Psychopathology – Late Life and Neurocognitive Disorders
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
Myths about late life
decline in cognition
decline in happiness
loneliness
Social selectivity with age
the tendency of individuals to become more selective in their social interactions with age
Problems in late life
physical decline, polypharmacy, research gap
Explain the problem of physical decline in late life
more than half of 60+ have a severely debilitating medical condition
quality and depth of sleep declines with age (causing cognitive, physical, and psychological problems)
Explain the problem of polypharmacy in late life
40% of elderly people are prescribed 5+ meds, clinicians not checking and patient underreporting causes dangerous interactions
Explain the problem of research gap in late life
researchers test drugs on younger people and overlook symptoms that are more serious in the elderly
more than 20% are prescribed inappropriate medication
STOPP/START is a screening tool that identifies them and offers alternatives

Effects in the study of aging
age effects → effects of being a certain age
cohort effects → effects of having grown up in a certain period
time of measurement effects → effects of being tested in a certain period
Pro and con of longitudinal experiments in developmental change
group differences have less effects
selective mortality, biased by attrition
Selective mortality
when people die before follow up
Prevalence and incidence of psychological disorders in late life
65+ have lowest prevalence of all age groups
most disorders have earlier onset, and most with disorders in late life have had them for a long time
late onset is common for drinking problems
Reasons for low prevalence of psych. disorders in late adulthood
positive emotionality and more close-knit social circles
methodological errors
Methodological issues in measuring late life psychopathology
response bias → may be more uncomfortable discussing mental health and drug use
cohort effects → time period of upbringing affects prevalence
selective mortality → those with psychopathology die younger
Treatment considerations for elderly (while most work for all ages…)
some psychiatric meds can be dangerous
therapy may need to be adjusted for loss of senses or mobility
with cognitive decline the presence of a caregiver and reminders can be helpful

Dementia symptomatology
cognitive deterioration which causes functional impairment
diagnosis is based on declines in cognitive abilities
memory loss is most common

Neuropsychiatric symptoms of dementia
psychiatric symptoms secondary to the neurological disease
affective and motivational symptoms (depression is most common, affecting half)
sleep disturbance, loss of impulse control, hallucination/delusion
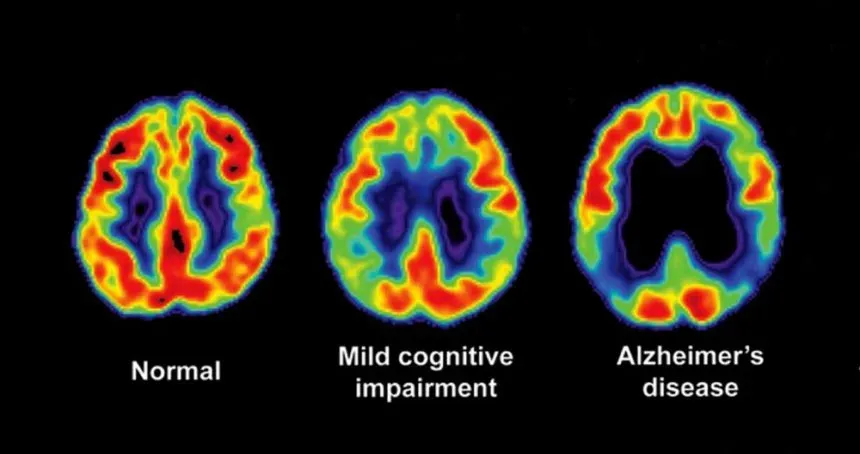
Dementia development
most forms develop slowly, first symptoms appear before impairment
early signs before functional impairment are called mild cognitive impairment (MCI)
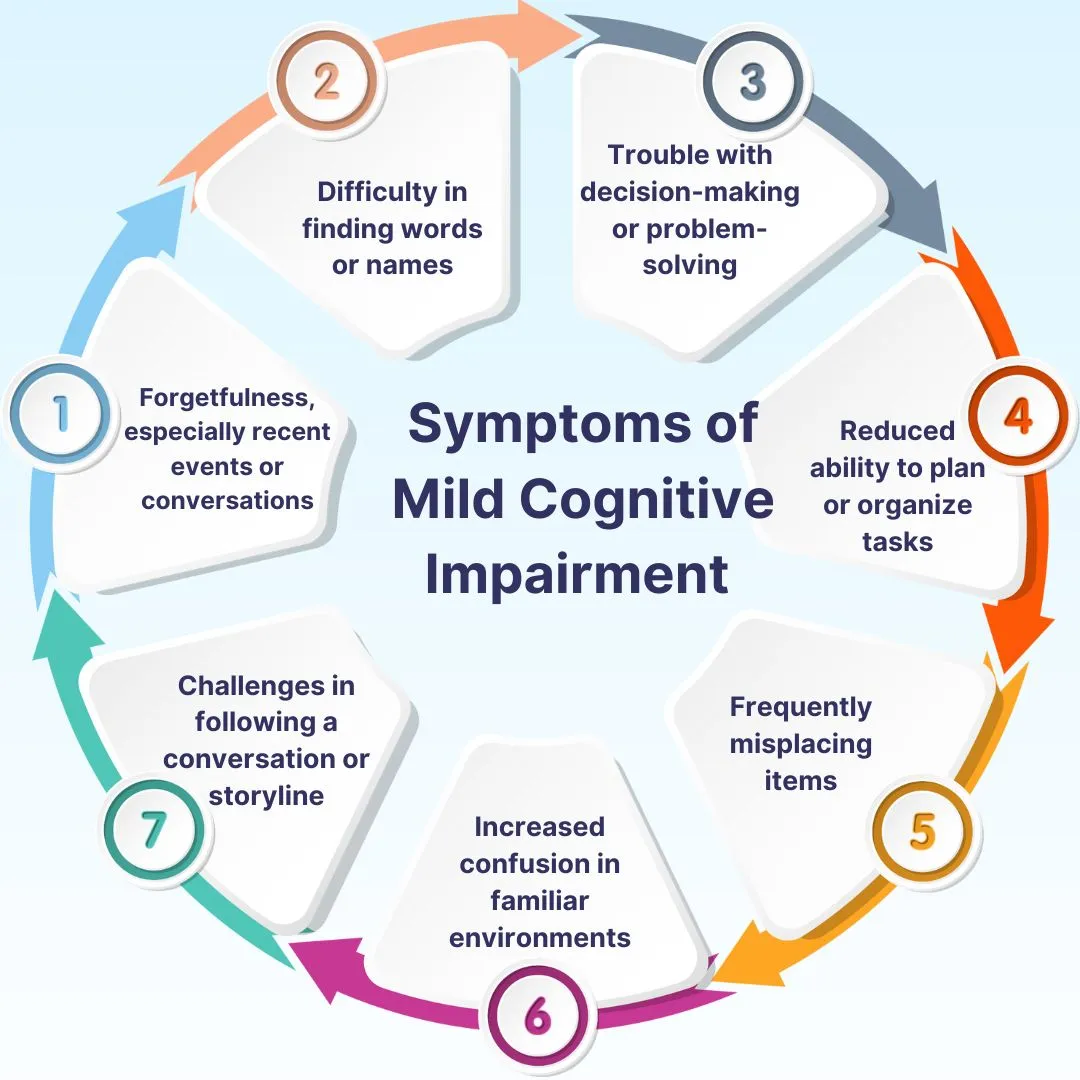
Mild neurocognitive disorder DSM-V
modest cognitive decline based on substantial neurocognitive impairment and concerns of patient, close other, or clinician,
does not interfere with independence or everyday activities but may require effort and accommodation
Consideration for diagnosing mild neurocognitive disorder
requires low score on one cognitive test but some tests are more reliable and using multiple tests can improve reliability
10% of the time cognitive decline is tied to reversible factors
10% with MCI and 1% without MCI will develop dementia in one year
Major neurocognitive disorder DSM-V
significant cognitive decline based on substantial neurocognitive impairment and concerns of patient, close other, or clinician
interferes with independence and everyday activities
Main symptoms of Alzheimer’s disease
memory loss → most prominent, may be overlooked for years
apathy → common before cognitive symptoms, one third develop MDD
language → problems word finding
visuospatial abilities → disorientation
Alzheimer’s progression
early → lack awareness, blame others, persecution delusions
moderate → impaired judgment and comprehension, disorientation, agitation
terminal → personality loss, narrowed social involvement, oblivion
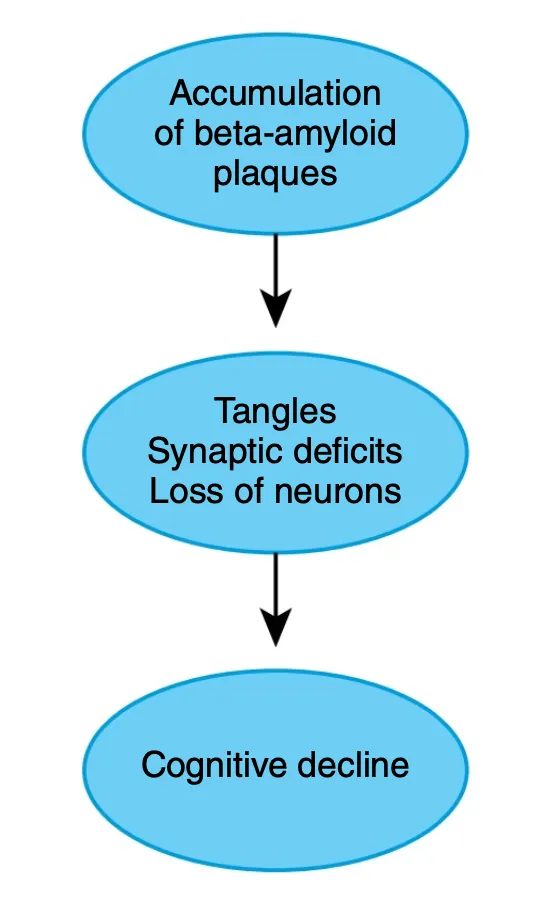
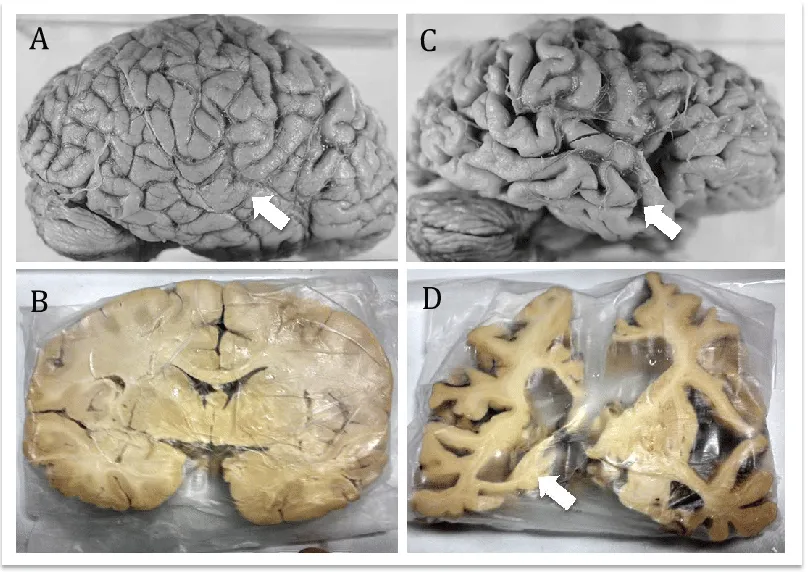
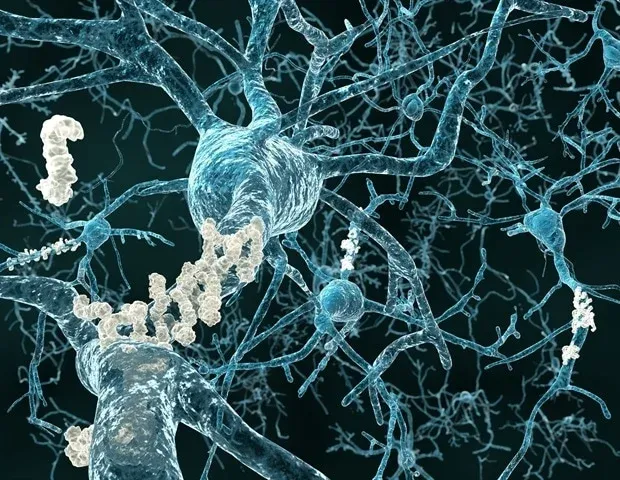
Biological causes of Alzheimer’s
more plaques → disrupt communication and trigger inflammation
more neurofibrillary tangles → disrupt cell function and trigger cell death starting in the hippocampus
Alzheimer’s late onset heritability
0.6-0.8
Genes associated with Alzheimer’s
APOE4 on chromosome 19, genes related to immune function and cholesterol metabolism
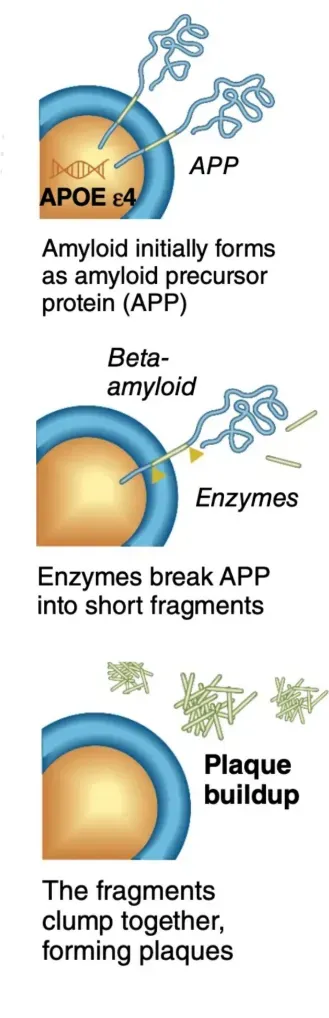
APOE4 and Alzheimer’s
causes overproduction of plaques, less beta-amyloid clearing, and less glucose metabolism in cerebral regions before symptom onset
Genes related to immune function and cholesterol metabolism in Alzheimers
triggers inflammation which increases risk
glycemia and diabetes also tied to Alzheimer’s
Lifestyle factors related to Alzheimers
exercise and intellectual engagement

Exercise in Alzheimer’s etiology
lower cognitive decline and plaque levels especially for those with APOE4 polymorphism
levels in mid-life and late-life are important

Intellectual activities in Alzheimers etiology
frequent engagement lowers risk
in those with similar levels of plaque and tangles those with higher engagement have less cognitive decline
Cognitive reserve
the idea that people can compensate for the disease by using different brain networks or cognitive strategies
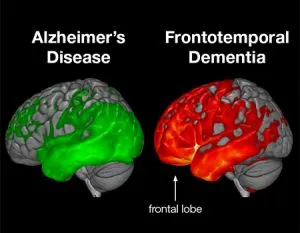
Frontotemporal dementia (FTD)
caused by a loss of neurons in frontal and temporal regions, especially the anterior temporal lobes and PFC
usually begins in late 50s and progresses rapidly, causing death within 5 years of diagnosis
<1%
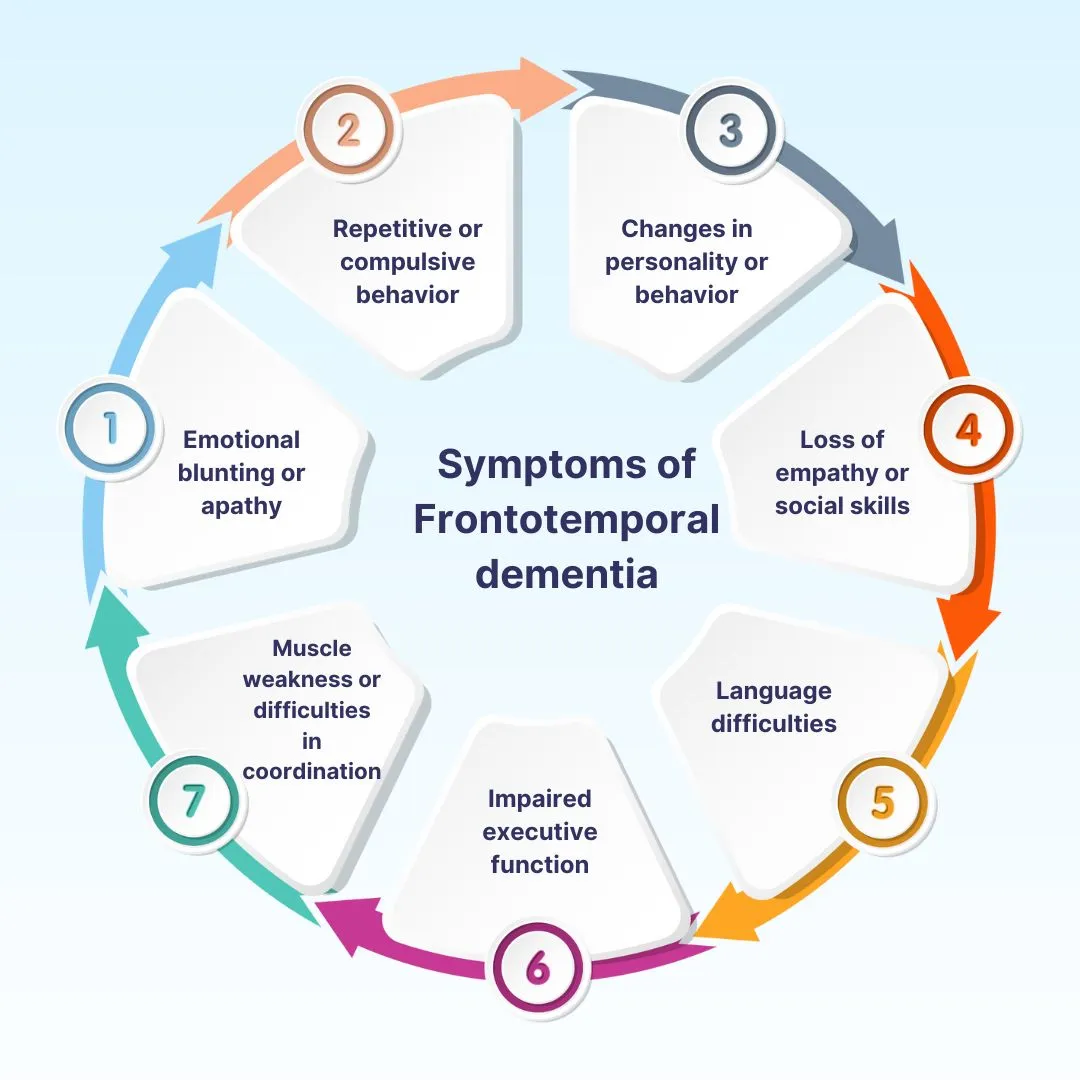
FTD symptoms and diagnosis
emotional dysregulation linked to inappropriate behavior
loss of sympathy and emotional responsiveness linked to damaged relationships
often misdiagnosed
FTD etiology
presence of pick bodies and high levels of tau protein
Vascular dementia
caused by cerebrovascular disease
most commonly caused by strokes
symptoms depend on stroke location
Vascular dementia risk factors
same as cardiovascular disease
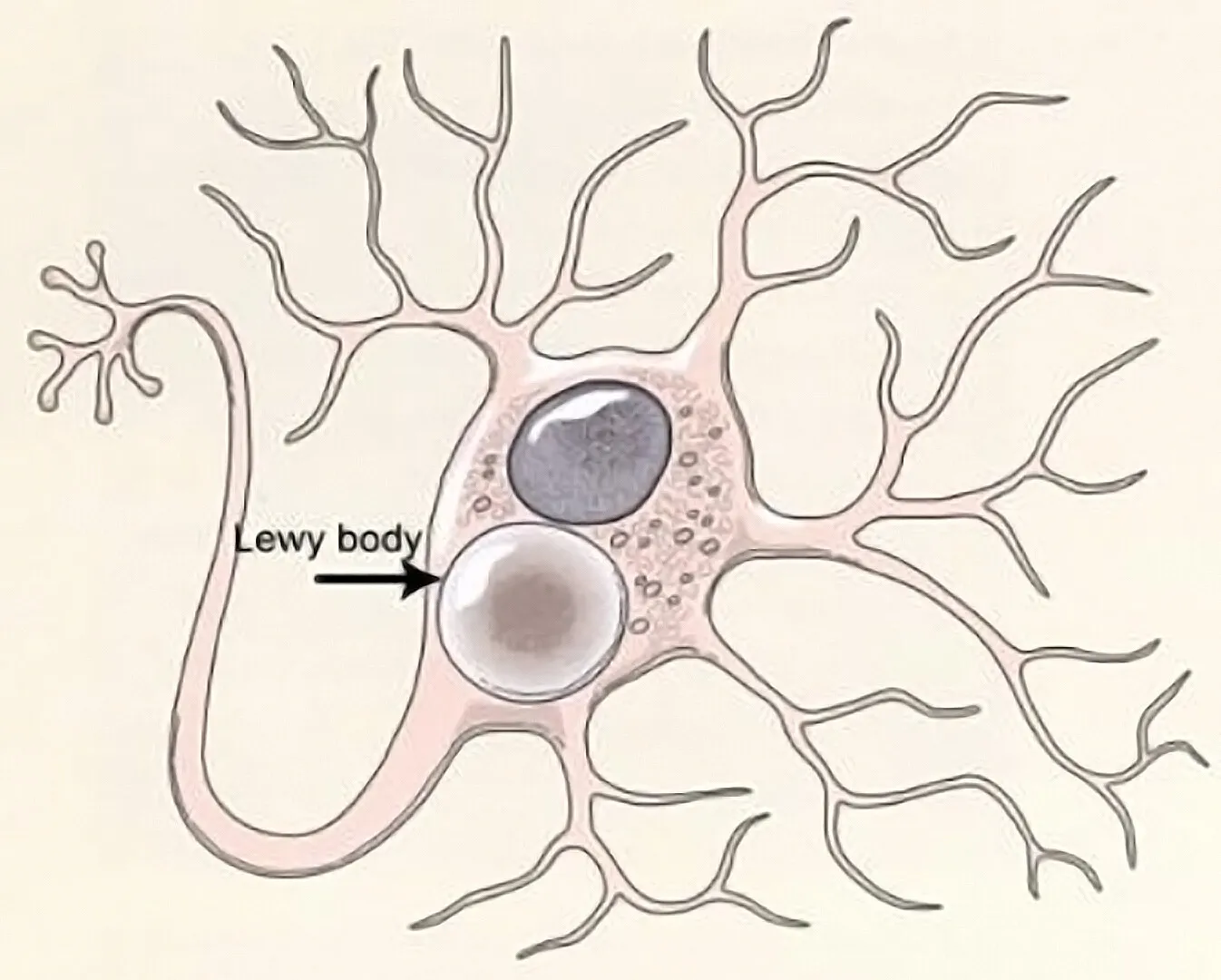
Lewy bodies
abnormal protein deposits in the brain found in DLB and Parkinsons
interfere with signaling and transmission
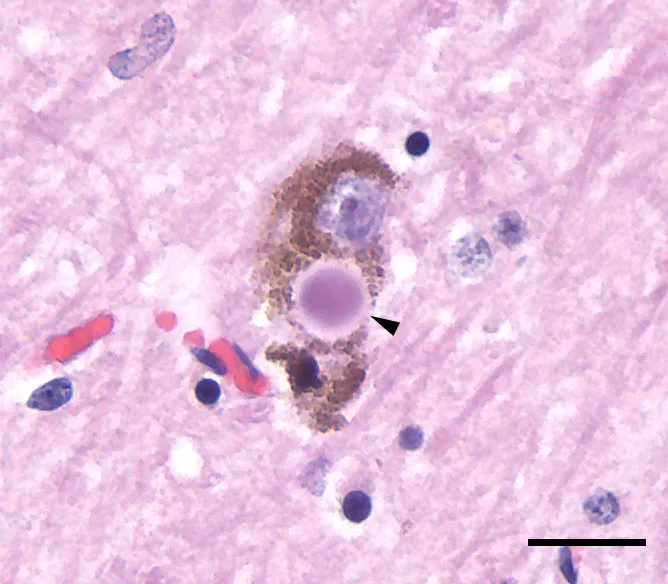
Lewy body dementia pathology
lewy bodies initially form in the olfactory bulb and brainstem
cognitive symptoms appear as they spread
affect regions for movement, memory, and perception

Dementia with lewy bodies symptoms
cognitive decline
motor symptoms
hallucinations
fluctuating attention and alertness
vivid dreams with movement and vocalization
severe sensitivity to antipsychotics
Diagnostic challenges in dementia with lewy bodies
often misdiagnosed as alzheimers or parkinsons
requires careful observation of fluctuations and hallucinations
Two most common medicinal dementia treatments
cholinesterase inhibitors, memantine
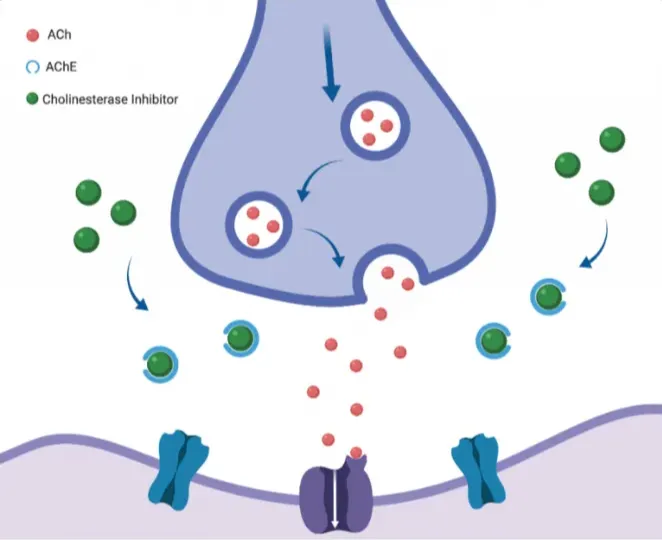
Cholinesterase inhibitors in dementia treatment
slow memory decline by preventing ach breakdown
do not restore lost memory and often cause nausea leading to discontinuation
donepezil

Memantine in dementia treatment
regulates glutamate (involved in memory) showing modest benefit for alzheimers
small effects

Medicinal treatment to manage psychological symptoms of dementia
antipsychotics offer some relief but increase death risk in early dementia
antidepressants reduce agitation but show mixed efficacy for depression symptoms

Vascular dementia treatment
controlling hypertension and cardiovascular health
may also slow alzheimers progression in those with hypertension
Past approach: Removal of beta-amyloid plaques
plaque accumulates years before symptoms so the treatment was often too late
sometimes worsened symptoms

Current approach: Early Prevention & Intervention
targeting early biological markers like plaques or tangles
prevent MCI from progressing
studying people at risk before symptoms appear

Emerging approach: electrical stimulation
may enhance memory recoding but is not yet approved for MCI or dementia
Psychological/Lifestyle Dementia Treatments
supportive psychotherapy
behavioral intervention
exercise and cognitive training
lifestyle intervention

Supportive psychotherapy in dementia treatment
therapist offers accurate information, home care strategies, and realistic coping approaches to prevent catastrophic thinking and foster confidence in management
Behavioral interventions in dementia treatment
memory aids compensates for memory loss
music therapy reduces agitation and disruptive behaviors
psychotherapy reduces depression
pleasant activities reduce depression and increase engagement

Exercise and cognitive training in dementia treatment
exercise moderately improves cognitive function in healthy elderly and those with MCI
cognitive training shows domain-specific improvements
meta-cognitive training shows broader cognitive improvements
more effective before development, especially for healthy older adults or those with MCI
Lifestyle interventions in dementia treatment
program of diet, exercise, and cognitive training may improve executive function
Delirium symptom categories
disturbed awareness/attention, cognition, and emotion/behavior
Delirium disturbance in attention and awareness
deficits in focus and attention
wandering thoughts and difficulty holding conversation
alternation between lucidity and confusion
sleep-wake cycle disturbance

Delirium cognitive disturbances
disorientation
memory impairment
incoherent speech and disorganized thinking
misinterpretation of environment
delusions and sometimes visual hallucinations
Delirium emotional and behavioral changes
mood swings
erratic behavior
fluctuations in motor activity (hyperactive to hypoactive)
sundowning (heightened agitation at night)
Delirium drug related etiology
drug intoxication or withdrawal, most common
Delirium and medical conditions
infections, metabolic or nutritional imbalances, post-operative stress
Delirium and neurological factors
head trauma, seizures, dementia
Delirium and environmental factors
dehydration, immobility and use of physical restraints
Older adults’ vulnerability to delirium
age-related physical decline
higher susceptibility to chronic diseases
polypharmacy
increased drug sensitivity
Medical treatment of delirium
address underlying causes
atypical antipsychotics
recovery time is 1-4 weeks but longer in elderly
Preventative care of delirium
ensure proper sleep-wake cycle and reduce sleep disruption
ensure proper hydration and nutrition
use re-orientation aids and restore use of glasses and hearing aids ASAP
Special considerations in treatment and diagnosis of delirium
delirium can be mistaken as dementia progression
families should be educated on delirium symptoms and recognize them as reversible with timely care