rheumatoid arthritis 4/10
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
rheumatoid arthritis
chronic systemic inflammatory disease
major subclassification within the category of diffuse CT diseases
affects 1-2% of US population (1.3 mil ppl)
considered an autoimmune disease (80% are RF+)
primary risk factors of RA
30-60 year old peak onset
females
initial RA joint changes
inflamed synovium
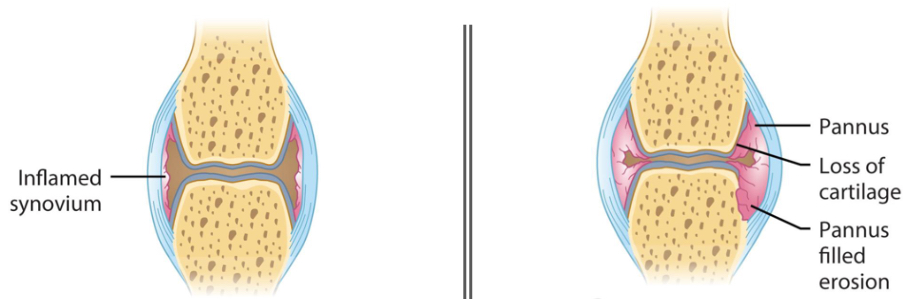
end stage RA joint changes
pannus, loss of cartilage, pannus-filled erosion
RA vs OA
initial onset can be younger or older (25-50 y/o), sudden, intermittent exacerbation & remission
affects 1% of US adults (and 30-50k children)
women affected 3x as men, more disabling and severe in men
multifactorial etiology
different clinical manifestations
has associated symptoms
synovial fluid has high WBC, low viscosity
rheumatoid factor present usually
C-reactive protein is a true indicator
age of onset
men: older than 45
women: 20-45
clinical manifestations
diffuse msk pain
fatigue, malaise, weight loss, fever
weakness
swelling/erythema
multiple joints with symmetric BIL presentation
prolonged morning stiffness lasting >1 hr
gradual loss of motion affecting gripping/holding objects
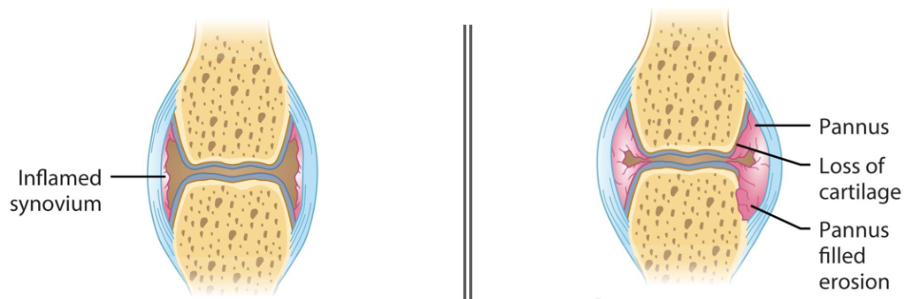
where does RA manifest?
any joint, but commonly small joints of hands and feet and C spine
inflammation is almost always present with redness, warmth, swelling
ulnar drift
RA is most common cause
leads to significant hand functional limitations
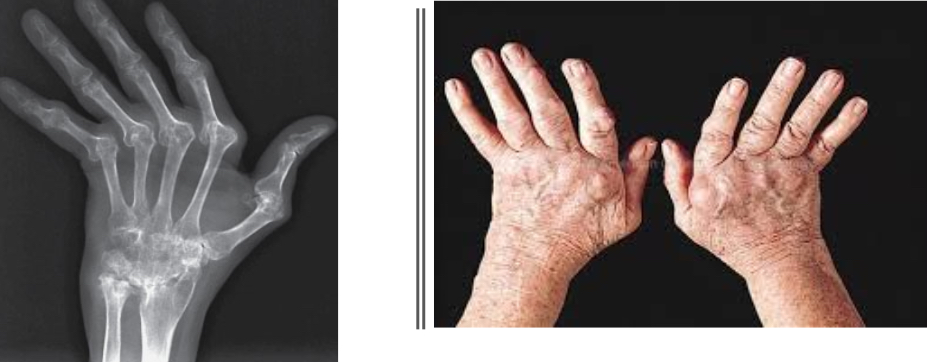
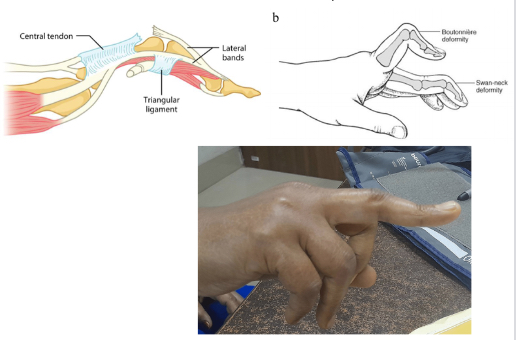
swan-neck deformity
boutonnière deformity
what systems are also affected?
heart, arteries
lungs
stomach
liver, gallbladder
goals of management
prevent/control joint damage
prevent function loss
decrease pain
decrease extra-articular manifestations of disease
poor prognosis is suggested by…
earlier age at disease onset
high titer of RF
elevated ESR
swelling of >20 joints
extra-articular manifestations (cardiopulmonary)
PREVENTATIVE medical management
new, more effective combination of drugs
behavioral interventions
education: healthy lifestyle, appropriate BW, no smoking, exercise
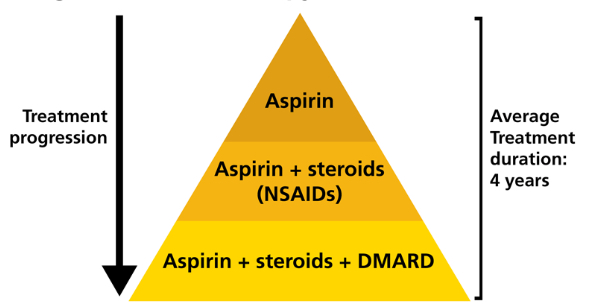
how WAS RA medically managed?
drug therapy—aspirin, aspirin +steroids (NSAIDs), aspirin + steroids + DMARD over 4 years
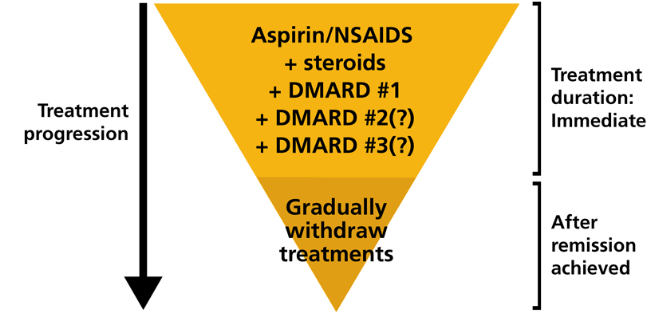
how IS RA medically managed?
aspirin/NSAIDs + steroids +DMARD 1 +DMARD 2? + DMARD 3? immediately
gradual withdrawal after remission
parameters for types & amount of intervention
determined by degree of synovitis, amount of joint destruction/deformity, pain tolerance, lifestyle
stage 1
early stage
notable by presence of synovial inflammation→joint swelling, pain w/ motion
immune cells→inflammation site→high cell counts in fluid
^ however—x-rays typically negative aside from possible presence of osteoporosis & soft tissue swelling
stage 1 treatment
focus on joint protection & inflammation control
stage 2
T and B cell proliferation and angiogenesis in synovium
synovial tissue grows into joint cavity across cartilage→destroys cartilage
typically no deformities, but mobility may become limited w/ muscle atrophy
mild malaise, presence of nodules
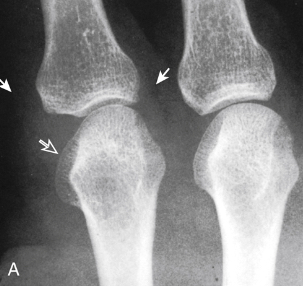
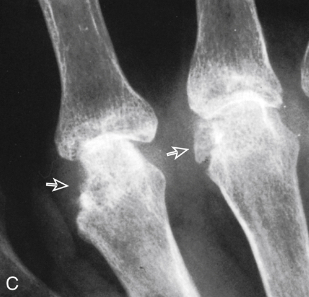
picture: solid arrows=swelling, open arrow=bone changes
stage 2 treatment
focus on joint protection & inflammation control
stage 3
accumulation of synovial fluid polymorphonuclear leukocytes (SFPMNs) as well as synovial cell proliferation
loss of cartilage→exposes bone
joint pain, swelling, limited ROM, morning stiffness, weakness, malaise, extensive atrophy, nodules, deformity
soft tissue swelling & cartilage loss shown on x-ray
picture: solid arrows=swelling, open arrow=erosion of MC

stage 3 treatment
pain relief & prevention of disability
stage 4
cessation of inflammatory process
formation of fibrous tissue and/or bone ankylosing (fusion)→cease joint function
MRI shows proliferative pannus (membrane of granular tissue)
joint pain, swelling, atrophy, nodules, deformity, limited ROM, morning stiffness (or general stiffness), weakness, malaise
picture: note osseous erosion
stage 4 treatment
reduce pain, stop additional joint damage
may undergo joint replacement surgery
classification of global functional status in RA
class 1-4
1=most independent, 4=least
class I
completely able to perform usual ADLs (self-care, vocational, avocational)
class II
able to perform usual self-care and vocational activities
limited in avocational activities
class III
able to perform saul self-care activities
limited in vocational and avocational activities
class IV
limited in ability to perform usual self-care, vocational, avocational activities
intervention during active stage
rest joints with splints/orthoses to maintain joint alignment and decrease pain/inflammation
APPROPRIATE rest to reduce inflammation
minimize trauma, reduce mechanical stress, large joints vs. small joints
use energy conservation principles
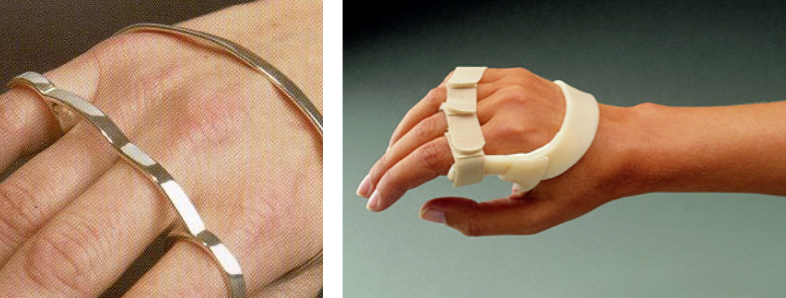
ring splints
decrease hypermobility of PIPs

ulnar drift splints
prolonged inactivity
loss of excs tolerance
incr weakness of muscles/ligaments
degeneration of joint cartilage
development of osteoporosis
inadequate loading of joint→reduce blood flow to synovium/cartilage
energy conservation principles
adequate nighttime rest: 8-10 hours
frequent rest periods & position changes
1 hour of rest during day to offset fatigue
goal of exercise
maximize joint motion, reduce soft tissue constriction
type of exercise
ROM exercises are safe & efficient in maintains joint motion without increasing damage/swelling
gentle ROM: AAROM or AROM without holding end position, 2-3 reps/day once a day
avoid PROM until after inflammation subsides
modalities?
goals for subacute disease
prevent deconditioning, maximize function
subacute interventions
modalities: heat prior to stretching
exercise: ROM, isometric, dynamic excs, progressive resistive training, aquatics, dance
ROM excs in subacute phase
AROM and PROm can be performed, end range position can be held
8-10 reps/day, frequency can increase, can be combined with flexibility
isom excs in subacute phase
increase reps and sets as tolerated
dynamic exercise with light resistance in subacute phase
more effective in incr strength than isom
monitor complications (ex. subluxations)
endorphin levels rise with increased intensity & freq of excs
freq & duration needed to produce change in muscle strength varies w/ severity & duration of disease
progressive resistive training for subacute phase
significantly increased lean body mass & fat-free mass w/o altering BW
overall QoL not affected, but less difficulty with advanced ADLs
no flare-ups or injuries occurred
intense training should be used to stimulate muscle growth in those w/ severe muscle wasting, pts with low-moderate disease activity would benefit more from low-impact moderate-intensity activity
aquatic excs for subacute phase
outcomes: incr aerobic capacity, CV endurance, better mood
buoyancy of water can resist or facilitate movement
waist-level water: BW=50%
neck-level: BW=10%
water temp: 82-86 F; relaxes muscle spasms and reduces pain
dance therapy
enhances functional outcomes & improves adherence to exercise
inactive disease/remission intervention
strengthening & aerobic conditioning
aerobic capacity, muscle strength, joint mobility, functional ability, mood have been shown to improve by 57% w/o apparent incr in joint symptoms/disease activity
strength from endurance training→stability to affected joints, improved shock absorption
encourage good joint protection techniques during excs sessions to use proper biomechanics
education on self-management allows pt to set realistic excs goals, monitor response, adapt to changing symptoms
implications for practice
improved outcomes in muscle strength, physical function, aerobic capacity w/ dynamic excs—more benefit w/ high intensity, best benefits w/ combined programs (strength & aerobics)
caution w/ using high impact excs to pts with high levels of baseline joint damage
no studies have addressed the effect of dynamic excs on CV outcomes in RA pts with CAD or its major risk factors—CAD = high risk for mortality in RA
don’t ignore benefits of excs with RA pts
if there is a benefit to excs, there will be a side effect (don’t encourage excs that cause more damage)
use caution in prescribing excs with pts who have significant joint damage (encourage more unloading activities, general physical activity is still beneficial for CV prevention)
juvenile idiopathic arthritis
similar to adult RA< but actually comprises a heterogeneous group of arthritides of unknown cause
children→18 y/o, occurs for at least 6 weeks
each classification (pauciarticular, polyarticular [RF+/RF-], systemic) has different presentations, genetic backgrounds, prognoses and is based on # of involved joints and presence of certain signs and symptoms
types of JIA in the population
50% pauciarticular
40% polyarticular
10% SOJIA
pauciarticular or oligoarticular JIA
affects four or fewer joints during first 6 mo of disease
usually in asymmetric pattern
most commonly involves knees, elbows, wrists, ankles
girls affected more than boys
usually btwn age 1-5
relatively mild, few extra articular features
parents may notice swollen joint, limp, abnormal gait, usually early after child wakes up in morning
leg-length discrepancy is common
pain is not a central feature at first, disease rarely manifests any constitutional symptoms
MOST COMMON
subtypes: antinuclear antibodies & high risk of uveitis; involved spine (in adolescence, HLA-B27 marker); joint involvement is extent of disease—no systemic signs
polyarticular JIA
affects five+ joints
most commonly includes large and small joints of wrists, C spine, TMJ, small joints of hands and feet, knees, ankles, hips
involvement usually symmetric, most like that of adult RA with potential for severe, destructive arthropathy
affects girls more than boys
subtypes: RF+ and RF-
RF+ polyarticular JIA
presence of rheumatoid factor (autoantibody found in blood of RA adults) and DR4 genetic type, also common in RA
subcutaneous nodules, C spine fusion, chronic uveitis (eye inflammation→irreversible damage and blindness), destructive hip disease can occur in this type
RF- polyarticular JIA
characterized only by joint involvement, usually less severe
negative rheumatoid factor
morning stiffness, fatigue, possible low grade fever
systemic onset JIA
affects boys and girls equally
with involvement of any # of joints
most severe extra articular manifestations, affects many body systems
begins w/ high fever (>102), chills that appear intermittently for weeks and may be accompanied by rash on thighs and chest that often goes away w/in a few hours
inflammatory arthritis typically develops at some point
95% of children have jiont symptoms w/in 1 year of initial symptoms
approx ½ of children w/ this type recover almost entirely
1/3 of affected children remain ill with persistent inflammation
JIA diagnosis
PMHx, physical exam, lab tests
serum evaluation: measure inflammation, detect antinuclear antibodies, RF, sometimes HLA-B27
signs of arthritis must be seen in 1+ joint for >6 wks in children under 16
pain often dull, aching, less severe; but presents in morning rather than more common presentation of nighttime growing pains
systemic features in systemic onset JIA are more readily diagnosed
JIA medical management
early use of DMARDS (MTX)
TNF inhibitors
IL-1 blockade for pts with macrophage activation syndrome
corticosteroids, anti-inflammatory for severe anemia, unrelenting fever, vasculitis
administered to control systemic and articular symptoms, and sometimes stop disease progression
bone marrow transplantation in cases where standard management isn’t effective
anti-TNF agents adverse effects
neuro disorders
weight gain
severe infection
hemorrhagic diarrhea
approximately 50% respond, but response is unsustained in many children
pt and family education for JIA
difficulty in getting appointments
long waiting lists
difficulty understanding/following therapist instructions
vocational, psychological counseling
exercise with JIA
improves functional ability, QoL, aerobic capacity
all outcome measures reported no worsening with excs therapy in short term
may safely participate in physical activities/sports w/o risking disease exacerbation
mod-sever impairment→tailor activities to lie w/in own pain limits
may benefit from combination of moderate aerobic, anaerobic, flexibility, strength training
appreciate differences between JIA subtypes
contraindications for exercise for JIA
should not participate in physical activity while febrile or any that temporarily increase joint pain/swelling
those w/ severe osteoporosis should avoid contact sports