Microcytic Hypochromic Anemias
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
Anemias associated with iron and heme
impaired production=
- lack of raw materials
- iron limiting factor= inflammation
- low protoporphyrin
Causes of Iron Deficiency
- diet
- pregnancy/growing
- chronic blood loss
- impaired absorption
Stages of iron deficiency
- Storage Iron depletion
- Transport Iron Depletion
- Functional Iron Depletion
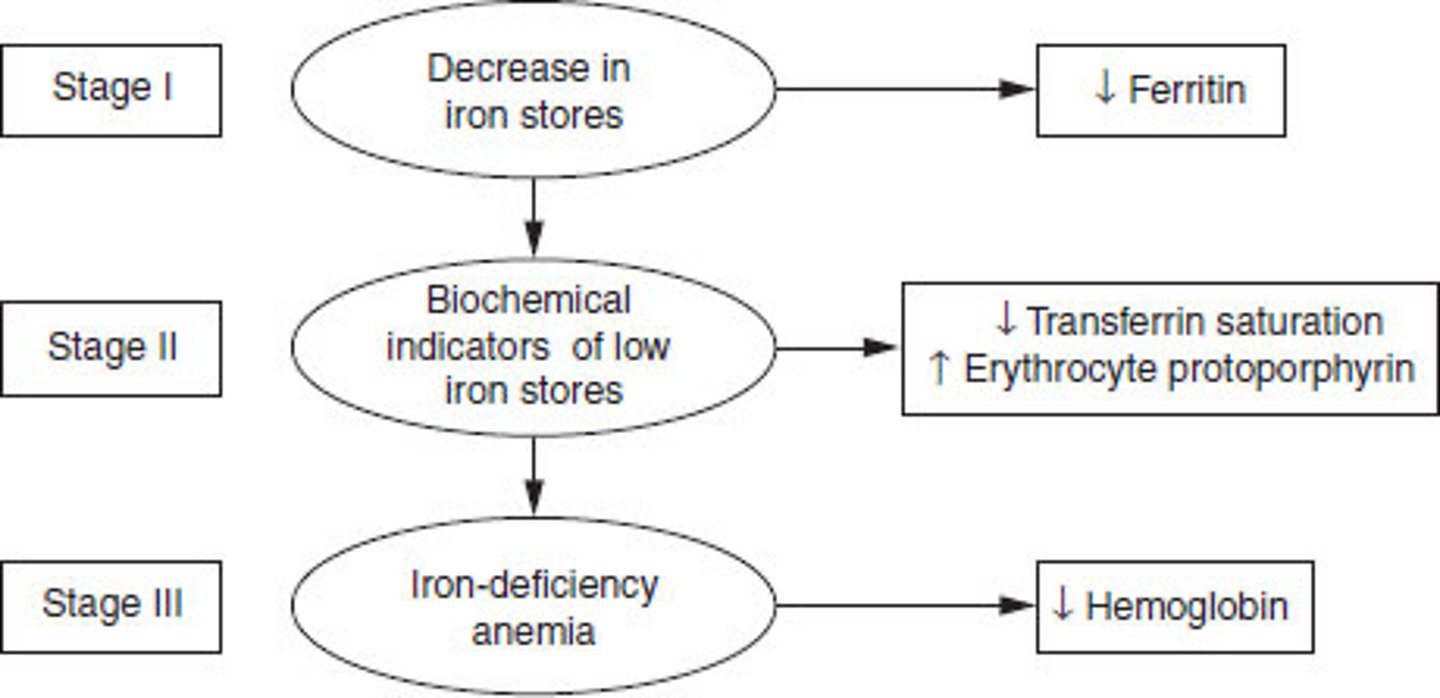
Stage I: Iron Depletion
- iron stores mobilized
- Ferritin decrease
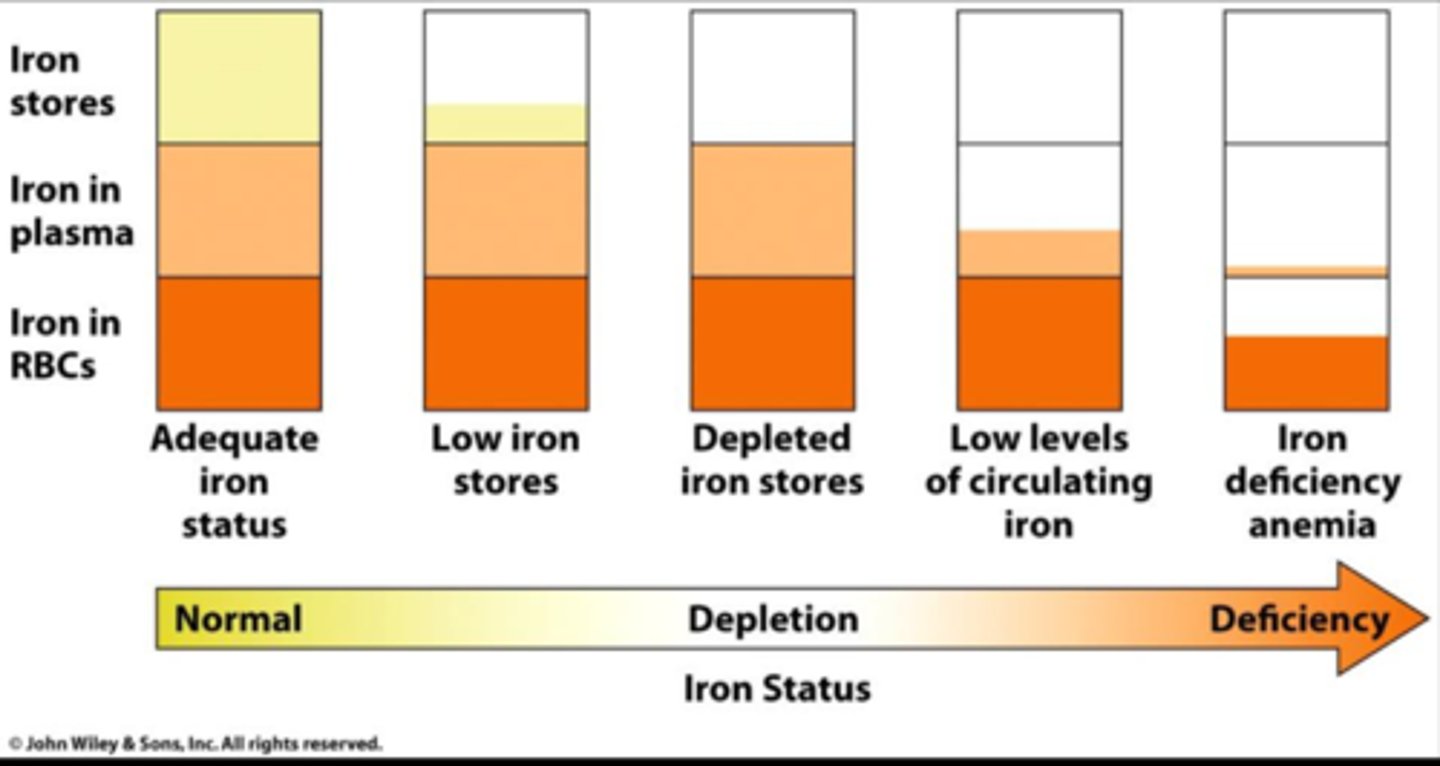
Stage II: Iron Deficient Erythropoiesis
- no iron storage pools
- hgb falls
- serum Fe= low
- Ferritin= low
- % trasnferrin saturation= low
- transferrin= high
- sTfR high
- ZPP build up
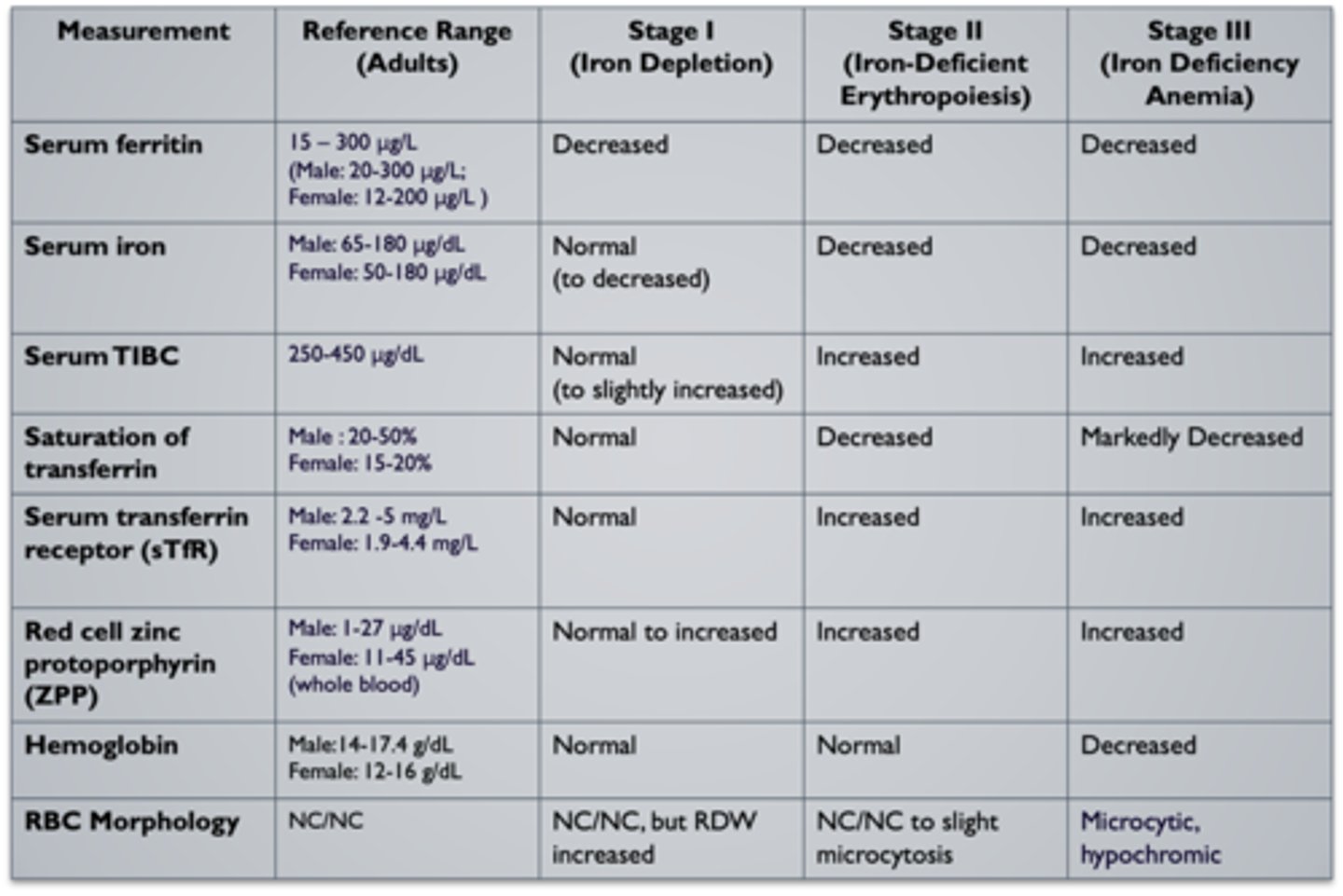
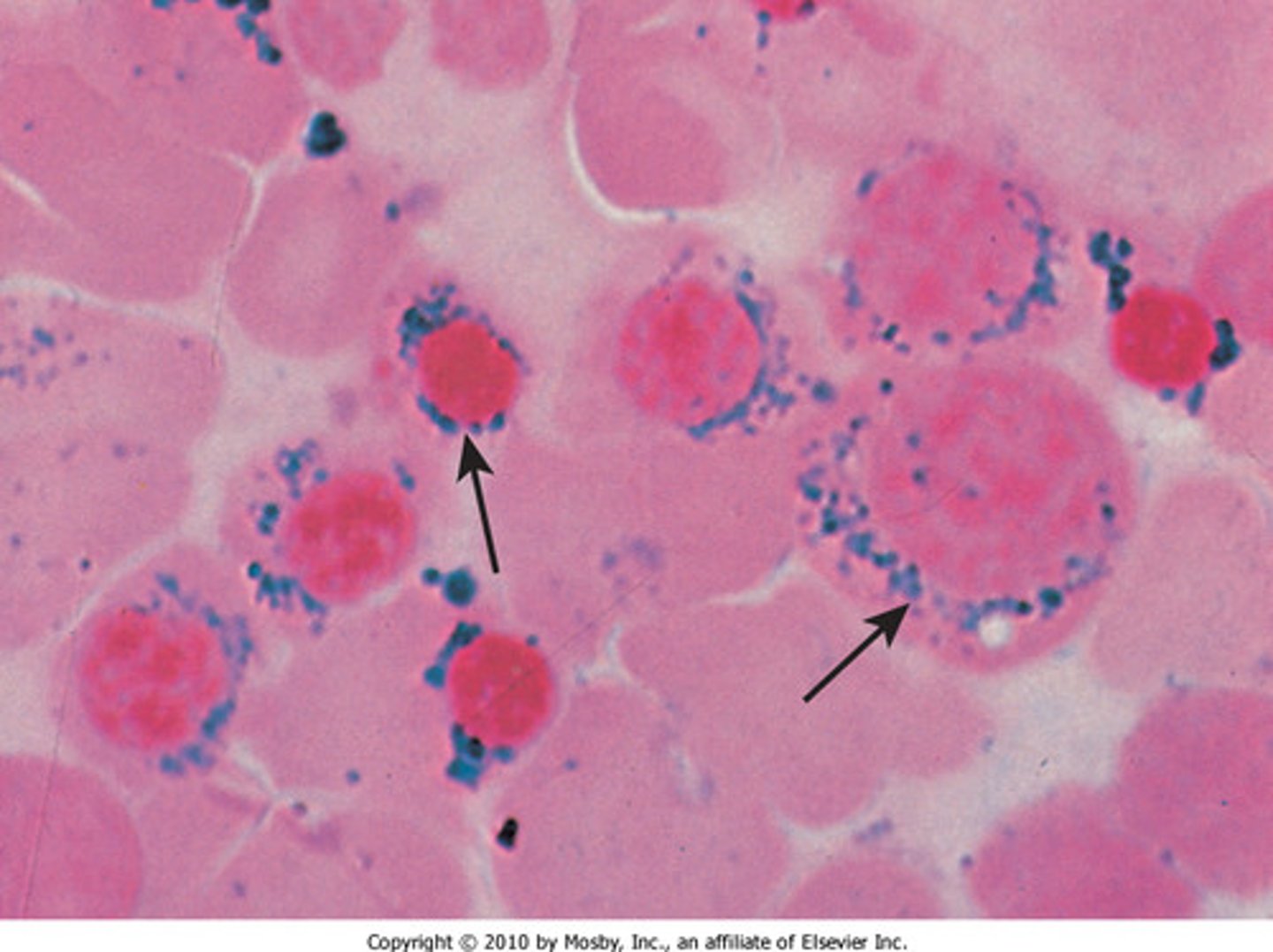
Stage III: Iron Deficiency Anemia
Microcytic, hypochromic RBCs
- hgb <10 mg/dL
- high RDW
- reticuloytes

Koilonychia
spoon nails
- with IDA

Glossitis
smooth tongue
- IDA

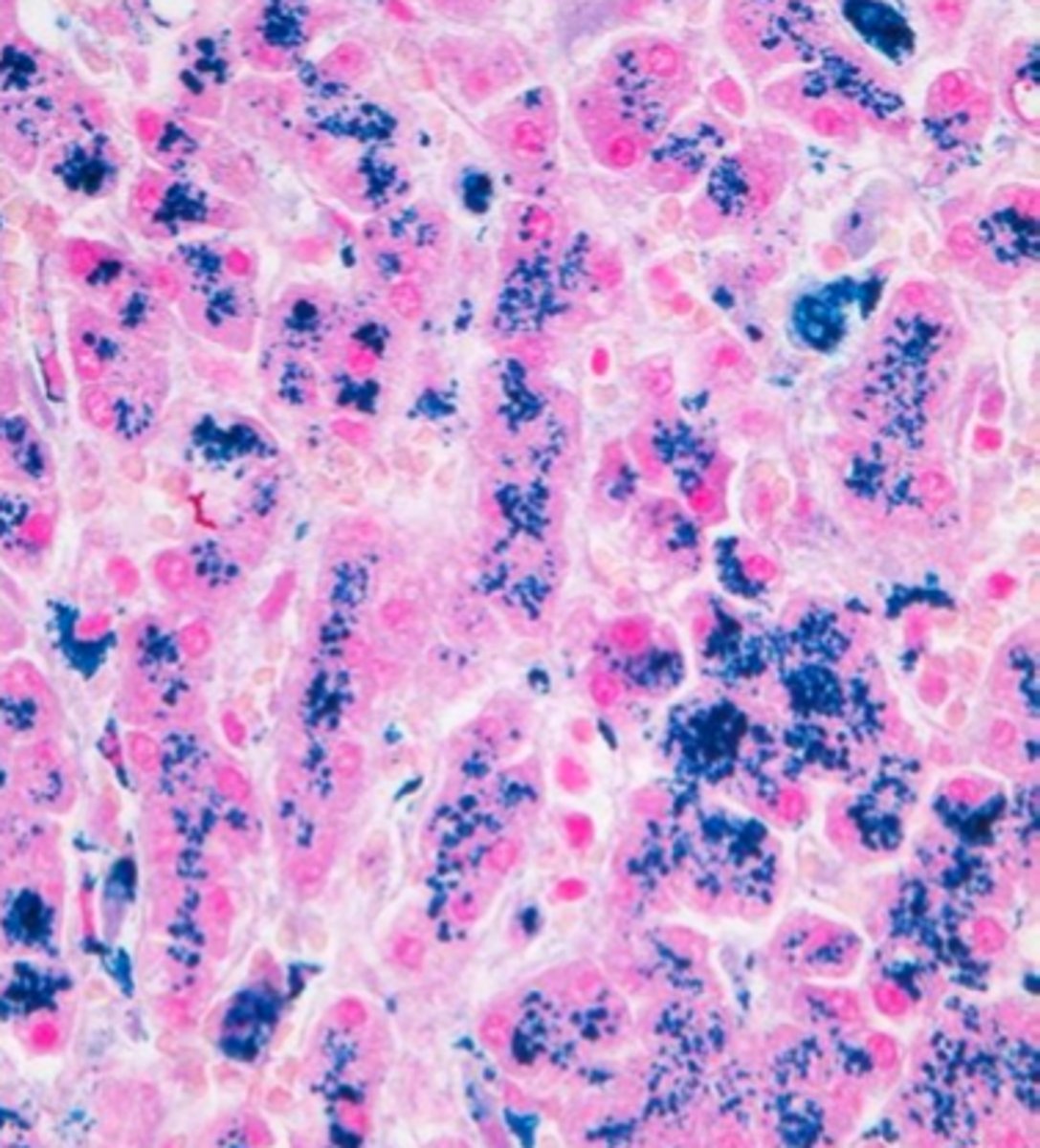
Anemia of Chronic Inflammation
Impaired iron mobilization because of chronic inflammation= iron restricted
ACI associated with
- autoimmune= RA, SLE
- infection
- neoplasms
ACI Due to:
1. Impaired ferrokinetics
2. Diminished erythropoiesis
3. shortened rbc life span
ACI lab values
- Decreased TIBC (trasnferrin)
- increased serum ferritin
- increased iron in BM macrophages
Hepcidin
acute phase reactant during inflammation
- regardless of iron levels
Inflammation
- decrease in iron absorption in GI
- increased iron retention in macrophages and hepatocytes
Lactoferrin
Iron binding protein in the granules of neutrophil
- higher avidity for iron than transferrin
Bone Marrow
iron in macrophages but not in erythroblasts
Diminished erythropoiesis
- cytokines= active T cells and macrophages
- erythroid progenitor cells ignore EPO
- EPO decreased by liver
Shortened RBC life span
Impaired ferrokinetics
- not clear
ACI diagnosis
- hgb 9-11 g/dL
- reticulocytes decreased
- inflammation= leukocytosis
ACI iron studies
- Serum iron and TIBC - decreased
- % transferrin saturation - normal or low
- Ferritin - normal to increased*
- ZPP (FEP) - increased
- sTfR - normal
- BM iron= increased
Sideroblastic Anemia type
Interference of Protoporphyrin Production
Sideroblastic anemia characteristics
- Unable to make heme
· Microcytic/ Hypochromic anemia
- iron overload
- Increased ring sideroblasts in BM
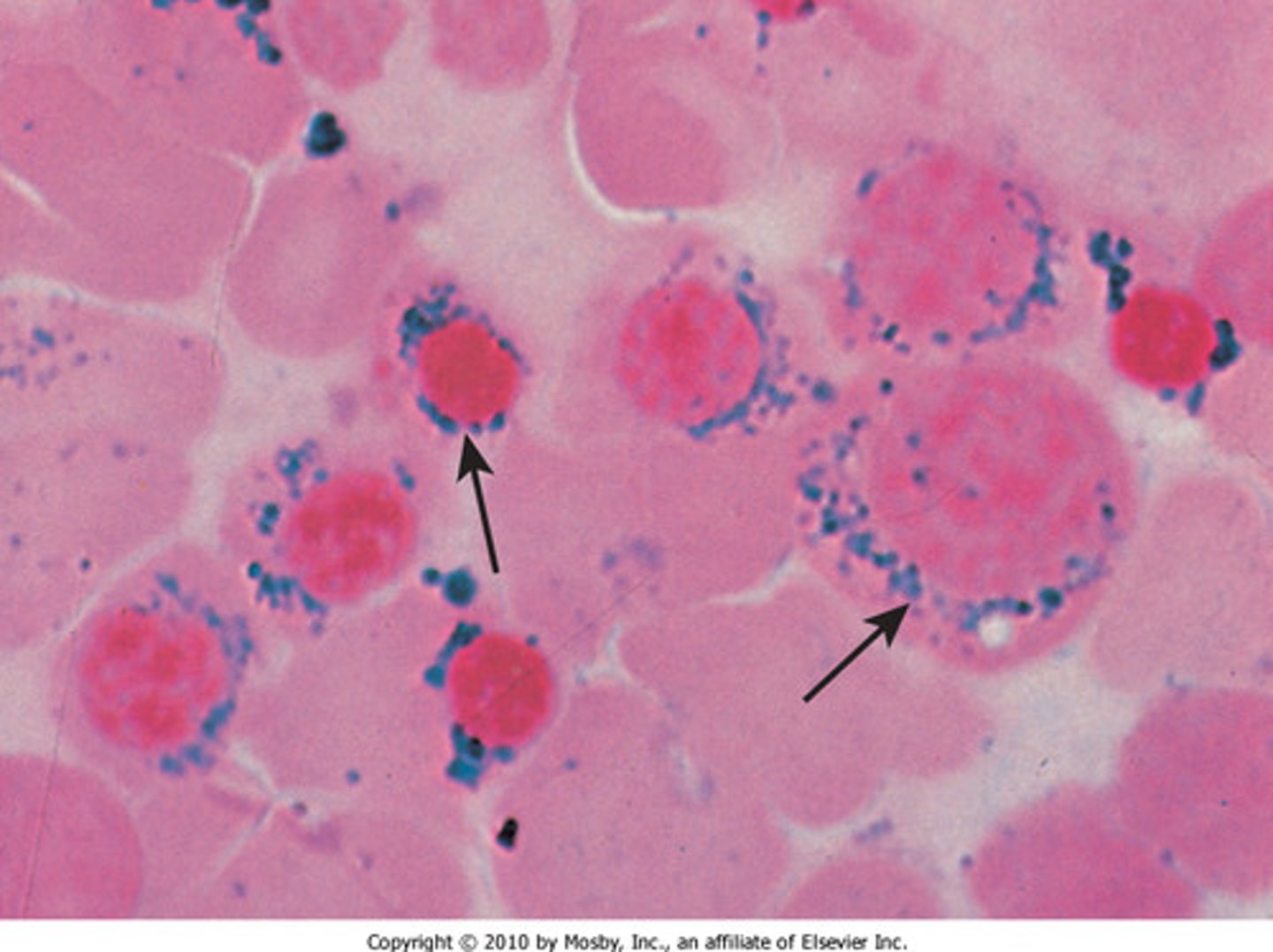
Acquired Sideroblastic
- primary= refractory
- secondary= drugs, lead, chemo
Sideroblastic CBC
- dimorphic RBCs= high RDW
- increased platelets
- pappenheimer bodies and basophillic stipplings**
Sideroblastic Iron study
- Ferritin - increased
- Serum iron - increased
- % transferrin saturation - increased
- TIBC - decreased to normal
- sTfR - normal or decreased
Sideroblastic Bone Marrow
- Erythroid hyperplasia
- increased iron in mitochondria= ringed sideroblasts
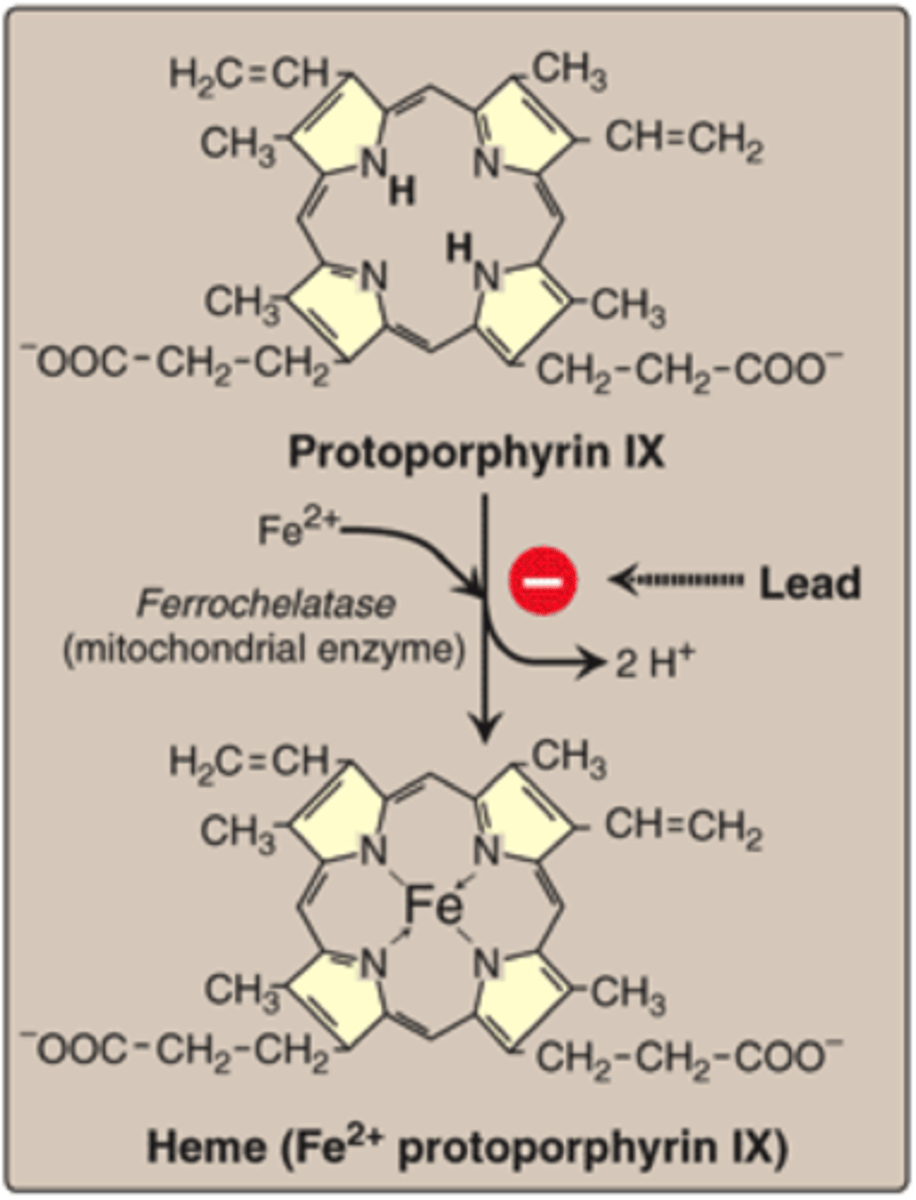
Lead poisoning
- Plubism
- interferes with 6 enzymes in porphyrin synthesis
ALA dyhydratase (PBG synthase)
- bad conversion of ALA to porphobilinogen (PBG)
- ALA in urine
ferrochelatase (heme synthase)
- incorporation of iron into protoporphyrin IX
- iron and protoporphyrin in mitochondria
- FEP or ZPP in RBCs
Lead RBC changes
- shortened survival
- basophilic stipplings= Lead inhibits pyrimidine 5'-nucleotidase= bad breakdown of RNA
- FEP accumulation
ALcoholism anemias
- Iron deficient= blood loss
- Sideroblastic= Toxic to enzymes for heme synthesis
- Megaloblastic= bad folate metabolism
Porphyria
Impair production of protoporphyrin
- Enzymes in heme synthesis is missing= byproducts accumulate
- fluorescent
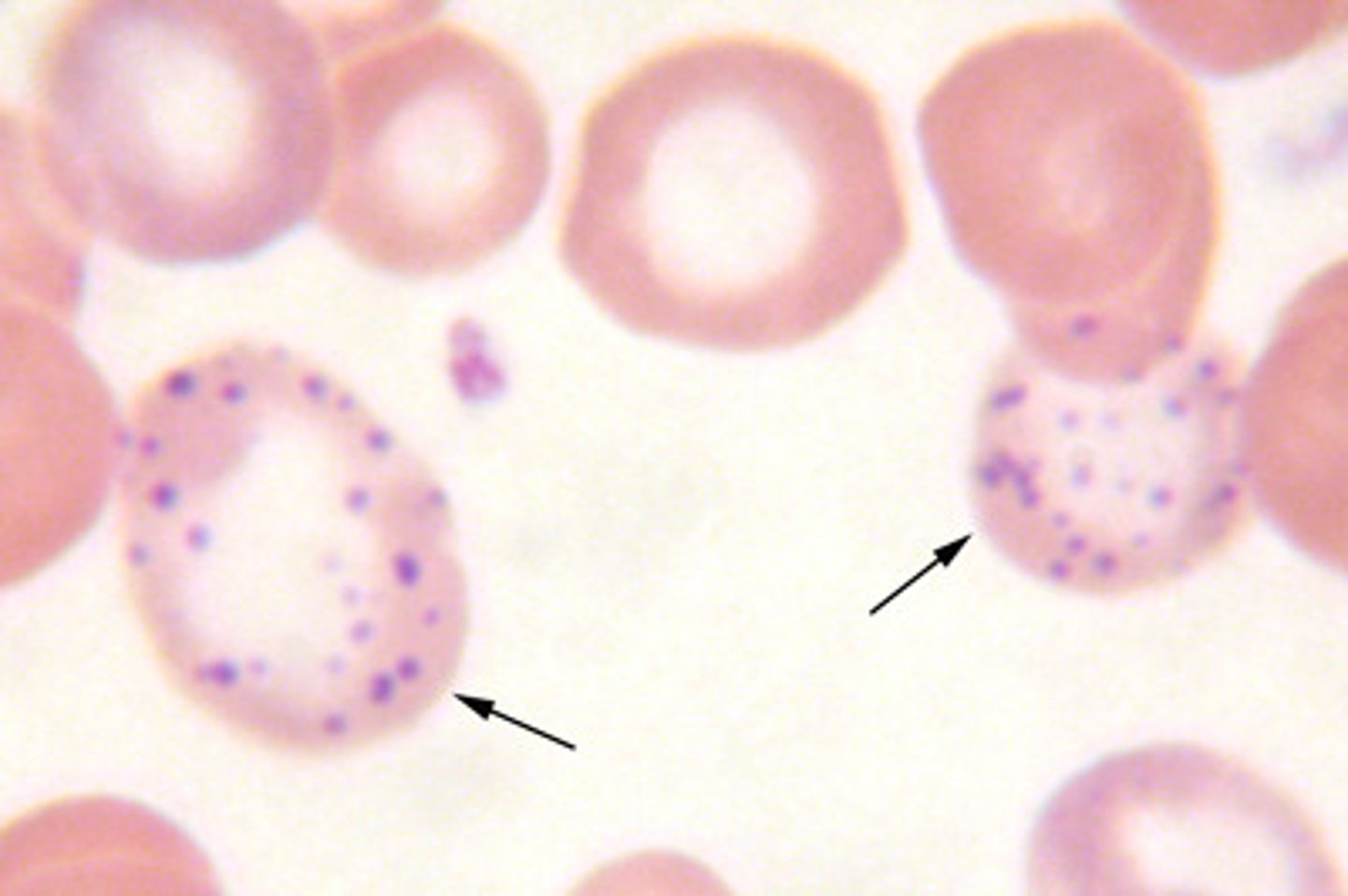
Hemochromatosis
iron overload
- bronze diabetes
- iron accumulates in pancreas, liver, and spleen
- treatment= therapeutic phlebotomoies
Hereditary Hemochromatosis
- increased ferritin, serum iron, % transferrin saturation (> 50%)
- normal to decreased TIBC
Hemosiderosis
Accumulation of excessive iron in macrophages
- treatment= iron-chelating drugs