Hematology Ch 16
1/20
Earn XP
Description and Tags
Quantitative and Qualitative Platelet Disorders
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
21 Terms
What are the two types of platelet disorders?
Qualitative
Less common
Problems with platelet function.
Assess via platelet aggregation studies and bleeding time.
Quantitative
More common
Includes various "thrombocytopenias" (assess via platelet count)
Either decreased production or increased destruction of platelets.
Qualitative Platelet Disorders
Inherited
impaired platelet function, usually bleeding time is prolonged.
Intrinsic defect of platelets
May be a disorder of adhesion and platelet release OR a storage pool defect.
Disorders of Adhesion
Von Willebrand's Disease (vWD)
Bernard Soulier Syndrome (BSS)
Glanzmann's Thrombasthenia (GT)
vWD (Von Willebrand's Disease)
Disorder of adhesion.
Qualitative or quantitative defect in Von Willebrand's Factor (vWF).
a large glycoprotein used for platelet adhesion
Symptoms:
Heavy menses (menorrhagia)
excessive bleeding after dental procedures
epistaxis (nose bleeds)
ecchymoses (bruising)
easy bleeding
vWD Lab Tests
•PLT count: usually normal
•PTT: increased most of the time
•Bleeding time: prolonged
GT (Glanzmann's Thrombasthenia)
Disorder of adhesion.
Autosomal recessive disorder
Abnormality of GPIIb and IIIa
important for aggregation
Variable bleeding patterns: Umbilical cord bleeding, gingival bleeding, purpura, prolonged bleeding from minor cuts
symptoms
normal platelet count and morphology, but abnormal platelet aggregation
treatment
oral contraceptives (for menorrhagia)
epsilon aminocaproic acid (used as a topical thrombin-inducing agent)
GT Tests
•Bleeding time: prolonged
•Platelet count: normal
•Normal platelet morphology
•Abnormal aggregation
all aggregating agents are present except for ristocetin
BSS (Bernard Soulier Syndrome)
Disorder of adhesion.
Rare adhesion defect of platelets involving GP Ib-IX receptor for vWF.
Ib-IX complex is site for: thrombin binding, regulating platelet shape, and regulating reactivity
inhibits platelets from sticking to collagen to create a platelet plug
symptoms
Epistaxis, Gingival bleeding, Menorrhagia, Purpura, Thrombocytopenia with giant platelets
treatment
platelet transfusion
What are some preanalytical factors that can cause thrombocytopenia?
blood not being filled to the line in light blue tubes
wrong ratio (supposed to be 9:1)
patient may have platelet satelitism
What are some causes of thrombocytopenia related to decreased production?
bone marrow issues
lack of platelets (aplasia) or megakaryocytes
leukemia
megaloblastic conditions (causes pancytopenia)
cytotoxic agents or chemotherapy
bacterial infections
viral infections
CMV, EBV, HCV, HIV, varicella, or rubella
How can altered distribution of platelets lead to thrombocytopenia?
the spleen holds 1/3 of all platelets
an enlarged spleen can cause blood to pool, withholding platelets from circulation
caused by myeloproliferative disorders, extramedullary hematopoiesis, and hemolytic anemias
splenectomy can cause thrombotic conditions due to increased platelets in circulation
Drug induced immune thrombocytopenia (DIT)
reduced platelet count
can be dangerous and cause significant bleeding
drugs that cause it:
quinines, NSAIDs, heparin, anticonvulsants, sulfanomides, diuretics, and amoxicilin
two things cause it:
ingestion results in anti-drug antibody formation that binds to platelets and eventually causes the removal of platelets from circulation (low PLT count)
drug combines with larger carrier proteins forming an antigen that triggers an antibody response, results in platelet destruction
Thrombocytopenia
•Low platelet count
•PLT <150 K/uL
•Bleeding signs: Gingival, nose (epistaxis), extensive bruising (ecchymoses), pinpoint hemorrhages (petechiae).
•60-100 K/uL will bleed in surgery
•30-50 K/uL will have petechiae in the absence of trauma.
•5 K/uL has a high risk of CNS hemorrhage.
•The first thing to do when PLT# is low is check the smear to confirm!!!
ITP (Idiopathic (Immune) Thrombocytopenic Purpura)
autoantibody (IgG) destroys platelets, leading to thrombocytopenia
Autoantibody (IgG) against GP IIb/IIIA or GP Ib-IX.
Two types
Chronic
Platelet count 30−60
Age 20−50 years.
Lasts months to years.
Acute
Platelet count as low as 20
Age usually 2−6 years.
Often caused by virus.
Lasts 2−6 weeks.
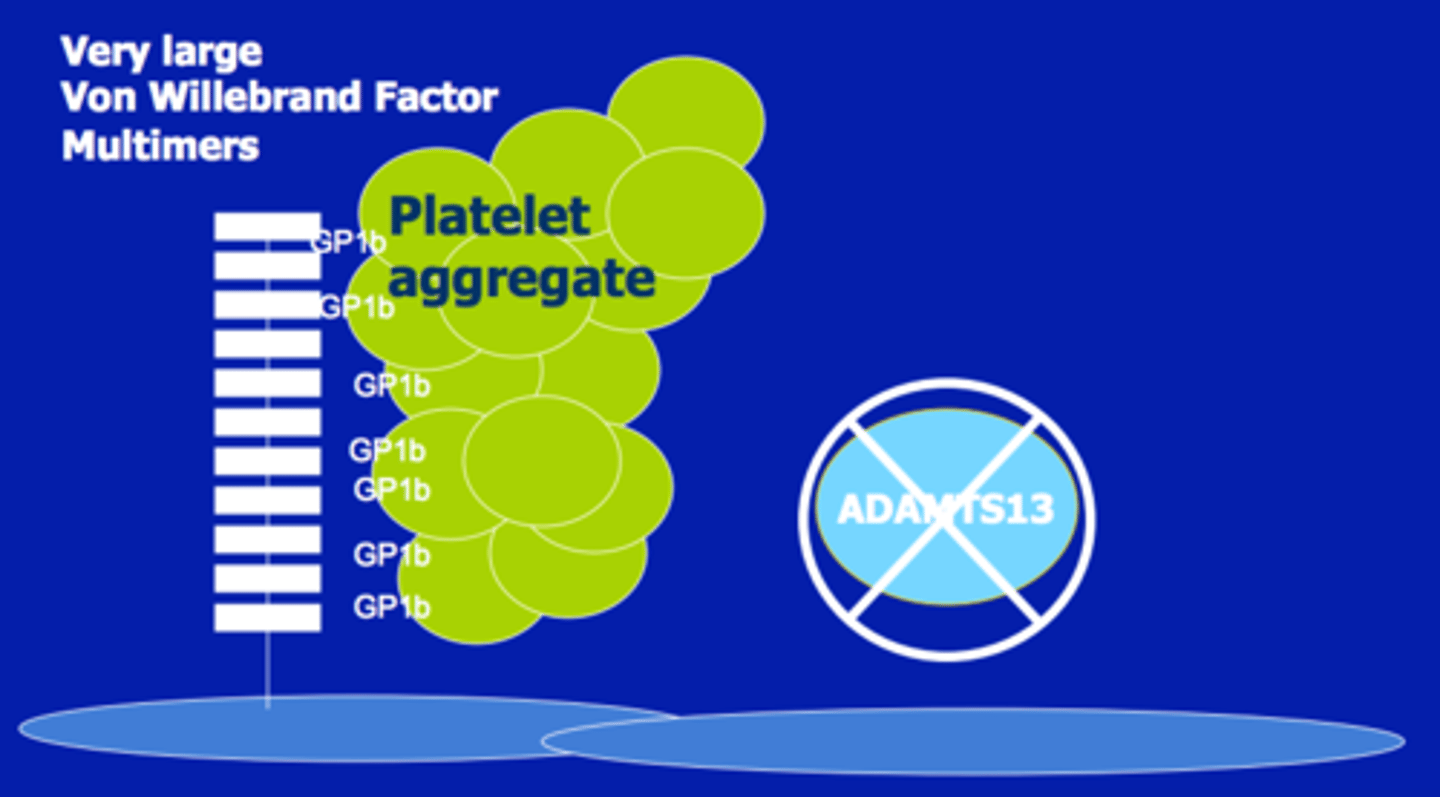
TTP (Thrombotic Thrombocytopenic Purpura)
acute and unpreditable thrombocytopenia
Platelet count <20
PT and PTT normal
excessive platelet adhesion and aggregation
Smear shows schistocytes resulting from clot formation.
Severe hemolytic anemia called microangiopathic hemolytic anemia.
HUS (Hemolytic Uremic Syndrome)
Thrombocytopenia
presence of nitrogenous waste products in blood (uremia)
Usually affects age 6 months−4 years
Mimics TTP except renal damage is more severe.
Renal damage caused by toxin produced by E. coli O157:H7 or Shigella.
Patients may present with:
Bloody diarrhea
Microangiopathic hemolytic anemia
Thrombocytopenia
Renal failure
Thrombocytosis
Platelet count is >450
Primary thrombocytosis
caused by myeloproliferative disorders
increased number, but impaired function
Secondary thrombocytosis
seen in acute and chronic blood loss (spleen throws out more platelets), chronic inflammatory disease, post-splenectomy (No place to store platelets anymore), and iron deficiency anemia
Platelet function is normal.
What are platelet release defects?
inherited disorders
characterized by abnormal secondary phases of platelet aggregation and granule release
associated with postoperative bleeding, menorrhagia, and easy bruising
platelet count is normal
What are 2 causes of acquired defects of platelet function?
drug-related defects
aspirin can inhibit production of platelet aggregator thromboxane A2
can also be used to prevent strokes, MIs, or other CV events
secondary disorders
renal disease, uremia, and multiple myeloma or Waldenstrom
How can skin, collagen, or blood vessel abnormalities cause platelet dysfunction?
can cause mucosal bleeding, purpura, petechia, ecchymosis, or telangiectasia
PLT count and function is normal
What is purpura?
small, reddish-purple spots on the skin, caused by small blood vessels leaking
nose bleeding, deep bruising, and gum bleeding are usually manifestations of which type of coagulation disorder?
platelet defects