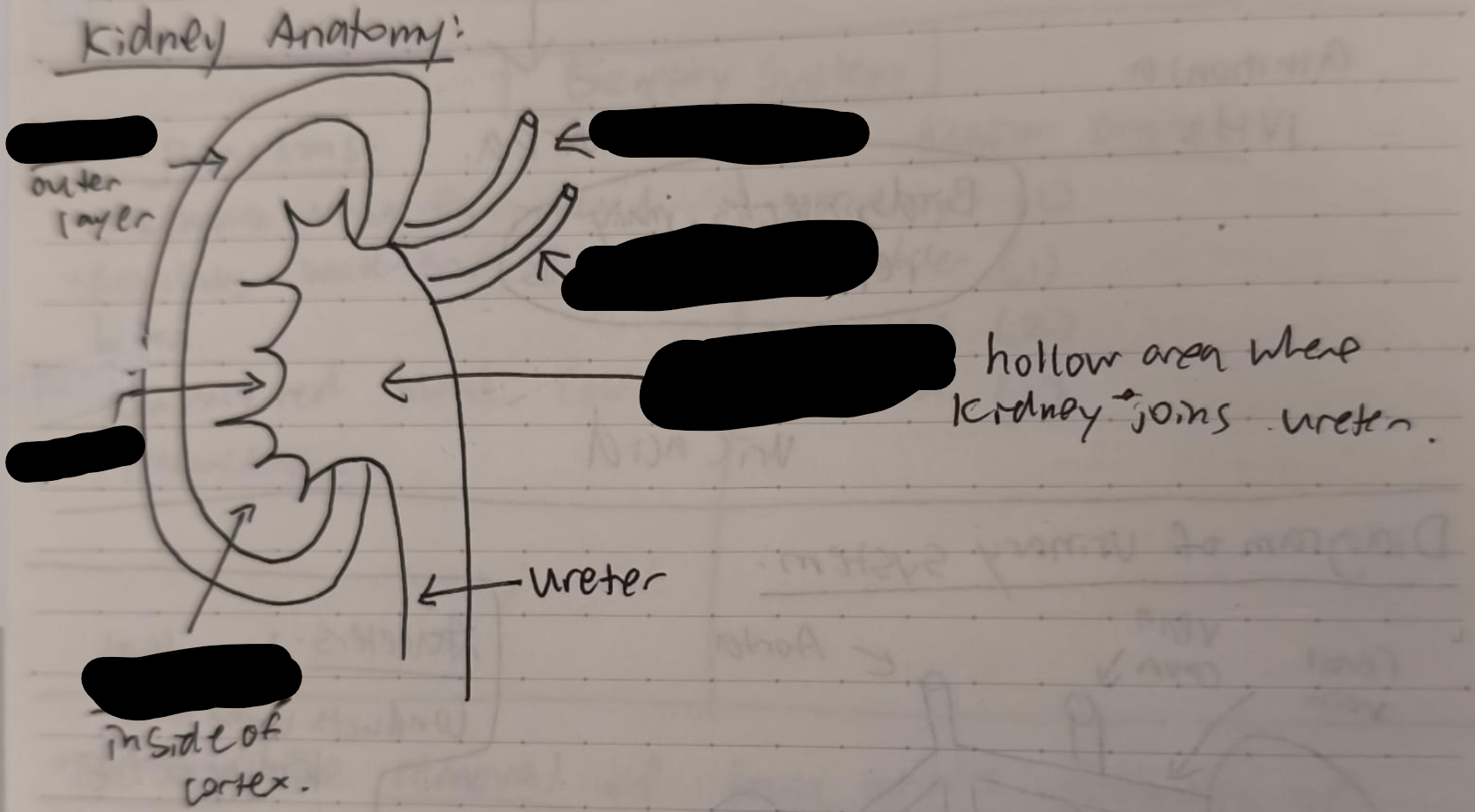
Label the kidney
What is urine composed of?
Urine is primarily composed of about 95% water.
urea (~9.3 g/L), chloride (~1.87 g/L), sodium (~1.17 g/L), potassium (~0.75 g/L), and creatinine (~0.67 g/L),