MicroLab - Quiz
1/107
Earn XP
Description and Tags
Control of Microbial Growth, Microbiome, and Biochemical Tests (Experiment 7)
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
108 Terms
aseptic techniques
Semmelweiss and Lister helped develop this to prevent contaminations of surgical wounds in 1800
before the development of aseptic techniques
nosocomial infections caused death in 10% of surgeries
up to 25% of mothers that delivered in hospitals died due to infections
early civilization practices for controlling microbial growth
salting
smoking
pickling
drying
exposure of food and clothing to sunlight
some use spices in cooking to mask the taste of spoiled food
some spices prevent spoilage
sterilization
killing or removing all forms of microbial life (including endospores) in a material or an object
the most commonly used method of sterilization
heating
commercial sterilziation
heat treatment that kills endospores of Clostridium botulinum which is the causative agent of botulism in canned food
does not kill endospores of thermophiles, which are not pathogens and may grow at temperatures above 45C
disinfection
reducing the number of pathogenic microorganisms to the point where they no longer cause diseases
usually involves the removal of vegetative or non-endospore forming pathogens
may use physical or chemical methods
disinfectant
applied to inanimate object
antiseptic
applied to living tissues (antisepsis)
degerming
mechanical removal of most microbes in a limited area
example: alcohol swab on the skin
sanitization
use of chemical agents on food-handling equipment to meet public health standards and minimize chances of disease transmission
example: hot soap and water
sepsis
comes from the Greek word for decay or putrid
indicates bacterial contamination
asepsis
absence of significant contamination
aseptic technique definition
used to prevent contamination of surgical instruments, medical personnel, and patients during surgery
also used to prevent bacterial contamination in the food industry
bacteriostatic agent
an agent that inhibits the growth of bacteria, but does not necessarily kill them.
suffix: -statis
to stop or steady
germicide
an agent that kills certain microorganisms
bactericide
kills bacteria; most do not kill endospores
viricide
kills or inactivates viruses
fungicide
kills fungi
sporicide
kills bacterial endospores and fungal spores
rate of microbial death
when the bacterial populations are heated or treated antimicrobial chemicals, they usually die at a constant rate
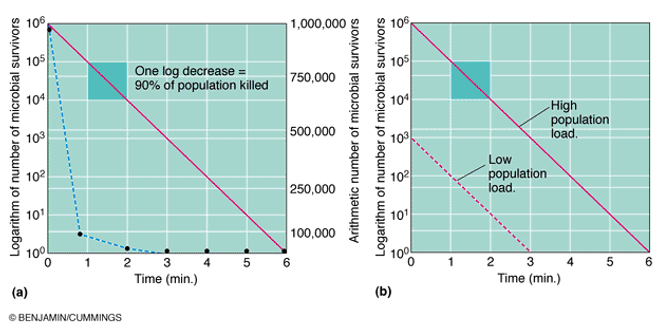
factors that influence the effectiveness of antimicrobial treatment
number of microbes = the more microbes present, the more time it takes to eliminate a population
type of microbe = endospores are very difficult to destroy. vegetative pathogens vary widely on susceptibility to different methods of microbial control
environmental influences = presence of organic material (blood, feces, saliva) tends to inhibit antimicrobials, pH, etc.
time of exposure = chemical antimicrobials and radiation treatments are more effective at longer times. in heat treatments, longer exposure compensates for lower temperatures
heat
kills microorganisms by denaturing their enzymes and other proteins
heat resistance varies widely among microbes
thermal death point (IDP)
lowest temperature at which all of the microbes in a liquid suspension will be killed in ten minutes
thermal death time (TDT)
minimal length of time in which all bacteria will be killed at a given temperature
decimal reduction time (DRT)
time in minutes at which 90% of bacteria at a given temperature will be killed; used in the canning industry
moist heat
kills microorganisms by coagulating their proteins
much more effective than dry heat
reliable sterilization with most heat required temperatures above that of boiling water
boiling
heat to 100C or more at sea level
hills vegetative forms of bacterial pathogens, almost all viruses, and fungi and their spores within 10 minutes or less.
endospores and some viruses are not destroyed this quickly. however, brief boiling will kill most pathogens
Hepatitis virus
can survive up to 30 minutes of boiling
endospores
can survive up to 20 hours or more of boiling
autoclave
chamber which is filled with hot steam under pressure
preferred method of sterilization, unless material is damaged by heat, moisture, or high pressure
temperature of the steam reaches 121C at twice the atmospheric pressure
most effective when organisms contact steam directly or are contained in a small volume of liquid
all organisms and endospores are killed within 15 minutes
require more time to reach the center of solid or large volume of liquid

pasteurization
developed by Louis Pasteur to prevent spoilage of beverages
used to reduce microbes responsible for the spoilage of beer, milk, wine, juices, etc.
Classic method of pasteurization
milk was exposed to 65C for 30 minutes
high temperature short time pasteurization (HTST)
used today, the milk is exposed to 72C for 15 seconds
ultra high temperature pasteurization (UHT)
milk is treated at 140C for 3 seconds then cooled very quickly in a vacuum chamber
advantage: milk ca be stored at room temperature for several months
dry heat
kills by oxidation effects
direct flaming
used to sterilize inoculating loops and needles; heat metal until it has a red glow
incineration
effective way to sterilize disposable items (paper cups, dressings) and biological wastes
hot air sterilziation
place objects in an oven
requires 2 hours at 170C for sterilization
dry heat transfers heat less effectively to a cool body than moist heat
filtration
removal of microbes by passage of a liquid or gas through a screen-like material with small pores.
used to sterilize heat sensitive materials like vaccines, enzymes, antibiotics, and some culture media
high efficiency particulate air filters (HEPA)
used in operating rooms and burn units to remove bacteria from the air
membrane filters
uniform pore size
used in the industry of research
different sizes of membrane filters
0,22 and 0.45 um pores = used to filter most bacteria; does not retain spirochetes, mycoplasmas, and viruses
0.01 um pores = retains all viruses and some large proteins
low temperature
effect depends on the microbe and treatment applied
refrigeration
temperatures from 0-7C
bacteriostatic effects
reduces metabolic rate of most microbes so they cannot reproduce or produce toxins
freezing
temperatures below 0C
over a third of vegetative bacteria may survive 1 year
most parasites are killed by a few days of freezing
flash freezing
does not kill most microbes
slow freeszing
more harmful because ice crystals disrupt cell structure
dessication
in the absence of water, microbes cannot grow or reproduce, but some remain viable for years
after water becomes available, they start growing again
susceptibility to dessication varies widely
Neisseria gonorrhea = only survives about one hour
Mycobacterium tuberculosis = may survive several months; viruses are fairly resistant
Clostridium spp. and Bacillus spp. = may survive decades
osmotic pressure
the use of high concentrations of salts and sugars in food is used to increase the osmotic pressure and create a hypertonic environment
yeasts and molds = more resistant to high osmotic pressure
Staphylococci spp. that live on skin = fairly resistant to high osmotic pressure
plasmolysis
as water leaves the cell, plasma membranes shrink away from the cell wall
cells may not die, but usually stops growing
ionizing radiation
gamma rays, x rays, electron beams, or higher energy rays
have short wavelengths (< 1 nanometer)
dislodges electrons from atoms and form ions
causes mutations in DNA and produce peroxides
used to sterilize pharmaceuticals and disposable medical supplies
disadvantages: penetrates human tissues; may cause genetic mutations in humans
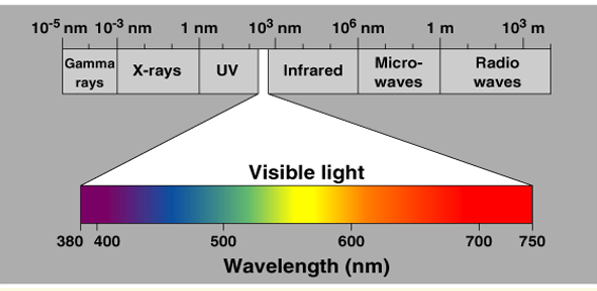
ultraviolet light (non-ionizing radiation)
wavelength is longer than 1 nanometer
damages DNA by producing thymine dimers, which causes mutations
used to disinfect operating rooms, nurseries, and cafeterias
disadvantages: damages skin, eyes; doesn’t penetrate paper, glass, or cloth
microwave radiation
wavelength ranges from 1 millimeter to 1 meter
heat is absorbed by water molecules
may kill vegetative cells in moist food
bacterial endospores, which does not contain water, are not damaged by microwave radiation
solid food are unevenly penetrated by microwaves
trichinosis outbreaks have been associated with port cooked in microwaves
types of disinfectants
phenols and phenolics
halogens
alcohols
heavy metals
quaternary ammonium compounds (quats)
aldehydes
gaseous sterilizers
peroxygens
phenol
carbolic acid
was first used by Lister as a disinfectant
rarely used today because it is a skin irritant and has a strong odor
used in some throat sprays and lozenges
acts as a local anesthetic
phenolics
chemical derivatives of phenol
cresols
derived from coal tar (lysol)
bisphenols (pHisoHex)
effective against gram-positive staphylococci and streptococci
used in nurseries
excessive use in infants may cause neurological damage
advantages of phenols and phenolics
destroy plasma membranes and denature proteins
stable
persist for longer times after application
remains active in the presence of organic compounds
halogens
effective alone or in compounds
iodine
tincture of iodine = alcohol solution; the first antiseptics used
combines with amino acid tyrosine in proteins and denatures proteins
stains the skin and clothes
somewhat irritating
iodophors
compounds with iodine that are slow releasing
takes several minutes to act
used as skin antiseptic in surgery
not effective against bacterial endospores
examples: betadine, isodine
alcohol
kills bacteria, fungi, but not endospores or naked viruses
acts by denaturing proteins and disrupting cell membranes
evaporate, leaving no residue
used to mechanically wipe microbes off skin before injections or blood drawing
not good for open wounds, because it causes proteins to coagulate
ethanol
drinking alcohol
optimum concentration is 70%
isopropanol
rubbing alcohol
better disinfectant than ethanol; cheaper and less volatile
heavy metals
includes copper, selenium, mercury, silver, and sic
oligodynamic action = very tiny amounts are effective
silver
1% silver nitrate used to protect infants against gonorrheal eye infections until recently
mercury
organic mercury compounds like Merthiolate and mercurochrome are used to disinfect skin wounds
copper
copper sulfate is used to kill algae in pools and fish tanks
selenium
kills fungi on their spores
used for fungal infections
also used in dandruff shampoos
zinc
zinc chloride = mouthwashes
zinc oxide = antifungal agents in paint
quaternary ammonium compounds (quats)
widely used surface active agents
cationic (positively charge) detergents
effective against gram—positive bacteria, less effective against gram-negative bacteria
can also destroy fungi, amoeba, and enveloped viruses
Zephiran, cepacol = also found in our lab spray bottles
Pseudomonas = strains that are resistant and can grow in the presence of quats are the big concern of hospitals
advantages: strong antimicrobial action, colorless, odorless, tasteless, stable, nontoxic
disadvantages: forms foam, organic matter interferes with effectiveness, neutralized by soap and anionic detergents
aldehydes
includes some of the most effective microbials
inactivates proteins by forming covalent crosslinks with several functional groups
formaldehyde gas
excellent disinfectants
commonly used as formalin, a 37% aqueous solution
formalin was used extensively to preserve biological specimens and inactivate viruses and bacteria in vaccines
irritates mucous membranes, and has a strong odor
also used in mortuaries for embalming
formaldehyde inactivates microorganisms by alkylating the amino and sulfhydryl groups of proteins and ring nitrogen atoms of purine bases.
glutaraldehyde
less irritating and more effective than formaldehyde
one of the few chemical disinfectants that is a sterilizing agent
a 2% solution of glutaraldehyde (Cidex)
bactericidal, tuberculocidal, and viricidal in 10 minutes
sporicidal in 3 to 10 hours
commonly used to disinfect hospital instruments
also used in mortuaries for embalming
gaseous sterilizers
chemicals that sterilize in a chamber similar to an autoclave
denatures proteins by replacing functional groups with alkyl groups
ethylene oxide
kills all microbes and endospores, but requires exposure of 4-18 hours
toxic and explosive in pure form
highly penetrating
most hospitals have ethylene oxide chambers to sterilize mattresses and large equipment
peroxygens (oxidizing agents)
oxidize cellular components of treated microbes
disrupts membranes and proteins
ozone
used along with chlorine to disinfect water
helps neutralize unpleasant tastes and odors
more effective killing agent than chlorine, but less stable and more expensive
highly reactive form of oxygen
made by exposing oxygen to electricity or UV light
hydrogen peroxide
used as an antiseptic
not good for open wounds because it can be quickly broken down by catalase that is present in human cells
effective in disinfection or inanimate objects
sporicidal at higher temperatures
used by the food industry and to disinfect contact lenses
benzoyl peroxide
used in acne medications
paracetic acid
one of the most effective liquid sporicides available
sterilant:
kills bacteria and fungi in less than 5 minutes
kills endospores and viruses within 30 minutes
used widely in disinfection of food and medical instruments because it does not leave toxic residues
microbiome or normal flora
microorganisms that are frequently found in a particular site in a normal, healthy individual
some are found in association with humans/animals only. majority are bacteria
symbolic relationship with the host
subject to constant changes
altered by antimicrobial agents
types of normal flora
commensals
residents
transients
carrier state
commensals
natural relationship with the host
residents
present for invariable periods
transients
establish itself briefly, excluded by host defenses or competition from residents
carrier state
potentially pathogenic
examples:
Streptococcus pneumoniae
Neisseria meningitidis in the throat of a healthy individual
origin of normal flors
newborn sterile in utero
after birth, exposed to flora of mother’s genital tract, skin, respiratory tract flora of those handling them, and organisms in the environment
beneficial effects of normal flora
immunostimulation = antibody development
exclusionary effect (vacuum effect) = protection from external invaders
production of essential nutrients = vitamin K and B by some normal intestinal flora
example: E.coli
immunostimulation
The gut microbiota (commensals) profoundly affects the host immune system and is a critical area of scientific and clinical importance. It is now evident that the gut flora influences autoimmune diseases both inside and outside the gut , where environmental factors like antibiotic overuse can increase the risk of these diseases through microbiota-mediated immunomodulation.
normal flora - may be a source of opportunistic infections
In patients with impaired defense mechanisms. eg Staphylococcus epidermidis, Escherichia coli
normal flora - some may cross react with normal tissue components
antibodies to various ABO group arise because of cross reaction between intestinal flora and the antigens of A &B blood substances.
normal flora - production of carcinogens
Some normal flora may modify through their enzymes chemicals in our diets into carcinogens.
example: artificial sweeteners may be enzymatically modified into bladder carcinogens
distribution of normal flora
internal organs (except alimentary tract) are sterile at health
local maintained by:
local defense mechanisms
chemical substances in serum and tissues
example: complement antibodies
phagocytic activity or polymorphmonomnucleocytes (PMN)
areas of the body with normal flors
GIT: mouth and large colon
urogenital tract = vagina, distal 1/3 of the urethra
skin
distribution and frequency of bacteria in the intestine
