Alzheimer's and Dementia
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
What is early onset Alzheimer’s Disease?
< 65 yrs. Old
Faster progression
Down syndrome have an increased risk.
Attributed to alterations on chromosome 1, 14, or 21.
Chromosome 14: PSEN1: Encodes presenilin 1 ( most aggressive)
What is late onset Alzheimer’s Disease?
65 and older
Most common
APoE gene on chromosome 19: has 3 alleles.
ε2 – appears to confer protection against AD
ε3 – most common / neutral role
ε4 – increased risk of AD
Both alleles ε4, then 91% risk of Alzheimer's Disease by 80 yrs. old.
What is the role of Amyloid Beta Plaques and Alzheimer’s Disease?
Overproduction and/or decreased clearance of alpha beta peptides.
Appearance of alpha beta to dementia is estimated at more than 20 years.
Normal processing of Amyloid Precursor Protein (APP):
Involves cleavage of alpha-secretase then gamma-secretase
Abnormal procession of Amyloid Precursor Protein (APP):
Involves cleavage by beta-secretase then gamma-secretase.
What is the role of neurofibrillary tangles and Alzheimer’s Disease?
Density of neurofibrillary tangles correlates with severity of dementia.
NFTs consist of hyperphosphorylated Tau protein, and these cannot bind to microtubules so the microtubules collapse.
Hyperphosphorylated tau aggregates together to form NFTs which fill the cytoplasm.
This hypothesis is the loss of cholinergic neurons and is a consequence not accuse of Alzheimer’s Disease:
-Cholinergic
This hypothesis inflammation occurs due to beta amyloid accumulation and tau tangles:
-Inflammation hypotheis
What is the role of Glutamate ( excitotoxicity) in Alzheimer’s Disease?
Glutamate is a major excitatory neurotransmitter in CNS.
Increased levels: over-stimulate nerve cells killing them through excitotoxicity.
What are modifiable risk factors of Alzheimer’s Disease?
Main factors are Cardiovascular risk factors:
Diabetes
Hypertension
Dyslipidemia
Obesity
Metabolic syndrome
Tobacco
Late-life depression
Early and mild-life cognitive
Hearing impairment
Less education
Social isolation
Head injury
What is the non-modifiable risk factors of Alzheimer’s Disease?
Increased age (> 65 yrs. Old)
Female
Family history of Alzheimer's Disease
Genetic risk factors
Cognitive symptoms of Alzheimer’s Disease?
Amnesia: memory loss
Aphasia: inability to generate coherent speech or understand spoken or written language.
Agnosia: Inability to recognize or identify objects, assuming intact sensory function.
Apraxia: Inability to execute motor activities, assuming intact motor abilities.
Disorientation
Impaired executive function
Noncognitive symptoms of Alzheimer’s Disease:
Depression
Sleep disturbances
Psychosis
Behavioral disturbances
What types of things can you see in a patient in the early stage of Alzheimer’s Disease?
Forgets names of laces
Word-finding difficulties
Trouble using household appliances.
Loss interest in activities
What do you expect to see in a patient in the middle stage of Alzheimer’s Disease?
Forget recent events.
Has trouble handling money
Agitated
Starts walking or roaming about
What is the behaviors seen in the end stage of Alzheimer’s Disease?
Patients become rigid.
Mute
Incontinent
bedridden
What is Vascular Dementia?
Cognitive disorders caused by vascular disease.
Most common is occlusion of cerebral blood vessels leading to brain injury.
What is Lewy body Dementia?
Found primarily in people who have Parkinson’s Disease.
Symptoms:
Cognitive decline
Visual hallucinations
Fluctuations in alertness and attention
Parkinsonian motor symptoms
What is Frontotemporal Dementia?
Symptoms:
Changes in behavior:
Withdrawn/disinhibited.
Decline in personal hygiene.
Repetitive actions.
Overheating or compulsively putting objects in the mouth
Changes in speech:
Speaking less/total loss of speech
Word finding difficulty.
Echoing what has been said by others.
Writing and reading are also affected.
What are the goals of treatment for Alzheimer’s Disease and Dementia?
Prevent or delay progression.
Maintain cognitive function.
Reduce behavioral symptoms.
Maintain or improve functional abilities.
What are the nonpharmacological therapy to treat Alzheimer’s Disease and Dementia?
Behavioral interventions
Communication
What is the pharmacological treatment for the Cognitive symptoms of Alzheimer’s Disease and Dementia?
Cholinesterase inhibitors:
NMDA inhibitors
Monoclonal Antibodies
Donepezil (Aricept): Used for mild , moderate, and severe Alzheimer’s Disease and used off label for multi-infarct dementia
Dosing:
5-10 mg QHS mild-moderate Alzheimer's Disease
10-23 mg QHs moderate-severe Alzheimer's Disease:
Incidence of weight loss increased at dose of 23 mg.
Effectiveness:
Modestly improves cognitive symptoms.
Safety:
Common Adverse effects: GI upset, N&V, diarrhea, insomnia, decreased appetite, weight loss ; Rare: GI bleeding, AV block
Give medication at bedtime to minimize GI side effects.
Galantamine (Razadyne): Used for mild and moderate Alzheimer's Disease. Used off label for Lewy Body Dementia, Parkinson’s disease dementia, and Vascular Dementia
Dosing:
Initial 8mg/day for 4 weeks then increase to 16 mg/day for 4 weeks; may increase to 24 mg/ day .
Retitrate after > 3 days of interrupted dosing.
For people with moderate renal or hepatic impairment max dose is 16 mg/day.
Do not use in severe renal or hepatic impairment.
Effectiveness:
Modestly improves cognitive symptoms.
Safety:
Common: Gi Uset, N&V, dementia, insomnia, decreased appetite, weight loss ; Rare: GI bleeding, AV block.
ER formulation may increase adherence:
When switching form IR tablet to ER capsule use same daily dosing.
Readily crosses the BBB with little effect in periphery.
Recommended to take this medication with food and plenty of fluids.
Rivastigmine (Exelon): Used for mild , moderate, and sever Alzheimer's Disease and Parkinson’s disease dementia. Used off label for Lewy Body Dementia and Vascular Dementia
Dosing:
Oral: 1.5 mg BID , increase by 1.5 mg/dose every 2 weeks with goal of 6 mg BID.
Patch: 4.6 mg patch q 24 hrs. for 4 weeks, then 9.6 mg q 24 hrs. , then 13.3 mg q 24 hr.
Converting Oral to Patch:
< 6 mg/day po = 4.6 mg patch every 24 hrs.
6-12 mg/day po = 9.5 mg patch every 24 hrs.
Apply patch the day after the last oral dose.
If the patient has mild/moderate hepatic impairment or a very low body weight: 4.6 mg dose for both initial and maintenance dose.
Effectiveness:
Modestly improves cognitive symptoms.
Safety:
Common: Gi upset, N&V, diarrhea, insomnia, decreased appetite, weight loss, dizziness, headache, tremor.
Transdermal: Erythema, pruritis
Rare: GI bleeding, AV block
Anticholinergic drugs can reduce efficacy.
If dosing is interrupted for 3 or more days, reinitiate at lowest dose.
Patch formulation may be of benefit to patients who refuse meds.
Apply patch to clean, dry , hairless skin on upper or lower back every 24 hrs.
What are some warning associated with Cholinesterase Inhibitors?
Neurological effects: exacerbate or induce EPS; worsening of PD tremor. May potentiate seizures.
Peptic ulcers/GI bleeding due increased acid secretion
Anesthesia with succinylcholine type muscle relaxation
Cardiac conduction effects
Urinary obstruction
Asthma/obstructive pulmonary disease
What are some contraindications associated with cholinesterase inhibitors?
Unstable or sever cardiac disease.
Uncontrolled epilepsy
Unexplained syncope
Active peptic ulcer disease
What do you do if the desired effects are not perceived within 12 weeks of maximal tolerable dose?
Cholinesterase inhibitors should be de-prescribed.
True/False: Anticholinergics drug should not be used in Dementia/Alzheimer’s patients
-True
NMDA Antagonists:
MOA:
Blocks the action of Glutamate at NMDA receptors.
NMDA receptors involved in memory and learning.
Namenda (Memantine): Used for Moderate to severe Alzheimer’s Disease. Used off labeled for Parkinson’s disease dementia, Lewy Body Dementia, Comorbid Vascular Dementia
Dosing:
IR tablets: 5 mg po every day for 1 week, then 5 mg po twice a day for 1 week, then 5 mg po every morning and 10 mg po at night for 1 week, then 10 mg.
ER capsules: 7mg po every day for 1 week, then 14 mg po every day for 1 week, then 21 mg po every day for one week, then 28 mg po every day.
Effectiveness:
Synergistic benefit when used with cholinesterase inhibitors.
Modestly improves cognitive symptoms.
Safety:
H.A, dizziness, sedation, agitation, constipation
Rare: Stevens Johnson syndrome, DVT
DO not take with Anticholinergic drugs ( will reduce the efficacy)
Start 2nd drug after several months on 1st without adverse effects.
Begin ER product day after last dose of IR:
If on 10 mg po BID = 28 mg po every day
Memantine and Donepezil ( Namzaric): Used for moderate to severe Alzheimer’s Disease
Dosing:
14 mg/10 mg and 28mg/10 mg
Effectiveness:
Combo may be associated with small improvement in cognition, behavior, and activities of daily living.
Used in patient is stable on either donepezil 10 mg po once daily or memantine 10 mg po bid or 28 mg ER po once daily.
Can open/sprinkle on applesauce.
Monoclonal Antibodies:
MOA:
Targets aggregated soluble and insoluble forms of alpha beta to reduce amyloid beta plaques.
Boxed Warning:
Amyloid relating imaging abnormalities (ARIA): cerebral edema, microhemorrhages and macrohemorrhage.
APoE ε4 homozygotes:
Higher incidence of ARIA
Testing should be performed before giving this medication.
Ginko Biloba:
Inconsistent efficacy
Increased risk of bleeding in patients taking: NSAIDs, ASA, Warfarin
NSAIDs , ASA, prednisone all associated with risks.
Estrogens have a significant risk of CVA/Stroke
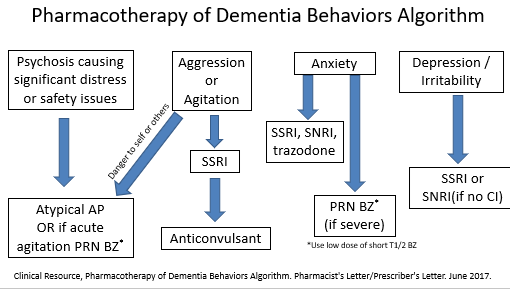
What is the pharmacological therapy to treat the Neuropsychiatric and Behavioral symptoms of Alzheimer’s Disease and Dementia?
-antidepressants, mood stabilizers, BZDs, antipsychotics
SSRIs: Used for depression, agitation, insomnia, irritability.
Avoid paroxetine as most anticholinergic side effects.
Avoid TCAs due to side effect profile.
Use escitalopram and citalopram.
Other antidepressants:
SNRIs:
Can be used but SSR preferred.
Avoid if side effects are problematic with patient history.
Mirtazapine:
Promotes sleep at lower doses.
Can improve appetite and weight gain.
Trazadone:
Useful at bedtime for sedation or daytime agitation.
Mood stabilizers:
Mood stabilizers:
Not FDA approved.
Used for delusions, hallucination, psychomotor agitation, combativeness.
Dextromethorphan and Quinidine (Nuedexta):
Indicted for pseudobulbar affect.
Used off label for agitation with Alzheimer's Disease and other dementias.
Dose 1 capsule once daily for 7 days and then twice a day
Quinidine dose is 1-3% of dose to treat cardiac arrhythmias.
Sedative hypnotics: Used Insomnia, Sleep- wake disturbance.
Consider melatonin.
PRN: Zaleplon, Zolpidem , Ramelteon
Safety:
Monitor for daytime sedation, dizziness, falls.
PRN and not routine use.
Avoid BZDs for sleep.
BZDs: Used for Anxiety, Insomnia, Acute Agitation
Not recommended
Efficacy:
Paradoxical agitation in elderly
Safety:
Drug accumulation, increased cognitive impairment, fall risk.
If no other option, use PRN at 1/3 to ½ usual dose for acute situations.
Antipsychotics:
Avoid use of 1st generation antipsychotics due to cardiac /EPS/TD
Can use 2nd generation antipsychotics but olanzapine is the worst at causing metabolic syndrome.
Pimavanserin (Nuplazid):
FDA approved for treatment of hallucinations and delusions associated with Parkinson’s Disease psychosis.
Not approved for Parkinson’s dementia.
Brexipiprazole:
FDA approved May 2023 for agitation associated with dementia due to Alzheimer’s disease.
Targeted dose: 2mg/day ; max dose 3 mg/day
Improvement in agitation
If no response after ~ 4 weeks , taper and withdraw.
Only brexipiprazole has an FDA indication
True/False: Always attempt non pharmacologic interventions before RX therapy
-True
Treatment Guidelines