Exam 1: Radiation
1/36
Earn XP
Description and Tags
Starred items were on test
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
37 Terms
sources of radiation exposure (3)
-anthropogenic sources (man-made): medical devices, electricity produced by nuclear reactors, used to kill/extend the shelf-life of foods, radioluminescence (glow-in-the-dark), heat generation in deep space missions
-primordial (largest source of radiation exposure): from when Earth was formed, radiation is in layers of ground (Radon gas is biggest contributor)
-cosmogenic: from space/atmosphere (increased risk of radiation if living at a higher altitude)
what is fluoroscopy + examples (4)
-continuous or pulsing x-ray beam that creates a live image on a monitor to guide a surgical procedure
-EX: C-arm in cath lab, ERCP, IR, pain management
radiation definition
when the nucleus of a radioactive atom (radionuclides) decay, they emit energy waves (EMR)/subatomic particles that crash into other molecules and knock out an electron (can then continue on into more molecules)
particle size relationship to speed and energy
-smaller particles = increased speed = increased energy/potential for damage
-larger particles = decreased speed = decreased energy/potential for damage
two main forms of radiation
ionizing and non-ionizing
non-ionizing radiation (definition + examples)
-waves/particles do not have enough energy to remove tightly bound electrons
-EX: visible light, microwaves
ionizing radiation (definition + examples)
-waves/particles DO have enough energy to remove tightly bound electrons (called “ionizing”)
-EX: medical radiation (gamma, x-rays for EMR; alpha/beta decay for non-EMR sources of radiation)
**more dangerous than non-ionizing radiation
ionizing forms of medical radiation from least to most damage (4)
-alpha particles (blocked by skin/paper; dangerous if inhaled/digested)
-beta particles (blocked by aluminum; can cause skin burns)
-x-rays, including fluoroscopy and CT (blocked by lead)
-gamma rays, including PET scan (blocked by dense shielding, like tungsten or concrete)
**MRI does not emit radiation as it uses magnets to create cross-section images
DNA damage one-strand vs two-strands
if it damages one strand of DNA, it might be able to repair itself; if it damage both strands of DNA then this is permanent damage that can lead to death and mutations
2 classifications of biological (somatic) effects of radiation exposure
-deterministic effects (threshold): only occur above a specific threshold of radiation exposure; increased effect severity with higher doses of radiation
-stochastic effects (probability): no safe threshold; instead, effect happens with the radiation dose (E.G., CA, mutations)
examples of deterministic (threshold) effects (2)
-chronic low-dose exposure: cataracts
-high-dose exposure: radiation sickness, skin burns, hair loss, dysrythmias
max regulatory standards for radiation exposure to body parts
-0.5 rem over course of pregnancy
-whole body: 5 rem/yr
what is latency?
CA caused by radiation that may not appear for years after initial exposure
what is radioactivity defined as + unit of measurement
-rate of radioactive decay
-Becquerel (Bq) in SI units and Curie (Ci) in Imperial units (1 Bq = 2.703 × 10^-11 Ci)
what is radiation absorbed dose defined as + unit of measurement
-energy deposited per mass, tells us the dose within a material
-Gray (gy) in SI units or rad in Imperial units (1 Gy = 100 rad = 1 J/kg)
what is radiation dose equivalent defined as + unit of measurement
-biological effect of dose based on dose of radiation and absorption by human tissue
-Sievert (Sv) in SI units or rem in Imperial units (1 Sv = 100 rem)
**this is what is used to set regulatory limits for radiation safety
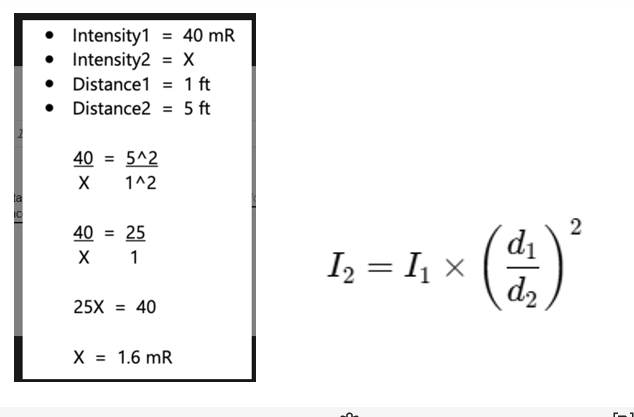
During fluoroscopy, patient receives 40 mR of radiation at a distance of 1 foot. How much radiation does the anesthesia provider receive at a distance of 5 ft?
**don’t forget exponent needs to be applied to both N and D
what organs are the most sensitive to radiation (5 and 2 that are not correct)
-bones, thyroid, lens of eyes, gonads (breasts, testes/ovaries)
-lymphocytes from lymph nodes (also includes spleen, thymus)
**generally any high rate reproducing cells are most at risk; NOT erythrocytes, skeletal muscle cells
what organs are moderately sensitive to radiation?
skin, GI
what organs are most resistant to radiation?
muscles, nerves
what are special populations that are at risk for serious effects of radioactivity? (5)
pregnant, fetuses in the womb, pediatric, geriatric, immunocompromised
why are children more sensitive to radioactivity?
their tissues are still growing/rapidly changing and they have a longer lifespan ahead of them which gives CA more time to mature
why do electromagnetic waves (EMR) exist?
electricity and magnetism always go together (direct proportional relationship), and can actually travel as particles AND waves (part of Quantum theory) at the speed of light (3.00 × 10^8 m/s)
examples of EMR (7)
radio waves, microwaves, infrared radiation, visible light, UV radiation, x-rays, gamma rays
EMR vs sound waves
-EMR has velocity that can exist in a vacuum
-sound waves cannot exist in a vacuum and must pass through a medium (e.g., why US needs gel to create a medium, or why you can’t hear someone scream in space)
trough
lowest point
peak
highest point
what is the most dangerous MRI zone?
Zone 4, as this is the area with highest magnetic force that can cause ferrous objects to have large amount of kinetic energy
what happens if O2 is ionized?
free radicals are created
parts of a C-arm (3)
-the bottom part of the C is the X-ray tube, which shoots radiation up
-the top part of the C is the image intensifier, which converts the waves into images
-collimator: focuses the beam, which then creates less exposure to radiation and a crisper image (e.g., think of a cone narrowing)
determinants of radiation exposure (2)
-time is directly proportional to radioactive exposure
-distance is inversely proportional to radioactive exposure (based on inverse square law, which states if you are at least 6 feet (2 m) away from the source of radiation, you are given ¼ exposure to the radiation)
**6 feet/2 m reduces radiation exposure 75-90%
what is the most effective way to protect yourself against radiation in the OR?
shielding (e.g., lead aprons, thyroid shields, leaded glasses, table skirt)
why does shielding work?
attenuation
dosimeter use
wear a dosimeter to measure radiation exposure on a clip that is placed at the level of the collarbone, facing the radiation source, and outside a lead apron
rules for wearing a dosimeter if pregnant
-in addition to the dosimeter at level of neck, also need to wear a fetal dosimeter at level of waist and under the lead apron
-also do double shielding and ask for reassignment if possible
ALARA Principle (as low as reasonably achievable)
-staff strategies (4): limiting time near radiation sources, standing as far away as practical from radiation source, using long extension tubing for IVs, stand on the image intensifier side of the C-arm and do not place body parts in the primary beam
-patient strategies (6): only perform if medically necessary, use pulse instead of continuous fluoroscopy, use last-image hold, limit the number of images taken, shield sensitive organs as able, dose adjustments if pediatric/underweight
what are common errors that increase radiation exposure in the OR? (4)
-failing to properly wear shields/dosimeters
-standing too close to radiation source/beam side
-unclear communication with radiation staff
-underestimating cumulative low-dose exposure