Parathyroid Hormone and Calcium Function
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
What is the physiological importance of calcium?
Provides structural integrity of skeleton and teeth, where 99% resides in bone and teeth as hydroxyapatite crystals
—
-1-2 kg calcium in adult body
- Intracellular calcium (0.9% of total calcium)
- Extracellular calcium (0.1% of total Ca):
- ~45% bound to plasma proteins such as albumin
- ~10% complexed with anions (citrate, phosphate, sulphate)
- ~45% in unbound form (Ca 2+ ) is physiologically active
Why do we need calcium homeostasis?
Concentration is tightly regulated at all locations:
Bone growth and remodelling
Acting as enzyme co-factor for blood coagulation
Muscle contraction, where needed for actin and myosin interactions
Neuronal function, where they regulate excitability by initiating AP and open VGCC
Enzyme action for metabolism
Exocytosis of hormones and neurotransmitters, triggered by Ca2+ influx
Intracellular signalling, as secondary messengers
Describe Glucose induced increases in [Ca2+]
Triggers insulin secretion from ß-cells:
Once glucose becomes metabolised, there is an increase of ATP in ß-cells
Causes the closure of ATP-sensitive K+ channels.
Results in a membrane potential change of the ß-cells, which causes the opening of the VSCa2+C enabling the influx of Ca2+ into the cell.
Increase in intracellular calcium, triggers an increased release of insulin from pancreatic ß-cells (via exocytosis) which results in a high concentration of glucose in cells.
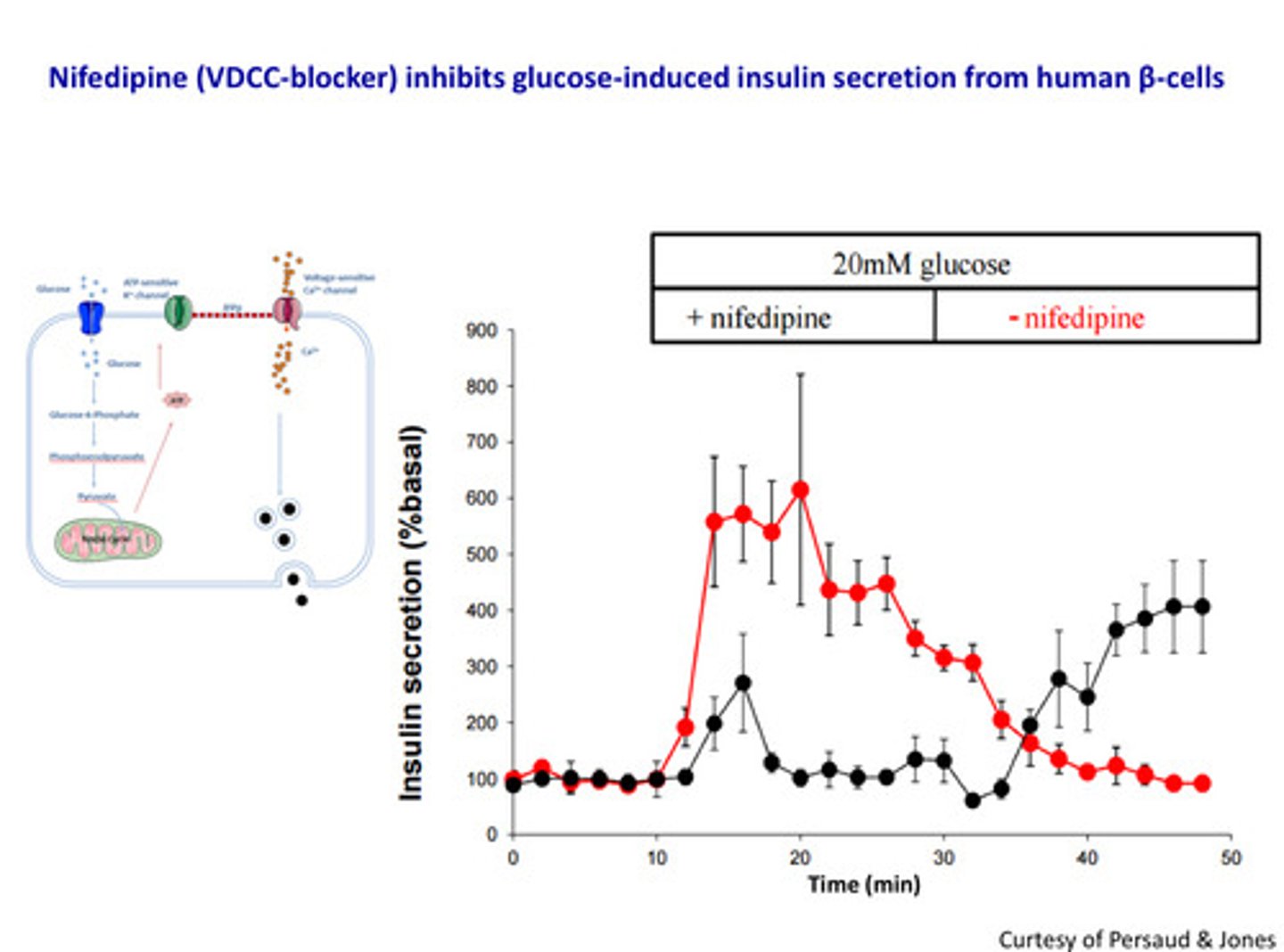
Nifedipine (CCB) inhibits glucose-induced insulin secretion from human ß- cells.
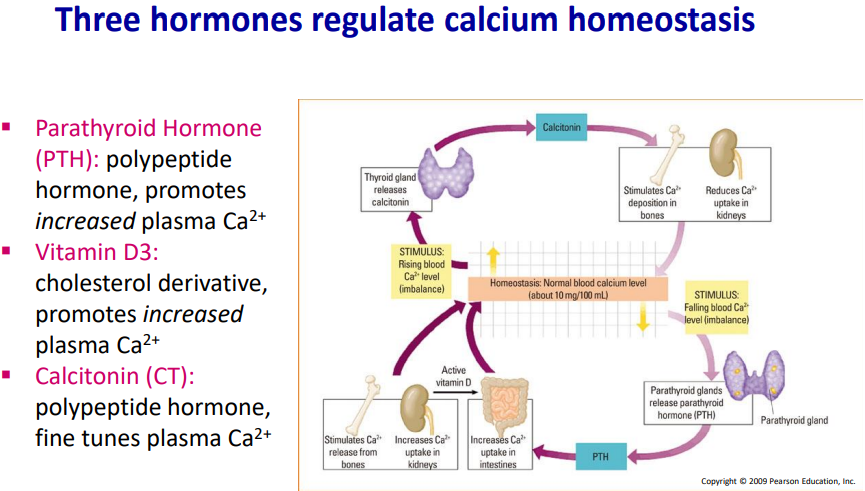
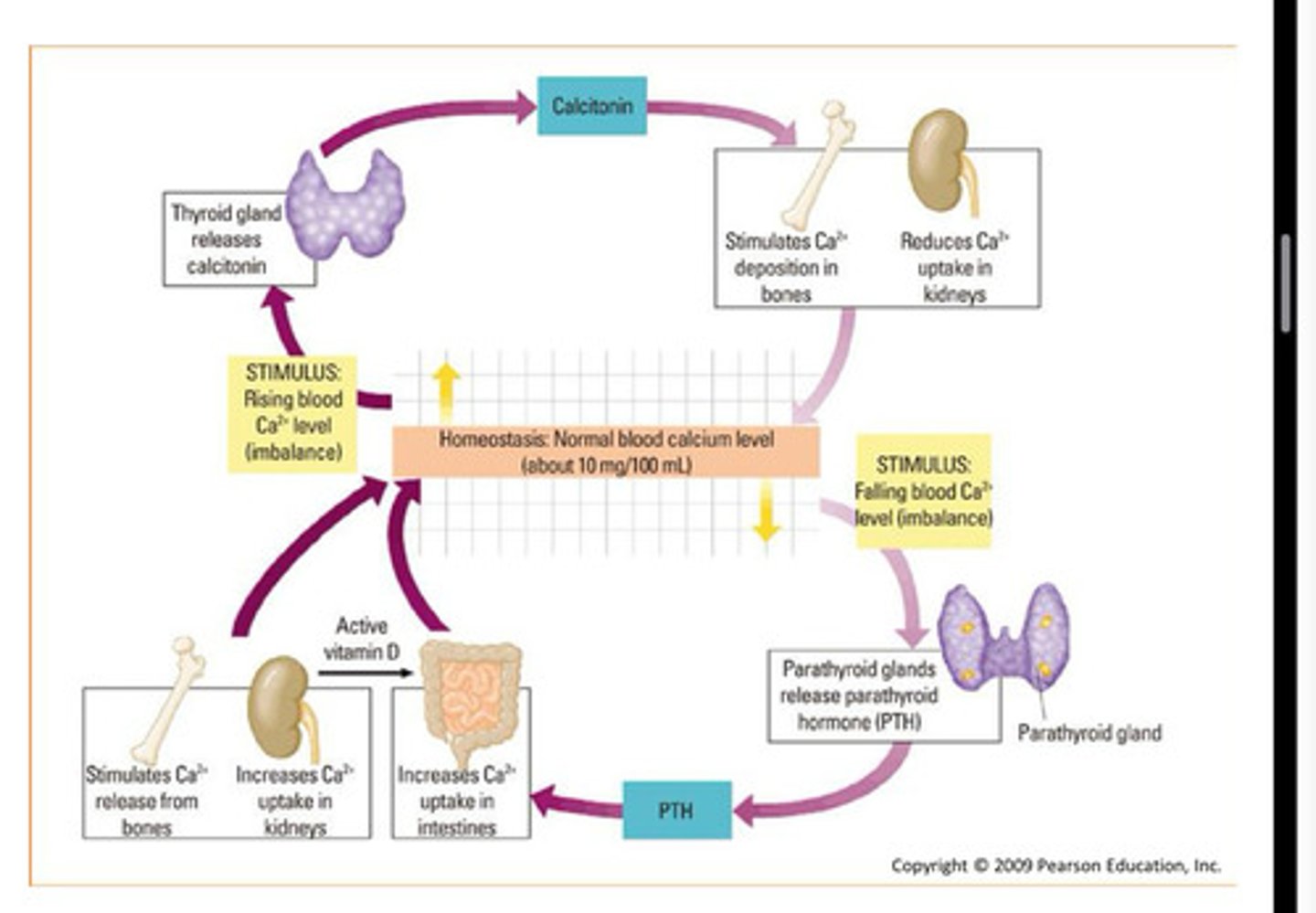
These are the three main tissues; bone, kidney and the intestine which regulate calcium homeostasis, by Calcitonin. Serum Ca2+ is increased by PTH and Vitamin D3.
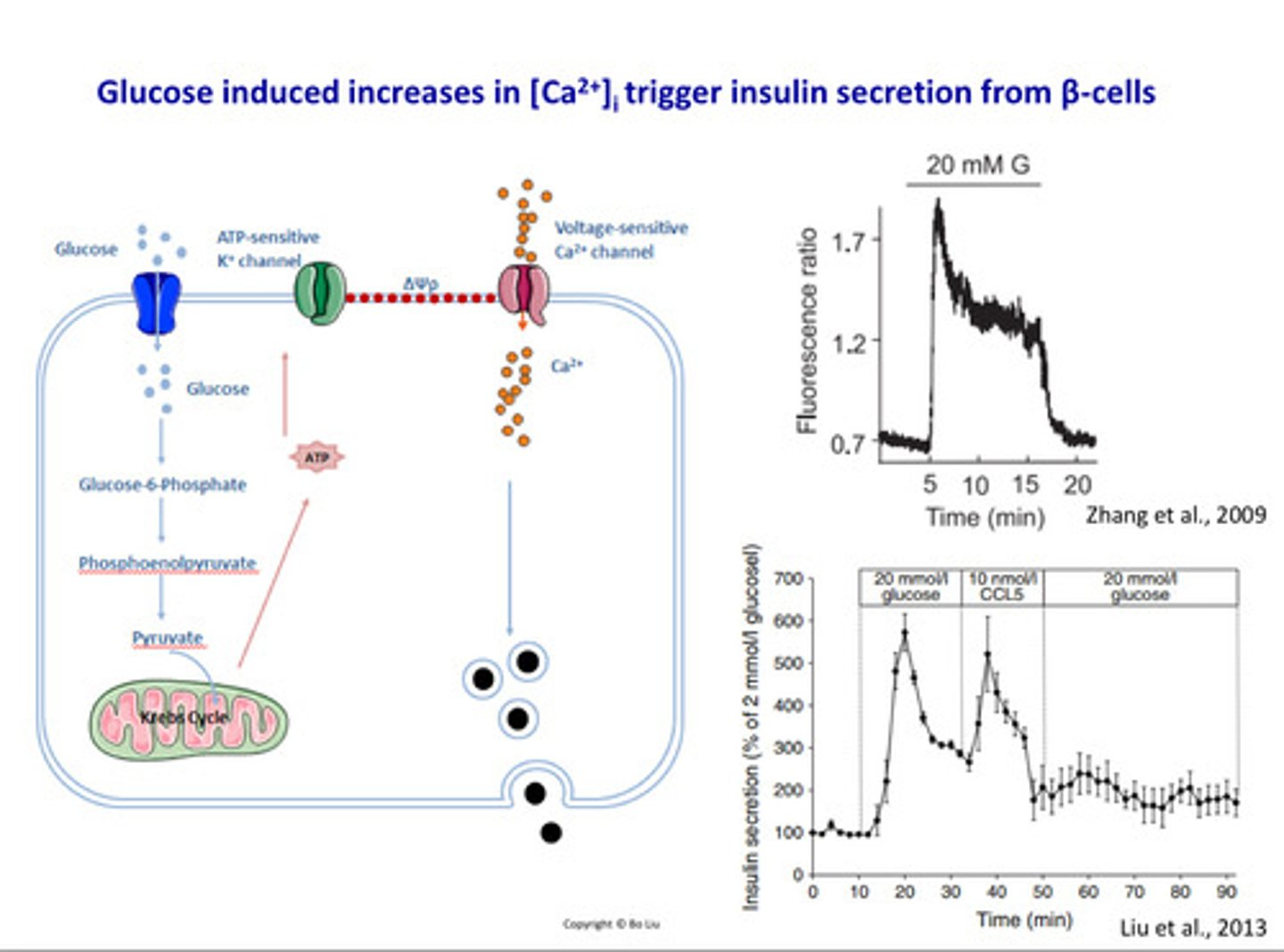
How do we know intracellular calcium increase triggers insulin secretion?
Studies:
-When we stimulate the beta cells with high levels of glucose e.g. 20 mM glucose, we can see from the graph there is a sharp increase of intracellular calcium cells which in turn increases the increase of insulin secretion into circulation from beta cells
- Nifedipine (VDCC (voltage-dependent calcium channels)-blocker) inhibits glucose-induced insulin secretion from Beta cells
How is calcium homeostasis maintained?
Serum calcium is increased by two hormones:
Parathyroid hormone (PTH) and Vitamin D
Regulation of calcium homeostasis:
Calcitonin and PHT-related peptide
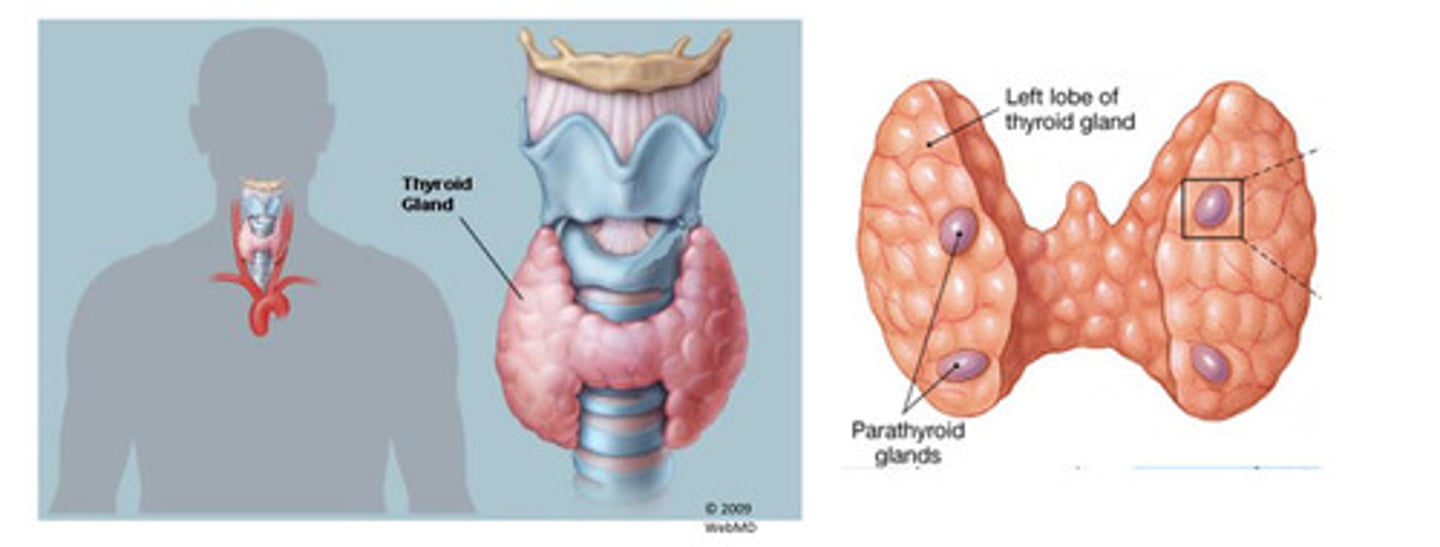
What is the anatomy of parathyroid gland?
- Embedded in posterior surface of thyroid gland but are anatomically and histologically distinct from thyroid
- Usually 4 but may vary- total weight of PTH tissue is ~150 mg
- Oxyphil cells (unknown function) and Chief cells (produce PTH, Parathyroid hormone)
—
- Contains a large amount of adipose tissue which expands in volume at puberty
- PTH-producing Chief cells have a prominent central nuclei and pale cytoplasm
- Oxyphil cells appear in clusters, have small, dark = nuclei and an acidophilic cytoplasm
What is the parathyroid hormone PTH?
PTH is produced by parathyroid Chief cells
Synthesized from the precursor molecule pre-pro-PTH (115 amino acids)
Precursor (pre-pro-PTH ) is subsequently cleaved to pro-PTH (90 amino acids)
PTH is a biologically active 84 amino acid peptide (the first 34aa are fully active)
—
PTH is synthesised continuously and released from PTH gland.
PTH is secreted by exocytosis in response to reduced plasma Ca2+ [Detected by calcium-sensing receptors (CaSR) on the surface of chief cells]
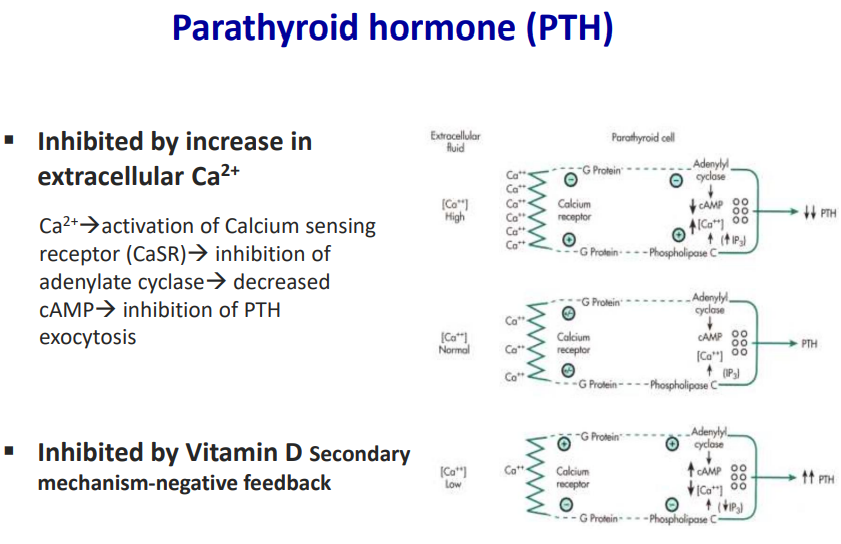
PTH is inhibited by an increased in extracellular Ca [Ca2+→activation of Calcium sensing receptor (CaSR)→ inhibition of adenylate cyclase→ decreased cAMP→ inhibition of PTH exocytosis]
PTH is inhibited by vitamin D (regulated by negative feedback)
![<ul><li><p>PTH is produced by <strong><mark data-color="red" style="background-color: red; color: inherit">parathyroid Chief cells</mark></strong></p></li><li><p><strong><mark data-color="blue" style="background-color: blue; color: inherit">Synthesized from the precursor molecule pre-pro-PTH (115 amino acids) </mark></strong></p></li><li><p><strong><mark data-color="blue" style="background-color: blue; color: inherit">Precursor (pre-pro-PTH ) is subsequently cleaved to pro-PTH (90 amino acids) </mark></strong></p></li><li><p><strong><mark data-color="blue" style="background-color: blue; color: inherit">PTH is a biologically active 84 amino acid peptide (the first 34aa are fully active)</mark></strong></p></li></ul><p>—</p><ul><li><p>PTH is <strong>synthesised continuously</strong> and released from PTH gland. </p></li></ul><ul><li><p>PTH is <strong>secreted by exocytosis</strong> in response to reduced plasma Ca2+ [Detected by calcium-sensing receptors (CaSR) on the surface of chief cells]</p></li><li><p>PTH is inhibited by an <strong>increased in extracellular Ca</strong> [Ca2+→activation of Calcium sensing receptor (CaSR)→ <strong>inhibition of adenylate cyclase</strong>→ decreased <strong>cAMP</strong>→ inhibition of PTH exocytosis]</p></li><li><p>PTH is inhibited by vitamin D (regulated by negative feedback)</p></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/4d6def49-4810-4894-87a3-dc6247262662.png)
What happens once PTH is released?
- Binds to G-protein coupled receptor PTH-R
- Activation of PTH-R causes increases in cAMP and calcium release from its intracellular stores
- Acts on bone, kidney and small intestine
- Subsequent action on bones: PTH-R on osteoblasts = initial bone formation, later on: bone resorption via cytokines from osteoblasts
- PTH is synthesised continuously once released from the parathyroid gland
- PTH is secreted by exocytosis in response to reduce plasma calcium: not under hypothalamic control but responds directly to changes in plasma calcium levels and detected by calcium-sensing receptors (CaSR) on the surface of Chief cells
How is PTH inhibited?
By an increase in extracellular calcium: Calcium activates CaSR = inhibits adenylyl cyclase = decreased cAMP = inhibits PTH exocytosis
By Vitamin D: via secondary negative feedback mechanism
What is the effect of PTH action on kidneys?
- PTH inhibits PO 4 reabsorption (inhibits NA-PO 4 cotransport in proximal convoluted tubule)
- Phosphaturia (-a condition where the body is unable to reabsorb phosphate from the glomerular filtrate, resulting in excess phosphate in the urine)
- Less complexed Ca-PO 4
- Increased plasma calcium
- Stimulates calcium reabsorption on distal convoluted tubule
- Phosphaturia and calcium reabsorption = increase in calcium concentration
—
Renal Ca2+ reabsorption is under hormonal control and 60% of plasma calcium is filtered in the glomerulus (ionised, non-bound fraction) and of this:
70% reabsorbed in the proximal tubule
20% reabsorbed in the Loop of Henle
9% reabsorbed in distal tubule
1% excreted in urine
What is the effect of PTH on the small intestine?
- PTH stimulates calcium reabsorption via activation of vitamin D
- PTH stimulates renal 1-alpha-hydroxylase = converts 25-hydroxycholecalciferol to 1, 25-dihydroxycholecalciferol = stimulates intestinal calcium absorption
—
Intestinal Ca2+ reabsorption is under hormonal control and 80% of dietary calcium is not absorbed. The absorption occurs in the small intestine. Active transport occurs in the duodenum and jejunum, whilst diffusion in the ileum. Transport involves intestinal and cytosolic calcium-binding proteins.
Which 3 hormones regulate calcium homeostasis?
- PTH: polypeptide hormone which promotes increased plasma calcium
- Vitamin D3: cholesterol derivative, promotes increased plasma calcium
- Calcitonin CT: polypeptide hormone, fine tunes plasma calcium
How does vitamin D regulate calcium homeostasis?
- Cholesterol derivative promoting increased plasma calcium
- Synthesised in skin keratinocytes from 7-
dehydrocholesterol via UV light and ingested in food
and absorbed into blood stream
- Metabolised in liver and kidneys to the activated form: 1, 25 di-hydroxyvitamin
D3
- Major site of regulation of synthesis is in kidney under PTH control
- Has a short half-life of a few hours
- Vitamin D circulates bound to specific binding proteins
- Binds to nuclear receptors (VDR)- alteration gene transcription
- Increases in calcium transport proteins = increased rate of calcium absorption
= rapid uptake of calcium from the gut
- Increases bone resorption and reduces urinary calcium loss at the kidneys
Why is Vitamin D not a vitamin but a steroid hormone?
- It is a substance that must be provided by the diet (~10%) and 90% from skin
- Calcitriol is produced in the kidney and released into systemic circulation- no
ducts involved
- Calcitriol acts on a distant organ- epithelial cells of small intestine
How can vitamin D deficiency be treated?
- UV light exposure
- Dietary sources- fish, milk, whole grains, cheese, butter
- Adding chalk-calcium carbonate to flour and vitamin D to margarine
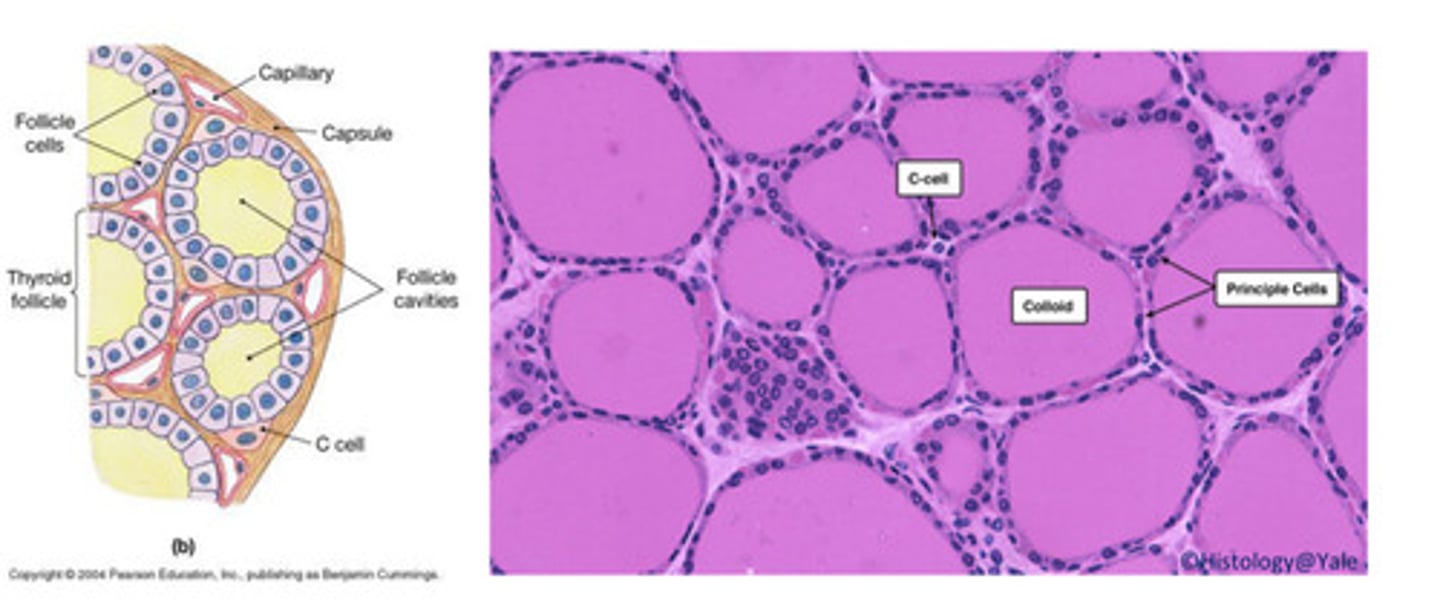
How is the thyroid gland and Calcitonin related?
- Lined by epithelial Principal cells: responsible for synthesis and secretion of
T3 and T4
- Clear Parafollicular cells (C cells): responsible for the synthesis and secrete calcitonin:
calcitonin regulates calcium homeostasis
How does Calcitonin regulate calcium homeostasis?
- Polypeptide hormone fine tunes plasma calcium, these polypeptide hormones
are produced by parafollicular cells of the thyroid glands released in response
to increased calcium in extracellular fluid
- Calcitonin is directly regulated by calcium concentrations- there is no
hypothalamus/pituitary control
- Calcitonin generally opposes PTH actions by inhibiting osteoclasts (protective
effect on bone calcium) and stimulates calcium release from kidneys
- Calcitonin physiological relevance is unclear: neither thyroidectomy (calcitonin
deficiency) nor thyroid tumours (excess calcitonin) has significant effect on
calcium homeostasis (PTH and Vitamin D3 dominate)
- Used clinically in treatment of hypercalcaemia and in certain bone diseases in
which sustained reduction of osteoclastic resorption is therapeutically
advantageous
What are the consequences of failure of calcium homeostasis?
- The physiological response to Hypocalcaemia:
- Decreased plasma calcium causes increased PTH: this causes mobilisation of
bone calcium and phosphate to try to restore plasma calcium levels,
increased renal phosphate excretion and calcium retention in kidneys,
increased vitamin D3 synthesis and rise in plasma calcium levels and
maintenance of normal phosphate levels
- The physiological response to Hypercalcaemia:
- Increased plasma calcium causes decreased PTH secretion: reduced
mobilisation of bone by osteoclasts and increased osteoblast formation,
decreased renal calcium absorption and reduced calcitriol synthesis, reduced
plasma calcium levels
What are the calcium-related pathologies?
- Hypocalcaemia: vitamin D deficiency, chronic renal failure (renal hydroxylation
of vitamin D), pseudohypoparathyroidism (tissue resistance to PTH),
Iatrogenic (damaged or removed during thyroid surgery), autoimmune
disorders (auto-antibodies destroy tissue)
- Hypercalcaemia: moans, groans, stones- depression, constipation, kidney-
calcification
How is PTH insufficiency characterised? Hypocalcaemia
- Tetanic muscle contracts: spasms laryngeal stridor muscle, seizures, cardiac
effect where repolarisation is delayed with prolonged QT interval, cataract due
to protein accumulation, dry and flaky skin, brittle nails, hand tetany
- Osteoporosis: brittle and fragile bones, hormonal changes, calcium/vitamin D
deficiency, long-term use of corticosteroids
- Rickets: associated with severe calcium dietary restriction
How is PTH excessiveness characterised?
- Adenoma/hyperplasia
- More common in women
- Chronically elevated plasma PTH causes hypercalcaemia, low phosphate
- Symptoms: moans, groans, bones, stones
- Psychic moans: depression of NS, slow reflex, depression
- Abdominal groans: decreased appetite, anorexia, constipation, vomiting
- Bones: osteitis fibrosa/arthritis, cystic area in bone- may contain fibrous
tissue, marrow fibrosis
- Stones: calcium phosphate crystals throughout body- kidney stones deposit in
kidney