E8- Disorders of calcium metabolism
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
describe calcium homeostasis
- very stable in the extracellular space
- input: gut
- excretion: kidney
- storage: bone
what are the fractions of serum calcium
- bound to proteins: albumin, globulins (47%)
- ultrafiltrable: ionised, complex bound (53%)
- serum level correction always happens through the ionised fraction (active)
which systems are affected by hypercalcaemia syndrome?
- CV
- GI
- renal
- neurological
- general
What are the CV symptoms of hypercalcemia syndrome
- hypertension
- bradycardia, I. AV block
- extrasystole, ventricular tachycardia
What are the GI symptoms of hypercalcemia syndrome
- loss of appetite
- nausea, vomiting
- constipation
- polydipsia
- rarely: acute pancreatitis
What are the renal symptoms of hypercalcemia syndrome
- polyuria due to hypercalciuria
- renal stones
What are the neurological symptoms of hypercalcemia syndrome
- decreased concentration
- anxiety, confusion
- personality disturbances
- depression
- somnolence, coma
What are the general symptoms of hypercalcemia syndrome
- muscle weakness
- exsiccosis
what are frequent causes of hypercalcaemia
1) primary/tertiary hyperparathyroidism
2) malignancies
ectopic PTH production (rare)
ectopic PTHrP production (common)
osteoclast activation
direct osteolysis
ectopic calcitriol production
which tumours produce PTHrP?
- lung
- kidney
- ovarium
- bladder
which tumours produce calcitriol?
- granulomatous tumours
- lymphomas, Hodgkin disease
What cancers cause local stimulation of bone resorption by tumour
Myeloma multiplex
Breast
What cancer causes direct osteolysis
Bone metastasis
what are less frequent causes of hypercalcaemia
granulomatous
sarcoidosis
drugs:
vit D and derivatives
thiazide diuretics
endocrine: thyrotoxicosis
immobilisation, long term parenteral feeding
what are symptoms of hypercalcaemia
- vast range
- fatigue, weakness
- poor appetite
- polyuria, exsiccosis
- constipation
- QT shortening
what are treatment methods of hypercalcaemia
General
solve underlying cause!
low calcium diet
avoid drugs known to increase serum calcium
stimulate urinary calcium excretion:
fluid and electrolyte substitution
salt diuresis
furosemide
dialysis
what is the treatment order of hypercalcaemic patient
1) fluids as these patients are usually dehydrated from polyuria
2) FSD
3) bisphosphonates (in good kidney function)/denosumab/corticosteroids (in haematological disease)
how do you inhibit of bone resorption
treatment of underlying disease
/+
mobilisation
calcitonin (fast acting so first few days)
antiresorptives:
bisphosphonates- clodronate, zoledronate
anti-RANKL (slow!)- denosumab
glucocorticoids (in calcitriol excess)
Describe primary hyperparathyroidism
autonomous hyper function → hypercalcemia
Primary hyperplasia of all parathyroid gland
In young age, as a part of multiple endocrine adenomatosis, rare
Autonomous tumour in one or more parathyroid gland
Adenoma, carcinoma- very rare
Describe secondary hyperparathyroidism
regulatory hyperfunction= compensatory process against hypocalcmia of any reason- always hyperplasia
Normocalcemia
Chronic renal failure
Malabsorption
Renal hypercalciuria
Describe tertiary hyperparathyroidism
in long term secondary hyperparathyroidism the regulatory hyperfunction can be transformed to an autonomous process
Resulting even more PTH production
Mostly adenoma or microadenoma
what are clinical symptoms of primary hyperparathyroidism
- osteopenia, osteoporosis
- bone pain, increased fragility
what are typical X-ray findings of primary hyperparathyroidism
cysts in long bones
Osteolysis
What is the renal form of hyperparathyroidism
calcium oxalate stone production in the urinary tract
Clinical manifestations
Recurrent and bilateral calcium stones in the kidney
Nephrocalcinosis
Idiopathic microhaematuria (in children)
What is the GI form of hyperparathyroidism
GI symptoms due to hypercalcaemia itself
Rarely
Peptic ulcer, acute pancreatitis
What is the neurogenic/ psychiatric forms of hyperparathyroidism
hypertension
Neuropathy, polyneuritis
Anxiety, depression
What is the dominant- asymptomatic form of hyperparathyroidism
“Chemical HPT” or “subtle HPT”
No clinical symptoms
No pathological findings on X ray
Only moderate hypercalcemia
Serum Ca 2.6-2.85mmol/l
Increased risk of CV and cognitive diseases
what is the localisation of parathyroid adenoma
- neck and thyroid US
- parathyroid scintigraphy
- neck and mediastinum CT
what are the indications for surgery in primary HPT
renal complications
Stones, calcinosis, decreasing GFR
low bone mass, fragility fractures
Or progression in the bone and kidney problems
serum calcium > 2.85mmol
suspicion of thyroid cancer
patient <50yrs
what to do if primary HPT patient is not eligible for surgery?
Prevention of bone loss
oestradiol
bisphosphonate
- calcimimetics
*all moderate and transient, and don't affect kidney stones
what are the complications of parathyroid surgery
transient complications:
post op hypocalcaemia
recalcification tetany
atrophy of remaining glands
hungry bone syndrome
long-term:
final hypoparathyroidism
hypothyroidism
vocal cord injury
what is hungry bone syndrome?
- prolonged hypocalcaemia after successful parathyroidectomy
- due to rapid calcium influx into the bones
describe secondary hyperparathyroidism
- compensation of hypocalcaemia of any reason
- e.g. chronic renal failure
- malabsorption
- renal hypercalciuria
describe tertiary hyperparathyroidism
- long term secondary hyperparathyroidism: regulatory function is converted into autonomous hyperfunction
- usually due to adenoma/microadenoma
Wha are
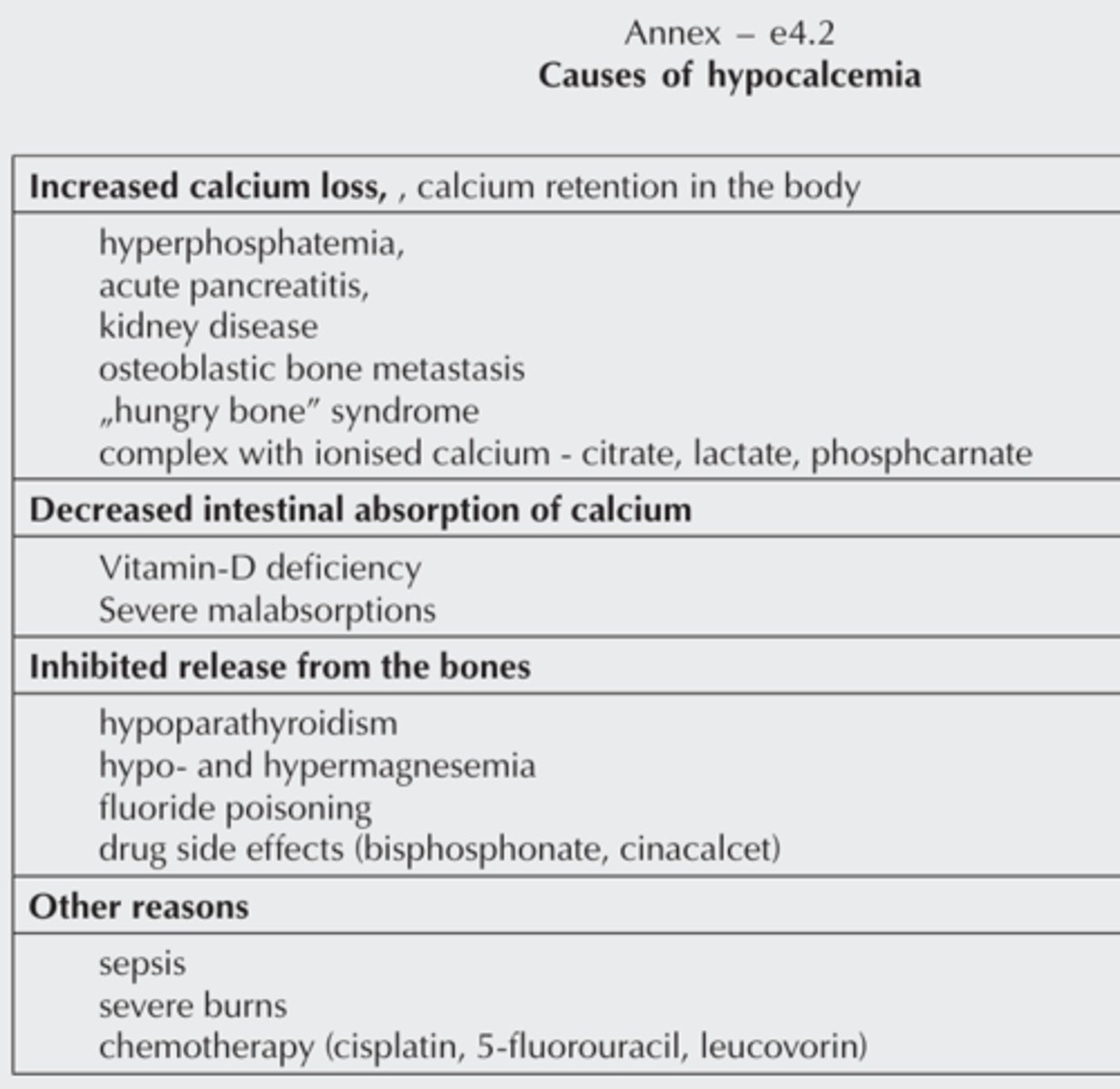
what are the causes of hypocalcaemia
- increased renal calcium loss
- decreased absorption (vit D deficiency)
- inhibited release from bone (hypoparathyroidism, hungry bone, osteoblastic metastasis)
- acute pancreatitis, large amounts of IV lactate/citrate
what are the symptoms of hypocalcaemia
- typical:
- myopathy, muscle spasm, twitches
- tetaniform seizures
- emotional instability
- prolonged QT: sudden cardiac arrhythmias
describe hyperventilation caused "hypocalcaemia"
- hyperventilation:
-> respiratory alkalosis
-> H+ dissociation from albumin
-> Ca2+ association to albumin, decreased [ionised Ca2+]
- do not treat with Ca2+! resolve underlying psychiatric/respiratory issue
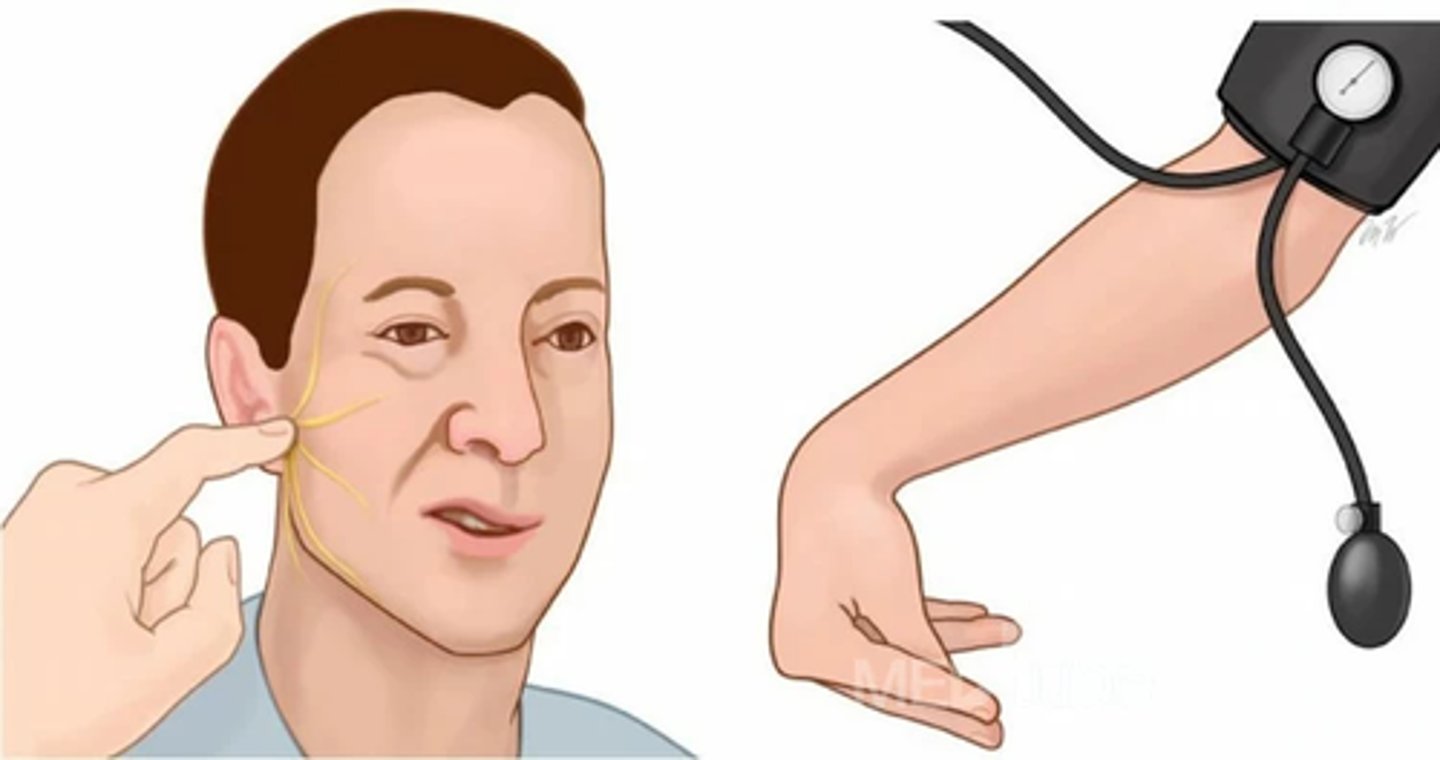
what are the ways to identify hypocalcaemia
Chvostek: tapping face
Trousseau: hand sign with inflated cuff
*if patient is Chvostek positive, you never do Trousseau because it can produce generalised tetany
what are the lab values of hypocalcaemia
albumin-adjusted Ca2+ is <2.25mmol/L
what is the treatment of hypocalcemia
- eliminate underlying cause
- treatment of hypoparathyroidism
- oral calcium supplementation
- Vit D and magnesium supplementation
why is osteoporosis significant as a medical issue?
-> fractures
-> surgery
-> pain, risks
-> expensive
-> immobilisation
-> imminent fracture
-> death
in Europe: 10 fractures per minute
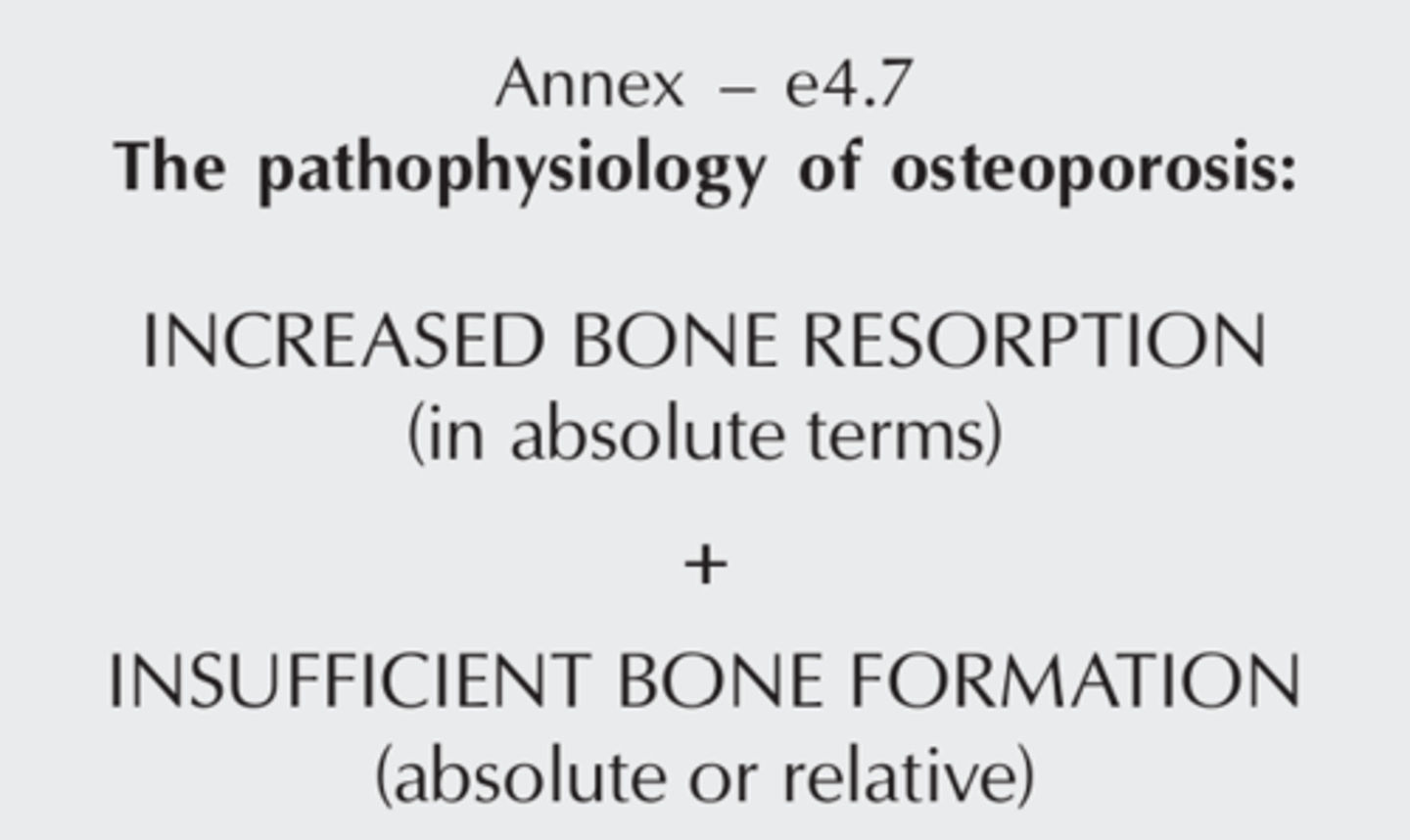
define osteoporosis
- generalised disease of the skeleton characterised by a progressive bone loss and deterioration of microstructure, followed by increased bone fragility
- i.e. even minor trauma can cause bone fractures
most common fractures in osteoporosis
- hip
- femur
- humerus
- vertebrae
What are the typical findings of osteoporosis
typical physcial findings = late iagnosis
no early symptoms, clincal signs
after years → fractures by small injury= low trauma fractures
Why do fractures occur
power effect- falling
+
mechnical competence decreases
loss of bone mass
loss of microstructure
decrease in bone quality
lab alterations in osteoporosis
none, especially in the early phases, no early symptoms
physical status of advanced osteoporosis
- shorter spine: cervical kyphosis, lumbar lordosis
- belly falls forward
- porotic leatherwood
- Christmas tree sign

possible clinical complaints in osteoporosis
- chronic musculoskeletal pain
- increasing spine curvature
- progressive loss of height
- fractures in minor trauma/fractures not explained by other causes
- abdominal complaints not explained by other causes
- muscle weakness, kidney stones
immobilisation related diseases
- venous thrombosis
- pulmonary embolism
- pneumonia
- decubitus
what is imminent fracture?
- refracture after first fracture
- there is a significant risk for this in the first two years
- influenced by site of fracture (e.g. hip has higher risk)
What are the risk factors for osteoporotic fractures
age
BMD
other
low body mass
previous low trauma fracture
porotic fracture of parents
smoking
long term steroid treatment
alcohol
rheumatoid arthritis
rate of bone loss
- bone mass peaks at age 25-30
- starts decreasing after menopause/age50-60 in men
- women have two phases of bone loss: rapid (menopause related) and slower (age-related)
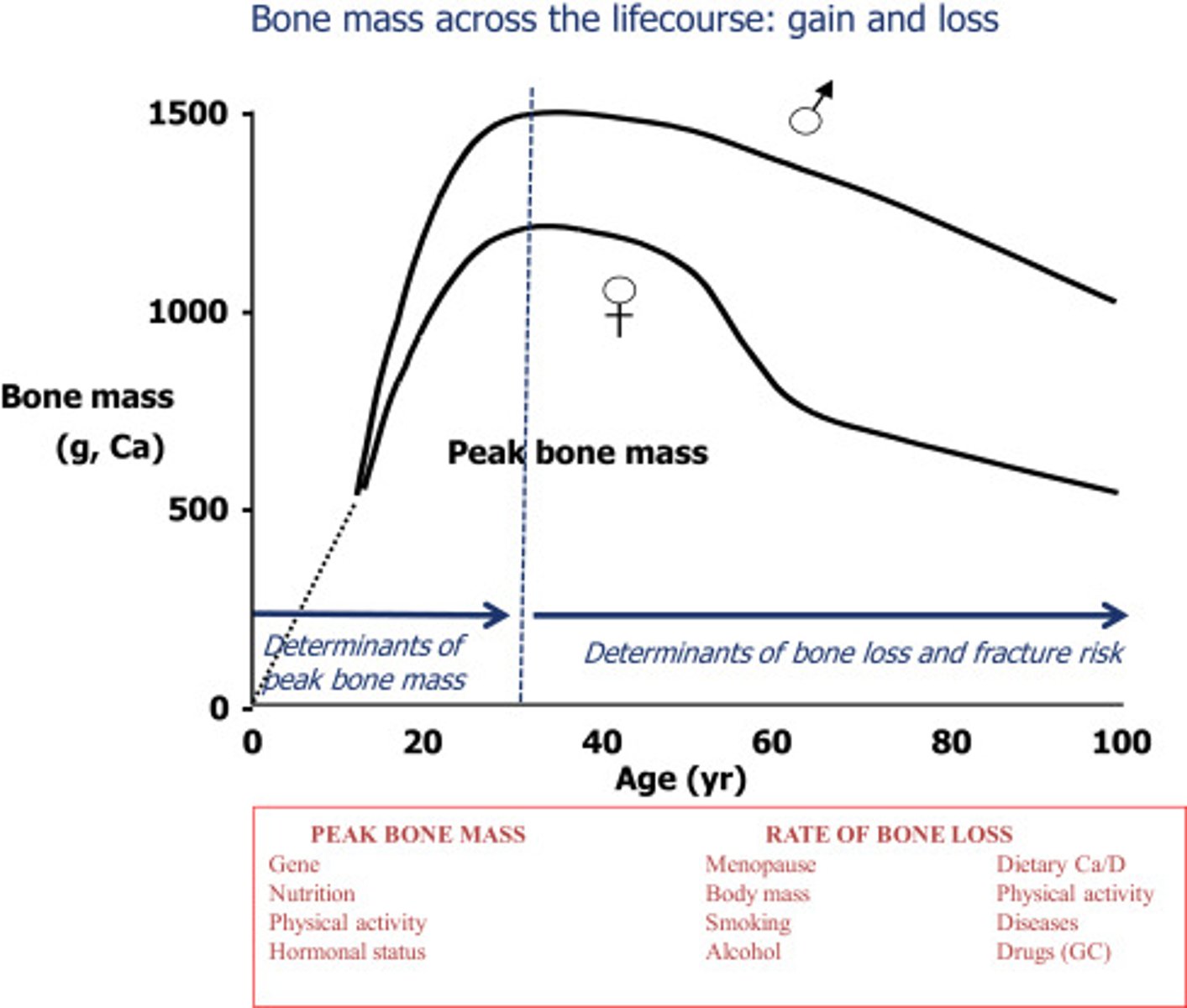
factors contributing to osteoporosis other than hormonal changes
- hypomobility in society
- decreased Vit D and calcium intake
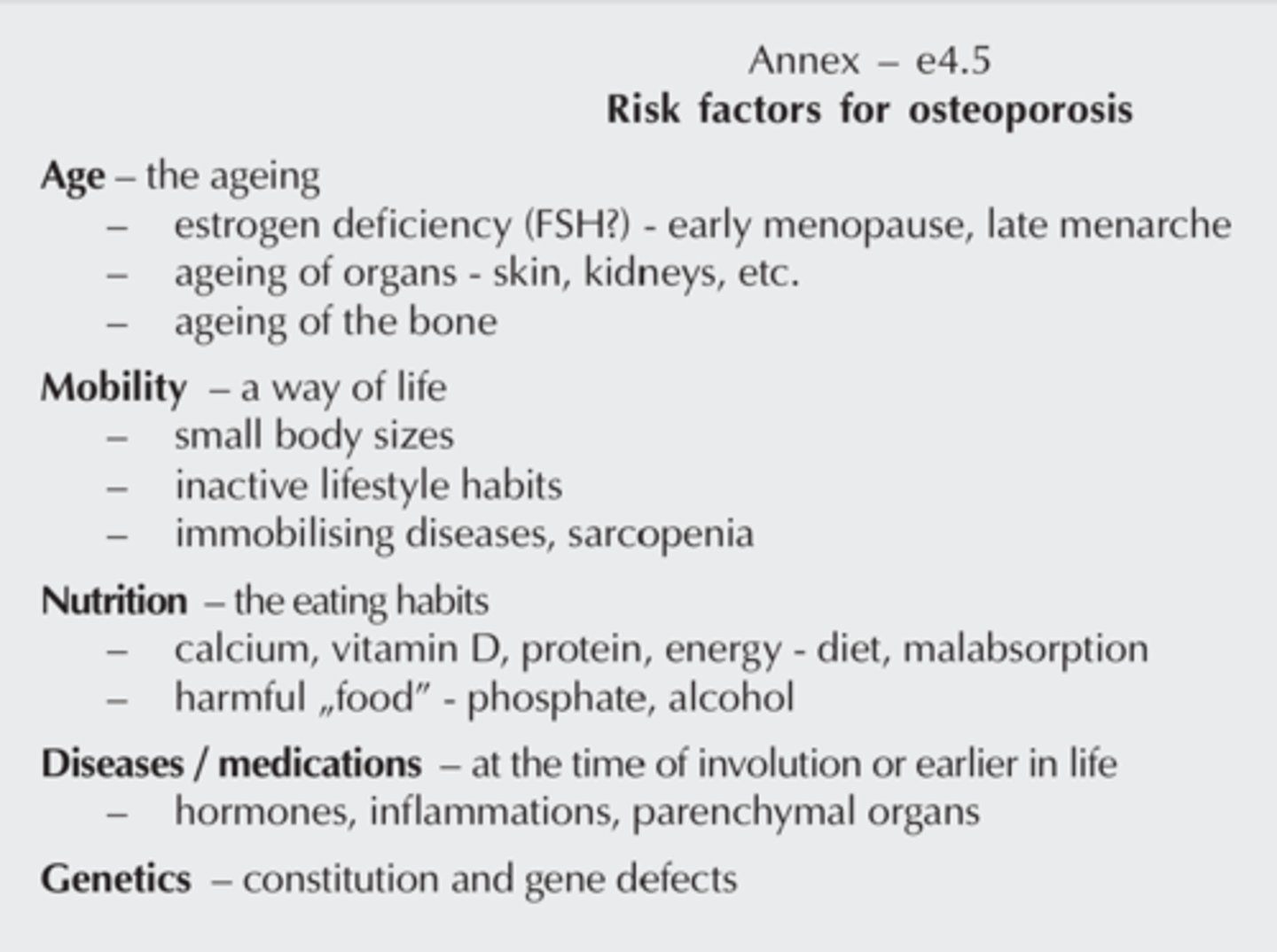
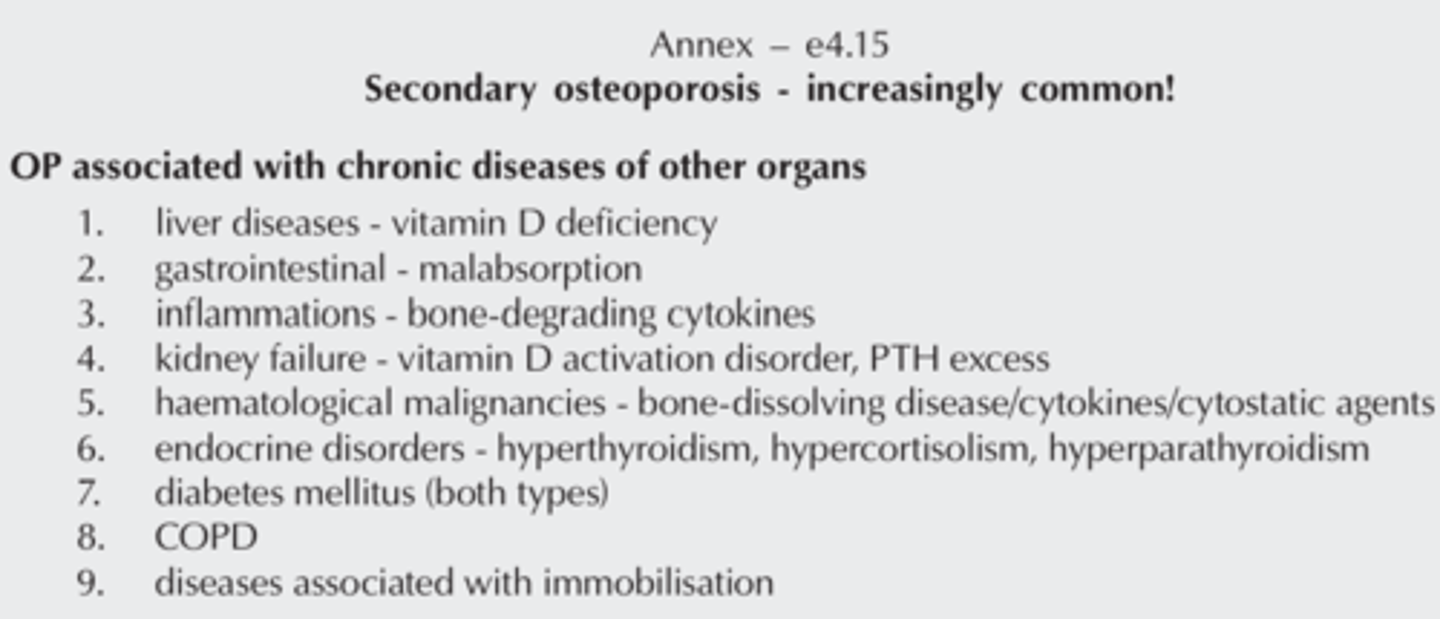
diseases that can accelerate osteoporosis ("secondary osteoporosis")
OP in diseases of other organs
liver- D deficiency
GI- malabsorption
inflammatory- bone resorbing cytokines
renal insufficiency- D activation, PTH excess
haematologic malignancies- bone resorbing disease, cytokines, cytostatics
immobilisation
endocrine- more thyroxine, steroire, less sex hormones
What is the treatment for preventing osteoporotic fractures
inhibit bone resorption
estradiol
bisphosphonates- alendronate, zolendronate
denosumab- RANK ligand antibody
stimulating bone formation
PTH analogues
Basis therapy
calcium and vitamin D supplements
What are the methods to measure bone mass
radiologic
X ray
radiogrammetry
Photon absorption- bone densitometry- ODM
radiographic absorptiometry
single or dual photon absorptiometry
quantitative CT
What is the use of measuring bone mass
photon absorption (osteo)densitometry
- can calculate bone mineral density
- can calculate fracture risk over the next decade
scoring of bone mass density (DEXA)
Z score
- compared to healthy individuals of same sex and age
- bewteen +2 and -2
- less than -2.5: osteoporosis
T score
- compared to healthy individuals age 30 and same sex
Normal
T score > -1
osteopenia
T score between -1 + -2.5
osteoporosis
T score < -2.5
What is the differential diagnosis of calcipenic osteopathies

who do we need to screen for osteoporosis?
- post-menopausal women
- men over 65
- family history of osteoporosis
- exogenous glucocorticoid treated patients/Cushing patients
- people with pathological fractures
drugs accelerating osteoporosis
- glucocorticoids
- anti-oestrogen therapies (breast tumours)
- anti-androgens (prostate carcinoma)
Describe bisphosphonate treatment
increases bone density
by 50-60% reduces rate of new fractures
PO daily/ weekly/ monthly or IV 4x/year
PO side effect- erosion/ ulcer in stomach/ oesophagus
rare- aseptic osteonecrosis in jaw
Describe denosumab treatment
IM injection
similar or more expressed cortcial bone
SE- infection, jaw osteonecrosis
describe PTH treatment in osteoporosis
Teriparatid
dramatic + quick increases spine density
reduces 70% of fractures
less effective in peripheral bone- small increase in density + smaller decrease in fracture rate
few SE- hypercalcemia, hypercalciuria, vertigo
limited to 18 month treatment