Bios 110 Unit 4
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
Types of Eaters
Carnivore
Omnivore
Herbivore
Suspension
sift food particles suspended in water through specialized structures, such as the gills
Substrate
dwell in or on their food source
Fluid
suck nutrient -rich fluids from a living host
Bulk
eat relatively large pieces of food (like us!)
Four Stages of Food Digestions
ingestion
digestion
absorption
elimination
Digestion Types
Mechanical and Chemical
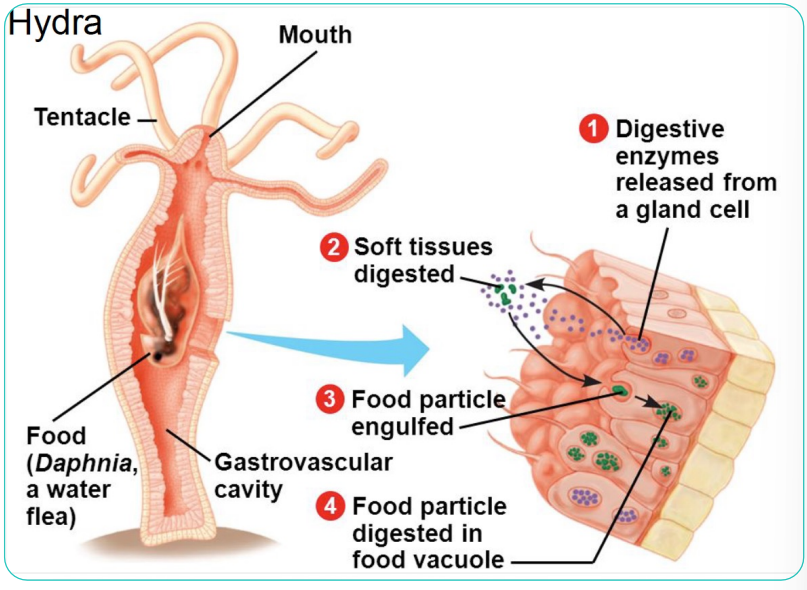
Anatomy - Gastrovascular Cavity
Digestive enzymes released from a gland cell
soft tissue digested
food particles engulfed
food particle digested in food vacuole
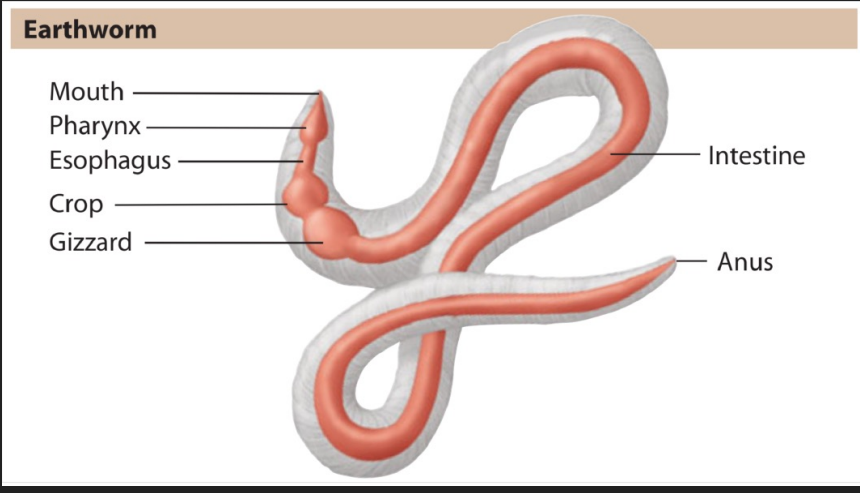
Anatomy – Alimentary Canal
Pharynx = throat
Esophagus = muscular tube that passes food to crop/stomach
Crop = softens food
Gizzard = churns and grinds food
The alimentary canal anatomy is reflective of the animal’s diets
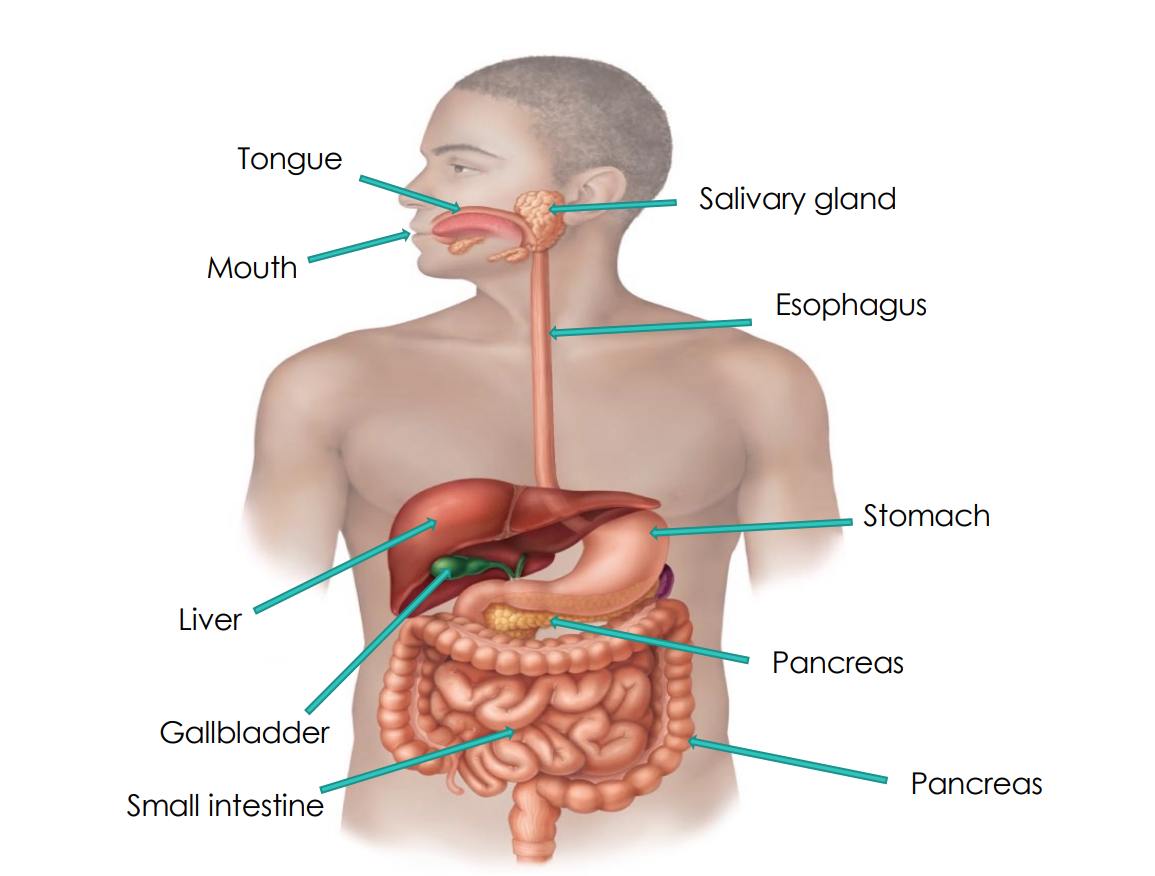
Human Digestive System
Two groups of organs
1. Alimentary canal (gastrointestinal or GI tract)
o Mouth to anus
o Digests food and absorbs fragments
o Mouth , pharynx, esophagus, stomach, small intestine and large intestine
2. Accessory digestive organs
o Teeth o Tongue
o Gallbladder
o Digestive glands
o Salivary glands
o Liver
o Pancreas
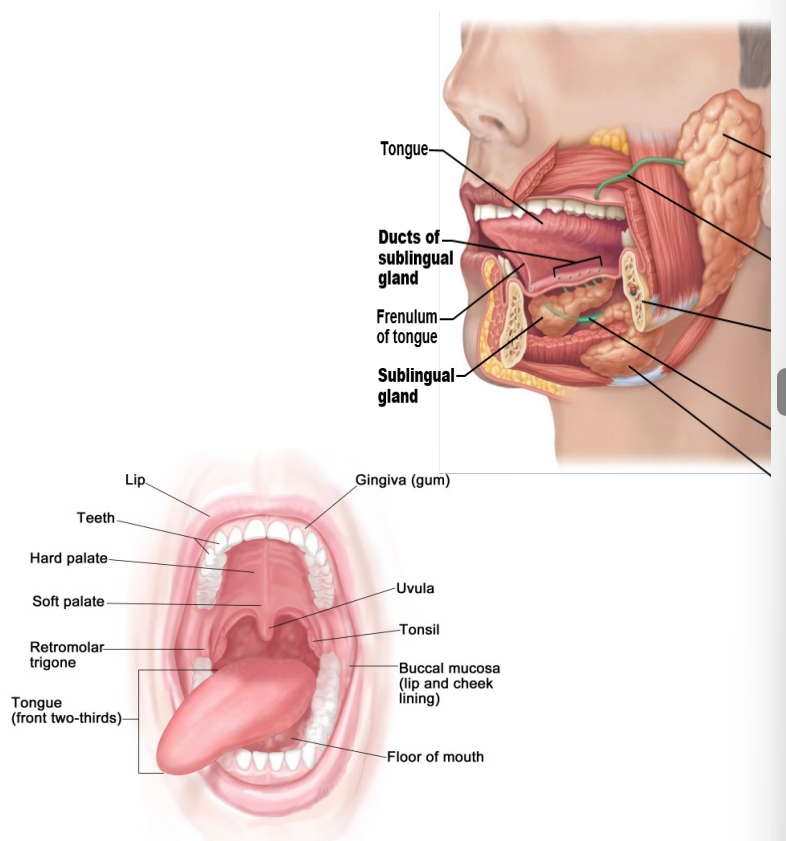
The mouth, tell me about it
The mouth and teeth are involved in mechanical digestion
Chemical digestion of carbohydrates is achieved with enzymes in saliva
o Salivary amylase
Saliva
o Mucus (lubrication)
o Buffers (neutralize)
o Antibacterial proteins
o Enzymes
What do we call food when it is in our mouth?
Bolus
Esophagus
is the hollow, muscular tube that passes food and liquid from your throat to your stomach. It functions as part of your digestive system.
Peristalsis
Adjacent segments of alimentary tract organs alternately contract and relax, moving food along the tract distally
Gastric juice, what is it made of?
Pepsin (enzyme) + HCl + mucus
What are the stimuli for gastric juice release
Smell
Stretch
parasympathetic nervous system input
Gastric pits
1. Parietal cells release HCl
2. HCl converts pepsinogen to pepsin
3. Pepsin converts pepsinogen into pepsin
Now what do we call the food after it goes down in our stomach?
Chyme !!!
Location of nutrient absorption
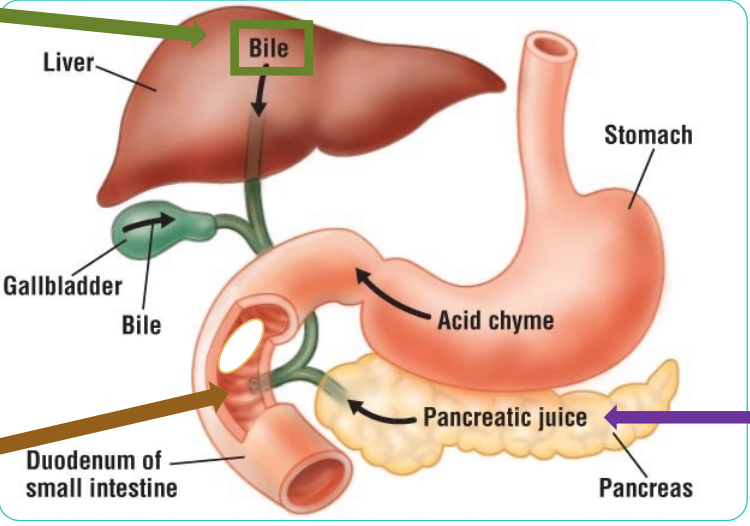
Bile (Emulsifies fat into small droplets)
Membrane bound enzymes (Chemical digestion)
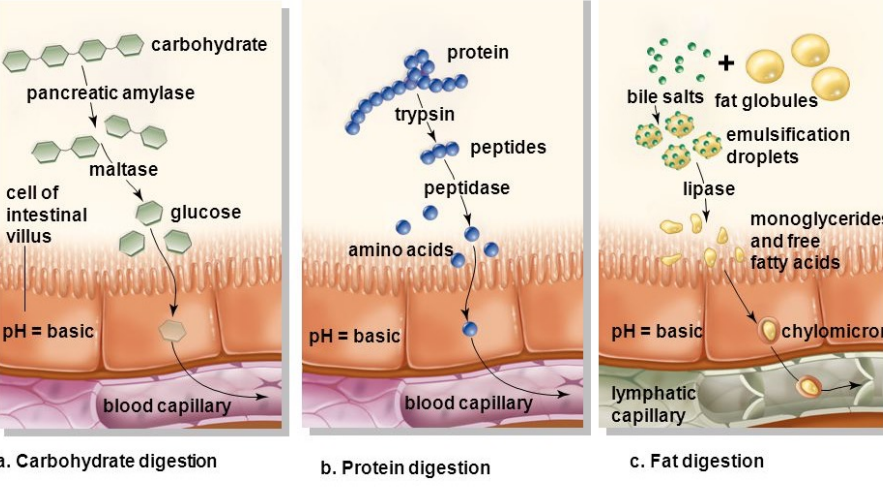
Pancreatic amylase (starch —> maltose)
Pancreatic lipase (triglyc. —> fatty acid + glycerol)
Pancreatic endopeptidase (protein—> amino acid)
Nuclease (DNA/RNA —> nucleotides)
Bicarbonate ions (neutralize stomach acids)
High surface are = what now?
High absorptive capacity
High Surface Area = High Absorptive Capacity
The transport of glucose and amino acids relies on secondary active transport whereas lipids are able to diffuse across the call of the small intestine due to their solubility.
However, lipid size limit their ability to get deposited in the blood so they first have to travel through lymphatic vessels while glucose and amino acids can directly go to the blood.
largely polar (carbohydrate & protein digestion)
What is the large intestine important for?
Water regulation
large intestine details, humans vs animals
Animals
plants are harder to digest then meat (animals have an easier doing this)
Humans
do not have the enzymes to break down plants
Fiber is super important
do not have cellulate
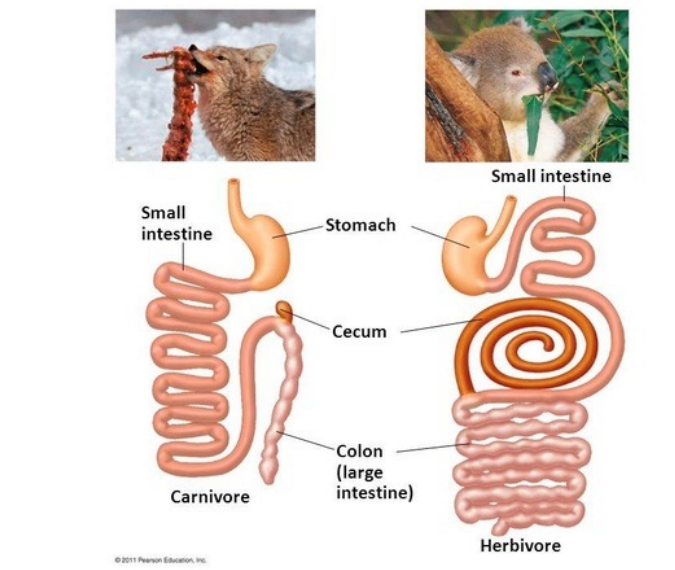
Anatomy reflects diet
Shorter tract Smaller stomach, cecum and colon for easy to digest meat
Longer tract Larger stomach, cecum and colon for difficult to digest plants
Why do we have a circulatory system?
We need a highway system to transport
• O2 and CO2
• Nutrients
• Water
• Hormones
• Immune Cells
• Waste
• Heat
But not all organisms need a circulatory system!
Some organisms are so thin and branched that their cells can connect with the outside world
However, this limits how large an organism can be
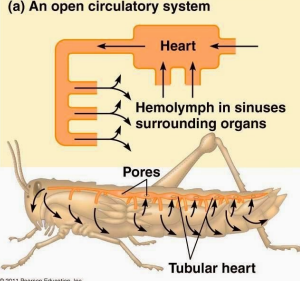
Open circulatory System
All organs are bathed and are floating in the hemolymph so no vessels
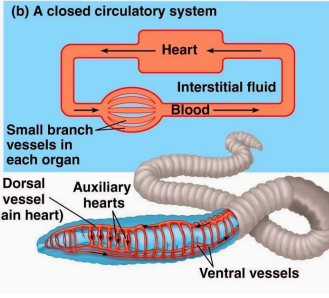
Close circulatory system
Blood is contained within vessels
Blood and interstitial fluid are separate
Explain the closed circulatory system
Arteries carry blood away from heart
Location of exchange; travel through tissues
veins carry blood towards heart
What is the difference between open and closed circulatory systems
Open
not under high pressure so not susceptible to hemorrhage
metabolically cheap
can’t distribute blood to specific tissues
Slow so not good for larger or metabolically very active animals
Closed
Can increase blood specific metabolically active tissues
can limit blood flow to the surface to decrease or increase heat exchange
fast so good for large or metabolically very active animals
under pressure so susceptible to hemorrhage
metabolically expensive
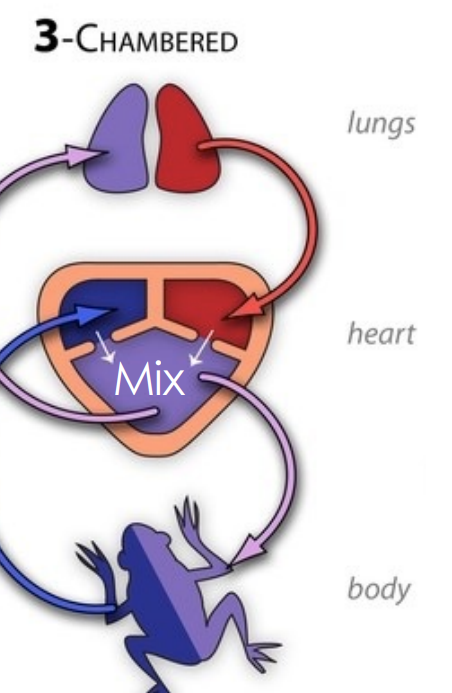
Types of closed circulatory system
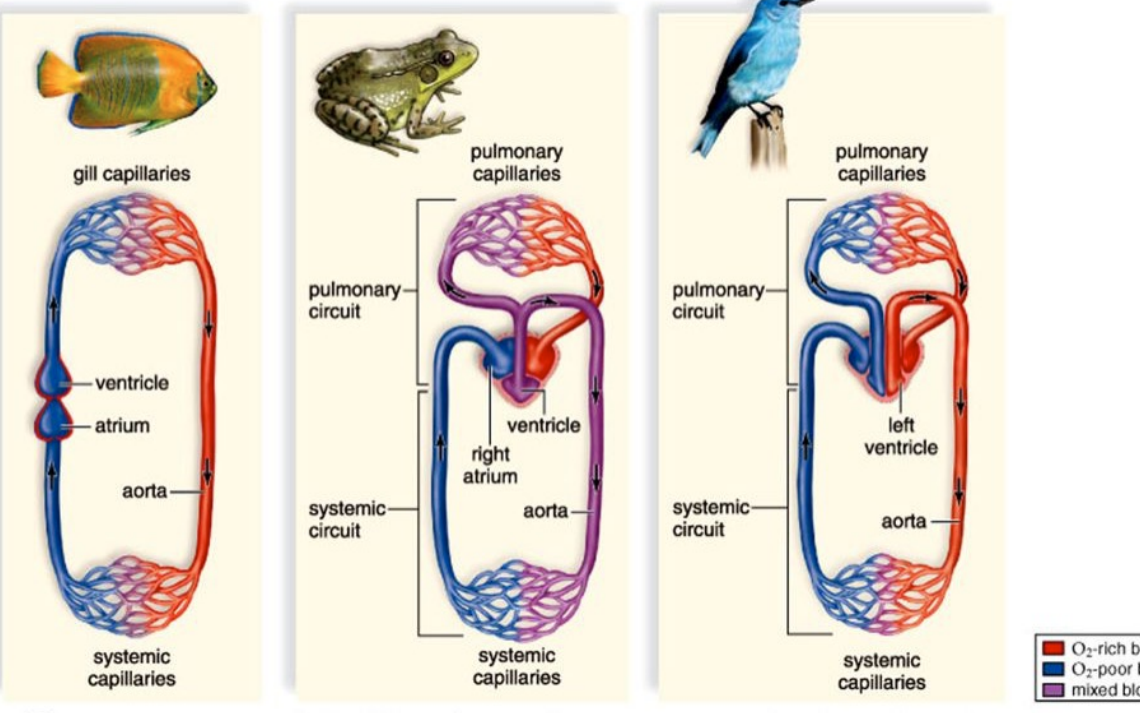
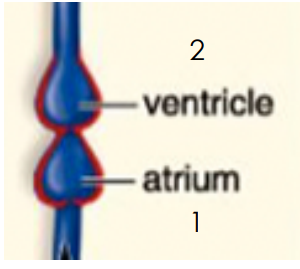
Gill capillaries (fish)
Blood flows through atria to ventricle
decrease in pressure
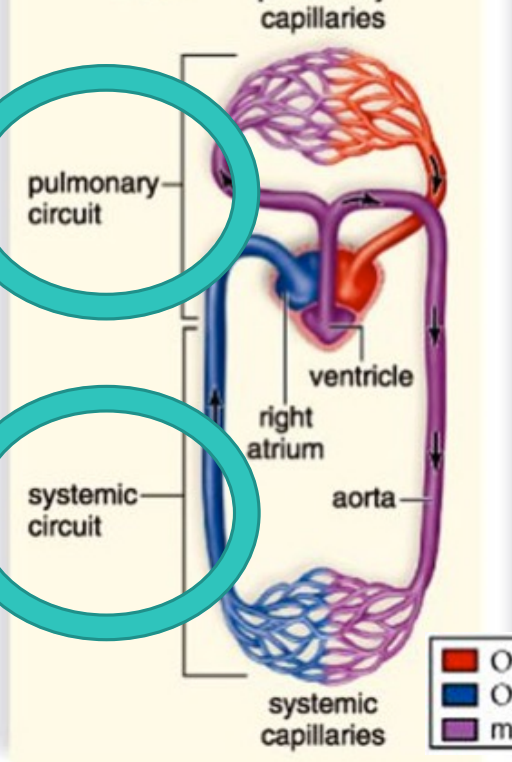
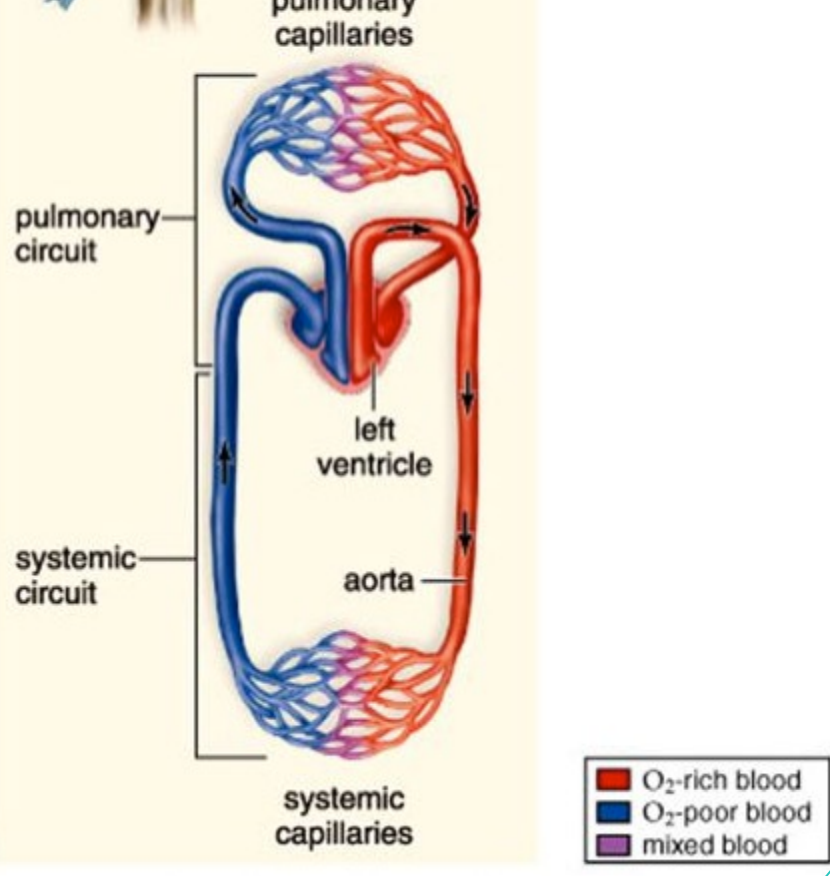
Pulmonary capillaries (frog)
Pulmonary circuit
Systemic circuit
2 atria and 1 ventricle
3 chambered
blood and O2 mix
Pulmonary Capillaries (bird)
2 atria
2 ventricles
blood and O2 does not mix
Pulmonary Circulation
1.Right ventricle
2.Pulmonary artery
3. Lungs
4.Pulmonary vein
5. Left atrium
Systemic Circulation
6. Left ventricle
7. Aorta
8. Body tissues
9. Vena cava
10. Right atrium
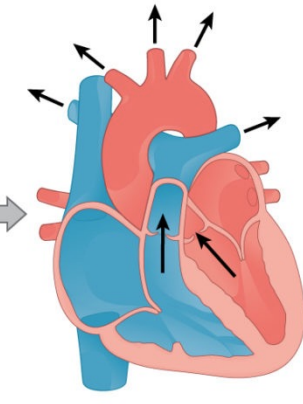
Diastole
Heart is relaxed Blood is entering atria
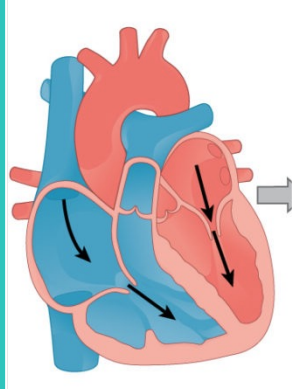
Systole
Heart contracts Blood is moving through and out of heart
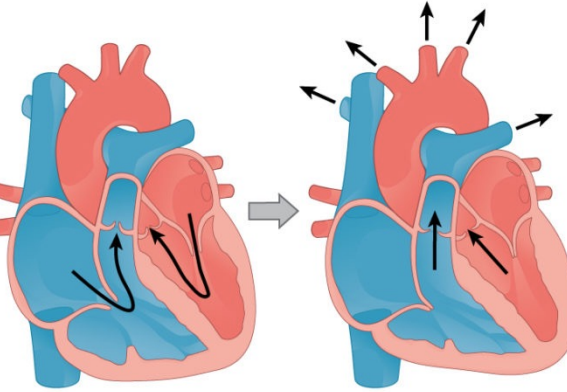
Atrial Systole
Atria contract Blood moves from atria to ventricle
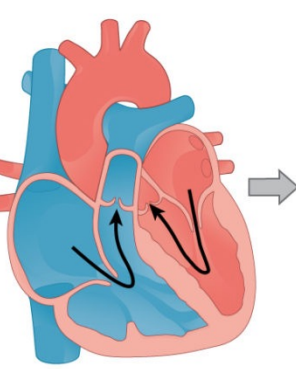
Ventricular Systole
Ventricles contract Blood moves from ventricle to arteries
When does the cardiac cycle occurs?
72 time/minute
diastole - 0.4 sec
systole - 0.1 sec and 0.3 sec
You can hear this!
Semilunar valves closing = “dub”
AV valves closing = “lub”
What causes these chambers contract and valves close?
Electrical impulses resulting in pressure changes
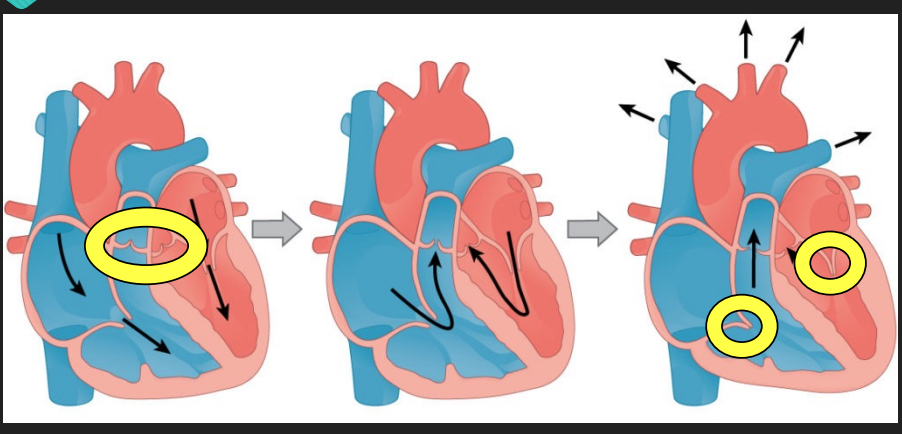
Cardiac muscle cells are what?
conductive and contractile
Intercalated discs = gap junctions
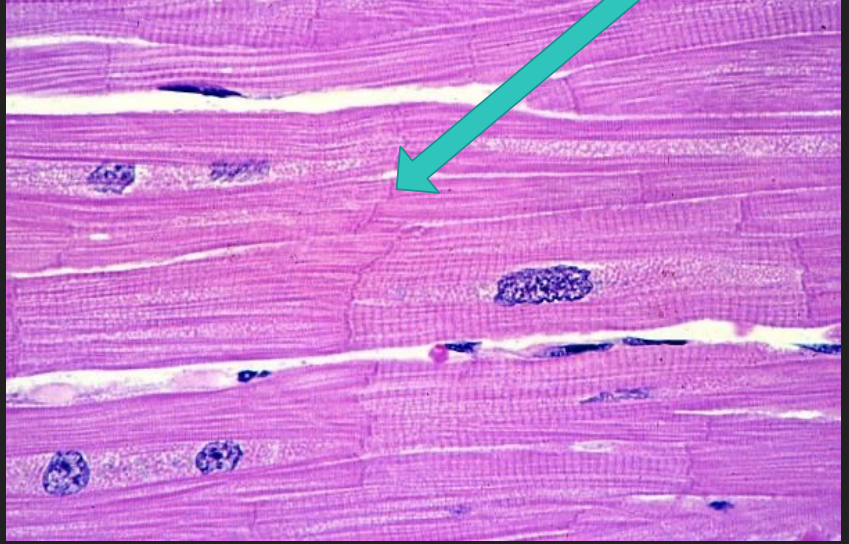
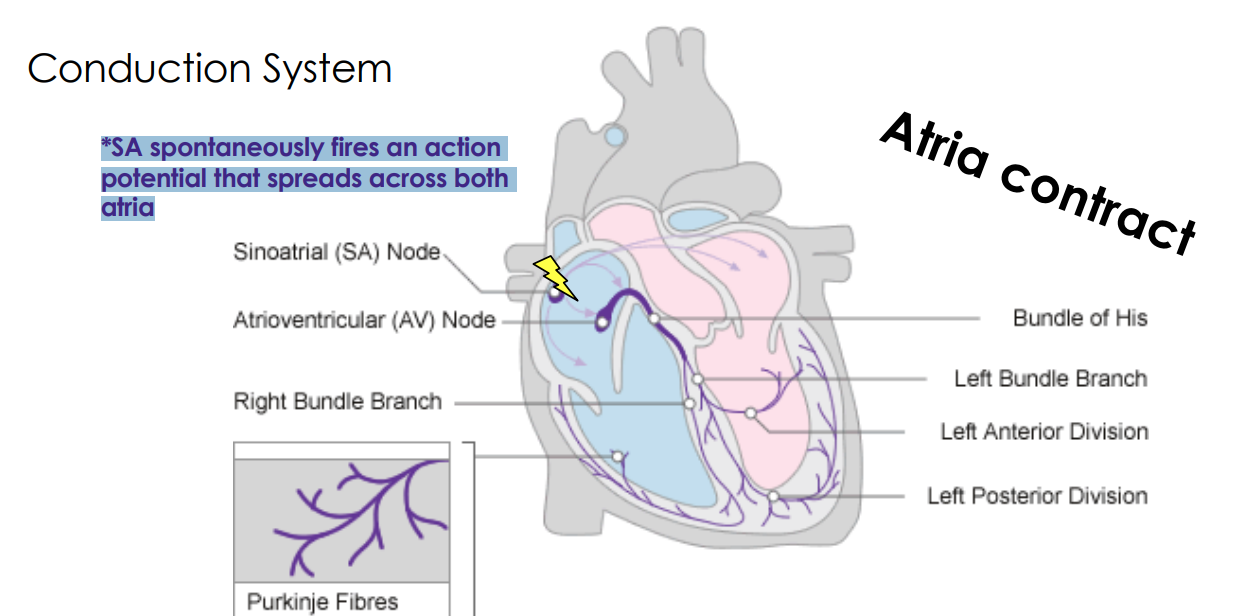
Atria contract
*SA spontaneously fires an action potential that spreads across both atria
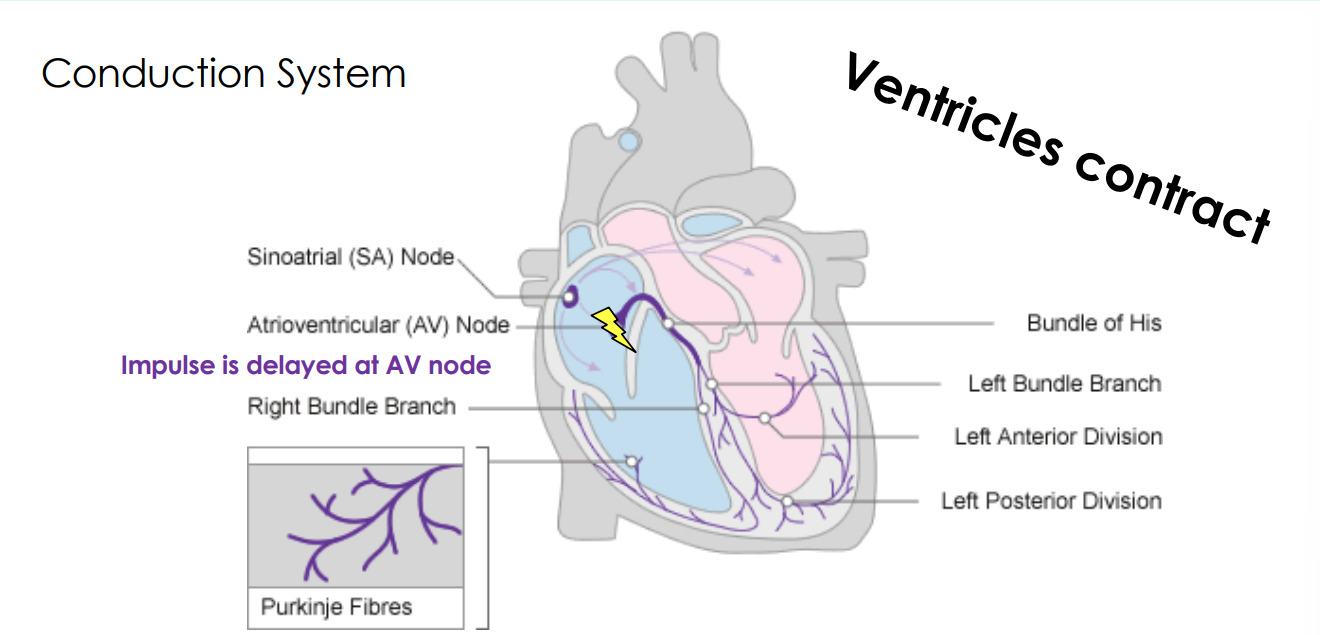
Ventricles contract
Impulse is delayed at AV node
Artery and vein has 3 layers what are they?
Epithelial layer
Muscular layer
Connective tissue layer
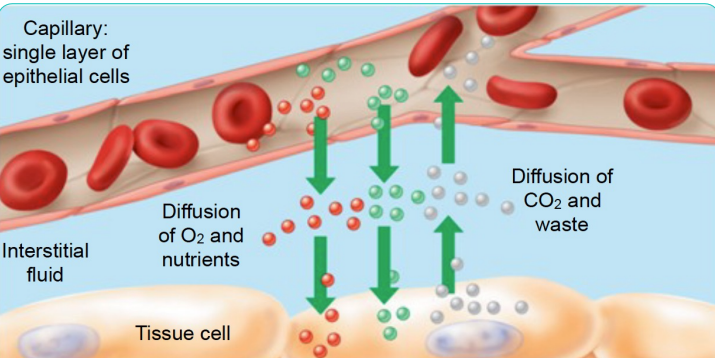
Capillary Exchange pt.1
The capillary wall is thin to allow for exchange of necessary materials (e.g., O2 and CO2), but not blood cells.
o Blood pressure also causes fluid to leave the capillary and enter the extracellular space
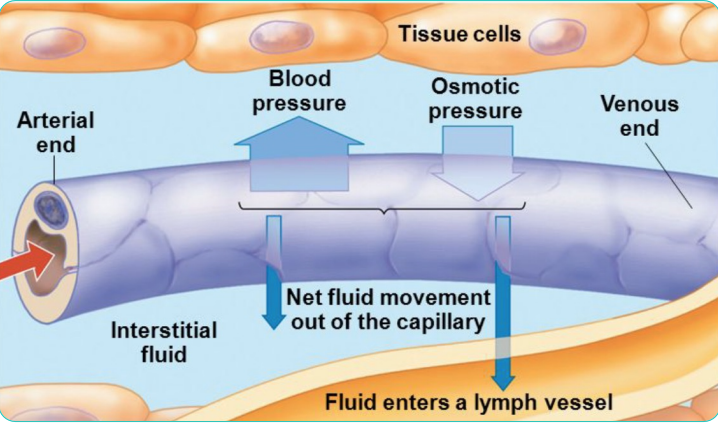
Capillary Exchange pt.2
The vein collects some, but not all, of the fluid leaked into the extracellular space due to osmotic pressure.
The excess interstitial fluid is collected by the lymphatic system
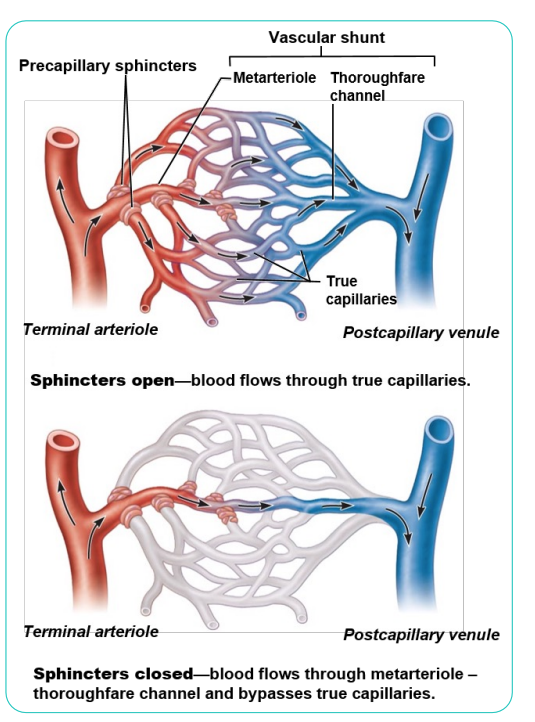
Distribution of Blood
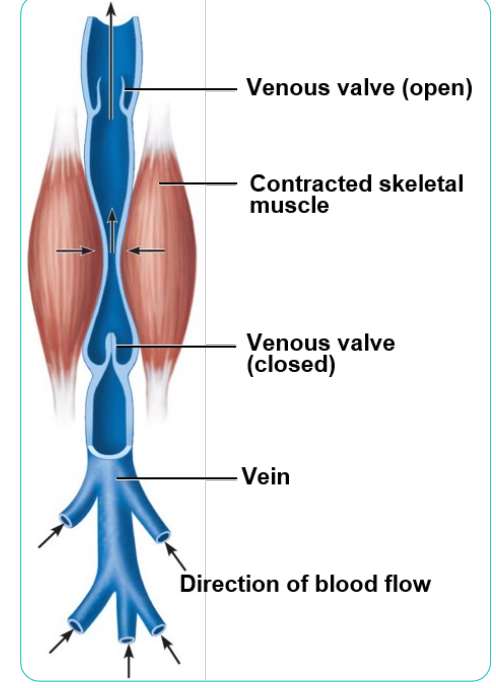
Venous Blood Pressure
1. Muscular pump: contraction of skeletal muscles "milks" blood toward heart 2. Respiratory pump: pressure changes during breathing move blood toward heart by squeezing abdominal veins as thoracic veins expand
3. Valves
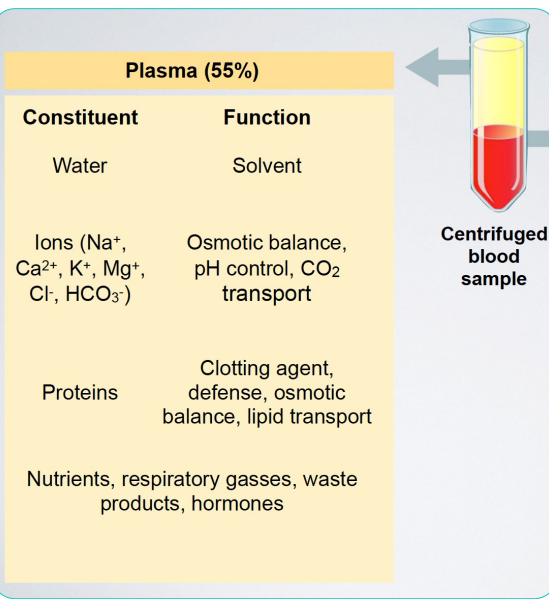
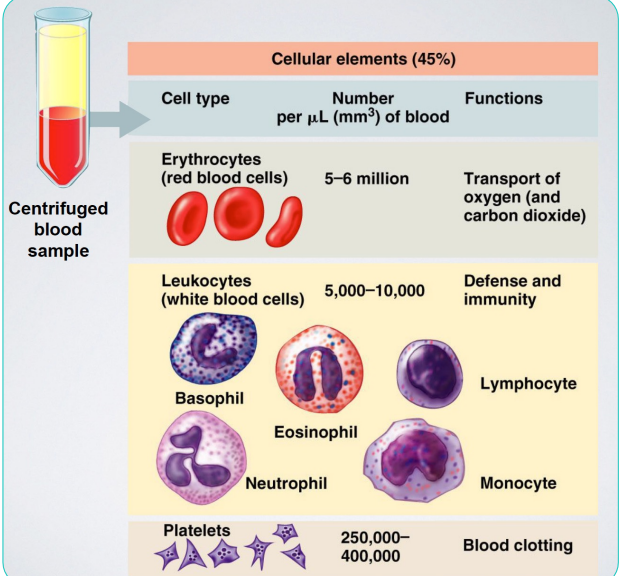
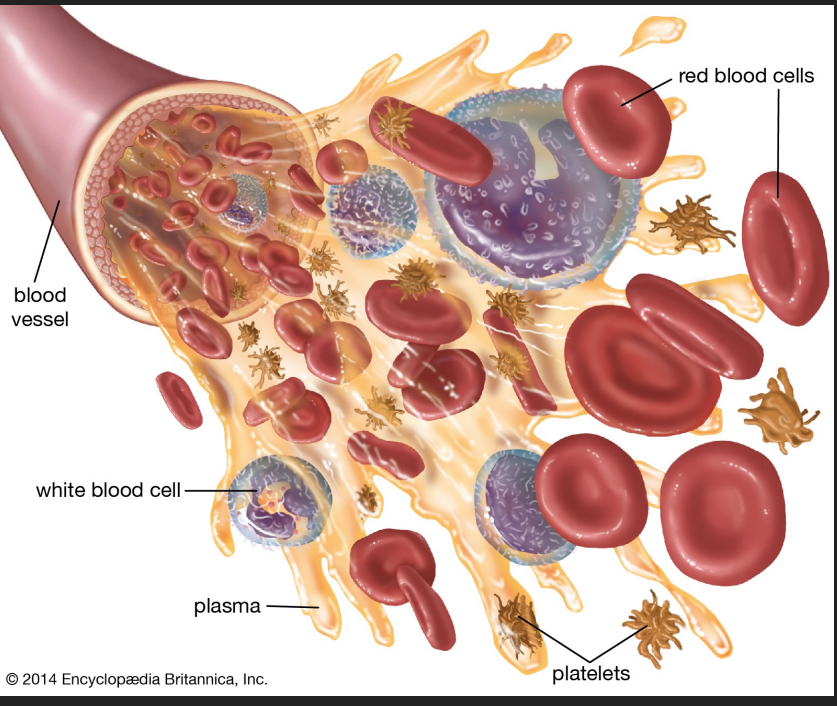
Components of blood pt.1
Components of blood pt.2
General Properties of Whole Blood
-Fraction of body weight
- Volume
- Temperature
- pH
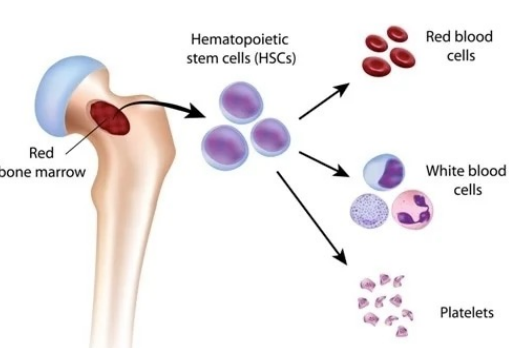
Hematopoiesis
Blood cell formation in red bone marrow
Hematopoietic stem cells (Hemocytoblasts)
• Give rise to all formed elements in blood
• Committed cells cannot change
Regulation of Erythropoiesis
Too few RBCs leads to tissue hypoxia
Too many RBCs increases blood viscosity
> 2 million RBCs made per second
Balance between RBC production and destruction depends on
• Hormonal controls
• Adequate supplies of iron, amino acids, and B vitamins
Hormonal Control of Erythropoiesis
Hormone Erythropoietin (EPO)
Direct stimulus for erythropoiesis
Always small amount in blood to maintain basal rate
• High RBC or O2 levels depress production
Released by kidneys (some from liver) in response to hypoxia
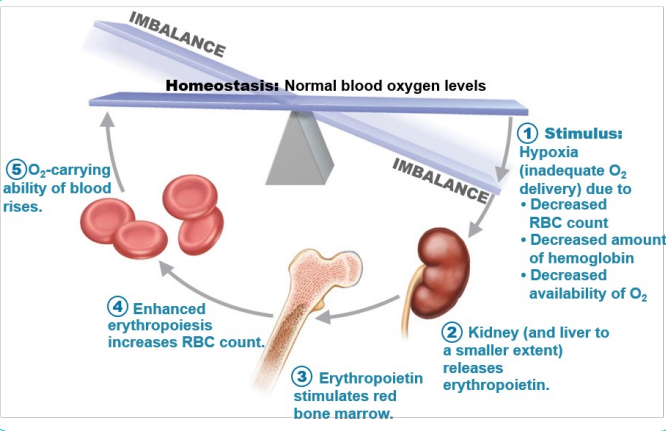
Causes of hypoxia
Decreased RBC numbers due to hemorrhage or increased destruction
Insufficient hemoglobin per RBC (e.g., iron deficiency)
Reduced availability of O2 (e.g., high altitudes)
Blood Oxygen Homeostasis
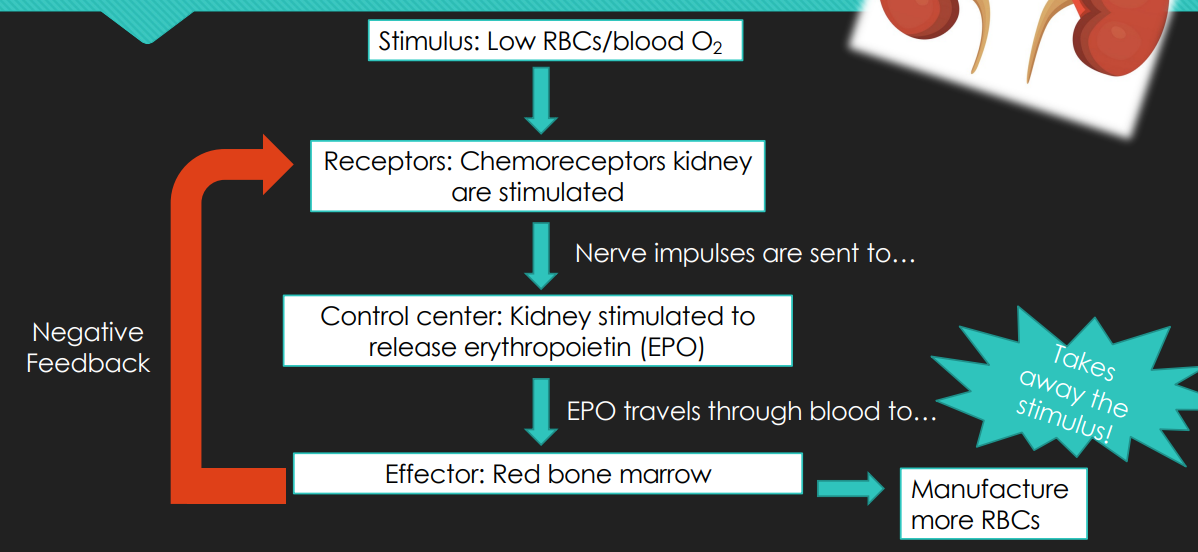
Hormonal Control of Erythropoiesis
Effects of EPO
• Rapid maturation of committed marrow cells
• Increased circulating reticulocyte count in 1–2 days
Some athletes abuse artificial EPO
• Dangerous consequences
Testosterone enhances EPO production, resulting in higher RBC counts in males

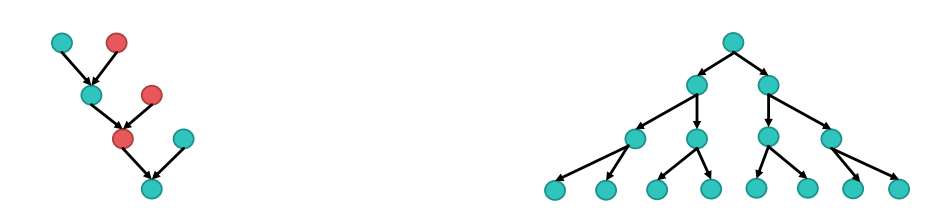
Sexual vs. Asexual Reproduction
Sexual
Pros: Genetic diversity
Cons: Egg must combine with sperm and so it takes twice as many cells
Asexual
Pros: No mate needed and makes many cells
Cons: No genetic diversity
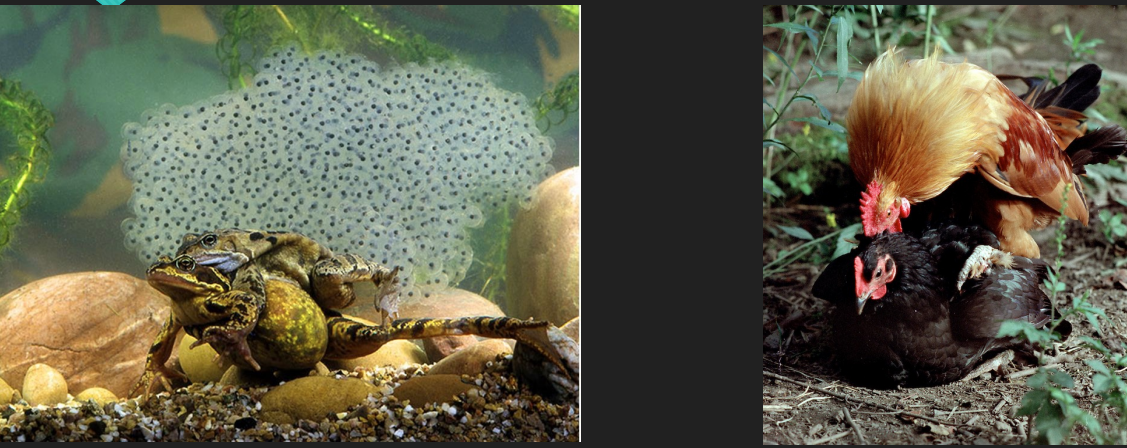
Methods of Fertilization
External fertilization - most aquatic
Internal fertilization - most terrestrial
Meiosis does not occur the same way in males and females. What differs?
Timing and end- product
Reproductive System
Primary sex organs (gonads): testes and ovaries
Produce sex cells (gametes) • Sperm – gametes in males • Ova(eggs) – gametes in females
Secrete steroid sex hormones • Androgens (males) • Estrogens and progesterone (females)
Accessory reproductive organs: ducts, glands, and external genitalia Sex hormones play roles in
Development and function of the reproductive organs
Sexual behavior and drives
Growth and development of many other organs and tissues
The Male Reproductive System
Testes:
Site of sperm production and testosterone synthesis
Epididymis:
Sperm storage and maturation
Vas Deferens:
Transports sperm from epididymis to urethra
Urethra:
Tube inside of penis transports sperm or urine exterior
Penis:
Organ of copulation
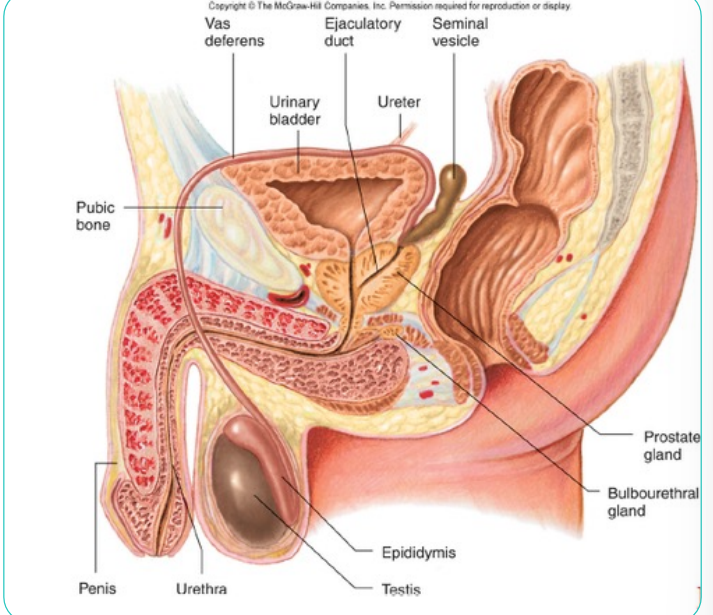
Biological Male Anatomy Recap
Sperm undergo spermatogenesis within the testes and become full fledged competent sperm upon completing spermiogenesis in the epididymis.
Tubes help to transport sperm outside of the body while glands produce secretions that are deposited into those tubes to add the other components of semen.
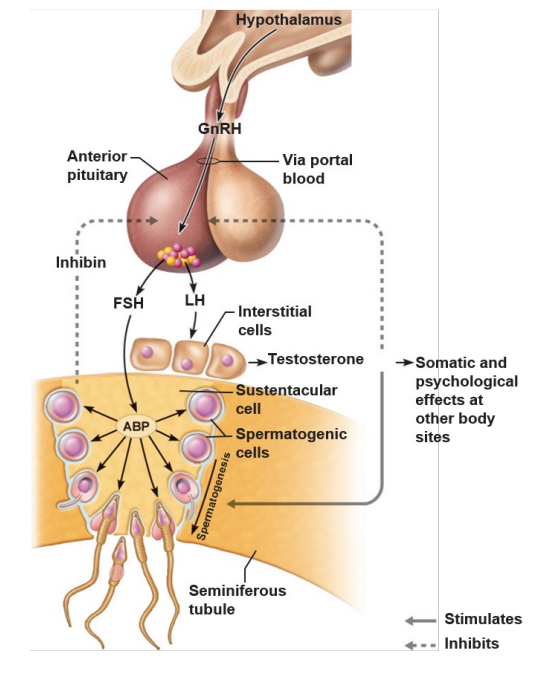
How do the testes know to make more sperm?
At puberty, the hypothalamus starts stimulating the pituitary to secrete gonad targeting hormones (LH and FSH).
o The testes respond to these hormones by producing testosterone which supports the maturation of sperm.
o This mechanism relies on negative feedback
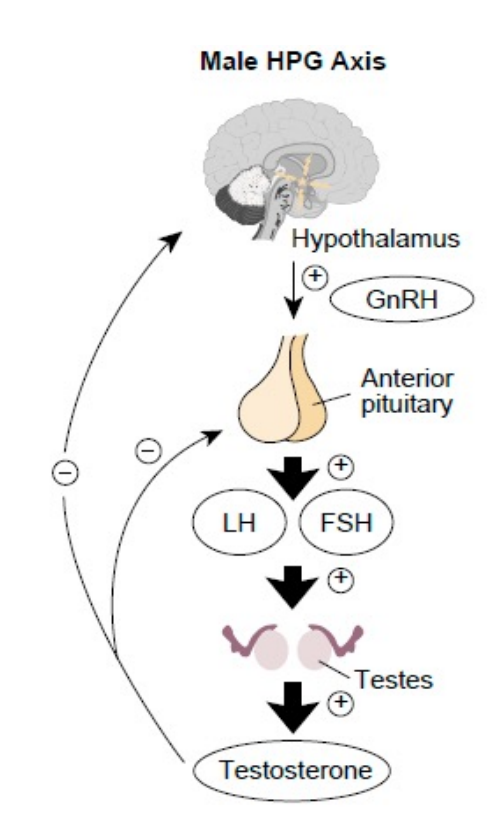
The Hypothalamic-Pituitary-Gonadal (HPG) Axis
o Hypothalamus secretes GnRH
o GnRH stimulates the anterior pituitary to secrete FSH and LH
o LH stimulates cells in the testes to release testosterone
o Testosterone is the final trigger for spermatogenesis
o FSH causes other cells to release androgen-binding protein (ABP), which makes spermatogenic cells receptive to testosterone
o Feedback inhibition on the hypothalamus and pituitary results from rising levels of testosterone and inhibin (released when sperm count is high)
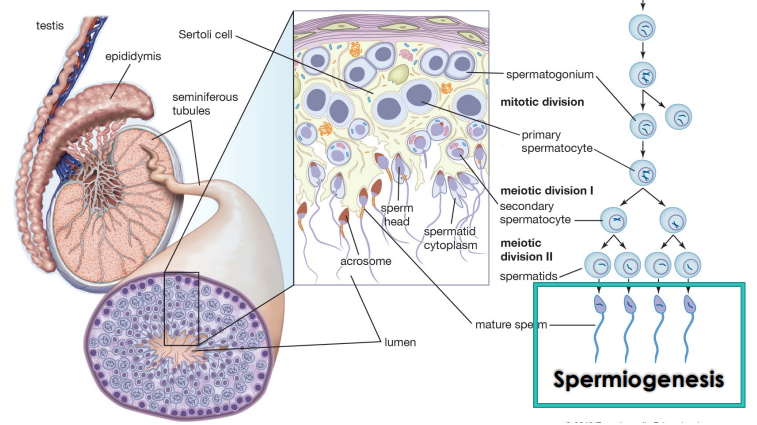
Spermatogenesis
Sperm acquire their fertilizing ability and forward motility properties during epididymal transit
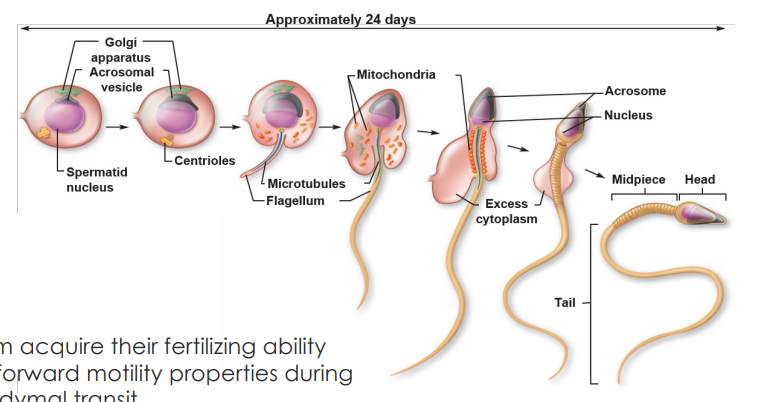
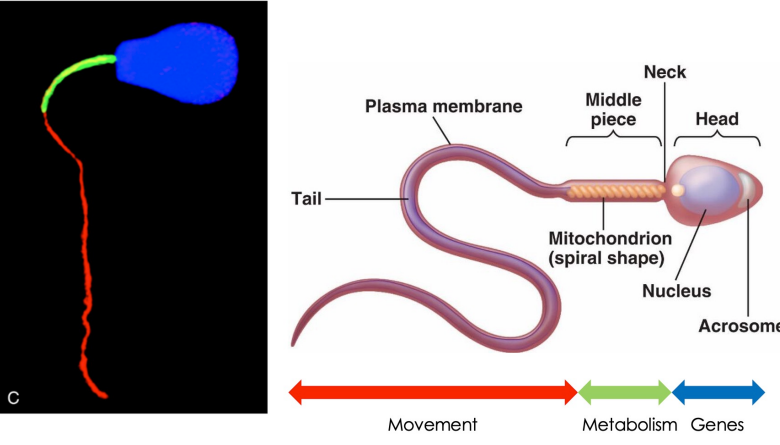
Sperm anatomy
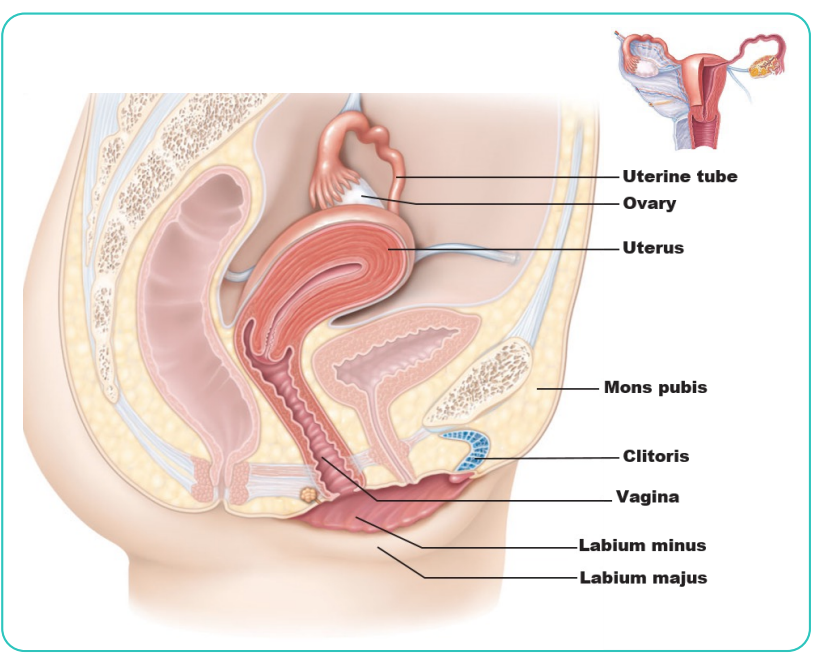
Female Reproductive System
Ovaries:
Produce egg
Fallopian tubes:
Site of fertilization Transport embryos to uterus
Uterus:
Site of embryonic development during gestation
Cervix:
Connects uterus and vagina Serve as barrier during pregnancy
Vagina:
Female organ of copulation at mating Birth canal
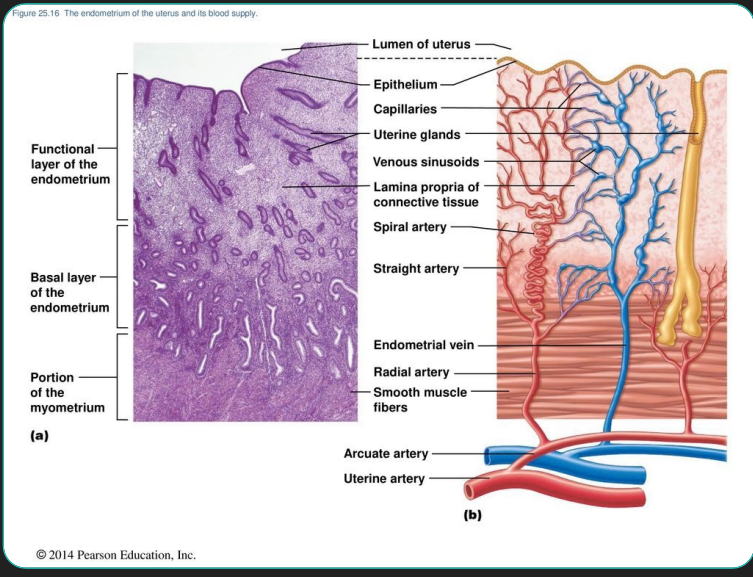
Uterine Wall
Three layers
1. Perimetrium: serous layer (visceral peritoneum)
2. Myometrium: interlacing layers of smooth muscle
3. Endometrium: mucosal linin
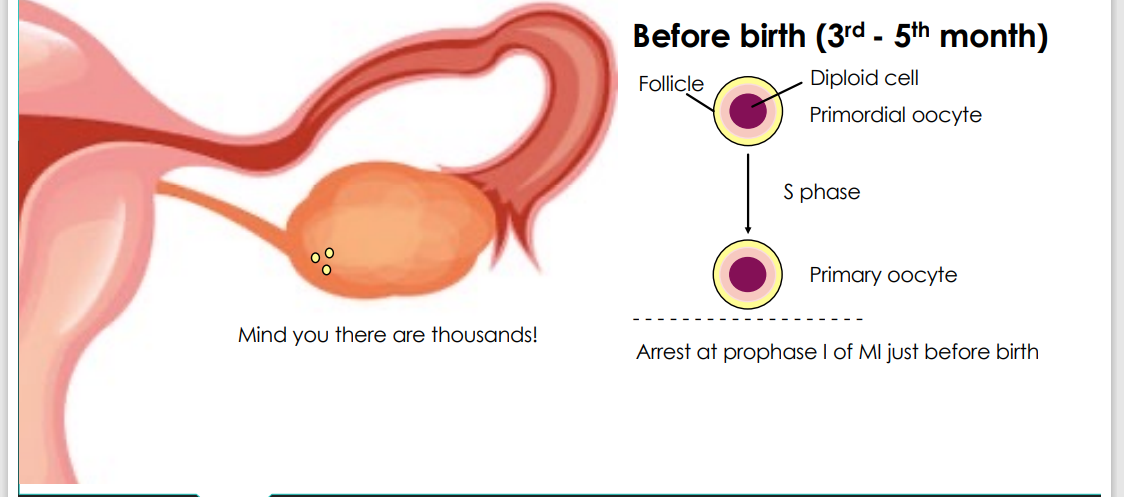
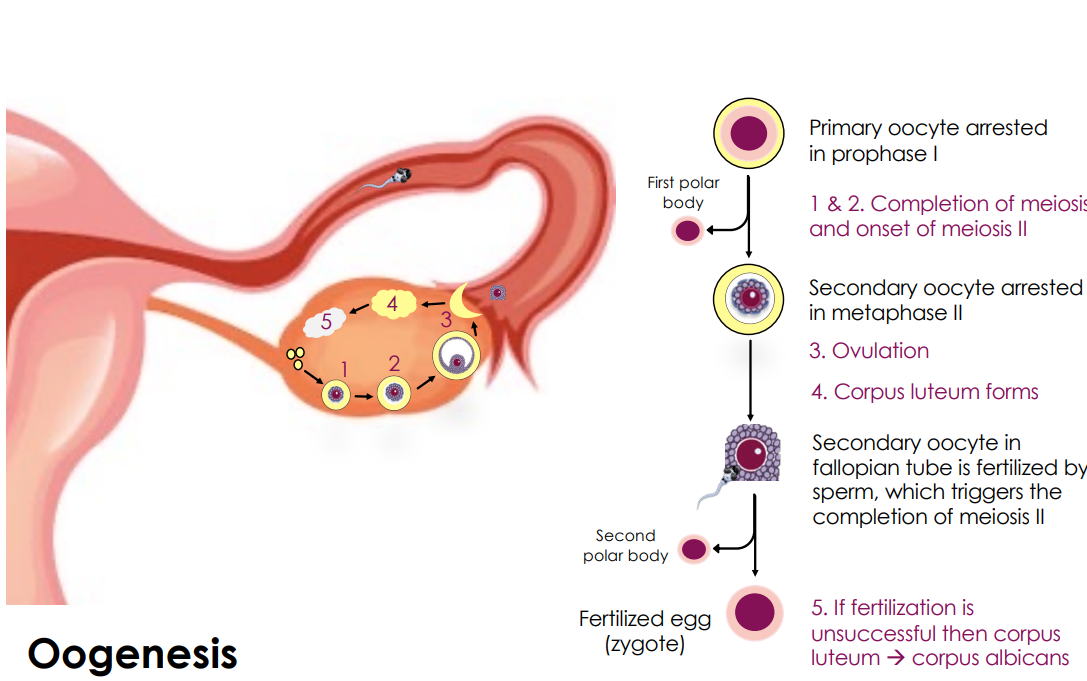
Before birth (3rd - 5th month)
At about 7 weeks gestation a human’s primordial germ cells are present and if the baby is a female they even start dividing before birth!
Follicles: ~ 6,000,000 at birth
Follicles: ~ 6,000,000 at birth, 180,000 at puberty and 1,000 at menopause
How do primary oocytes get to be fertilized eggs?
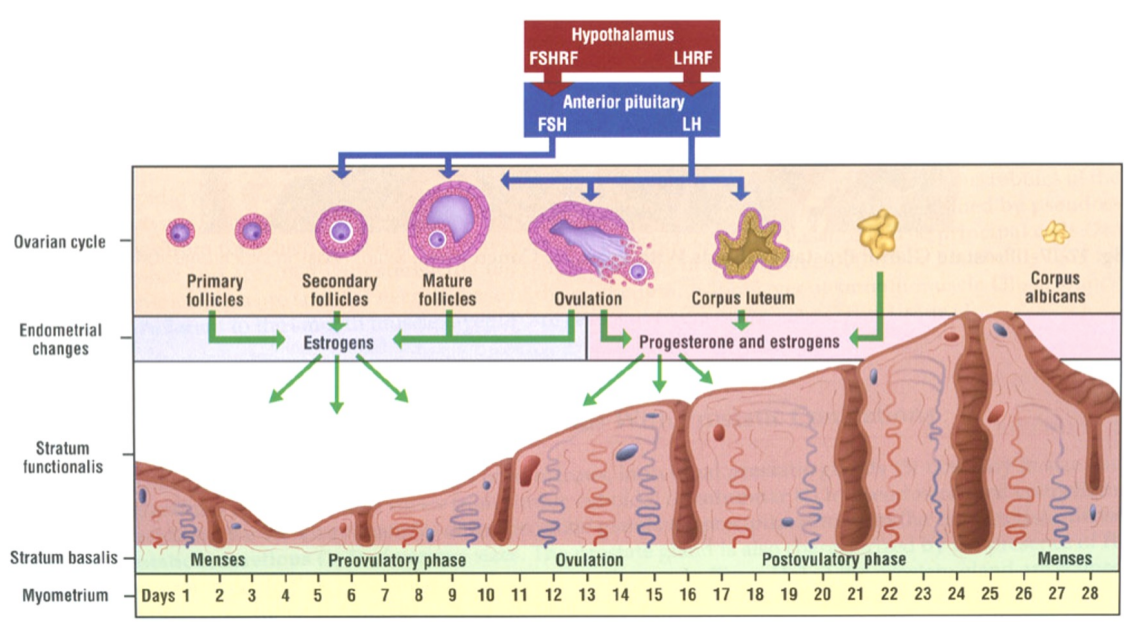
The Ovarian Cycle
What does the ovarian cycle entail?
Strongly linked to precise levels of the endocrine hormones
• GnRH, LH, FSH, Estrogen, Progesterone, HCG
Typically cycles through about every 28 days
Phases within the cycle
• Follicular Phase • Ovulation • Luteal Phase
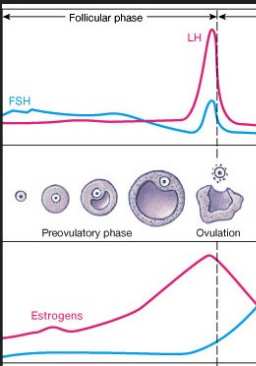
The Follicular Phase (Day 1-14)
Hypothalamus stimulated to secrete GnRH in response to low estrogen levels.
FSH and LH are secreted from the anterior pituitary.
Follicle cells begin to multiply around the developing oocyte.
• Produce and release estrogen
• Negatively feedback to hypothalamus and anterior pituitary
• Cause uterine lining to thicken

Ovulation – Day 14
High enough levels of estrogen positively feedback to the hypothalamus and anterior pituitary to secrete a surge of LH.
This surge stimulates ovulation of the oocyte.
Luteal Phase (Day 14-28)
Remaining follicle cells become the corpus luteum .
Corpus luteum secretes progesterone and a small level of estrogen.
• Promotes maintenance of the endometrium
As progesterone and estrogen build, they inhibit the release of FSH and LH from the pituitary

To Fertilize or Not to Fertilize
The cycle can conclude in one of two ways.
Option 1: If a sperm is present and fertilization occurs, hCG is produced and keeps the corpus luteum alive.
Option 2: Lack of fertilization causes the corpus luteum to deteriorate and thus decrease the levels of estrogen and progesterone.
• This causes the endometrial lining to shed à menstruation
Hormonal Regulation of Uterine Cycle
(1) PROLIFERATIVE PHASE concurrent with follicular maturation and influenced by estrogens (2) SECRETORY PHASE concurrent with luteal phase and influenced by progesterone (3) MENSTRUAL PHASE commences as hormone production by corpus luteum declines
Oogenesis
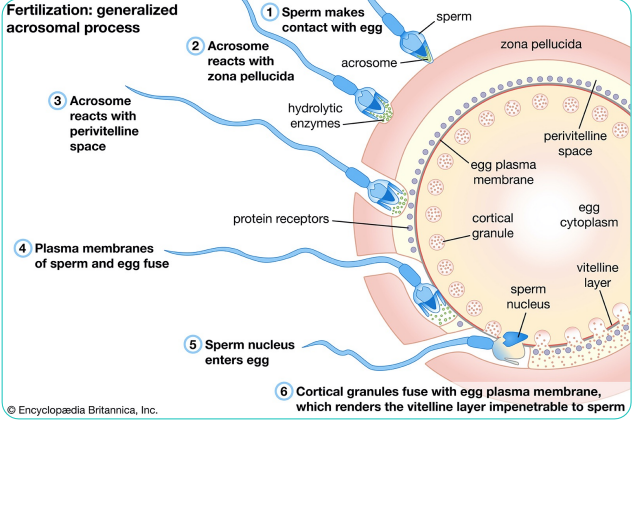
Fertilization in More Detail
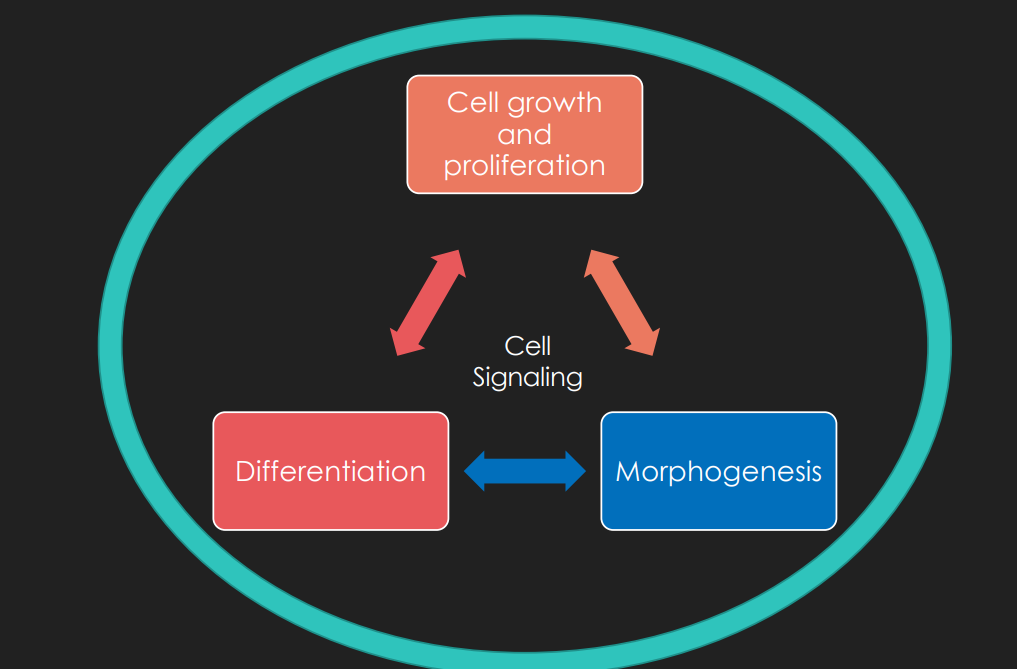
What is development?
1. Cell growth and proliferation
2. Differentiation
3. Morphogenesis
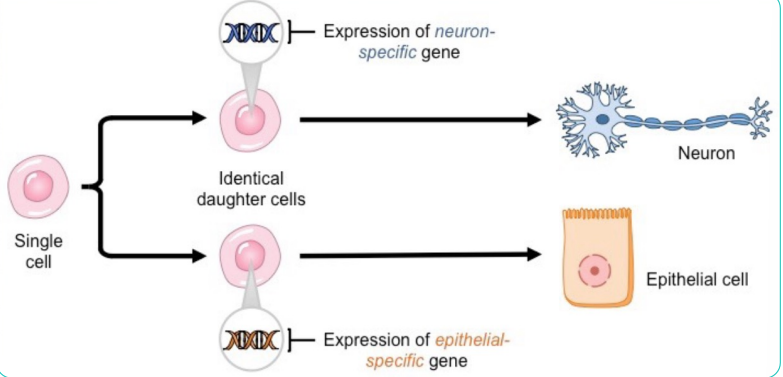
Differentiation
What type of cell will a cell become
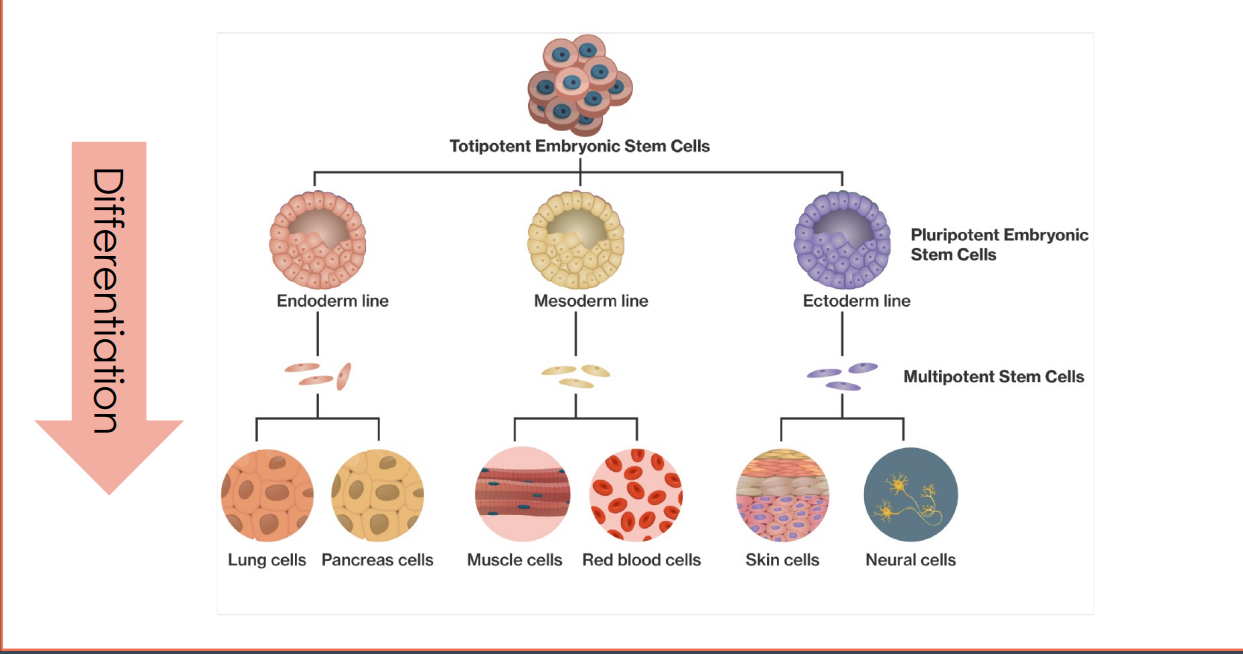
What causes cells to differentiate into certain types?
Remember! All cells have the same genes. So what differs is not their genetic makeup, but rather their gene expression
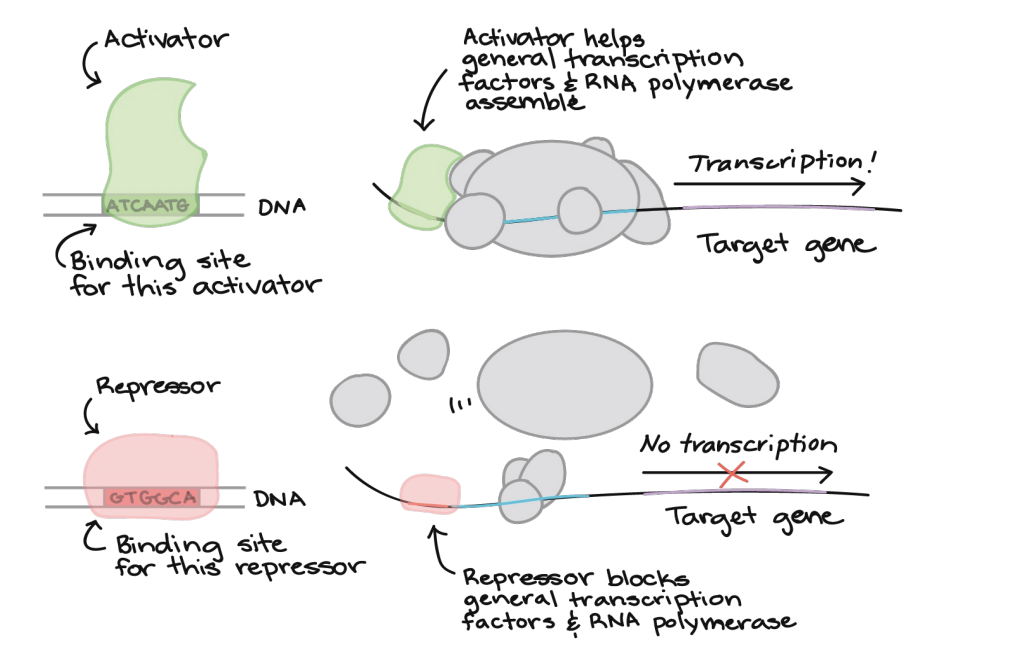
Transcription Factors
include a wide number of proteins, excluding RNA polymerase, that initiate and regulate the transcription of genes
What causes cells to differentiate into certain types?
Neuron specific transcription factors
Epithelial specific transcription factors
Brain specific transcription factors
Eye specific transcription factors
Ear specific transcription factors
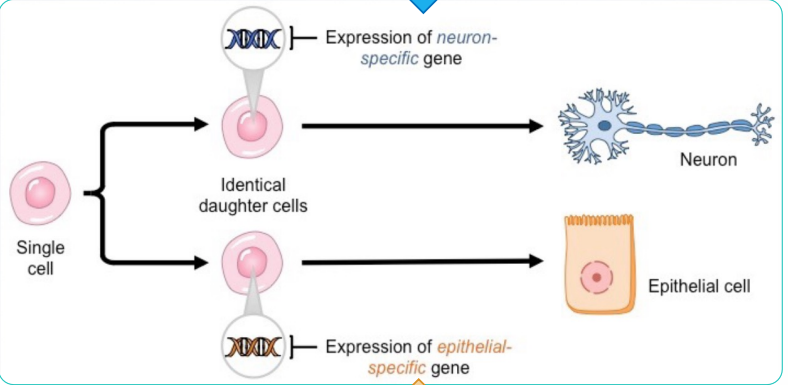
Differentiation Conclusions
Throughout differentiation, the specialization of a cell becomes increasingly more fixed.
Differentiation is a consequence of differential gene expression and is controlled by transcription factors.
Differentiation is, in general, irreversible
Morphogenesis
o The process that causes an organism to develop its shape
o Ex: Neurons are made, but they need to take on the shape of the brain for the organ to function properly.
o Occurs in response to cell growth, proliferation and differentiation
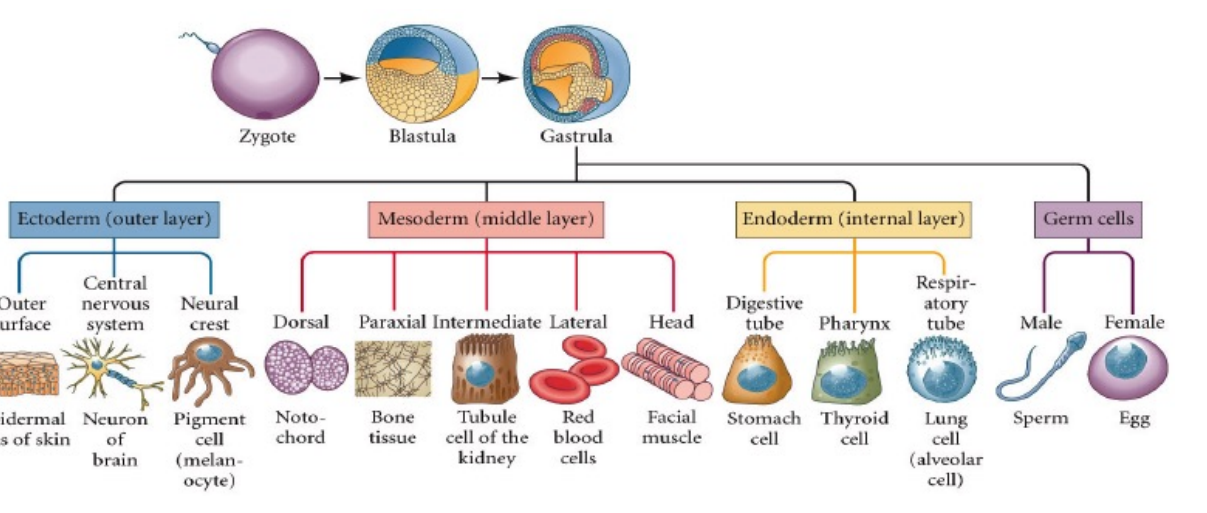
Embryogenesis
The formation and development of an embryo.
an early process of creating more cells from a zygote and differentiating them into three layers of cells
What are the 3 layers? Explain them
Ectoderm (outer layer)
Mesoderm (middle layer)
Endoderm (internal layer)
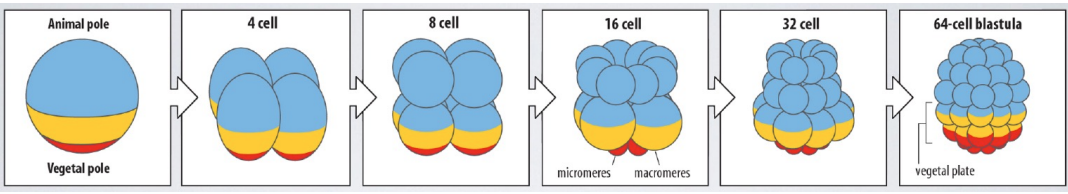
(Throughout cleavage, transcription factors that regulate gene expression of specific cell types are grouped together)
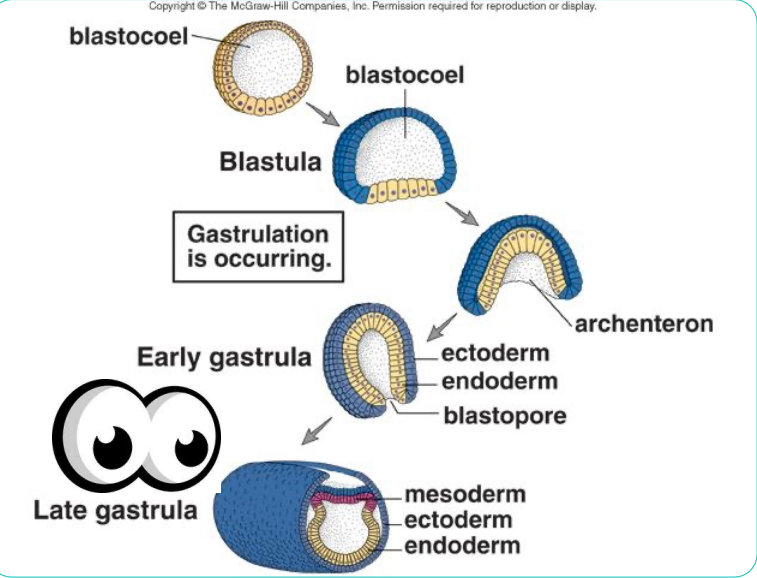
Gastrulation
an early developmental process in which an embryo transforms from a one-dimensional layer of epithelial cells, a blastula, and reorganizes into a multilayered and multidimensional structure called the gastrula
Somitogenesis
the process by which somites form. Somites are bilaterally paired blocks of paraxial mesoderm that form along the anterior-posterior axis of the developing embryo in segmented animals. In vertebrates, somites give rise to skeletal muscle, cartilage, tendons, endothelium, and dermis.
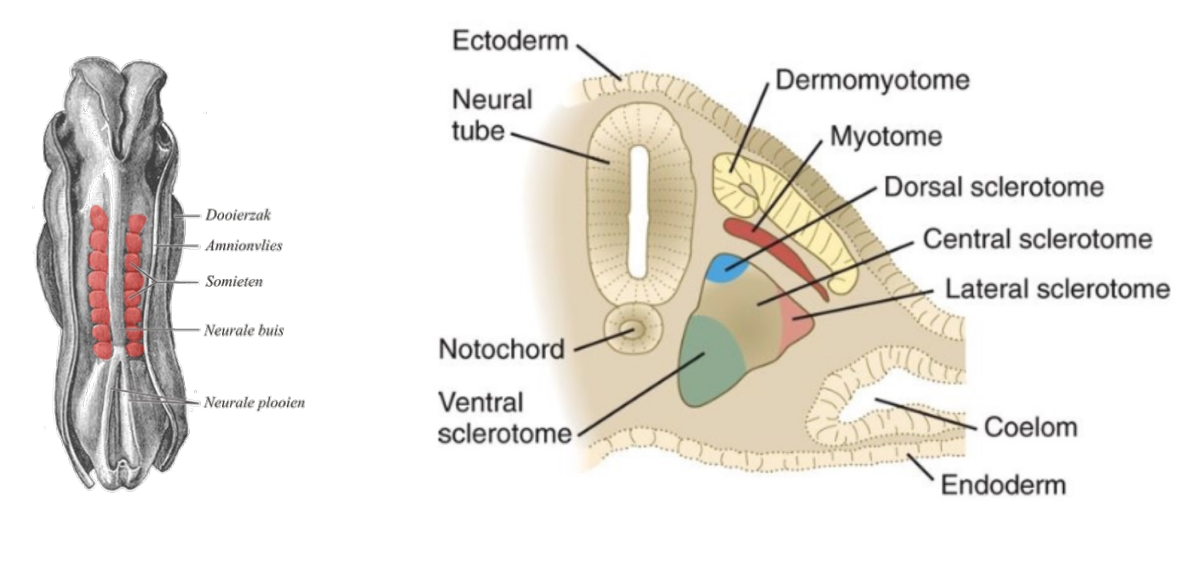
Somites
are a set of bilaterally paired blocks of mesoderm that form in the embryonic stage of somitogenesis, along the head-to-tail axis in segmented animals.

Homeotic Genes
Hox genes expressed in a distinctive pattern along the anterior-posterior axis after segments are established.
These genes code for regulatory transcription factors that trigger the production of segment-specific structures.
“Homeobox”: the site along the DNA where the transcription factors bind; very similar between different organisms
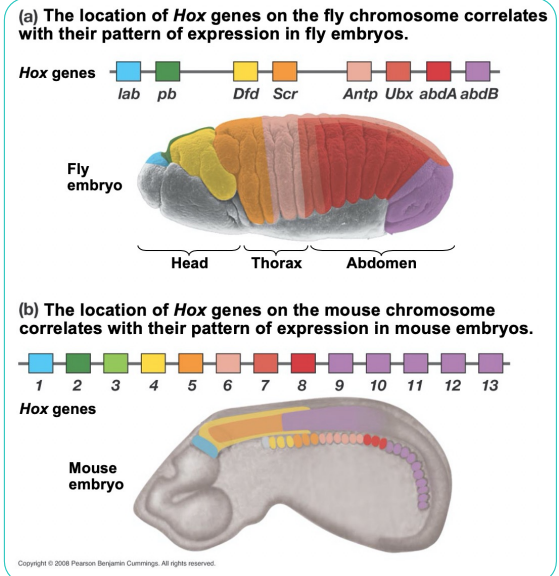
Hox gene key points:
o Hox genes are very very closely related in creatures as distinct as fruit flies and humans.
o This similarity implies a very ancient origin of these genes.
o Shifting the expression of these genes just a little, through alteration in transcription factors (enhancers and silencers) binding can lead to the development of new forms.
o This shift in developmental expression is now thought to be a key factor in evolutionary change
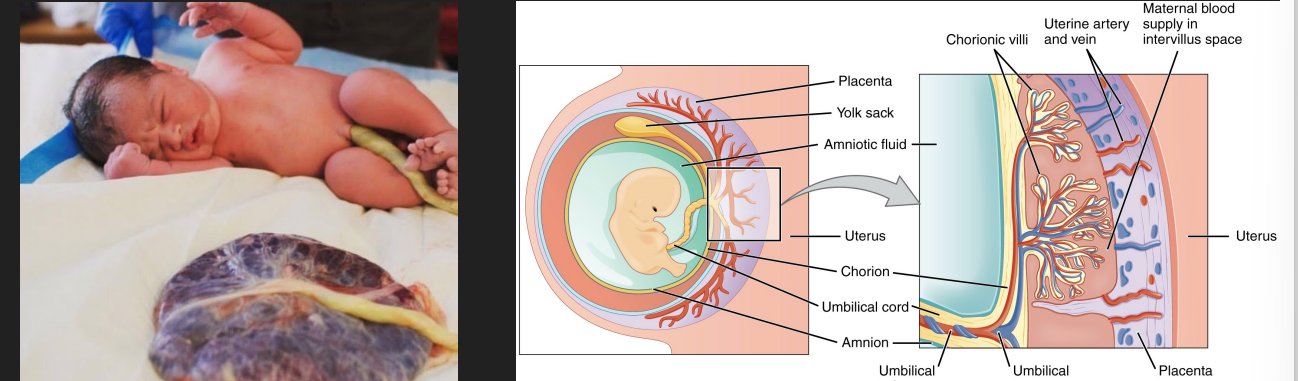
The Placenta
Nutritive and waste-removal structure seen in placental mammals
Allows for exchange between mother and baby bloodstreams by transport processes (e.g. diffusion and active transport)
Secretes estrogen and progesterone to support pregnancy and prepare mammary glands for lactation
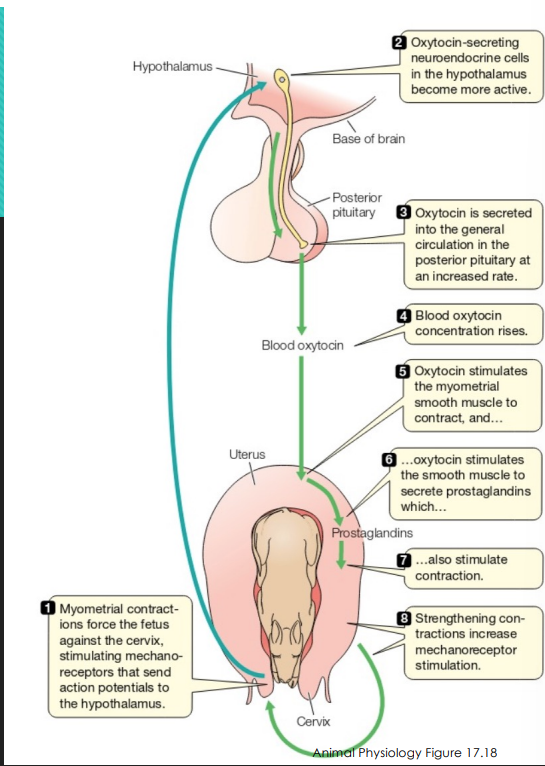
Birth
Estrogen rises to prepare myometrium to contract by manufacturing gap junctions and making myometrial cells receptive to oxytocin
Oxytocin and prostaglandins strongly stimulate smooth muscle contraction Mechanoreceptor stimulation of cervix stimulates birthing process
Positive feedback mechanism
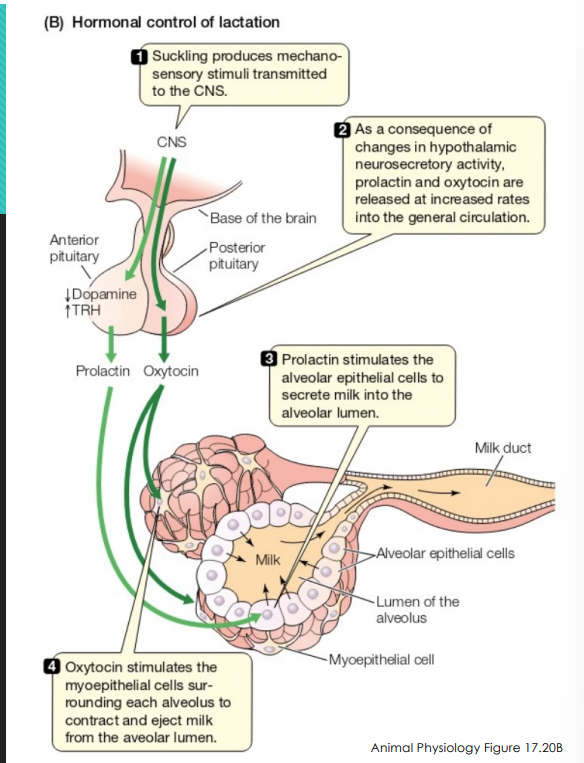
Lactation
Positive feedback mechanism
• Suckling increases prolactin and oxytocin secretion
Prolactin stimulates milk secretion, while oxytocin causes milk let-down
When not pregnant, dopamine inhibits lactation
When lactating, GnRH release is suppressed
• Lactation anestrus/anovulation
Galactorrhea
Discharge of milk or a milk-like secretion from the breast in the absence of parturition or beyond six months' post-partum.
Medications, such as certain sedatives, antidepressants, antipsychotics and high blood pressure drugs. Opioid use. Herbal supplements, such as fennel, anise or fenugreek seed.
Treatment with a low-dose dopamine agonist