Gastroenterology - Small and Large Intestine
1/114
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
115 Terms
Emily, a 18-year-old, presents with chronic fatigue, bloating, and frequent loose stools over the past several months. She reports diarrhea, steatorrhea, and abdominal distention. She's also noticed weight loss despite a good appetite. She denies recent travel, antibiotic use, or sick contacts.
Physical exam reveals mild abdominal distention and dermatitis herpetiformis—a pruritic, blistering rash on her elbows and knees. Laboratory studies reveal:
Mild iron-deficiency anemia
Negative stool cultures and ova/parasites
Positive tissue transglutaminase IgA antibodies (tTG-IgA)
Genetic testing revealed the presence of HLA-DQ2 allele.
1.) What additional testing is recommended to confirm positive serological testing results?
2.) What is the diagnosis?
3.) What is the treatment?
1.) Small Bowel Biopsy
2.) Celiac Disease
3.) Gluten free diet with the addition of supplements.
Dermatitis Herpetiformis is associated with which GI condition?
Celiac disease

What type of bacteria is T. Whipplei?
Gram positive bacillus
Thomas, a 54-year-old man, presents with chronic diarrhea, unintentional weight loss, and joint pain over the past 4 months. He reports 4-5 loose, greasy, foul-smelling stools per day and says his knees and wrists ache, especially in the morning. He also complains of intermittent low-grade fever and general fatigue. On exam, he appears thin and pale. He has hyperpigmentation on his face and mild abdominal tenderness. Neurologic exam reveals mild confusion and memory issues.
His vitals are as follows:
Temperature: 103F
BP: 95/70
O2: 99%
HR: 100bpm
How do you treat this patient?
Thomas has Whipple's Disease
We need to treat him with Ceftriaxone or meropenem for 2 weeks followed by oral bactrim for 1 year.
We should see dramatic improvement within several weeks.
What are some common symptoms of bacterial overgrowth syndrome?
Distention, bloating, flatulence, diarrhea
Liz, a 68-year-old woman, presents with bloating, excessive gas, distention, and chronic diarrhea for the past several months. She reports that her stools are loose, bulky, and malodorous, and often float in the toilet. She has lost about 8 pounds unintentionally. Her symptoms worsen after meals. Her past medical history includes scleroderma, hypothyroidism, and diverticulosis.
On physical exam, she has mild abdominal distention and diffuse tenderness without guarding. Lab work reveals:
Macrocytic anemia
Low vitamin B12
Elevated folate
A hydrogen breath test is ordered and comes back positive.
What non-surgical treatment options do you provide the patient?
Liz has bacterial overgrowth syndrome you can treat her with broad spectrum antibiotics for 7-10 days
Cipro 500mg BID, Norfloxacin 400mg BID
Augmentin 875mg BID
Bactrim DS BID
Carlos, a 45-year-old man, presents to the clinic with chronic diarrhea, fatigue, and unintentional weight loss over the past several months. He recently returned from living in rural Southeast Asia for 1 year, where he was working as a teacher. He describes his stools as fatty, occurring 4-5 times a day for the past two weeks. He also reports sore tongue, numbness in his feet, and occasional bloating. You order a stool sample on three separate occasions and the presence of cysts and trophozoites were not found in either sample. You conduct a bowel biopsy which reveals shortened, blunted villi and elongated crypts with increased inflammatory cells. You rule out celiac disease since a gluten free diet does not improve histologic improvement.
If you ordered a CBC what results would you expect to find?
What are some bacteria that could be causing this?
What treatment do you recommend?
Carlos has tropical sprue.
A CBC would demonstrate macrocytic anemia due to folate/B12 deficiency
Some bacteria found in tropical sprues are G. lambia, Y. enterocolitica, C. Difficile, C. Parvum, and C. cayetanesis.
We can treat Carlos with broad spectrum antibiotics. Specifically tetracycline for 6 months
Jacob, a 60-year-old man, presents to the gastroenterology clinic with chronic watery diarrhea, weight loss, and signs of malnutrition. He has a history of Crohn's disease, for which he underwent a small bowel resection 6 months ago, removing a large portion of the ileum and proximal colon. Since the surgery, he has steatorrhea, diarrhea, malabsorption, poor appetite, and has lost 20 pounds. He now reports fatigue, tingling in his feet, and muscle cramping.
What is the diagnosis?
How do you treat this patient?
1.) Short Bowel Syndrome
2.) Diet modification - high complex carbs, low fat diet, electrolyte, Loperamide for treatment of diarrhea. Bile salt-binding resins such as cholestyramine can help with diarrhea.
Aisha, a 28-year-old woman, presents to the clinic with complaints of bloating, crampy abdominal pain, flatulence, and diarrhea that occur after meals, especially when she eats ice cream, yogurt, or milk. She reports that her symptoms typically begin within 30 minutes to 2 hours after consuming dairy. She denies blood in the stool, fever, or weight loss. She is otherwise healthy and takes no medications. Physical examination is normal. Stool studies are negative for blood and infection.
What test can you order to confirm your suspected diagnosis?
How do you treat this patient?
1.) Hydrogen breath test.
The patient will drink 50-75g of lactose. If there is 20ppm increase in H in 90 minutes, this indicates malabsorption of lactose. Based on her symptoms Aisha would likely have a positive result.
2.) Lactase enzyme prep
Lactose free diet
Maya, a 63-year-old woman with a history of cirrhosis due to hepatitis C, presents to the emergency department with abdominal pain, fever, and progressive confusion over the past 24 hours. Her family reports she has been more lethargic and not eating well. She denies vomiting or diarrhea. On exam, she is febrile to 101.8°F (38.8°C), blood pressure is 92/58 mmHg, and her abdomen is distended, tender to palpation, with rebound tenderness and guarding. You note shifting dullness and a positive fluid wave.
1.) What is the diagnosis?
2.) What is the treatment?
1.) Primary acute peritonitis
2.) Antibiotic therapy targeting the underlying abnormalities?
For Maya, ceftriaxone is a good initial treatment.
Marcus, a 70-year-old man, is hospitalized following a laparoscopic colectomy for colon cancer. On post-op day 3, he develops progressive abdominal distention, nausea, and inability to pass gas or have a bowel movement. He denies significant abdominal pain but reports persistent bloating and discomfort. He has not vomited. He is tolerating sips of water.
On physical exam, his abdomen is distended but nontender with decreased bowel sounds. No rebound or guarding is noted. Vital signs are stable.
You order an abdominal x-ray. What do you find?
What is the treatment?
1.) A supine abdominal X-ray shows diffusely dilated loops of bowel (small and large) with no transition point and no air-fluid levels.
2.) Treat the primary or surgical disease.
In Marcus' case we need to ensure bowel rest to reduce distention and further dysfunction.
Eleanor, an 82-year-old woman with a history of stroke and dementia, is admitted to the hospital for pneumonia. On hospital day 5, she develops progressive abdominal distention, nausea, and mild abdominal discomfort, but has no bowel movements or flatus. She has no history of recent surgery. On physical exam, her abdomen is tense and distended, but only mildly tender, with decreased bowel sounds. There is no rebound or guarding, and no signs of peritonitis. Vital signs are stable.
An abdominal X-ray shows marked colonic dilation, especially of the cecum (up to 11 cm), without evidence of air-fluid levels or a transition point.
1.)What is the diagnosis
Ogilvie's syndrome
(Acute colonic pseudo-obstruction)

Catherine, a 45-year-old woman with a history of systemic lupus erythematosus (SLE) and prior abdominal surgery, presents with intermittent abdominal bloating, early satiety, nausea, and vomiting for the past 6 months. Her symptoms wax and wane, but she has had multiple ED visits for what was thought to be bowel obstruction. However, CT scans have consistently shown dilated loops of bowel without any transition point.
She also reports alternating episodes of diarrhea and constipation, and a recent 12-pound weight loss. After a recent meal, she vomited undigested food 2 hours later.
What is the treatment?
What is the diagnosis?
1.) NG tube, IVF
2.) Diagnosis is chronic intestinal pseudo-obstruction with gastroparesis
James, a 66-year-old man, presents to the emergency department with acute-onset, crampy abdominal pain that started 12 hours ago. He describes it as colicky and notes nausea, vomiting, obstipation, and progressive abdominal distention. He hasn't passed flatus or had a bowel movement in over a day. He had abdominal surgery 10 years ago for a perforated ulcer.
On arrival, he appears lethargic.
Vitals:
HR: 108 bpm
BP: 100/64 mmHg
Temp: 99.2°F
RR: 18
On exam:
Abdomen is distended and tympanic
Tinkling, high-pitched bowel sounds are noted early during auscultation
Later, bowel sounds become hypoactive
No rebound or guarding, but diffuse mild tenderness
A well-healed surgical scar is noted across the lower abdomen.
What imaging should you order?
Based on his clinical presentation, what would you expect to find on his imaging?
What is the diagnosis?
What is the treatment?
1.) Abdominal Series x-ray: Supine/upright abdomen, upright chest
- CT oral contrast
2.) Free air, pneumatosis intestinalis, proximal bowel distention, distal bowel collapse
3.) Small Bowel Obstruction
4.) Surgery

Gloria, a 74-year-old woman with a history of chronic constipation and diverticulosis, presents with progressive abdominal distention, abdominal discomfort, and inability to pass stool or flatus for the past 3 days. She reports mild nausea but no vomiting. She has unintentionally lost 15 pounds over the last few months. Her last bowel movement was 4 days ago. She denies recent surgeries. An x ray was ordered showing dilated loops of colon, visible haustra, no gas in the rectum and a cecum that measures 10.5 cm.
What is the diagnosis?
Large Bowel Obstruction
65% of large bowel obstructions are caused by -----------------.
adenocarcinoma
What is the most common site of large bowel obstruction?
Sigmoid colon
What is the triad for intussusception?
Vomiting
Abdominal pain
Passage of blood per rectum "currant jelly stools"
Noah, a previously healthy 2-year-old boy, is brought to the emergency department by his parents because of intermittent episodes of intense abdominal pain over the past 6 hours. During these episodes, he draws his knees up to his chest and cries inconsolably for a few minutes, then appears relatively normal between episodes. He has vomited twice and now appears more lethargic.
His parents report one episode of a "jelly-like" stool mixed with blood and mucus. He has no history of recent travel, diarrhea, or antibiotic use.
What tests are needed to confirm diagnosis?
What is the treatment?
1.) Radiographs, CT scan, or US
2.) Since this is a child, contrast or air enema can treat the patient.
If Noah were an adult, he would need surgery
He has intussusception
Olivia, a 21-year-old college student, presents to the emergency department with abdominal pain that started about 18 hours ago. She reports that the pain began around her belly button but has since migrated to the right lower quadrant (RLQ). She also has experienced nausea, anorexia, and low-grade fever. She denies diarrhea or urinary symptoms.
On physical exam:
Temp: 100.6°F (38.1°C), HR: 102 bpm
Based on these symptoms would you find on physical exam?
What would her abdominal exam reveal?
What tests would you order?
What is the diagnosis?
What is the treatment?
1.) Abdominal exam reveals:
Tenderness in the RLQ at McBurney's point
Rebound tenderness
Positive Rovsing's sign (pain in RLQ when pressing on LLQ)
Positive psoas sign
2.) WBC - mild elevation with left shift
CT-Scan --> dilation greater then 6 mm with wall thickening. Fatty tissue or air around appendix
The patient is an adult, so it would not be ordered here, but in children, US is the popular choice.
3.) Acute Appendicitis
4.) Surgery needed - appendectomy
Leo, a 2-year-old boy, is brought to the pediatric emergency department by his parents due to painless rectal bleeding. They report he passed a large amount of bright red blood mixed with stool earlier today. He has no fever, no abdominal pain, and has been otherwise acting normally. He has no history of constipation, diarrhea, or recent illness.
What test should be ordered?
What is the diagnosis?
What is the treatment?
1.) Meckel's scan
2.) Meckel's diverticulitis
3.) Surgery

List of the rule of 2s. Which condition are the found in?
2% of population
2 ft from ileocecal valve
2% symptomatic
2 in in length
2 types of ectopic tissue (gastric or pancreatic)
2 yrs old- time of presentation
2 times more M > F
Meckel's Diverticulum
What condition occurs when the splanchnic perfusion fails to meet demands of the intestine which leads to ischemic tissue injury?
Visceral Artery Insufficiency
Greg, a 68-year-old man with a history of atrial fibrillation and hypertension, presents to the emergency department with sudden-onset, severe abdominal pain that began 4 hours ago. He describes the pain as diffuse, steady, and worsening. He also reports nausea and vomiting, but no bowel movement or flatus today. He appears anxious and uncomfortable, repeatedly stating, "This is the worst pain I've ever had."
On physical exam:
Temp: 99.5°F, HR: 116 bpm (irregularly irregular), BP: 130/74
Abdomen: soft, non-distended, minimal tenderness, no rebound or guarding
Exam is strikingly out of proportion to the severity of pain reported
The following labs were ordered:
WBC: 18,400/mm³
Lactate: elevated
ABG: Metabolic acidosis
EKG: Atrial fibrillation
Imaging not yet performed.
What is the next best step?
Immediate exploratory laparotomy (emergent surgery)
Not CT Angiography -- Surgery should not be delayed for imaging when signs of infarction or perforation are present.
He has acute mesenteric ischemia
Based on the below description on visceral artery insufficiency, what is type of ischemia is present?
Occlusive arterial disease - embolic or thrombosis
Acute Mesenteric Ischemia
Based on the below description on visceral artery insufficiency, what is type of ischemia is present?
low flow due to heart failure, sepsis, hypotension
Nonocclusive mesenteric ischemia
Based on the below description on visceral artery insufficiency, what is type of ischemia is present?
"angina", demand not met during feeding
Chronic mesenteric ischemia
Based on the below description on visceral artery insufficiency, what is type of ischemia is present?
variant, inferior mesenteric artery- ischemia and sloughing
Ischemic colitis
What are the most common locations of mesenteric vascular insufficiency?
Griffith's point and Sudeck's point
Margaret, a 74-year-old woman with a history of hypertension, coronary artery disease, and atrial fibrillation, presents to the emergency department with sudden-onset crampy left lower quadrant (LLQ) abdominal pain and bloody diarrhea that started earlier today. She reports having similar, milder symptoms in the past after long walks, but nothing this severe. She is on warfarin for atrial fibrillation.
Based on this information what is her diagnosis?
Ischemic Colitis
Erica, a 38-year-old woman with a history of systemic lupus erythematosus (SLE) and recurrent miscarriages, presents to the ED with gradual-onset abdominal discomfort over the past 2 days. She reports a dull, crampy abdominal pain that worsens after eating. She also notes bloating, nausea, and one episode of dark stool. She denies vomiting or prior GI issues.
Physical Exam:
Vitals: HR 98 bpm, BP 124/80, Temp 99.1°F
Abdomen: Distended, mild diffuse tenderness, no peritoneal signs
What test is needed to diagnose this condition?
What is the treatment?
1.) Spiral CT angiography
2.) Anticoagulation, bowel rest
She has chronic mesenteric ischemia
What are the two types of diverticula?
Explain the difference between them.
True: Saclike herniation through the entire bowel wall
False/pseudo = Involves only protrusion of mucosa and submucosa through the muscularis propria - most commonly affecting the colon
Which structure of the GI system is always spared in diverticular disease?
Rectum
What is the most common cause of hematochezia in patients greater than 50?
Hemorrhage
Diverticular disease commonly affects the --------- colon.
left sigmoid
Thomas, a 70-year-old man with a history of hypertension and chronic constipation, presents to the emergency department after experiencing sudden onset of painless bright red blood per rectum. He denies abdominal pain, nausea, vomiting, fever, or recent changes in bowel habits. He reports passing a large amount of blood in the toilet but feels otherwise well.
Vitals: HR 98 bpm, BP 112/70, Temp 98.9°F
Abdomen: Soft, non-tender, no distention
Rectal exam: Bright red blood in the rectal vault, no masses
What should you do next?
Order a colonoscopy. The patient likely has diverticular bleeding and is stable.
How do you treat a stable patient with diverticular bleeding ?
You can order IR angiography for coil embolization.
For context, coil embolization is a minimally invasive procedure where a metal coil is inserted into bleeding vessel to stop the hemorrhage.
Colonoscopy with epi injection may also be used.
How to treat an unstable patient with diverticular bleeding?
emergent surgery
Leonard, a 63-year-old man with a history of chronic constipation, presents to the ED with 4 days of worsening left lower quadrant (LLQ) abdominal pain, fever, and nausea. He reports decreased appetite and loose stools, but no vomiting. He noticed some streaks of blood on the toilet paper. He also complains of mild bloating. He has never had anything like this before.
Temp: 101.4°F, HR: 96, BP: 134/78
Abdomen: Tenderness with mild guarding in the LLQ, no rebound
A palpable mass is appreciated in the LLQ
Rectal exam: positive FOBT
Workup:
CBC: WBC 15,400/µL
CMP: mild electrolyte imbalance
KUB X-ray: shows air-fluid levels suggestive of possible ileus
CT abdomen/pelvis with contrast:
- Sigmoid wall thickening
- Fat stranding
- Small pericolonic fluid collection (suggesting early abscess)
What is the diagnosis?
What is the treatment?
1.) Acute diverticulitis with localized abscess
2.) Cefoxitin or Zosyn for 5-7 days
What procedure/test do you want to order once diverticulitis is resolved?
Colonoscopy, but must wait at least 6 weeks after diverticulitis
How do you treat asymptomatic diverticulitis?
Lifestyle changes
How do you treat symptomatic uncomplicated diverticular disease outpatient? No abscess.
Clear liquids for 3 days
How do you treat outpatient symptomatic diverticulitis with abscess less then 3-4cm?
Augmentin BID 7-10 days
How do you treat inpatient diverticulitis?
Inpatient - NPO, NG Tube, IVF, Abx
- Cefoxitin or zosyn 5-7 days
When would you need a surgery consult for diverticulitis?
Severe disease or failure to respond to treatment within 72 hrs
Abscess greater then 4cm --> percutaneous drainage
Generalized peritonitis, large abscesses, clinical deterioration --> surgery
Elective one stage resection after recovery
What is the size of toxic megacolon?
Greater then 6cm
What are the number one causes of toxic megacolon?
ulcerative colitis and crohn's disease.
Hirschsprung disease is a congenital aganglionic colon (neurogenic bowel obstruction) that can lead to ---------------.
Toxic Megacolon
What are the physical exam findings in someone with toxic megacolon?
Abdominal pain
Distention
Fever
Tachycardia
Dehydration
Hypotension
AMS
How do you diagnose toxic megacolon?
Kidney Ureters, Bladder (KUB) x ray
Large colon greater then 6 cm.
How do you treat toxic megacolon?
Decompression - bowel rest, NGT
Antibiotics
Colostomy in refractory cases
What are the two major types of inflammatory Bowel Disease (IBD)?
1.) Ulcerative Colitis
2.) Crohn's Disease
Which disease involves "mouth to anus" pathology?
Crohn's Disease
In CD the rectum is spared in -------%
40%
True/False CD is transmural.
True!
What is a microscopic feature that you might find in someone who has CD?
Noncaseating granulomas
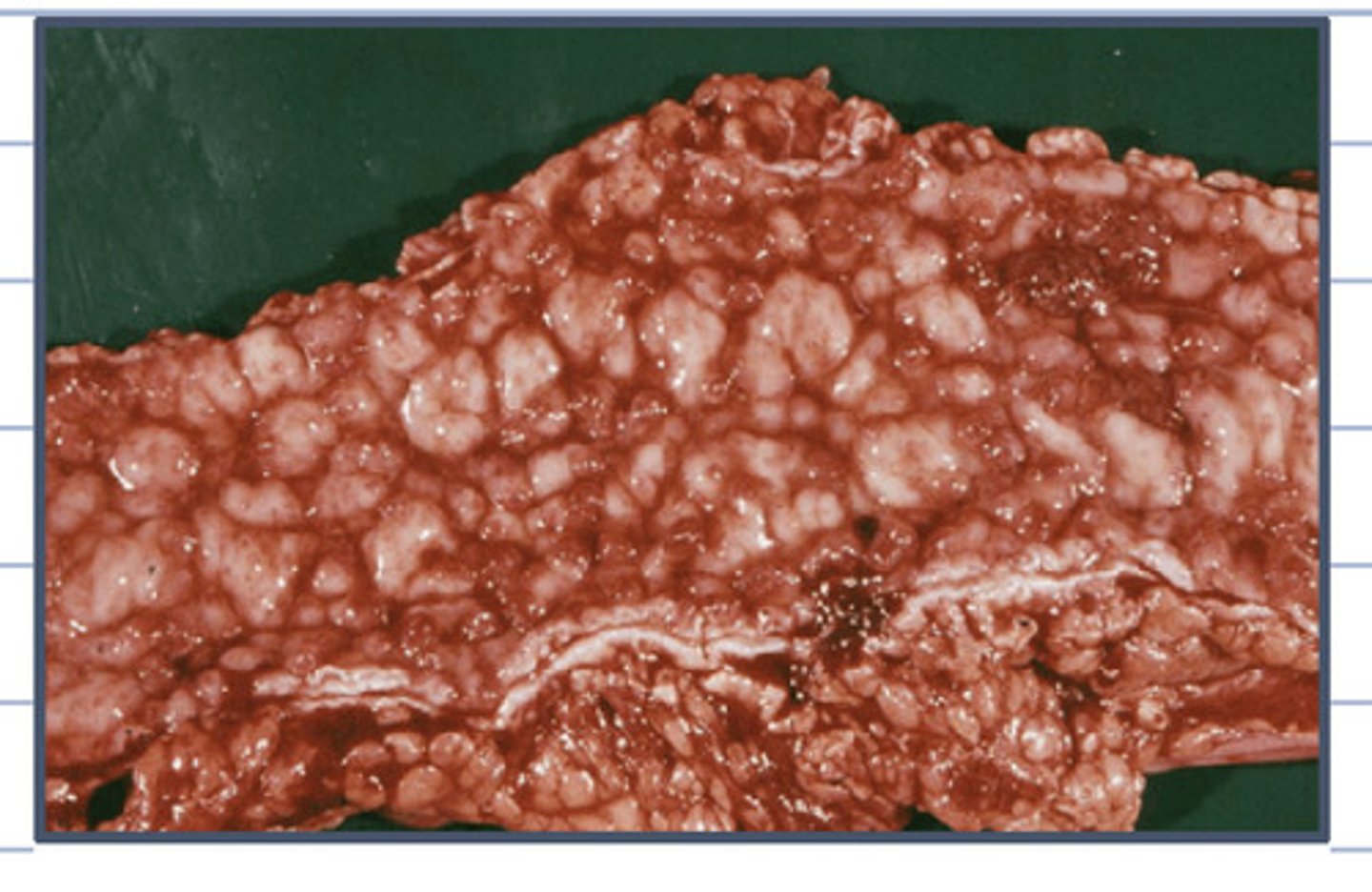
What is the gross pathology of someone with Crohn's disease?
Cobblestone appearance
What are the symptoms of Crohn's Disease?
Abdominal Pain, diarrhea (with or without bleeding), fatigue, weight loss
David, a 29-year-old man, presents to the gastroenterology clinic with a 9-month history of intermittent crampy abdominal pain, chronic diarrhea, and 15-pound weight loss. He reports fatigue, low-grade fevers, and a recent episode of nausea and vomiting. He also complains of bloating, and says his stools are often loose, oily, and difficult to flush. Over the past month, he's felt a tender mass in the right lower abdomen.
Seriologic markers indicate + ANCA and - p-ANCA.
Endoscopy indicates rectal sparing, aphthoid ulcerations, fistulas and skip lesions.
You order a biopsy and test results demonstrate that granuloma is highly suggestive.
Based on this information what sign would you see on an x ray?
What are complications associated with this diagnosis?
How do you treat this?
David has Crohn's disease
1.) Thumbprinting on x ray
2.) Complications: Rectal sparing, aphthoid/linear/stellate ulcerations, fistulas, and skip lesions
3.) Complications include fistula formation
- Rectovaginal
- Abdominal
-Enterovesical
Perianal disease
4.) Since David's disease is severe you would treat with low roughage diet (no raw fruit, nuts, vegetables), B12 and Vitamin D, low fat diet, loperamide
Medications
- Combo of biologic (Anti-TNF) + Immunomodulator medications for induction
Prescribe infliximab + Azatheoprine or 6-Mercaptopurine
How do you treat mild Crohn's Disease?
Loperamide up to 4x for diarrhea
Balanced diet, smaller but more frequent meals, hydration, dairy restriction.
What is the most affected site of Crohn's disease?
Terminal Ileum
What are symptoms of gastroduodenal disease?
N/V
Epigastric Pain
H. Pylori negative gastritis
What are symptoms of jejunoilelitis?
Malabsorption, nutritional deficiencies and steatorrhea, diarrhea
Recurrent colicky RLQ pain relieved by defecation and diarrhea. Pronounced RLQ pain and palpable mass.
Ileocolitis
Crampy abdominal pain
Hematochezia, fecal urgency
- Gross bleeding not as common as it is in ulcerative colitis
Colitis
Fecal incontinence
Large hemorrhoidal tags
Anal strictures
Anorectal fistulae
Perirectal abscesses
Perianal Disease
Diagnostic Findings:
Elevated ESR and CRP
Hypoalbuminemia
Anemia
Leukocytosis
Fecal calprotectin and lactoferrin
Serological Markers:
+ ASCA, - p-ANCA
Exclude infectious colitis
Crohn's Disease Diagnostic tests.
What would you find on a CD CT?
Multiple strictures and hyper-vasculature on recon CT
When would you use 5-ASA?
Use it only in mild cases of Crohn's if there is a desire to avoid steroids.
When would you use Mesalamine 2.4g PO daily?
Ileocolonic disease
When would you use sulfasalazine 1.5-3 g PO daily?
Mild colonic disease only
What are the criteria that should be used to determine if Crohn's mild treatment is appropriate?
Normal to mild increases in CRP/fecal calprotectin
Dx > 30 years of age
Limited distribution
Superficial ulceration
Lack of perianal complications
No resections
No fistulas
What are the criteria that should be used to determine if Crohn's moderate to severe treatment is appropriate?
● Diagnosis at a younger age (<30 years)
●History of active or recent tobacco use
●Elevated C-reactive protein and/or fecal calprotectin levels
●Deep ulcers on colonoscopy
●Long segments of small and/or large bowel involvement
●Perianal disease
●Extra-intestinal manifestations
●History of bowel resections
How do you treat severe Crohn's disease?
Combo of Biologic (Anti-TNF) + immunomodulator medications for induction (especially of disease with fistula).
Monotherapy without fistula
Monotherapy for over 60 or young males at risk for infection/maligancy
What medication options are used to treat severe Crohn's with fistula ?
Anti TNF + Immunomodulator medications for induction
Infliximab (Remicade) + Azatheoprine (Imuran) or 6-Mercaptopurine (Purinethol)
Adalimumab (Humira) + Azatheoprine or 6-Mercaptopurine
What medication options are used to treat severe Crohn's without fistula in biologic naive patients?
Monotherapy induction for disease without fistula (Biologic naive)
Anti-IL 12/23 -Ustekinumab (Stelara)
Anti-Integrin - Vedolizumab (Entyvio)
What medication options are used to treat severe Crohn's without fistula in men over 60 or young males at risk for infection or malignancy
infliximab
How to treat moderate to severe Crohn's disease with monotherapy?
Monotherapy induction with Budesonide or Prednisone
8 weeks, then bridge to biologic, thiopurine or Methotrexate
What is the maintenance therapy for Crohn's Disease in moderate to severe disease?
Monotherapy induction with Budesonide or Prednisone
8 weeks, then bridge to biologic, thiopurine or Methotrexate
What percentage of those with CD have moderate to severe disease?
50%
Abscesses
Hemorrhage
Fistula
Obstruction
How do you treat mild Crohn's disease on the right side?
•5-ASA (Mesalamine or Sulfasalazine) ORAL.
OR
•Budesonide
How do you treat mild, diffuse or left sided Crohn's disease?
Prednisone
How you treat moderate to severe Crohn's disease?
Anti-TNF + Immunomodulator (Infliximab + Azatheoprine/6-mercaptopurine)
Anti-IL 12/23 (Stelara)
Anti-Integrin (Entyvio)
Ulcerative colitis involves pathology in -----------% of the rectum.
100
Involves rectum – 100%
Extends proximally to involve all or part of the colon
Submucosal/mucosal involvement
Microscopic features
Crypt architecture of the colon is distorted
Basal plasma cells and multiple basal lymphoid aggregates
Pathology of Ulcerative Colitis
Lena, a 32-year-old woman, presents to the clinic with a 3-month history of frequent episodes of bloody diarrhea. She reports 7-8 loose stools per day, often associated with urgent bowel movements and abdominal cramping, especially in the lower left quadrant. She also mentions fatigue, mild weight loss, and intermittent low-grade fevers. She denies recent travel, antibiotic use, or sick contacts. No joint or skin symptoms.
On physical exam, Lena appears tired but stable. Her abdomen is soft with mild LLQ tenderness, no rebound or guarding. Rectal exam reveals gross blood. Infectious colitis was ruled out.
What serological markers help confirm this diagnosis?
What procedural diagnostic test is used to assess the severity of the condition prior to treatment?
How severe is this condition?
What is the condition?
What is the treatment?
1.) -ASCA, + p-ANCA
2.) Sigmoidoscopy
3.) Due to the stool frequency being greater then 6 and fevers. Lena has severe UC.
4.) Treatment - Prednisone 40mg daily slowly taper after improvement. Add inflixmab to maintain. If there is severe hemorrhage, perforation or carcinoma, surgery is needed.
Moderate Ulcerative Colitis
Stool Per day?
Pulse Bpm?
Hematocrit%?
Weight Loss%?
Temperature?
ESR?
Albumin?
Stools per day ---- 4-6
Pulse Bpm -------- 90-100
Hematocrit % ----- Normal
Weight loss % ------- None
Temperature ----- Normal
ESR --- <20
Albumin ---- Normal
What is the mild to moderate treatment for ulcerative colitis in rectum and rectosigmoid?
Mesalamine suppository 1000mg PR QHS: Proctitis
Mesalamine enema 4g QHS: Proctosigmoiditis
What is the mild to moderate treatment for proximal to sigmoid UC?
Combo oral Mesalamine 2-3 g PO daily and rectal 5-ASA
Add Budesonide 9mg daily 4-8 wks for resistance disease
Infliximab + Thiopurine are treatments for -------------------.
Severe UC
What are the complications of UC?
Toxic megacolon
Stricture
Malignancy
What are the extraintestinal symptoms of inflammatory bowel disease?
Erythema Nodosum
Peripheral arthritis - Most common
Pyoderma Gangrenosum
Primary Sclerosing cholangitis
What area is affected in UC?
Limited to the colon begins in the rectum and spreads proximally to the colon.
RECTUM ALWAYS INVOLVED
What layers does ulcerative colitis penetrate?
mucosa and submucosa only
What are the clinical manifestation of UC?
LLQ Pain - Colicky
Tenesmus - urgency
Bloody diarrhea = HALLMARK
What are the complications of UC?
Colon Cancer
Toxic mega colon
Smoking lowers risk for ---
UC
What findings would a colonoscopy of UC reveal?
Uniform inflammation +/- ulceration in rectum and/or colon "sandpaper" appearance. Pseudopolyps
What are you findings in barium studies of UC?
"Stovetop sign" or "Lead pipe" - Loss of haustral markings
What inflammatory bowel disease has +P-ANCA?
Ulcerative Colitis