Ch.18 Neurological Emergencies
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
39 Terms
seizures may occur as a result of:
recent or prior head injury
brain tumor
metabolic problems
fever
a genetic disposition
possible causes of altered mental status:
intoxication
head injury
hypoxia
stroke
metabolic disturbances
brainstem
controls breathing, BP, swallowing, and pupil constriction
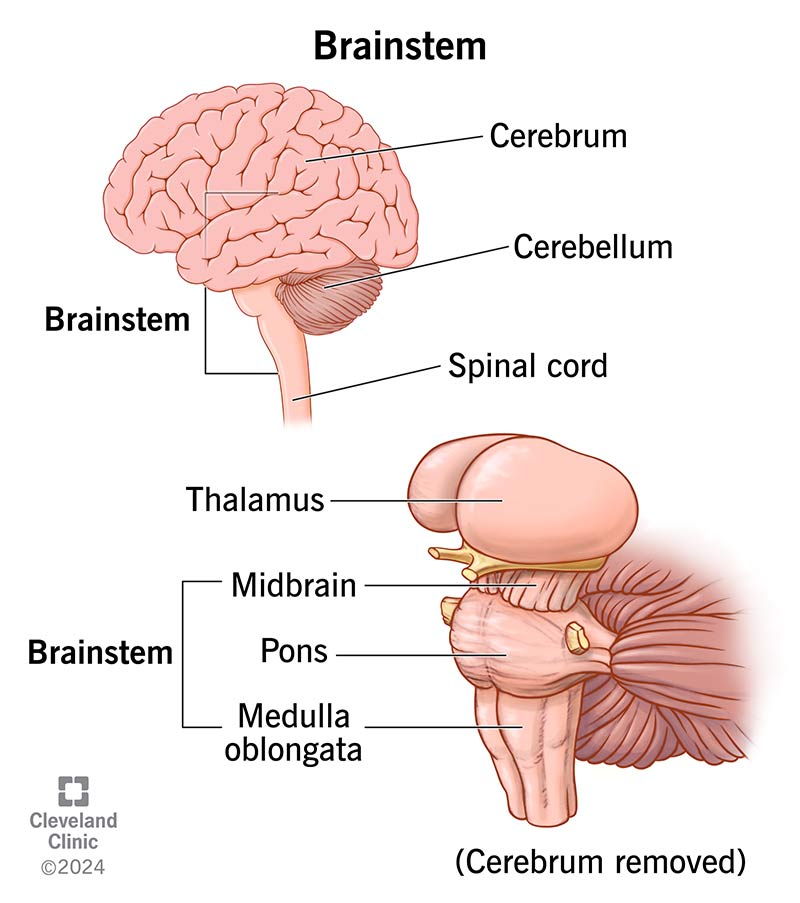
cerebellum
controls muscle and body coordination

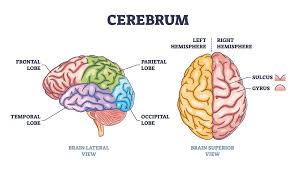
cerebrum
divided into right and left hemispheres - each controls the activities on the opposite side of the body
front - controls emotion and thought
middle - controls sensation and movement
back - processes sight
speech is usually controlled on the left side of the brain near the middle of the cerebrum
how many cranial nerves are there?
12
at each vertebra in the neck and back, ___ nerves branch out from the spinal cord and carry signals to and from the body
2
the brain is most sensitive to changes in ____, ____, and ____ levels
oxygen, glucose, and temperature
tension headache
cause: muscle contractions in the head/neck and attributed to stress
pain: usually described as squeezing, dull, or as an ache
severity: usually does not require medical attention
migraine headaches
cause: changes in the blood vessel size in the base of the brain
pain: usually describes as pounding, throbbing, and pulsating
often associated with nausea and vomiting and may be preceded by visual warning signs such as flashing lights or partial vision loss
duration: several hours to days
sinus headaches
cause: pressure that results from accumulated fluid in the sinuses
severity: prehospital care is not needed
pts may have cold-like signs and symptoms of nasal congestion, cough, and fever
serious conditions that include headache as a symptom are _____, _____, and _____
hemorrhagic stroke, brain tumors, and meningitis
stroke (cerebrovascular accident; CVA)
an interruption of blood flow to an area within the brain that results in the loss of brain function
ischemic stroke
most common
results from: thrombosis or an embolus
symptoms: may range from nothing at all to complete paralysis
cause: atherosclerosis in the blood vessels is usually the cause
hemorrhagic stroke
accounts for 13% of strokes
occurs: when a blood vessel ruptures, and the accumulated blood forms a blood clot which compresses brain tissue
often massive and fatal
high risk: people experiencing stress, exertion, pts with extremely high BP, and pts with long-term untreated hypertension
common cause: berry aneurysms in healthy, young people
aneurysm
a swelling or enlargement of the wall of an artery resulting from a defect or weakening of the arterial wall
berry aneurysms
common cause of hemorrhagic strokes in healthy, young people
presents as the “worst headache of their life”
causes a subarachnoid hemorrhage
transient ischemic attack (TIA)
symptoms: stroke-like symptoms go away on their own in < 24 hrs
may be a warning sign of a larger stroke to come
all pts should be evaluated by a physician
signs and symptoms of a stroke
facial drooping
sudden weakness or numbess in the face, arm, leg, or one side of the body
decreased or absent movement and sensation on one side of the body
lack of muscle coordination (ataxia) or loss of balance
sudden vision loss in one eye, blurred and double vision
difficulty swallowing
decreased level of responsiveness
speech disorders
aphasia
slurred speech (dysarthria)
sudden and severe headache
confusion
dizziness
weakness
combativeness
restlessness
tongue deviation
coma
stroke in the left hemisphere
may cause aphasia (inability to produce or understand speech)
can cause paralysis of the right side of the body
stroke in the right hemisphere
can cause paralysis of the left side of the body
usually, pts will understand language and be able to speak, but their words may be slurred
pts may be oblivious to their problems (neglect)
bleeding in the brain
pts may have a very high BP
significant drops may occur as the pt’s condition worsens
conditions that may mimic a stroke
hypoglycemia
postictal state
subdural or epidural bleeding
seizure
a neurological episode caused by a surge of electrical activity in the brain
generalized (tonic-clonic) seizure
cause: abnormal electrical discharges from large areas of he brain, usually involving both hemispheres
typically characterized by unconsciousness and severe twitching of all muscles that lasts several minutes or longer
absence seizure
does not involve any changes in motor activity
characterized by a brief lapse of consciousness in which the pt seems to stare and not respond
partial (focal) seizure
no change in the pt’s LOC
symptoms: numbness, weakness, dizziness, visual changes, unusual smells and tastes
may cause some twitching or brief paralysis
focal-onset, impaired-awareness seizure
pt has an altered mental status and does not interact normally with his or her environment
cause: abnormal discharges from the temporal lobe of the brain
characteristics: lip smacking, eye blinking, isolated jerking
symptoms: unpleasant smells, visual hallucinations, pts may exhibit uncontrollable fear, or perform repetitive physical behavior
status epilepticus
seizures that continues every few minutes without the person regaining consciousness or last longer than 30 minutes
causes of seizures
congenital
structural
metabolic
febrile
epileptic seizures
medications commonly used to treat seizures
Levetiracetam (Keppra)
Phenytoin (Dilantin)
Phenobarbital
Carbamazepine (Tegretol)
Valproate (Depakote)
Topiramate (Topamax)
Clonazepam (Klonopin)
postictal state
following the seizure, a pt’s muscles relax, and the breathing becomes labored
may be characterized by hemiparesis, or weakness on one side of the body
commonly characterized by lethargy and confusion
if pt’s condition does not improve, you should consider other possible underlying conditions
differences between seizures and syncope
fainting typically occurs while the pt is standing
seizures may occur in any position
fainting is not associated with a postictal state
emergencies that could present with altered mental status
hypoglycemia
hypoxemia
intoxication
delirium
drug overdose
unrecognized head injury
brain infection
body temperature abnormality
brain tumor
overdose and/or poisoning
treatment for migraine
appt high-flow oxygen
provide a darkened and quiet environment
do not use light and sirens
treatment for a stroke
support the XABCs
maintain a SpO2 level of at least 94%
routine use of oxygen is not recommended unless the pt is showing signs of respiratory distress or hypoxia
fibrinolytic therapy and other methods may reverse stroke symptoms and even stop the stroke if given within 3 - 6 hrs
if possible, transport to a designated stroke center
treatment for a seizure
continue to assess and treat the XABCs
protect the pt from harm
if pt refuses transport after seizure, contact online medical control and ask them to speak directly with the pt
treatment for altered mental status
determine the cause
provide spinal motion restriction, airway, and ventilatory support as indicated
transport to appropriate facility