Adrenal Glands
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
12 Terms
What is the organization and vascularization of the adrenal gland?
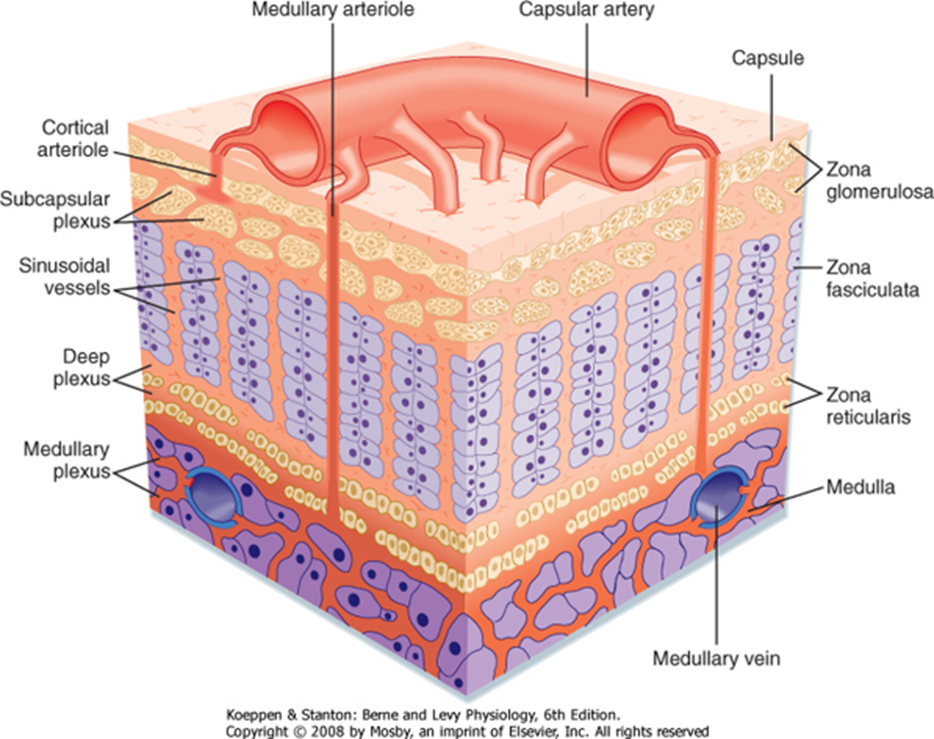
The adrenal gland or suprarenal gland is supplied by three suprarenal (superior, middle, inferior) arteries which all eventually drain into the suprarenal veins.
The adrenal gland itself is organized into the cortex and medulla
1) Cortex has three layers and produces steroid hormones
→ Zona Glomerulosa - production of mineralocorticoids
→ Zona Fasciculata - production of glucocorticoids
→ Zona Reticularis - production of androgens
2) Medulla sits underneath the cortex and is responsible for the production of catecholamines as an extension of the sympathetic nervous system
What is the shared precursor and first step for adrenocortical hormones?
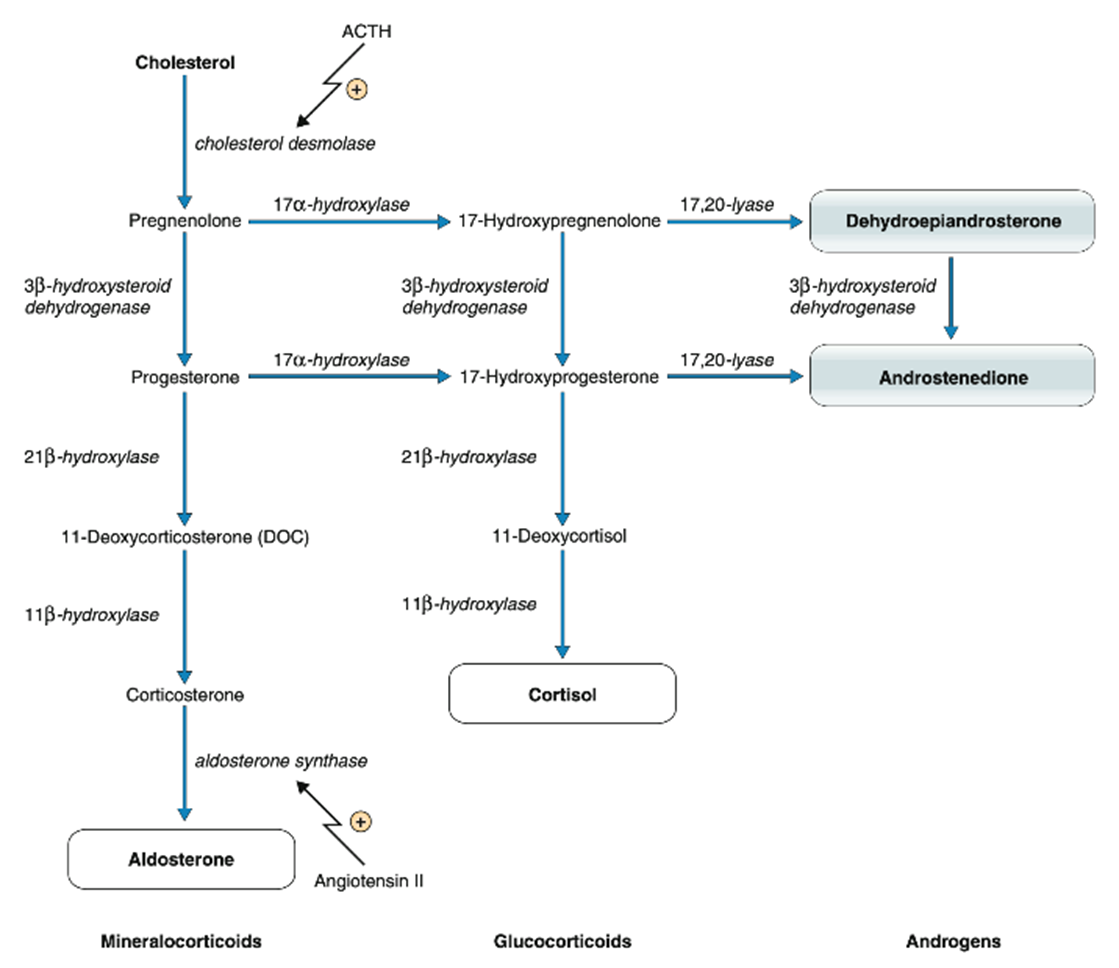
All adrenocortical hormones are steroid hormones and will share a common cholesterol precursor that is carried to the suprarenal glands via LDL
1) The first step for biosynthesis of adrenocortical hormones involves the conversion of cholesterol to pregnenolone via the activation of cholesterol desmolase
→ cholesterol desmolase is part of the cytochrome p450 family and is known as CYP11A1
→ the activity of this enzyme is activated by adrenocorticotropic hormone
What is biosynthesis of mineralocorticoids? Two major regulators?
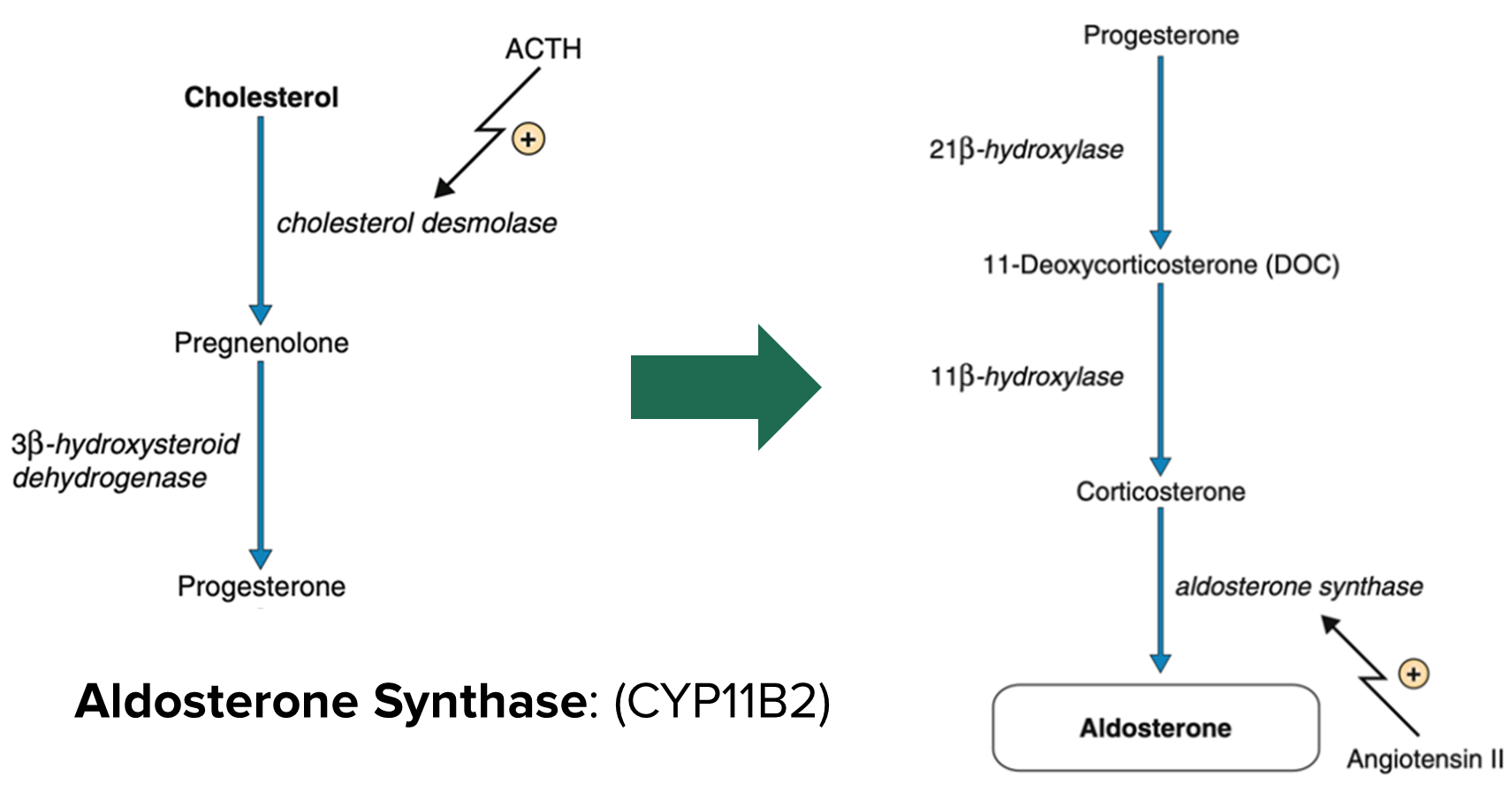
In the zona glomerulosa the major enzyme involved in the conversion of cholesterol to aldosterone is via aldosterone synthase (CYP11B2)
1) Aldosterone Synthase is activated primarily by angiotensin II produced from the renin-angiotensin system
→ increases in sodium is sensed by the macula densa, causing vasoconstriction of the afferent arteriole, reducing blood flow and activating the juxtaglomerular apparatus to secrete renin
→ renin will lead to production of angiotensin II
→ Angiotensin II will bind to Gq receptors leading to activation of PKC which triggers activation of aldosterone synthase
2) Aldosterone is also regulated by potassium concentration
→ rising potassium concentration is sensed by the zona glomerulosa, causing depolarization
→ allows for entry of calcium via activation of the voltage gated calcium channels which will lead to activation of aldosterone synthase
What does aldosterone do? What other hormone can bind to the same receptor?
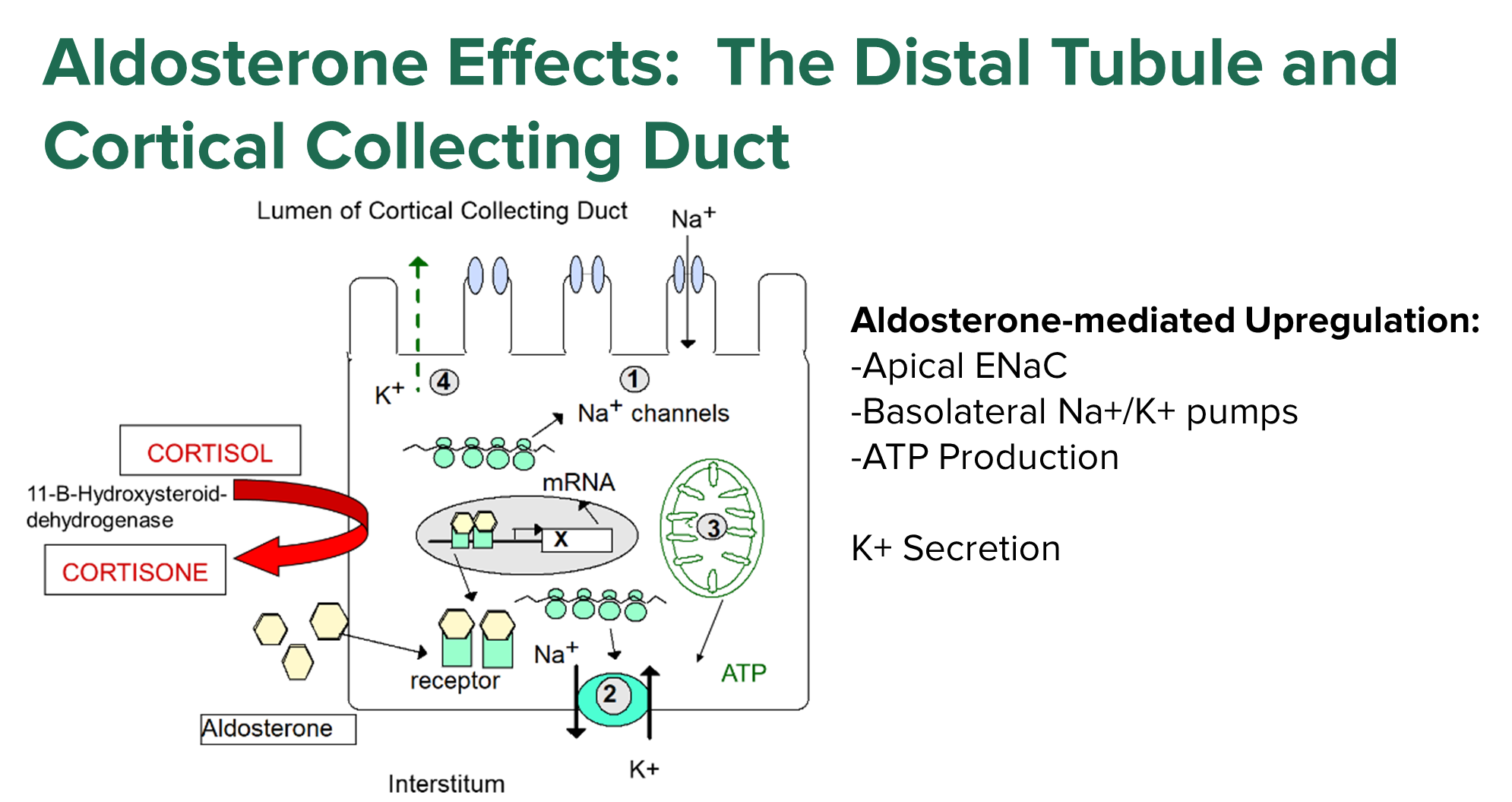
Aldosterone will bind intracellularly and will cause four major changes at the distal tubule, promoting reabsorption of sodium and water
→ importantly Cortisol can bind to the aldosterone receptor, but cortisol is converted into cortisone in order to prevent this activation
1) Increased expression of ENaC on the apical surface of the distal tubule
→ allows for increased reabsorption of sodium at the apical membrane
2) Increased expression of sodium/potassium pumps on the basolateral surface
→ the increased expression allows for sodium and water to be reabsorbed across the basolateral surface while also promoting potassium secretion into the urine
3) Increased ATP production necessary for activity of the sodium potassium pump
4) Increased Potassium secretion
→ as seen with increasing sodium/potassium pump expression
5) Aldosterone promotes H+ ATPase activity in the alpha-intercalated cells
→ promotes hydrogen secretion to acidify our urine
What are the stimulatory and inhibitory signals for glucocorticoid production and how are glucocorticoids made?
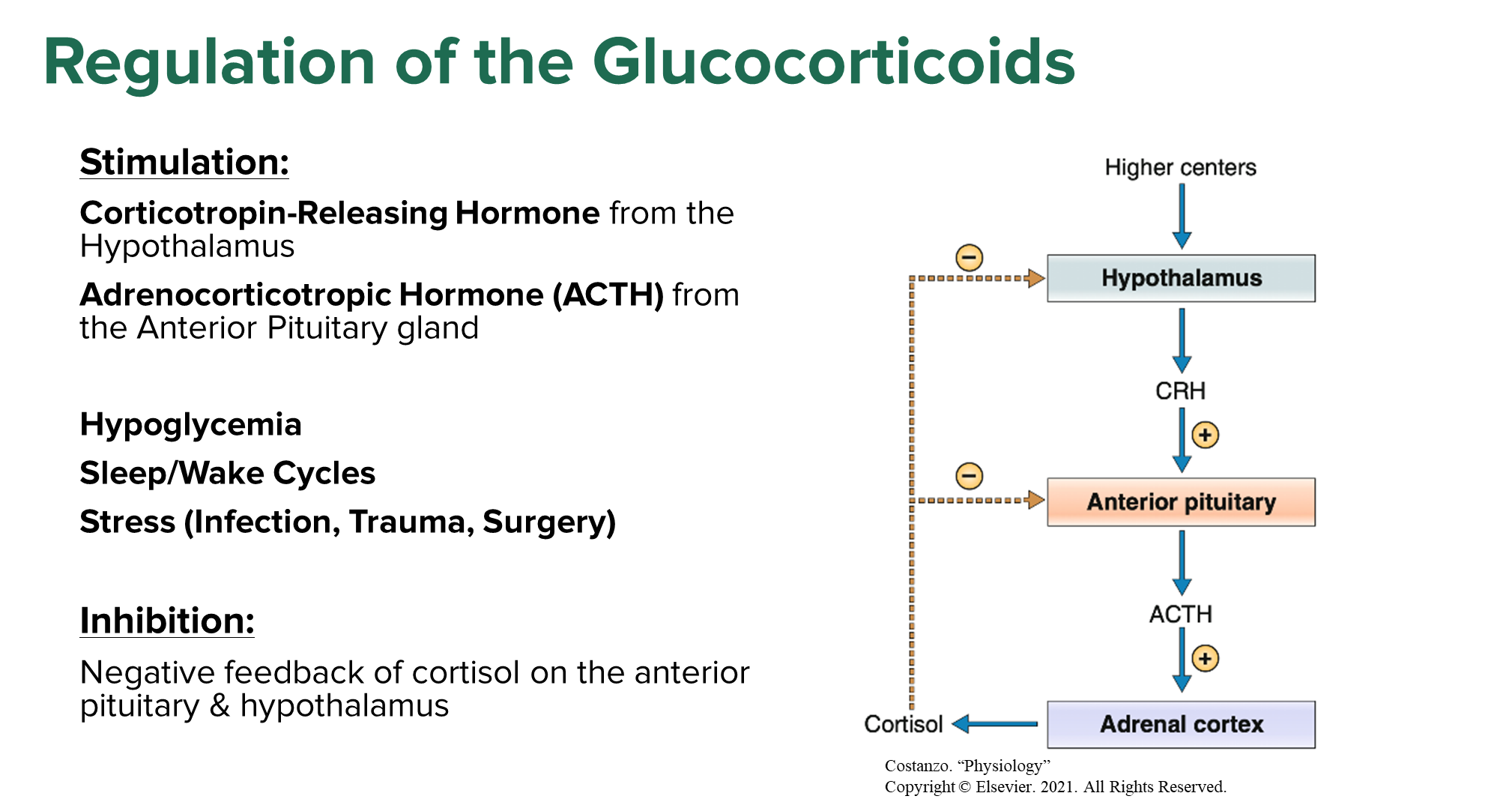
Cortisol is a glucocorticoid which is produced in the zona fasciculata
1) Cortisol secretion is stimulated in a pulsatile manner, stimulated for release by corticotropin releasing hormone and ACTH released from the hypothalamus and anterior pituitary
→ ACTH is the main stimulator of cortisol production, increasing activity of cholesterol desmolase by binding to a Gs receptor
→ ACTH also promotes LDL receptor expression, allowing for increased cholesterol uptake for production of cortisol
2) Also positively regulated by several external stimuli
→ Hypoglycemia
→ Sleep/Wake Cycles
→ Stress
3) Inhibited by negative feedback of cortisol on the pituitary and hypothalamus
When are levels of Cortisol the highest?
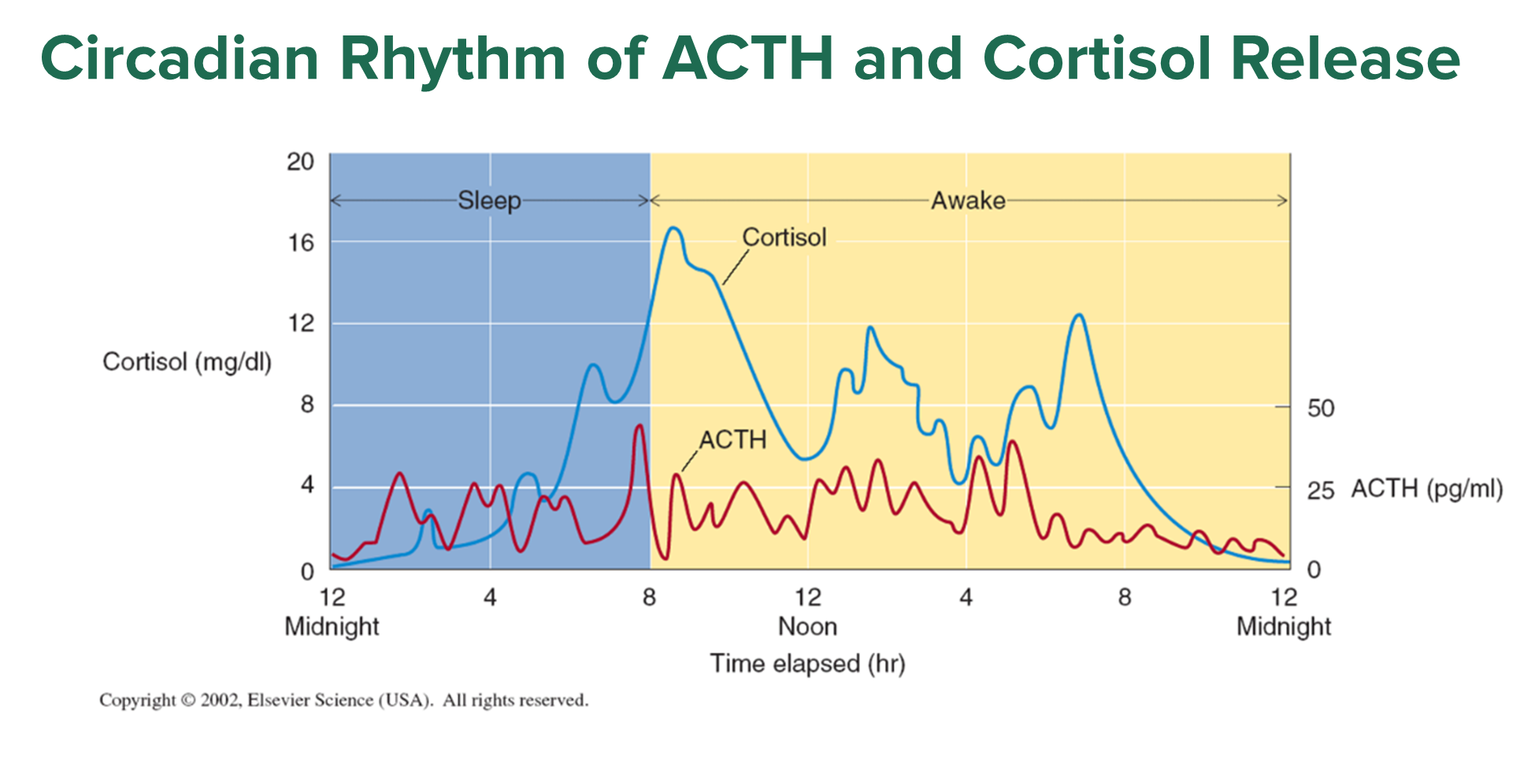
Cortisol follows a pulsatile secretion that follows a 24 hour circadian rhythm
→ Cortisol is often highest in the morning when we wake up
→ Because cortisol increases blood glucose, cortisol will increase in between meal times and when we are asleep/fasting
What is the effect of cortisol?
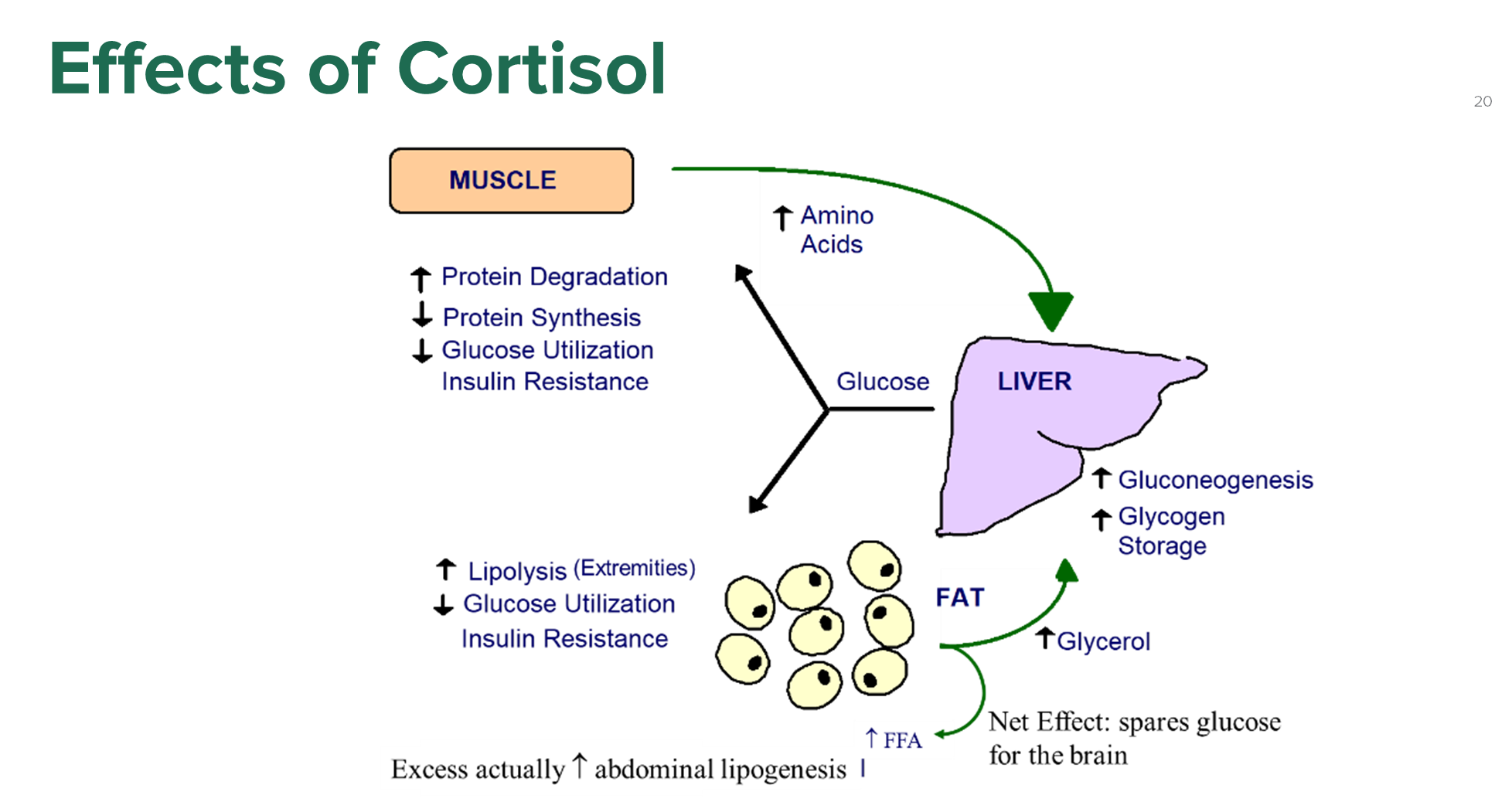
Cortisol’s main effect is to increase blood glucose via gluconeogenesis by acting on the muscle, adipose tissue, and liver
1) Liver
→ increases gluconeogenesis
2) Adipose Tissue and Muscle
→ increase in protein degradation and lipolysis in order to gain more substrates like amino acids and glycerol which can be used for gluconeogenesis
→ will also decrease glucose uptake and utilization in these areas
3) When a patient has chronically high cortisol levels, the opposite can occur where there is lipogenesis in the trunk with thin arms and legs
4) Cortisol is also an immunosuppressant and anti-inflammatory agent
What are the adrenal androgens and where are they produced?
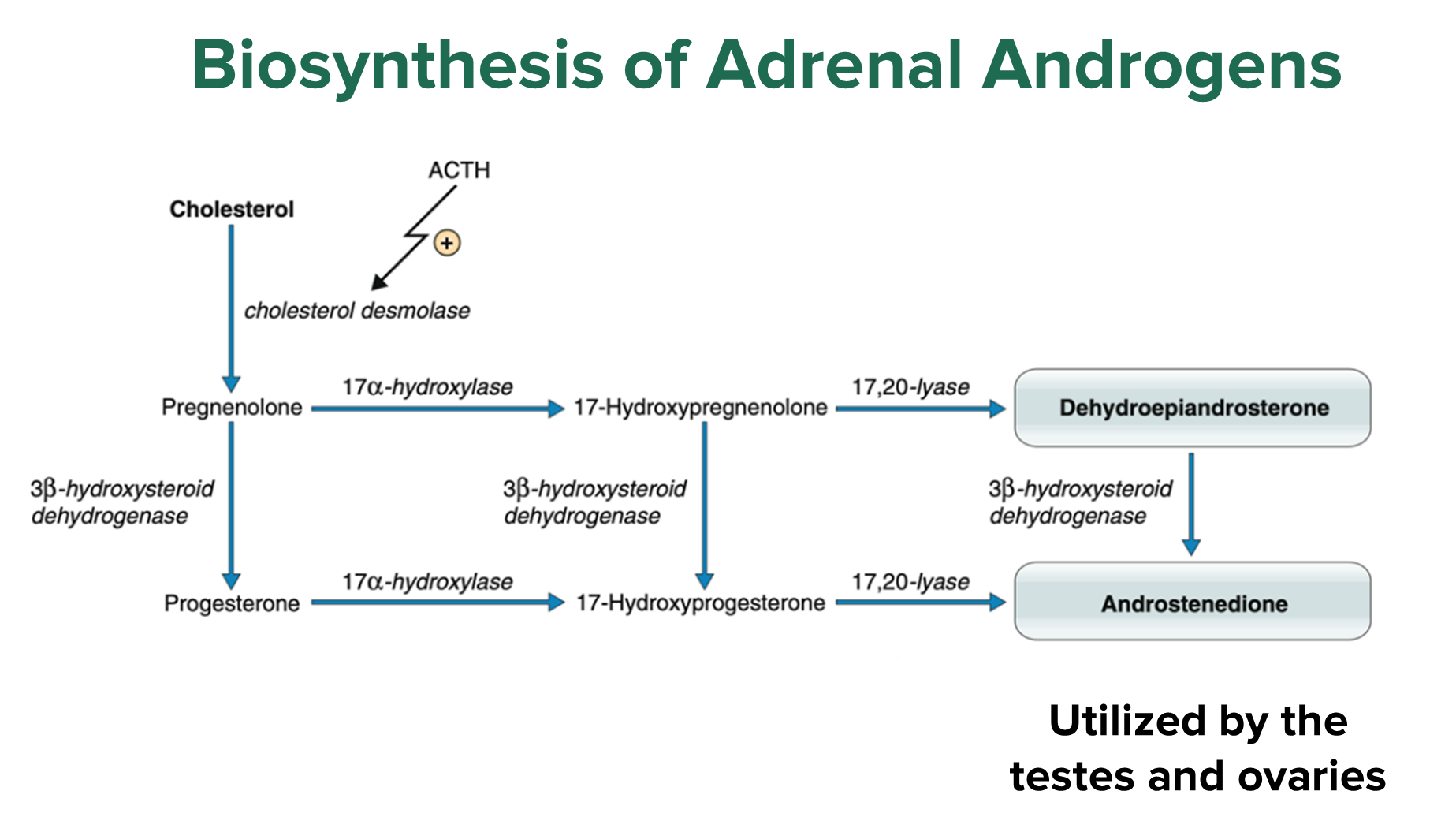
Adrenal Androgens are produced at the zona reticularis, with the two main ones being dehydroepiandrosterone and androstenedione
→ considered weak sex steroids and are converted into other sex hormones at the testes and ovaries
What is the function of the adrenal medulla?
The Adrenal Medulla is a extension of the sympathetic nervous system
1) Sympathetic preganglionic neurons will synapse a the chromaffin cells releasing acetylcholine which binds to nicotinic receptors
2) Chromaffin cells will release catecholamines like epinephrine into the periphery in response to acetylcholine binding
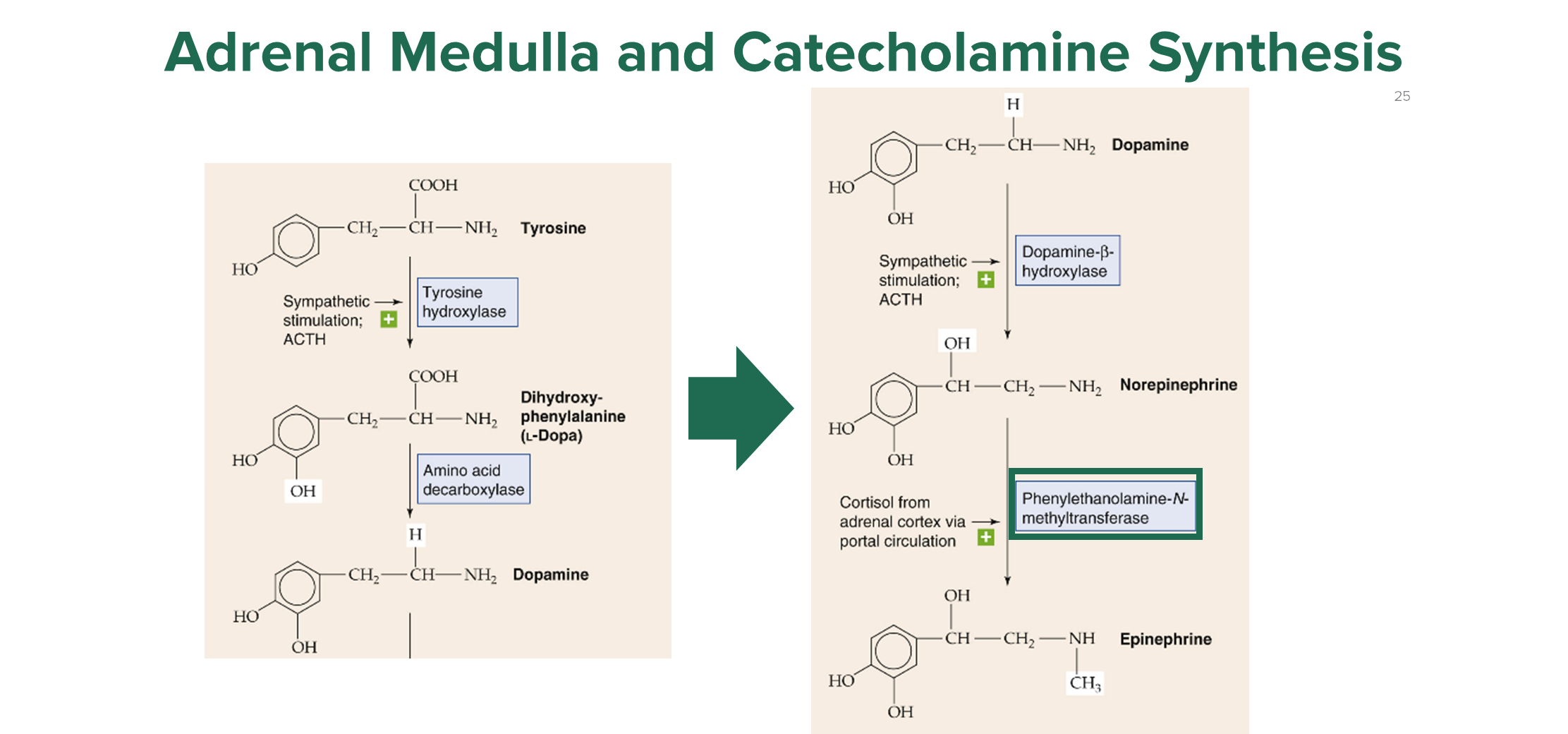
→ tyrosine is converted to DOPA via the action of tyrosine hydroxylase
→ the action of phenylethanolamine-N-methyltransferase (PMNT) is responsible for the conversion of norepinephrine to epinephrine
3) Cortisol can also bind to the adrenal medulla and lead to increased activity of PMNT allowing for increased conversion of NE to epinephrine
What is the difference between aldosterone deficiency and excess?
Aldosterone Deficiency
→ patients will have low levels of salt and water due to inactivity of aldosterone
→ patients will be hyponatremic and dehydrated
→ because aldosterone promotes hydrogen ATPases to push hydrogen ions out of our body, we can also have acidosis
→ we may also have hypotension
Aldosterone Excess
→ hypernatremia with hypokalemia
→ hypertension
→ patients may have alkalosis
What is Cortisol Deficiency?
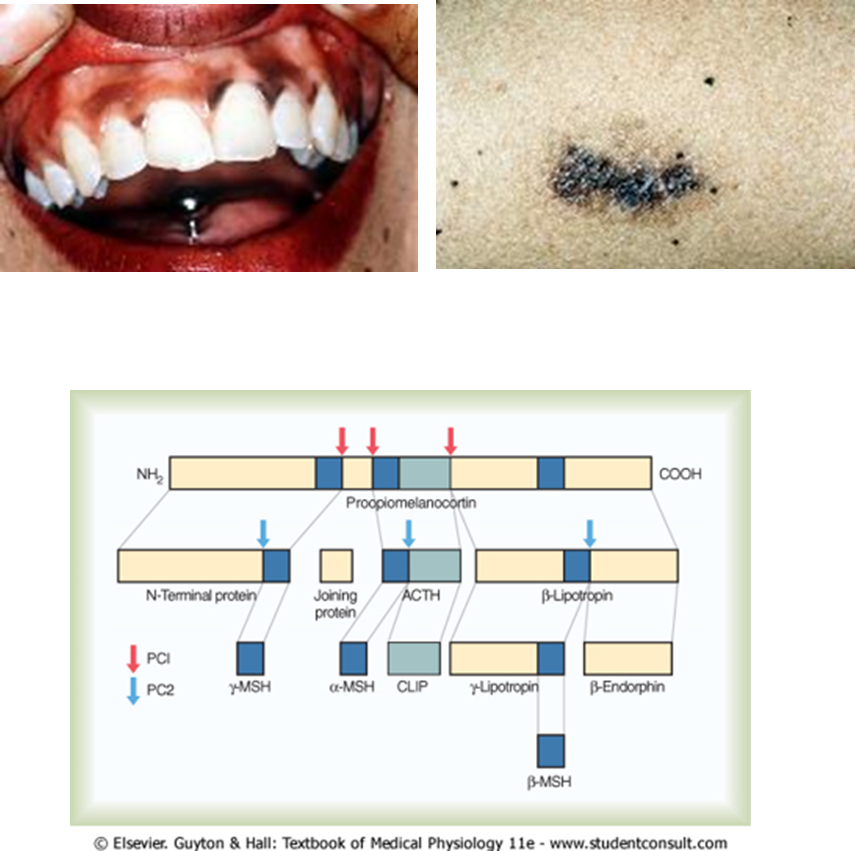
Cortisol Deficiency can be seen in patients like Addison’s Disease where there is destruction of the adrenal cortex
1) Patients will have low cortisol levels resulting in abnormally low glucose levels in the blood (hypoglycemia)
→ patients are weak and fatigued
→ patients may have weight loss and anorexia
→ hypotension
→ hyperpigmentation due to elevated levels of ACTH
What is Congenital Adrenal Hyperplasia?
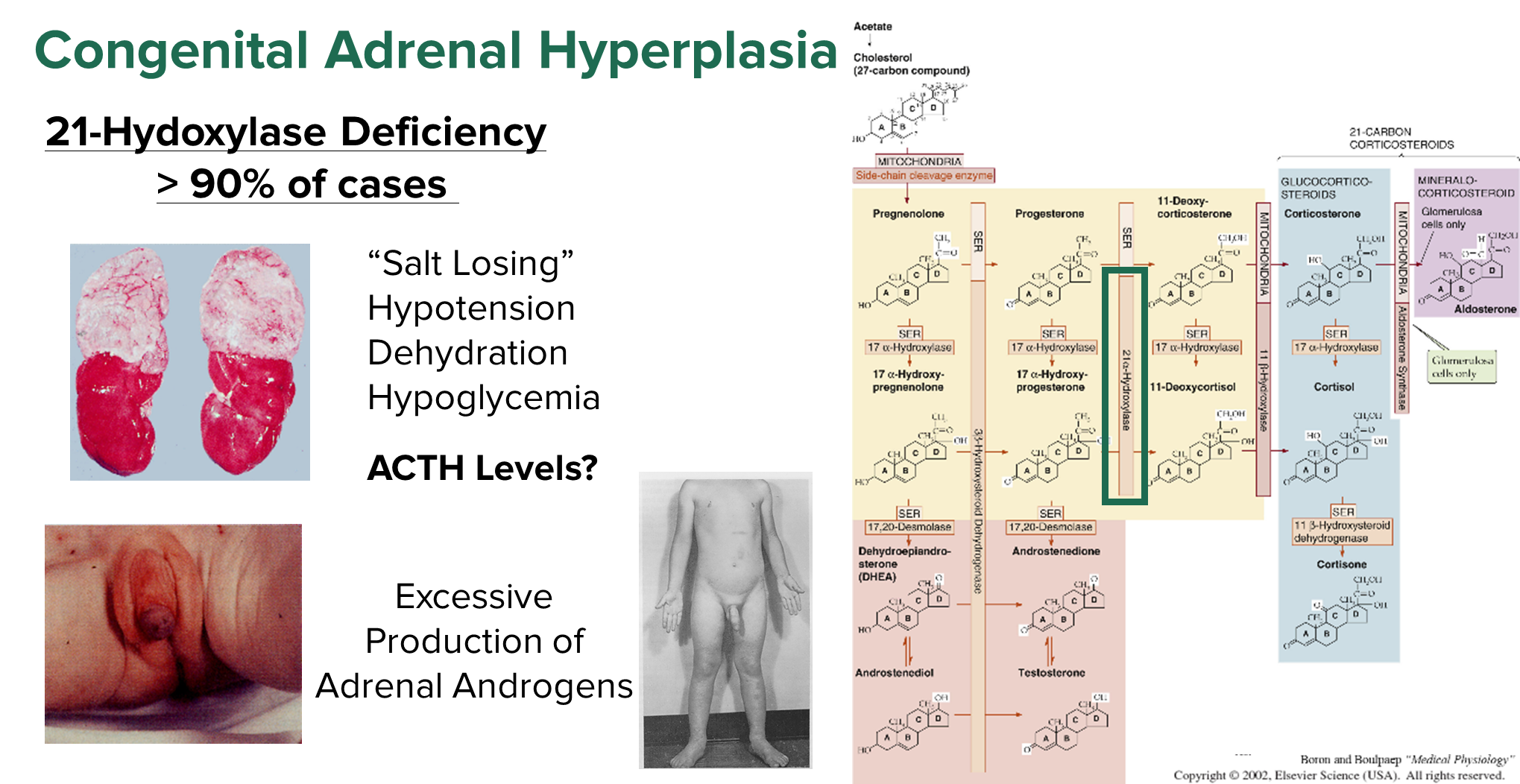
Congenital Adrenal Hyperplasia is a 21-hydroxylase deficiency resulting in a decrease in cortisol and aldosterone
1) Can lead to patients have massive losses of salt with dehydration
→ patients will often be hypoglycemic and hypotensive
2) Patients will have extremely high ACTH levels due to a decrease in cortisol
→ this high ACTH will lead to excessive production of adrenal androgens produced in the zona reticularis instead of production of cortisol and aldosterone
→ can see boys with early puberty and females manifesting with male sex characteristics