Gross Anatomy 16 - Abdomen IV
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
On anterior abdominal organ view, which organs are typically visible?
Liver occupies right upper quadrant, stomach lies left upper quadrant, transverse colon crosses abdomen, and small intestine occupies central abdomen.
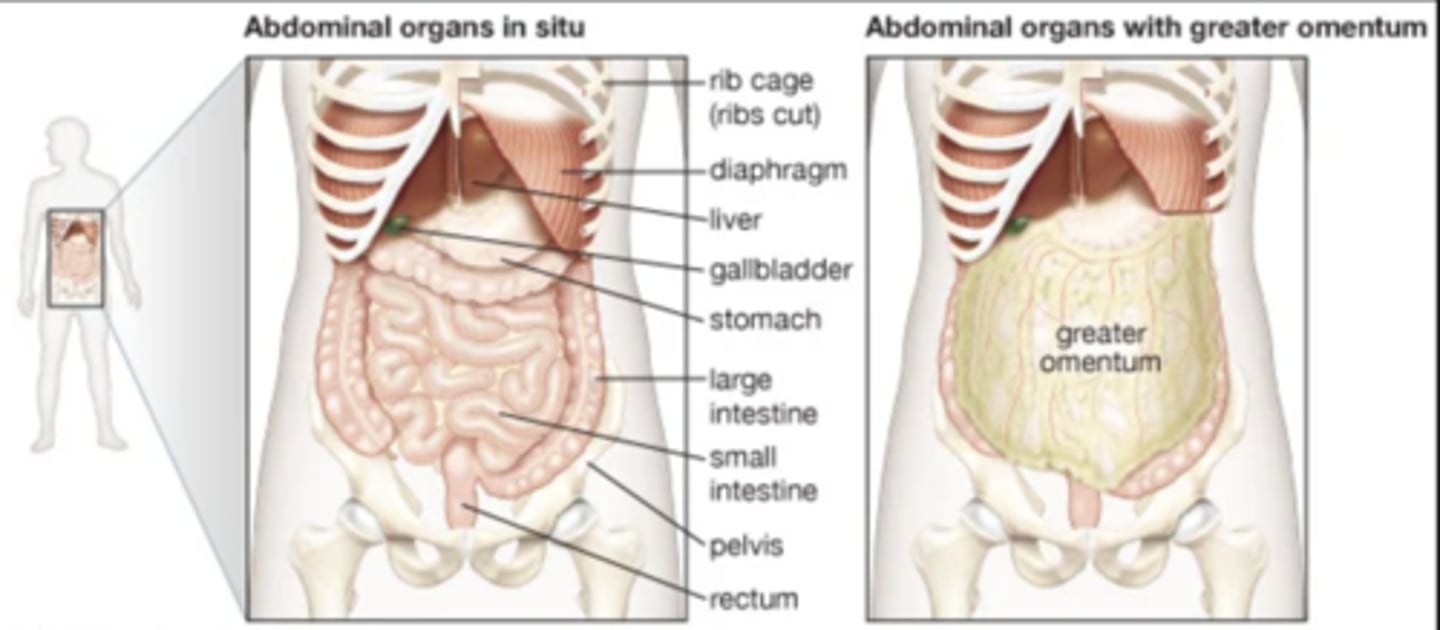
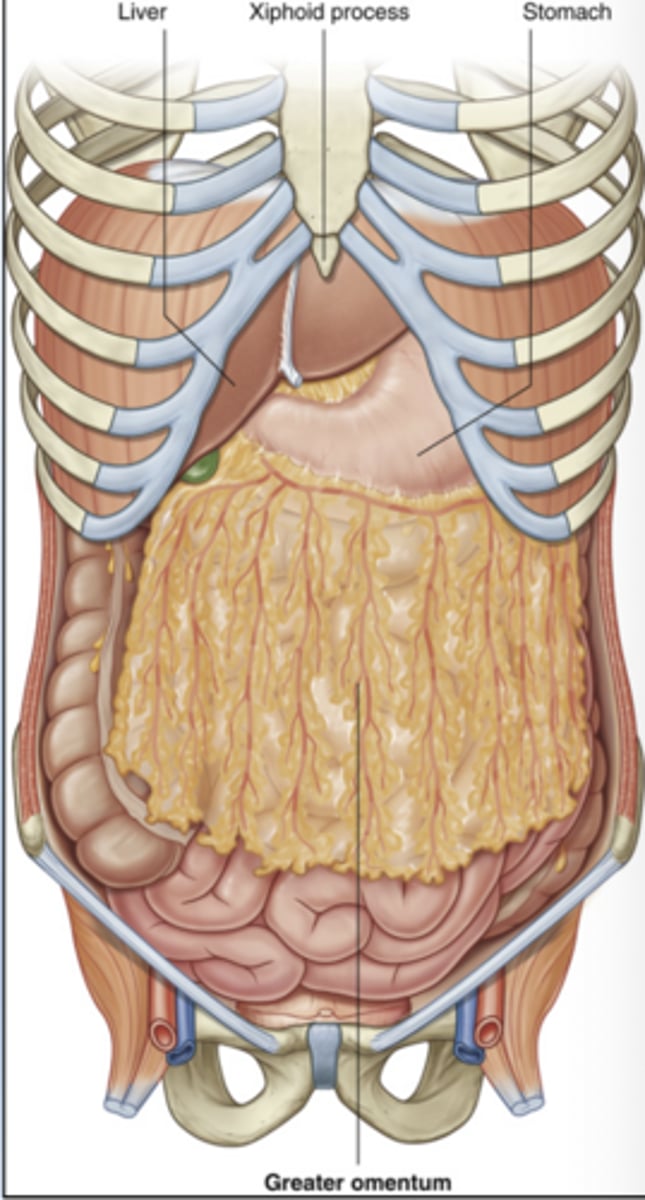
What is the role of the greater omentum and why is it clinically important?
Protects abdominal organs, stores fat, and provides immune surveillance.
It can migrate toward inflamed areas.
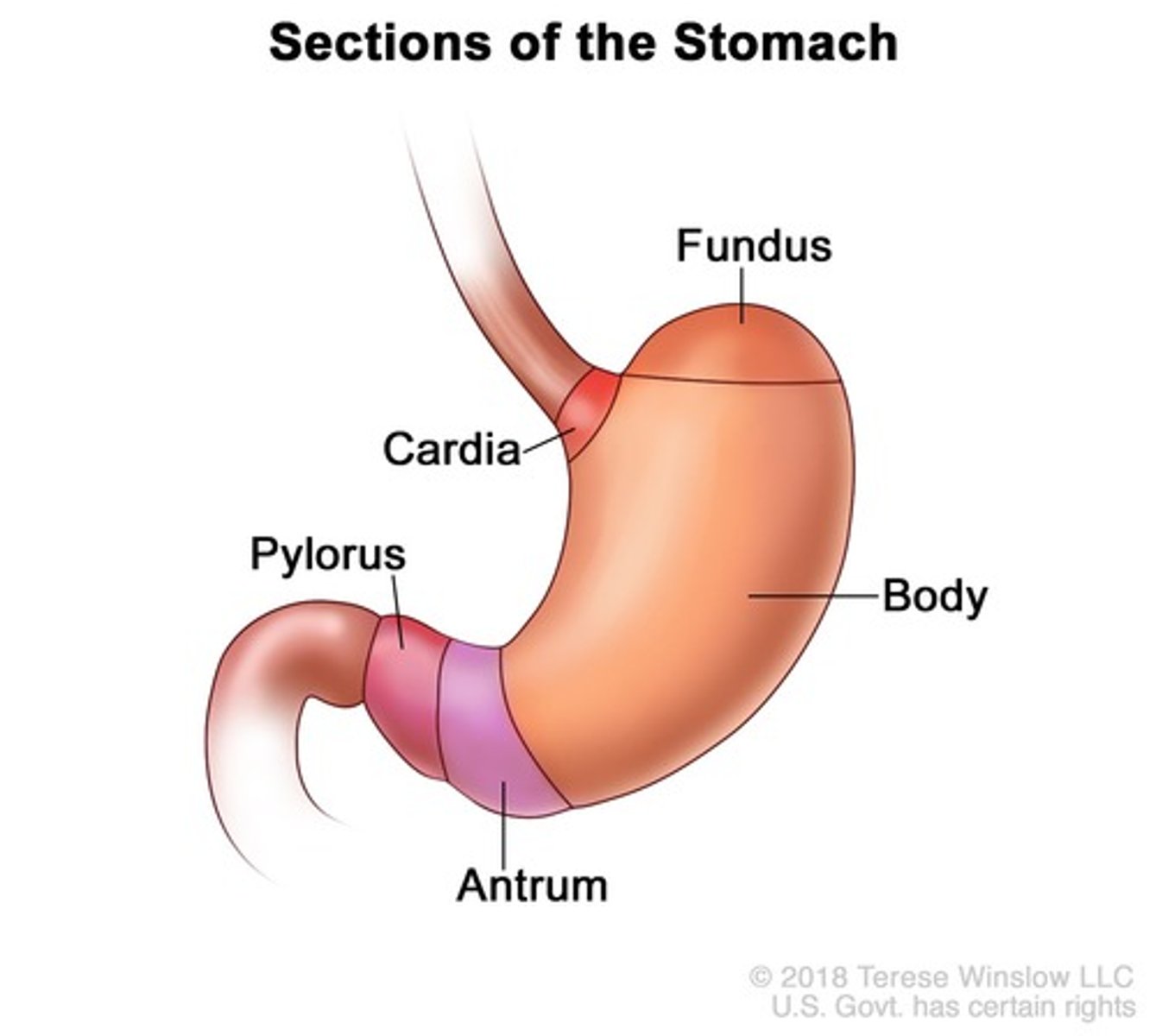
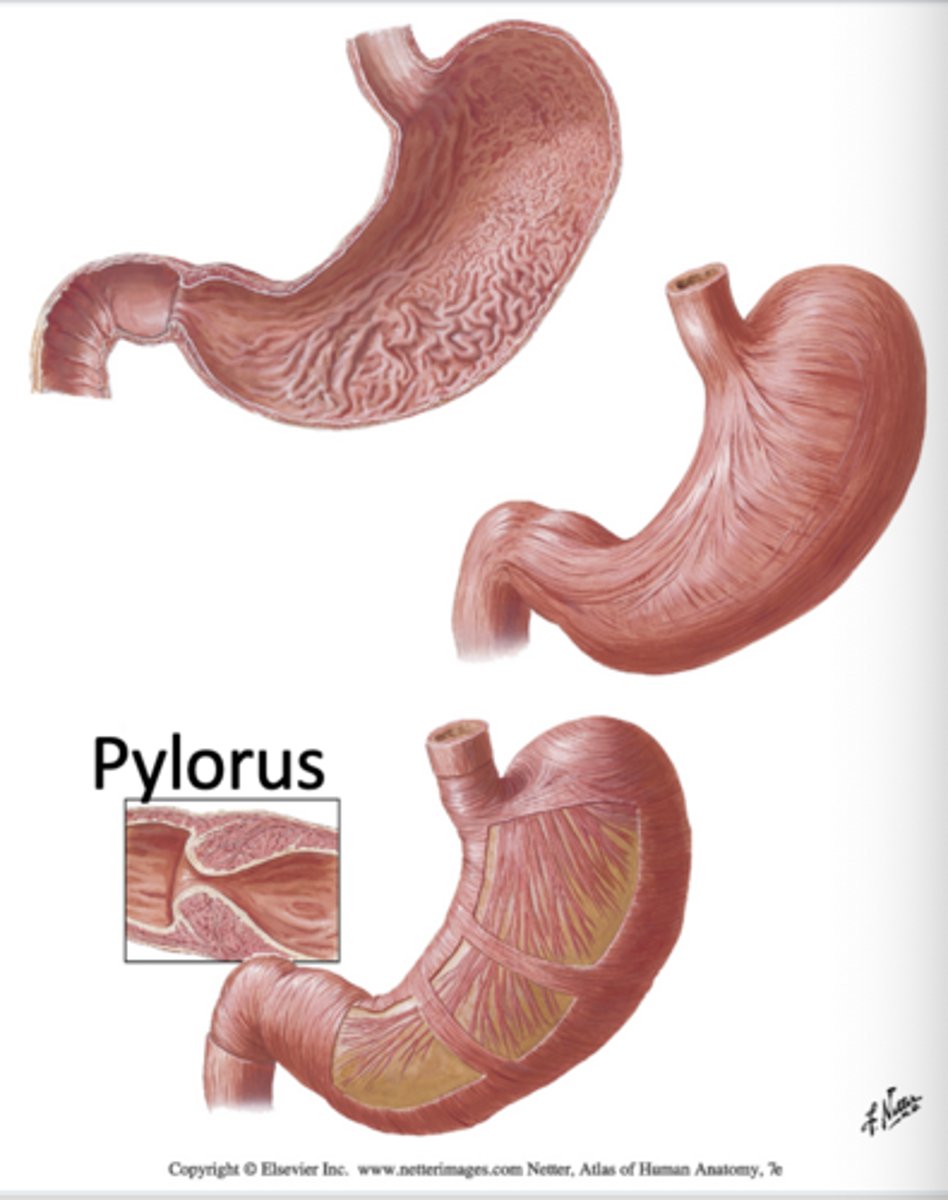
What are the 5 parts of the stomach?
cardia, fundus, body, antrum, pylorus
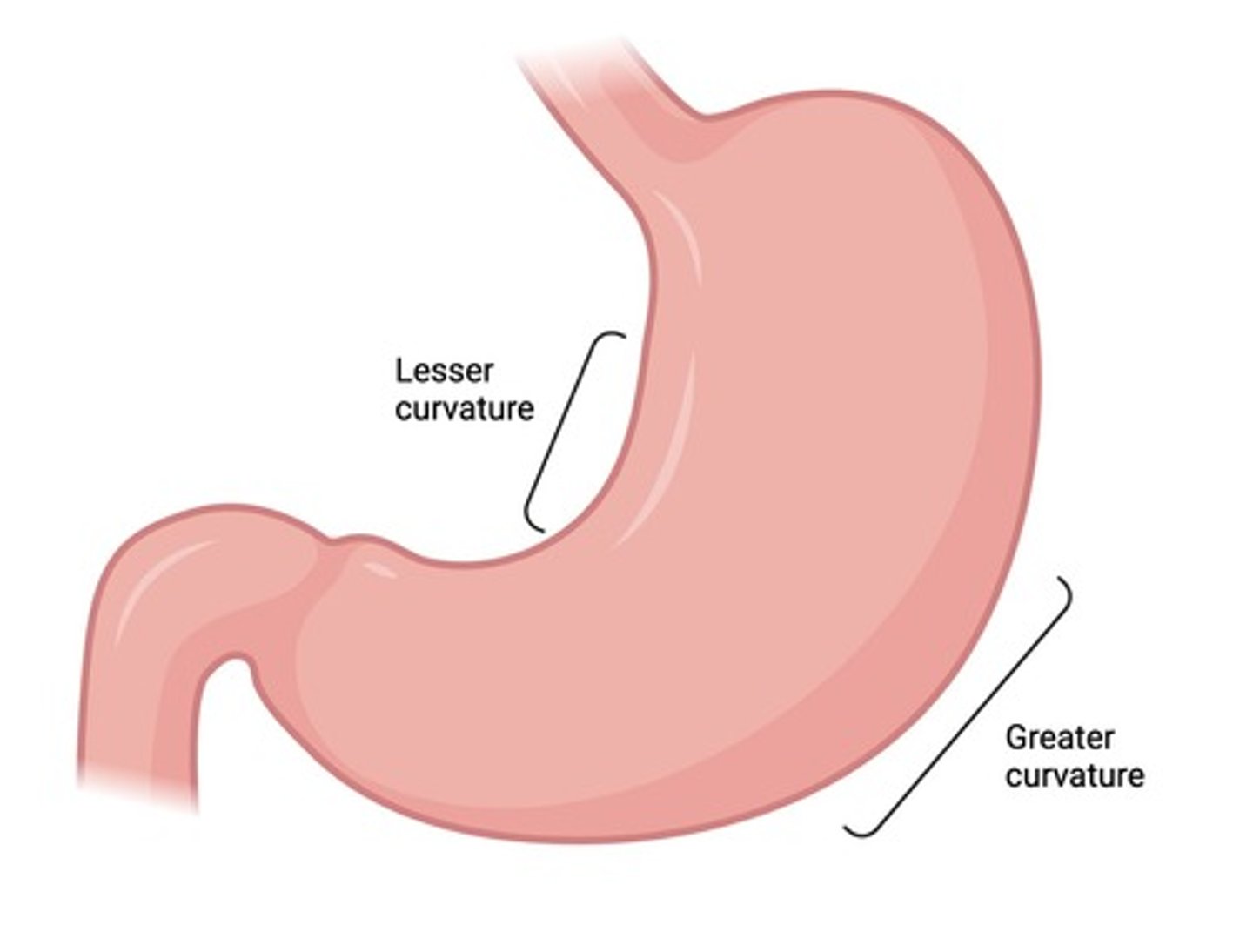
What are the two curvatures of the stomach?
greater curvature (where greater omentum attaches) and lesser curvature
What are the major structural features of the stomach?
The stomach has three muscular layers, mucosal folds (rugae), and a pylorus sphincter that regulates gastric emptying.
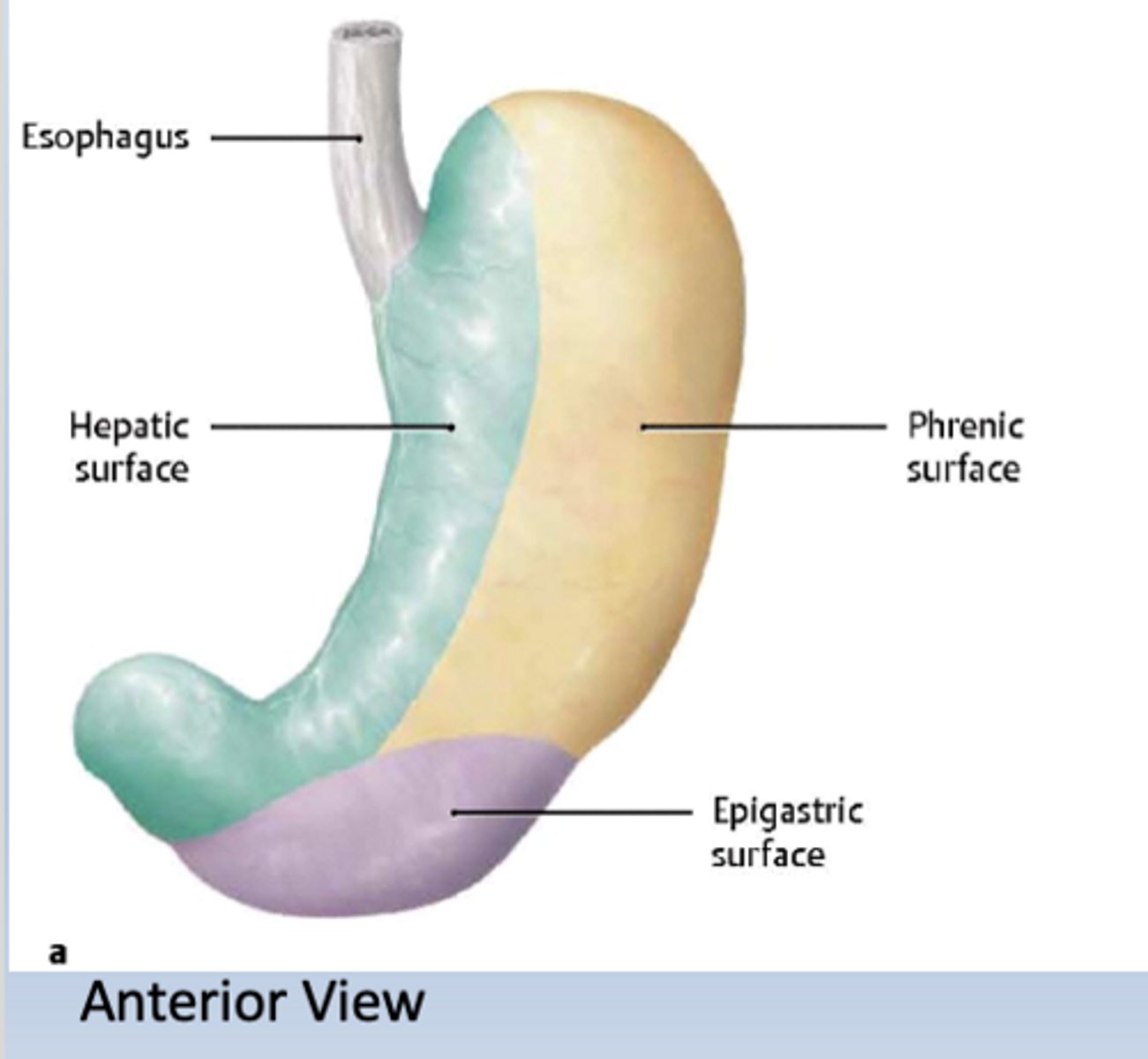
What are the major anterior relationships of the stomach?
hepatic surface (liver), epigastric surface, and phrenic surface (diaphragm).
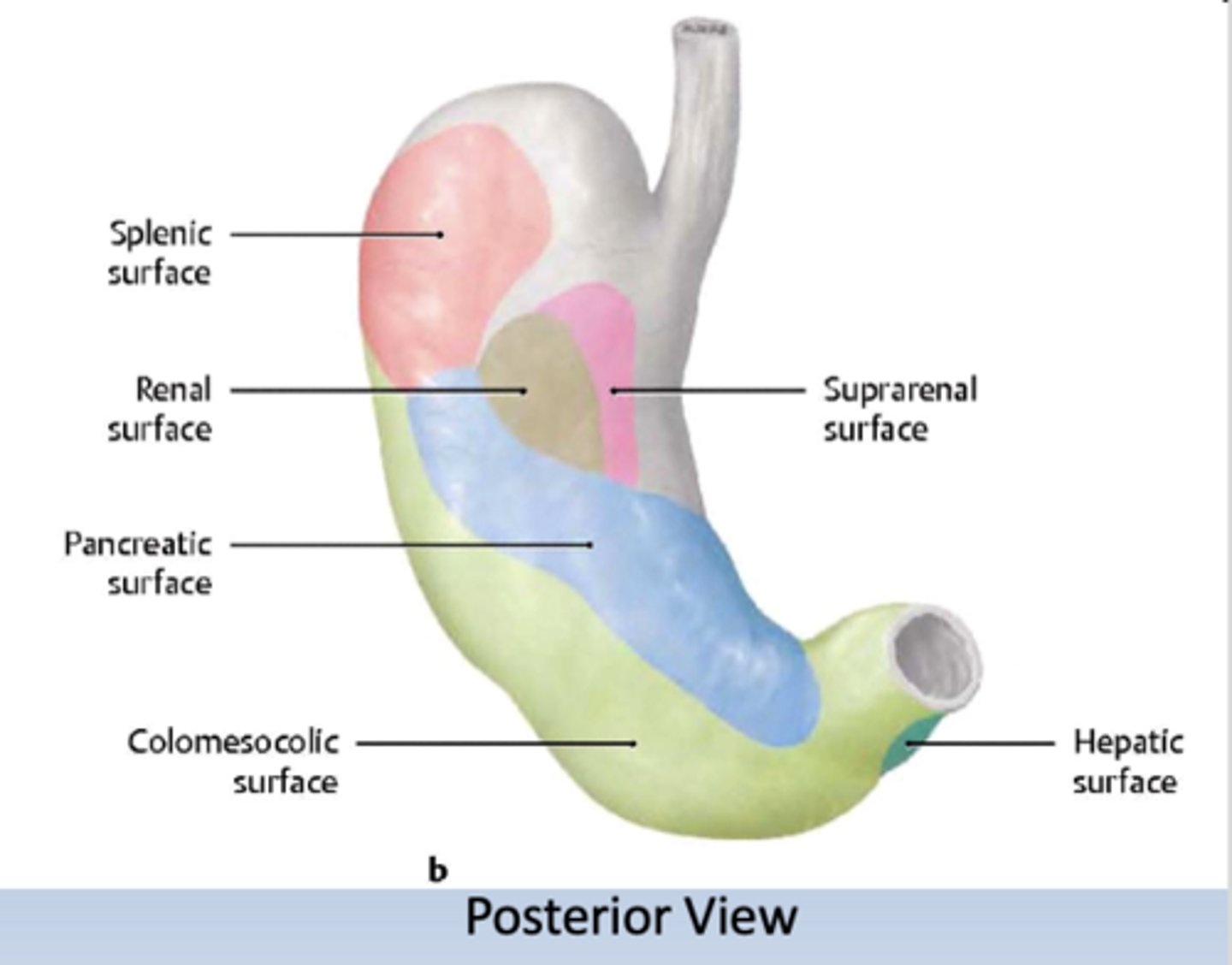
What are the major posterior relationships of the stomach?
pancreatic surface, splenic surface, renal surface, colomesolic surface, suprarenal surface and hepatic surface
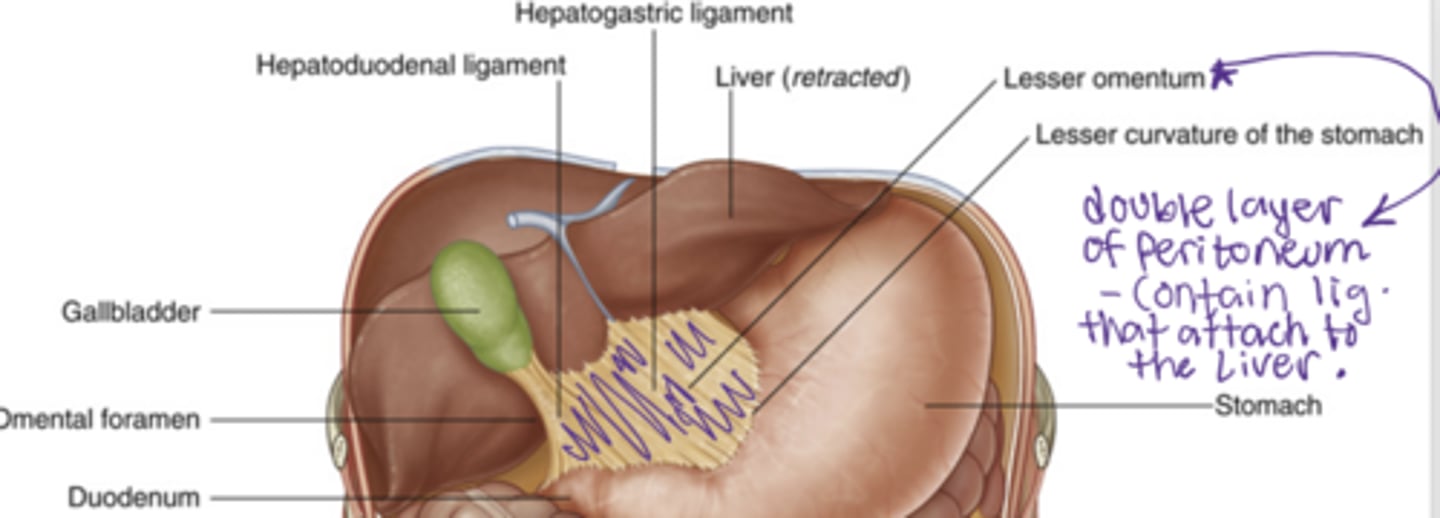
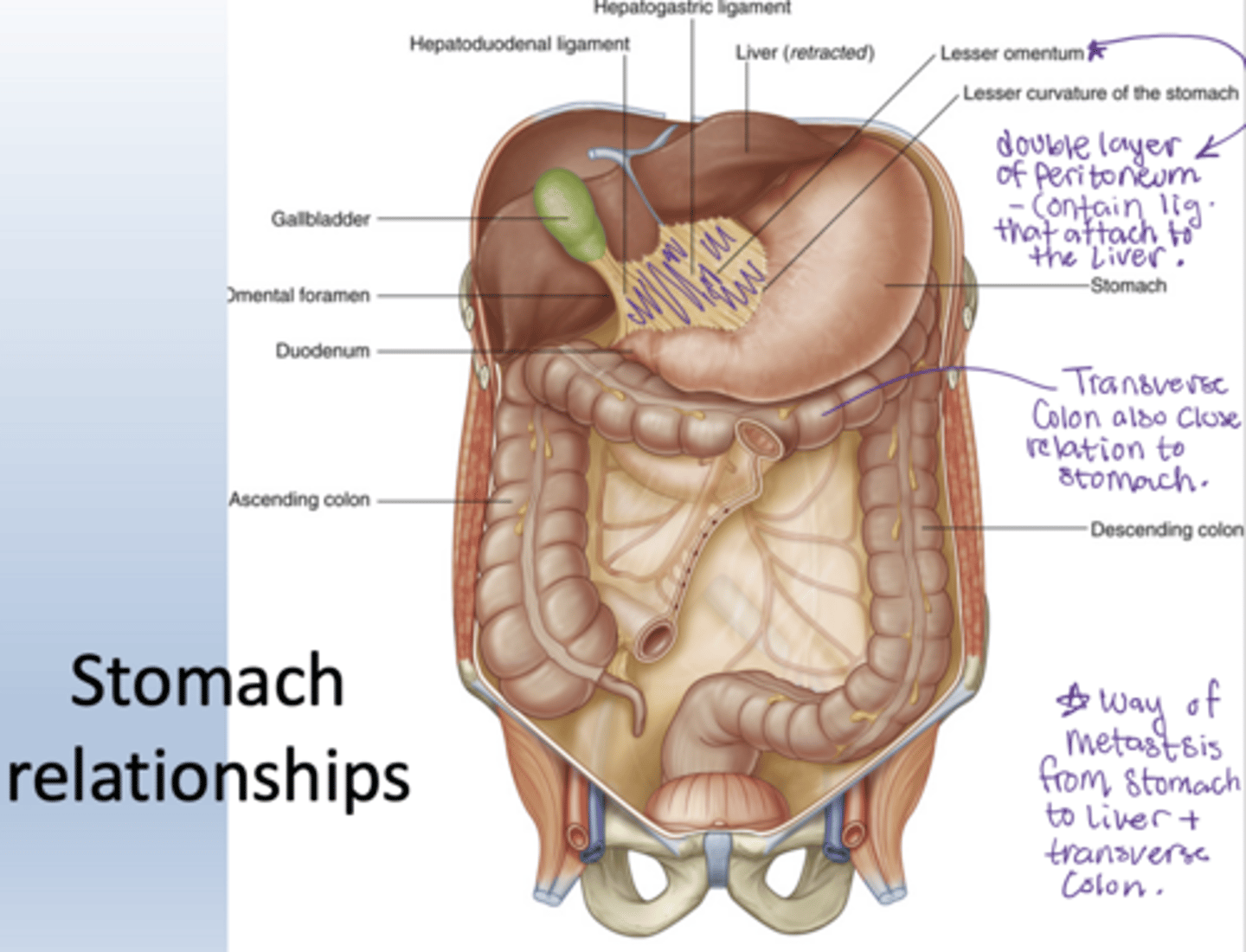
What is the lesser omentum?
double layer of peritoneum that connects the lesser curvature of the stomach and the proximal end of the duodenum to the liver
contain 2 ligaments
What ligaments are found within the lesser omentum?
hepatogastric ligament and hepatoduodenal ligament
What's found in close relation to the stomach and why is this clinically important
pancreas, transverse colon, liver
way of metastsis from stomach to liver and TRC (pancreas mainly with ulcers)
Why is the stomach considered intraperitoneal?
It is completely covered by visceral peritoneum and suspended by mesenteries.
What are the three parts of the small intestine?
duodenum, jejunum, ileum (DJI)
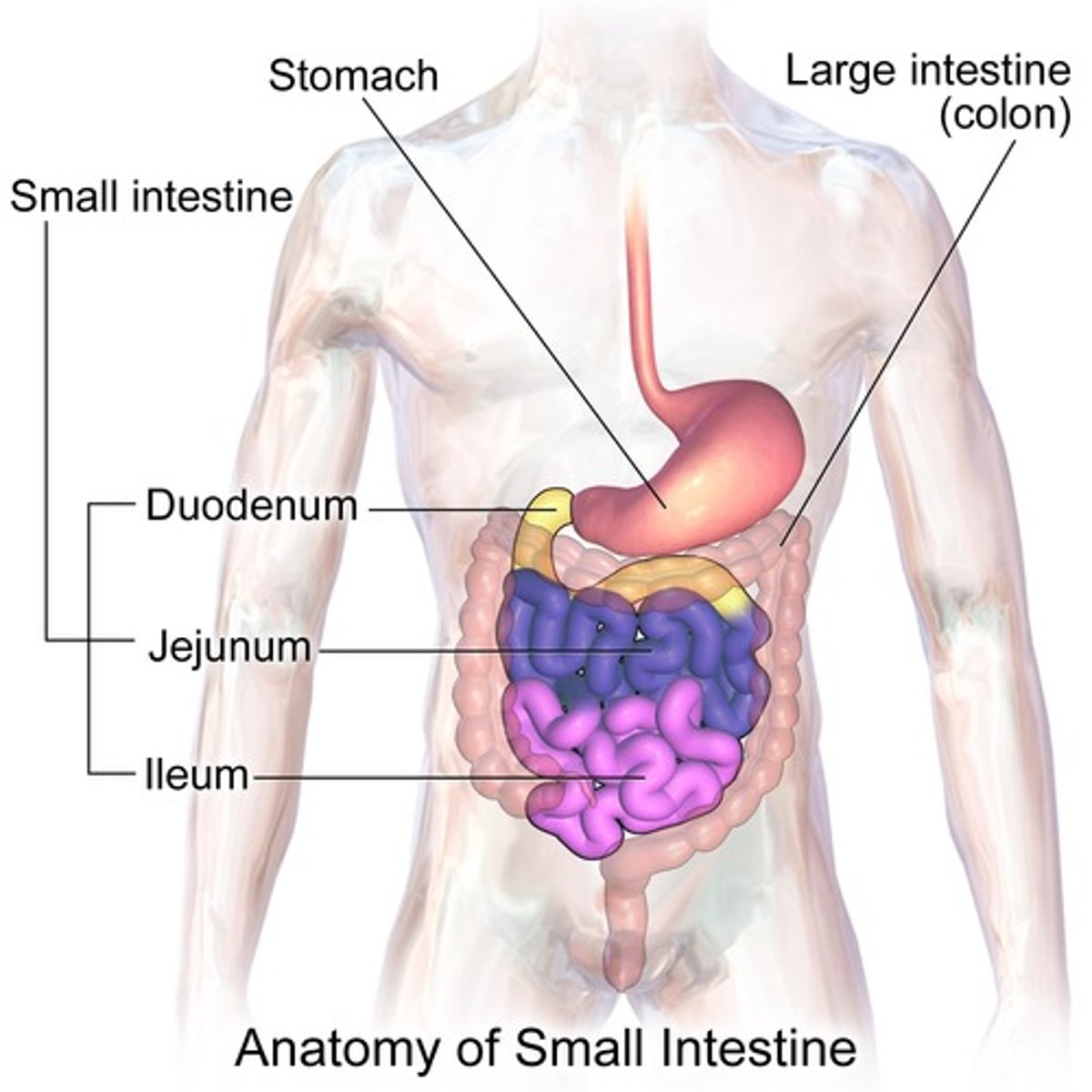
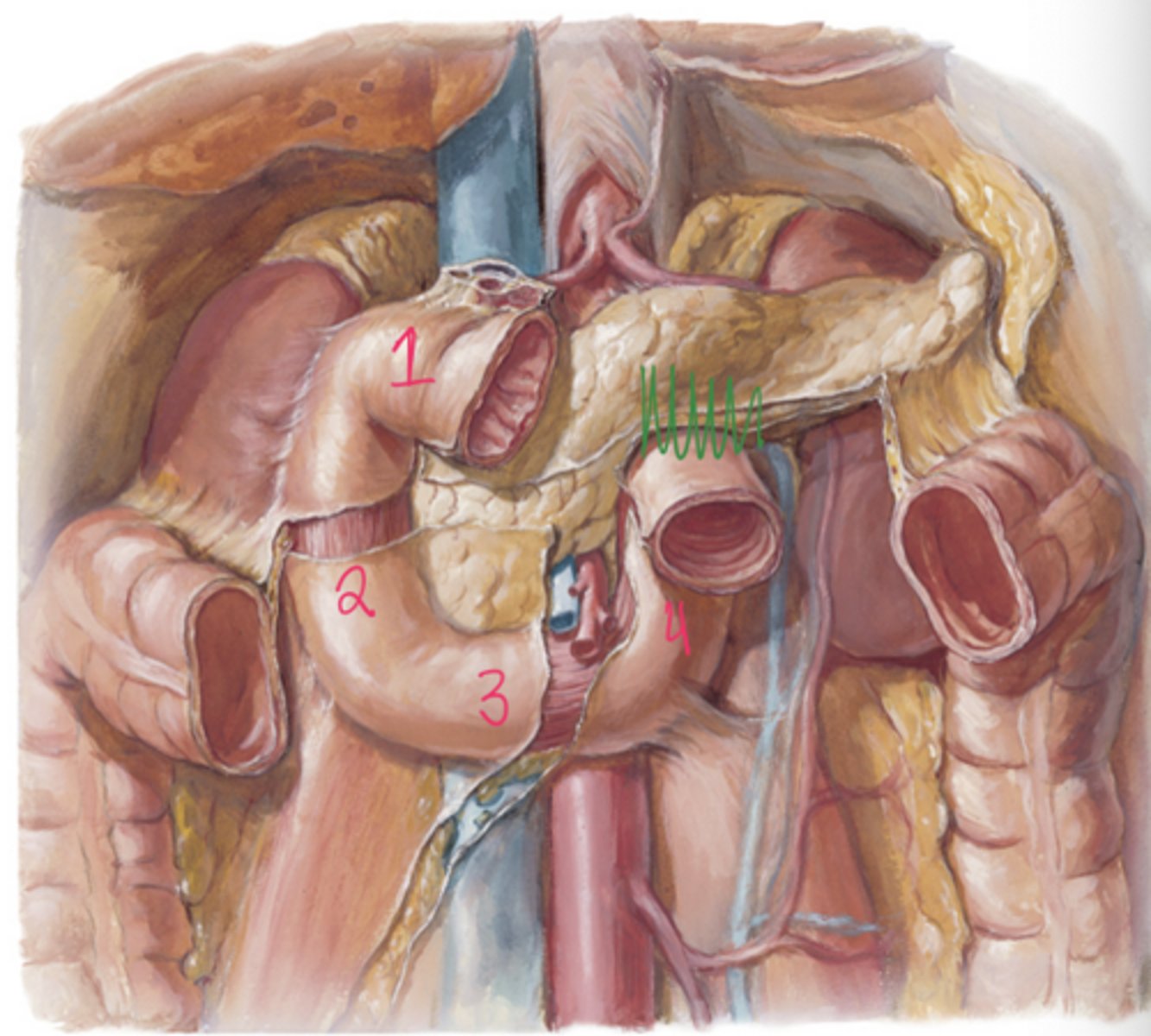
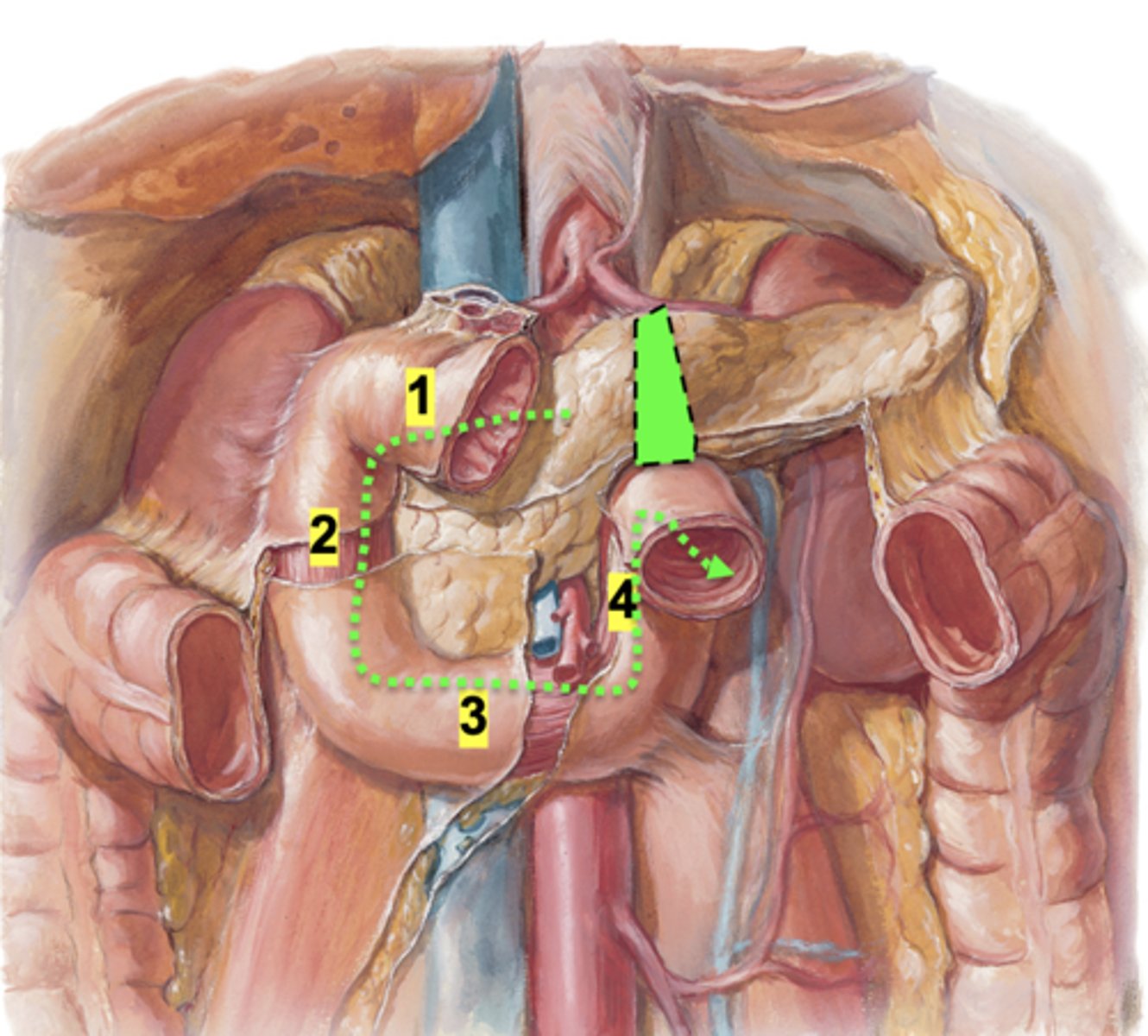
What are the four parts of the duodenum?
Superior (1st), descending (2nd), inferior (3rd), and ascending (4th) portions.
Where are ulcers most commonly found?
stomach and superior part of the duodenum
What is the ligament of trietz?
a thin band of tissue (peritoneum) that connects and supports the end of the duodenum (ascending part) and beginning of the jejunum in the small intestine.
It's also called the suspensory muscle of duodenum
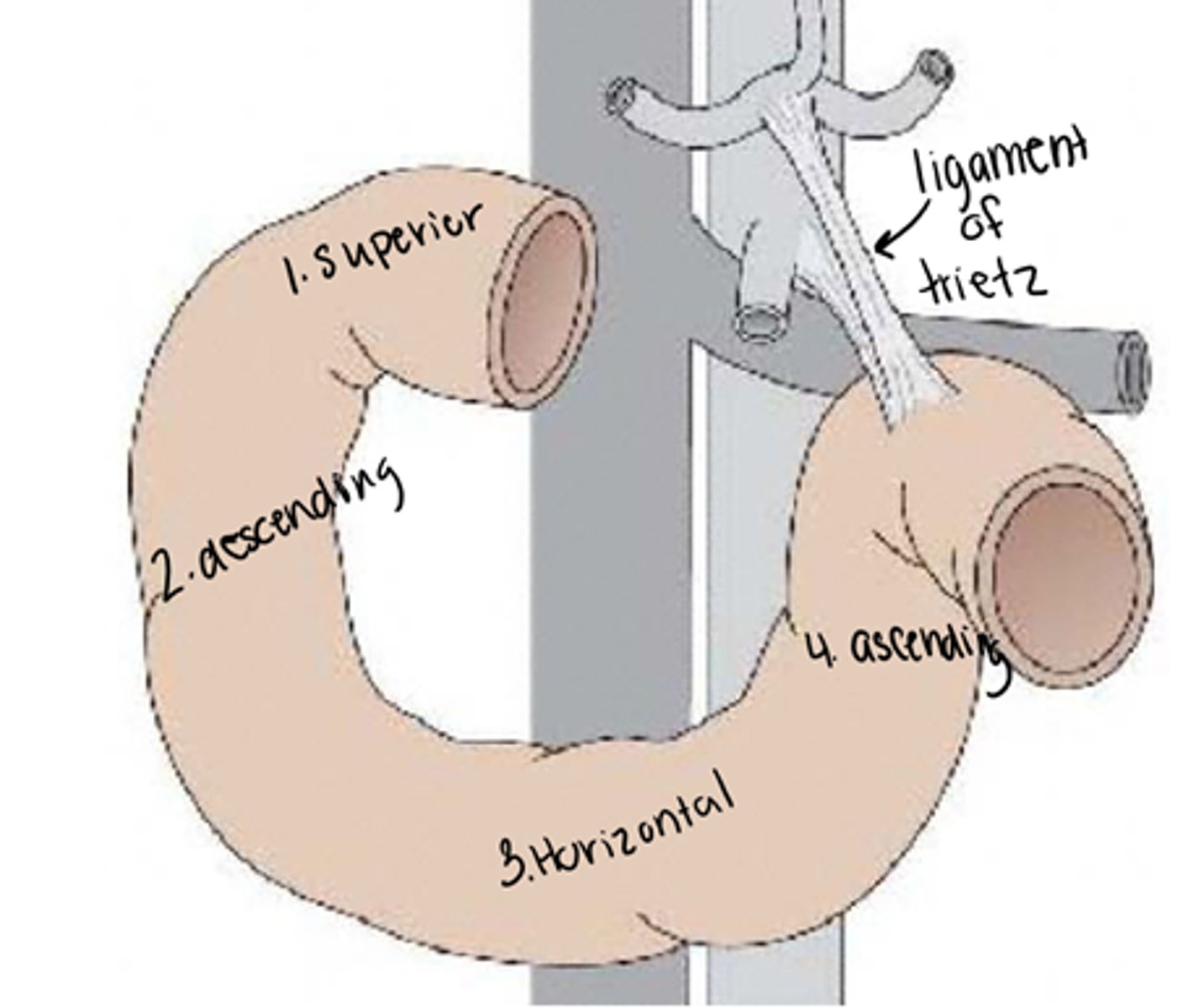
What is the clinical importance of the ligament of trietz?
Injury before the ligament - GI blood appear dark, tarry stool (melena)
Injury after the ligament - GI blood appear bright red
How do you identify the duodenojejunal junction on imaging?
Located left of midline at ligament of Treitz where bowel becomes intraperitoneal jejunum.
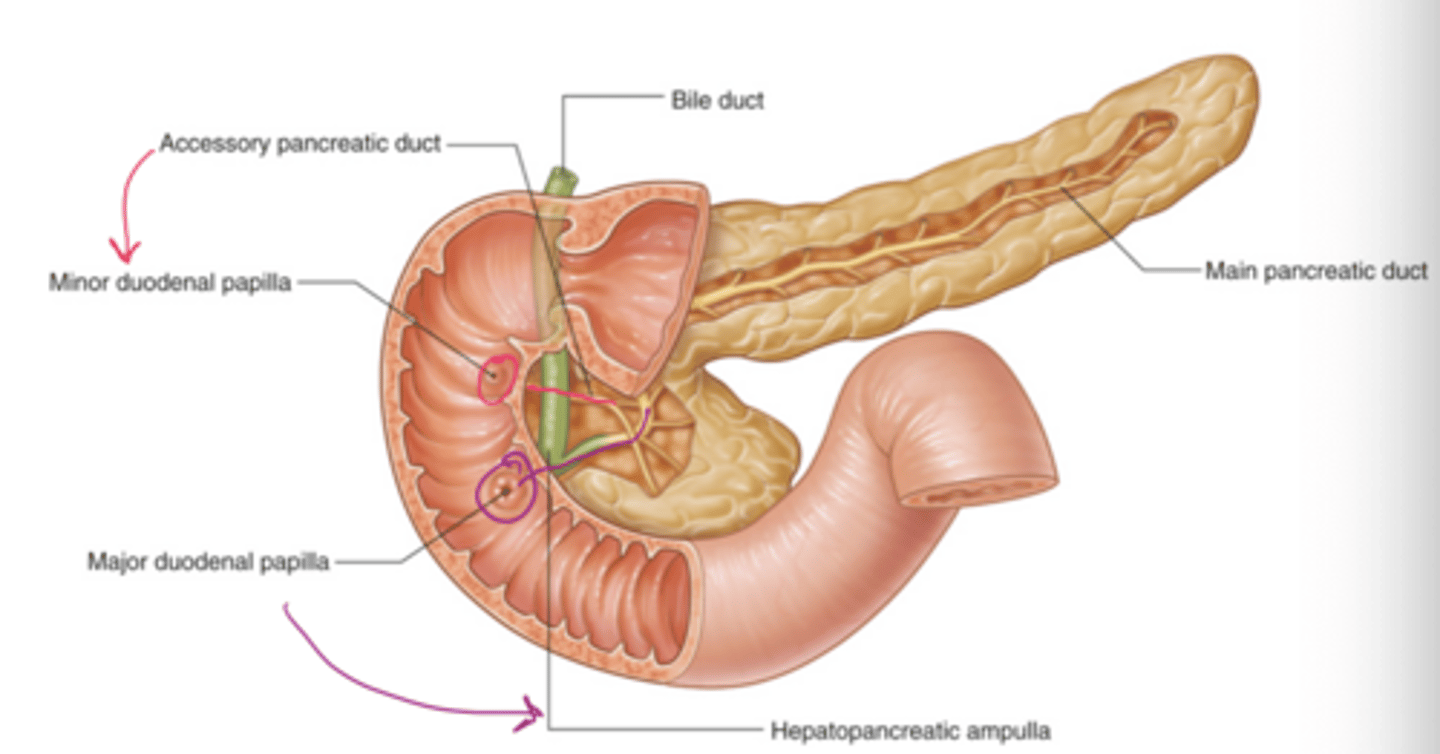
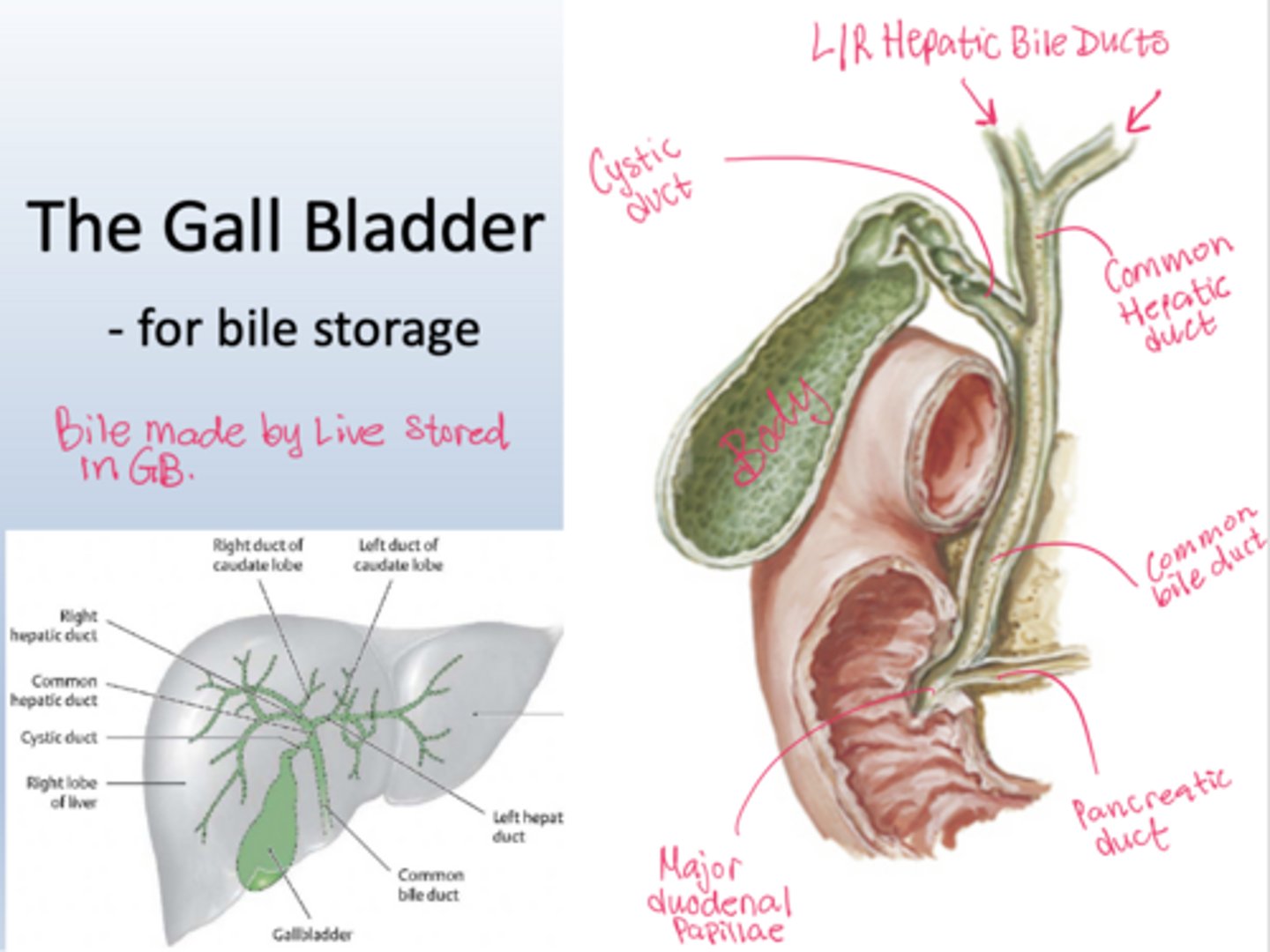
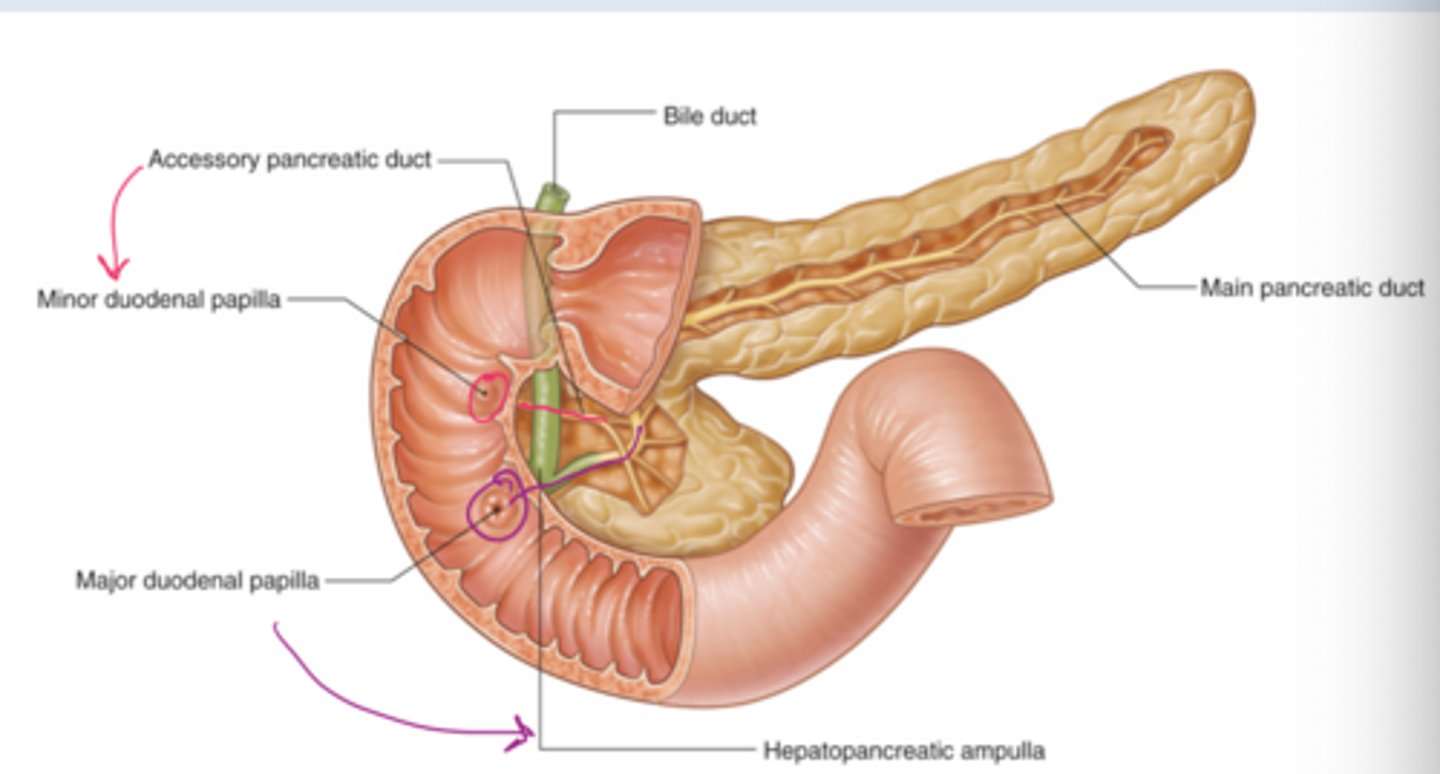
Where do the pancreatic and bile ducts enter the duodenum?
They enter the second (descending) part of the duodenum at the major duodenal papilla
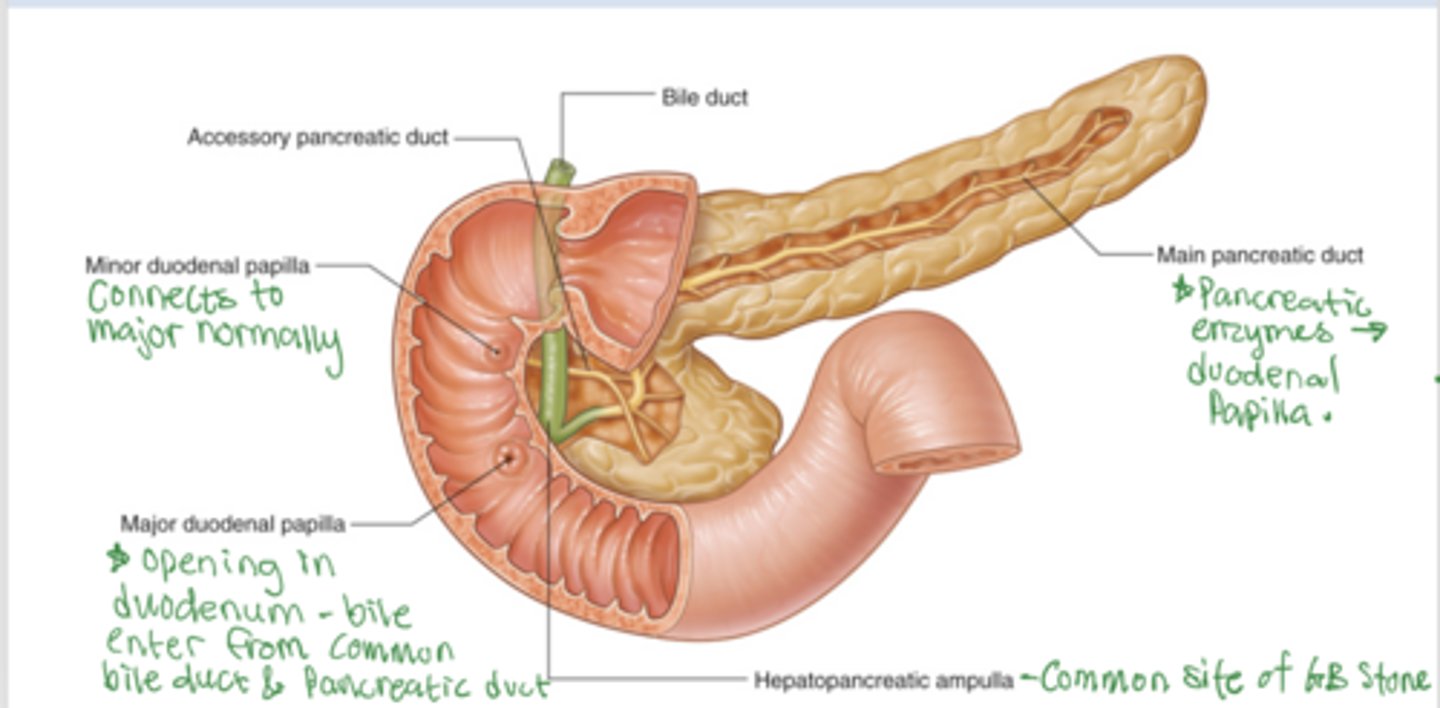
What is the accessory pancreatic duct?
smaller duct that empties directly into duodenum via minor duodenal papillae (NOTICE this is ONLY pancreatic juices NOT BILE)
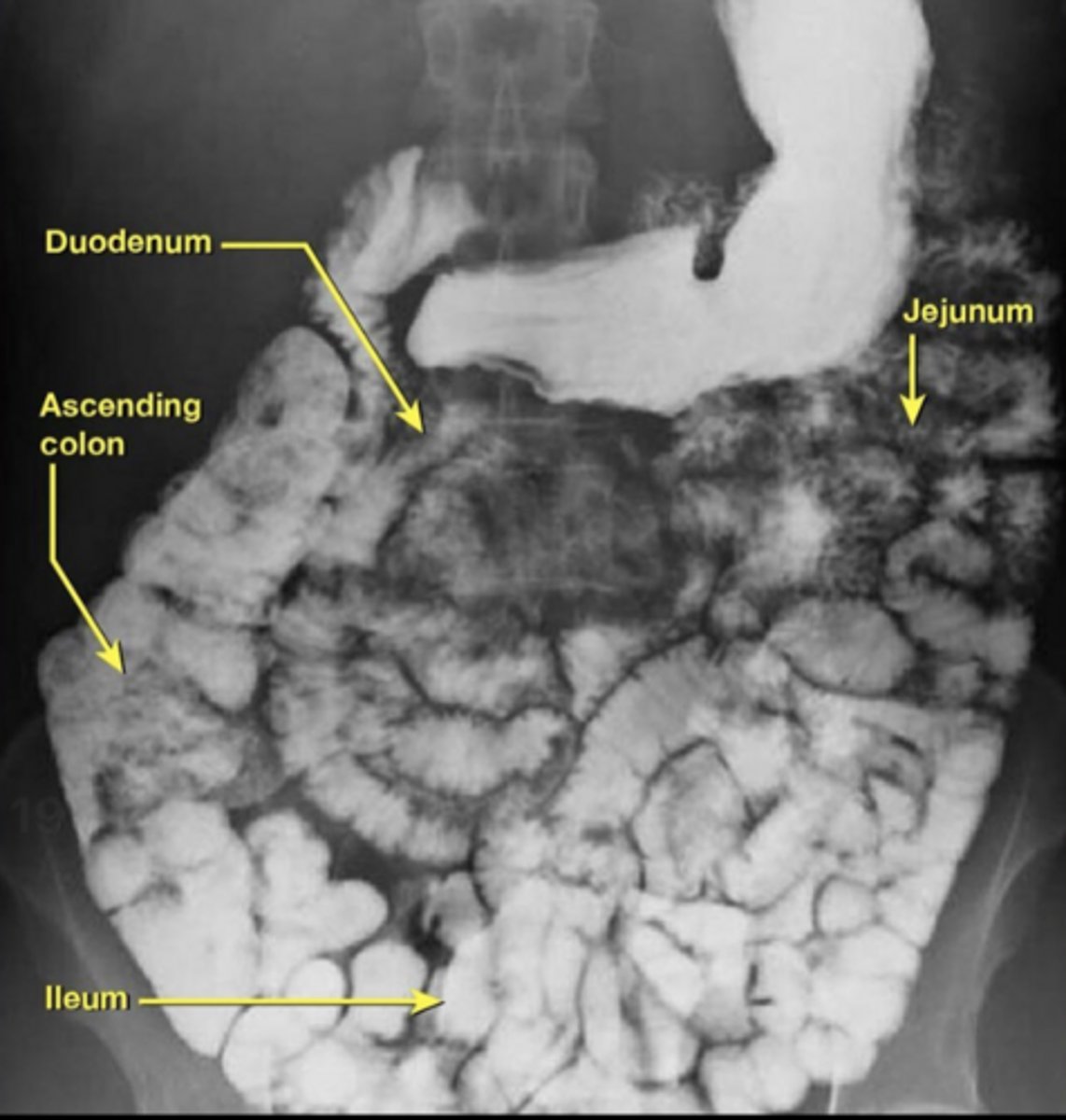
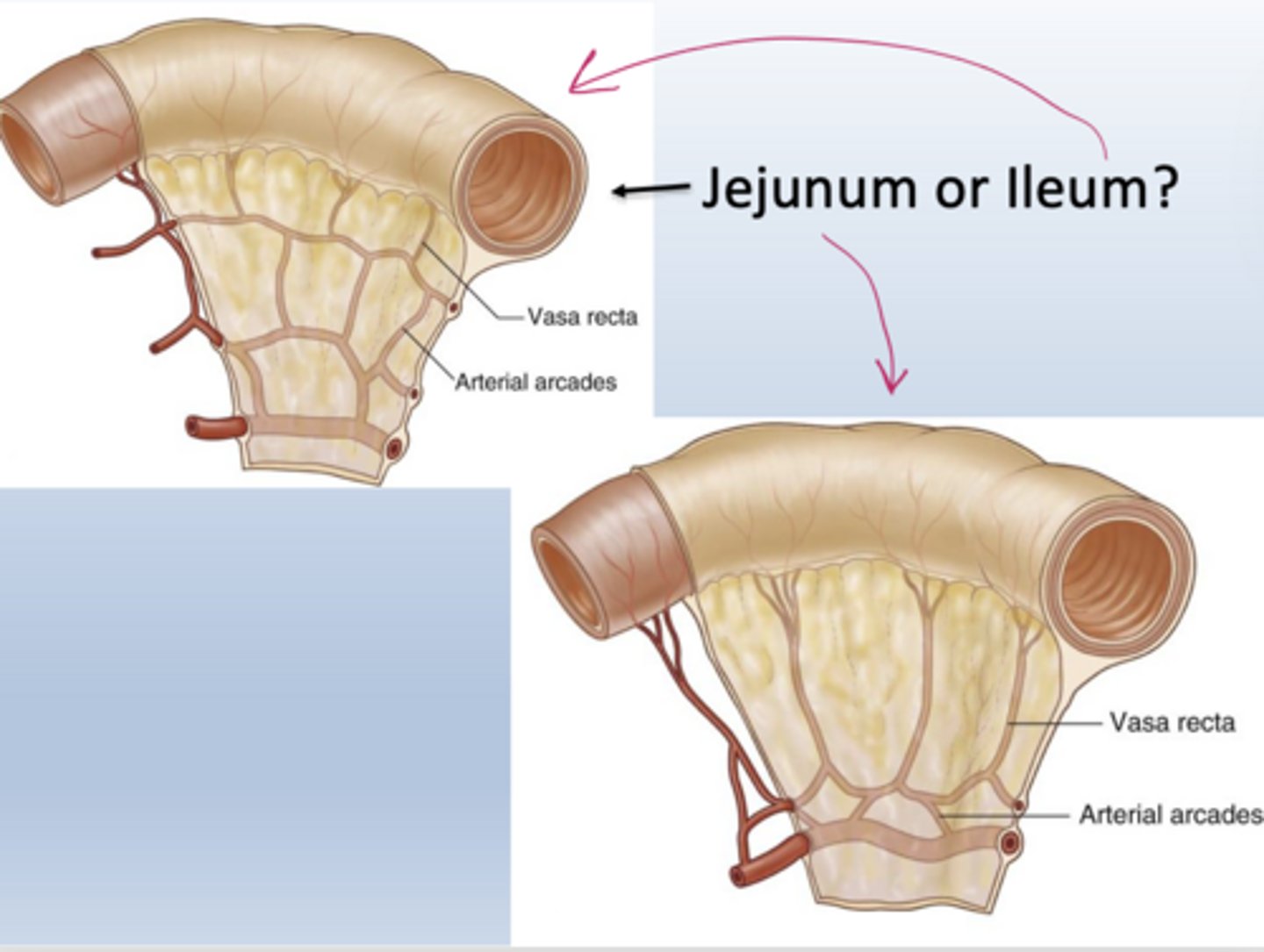
How can you distinguish jejunum from ileum anatomically?
Jejunum has a larger diameter, numerous mucosal folds, long vasa recta, and fewer arterial arcades.
Ileum has a smaller diameter, fewer folds, short vasa recta, and more complex arcades.
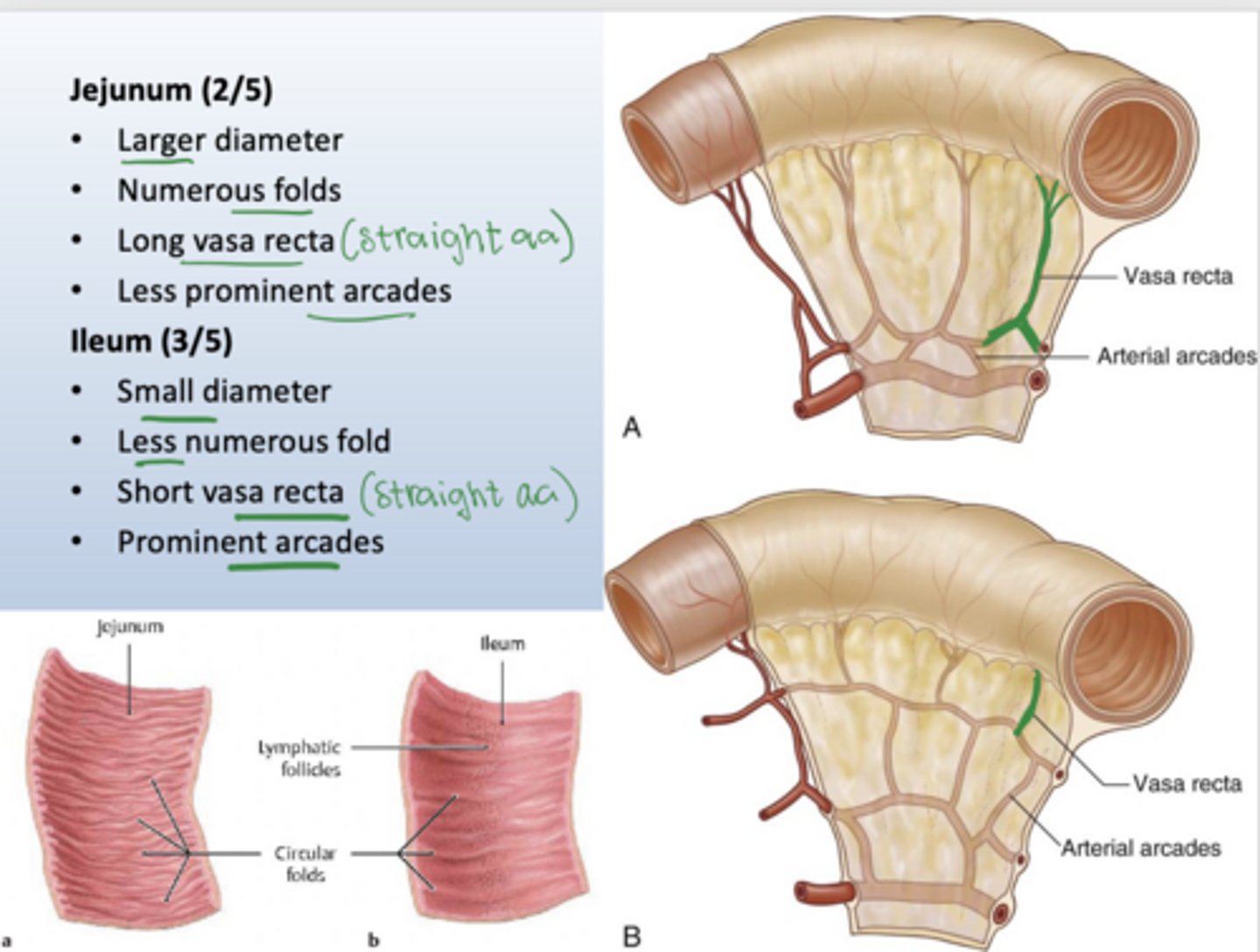
On imaging, how do you distinguish jejunum from ileum?
Jejunum shows thick walls and numerous folds; ileum has smoother walls and fewer folds.
What is the ileocecal junction?
The junction where the ileum empties into the cecum of the large intestine, controlled by the ileocecal valve.
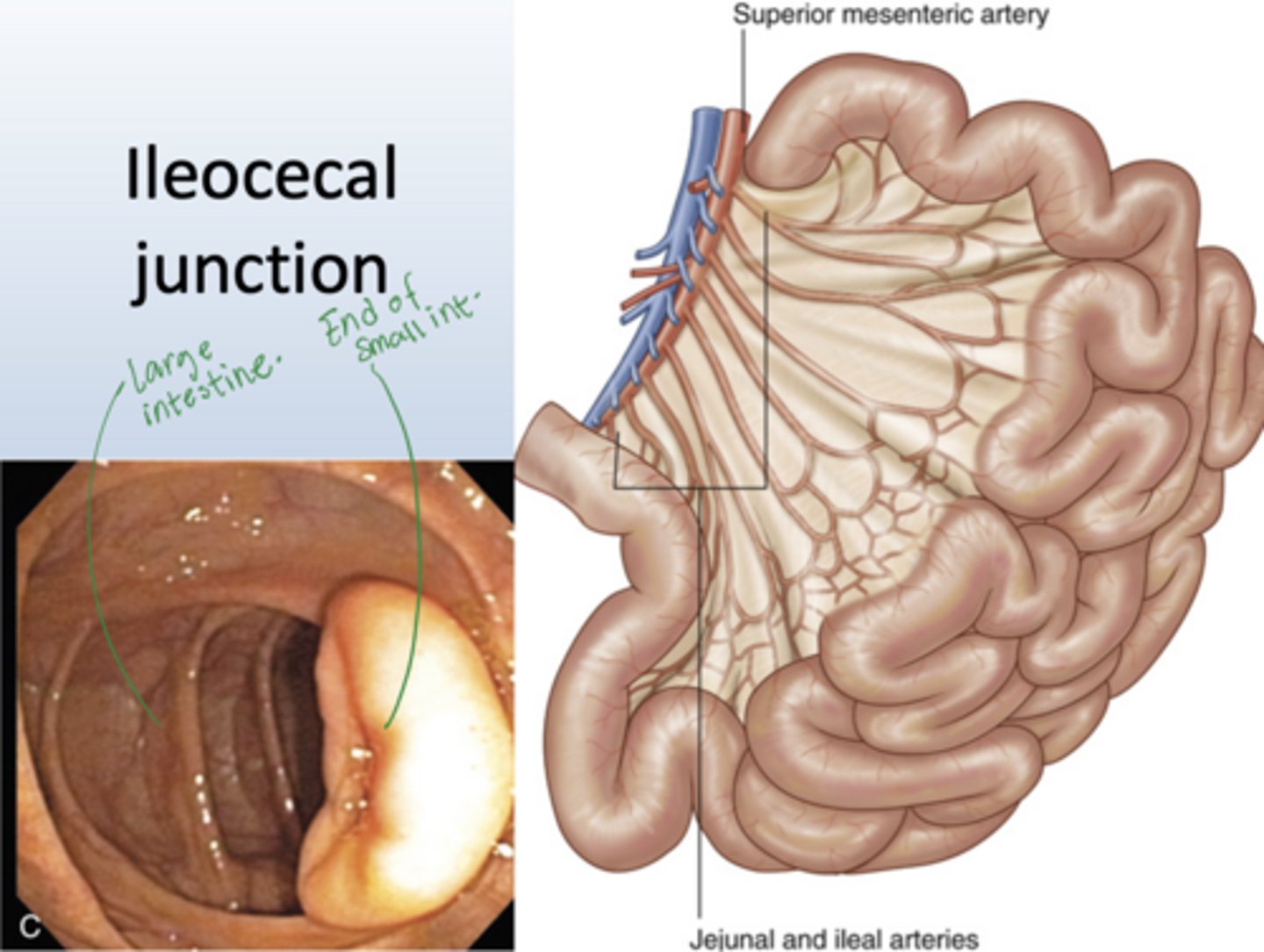
Where is the ileocecal junction seen anatomically?
In right lower quadrant where terminal ileum enters cecum.
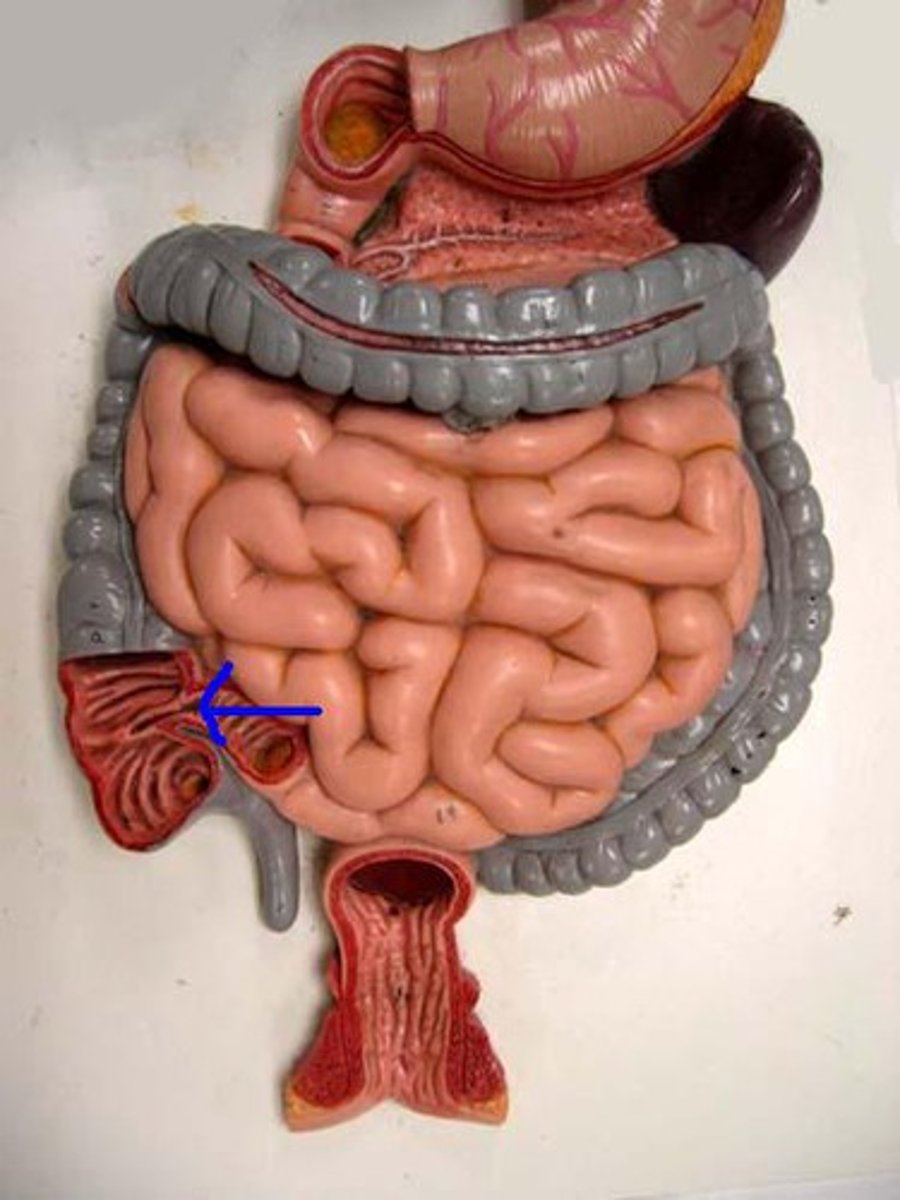
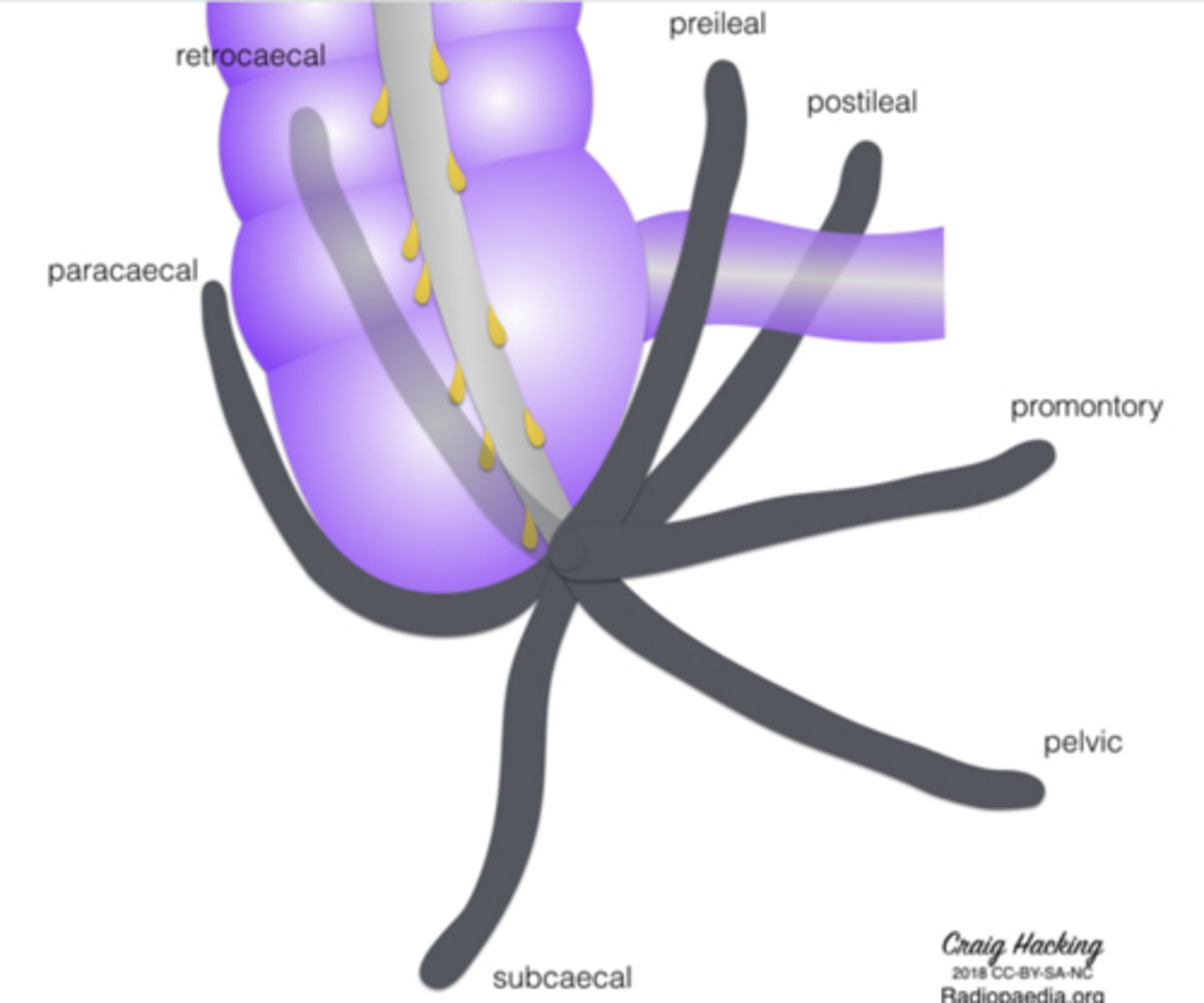
Why is appendiceal position clinically variable?
The appendix can occupy several positions, altering pain location and exam findings in appendicitis.
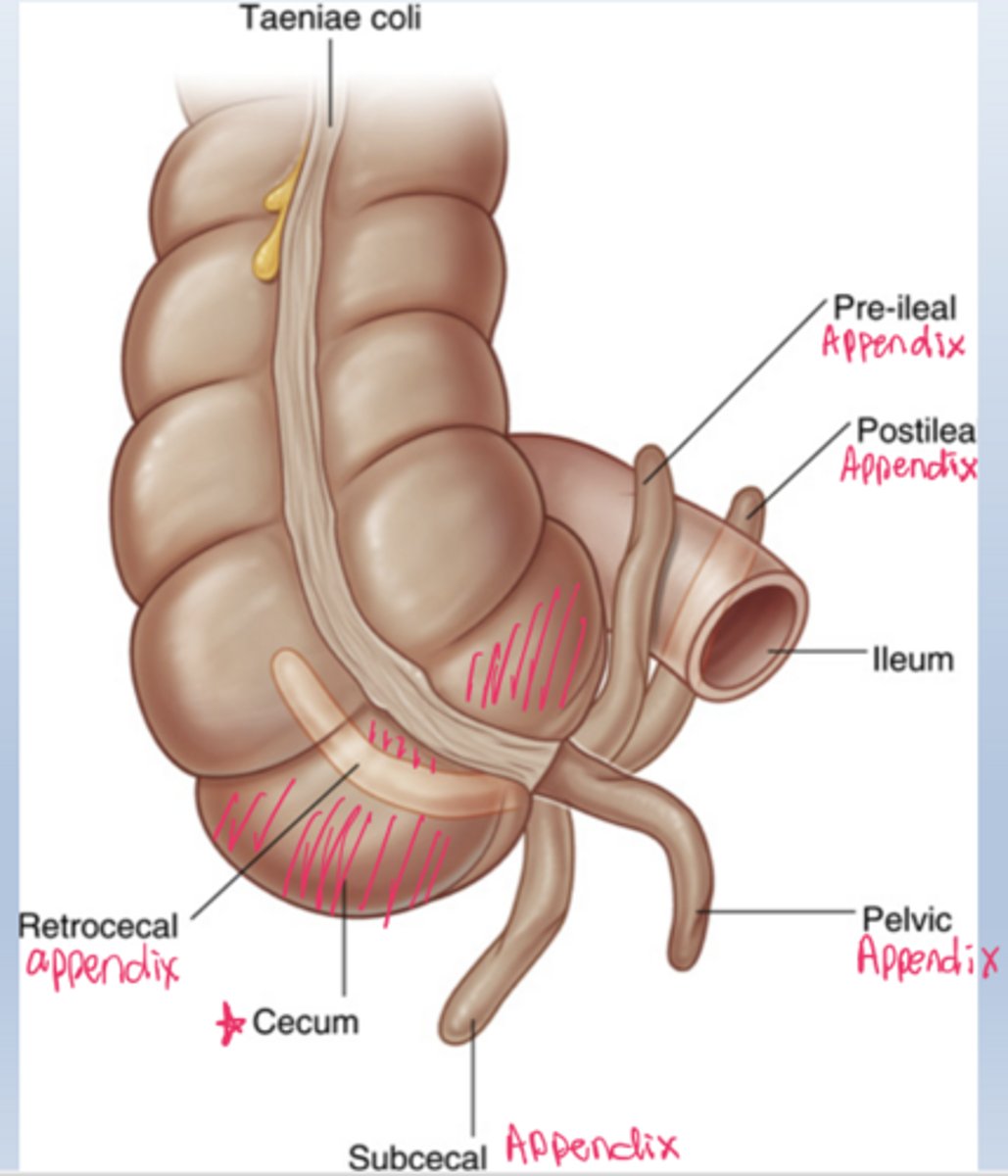
What appendiceal positions may be seen on imaging?
Pelvic
Retrocecal
Preileal
Subcecal
Subileal
explaining variable appendicitis pain.
Think Please Remember People Study Seriously
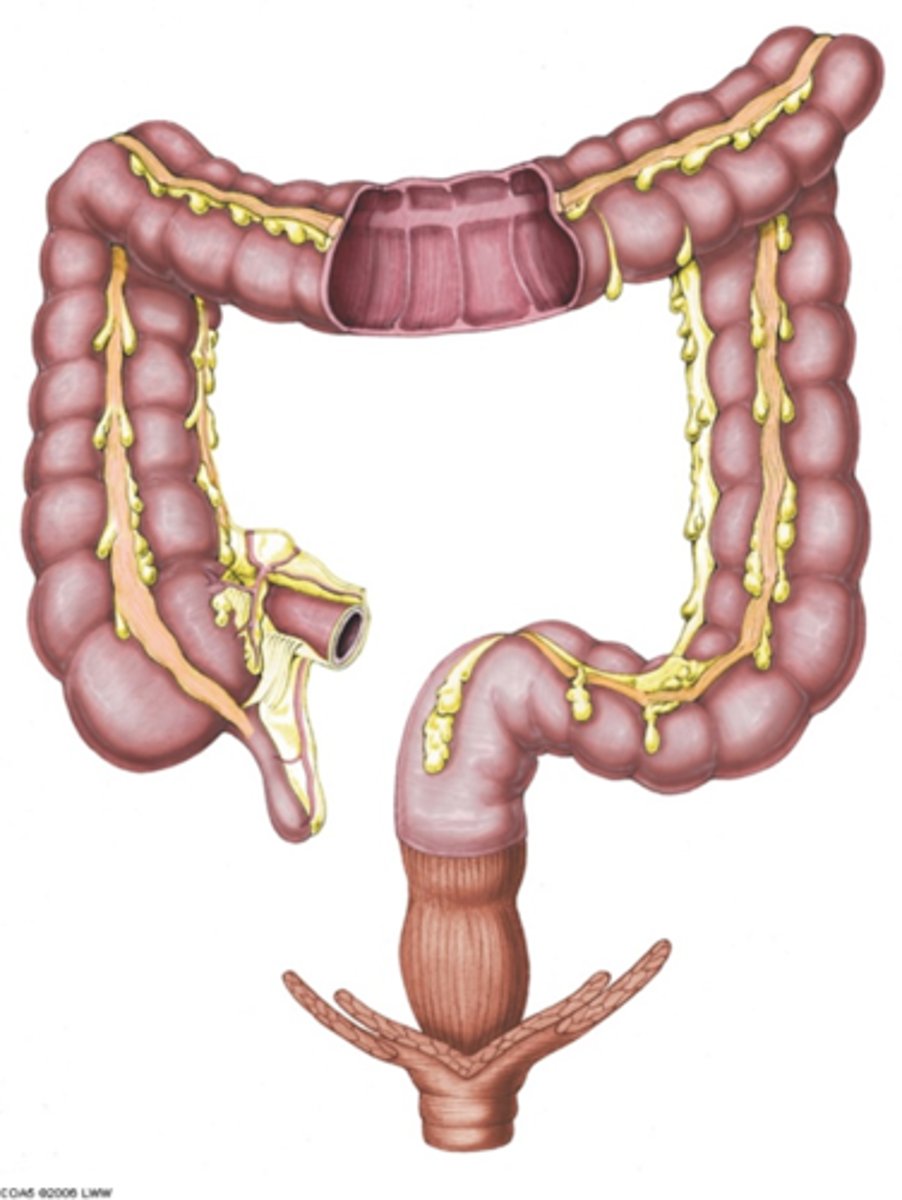
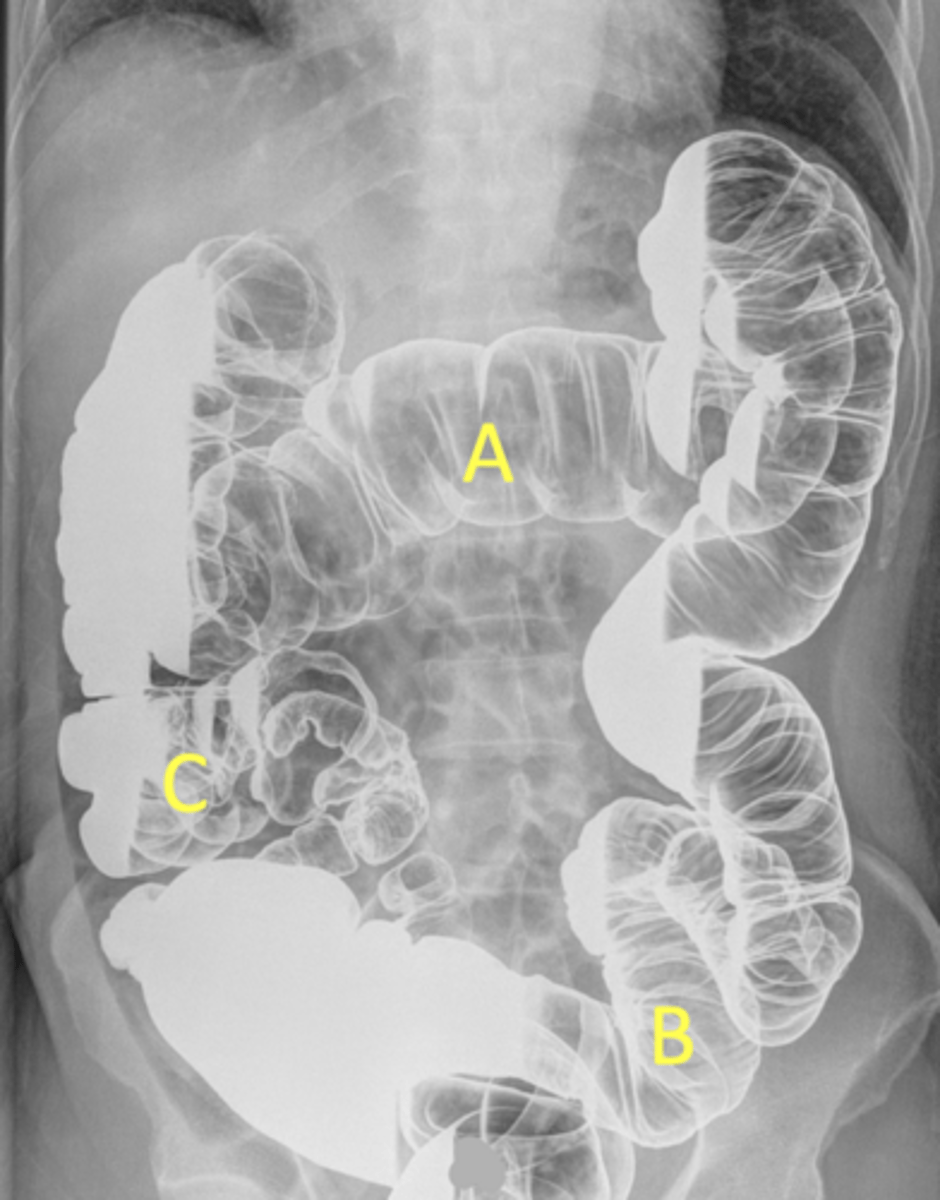
Be able to label the different regions of the colon (large intestine)
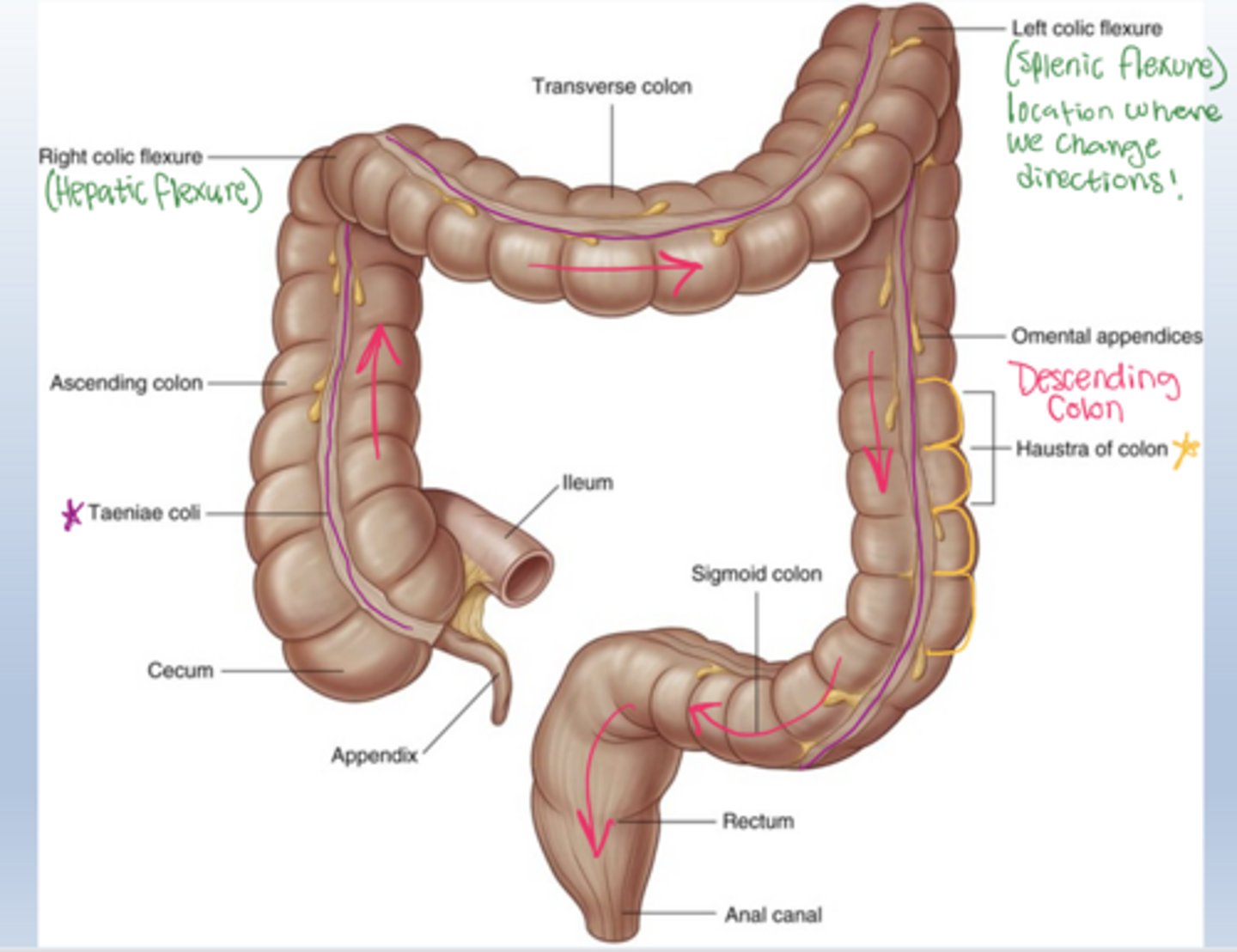
What are the right colic and left colic fissure?
Right colic (hepatic) fissure part of colon in contact with the liver
Left colic (splenic) fissure part of colon in contact with spleen
also areas of colon where it will change directions
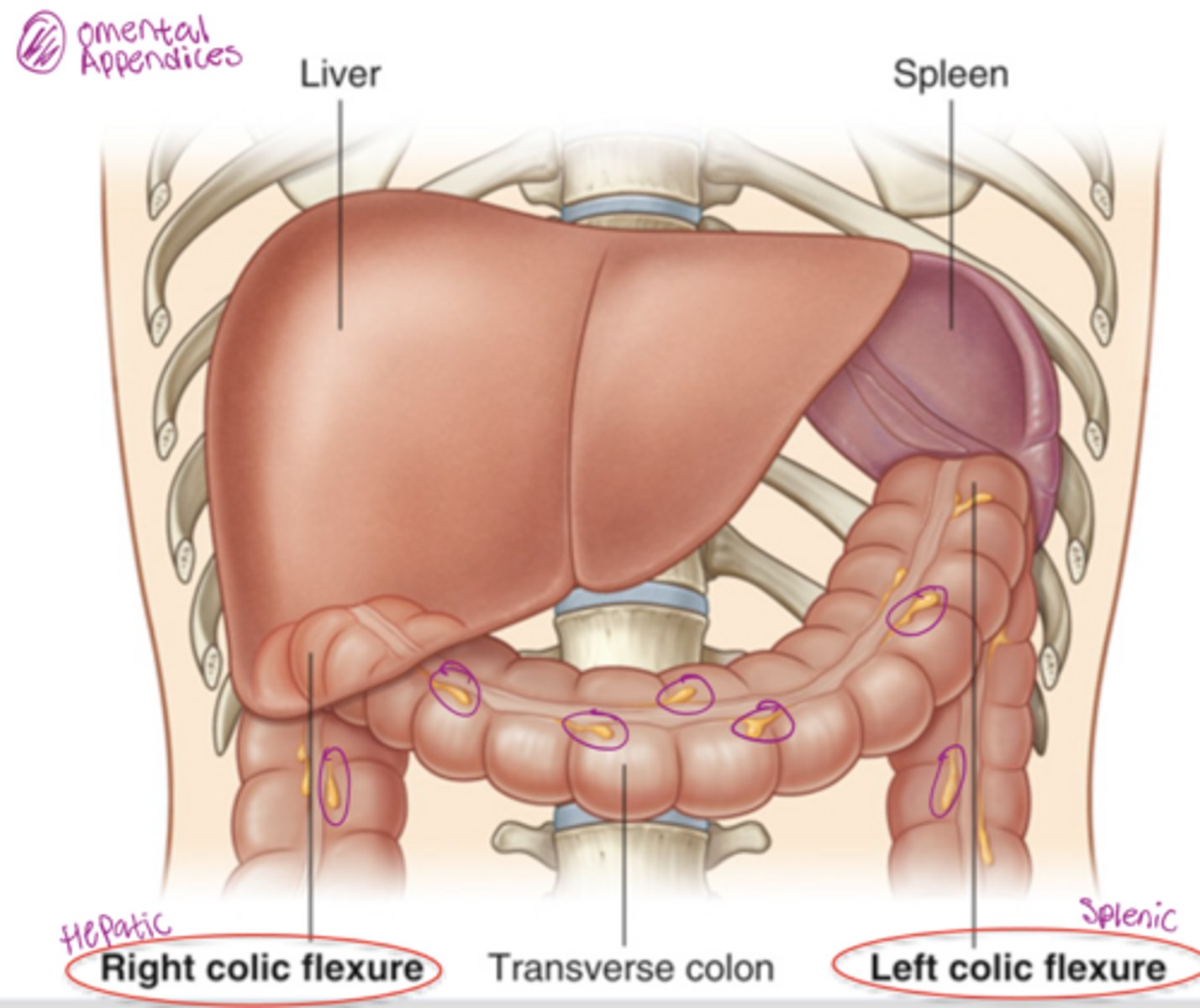
What are omental appendices?
fatty projections on the wall of the colon (large intestine)
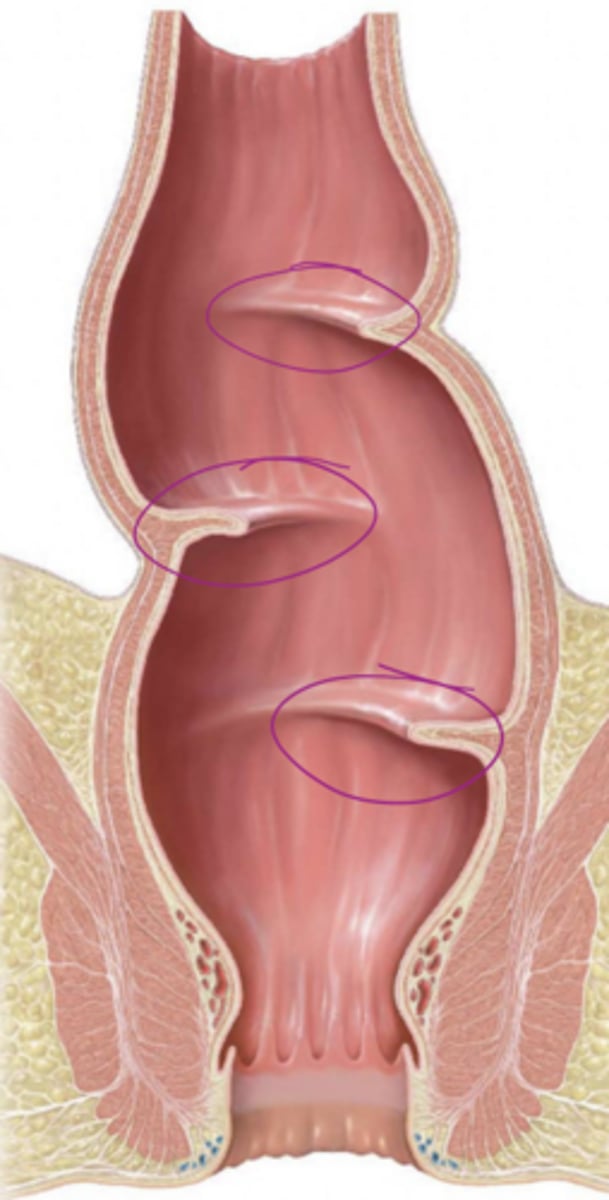
What are transverse rectal folds and why do they matter?
2-4 semilunar indentations that control the urge of defecation
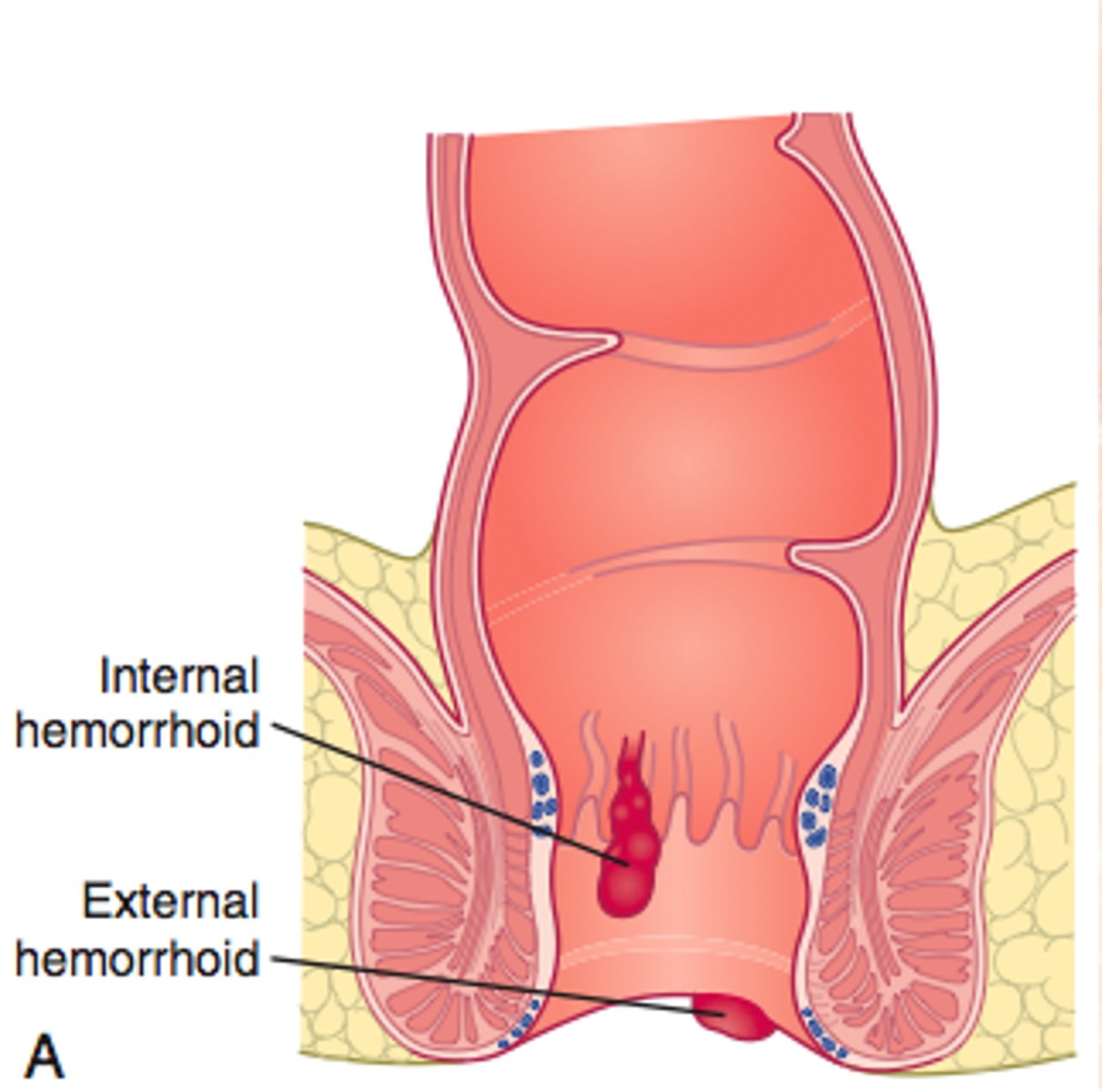
What is the pectinate line and why is it clinically important?
AKA Dentate line - it marks the transition to distinct changes in neurovascular supply, lymphatic drainage, and embryologic origin, making it essential for understanding pain, cancer spread, and hemorrhoid location
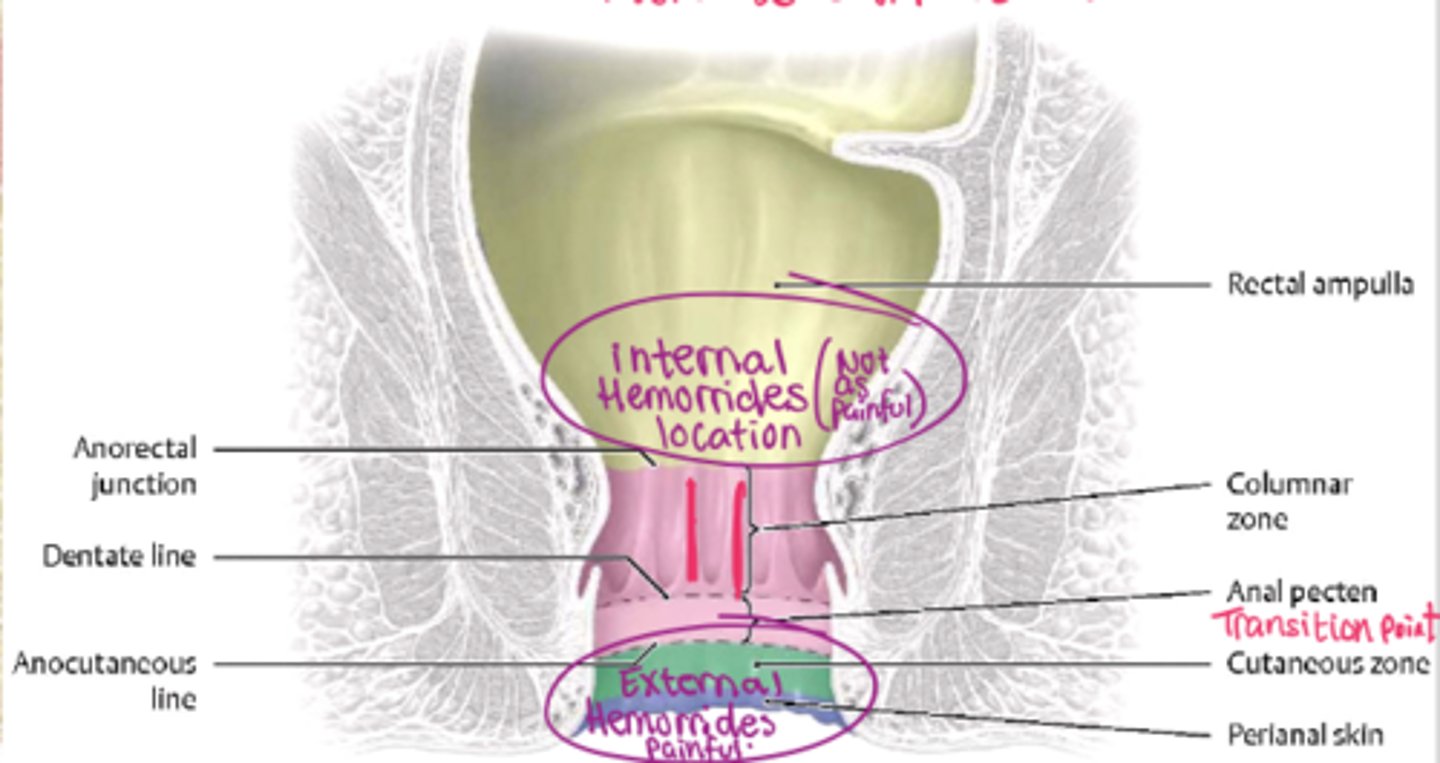
What are internal hemorrhoids?
-prolapses of rectal mucosa containing superior rectal veins. -They occur above the pectinate line.
Painless bleeding, autonomic nerve supply
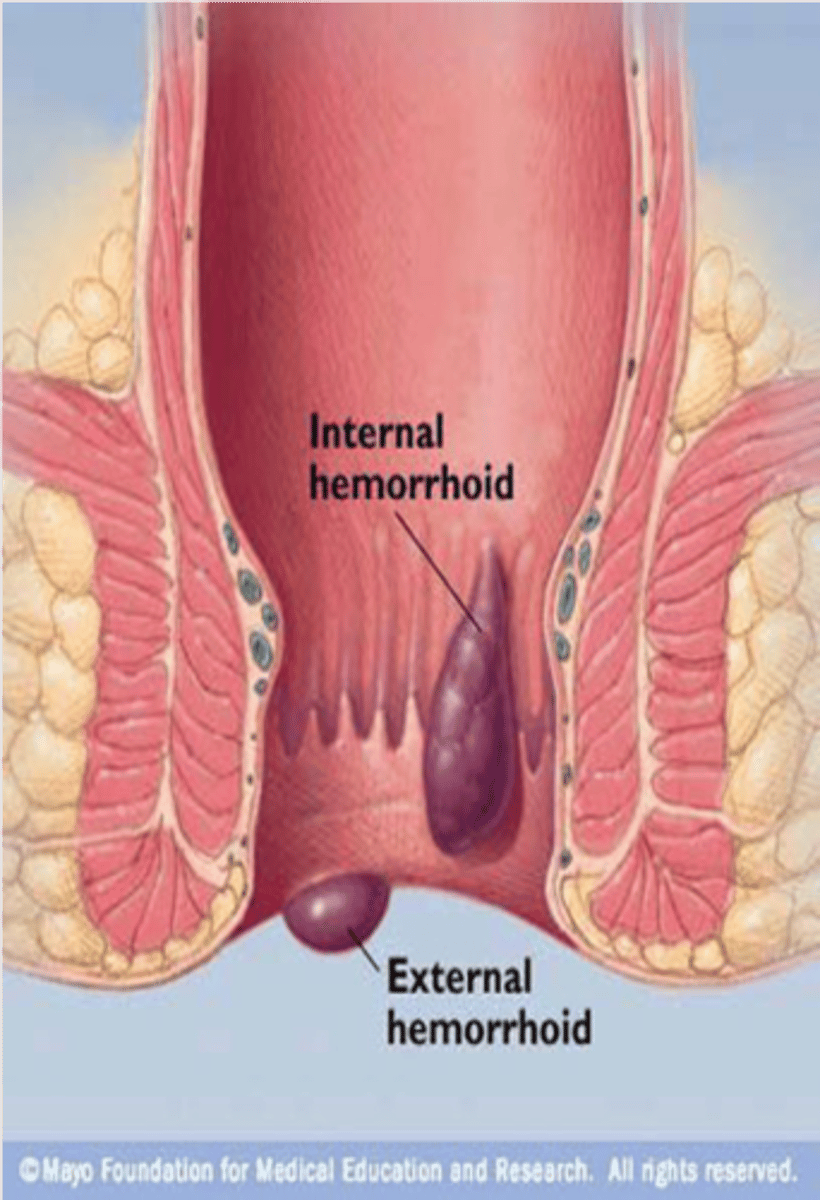
What are external hemorrhoids?
- involve blood clots within veins of the external rectal plexus
- covered by skin
- somatic inn. - PAINFUL
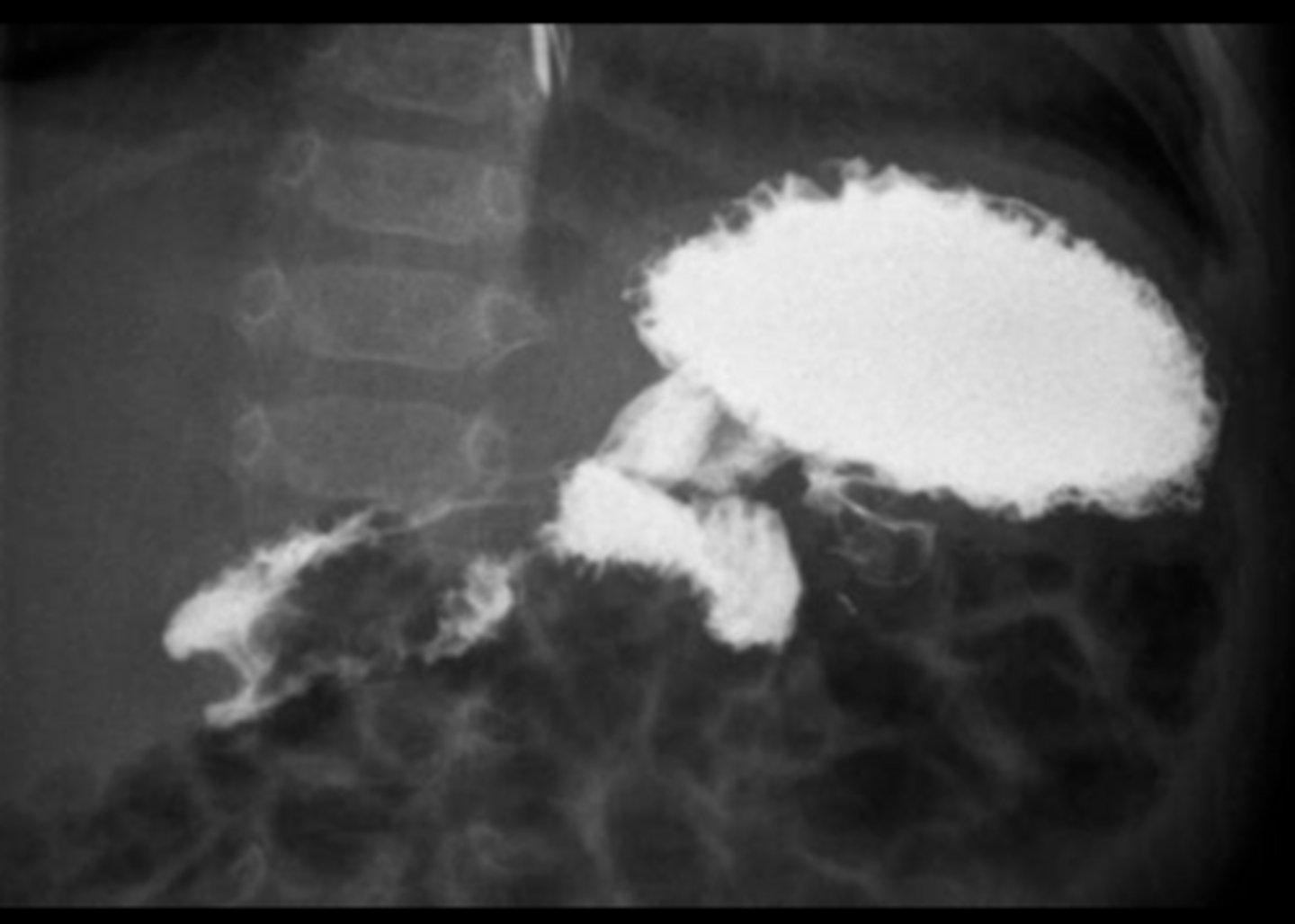
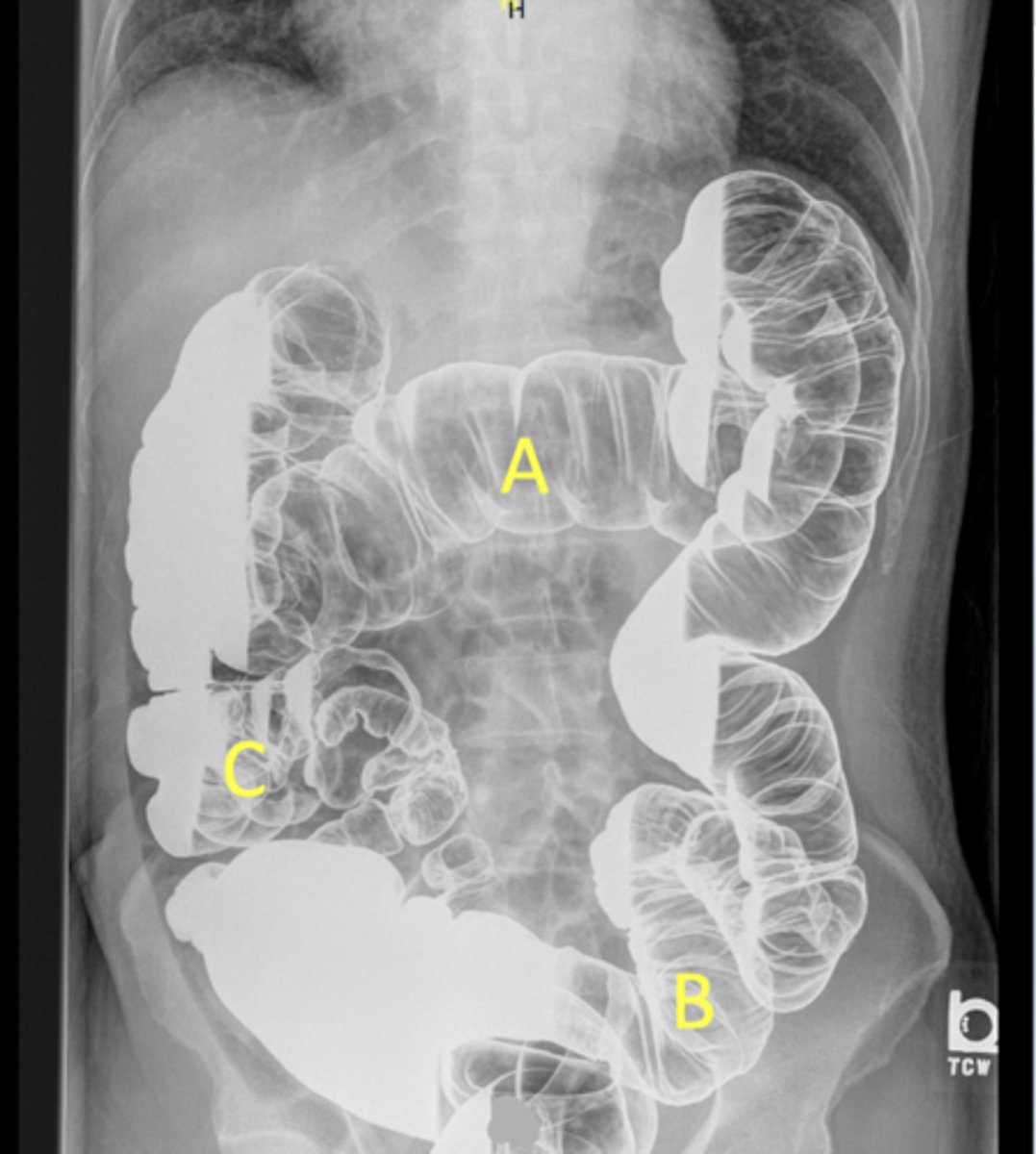
A - Transverse colon
B - Sigmoid colon
C - Cecum/ascending colon/iliocecal junction
pt is on their side due to seeing white fluid and haustra
Label the radiograph
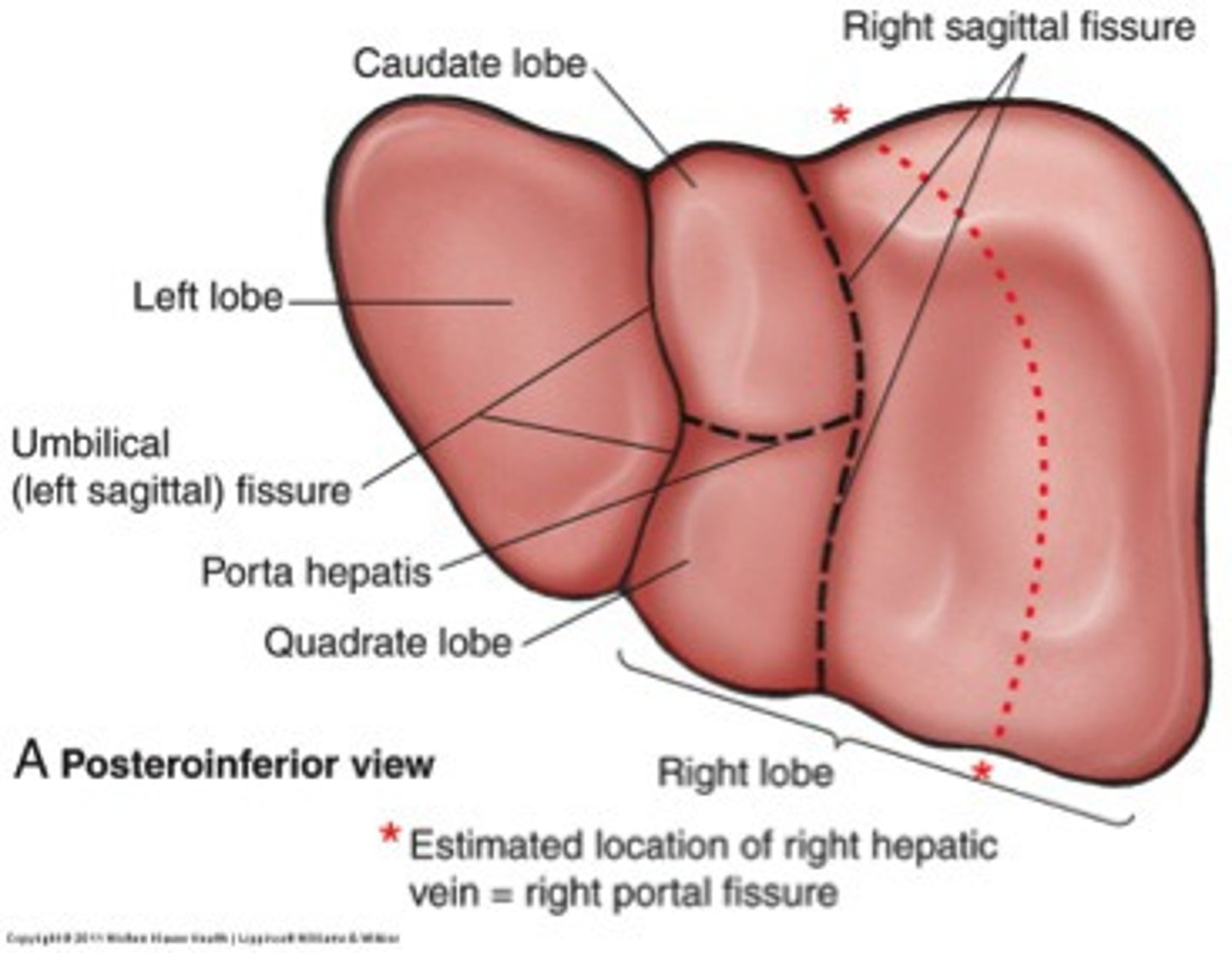
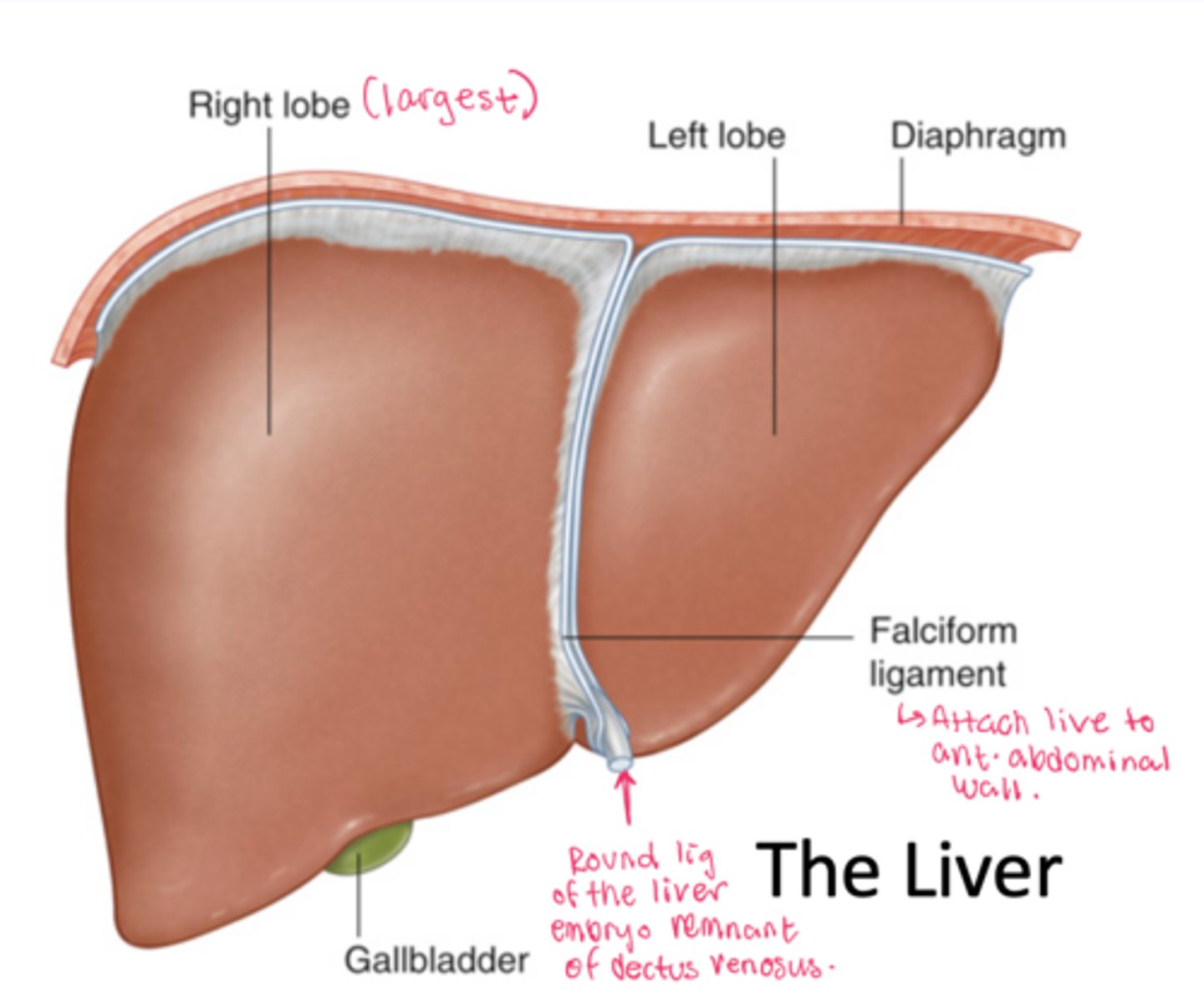
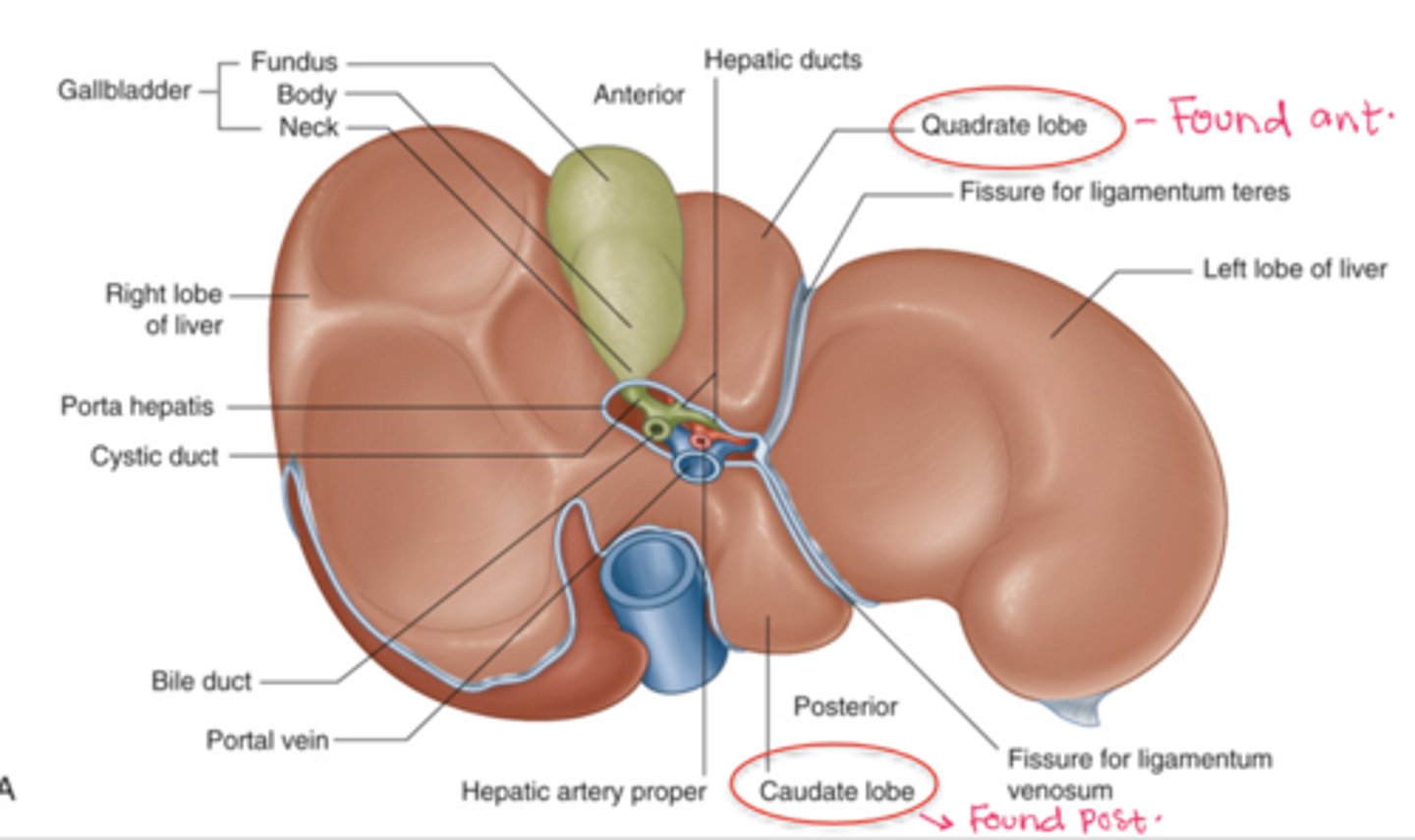
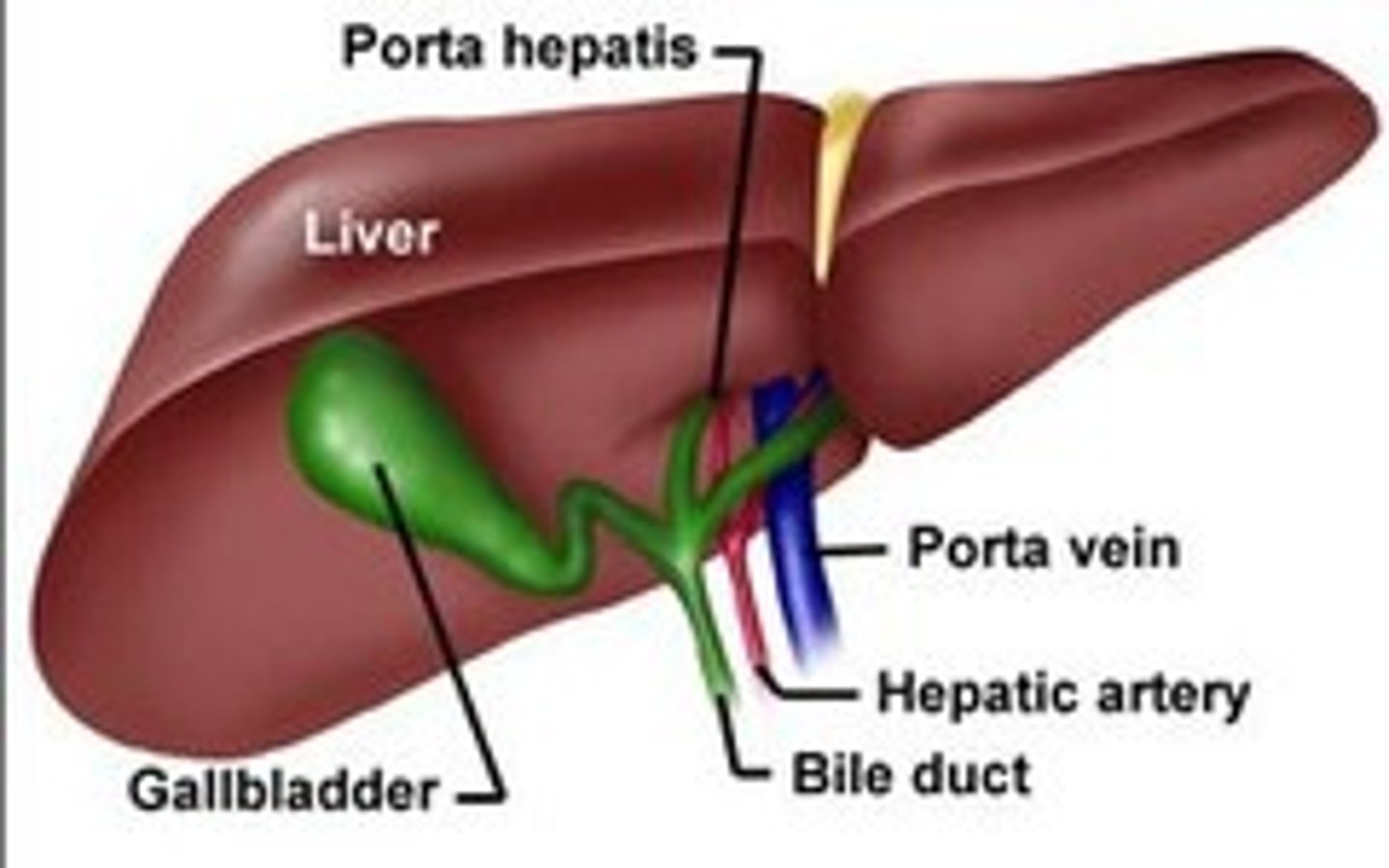
What are the lobes of the liver?
right (largest), left, caudate, quadrate
What is the falciform ligament? What is found within it?
Connects liver to anterior abdominal wall.
Round ligament of the liver (embryo remnant of L umbilical vein)
What is the bare area of the liver?
posterior section of the liver against the diaphragm that is bare without peritoneal covering
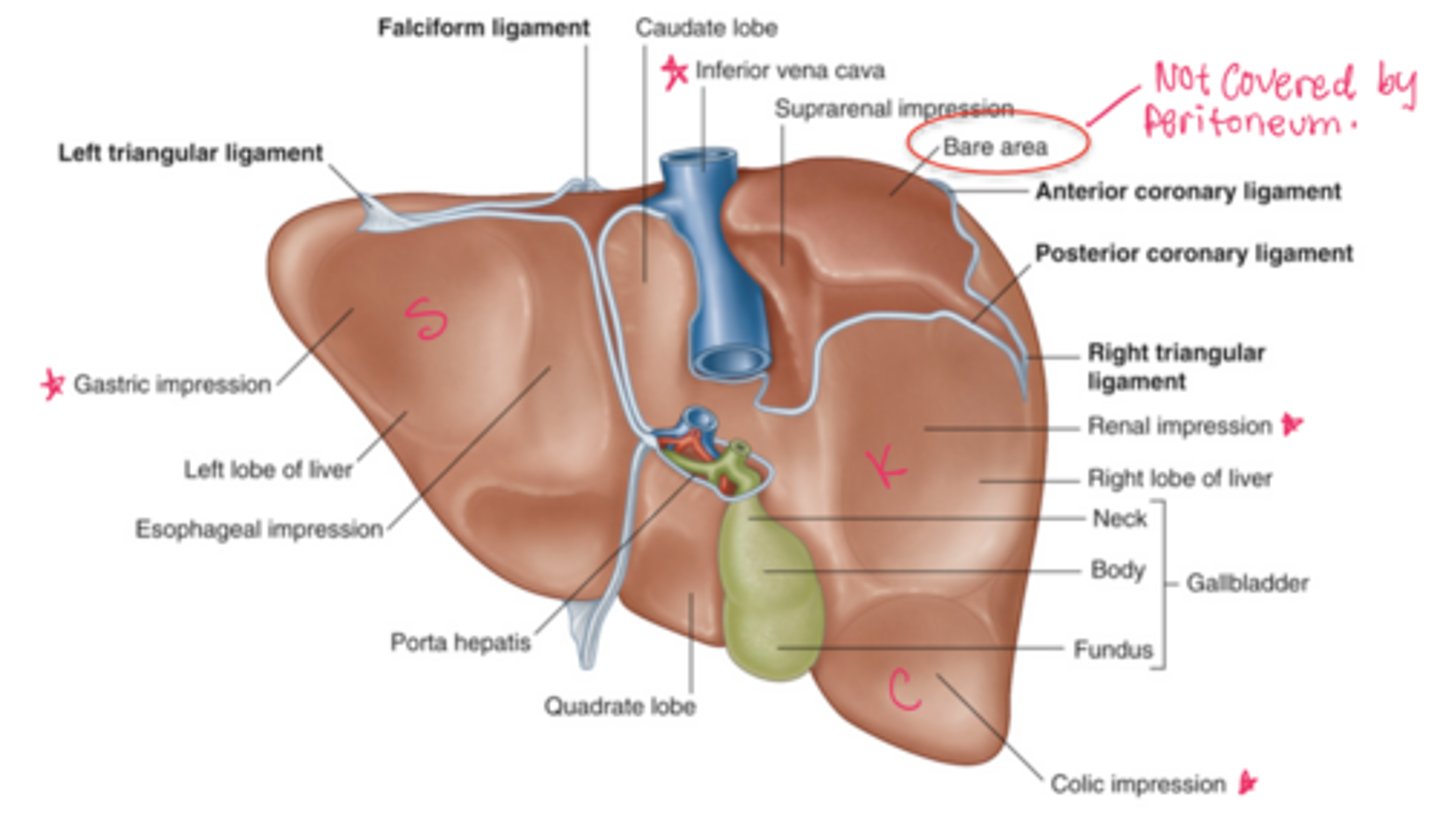
What impressions are found on the posterior view of the liver?
Gastric, colic, renal and suprarenal impression
What are the different parts of the gallbladder?
fundus, body, neck
What is the function of the gallbladder?
It stores and concentrates bile that is produced by the liver.
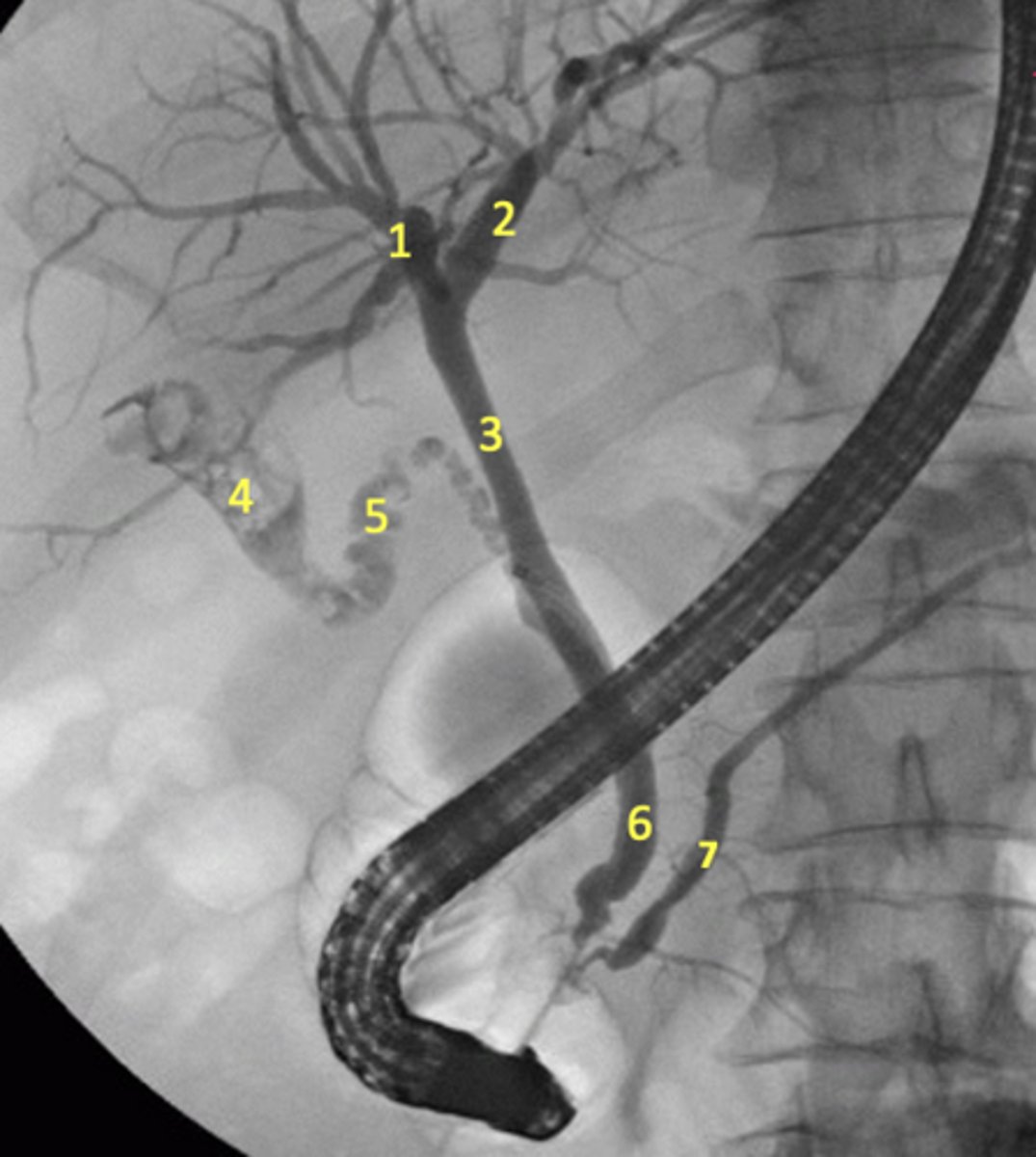
How does bile drain?
Liver makes bile -> flows into R and L hepatic bile ducts which join to form the common hepatic duct
Between meals: the sphincter of Oddi is closed, so bile cannot enter the duodenum and instead backs up through the cystic duct into the gallbladder for storage.
During meals: the sphincter of Oddi relaxes and the gallbladder contracts, so bile flows from both the liver and gallbladder through the common bile duct into the duodenum via major duodenal papillae
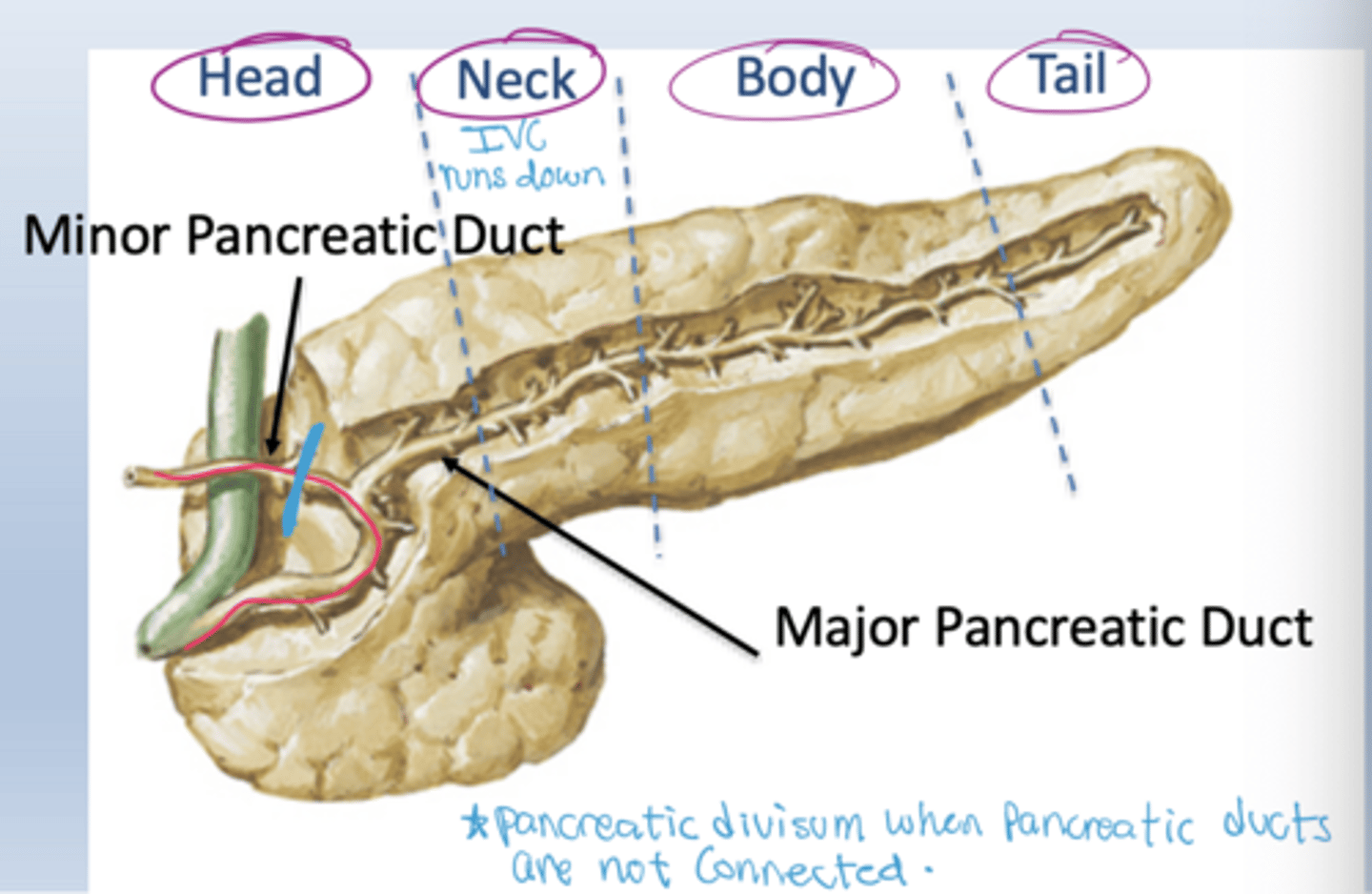
What are the anatomical parts of the pancreas?
Head, neck, body, and tail.
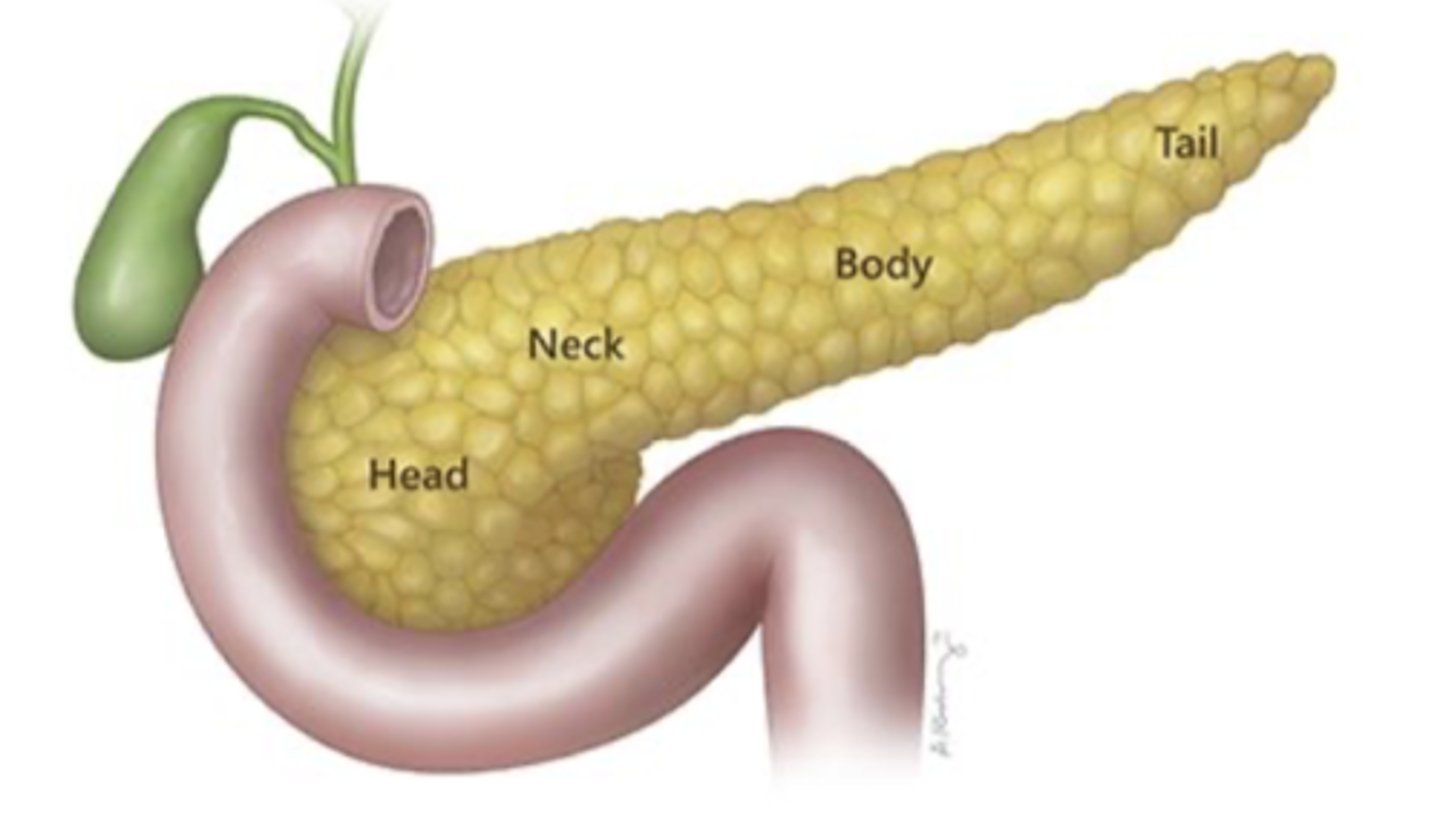
What structures lie near the pancreatic head?
The duodenum curves around the pancreatic head.
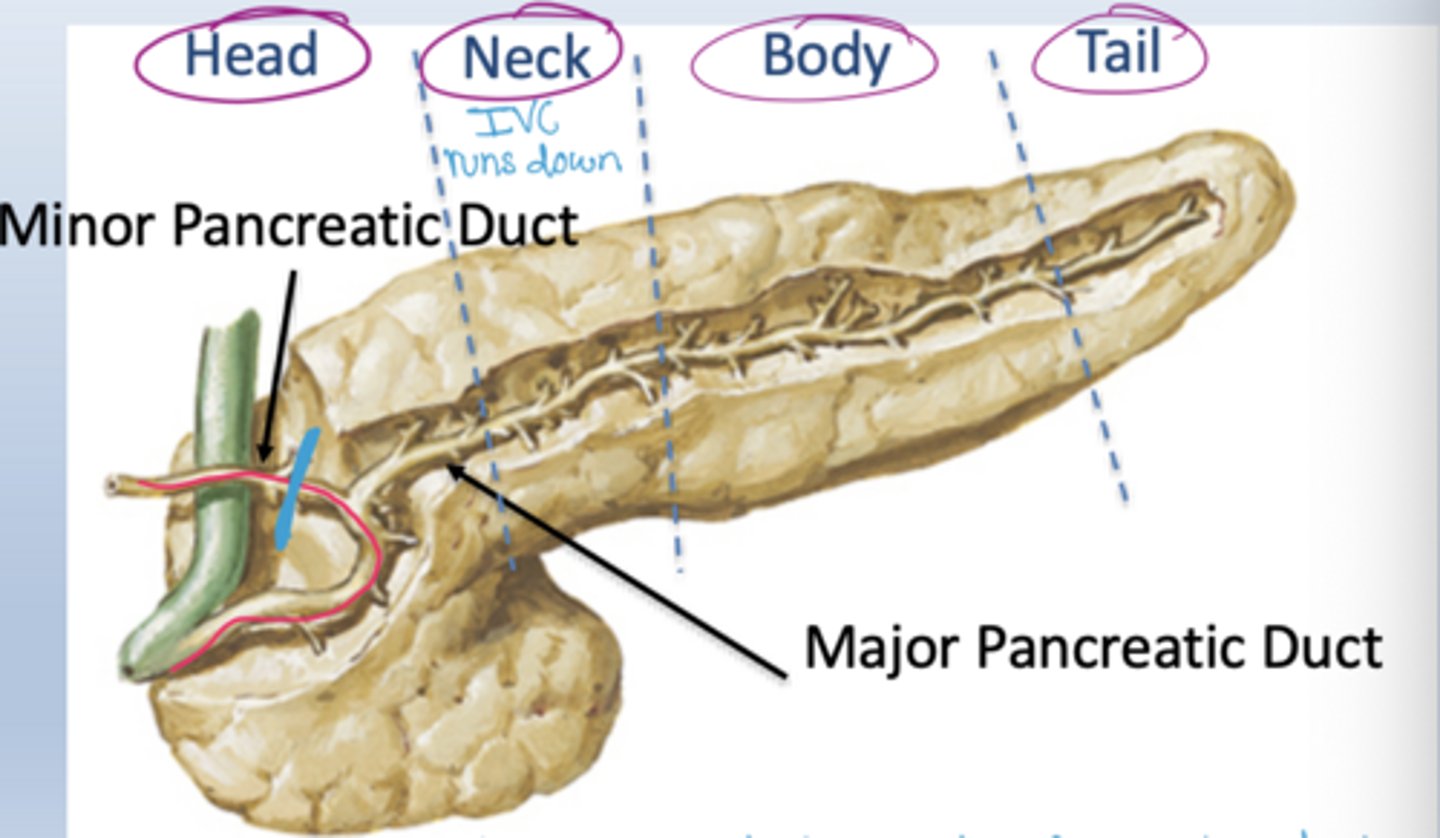
Where does the pancreatic tail extend?
Toward the spleen within the splenorenal ligament.
What are the two pancreatic ducts?
Major pancreatic duct and minor pancreatic duct.
Where do pancreatic ducts empty?
Typically into the second part of the duodenum at the major and minor duodenal papillae
What is pancreatic divism?
The pancreatic ducts are not connected
Be able to label the radiograph
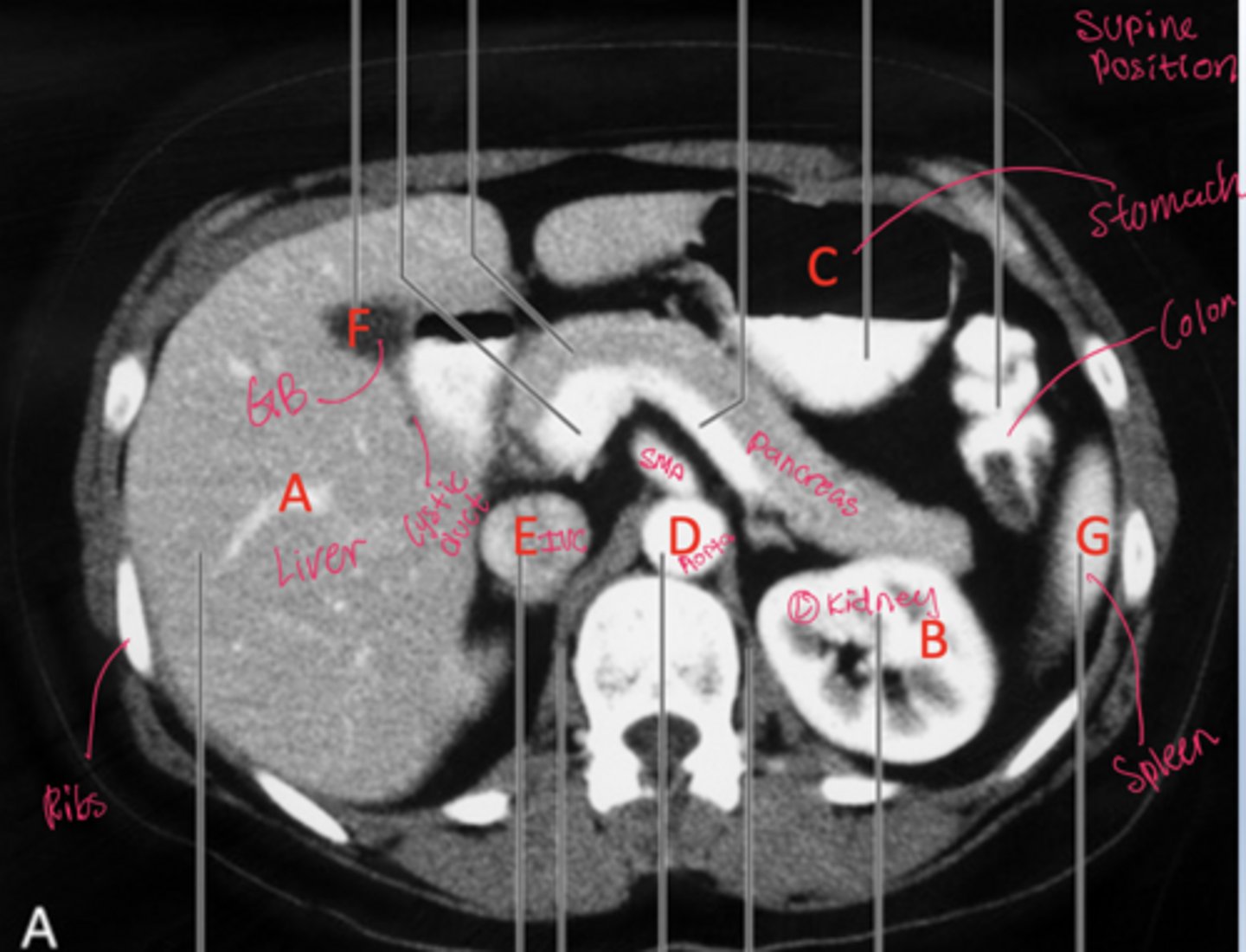
How can patient position on CT be determined using fluid and air distribution?
Fluid moves to the dependent (lowest) side, while air rises to the non-dependent (highest) side due to gravity
Where do fluid and air collect on CT when a patient is supine?
Fluid collects posteriorly (toward the back) and air collects anteriorly.
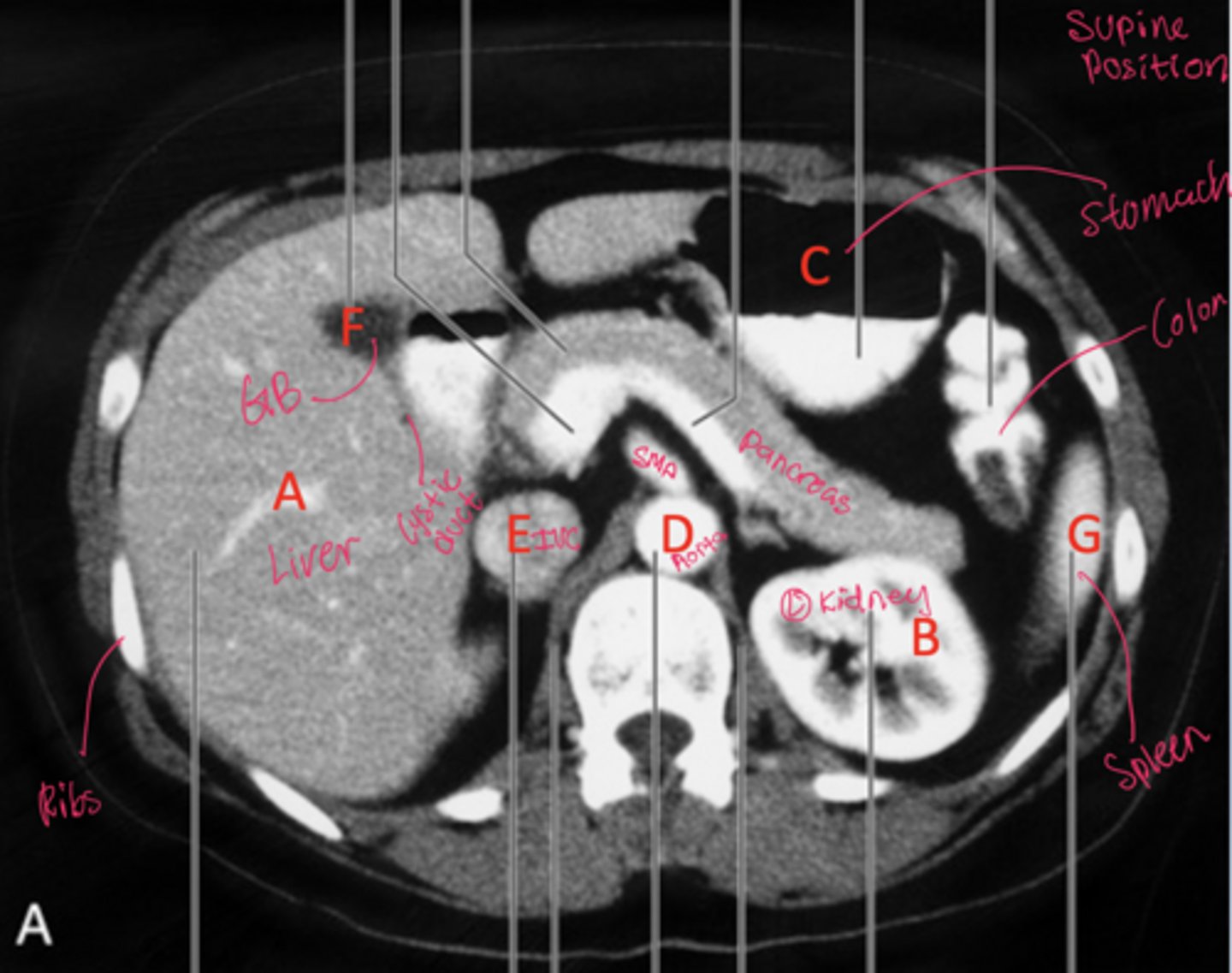
Where do fluid and air collect on CT when a patient is prone?
Fluid collects anteriorly, while air shifts posteriorly.
How do fluid and air distribute in a side-lying (lateral decubitus) CT?
Fluid settles on the down side, and air rises to the up side.
1. R hepatic duct
2. L hepatic duct
3. Common hepatic duct
4. Gallbladder
5. Cystic duct
6. Common bile duct
7. Pancreatic duct (major)
Endoscope also seen
Label the radiograph
What is the spleen's general anatomical significance?
A highly vascular organ in the left upper quadrant involved in blood filtration and immune function.
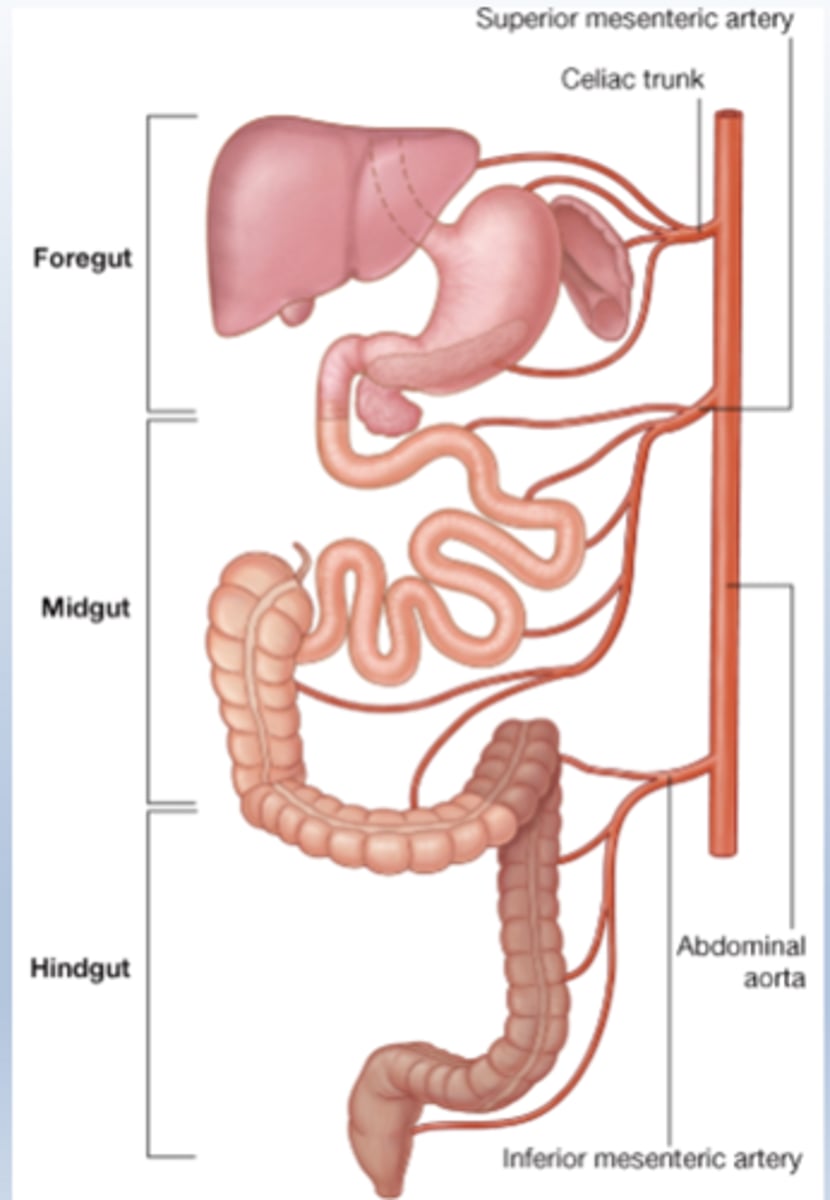
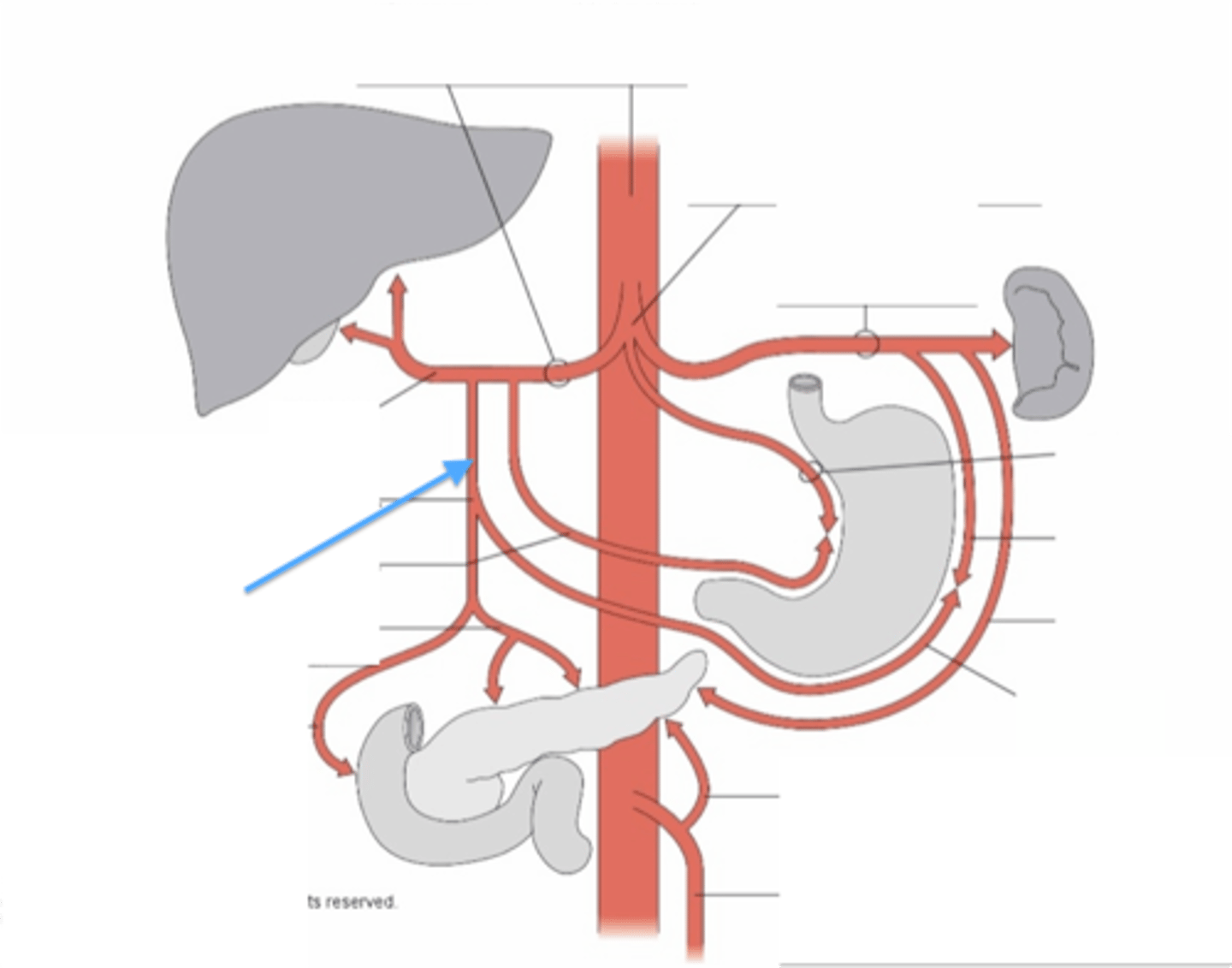
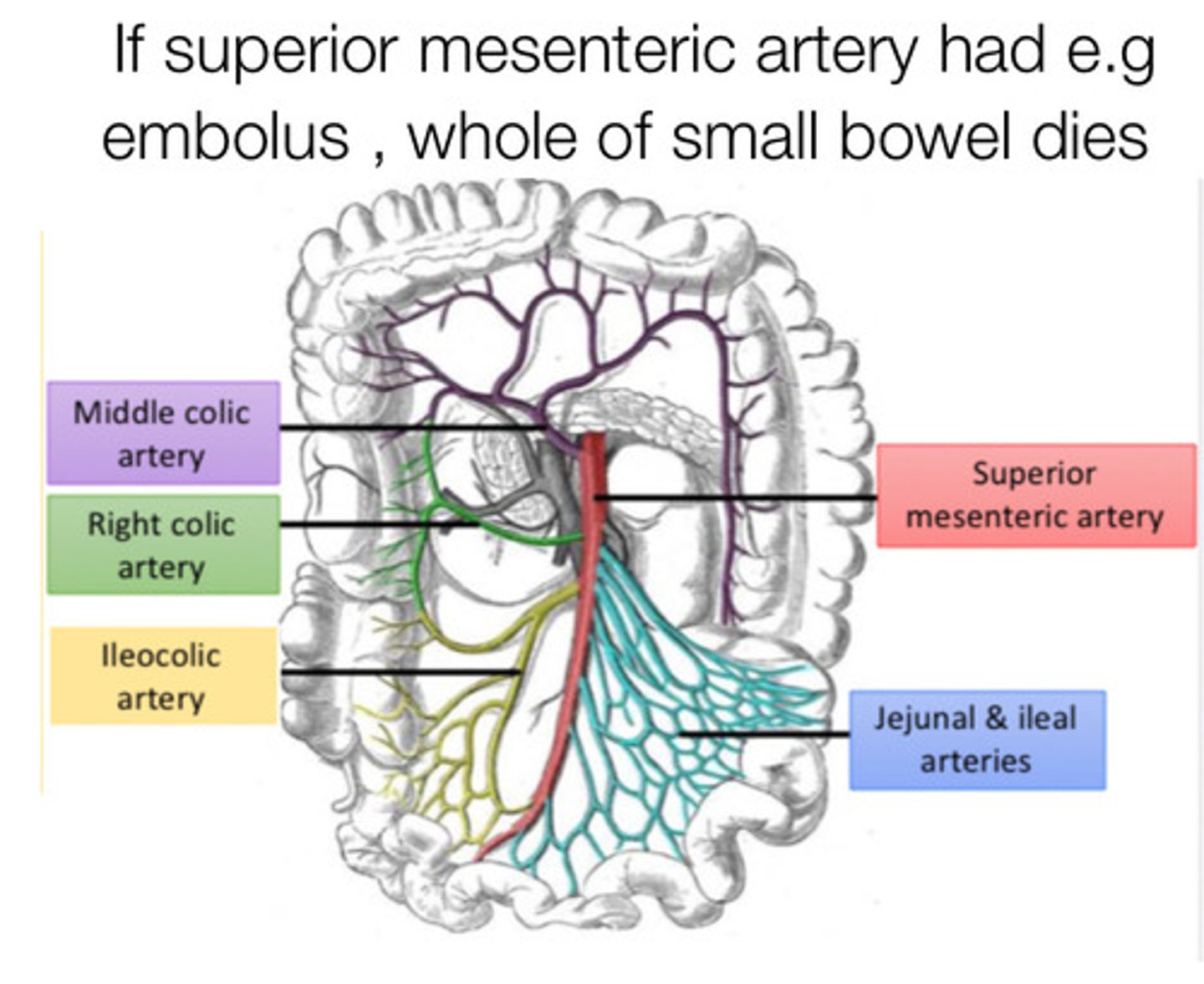
What are the three main unpaired arteries supplying the GI tract?
Celiac trunk, superior mesenteric artery (SMA), inferior mesenteric artery (IMA).
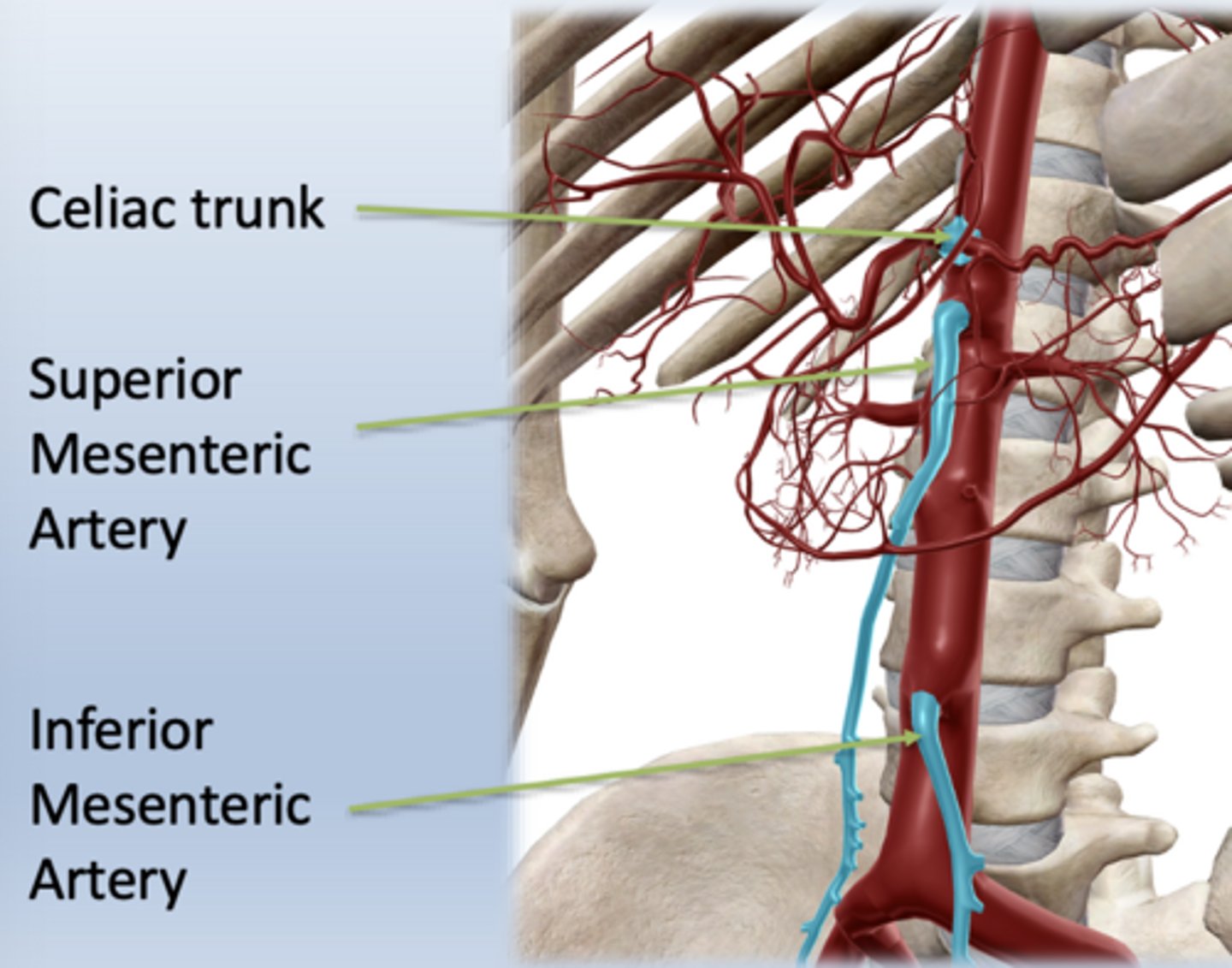
What embryologic regions correspond to these arteries?
Celiac trunk — foregut
SMA — midgut
IMA — hindgut
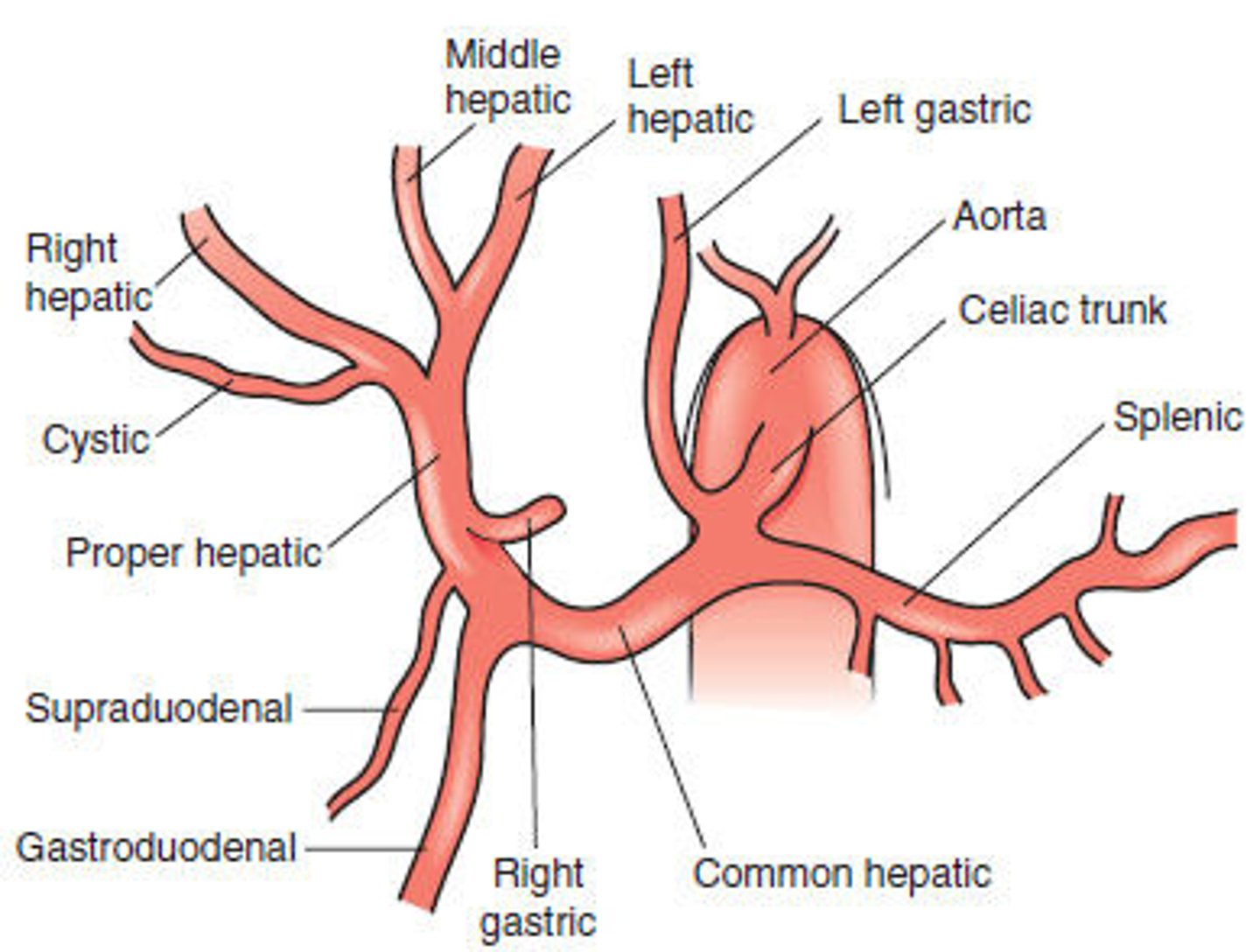
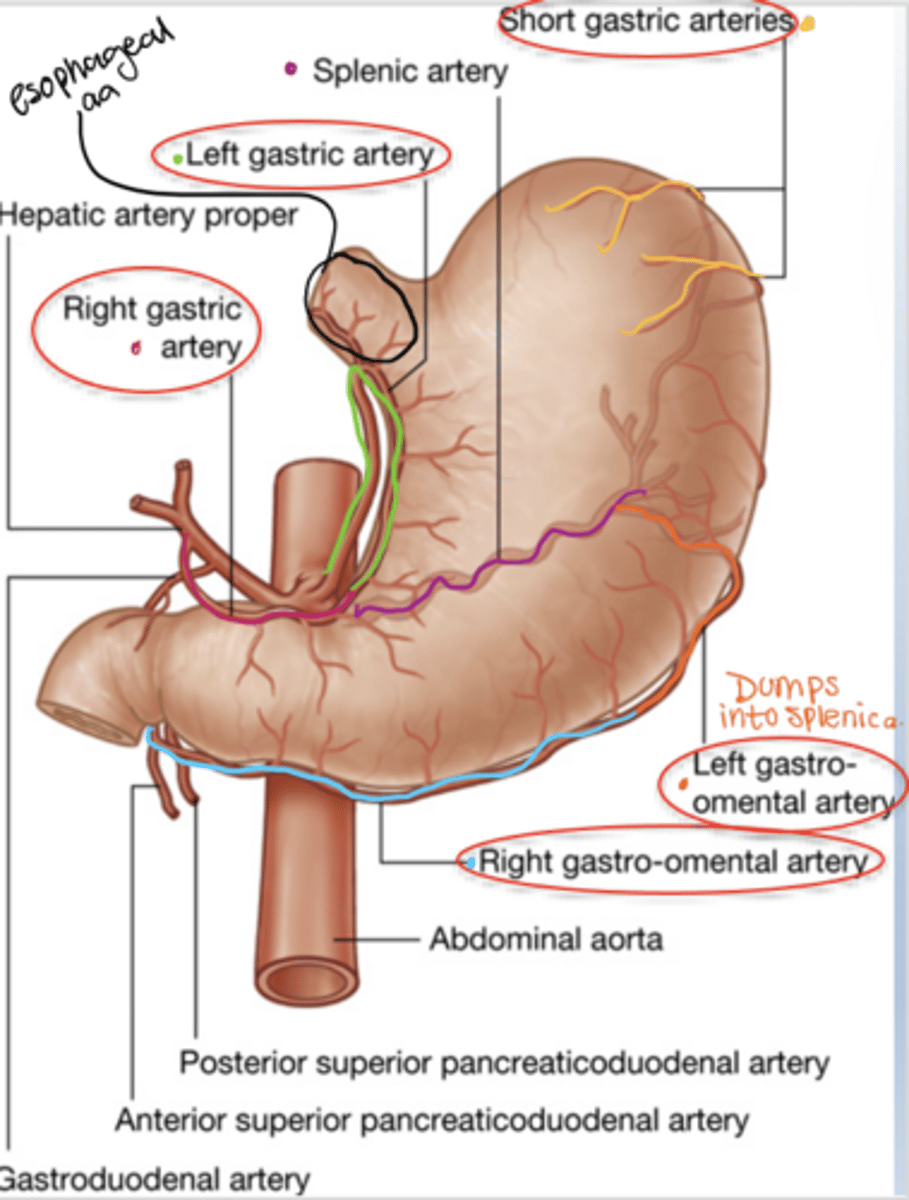
What are the three primary branches of the celiac trunk?
Left gastric artery, splenic artery, and common hepatic artery.
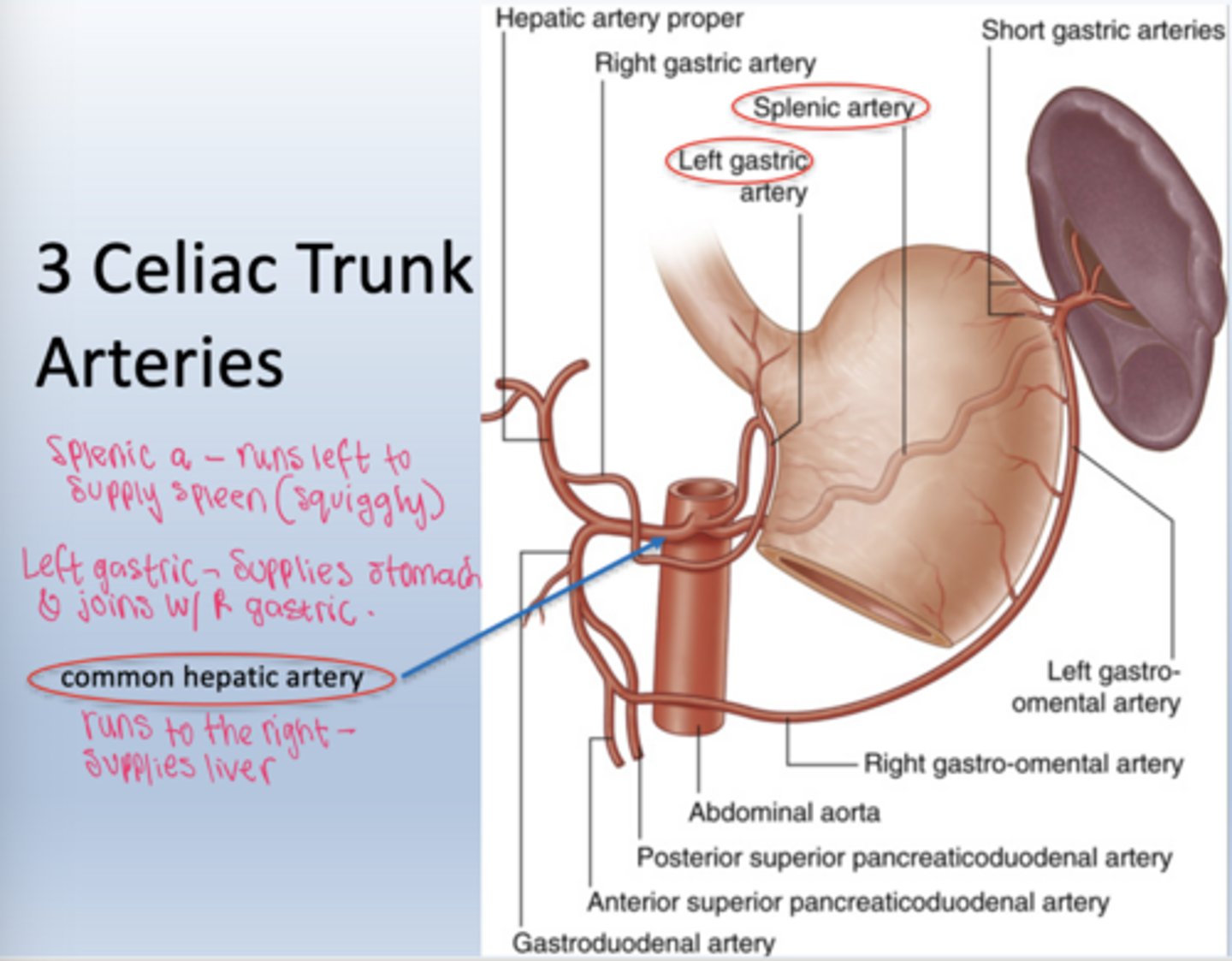
What is the course of the common hepatic artery?
It travels toward the liver and supplies the stomach, duodenum, pancreas, and liver.
What are the branches of the common hepatic?
1. Right gastric
2. Gastroduodenal (descends behind duodenum)
3. Proper hepatic (heading towards liver)
Hepatic artery proper runs in the ________________ with _______ and _________, together they form the portal triad
hepatoduodenal ligament
Portal vein and common bile duct
What does the hepatic artery proper divides into?
right and left hepatic artery supplying the right and left lobe of the liver
What is the cystic artery?
from the right hepatic artery a branch arises known as the cystic artery which supplies the gallbladder
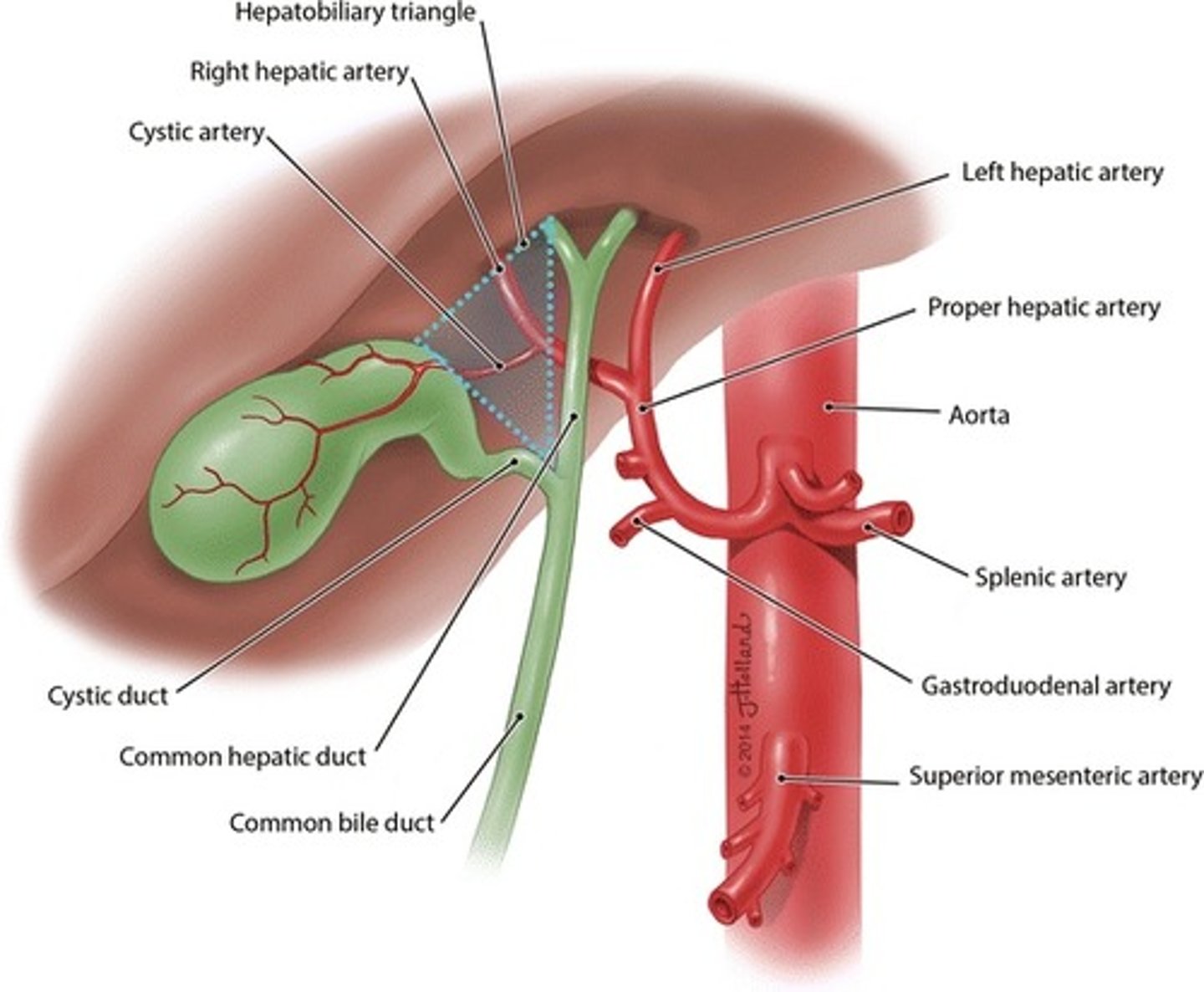
What are the branches of the celiac trunk?
left gastric artery, splenic artery, common hepatic artery (gastroduodenal, hepatic proper, R/L hepatic, and cystic a)
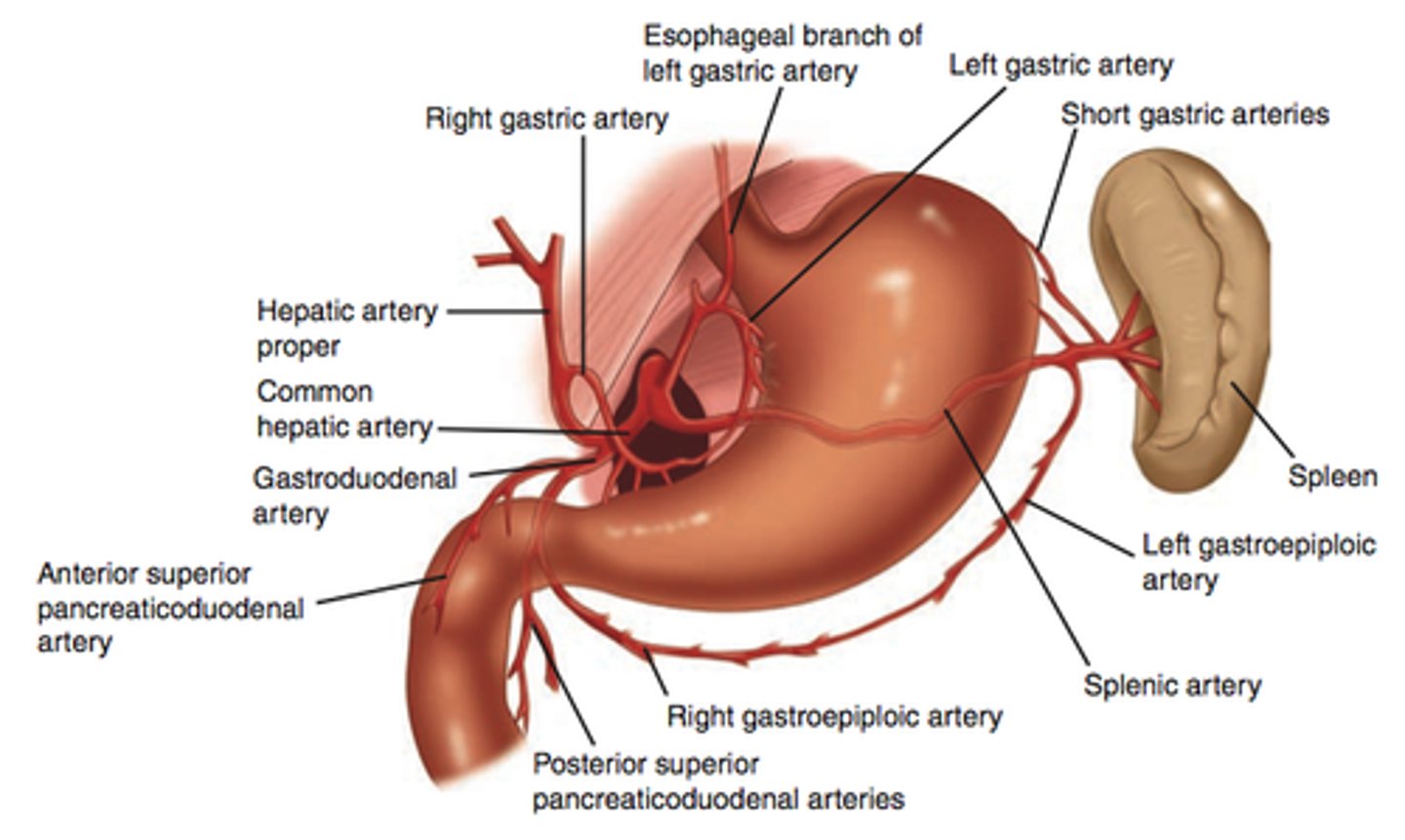
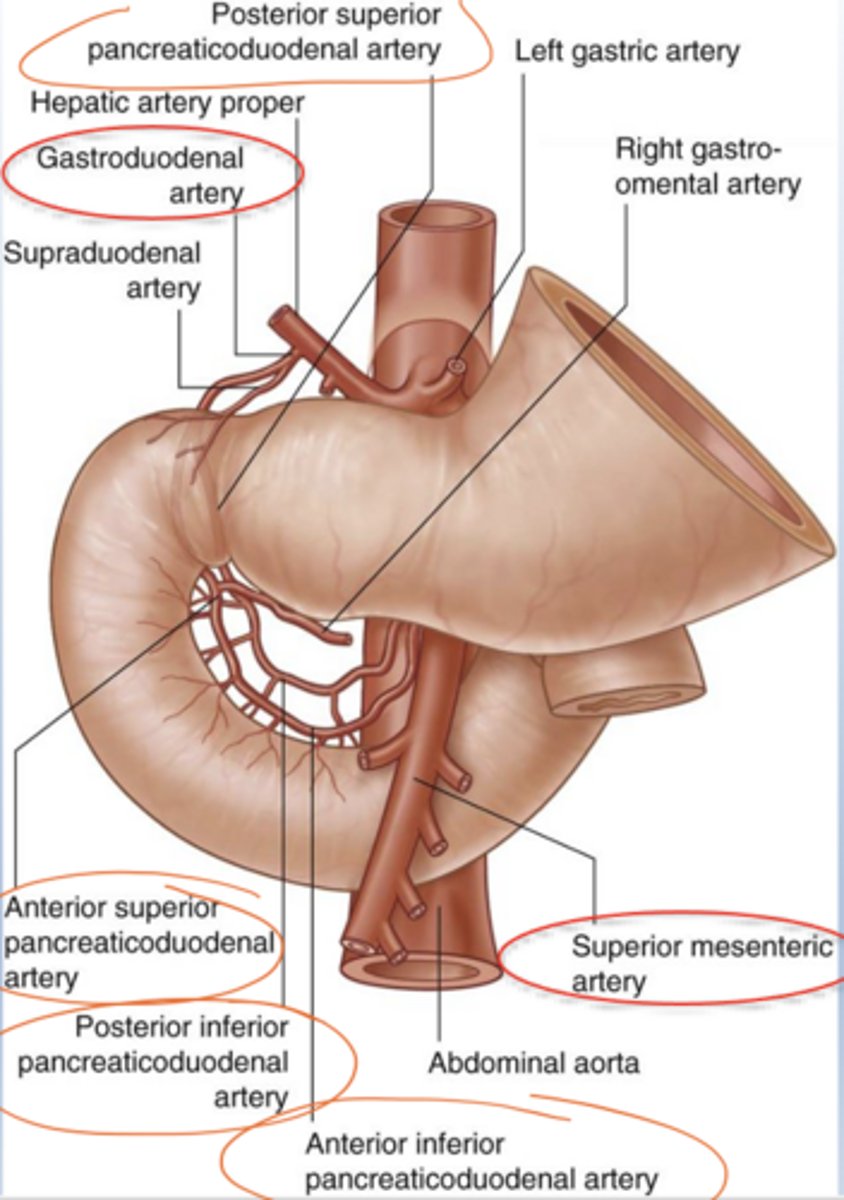
What does the gastroduodenal artery divide into?
right gastroepiploic artery
superior pancreaticoduodenal artery
What vessels supply the stomach?
Left and right gastric arteries along the lesser curvature, left and right gastroepiploic arteries along the greater curvature, plus short gastric arteries.
How is the duodenum supplied arterially?
By branches from both the celiac trunk and SMA.
- Gastroduodenal a
- Post. superior pancreaticoduodenal
- Ant. superior pancreaticoduodenal
- Post. inferior pancreaticoduodenal
- Ant. inferior pancreaticoduodenal
- Superior mesenteric artery
What vessels supply jejunum and ileum?
Jejunal and ileal arteries from SMA forming arcades and vasa recta.
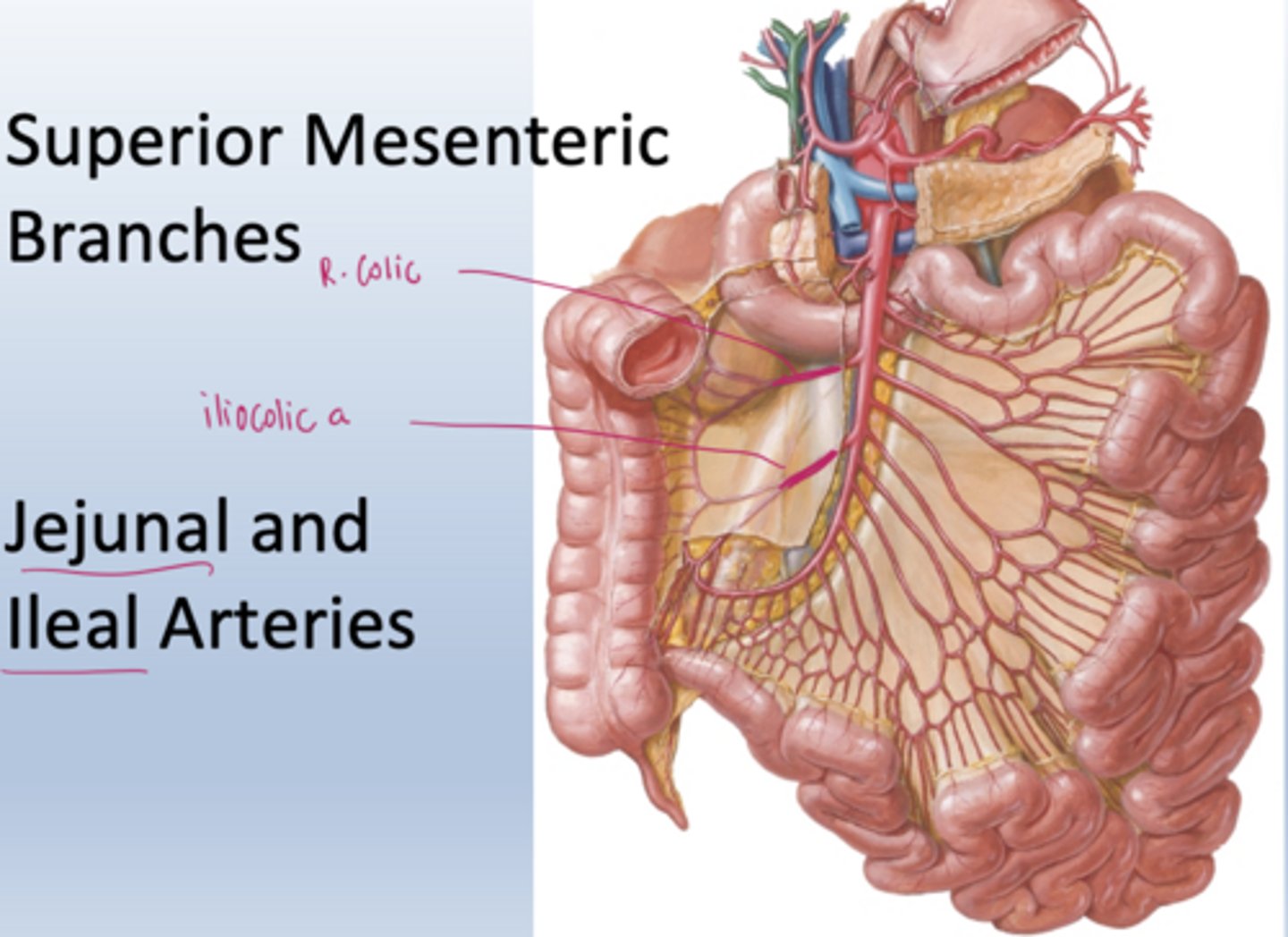
What does the right colic artery supply?
ascending and transverse colon
What does the R. iliocolic artery supply?
ileum and cecum
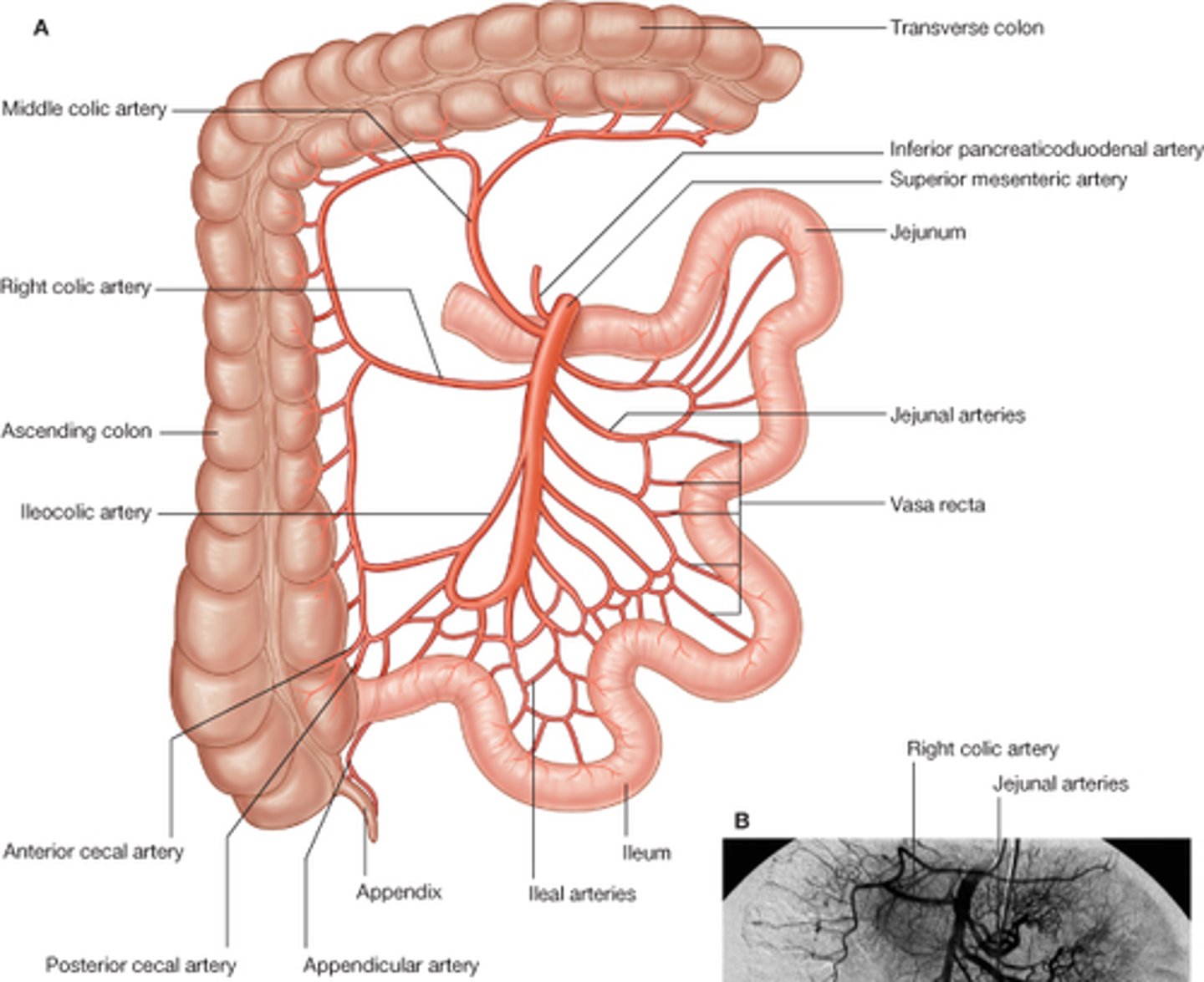
How do vascular patterns help distinguish jejunum and ileum?
Jejunum has long vasa recta and fewer arcades; ileum has short vasa recta and many arcades.
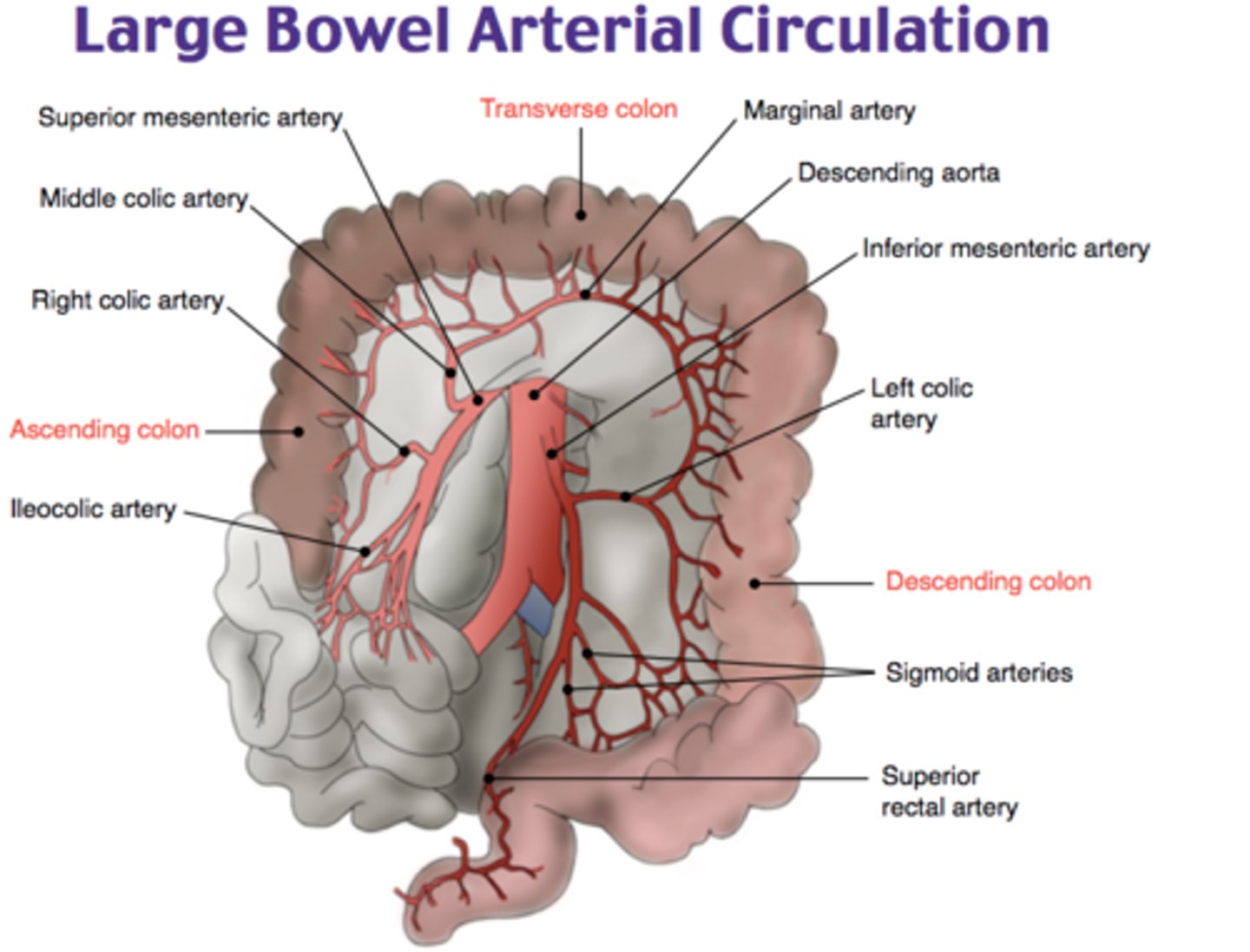
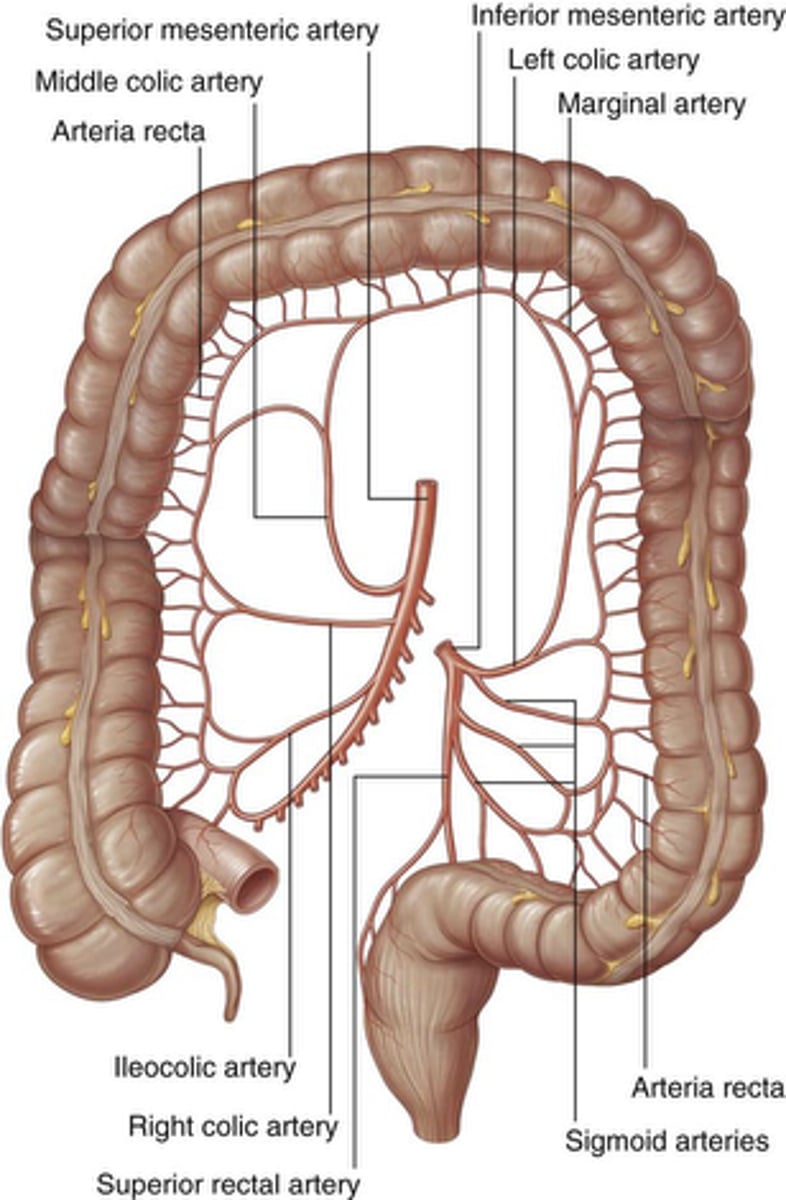
Which arteries supply the colon?
Branches from SMA and IMA depending on segment location.
Know the colonic vasculature
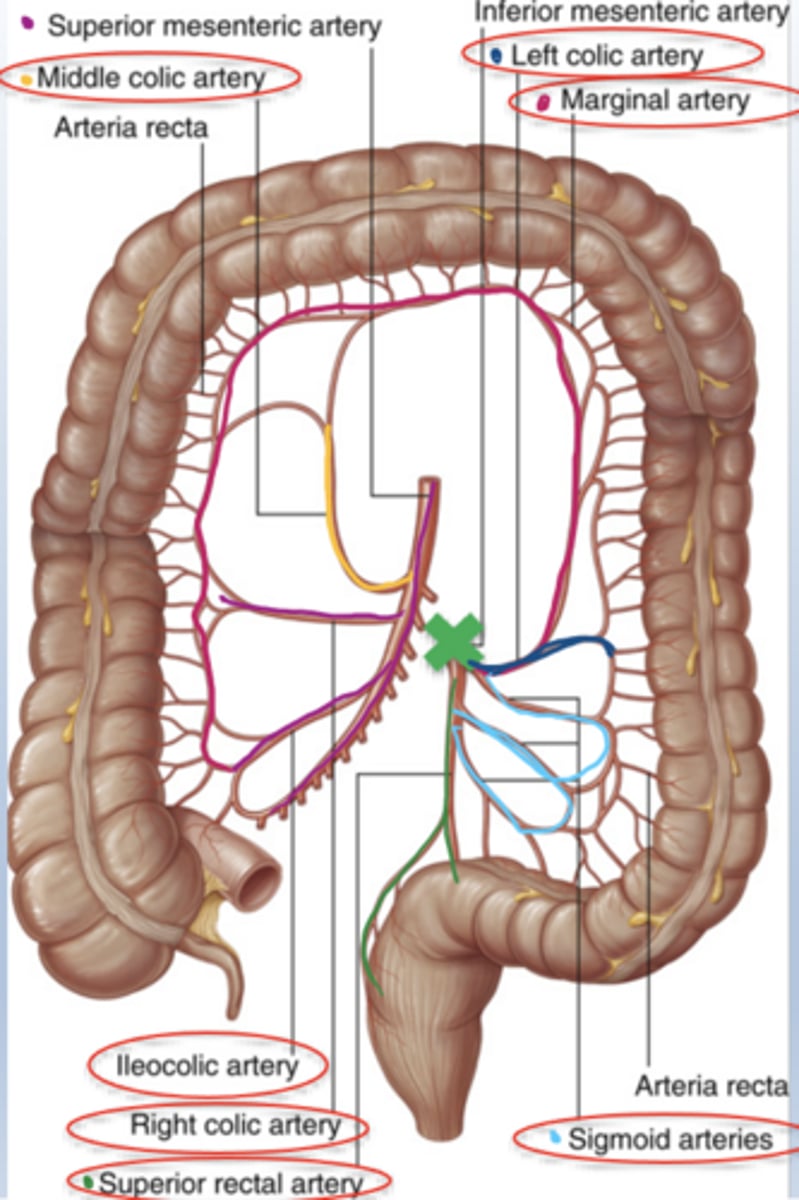
What does the middle colic artery supply?
proximal 2/3 of transverse colon
What does the left colic artery supply?
distal 1/3 of transverse colon and descending colon
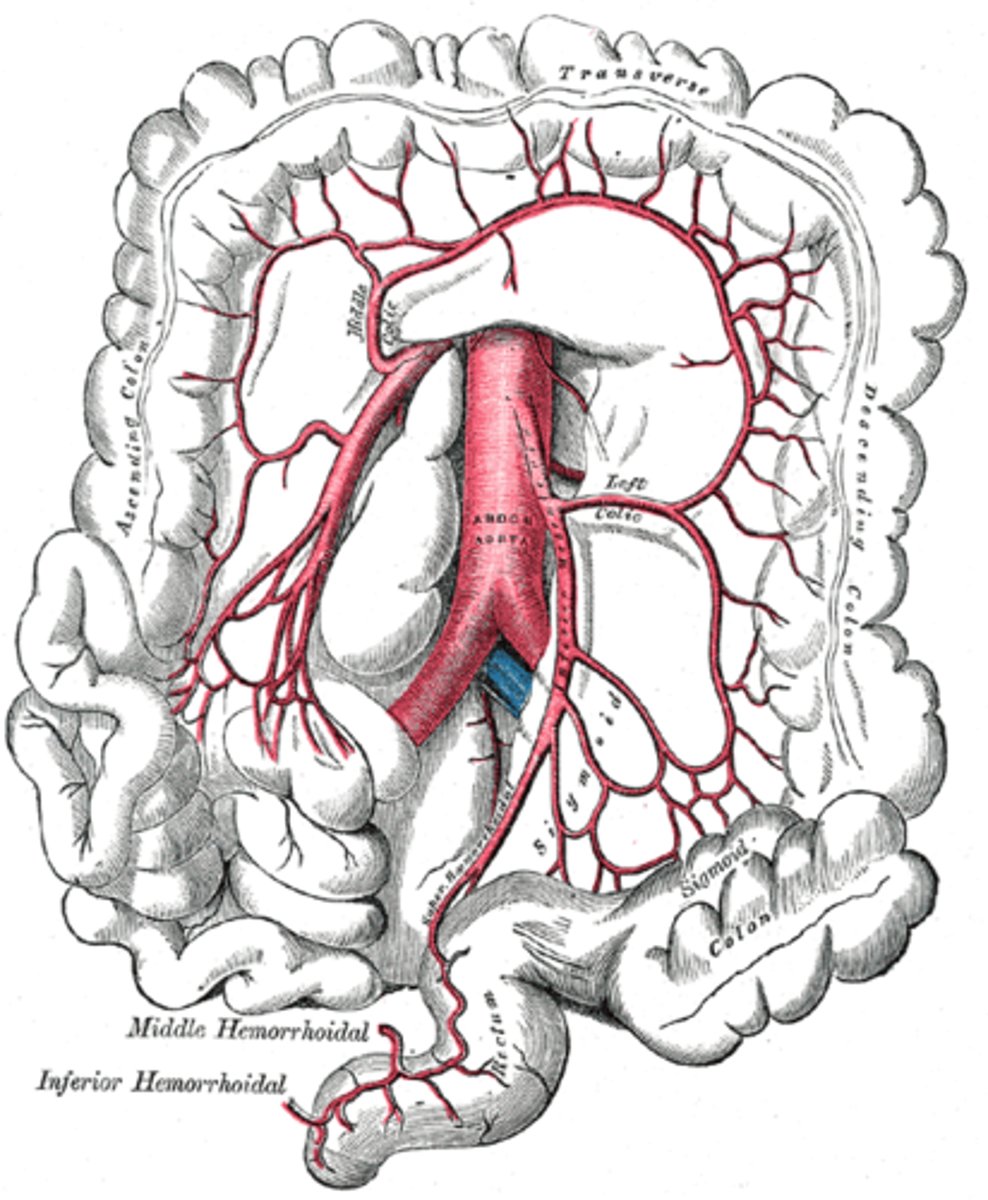
What do the sigmoidal arteries supply?
sigmoid colon
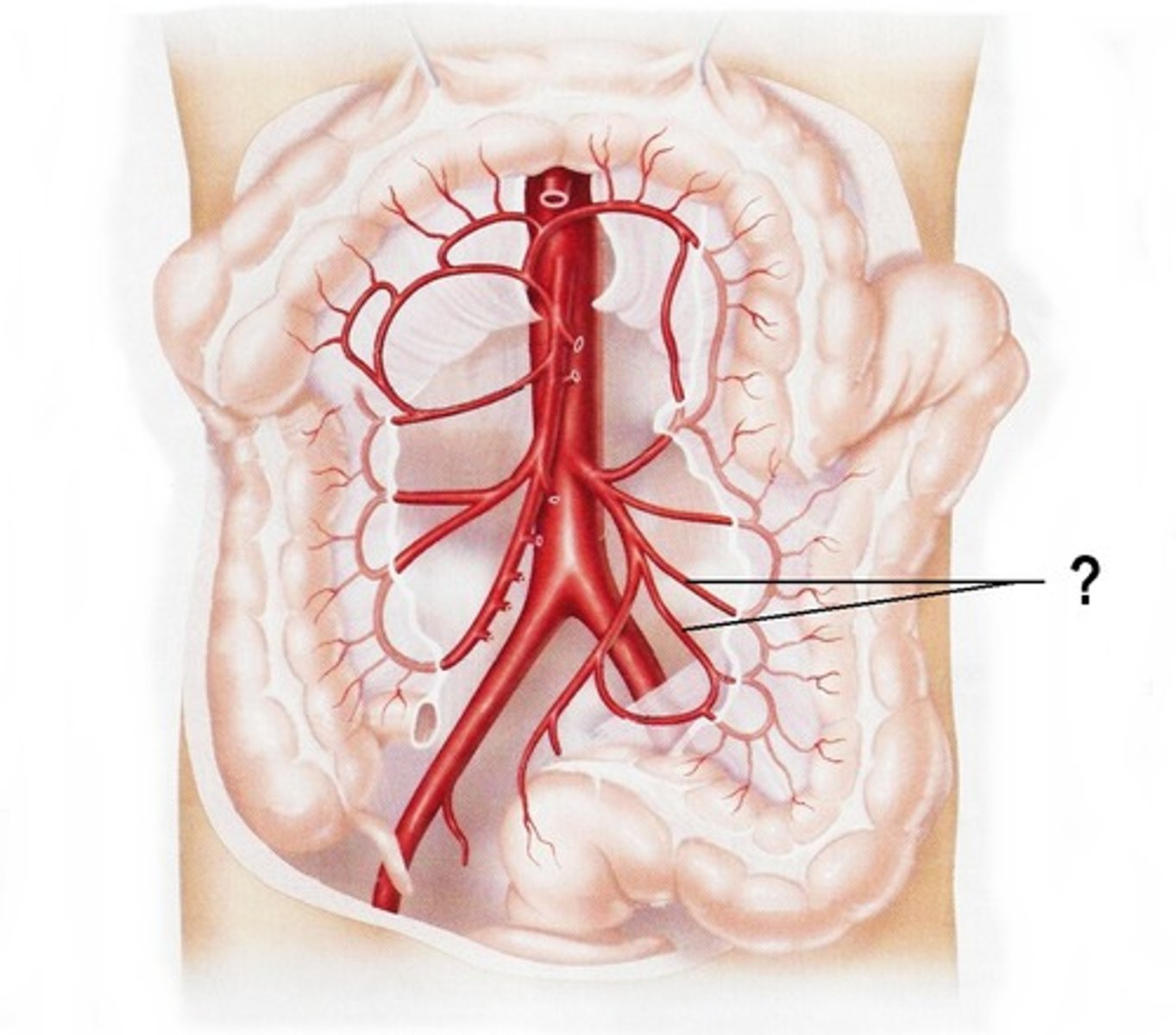
What do the superior rectal arteries supply?
rectum
What does the marginal artery supply?
is a continuous arterial channel running along the inner border of the colon, supplies cecum to rectum
formed by connections between branches of superior mesenteric artery (SMA) and inferior mesenteric artery (IMA).
It acts as a collateral circulation pathway.
What is the hepatic portal system?
A venous system transporting blood from GI tract to liver for processing.
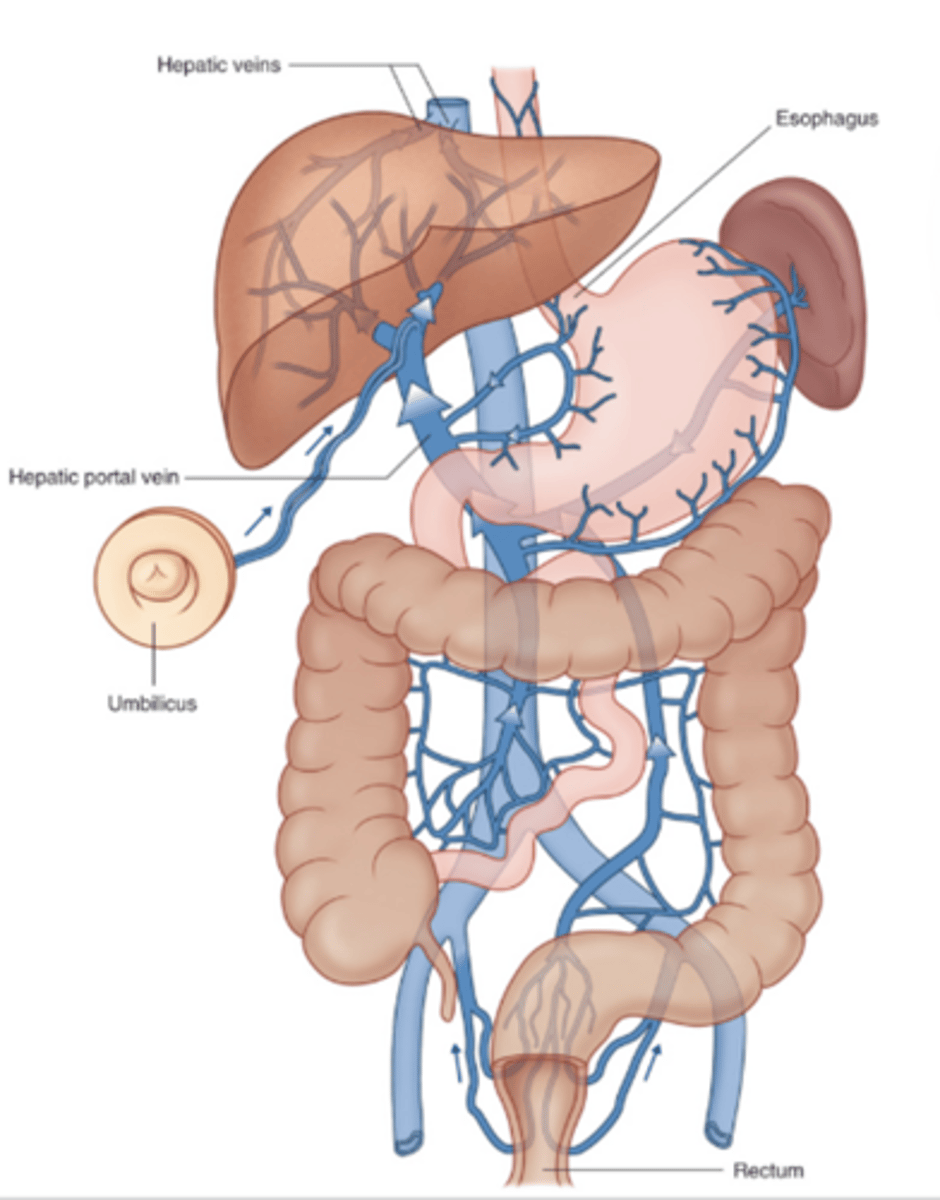
What is the portal triad?
hepatic proper, portal vein, common bile duct
Why does blood enter liver first before the heart?
because the liver functions to filter out toxins and further absorb the necessary nutrients from the blood before sending it to the inferior vena cava.
Where are major portocaval anastomoses located?
Lower esophagus, umbilical region, and upper anal canal.
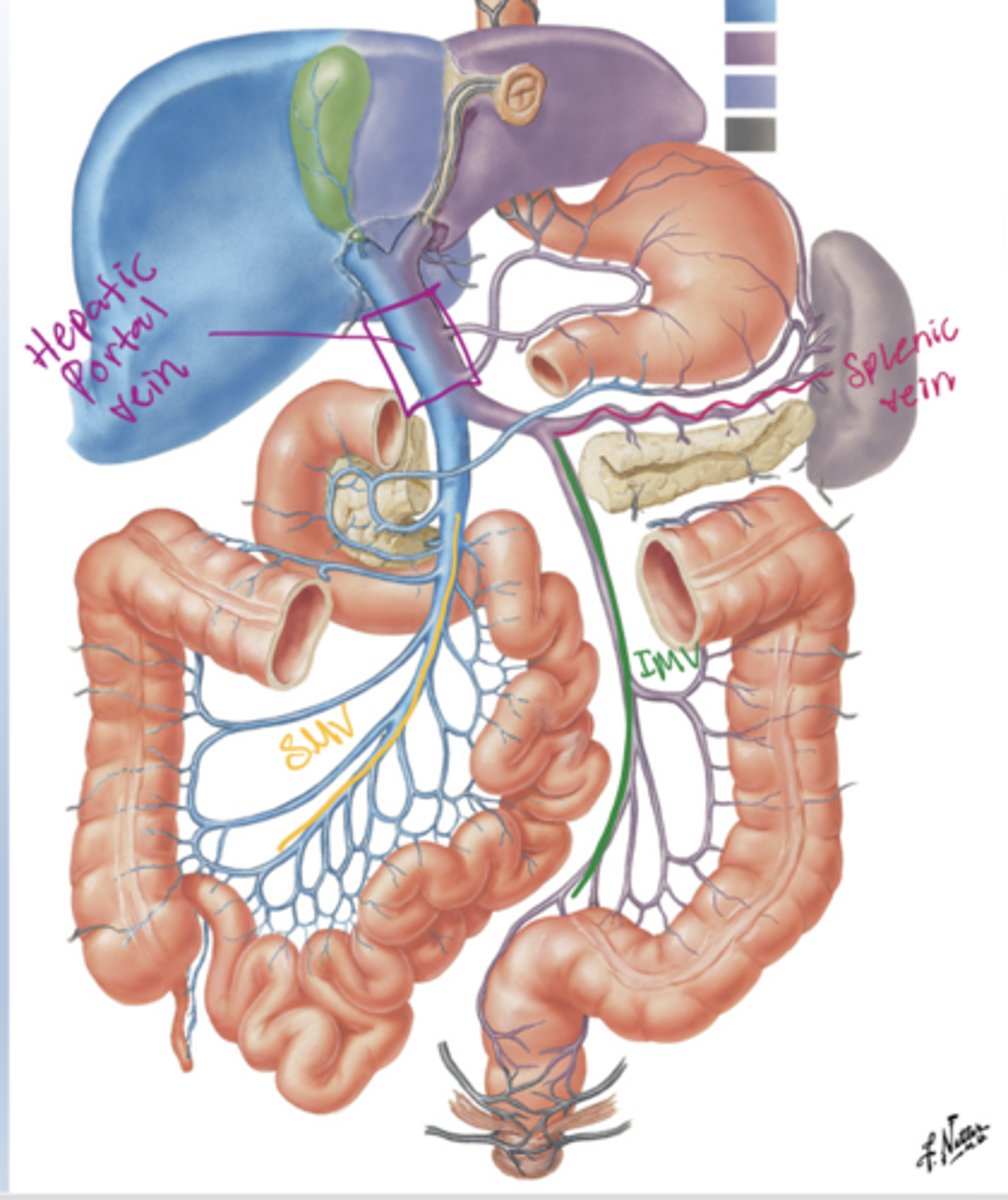
Why are portocaval anastomoses clinically important?
Portal hypertension causes dilation of these sites producing varices.
A 52-year-old male presented to the outpatient department with progressive abdominal distension and prominent veins over the anterior abdominal wall for the past 3 months. He also complained of easy fatigability, reduced appetite, and occasional episodes of hematemesis
Caput medusa (secondary to liver failure)

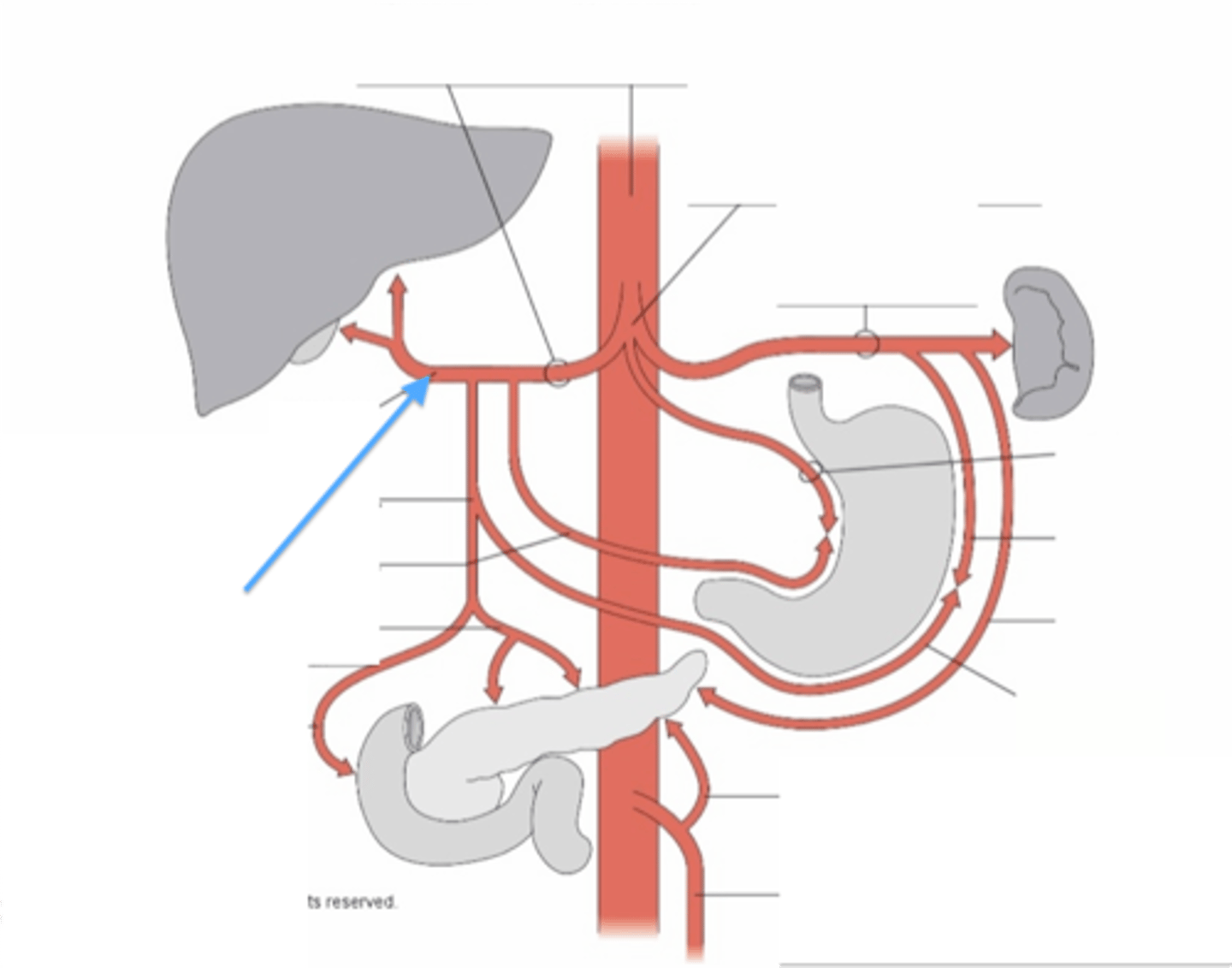
1. Splenic a
2. Common hepatic a
3. L hepatic a
4. R hepatic a
5. Gastroduodenal a
6. R Gastro-omentum a
7. L gastric a
8. Hepatic proper a
Pink circle - celiac trunk
Label the radiograph

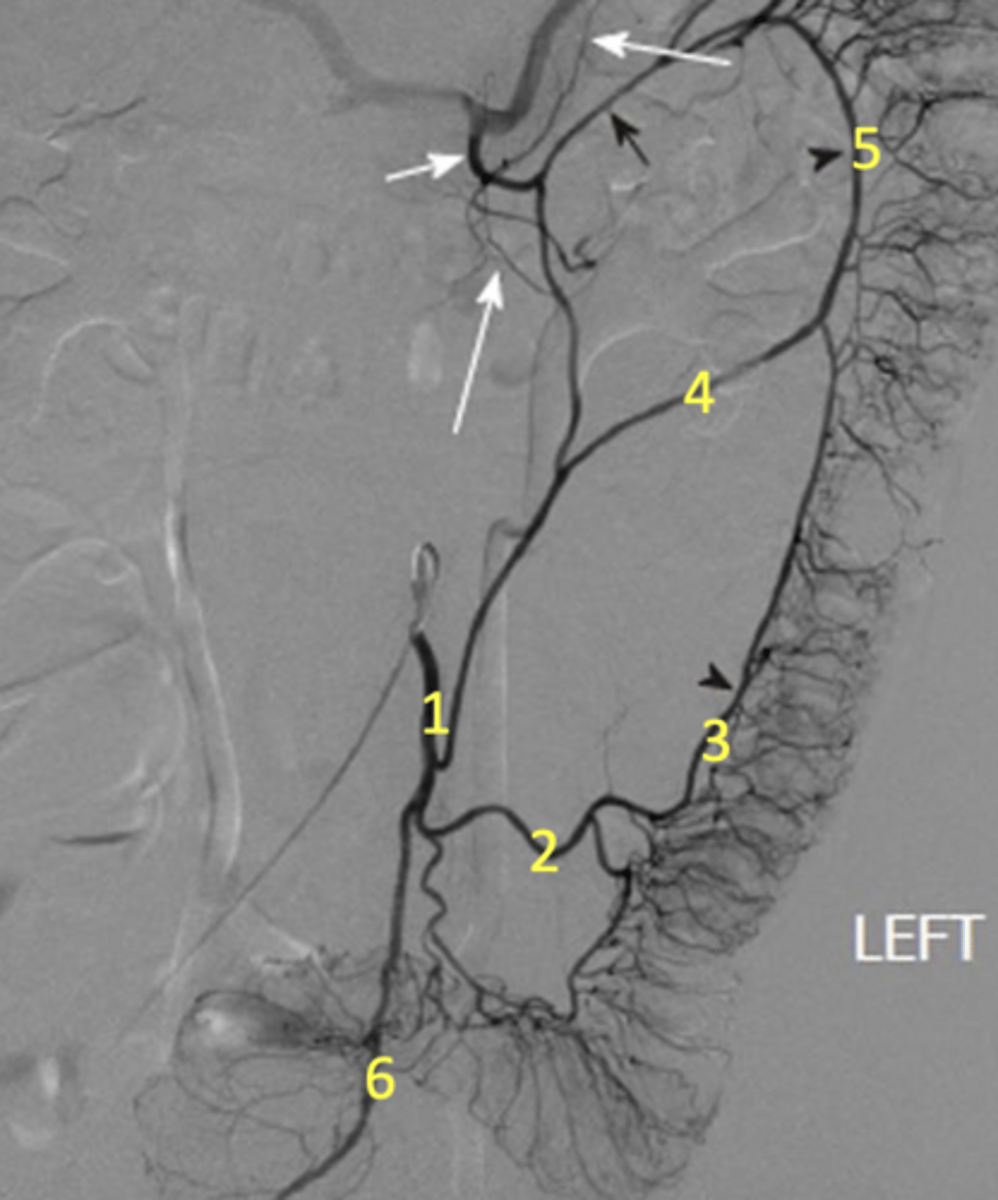
1. Inf. mesenteric a
2. sigmoidal a
3. marginal a
4. left colic a
5. marginal a again
6. superior rectal a
Label the radiograph
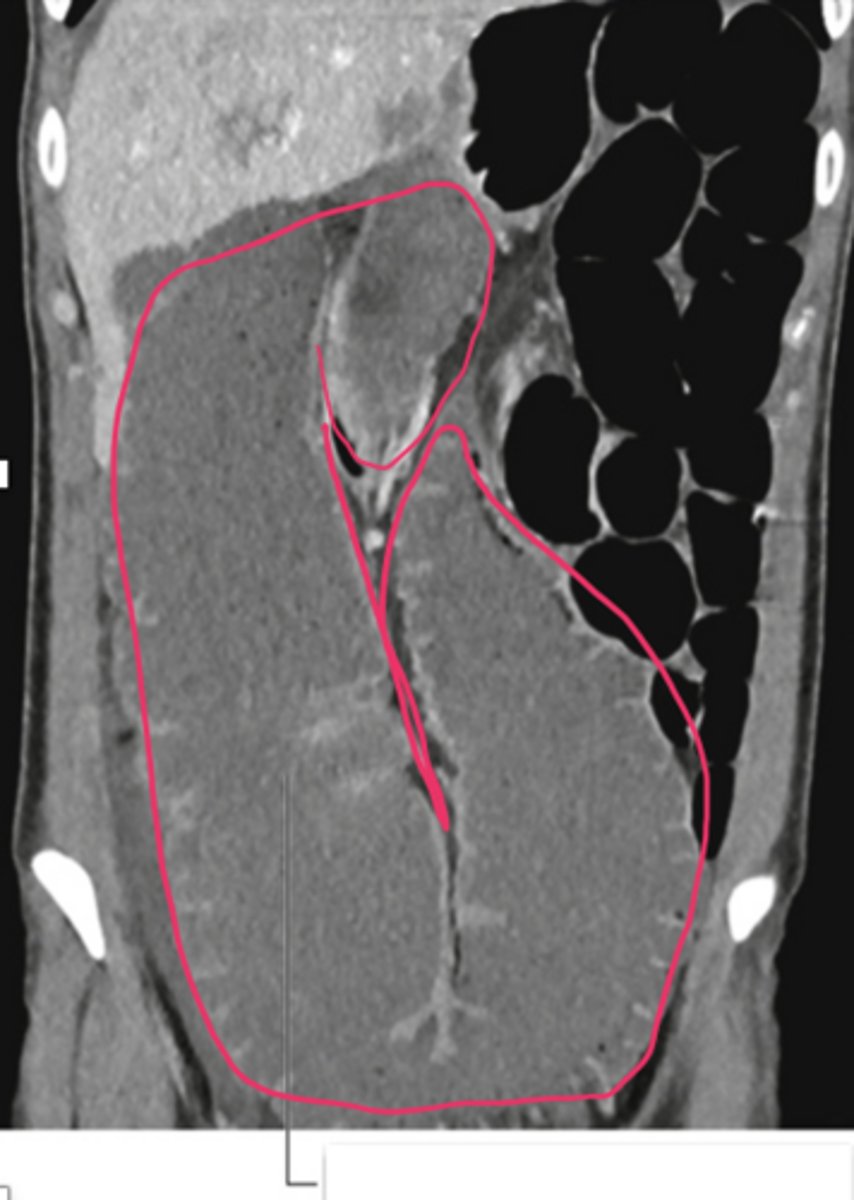
A 65-year-old male presented to the emergency department with complaints of progressive abdominal distension, colicky abdominal pain, and constipation for 7 days. He also reported absolute constipation with failure to pass flatus for the last 3 days. There was a history of unexplained weight loss, loss of appetite, and intermittent episodes of altered bowel habits over the past 4 months.
On physical examination, the patient appeared ill and dehydrated. Vital signs showed mild tachycardia. The abdomen was grossly distended and more prominent in the lower abdomen. On palpation, the abdomen was tympanic and mildly tender, with no palpable mass. Digital rectal examination revealed an empty rectum with no palpable growth.
Large colon due to bowl obstruction
What is caput medusa?
Tortuous vessels around the umbilicus caused by portal HTN
