Growth/Development + Anatomy/Physiology - Pediatrics
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
29 Terms
Infancy
First year of life
neonatal/newborn
First month of life
Spend most of their time sleeping (up to 16 hrs/day), eating
Can’t tell the difference between caregivers and strangers
Sucking reflex
Can focus on faces
0-2 mo
More active - smile, make eye contact, follow objects with their eyes
Recognize caregivers
Use hands to examine objects, roll over
Active extremity movement
2-6 mo
Babble, say their 1st word
Sit w/out support, crawling, learn to walk
Teething, put things in their mouth
Cry when separated from their parents - separation anxiety
6-12 mo
Warm the stethoscope
Use a pacifier
Let the parent hold the infant
Do the more painful or uncomfortable procedures last
Explain each procedure
How should you assess infants?
Toddler
1-3 yo
Walk, open doors/drawers - explore
Imitate the behaviors of older children/parents
Speak 4-6 words
12-18 mo
Vocabulary 10-15 words
2 yo - pronounce 100 words
Point to a common object - toddlers can name it
Understand cause and effect
Balance, gait improving, running, climbing
Cling to their parents, special objects (blanket, stuffed animal).
18-24 mo
Preschool
Rapid increase in language
Walk, run well, begin throwing/catching/kicking
Learning which behaviors are appropriate
3-6 yo
School-age
Can think in concrete terms, respond to direct questions, help take care of themselves
School - concerns about popularity, peer pressure
Understand that death is final
6-12 yo
True
Only in toddlers and preschool age should you begin assessing the feet first and move to the head
True or false: when assessing children between the ages of 6-12, begin your assessment at the head and move toward the feet.
Adolescents
Think abstractly, participate in decision making
Personal morals - values/beliefs
Shift from relying on family to relying on friends for emotional support, social development, acceptance from their peers
Puberty
12-18 yo
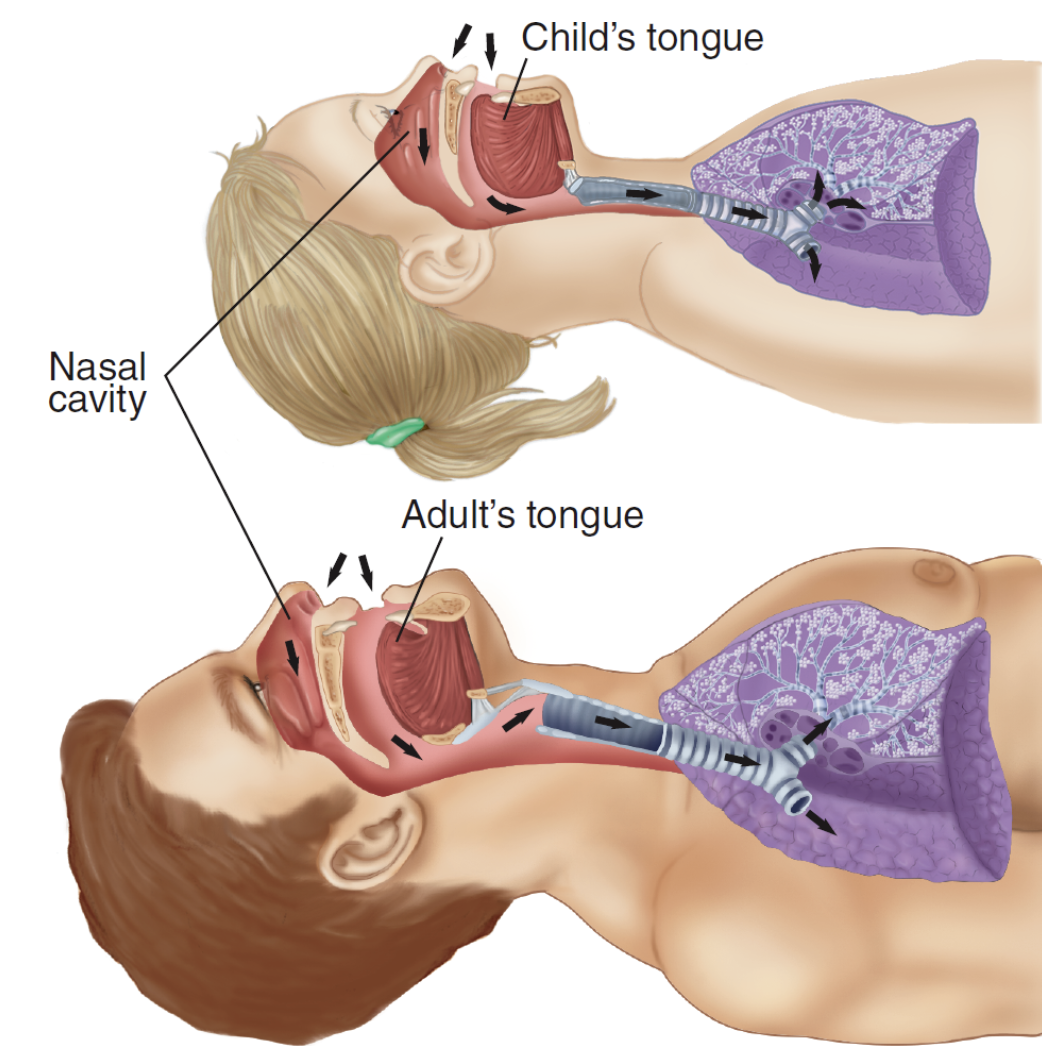
Smaller lungs, heart’s higher in the chest
Glottic opening (vocal cords) - higher, more anterior
Long, floppy, U-shaped epiglottis
Larger/rounder occiput
Larger tongue, more anterior
Less developed rings of cartilage in the trachea - collapses if the neck is hyperextended
How is the pediatric airway different from an adult’s?
False - nose breathers
True or false: infants are mouth breathers, requiring more suctioning to maintain a clear airway
Higher O2 demand, smaller O2 reserve (smaller lungs = smaller reserve)
Underdeveloped intercostal muscles (muscle fatigue onset is faster)
Belly breathers - rely on their diaphragm
Why do infants have a greater risk of hypoxia?
Infant (1mo-1yo): 30-60
Toddler (1-3 yo): 24-40
Preschool (4-5): 22-34
School age (6-12): 18-30
Adolescent (13-18): 12-16
RR for infant - adolescent
They have thinner chest walls
Why are breath sounds easier to hear in children?
Newborn - 3 mo: 85-205
3 mo - 2 yo: 10 -190
2 - 10 yo: 60-140
>10 yo: 60-100
HR newborn to >10 yo
pallor, weak distal pulse, delayed cap refill (>2 sec), cool hands/feet
Signs of vasoconstriction
Occipital region is larger, increasing the momentum of the head during a fall
Subarachnoid space - smaller, less cushioning for the brain
Brain tissue, cerebral vasculature - fragile, susceptible to bleeding from shearing forces
Needs a higher amount of cerebral blood flow, O2, glucose - secondary damage from hypotension/hypoxia
Why is the brain at an increased risk for injury in children?
False - less common in children, C-spine injury most likely to the ligaments
True or false: spinal cord injuries are more common in pediatric pts than adults
Internal organs are closer together (Liver, spleen, kidneys - more frequently injured)
Why are children at greater risk for multiple organ injury?
Liver and spleen (larger and anterior)
What 2 organs are more susceptible to bleeding and injury from blunt or penetrating trauma?
Fontanelles
Soft areas where the baby’s skull has not fused together. Fused by 18 mo (anterior), 6 mo (posterior).
False - normal
True or false: bulging is an ominous sign when an infant is crying, coughing, or lying on their back/stomach
increased intracranial pressure
Bulging fontanelles when the infant isn’t crying indicates ….
dehydration
Sunken fontanelles indicate
True
True or false: growth plates are weaker than ligaments and tendons