NSPT and Periodontal Surgery
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
1.) All of the following are contraindications or reasons for a delay in periodontal surgery except one. Which one is the exception?
a) Poor oral hygiene
b) Periodontal abscesses
c) Unstable hypertension
d) Intravenous bisphosphonates
e) Uncontrolled diabetes mellitus
a) Poor oral hygiene
b) Periodontal abscesses
c) Unstable hypertension
d) Intravenous bisphosphonates
e) Uncontrolled diabetes mellitus
2.) Which of the following types of surgery is best to treat a periodontal bony lesion with deep pockets and vertical bone loss (three-wall defect)?
a) Connective tissue graft
b) Free gingival graft
c) Modified Widman flap
d) Regenerative bone graft
a) Connective tissue graft
b) Free gingival graft
c) Modified Widman flap
d) Regenerative bone graft
3.) Which of the following periodontal conditions is best treated with a subepithelial connective tissue graft?
a) Three wall bony defect
b) Soft tissue recession with root exposure
c) One wall bony defect
d) Class III furcation defect
a) Three wall bony defect
b) Soft tissue recession with root exposure
c) One wall bony defect
d) Class III furcation defect
4.) Which of the following healing responses of periodontal tissues after surgery describes the reformation of tissues that were destroyed due to periodontal disease?
a) New attachment
b) Repair
c) Regeneration
d) Reattachment
a) New attachment
b) Repair
c) Regeneration
d) Reattachment
5.) Which one of the following should be used by a patient to help reduce inflammation and swelling immediately after periodontal surgery?
a) Ice packs
b) Salt water rinsing
c) Aspirin
d) Heat packs
a) Ice packs
b) Salt water rinsing
c) Aspirin
d) Heat packs
6.) Which of the following surgical techniques is indicated for a patient who has gingival enlargement due to nifedipine but no bone loss?
a) Free gingival graft
b) Gingivectomy
c) Connective tissue graft
d) Osseous surgery
a) Free gingival graft
b) Gingivectomy
c) Connective tissue graft
d) Osseous surgery
7.) Which of the following defects heals best with periodontal surgical regeneration?
a) Grade III maxillary molar furcation
b) Horizontal bone loss
c) Three wall bony defect
d) One wall bony defect
a) Grade III maxillary molar furcation
b) Horizontal bone loss
c) Three wall bony defect
d) One wall bony defect
8.) Which of the following bone grafts is taken from an existing mandibular tori in the patient's mouth?
a) Autograft
b) Allograft
c) Xenograft
d) Alloplast
a) Autograft
b) Allograft
c) Xenograft
d) Alloplast
9.) Which of the following bone grafts is taken from human cadavers?
a) Xenograft
b) Alloplast
c) Autograft
d) Allograft
a) Xenograft
b) Alloplast
c) Autograft
d) Allograft
10.) Which of the following materials is used to inhibit epithelial migration into the surgical site?
a) Bone grafts
b) Barrier membranes
c) Sutures
d) Connective tissue
a) Bone grafts
b) Barrier membranes
c) Sutures
d) Connective tissue
11.) Which of the following terms is used for a surgical procedure that will impede the epithelial migration during healing of the periodontal wound?
a) Guided tissue regeneration
b) Incision and drainage
c) Gingival curettage
d) Connective tissue graft
a) Guided tissue regeneration
b) Incision and drainage
c) Gingival curettage
d) Connective tissue graft
Name four Phase I Goals of Treatment:
a.
b.
c.
d.
Name four Phase I Goals of Treatment:
a. complete removal of calculus
b. correction/replacement of poorly-fitting restorations and prosthetics
c. restoration of caries
d. extraction of hopeless teeth
Re-evaluation of tissue response should occur _____ to _____ weeks after periodontal debridement (non-surgical).
Re-evaluation of tissue response should occur 4 to 8 weeks after periodontal debridement (non-surgical).
Non-surgical debridement becomes less effective when probing depths are above _____ mm.
Non-surgical debridement becomes less effective when probing depths are above 4 mm.
TRUE or FALSE: A gain in clinical attachment is possible with non-surgical therapy.
FALSE
The rate of subgingival biofilm recolonization is dependent upon ____________________________.
The rate of subgingival biofilm recolonization is dependent upon supragingival biofilm accumulation (oral hygiene self-care).
TRUE or FALSE: NSPT is used to regenerate tissues.
FALSE
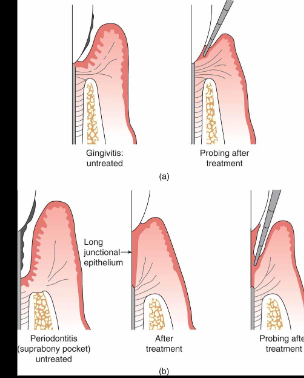
Following NSPT, the epithelium forms a ________ ___________ ____________.
Following NSPT, the epithelium forms a long junctional epithelium.
In the lamina propria, the inflammatory infiltrate will be replaced by collagen but the JE does not allow a new CT attachment to form. Why?
NSPT allows for the repair, not the regeneration, of tissues. The healed tissue is a scar, and the destroyed CT attachment is replaced with a long JE. The destruction/damage done to the CT attachment and root surface CANNOT return to a state of pristine health, nor can it be regenerated via NSPT.
Repair and healing can be altered and/or delayed in patients who are:
a.
b.
c.
Repair and healing can be altered and/or delayed in patients who are:
a. diabetic
b. immunocompromised
c. smokers
Reduction in probing depths after NSPT is due to what?
A combination of gingival recession (shrinkage) and an increase (NOT regeneration!) of the clinical attachment (top of the long JE).
Periodontal debridement becomes less effective in pockets that are _____________.
Periodontal debridement becomes less effective in pockets that are >4mm.
Re-evaluation of initial therapy includes:
a.
b.
c.
d.
Re-evaluation of initial therapy includes:
a. Tissue response and condition (color, contour, texture, consistency)
b. Probing depths, BOP, CAL
c. Mobility and furcation involvement
d. Evidence of inflammation
Name five objectives of periodontal therapy:
a.
b.
c.
d.
e.
Name five objectives of periodontal therapy:
a. Reduction in pocket depth to allow for better access for plaque control; to create an oral environment that is maintainable by the pt and DH
b. Gain access to the root and underlying bone, removing remaining calculus, smoothing out gouges and Sharpey’s fibers pits
c. Regenerate periodontal tissues destroyed due to disease
d. Arrest disease progression
e. Improvement of the prognosis of teeth and their replacements, including esthetics
Name five contraindications or precautions for periodontal surgery:
a.
b.
c.
d.
e.
Name five contraindications or precautions for periodontal surgery:
a. uncontrolled DM
b. HIV
c. smokers
d. CV conditions
e. pts who are noncompliant with plaque control or perio maintenance appts
DEFINE:
a. reattachment
b. regeneration
DEFINE:
a. reattachment: reunion of epithelial or connective tissue to a root surface that was not damaged or destroyed by periodontal disease
b. regeneration: attachment apparatus (bone, cementum, PDL) is reformed on a root surface that was previously pathologically exposed
Epithelial tissues are fast-growing and can migrate up to ______ mm/day.
Epithelial tissues are fast-growing and can migrate up to 0.5 mm/day.
How does the fast-growing epithelial tissue interfere with healing and regeneration?
Epithelial growth occurs faster than bone and CT, allowing it to displace bone and tissue grafts and to prevent angiogenesis.
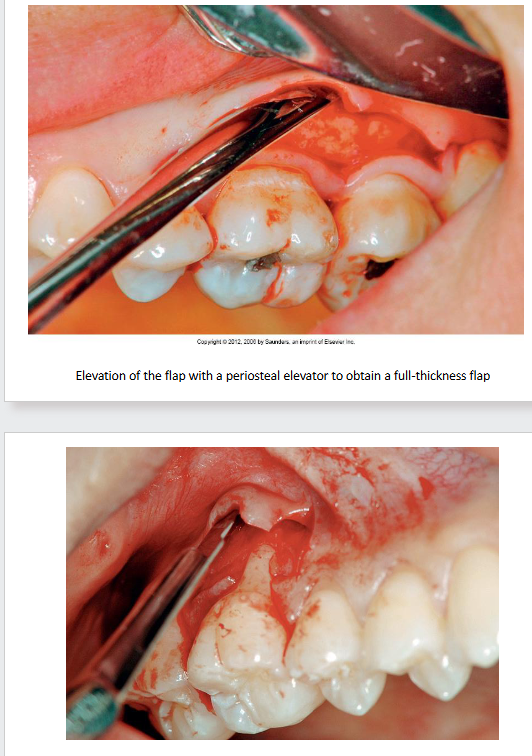
DEFINE:
a. full- (mucoperiosteal) thickness flap
b. partial- (split) thickness flap
DEFINE:
a. full- (mucoperiosteal) thickness flap: gingiva, alveolar mucosa, and periosteum are reflected from the root and underlying bone surface
b. partial- (split) thickness flap: periosteum and some gingival connective tissues are left attached to the bone and are not included in the reflected flap
Why is a crown lengthening procedure done?
A crown lengthening procedure exposes more tooth structure (creates an area for supracrestal tissue attachment) for the purpose of properly restoring a tooth, especially one that is fractured or decayed close to/at/apical to the AC.
DEFINE:
a. ostectomy
b. osteoplasty
DEFINE:
a. ostectomy: removal of tooth-supporting bone
b. osteoplasty: reshaping
A ____ -wall bony defect responds best to regeneration.
A 3-wall bony defect responds best to regeneration.
DEFINE:
a. autogenous
b. allograft
c. xenograft
d. DFDBA
e. osteogenic
f. osteoinductive
g. osteoconductive
DEFINE:
a. autogenous: material harvested from one part of the body and grafted to another part of the pt’s body; the gold-standard grafting material; osteogenic
b. allograft: material obtained from other individuals of the same species but that are genetically different; osteoinductive
c. xenograft: type of natural bone substitute obtained from a genetically-different species; osteoinductive when used with allografts or osteoconductive when used alone
d. DFDBA: demineralized freeze-dried bone allograft; one of the main forms of bone allografts; osteoinductive
e. osteogenic: process of new bone formation by bone cells from the host or the graft; ex: autogenous bone (autograft)
f. osteoinductive: mesenchymal stem cells from the graft are induced to differentiate into osteoblasts which produce new bone; ex: allografts like DFDBA, BMP-2, and growth factors like PDGF
g. osteoconductive: bone material serves as a scaffold or filler that allows bone from the surrounding area to grow over and into them; does NOT produce new bone and requires the presence of existing bone; ex: alloplasts, xenografts when used alone
Name four adverse effects of periodontal surgical procedures:
a.
b.
c.
d.
Name four adverse effects of periodontal surgical procedures:
a. cellulitis/infection
b. tooth mobility
c. gingival recession
d. loss of sensation
Name the three types of soft tissue grafts:
a.
b.
c.
Name the three types of soft tissue grafts:
a. pedicle graft
b. free gingival graft (FGG)
c. connective tissue graft (CTG)
Which type of soft tissue graft is better for augmentation of attached gingiva than for esthetic results?
free gingival graft (FGG)
Which type of soft tissue graft is better for esthetics and root coverage?
subepithelial connective tissue graft (CTG)
Name two sources of tissue for soft tissue grafts:
a.
b.
Name two sources of tissue for soft tissue grafts:
a. surface of palate
b. underneath surface of palate
Debridement
The rate of subgingival biofilm recolonization is dependent upon supragingival biofilm accumulation, making OH self-care and professional periodontal debridement essential!
Oral prophylaxis: removal of biofilm, calculus, and stains from the exposed and unexposed surfaces of the teeth by scaling and polishing as a preventive measure for the control of local irritants
Periodontal debridement: removal of calculus, debris, and dental biofilms and their byproducts from the tooth surface and gingival crevice to treat gingival and periodontal inflammation
NSPT (initial phase/Phase I): thorough debridement in conjunction with a high degree of oral hygiene with the goal of returning the tissue to a state of “maintainable health” and a reduction of inflammation
SRP = scaling and root planing
scaling: removal of dental biofilm, calculus, and stains from tooth surface
root planing: removes necrotic cementum and surface dentin that is rough, impregnated with calculus, or contaminated with toxins (LOS) or microorganisms
the removal of subgingival microbial flora results in a delay in repopulation of pathogenic microbes
Surgical Intervention (Phase II):
gain access to the root and underlying bone to remove any remaining calculus, smooth out existing gouges and Sharpey’s fiber pits
regenerate periodontal tissues destroyed due to disease
arrest disease progression
reduce pocket depth to allow for better access for plaque control, improve the prognosis of teeth and their replacements
esthetic improvement
to create an oral environment that is maintainable by the pt and DH
NSPT (Non-surgical Periodontal Treatment)
Goals of NSPT:
Immediate goal: to prevent, arrest, control, or eliminate periodontal diseases
Ideal goal: promote healing through regeneration of lost form, function, esthetics, and comfort
Accepted goal: to repair damaged tissue
Ultimate goal: to sustain masticatory system in a state of health
.
Determinants of Success:
use of appropriate equipment, professional knowledge, skill, experience, knowing your capabilities
pt compliance
severity of disease
host immune response
.
Limitations of Periodontal Debridement:
becomes less effective when PD >4mm
increased PD → greater % of tooth surfaces exhibit residual calculus
NSPT: 17-69% residual
surgical access: 14-24% residual
concavities
furcations
.
Outcomes of Periodontal Debridement
Measurable endpoints: CAL, PDs, visual signs of inflammation, reduction in BOP % score, reduction in PI score, alterations and reductions in subgingival biofilms
Phase I
Goals:
complete removal of calculus
correction or replacement of poorly fitting restorations and prosthetics
restoration of caries
orthodontics
elimination of food impaction areas
management of occlusal trauma
extraction of hopeless teeth
antimicrobials and host modulators
.
Sequence:
OHI (plaque control instruction)
Scaling (removal of sub and supragingival deposits)
Recontouring defective restorations and crowns
Caries control
Tissue reevaluation
Tissue Changes After Periodontal Debridement: Gingivitis
Once biofilm and calculus are removed, healing occurs…
pocket epithelium → JE → forms an attachment to adjacent tooth surface via hemidesmosomes
inflammatory infiltrate → gradually replaced by maturing collagen fibers → organize into functionally orientated bundles
final healing = long junctional epithelium
color changes: red → uniform pink
PD changes → formation of a physiological gingival sulcus with a goal of a “normal” PD of 1-3mm
Since there was NO loss of attachment and the root surface was not damaged, gingivitis is considered REVERSIBLE. Healing results in tissues that are restored to CLINICAL GINGIVAL HEALTH (but NOT PRISTINE).
Tissue Changes After Debridement (NSPT/SRP): Periodontitis
Once biofilm and calculus are removed, healing should occur…
pocket epithelium → JE → covers the root surface down to the base of the original pocket (long epithelial attachment)
epithelial cells move very quickly to repopulate the root surface
inflammatory infiltrate of lamina propria → replaced by collagen, but the fast reproduction of the JE does NOT allow a new CT attachment to form
.
Complete healing in 1-2 weeks depends on:
severity of inflammation
PD
effectiveness of debridement
resolution of inflammation
.
Host repair and healing capacity are altered with:
diabetes
immunocompromised host
smoking status
Gain in Clinical Attachment
REPAIR ≠ REGENERATION
Non-surgical (Periodontal Debridement/NSPT): removal of plaque biofilms, calculus, and contaminated cementum → eliminates inflammation and allows tissues to REPAIR
Surgery: attempts are made for REGENERATION
Connective Tissue Attachment Level: the level on the root at which the most coronal fibers are attached (histologically); corresponds roughly to the base of the pocket as identified by probing in periodontitis
a “gain” in clinical attachment refers to a DECREASED PENETRATION OF THE PROBE at the base of the pocket after tx, NOT new connective tissue attachment
reduction of pocket depths = long epithelial attachment (NO real CT attachment is reformed — the JE is a weak attachment and can easily let go, contributing to the pt’s high susceptibility for recurrence of periodontitis)
Factors Affecting CAL Measurement:
pseudopocket (gingival inflammation = coronal migration of FGM)
probing technique (overangulation, pressure and integrity of JE)
tooth anatomy
presence of calculus (probe hits calc and not the pocket base)
reduction in PD due to recession and/or an increase in clinical attachment via the top of a long JE
Cementum and NSPT
When exposed in a periodontal pocket, cementum…
becomes contaminated
endotoxin (LOS) is loosely and superficially attached to the root surface (no need for extensive root planing)
calculus forms in Sharpey’s fibers pits
Note: It is NOT always easy to determine the end point for debridement!
Reevaluation of Initial Therapy
Purpose: Determine the need for Phase II (Surgical Intervention)
tissue response (evaluated after 4-8 wks)
color, contour, texture, consistency
BOP / Evidence of Inflammation
PD
OIC
Mobility
Furcations
CAL
Phase II (Surgical Intervention)
Types of Periodontal Surgery:
Gingivectomy
Gingivoplasty
Periodontal Flap Surgery
Flap Surgery with Osseous Recontouring
Periodontal Plastic Surgery
Periodontal Regeneration
Indications:
Pocket elimination/reduction
Correction of mucogingival defects
root coverage
increase in keratinized/attached gingiva
Create a favorable restorative environment
crown lengthening (restoring supracrestal attachment)
Esthetics
.
Contraindications: Systemic diseases that CANNOT BE CONTROLLED by medications or otherwise
uncontrolled DM
CV conditions
HIV
smokers
bleeding disorders (hemophilia, blood thinners)
IV bisphosphonates
noncompliance with plaque control or perio maintenance appts
concern for cosmetic outcome
hopeless teeth
Preoperative Preparation:
successful completion of Phase I (increases manageability of tissues during surgery and better healing)
addressed uncontrolled/poorly controlled systemic diseases
elimination of plaque-retentive restorations
endo procedures
smoking cessation
Postoperative Healing Following Periodontal Surgery
REPAIRATIVE Procedures (not regenerative):
scar formation (healing occurs, but scar tissue is different from original tissue)
destruction of CT attachment is healed with a long JE
Reattachment: reunion of epithelium or CT to a root surface that was not damaged or destroyed by periodontal disease
Regeneration: attachment apparatus (bone, cementum, & PDL) is reformed on a root surface that was previously pathologically exposed
regeneration is the IDEAL healing response but is NOT ALWAYS ATTAINABLE (usually a PARTIAL regeneration is obtained)
epithelial cells migrate (0.5mm/day) MUCH FASTER than bone or CT which interferes with total regeneration
epithelial growth can displace bone/tissue grafts and can prevent angiogenesis
Periodontal Surgery: Gingivectomy/Gingivoplasty
Gingivectomy: excision or removal of gingiva in order to eliminate a pocket
Gingivoplasty: reshaping of gingiva
.
Indications:
gingival enlargement due to inflammation or medication
pseudopockets
suprabony pockets
Contraindications:
lack of attached gingiva
infrabony pockets
limited use
.
Procedure:
surgical anesthesia
mark base of pocket
incision with blade angled 45 degrees to gingiva and apical to the base of the pocket
a wedge of gingiva is removed (gingivectomy)
gingivoplasty is performed to reshape gingiva
complete healing: 4-5 weeks
Periodontal Surgery: Periodontal Flap Surgery
Purpose: to gain access to the root surface and bone
Flap: loosened portion of gingiva and alveolar mucosa that is separated from the underlying structures (except for its base because this is where the flap receives blood supply)
Full-thickness (mucoperiosteal) Flap: gingiva, alveolar mucosa, and periosteum are reflected from the root and underlying bone surface
Partial-thickness (split) Flap: periosteum and some gingival connective tissue are left attached to the bone and are not included in the reflected flap
.
Types of Surgical Flap Procedures:
Pocket Reduction
apically-positioned flap
Bone Graft
coronally-positioned flap (attempt to cover surgical site after placement of a bone graft)
For Improved Periodontal Debridement & Reduction in Inflammation and Pocket Depths
Modified Widman Flap (conservative surgical approach with no osseous contouring that better preserves esthetics in mx. ant.)
.
Healing
tissues look healed within a few weeks
complete tissue maturation is complete in 1-2 months
Periodontal Surgery: Crown Lengthening
Purpose: expose more tooth structure for the purpose of properly restoring a tooth; creates an area for supracrestal tissue attachment (biologic width)
Indications: teeth that have fracture or decay close to, at, or apical to, the AC of bone

Periodontal Surgery: Treatment of Osseous Defects
Ostectomy: removal of tooth-supporting bone
Osteoplasty: reshaping
Reshaping of Osseous Architecture: both ostectomy and osteoplasty are used to recreate natural contours and relationships; gingiva follows the form of the bone
Bone Regeneration (Bone Grafts)
Periodontal Surgery: Bone Regeneration (Bone Grafts)
3-Wall Infrabony defects respond BEST with regeneration bone fill because the 3 remaining walls help contain the graft material.
Defects with HBL CANNOT be treated with regenerative surgery because there is no place to put the graft.
.
Types of Bone Regeneration:
Osteogenic: process of NEW bone formation by BONE CELLS from the host or the graft (e.g. autogenous/autograft)
Autogenous bone is considered to be the GOLD STANDARD of grafting materials in terms of stimulating NEW BONE FORMATION
Osteoinductive: MESENCHYMAL STEM CELLS from the graft are induced to differentiate into osteoblasts which produce new bone (e.g. allografts like DFDBA, BMP-2 / Bone Morphogenic Protein, Growth Factors like PDGF / Platelet Derived Growth Factor, xenografts when used with allografts)
Osteoconductive: bone material serves as a SCAFFOLD or FILLER that allows bone from the surrounding area to grow over and into them; does NOT PRODUCE NEW BONE; requires the presence of existing bone (more existing bone = greater chance of success); (e.g. alloplasts, xenografts when used alone)
.
Types of Bone Grafts:
Autografts: bone harvested from one part of the body (mx. tuberosity, edentulous area, chin, extraction socket, mnd. torus, iliac crest) and grafted to another part of the SAME PATIENT’S BODY; osteogenic
Allografts: bone material obtained from OTHER INDIVIDUALS of the SAME SPECIES but GENETICALLY DIFFERENT (human cadavers); material is sterilized and stored in bone banks, usually in the form of demineralized freeze-dried bone (DFDBA) or freeze-dried bone (FDBA); osteoinductive
Alloplasts: made of biocompatible, organic, inert materials (synthetic hydroxyapatite, calcium sulfate, bioactive glass, tricalcium phosphate, collagen); osteoconductive
Xenografts: a type of natural bone substitute derived from a GENETICALLY DIFFERENT species (e.g. bovine); osteoinductive when used with allografts or osteoconductive when used alone
.
Biological Materials: growth factors are only found in LIVING cells (bone, blood platelets, etc.)
GEM21 (platelet-derived growth factor / PDGF)
Emdogain (porcine enamel matrix protein derivative, enamel-related proteins from HERS)
Bone Morphogenic Proteins / BMPs (found in bone and induces new bone formation)
.
Epithelium, Membranes, and Healing
Membranes are used as barriers to increase the success for bone regeneration.
Membranes placed over the bony defect with the flap sutured will prevent the epithelium/CT inside the flap from filling in the defect.
The “space” created between the tooth and the flap by the membrane allows the PDL cells (osteoblasts, fibroblasts, cementoblasts) to migrate from the PDL onto the tooth surface and into the defect.
Types of Membranes:
Nonabsorbable
second surgery is needed for removal; first used in clinical periodontics
Absorbable
preferred membranes because a second surgery is not needed for removal; remain in place for 3-4 weeks
Periodontal Surgery: Root Resection
Root Resection (aka: root amputation, hemisection): removal of a root while leaving the crown on a multirooted tooth
Note: now a rare procedure
Periodontal Surgery: Plastic Surgery
Indications:
inadequate width and thickness of attached gingiva
sites that show progressive gingival recession
sites of inadequate attached gingiva with a subgingival restoration
sites of inadequate attached gingiva that require orthodontics
elimination of frenum/muscle pull at or near the GM of a tooth
base of periodontal pocket extends to, or beyond, the MGJ
Purposes:
deepen the buccal vestibule for dentures or restorations
esthetics (cover exposed root surfaces)
modification (gingival augmentation) of edentulous ridges prior to prosthetic reconstruction
Mucogingival Conditions Around Natural Teeth
Recession: an apical shift of the GM caused by different conditions and pathologies
associated with clinical attachment loss
can apply to all surfaces (buccal/lingual/interprox.)
tendency to increase with age
88% of people aged ≥ 65 years
50% of people aged 18-64
occurs in populations with both high and low standards of oral hygiene
.
Consequences of Recession/Root Exposure:
impaired esthetics
dentinal hypersensitivity
root caries
NCCLs (due to abrasion/erosion)
.
Features Used to Describe Mucogingival Conditions Involving Gingival Recession:
Interdental CAL
Gingival Phenotype (gingival thickness and KTW)
Root surface condition (NCCLs, Root Caries)
Detection of CEJ
Tooth position
Aberrant frenum
Vestibular Depth
Number of adjacent restorations
NOTE: Mucogingival conditions can be present WITHOUT GINGIVAL RECESSION!
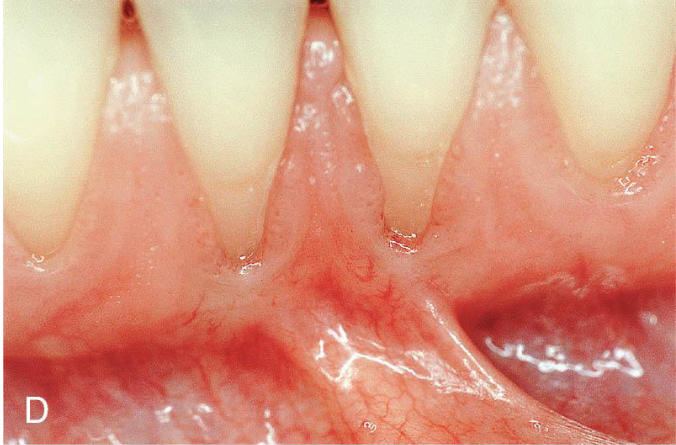
Periodontal Phenotype and Recession
Periodontal Phenotype: determined by the gingival phenotype and bone morphotype; indicates a dimension that may change through time (environmental factors, clinical intervention, etc.) and can be site-specific
Gingival phenotype: 3D gingival volume considering the thickness of gingival tissue and width of keratinized tissue/KTW)
Bone morphotype: thickness of buccal bone plate
.
Assessing Periodontal Phenotype:
KTW = distance from FGM to MGJ
gingival thickness: observe the probe shining through the gingival tissue after inserting it into the sulcus
thin: probe VISIBLE (≤1mm)
thick: probe NOT visible (>1mm)
Notes:
A THIN phenotype INCREASES the risk for gingival recession and its progression.
ANY AMOUNT of gingiva is sufficient to maintain periodontal health WHEN optimal OH is attainable (aka an “inadequate” thickness and KTW of gingiva makes optimal OH difficult to achieve)
there is INCONCLUSIVE DATA that improper toothbrushing influences the development and progression of recession
there MAY BE AN ASSOCIATION between intrasulcular restorative/prosthetic cervical margin placement and the development of recession particularly in thin phenotypes (gingiva cannot attach to Class V Restorations or NCCLs)
SEVERAL STUDIES REPORT observation of recession following orthodontic tx (esp. mnd. incisors)
the development and progression of gingival recession is NOT ASSOCIATED WITH INCREASED TOOTH MORTALITY
recession is frequently associated with dentin hypersensitivity and carious/NCCLs
there is NOT ENOUGH EVIDENCE to conclude that surgical root coverage reduces cervical dentin hypersensitivity
esthetic concerns, dentin hypersensitivity, cervical lesions, thin phenotypes, and mucogingival deformities are best addressed by mucogingival intervention when deemed necessary
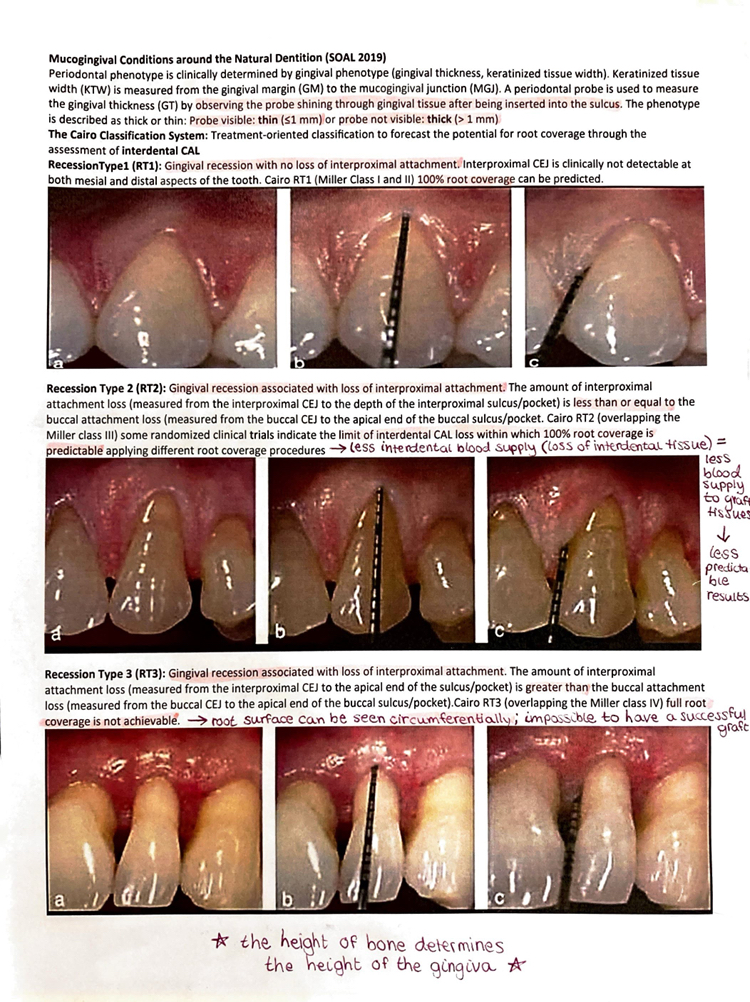
Cairo Classification System
Cairo Classification System: treatment-oriented classification to forecast the potential for root coverage throughout the assessment of interdental CAL
RecessionType1 (RT1): recession with NO loss of interprox. attachment
CEJ is not clinically detectable at mesial/distal aspects
100% root coverage can be predicted
RecessionType2 (RT2): recession WITH loss of interprox. attachment
interprox attachment loss is ≤ buccal attachment loss
some clinical trials indicate the limit of interdental CAL loss within which 100% root coverage is predictable using root coverage procedures
RecessionType3 (RT3): recession WITH loss of interprox. attachment;
interprox attachment loss is > buccal attachment loss
full root coverage is NOT achievable
Soft Tissue Grafts
Types of Soft Tissue Grafts:
Pedicle Graft
MOVES (WITHOUT ACTUALLY REMOVING) gingiva from an adjacent tooth/edentulous area with adequate amounts of gingiva (donor site) to an adjacent tooth with inadequate amounts of attached gingiva (recipient site)
limited application
Free Gingival Graft (FGG)
tissue is HARVESTED from the SURFACE OF THE PALATE
more predictable for augmentation of attached gingiva than for root coverage
not as esthetic as CTG
Subepithelial Connective Tissue Graft (CTG)
tissue is HARVESTED from UNDERNEATH THE SURFACE OF THE PALATE
procedure of choice for root coverage because…
less shrinkage of tissue occurs
no open wound on palate
better blood supply
better esthetics (tissue color blend)
indicated for single or multiple adjacent teeth with gingival recession and root exposure
Allografts (Alloderm)
regeneration tissue matrix
biomaterial from human tissue with all epidermal and dermal cells removed
attempt for root coverage
material must be refrigerated and rehydrated
.
Mucosal Release: the mucosa that is flapped back and then stretched over the donor site
.
Periodontal Dressing (Coe-pak)
some surgeons use a dressing or packing after surgery, but others do not because it creates an anaerobic environment
a noneugenol, non-irritating/non-burning type is available
purpose: pt comfort
stents can be placed over donor sites
.
Surgical Complications
fear, anxiety, syncope, hypoglycemia, tachycardia from epi (lido 1:50,000), excessive bleeding
pain (ice pack 15-20 mins on and off to reduce swelling and pain; the more bony involvement and mucosal release, the more pain experienced, use oral analgesics)
.
Postoperative Visit Management
7-10 days after surgery for dressing and suture removal, wound cleansing (CHX & H2O2)
limited OH
.
Adverse Effects
cellulitis/infection
brusing
tooth mobility (should decrease over time/may need occlusal adjustment)
gingival recession (tissue can rebound, initially scar tissue)
loss of sensation (scar tissue, paresthesia from swelling/trauma/anesthetic)
dentinal hypersensitivity
changes in taste (CHX, dentures)
open embrasures (may fill in)